The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Reproductive Biotechnology interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Reproductive Biotechnology Interview
Q 1. Describe the process of in-vitro fertilization (IVF).
In-vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child. It involves retrieving eggs from the ovaries and fertilizing them with sperm in a laboratory. The fertilized egg (embryo) is then transferred to the uterus.
- Ovarian Stimulation: Medications are used to stimulate the ovaries to produce multiple mature eggs. This is crucial as not all eggs will be successfully fertilized.
- Egg Retrieval: A minor surgical procedure uses ultrasound guidance to retrieve the mature eggs from the ovaries.
- Fertilization: The eggs are mixed with sperm in a petri dish, allowing fertilization to occur naturally. Alternatively, Intracytoplasmic Sperm Injection (ICSI) can be used, where a single sperm is directly injected into the egg. ICSI is particularly useful when sperm count is low or sperm motility is poor.
- Embryo Culture: The fertilized eggs are incubated in a specialized environment that mimics the conditions of the fallopian tubes, allowing them to develop for several days.
- Embryo Transfer: After a few days, one or more embryos are carefully transferred into the woman’s uterus using a thin catheter. The number of embryos transferred depends on various factors, including the woman’s age and the quality of the embryos.
- Pregnancy Test: A pregnancy test is performed approximately two weeks after embryo transfer to confirm successful implantation.
For example, a couple struggling with unexplained infertility might opt for IVF. The process offers a chance to conceive despite difficulties with natural conception.
Q 2. Explain the role of assisted hatching in IVF.
Assisted hatching is an IVF procedure where a tiny hole is made in the zona pellucida, the outer shell of a fertilized egg (embryo). This is done to help the embryo ‘hatch’ from its shell and implant in the uterine lining. The zona pellucida can sometimes be abnormally thick or hardened, making it difficult for the embryo to break through and implant. Assisted hatching aims to improve the chances of successful implantation.
Several methods exist, including laser assisted hatching (LAH) which uses a laser to create a small opening, and mechanical assisted hatching, utilizing a special instrument to create a small break in the zona pellucida. The choice of method depends on factors like the embryo’s quality and the clinic’s preferences.
For instance, if an embryo has consistently failed to implant in previous IVF cycles, assisted hatching might be considered as a potential solution to improve its ability to implant.
Q 3. What are the different types of gamete intrafallopian transfer (GIFT)?
Gamete Intrafallopian Transfer (GIFT) is a fertility treatment where eggs and sperm are placed into a fallopian tube to allow fertilization to occur naturally in vivo. There are primarily two types:
- Conventional GIFT: In this method, both eggs and sperm are collected and transferred directly into the fallopian tube. Fertilization takes place naturally within the fallopian tube.
- Pro-nuclear GIFT (or pronuclear GIFT): This is a less common variation. The eggs are fertilized in vitro and then the resulting zygotes (single-celled embryos) are transferred to the fallopian tube. This essentially combines elements of IVF and GIFT.
GIFT is less frequently used compared to IVF now because it requires laparoscopy (a small surgical incision), and the success rates are lower than IVF, as the natural fertilization process within the fallopian tubes is less controlled.
Q 4. Describe the process of preimplantation genetic testing (PGT).
Preimplantation Genetic Testing (PGT) is a procedure used to screen embryos for genetic abnormalities before they are implanted in the uterus during IVF. This helps select embryos that are likely to be free from certain genetic conditions. There are several types of PGT:
- PGT-A (Aneuploidy): Tests for abnormal chromosome number in the embryo. This is relevant as aneuploidy (extra or missing chromosomes) is a leading cause of miscarriage and birth defects.
- PGT-M (Monogenic): Screens for specific gene mutations that cause inherited genetic disorders (e.g., cystic fibrosis, Huntington’s disease). This is usually employed when parents carry a gene for a specific disease.
- PGT-SR (Structural Rearrangements): Detects chromosomal translocations and inversions, that may lead to unbalanced chromosome complements in the offspring.
In PGT, a single cell or a small number of cells are removed from the embryo for genetic analysis. Only embryos that are genetically normal are transferred to the uterus. For example, a couple with a family history of a specific genetic disease might opt for PGT-M to ensure their child is not affected.
Q 5. What are the ethical considerations surrounding reproductive biotechnology?
Reproductive biotechnology raises several significant ethical considerations:
- Embryo Selection and Disposal: The creation and selection of embryos raise questions about the moral status of embryos and the ethical implications of discarding or destroying embryos that are deemed unsuitable.
- Genetic Engineering: Concerns exist regarding the potential for designer babies and the societal impacts of altering the human genome through technologies like gene editing.
- Access and Equity: The high cost of reproductive technologies creates significant equity issues, making them inaccessible to many individuals and families.
- Safety and Risks: The potential risks associated with these procedures, both for the mother and the child, are a vital consideration.
- Surrogacy: Ethical questions surrounding commercial surrogacy involve exploitation, parental rights, and the well-being of the surrogate mother.
These dilemmas necessitate careful consideration of the ethical, social, and legal frameworks within which reproductive biotechnology operates. Ongoing public debate and regulatory oversight are crucial to ensure responsible use of these powerful technologies.
Q 6. Explain the principles of cryopreservation for gametes and embryos.
Cryopreservation, or freezing, is a crucial technique in reproductive biotechnology that allows for the preservation of gametes (sperm and eggs) and embryos for future use. The process involves a controlled slow-freezing procedure which minimizes ice crystal formation that would damage the cells. Vitrification, a newer method, involves rapidly cooling the cells to extremely low temperatures, reducing ice crystal formation.
Principles:
- Slow Freezing (conventional cryopreservation): Involves a gradual reduction in temperature using cryoprotective agents (CPAs) to prevent ice crystal formation that damages the cells. CPAs are chemicals added to the cell suspension that protect the cells from ice crystal damage.
- Vitrification: A rapid freezing method that bypasses ice crystal formation by plunging the cells into a cryoprotective agent solution at ultra-low temperatures. This approach is associated with higher survival rates in many cases.
- Thawing: The frozen gametes or embryos are thawed rapidly to restore them to their normal temperature and state.
Cryopreservation allows couples to preserve their fertility options, undergo multiple IVF cycles with fewer retrievals, and improve the success rate by selecting the best embryos for transfer from a frozen batch.
Q 7. What are the common causes of male infertility?
Male infertility, the inability to conceive a child, can stem from various factors:
- Low Sperm Count (Oligospermia): Insufficient number of sperm in the ejaculate.
- Poor Sperm Motility (Asthenospermia): Sperm have reduced ability to move effectively toward the egg.
- Abnormal Sperm Morphology (Teratospermia): Sperm have unusual shapes or structures, impacting their ability to fertilize an egg.
- Varicocele: Enlarged veins in the scrotum that increase testicular temperature, affecting sperm production.
- Hormonal Imbalances: Problems with testosterone or other hormones can affect sperm production.
- Genetic Factors: Genetic conditions or chromosomal abnormalities can lead to impaired sperm production.
- Obstructions: Blockages in the reproductive tract prevent sperm from reaching the ejaculatory duct.
- Infections: Infections like epididymitis or prostatitis can damage the reproductive system and affect sperm quality.
- Lifestyle Factors: Smoking, excessive alcohol consumption, drug use, and obesity can negatively impact sperm production and function.
Diagnosing the cause of male infertility usually involves a semen analysis and a comprehensive evaluation of the male reproductive system. Treatment options vary depending on the underlying cause and may include lifestyle changes, medication, surgery, or assisted reproductive technologies like IVF with ICSI.
Q 8. What are the common causes of female infertility?
Female infertility, the inability to conceive after a year of unprotected intercourse, stems from a variety of factors. These can broadly be categorized into issues with ovulation, fallopian tubes, uterus, or cervix, as well as overall reproductive health.
- Ovulatory Disorders: Conditions like Polycystic Ovary Syndrome (PCOS), premature ovarian failure, and hormonal imbalances can disrupt or prevent ovulation – the release of an egg from the ovary. Think of it like a car’s engine not firing – no egg, no pregnancy.
- Fallopian Tube Problems: Blockages in the fallopian tubes, often due to infections like pelvic inflammatory disease (PID) or endometriosis, prevent the sperm from reaching the egg or the fertilized egg from reaching the uterus. Imagine a blocked highway – the egg or sperm can’t reach their destination.
- Uterine Factors: Conditions like uterine fibroids (benign tumors) or polyps can interfere with implantation of the fertilized egg. This is like having a bumpy road preventing the car from settling smoothly.
- Cervical Issues: Cervical stenosis (narrowing of the cervix) or cervical mucus abnormalities can hinder sperm passage. This is similar to a gate being too narrow for the car to pass through.
- Other Factors: Age (diminished egg quality and quantity with advancing age), endometriosis (growth of uterine tissue outside the uterus), autoimmune disorders, and unexplained infertility also play significant roles.
Diagnosis typically involves a comprehensive evaluation, including blood tests, ultrasound scans, and potentially laparoscopy (a minimally invasive surgical procedure).
Q 9. Describe different methods for sperm selection and preparation.
Sperm selection and preparation are crucial steps in assisted reproductive technologies (ART) like IVF, significantly impacting the success rate. The goal is to obtain a highly concentrated sample of motile (moving), morphologically normal (healthy-shaped), and viable (alive) sperm.
- Density Gradient Centrifugation: This is a common method. Sperm are layered onto a density gradient medium, and centrifugation separates the healthy, motile sperm from the seminal fluid and debris. Think of it like separating gold from sand using its density – the heavier, healthier sperm sink to the bottom.
- Swim-up Technique: Sperm are allowed to ‘swim up’ into a medium, leaving behind less motile sperm and debris. This is a simpler technique compared to density gradient centrifugation, but it may not be as effective in selecting the best sperm.
- Sperm Sorting (Microsort): This technique uses fluorescence-activated cell sorting (FACS) to separate X-chromosome-bearing sperm (which lead to female offspring) from Y-chromosome-bearing sperm (which lead to male offspring). It’s used for sex selection for medical reasons or personal preference, although ethical considerations are often debated.
- Intracytoplasmic Sperm Injection (ICSI): This is a specialized technique used when there is severe male factor infertility. A single sperm is directly injected into an egg, bypassing the need for fertilization to occur naturally. It is quite successful and can help couples facing severe sperm problems to achieve pregnancy.
Post-selection, sperm are typically prepared in a specialized culture medium to optimize their survival and fertilization capacity. This ensures the sperm are in top condition when used for insemination or ICSI.
Q 10. Explain the role of hormone replacement therapy in IVF cycles.
Hormone replacement therapy (HRT) in IVF cycles plays a vital role in preparing the uterine lining (endometrium) for embryo implantation. It mimics the natural hormonal changes that occur during the menstrual cycle to create a receptive environment for the embryo.
In IVF, a woman’s natural hormonal cycle is suppressed using medications, then controlled hormone stimulation is done to produce multiple eggs. Once the eggs are retrieved and fertilized, the HRT helps to synchronise the endometrial development with the timing of embryo transfer. Without HRT, the uterus may not be sufficiently prepared to receive and support the developing embryo. Think of HRT as preparing the ‘soil’ for planting the ‘seed’ (embryo).
Typical HRT involves the use of estrogen and progesterone. Estrogen stimulates the growth of the endometrium, while progesterone helps to maintain the lining in a receptive state. Dosage and timing are carefully monitored through blood tests and ultrasound scans to optimize endometrial thickness and receptivity.
Q 11. What are the different types of ovarian stimulation protocols?
Ovarian stimulation protocols in IVF aim to induce the development of multiple mature follicles (fluid-filled sacs containing eggs) in the ovaries. Several protocols exist, each tailored to the patient’s individual characteristics and reproductive history.
- Long Protocol: This involves suppressing the natural hormone production using GnRH agonists (like Lupron) for several weeks before starting stimulation with gonadotropins (FSH and LH). This provides a controlled start to the stimulation, giving better control over the number of follicles.
- Short Protocol: This uses a shorter period of GnRH agonist suppression, typically only a few days, before starting gonadotropin stimulation. It’s less time-consuming than the long protocol, making it a popular choice.
- Antagonist Protocol: This protocol uses a GnRH antagonist (like Cetrotide) to prevent premature ovulation. The antagonist is added once the follicles reach a certain size, providing a fine-tuned control of the stimulation.
- Microdose Flare Protocol: This involves a low dose of GnRH agonist given for a short period to encourage better ovarian response in patients with poor ovarian reserve.
The choice of protocol depends on factors like age, ovarian reserve (the number of remaining eggs), and previous IVF outcomes. A reproductive endocrinologist selects the protocol best suited for each patient.
Q 12. How is embryo quality assessed?
Embryo quality assessment is crucial in IVF, as it directly impacts the chances of successful implantation and pregnancy. Assessment is performed using a combination of morphological criteria (visual appearance) and sometimes advanced techniques.
- Morphology: Embryologists examine the embryo’s appearance under a microscope, looking at factors like the number of cells, fragmentation (cell debris), symmetry, and the presence of a blastocyst cavity (a fluid-filled cavity that develops in the embryo). A high-quality embryo is typically characterized by a large number of cells, minimal fragmentation, and good symmetry.
- Time-lapse Imaging: This advanced technique uses automated imaging systems to monitor the embryo’s development over time, providing detailed information about its growth kinetics. This can help identify embryos with superior developmental potential.
- Preimplantation Genetic Testing (PGT): PGT involves analyzing the embryo’s genetic material to identify chromosomal abnormalities or specific gene mutations before implantation. This can help reduce the risk of miscarriage or genetic disorders.
The selection of an embryo for transfer is based on a holistic evaluation of its morphological features and potentially genetic information, aiming to select the embryo with the highest chance of implantation and resulting in a healthy pregnancy.
Q 13. Describe the different methods of embryo transfer.
Embryo transfer is the process of placing the selected embryo(s) into the uterus. Different methods exist, mainly differing in the stage of embryo development at the time of transfer.
- Cleavage-stage embryo transfer: This involves transferring embryos that are at the early stages of development (typically day 2 or 3), before the blastocyst stage.
- Blastocyst transfer: This involves transferring embryos that have reached the blastocyst stage (day 5 or 6), a more advanced stage of development. Blastocysts have a higher implantation potential than cleavage-stage embryos, but not all embryos make it to this stage.
The procedure itself is minimally invasive. The embryos are loaded into a thin catheter, which is gently passed through the cervix and into the uterine cavity. Ultrasound guidance is commonly used to ensure accurate placement of the catheter and embryos. The entire process is usually painless or minimally uncomfortable.
Q 14. What are the potential risks and complications associated with IVF?
IVF, while highly effective for many couples, carries potential risks and complications. It’s crucial for patients to be fully aware of these before proceeding.
- Ovarian Hyperstimulation Syndrome (OHSS): This is a potentially serious complication characterized by ovarian enlargement and fluid accumulation. It occurs when the ovaries overrespond to stimulation medications. Symptoms can range from mild discomfort to severe abdominal pain and shortness of breath, requiring hospitalization in severe cases.
- Multiple Pregnancy: IVF often results in multiple pregnancies (twins, triplets, etc.) due to the transfer of multiple embryos. This increases the risk of complications during pregnancy and delivery.
- Ectopic Pregnancy: In rare cases, the fertilized egg implants outside the uterus, often in the fallopian tube (ectopic pregnancy), which can be life-threatening.
- Miscarriage: The risk of miscarriage is slightly higher in IVF pregnancies compared to naturally conceived pregnancies.
- Infection: There’s a small risk of infection at the puncture site during egg retrieval.
- Emotional Distress: The IVF process can be emotionally and psychologically taxing for couples.
These risks are managed by careful monitoring and appropriate medical interventions. Open communication between the patient and the healthcare team is essential to minimize these risks and ensure a successful outcome.
Q 15. What are the legal and regulatory aspects of reproductive biotechnology?
The legal and regulatory landscape of reproductive biotechnology is complex and varies significantly between countries. It’s governed by a combination of national laws, ethical guidelines, and professional standards. Key areas include informed consent, ensuring patient privacy (HIPAA in the US, GDPR in Europe), regulations surrounding gamete donation and surrogacy, genetic testing regulations, and the licensing and accreditation of clinics and laboratories. For example, many jurisdictions have strict rules about embryo selection and disposal, often limiting the number of embryos that can be implanted or requiring specific criteria for freezing or discarding embryos. Similarly, regulations on genetic screening often dictate what tests can be performed and how results are communicated to patients. These regulations aim to balance the advancement of reproductive technologies with ethical considerations and the protection of patient rights.
Clinics must adhere to stringent quality control measures and are often subject to regular inspections to ensure compliance. Non-compliance can lead to hefty fines, license revocation, and legal action. Staying updated on these ever-evolving regulations is crucial for anyone working in this field.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you troubleshoot issues related to fertilization failure?
Troubleshooting fertilization failure involves a systematic approach, starting with a thorough review of all aspects of the process. This includes assessing the quality of the gametes (sperm and eggs). We’d examine sperm parameters like motility, morphology, and concentration using sophisticated analysis techniques. For the oocytes, we’d look at maturity, morphology and assess the presence of any cytoplasmic abnormalities. The fertilization medium’s composition and incubation conditions are critically examined, and the timing of insemination or ICSI (intracytoplasmic sperm injection) is reviewed.
If the problem seems to be with the oocytes, we might investigate hormonal profiles of the female patient to understand if there were any underlying issues affecting oocyte maturation. If the sperm is the problem, we might suggest further investigations into the male patient’s reproductive health. In cases of recurrent fertilization failure, advanced diagnostic tests such as genetic testing might be considered to rule out any chromosomal abnormalities. It’s a collaborative process involving close communication with the embryologists, andrologists, and reproductive endocrinologists to pinpoint the cause and develop a personalized solution for the couple.
Q 17. How do you monitor embryo development in the lab?
Embryo development monitoring in the lab involves regular observation under a time-lapse microscope. This non-invasive technique allows us to capture images at regular intervals, providing a detailed record of cleavage (cell division) patterns, morphological characteristics (e.g., fragmentation, symmetry), and overall embryo quality. Time-lapse imaging provides significantly more data compared to traditional methods, where embryos are viewed only at limited time points.
We look for key developmental milestones, such as the timing of the first and subsequent cleavages, the appearance of blastomeres (embryonic cells), and the formation of the blastocyst (a hollow ball of cells). Software analysis can help to quantify embryo parameters objectively, assisting in selecting the embryos with the highest potential for implantation. This data is crucial for the embryologist to select the best embryos for transfer or cryopreservation, significantly improving the chances of a successful pregnancy. The time-lapse system also provides valuable information for research purposes, aiding in the understanding of developmental processes and the identification of biomarkers predicting embryo viability.
Q 18. Explain the importance of quality control in a reproductive biology lab.
Quality control in a reproductive biology lab is paramount, as it directly impacts the success rate of assisted reproductive technologies (ART) and the safety of patients. It’s a multi-faceted approach encompassing every aspect of the laboratory, from personnel training to equipment calibration and reagent quality. We adhere to strict protocols to minimize contamination risks, validate the performance of all equipment, regularly monitor media quality, and maintain meticulous records.
For instance, we conduct regular sterility testing of media and equipment using bacterial and fungal cultures. We employ stringent cleaning and sterilization protocols, including autoclaving, UV irradiation, and the use of HEPA-filtered laminar flow hoods. Regular internal audits and external proficiency testing are conducted to ensure compliance with national and international standards, such as ISO 15189 and CAP. Comprehensive quality control not only ensures the accuracy and reliability of results but also fosters a culture of excellence that enhances patient safety and clinical outcomes. It’s a continuous process of improvement and adaptation to emerging technologies and best practices.
Q 19. Describe different techniques used for sperm analysis.
Sperm analysis, or semen analysis, is crucial for evaluating male fertility. Several techniques are used, providing a comprehensive picture of sperm characteristics. The most basic involves a macroscopic evaluation assessing semen volume and viscosity. Microscopic analysis is essential, focusing on sperm concentration (number of sperm per milliliter), motility (percentage of moving sperm and their progressive movement), and morphology (the percentage of sperm with normal shape).
Advanced techniques such as computer-assisted semen analysis (CASA) provide objective and quantitative data on sperm motility parameters, reducing subjectivity. CASA systems automatically analyze sperm movement, providing detailed information on velocity, trajectory, and other kinematic parameters. Other sophisticated techniques, like flow cytometry, allow for the assessment of sperm DNA fragmentation, which is increasingly recognized as a major factor affecting fertility. Furthermore, tests for sperm viability (the percentage of live sperm) and acrosome reaction (a crucial step in fertilization) can be employed to gain a more comprehensive understanding of sperm function.
Q 20. How do you handle and manage patient samples effectively?
Handling and managing patient samples requires strict adherence to established protocols to maintain sample integrity and prevent contamination. Upon arrival in the lab, samples are immediately logged and their identity verified against patient records. Chain of custody is strictly maintained and documented throughout the entire process. Samples are stored under appropriate conditions; for example, sperm samples are often stored at room temperature or refrigerated, while oocytes require more stringent temperature control and specific culture media. Each step, from collection to disposal, is documented meticulously in a laboratory information system (LIS).
We employ strict identification systems, such as barcode scanning, to minimize the risk of sample misidentification. Our protocols include specific instructions for the handling of each sample type, including precautions to avoid contamination and ensure the appropriate incubation conditions. This meticulous tracking and management of patient samples are essential for ensuring accurate results and preventing errors that could compromise the outcome of ART procedures.
Q 21. How do you maintain sterility and minimize contamination in the lab?
Maintaining sterility and minimizing contamination is of paramount importance in a reproductive biology lab. We utilize a multi-layered approach incorporating a range of techniques and procedures. This starts with proper personal protective equipment (PPE), including sterile gloves, lab coats, and face masks. The lab environment is carefully controlled with HEPA-filtered laminar flow hoods providing a clean working area, and regular cleaning and disinfection of work surfaces are routinely performed with appropriate disinfectants.
All equipment used is either sterile or meticulously cleaned and sterilized using autoclaves or other sterilization methods. We use only high-quality, sterile reagents and culture media. Regular environmental monitoring is conducted to assess the sterility of the lab environment, including air and surface sampling to detect any microbial contamination. Strict adherence to these procedures is crucial to prevent contamination, which could lead to infection, failed fertilization, or compromised embryo development, ultimately impacting the success of ART procedures and potentially causing serious complications for the patients.
Q 22. What is the role of genetics in reproductive health?
Genetics plays a fundamental role in reproductive health, influencing everything from fertility to the likelihood of genetic disorders in offspring. Our genes dictate the development and function of the reproductive system, including hormone production, gamete (sperm and egg) formation, and the processes of fertilization and embryonic development.
For example, genetic mutations can cause conditions like cystic fibrosis or Klinefelter syndrome, which directly impact fertility. Genetic testing can identify these predispositions, allowing for informed family planning and reproductive choices. Furthermore, genetic screening of embryos through techniques like preimplantation genetic testing (PGT) can help couples avoid transmitting known genetic disorders to their children. Understanding an individual’s genetic profile is increasingly important for personalized reproductive healthcare.
Q 23. What are the different types of infertility treatments available?
Infertility treatments encompass a wide range of approaches, tailored to the specific cause of infertility. These treatments can be broadly categorized as:
- Medications: These stimulate ovulation (like Clomiphene Citrate or Letrozole) or improve sperm production. For example, a woman with anovulatory infertility might benefit from Clomiphene Citrate to trigger egg release.
- Intrauterine Insemination (IUI): Prepared sperm is directly placed into the uterus to increase the chances of fertilization. IUI is often used in cases of mild male factor infertility or unexplained infertility.
- In Vitro Fertilization (IVF): Eggs are retrieved from the ovaries, fertilized with sperm in a laboratory setting, and then the resulting embryos are transferred back into the uterus. IVF is a powerful tool for various infertility causes, including endometriosis, tubal damage, or severe male factor infertility.
- Intracytoplasmic Sperm Injection (ICSI): A specialized form of IVF where a single sperm is directly injected into an egg. This is often used when there’s a severe male factor infertility, such as low sperm count or poor sperm motility.
- Assisted Hatching: A procedure that assists the embryo in breaking out of its protective shell (zona pellucida), improving implantation rates. This is sometimes used in conjunction with IVF.
- Gamete Intrafallopian Transfer (GIFT) and Zygote Intrafallopian Transfer (ZIFT): Older techniques where eggs and sperm (GIFT) or fertilized embryos (ZIFT) are placed into the fallopian tubes. These are less commonly used now compared to IVF.
The choice of treatment depends on factors like the couple’s age, cause of infertility, overall health, and personal preferences. A thorough evaluation by a reproductive endocrinologist is crucial to determine the best course of action.
Q 24. Explain your understanding of the human reproductive system.
The human reproductive system is a complex interplay of organs and hormones responsible for the production of gametes (sperm and eggs), sexual intercourse, fertilization, and the development of a fetus.
In males, the testes produce sperm, which are then transported through the epididymis, vas deferens, and ejaculatory ducts. The seminal vesicles, prostate gland, and bulbourethral glands add fluids to create semen. Hormones like testosterone are crucial for sperm production and secondary sexual characteristics.
In females, the ovaries produce eggs (ova) through a process called oogenesis. The eggs are released during ovulation and travel through the fallopian tubes, where fertilization typically occurs. The fertilized egg implants in the uterus, where it develops into a fetus. Hormones like estrogen and progesterone regulate the menstrual cycle and pregnancy. The entire process is under the control of the hypothalamus and pituitary gland which release hormones in a complex feedback loop.
Understanding the intricate workings of this system is essential for diagnosing and treating fertility issues.
Q 25. What is the role of the zona pellucida in fertilization?
The zona pellucida (ZP) is a glycoprotein layer surrounding the mammalian egg. It plays a crucial role in fertilization by:
- Species-Specific Sperm Binding: The ZP contains species-specific receptors that ensure only sperm of the same species can bind to the egg. This prevents cross-species fertilization.
- Sperm-Egg Recognition and Interaction: Specific molecules on the sperm’s surface interact with the ZP, triggering the acrosome reaction. The acrosome reaction is the release of enzymes from the sperm head, allowing it to penetrate the ZP.
- Preventing Polyspermy: After a sperm successfully penetrates the ZP, changes occur in the ZP that prevent further sperm from entering, ensuring only one sperm fertilizes the egg. This is crucial for normal embryonic development.
Disruptions to the ZP structure or function can lead to fertilization failure. Assisted reproductive technologies like assisted hatching aim to overcome ZP-related barriers to fertilization.
Q 26. What is the difference between intracytoplasmic sperm injection (ICSI) and IVF?
Both ICSI and IVF are assisted reproductive technologies (ART) used to treat infertility, but they differ in their approach to fertilization:
- In Vitro Fertilization (IVF): Eggs are retrieved from the ovaries and placed in a culture dish with sperm. Fertilization occurs naturally; the sperm must swim to and penetrate the egg independently.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is directly injected into an egg using a microneedle. This bypasses the need for the sperm to swim and penetrate the egg on its own.
ICSI is typically used when there are severe male factor infertility issues, such as very low sperm counts, poor sperm motility, or abnormal sperm morphology. IVF is a more general approach suitable for various causes of infertility, including female factor infertility. The choice between IVF and ICSI is made on a case-by-case basis after careful evaluation of the couple’s situation.
Q 27. How do you interpret results from semen analysis?
Semen analysis is a crucial test in evaluating male fertility. The results are interpreted by considering several key parameters:
- Sperm Concentration: The number of sperm per milliliter of semen. Low concentration (oligospermia) is a common cause of infertility.
- Sperm Motility: The percentage of sperm that are actively moving. Poor motility (asthenospermia) hinders fertilization.
- Sperm Morphology: The percentage of sperm with a normal shape. Abnormal morphology (teratospermia) can impair fertilization.
- Semen Volume: The total amount of semen produced. Low volume can indicate a problem with the accessory glands.
- pH: The acidity or alkalinity of the semen. Abnormal pH can affect sperm survival.
- Liquefaction Time: The time it takes for the semen to become liquid. Prolonged liquefaction can hinder sperm motility.
Interpretation involves comparing the results to established reference ranges. A single abnormal parameter might not necessarily indicate infertility, but a combination of abnormalities significantly reduces the chances of natural conception. The interpretation is always done in the context of the overall clinical picture and other diagnostic tests.
Q 28. Explain your experience with specific laboratory equipment used in reproductive biology.
My experience includes extensive work with various laboratory equipment crucial to reproductive biology. This includes:
- Inverted Microscopes: Essential for visualizing and assessing gametes (eggs and sperm), embryos, and cell cultures. I’m proficient in using phase contrast and Hoffman modulation contrast microscopy for detailed cellular examination.
- Incubators: Precisely controlled environments are critical for culturing embryos. I have experience maintaining optimal temperature, humidity, and gas concentrations (CO2 and O2) for embryo development.
- Microinjectors: Used in techniques like ICSI, requiring skill and precision in handling microneedles to inject sperm into eggs. I have extensive training and practice in this sensitive procedure.
- Micromanipulators: These devices allow precise control and movement of microneedles and other micro-tools during procedures like ICSI, assisted hatching, and biopsy. Mastering their use is fundamental to successful ART procedures.
- Centrifuges: Used for various purposes, such as separating sperm from seminal fluid, preparing samples for analysis, and concentrating cells. I am familiar with operating different types of centrifuges at appropriate speeds and settings.
- Image Analysis Software: Software like CASA (Computer-Assisted Semen Analysis) is used for automated semen analysis, providing objective measures of sperm parameters. I have extensive expertise in using and interpreting data from CASA and other image analysis programs.
My proficiency with this equipment, coupled with my understanding of the underlying principles of reproductive biology, has enabled me to contribute significantly to successful IVF and ICSI outcomes.
Key Topics to Learn for Reproductive Biotechnology Interview
- Assisted Reproductive Technologies (ART): Understand the principles and procedures of IVF, ICSI, ZIFT, GIFT, and other ART methods. Consider the ethical implications and potential challenges.
- Gamete and Embryo Handling: Master the practical aspects of handling and culturing gametes and embryos, including cryopreservation techniques and quality assessment methods.
- Genetic Screening and Diagnosis: Explore preimplantation genetic testing (PGT) methods like PGT-A, PGT-M, and PGT-SR. Understand their applications and limitations in preventing genetic diseases.
- Reproductive Endocrinology: Familiarize yourself with hormonal regulation of reproduction, ovarian stimulation protocols, and the management of infertility related to hormonal imbalances.
- Embryo Development and Culture: Learn about the stages of embryo development, the impact of culture media on embryo quality, and the assessment of embryo morphology and viability.
- Stem Cell Technology in Reproduction: Explore the potential applications of stem cells in reproductive medicine, including gamete and germline derivation and tissue regeneration.
- Ethical and Legal Considerations: Understand the ethical dilemmas and legal frameworks surrounding reproductive technologies, including embryo selection, genetic modification, and surrogacy.
- Data Analysis and Interpretation: Develop skills in analyzing and interpreting data from reproductive technologies, including embryo morphology scores, genetic test results, and pregnancy outcomes.
- Troubleshooting and Problem-Solving: Practice identifying and addressing potential problems in ART procedures, such as fertilization failure, embryo arrest, and implantation failure.
- Laboratory Management and Quality Control: Understand the importance of maintaining high standards of laboratory practice and quality control in reproductive biotechnology settings.
Next Steps
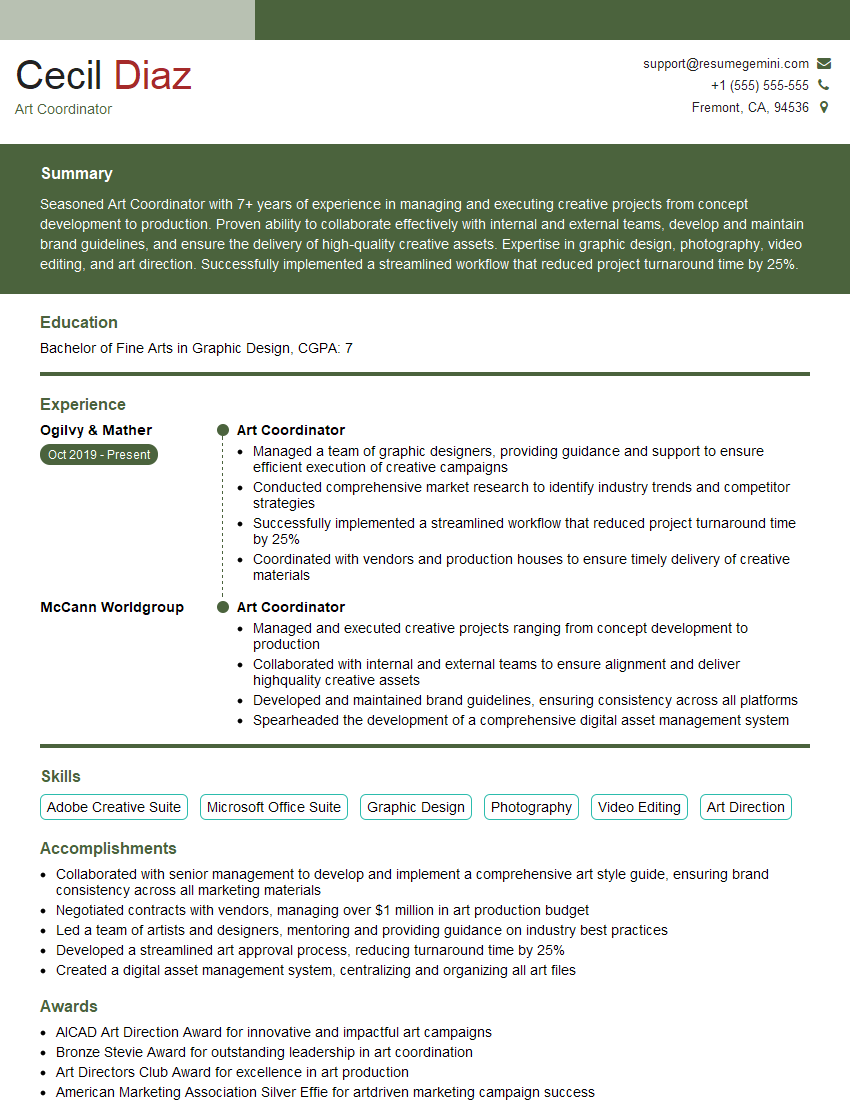
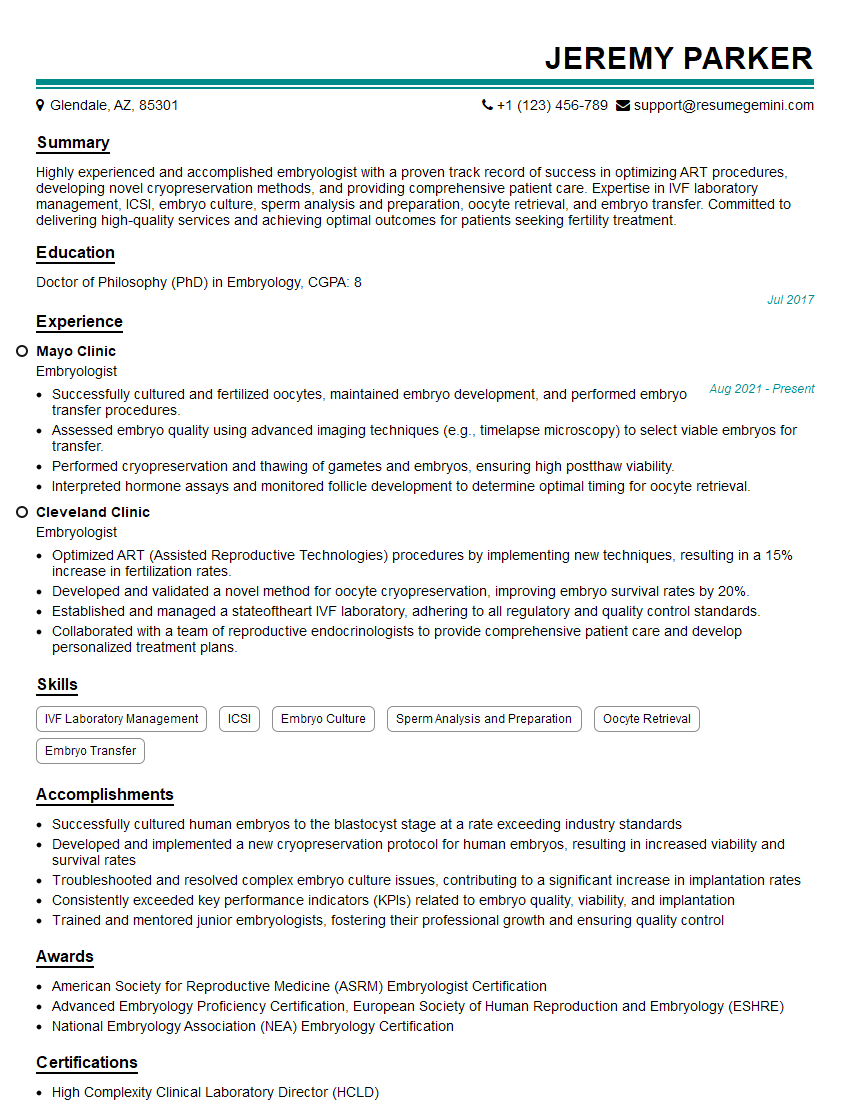
Mastering Reproductive Biotechnology opens doors to exciting and impactful careers in a rapidly growing field. A strong understanding of these concepts is crucial for success in interviews and building a rewarding professional life. To significantly enhance your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, optimized for Applicant Tracking Systems. Examples of resumes tailored specifically to Reproductive Biotechnology are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good