Preparation is the key to success in any interview. In this post, we’ll explore crucial Hands-on Experience with Histopathology and Tissue Staining Techniques interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Hands-on Experience with Histopathology and Tissue Staining Techniques Interview
Q 1. Describe the process of tissue fixation and its importance in histopathology.
Tissue fixation is the crucial first step in histopathology, aiming to preserve tissue structure and prevent degradation. It essentially ‘freezes’ the tissue in time, mimicking its in vivo state as closely as possible. This is achieved by using fixatives, chemical solutions that cross-link proteins and inactivate enzymes, preventing autolysis (self-digestion) and putrefaction.
The most common fixative is formalin (10% neutral buffered formalin), which is readily available and effective for many tissues. However, the choice of fixative depends on the specific tissue type and the intended staining procedures. For example, glutaraldehyde is preferred for electron microscopy due to its superior preservation of ultrastructure. Inadequate fixation leads to artifacts like tissue shrinkage, poor staining, and distorted morphology, making accurate diagnosis impossible. Think of it like preserving a delicate sculpture; you need the right method to maintain its integrity and prevent damage.
The importance lies in maintaining the integrity of the tissue’s cellular architecture and molecular components, ensuring the diagnosis is accurate and reliable. Without proper fixation, any subsequent processing steps are meaningless. We’ve all seen instances where inadequate fixation compromised the quality of the slides, leading to delays and even misinterpretations.
Q 2. Explain the different types of tissue processing methods and their applications.
Tissue processing involves a series of steps to prepare the fixed tissue for embedding and sectioning. The goal is to remove water and replace it with a supporting medium (paraffin wax) that allows for thin sectioning. Several methods exist, each with its advantages and disadvantages.
- Manual Processing: This traditional method involves manually transferring tissues through a series of graded alcohols, clearing agents (like xylene), and paraffin wax. It’s time-consuming but allows for precise control over each step. This is useful when dealing with smaller batches of samples or specialized tissues that require specific handling.
- Automated Tissue Processors: These machines automate the entire processing procedure, significantly reducing the time required and improving consistency. This is the gold standard in most histopathology labs, especially those with high throughput. The automated system offers programmable parameters, ensuring consistency across various sample types.
- Microwave Processing: This rapid method uses microwaves to accelerate the infiltration of reagents into the tissue, significantly reducing processing time. However, it requires careful monitoring to avoid overheating and tissue damage. The advantage here is speed and efficiency, particularly beneficial during urgent cases.
The choice of method depends on factors such as laboratory workload, the type of tissue, and available resources. In my experience, automated processors are preferred for their efficiency and reproducibility, but manual processing may be necessary for specialized techniques or delicate samples.
Q 3. What are the common embedding media used in histology, and what are their properties?
Embedding media provide support for the processed tissue, allowing it to be sectioned into thin slices. The most common is paraffin wax, a hydrophobic substance that solidifies at room temperature. Paraffin offers a balance of hardness, allowing for fine sectioning, and ease of use. It’s compatible with most staining techniques.
- Paraffin Wax: Its melting point allows for easy embedding and provides excellent support for sectioning most tissues. Different melting points are available depending on the desired hardness of the block.
- Agar: A hydrophilic gel that is useful for embedding delicate tissues or those that are difficult to infiltrate with paraffin. Its water solubility can pose challenges with certain staining procedures.
- Resin-based media (e.g., epoxy resins): Used for electron microscopy, these media provide exceptional ultrastructural preservation but require specialized equipment and techniques. They offer high resolution needed for the visualization of subcellular structures.
The selection of embedding media is critical for optimal sectioning and staining quality. The properties of each medium dictate its suitability for different applications and tissue types; a delicate specimen may require a softer embedment to avoid compression during sectioning.
Q 4. Describe the microtomy techniques used for sectioning different types of tissues.
Microtomy involves sectioning the embedded tissue into thin slices (typically 3-5 micrometers thick) using a microtome. The technique varies slightly depending on the tissue type and embedding medium.
- Rotary Microtome: The most common type, it uses a rotating wheel to advance the tissue block against a sharp blade, producing serial sections. This is ideal for paraffin-embedded tissues and provides consistent section thickness.
- Cryostat Microtome: This microtome operates at low temperatures (-20°C to -30°C), allowing for the sectioning of frozen tissues. This is particularly useful for rapid diagnosis or when preservation of tissue enzyme activity is crucial. Frozen sections are often used for rapid immunofluorescence or enzyme histochemistry.
- Vibratome/Ultramicrotome: Vibratomes use vibrations to section fresh or fixed tissues without embedding. Ultramicrotomes produce extremely thin sections (less than 1 µm) for electron microscopy. They are valuable for preserving delicate structures and require significant skill.
Different tissue types require specific adjustments to the microtome settings: hard tissues necessitate sharper blades and a slower advance rate to avoid tearing, whereas softer tissues require gentler handling and potentially a different blade angle.
Q 5. Explain the principle of hematoxylin and eosin (H&E) staining.
Hematoxylin and eosin (H&E) staining is the most common staining method in histopathology. It’s a differential stain, meaning it highlights different tissue components in contrasting colors. Hematoxylin, a basic dye, stains acidic components like nuclei a dark blue-purple color. Eosin, an acidic dye, stains basic components like cytoplasm and extracellular matrix a pink color.
The principle lies in the interaction between the charged dyes and the charged components within the tissue. Hematoxylin’s positive charge binds to the negatively charged DNA and RNA in the nucleus, while eosin’s negative charge binds to the positively charged proteins in the cytoplasm. This differential staining enables pathologists to distinguish between various cell types and structures, forming the basis for microscopic tissue analysis.
Think of it as highlighting the key features of a complex document; the nuclei (the ‘headings’) are clearly marked in blue-purple, while the rest of the text (cytoplasm and extracellular matrix) appears in pink, enhancing readability and clarity.
Q 6. What are the common artifacts encountered during tissue processing and sectioning, and how can they be minimized?
Several artifacts can arise during tissue processing and sectioning, compromising the quality of the stained slides. These can lead to misinterpretation and inaccurate diagnoses.
- Tissue shrinkage and distortion: Caused by improper fixation or processing, leading to altered tissue morphology. Minimized by careful attention to fixation time and appropriate processing techniques.
- Folding and tearing of sections: Occurs during sectioning due to improper microtome settings or handling. Avoided by adjusting microtome settings, ensuring sharp blades, and careful handling of the sections.
- Air bubbles in the sections: Introduced during mounting or staining, causing clear spaces in the tissue. Prevented by proper mounting techniques and gentle handling.
- Precipitate formation: Due to contamination of reagents or improper staining techniques. Minimized through meticulous reagent preparation and standardization of staining protocols.
- Loss of tissue components: May occur during processing, particularly with water-soluble components. Mitigated through optimized protocols and potentially alternative fixation methods.
Careful attention to detail at each step of the process, along with regular maintenance and quality control measures, are essential to minimize these artifacts. Regularly checking the equipment, using high-quality reagents, and proper training of personnel are crucial for preventing these issues.
Q 7. Describe the troubleshooting steps for common problems encountered during staining procedures.
Troubleshooting staining issues is a critical skill in histopathology. Here are some common problems and their solutions:
- Pale or faint staining: This could be due to insufficient staining time, over-differentiation, or degraded reagents. Solution: Increase staining time, reduce differentiation time, or prepare fresh reagents.
- Uneven staining: Inconsistent staining intensity across the section suggests problems with reagent preparation or tissue processing. Solution: Review the staining protocol, ensure proper reagent mixing, and re-process problematic tissue if needed.
- Background staining: Excess dye staining the background may be due to over-staining or improper rinsing. Solution: Reduce staining time, carefully rinse slides, and check for reagent contamination.
- Precipitate formation: Deposits on the slide indicate reagent contamination or improper washing. Solution: Filter reagents, replace old solutions, and thoroughly wash slides.
- Nuclear fading: Loss of hematoxylin stain may be due to over-differentiation or poor quality hematoxylin. Solution: Adjust differentiation time and use fresh hematoxylin.
A systematic approach, focusing on each step of the staining procedure, is crucial. Maintaining detailed records and regularly evaluating staining quality are essential in identifying and resolving such issues. Documenting the troubleshooting process also aids in preventing recurrence.
Q 8. Explain the principles and applications of immunohistochemistry (IHC).
Immunohistochemistry (IHC) is a powerful technique that uses antibodies to identify specific proteins within tissue sections. Imagine it like a highly specific molecular fishing expedition – we use antibodies (the ‘bait’) to ‘catch’ particular proteins (the ‘fish’) within the tissue sample. This allows us to visualize the location and abundance of these proteins, which is crucial for diagnosis and research.
The principles involve the antigen-antibody interaction. A known antibody, specific to a target protein, is applied to a tissue sample. If the target protein is present, the antibody binds to it. This binding is then detected using a detection system, typically involving an enzyme or a fluorescent tag. This detection system produces a color change or fluorescence signal, allowing us to see exactly where the protein is located within the tissue under a microscope.
Applications are vast. In cancer diagnosis, IHC helps determine the type and grade of cancer, predict prognosis, and guide treatment decisions. For example, identifying estrogen receptor (ER) and progesterone receptor (PR) in breast cancer tissue is crucial for determining hormonal therapy suitability. In other applications, IHC can be used to diagnose infectious diseases (identifying viral or bacterial proteins), assess neurological disorders (detecting specific proteins in brain tissue), and investigate autoimmune diseases (identifying the presence of immune cells and proteins).
Q 9. Describe the process of performing in situ hybridization (ISH).
In situ hybridization (ISH) is a technique used to detect specific DNA or RNA sequences within tissue sections. Think of it as searching for a specific piece of genetic information within a complex mixture of cellular material. This allows us to pinpoint the location of specific genes or RNA transcripts, providing insights into gene expression and disease processes.
The process typically involves the use of labeled probes – single-stranded DNA or RNA molecules complementary to the target sequence. These probes are designed to bind specifically to the target nucleic acid. Once the probe binds, the signal (generated by the label, usually fluorescence or a colorimetric reaction) can be detected using microscopy.
The procedure generally involves fixing and permeabilizing the tissue to allow probe access to the target nucleic acids, then hybridizing the labeled probe to the target sequence. Stringent washing steps remove unbound probes and signal amplification may be incorporated to improve sensitivity. Finally, the sample is visualized under a microscope, with the signal indicating the precise location of the target sequence in the tissue.
Examples of ISH applications include diagnosing infectious diseases (detecting viral or bacterial genetic material), characterizing cancer subtypes (detecting specific gene rearrangements), and studying gene expression during development or in response to disease.
Q 10. What are special stains, and what are some examples of their applications in diagnosis?
Special stains are histochemical methods that highlight specific tissue components, providing additional information beyond what’s offered by routine Hematoxylin and Eosin (H&E) staining. While H&E gives a general overview of tissue architecture, special stains focus on particular structures like collagen, amyloid, or microorganisms. They are like specialized tools for a specific job, revealing features that might be missed with routine staining.
Examples and their diagnostic applications include:
- Masson’s Trichrome: Highlights collagen fibers in blue, used in evaluating fibrosis in liver disease or scar tissue formation.
- Periodic Acid-Schiff (PAS): Detects carbohydrates and glycoproteins, useful in identifying fungal infections, glycogen storage diseases, and certain types of tumors.
- Congo Red: Stains amyloid deposits in tissues, crucial for diagnosing amyloid-related diseases like Alzheimer’s disease.
- Silver stains: Detect microorganisms like bacteria and fungi, or nerve fibers, aiding in diagnosis of infections and neurological conditions.
- Oil Red O: Identifies lipids, important for assessing fatty changes in the liver or other organs.
Special stains greatly enhance diagnostic accuracy by providing crucial information that complements H&E staining, particularly when identifying subtle changes or specific pathogens.
Q 11. Explain the importance of quality control in histopathology.
Quality control (QC) in histopathology is paramount for ensuring accurate and reliable diagnoses. It’s the backbone of patient safety and maintaining laboratory credibility. Think of QC as a safety net, catching potential errors before they impact patient care.
QC measures cover various aspects of the workflow, including:
- Specimen identification and tracking: Ensuring correct labeling and matching of specimens throughout the process.
- Tissue processing: Monitoring fixation, embedding, and sectioning parameters for optimal tissue preservation and section quality.
- Staining techniques: Regular checks on staining protocols and reagents to ensure consistent and accurate results. We employ control slides with known positive and negative reactions to validate our staining.
- Microscopy and image analysis: Maintaining microscope calibration and ensuring that image capture and analysis are performed consistently.
- External quality assessment (EQA): Participating in proficiency testing programs to compare our performance with other laboratories and identify areas for improvement.
Robust QC procedures minimize errors, enhance diagnostic accuracy, and instill confidence in the results, ultimately benefiting patients.
Q 12. How do you ensure proper labeling and tracking of specimens in a histopathology laboratory?
Proper specimen labeling and tracking is essential to avoid misidentification and errors that could have significant consequences. This is accomplished through a combination of stringent protocols and technologies. From the moment a specimen is received in the lab, it receives a unique identifier, often a barcode, that follows it through every step of the process.
The steps include:
- Accessioning: Assigning a unique accession number to each specimen upon arrival. This number is carefully recorded in our laboratory information system (LIS).
- Barcode labeling: Attaching a barcode label to the specimen container and corresponding cassettes, slides, and blocks. These barcodes are scanned at each stage of processing to ensure accurate tracking.
- LIS integration: Using a sophisticated LIS that integrates all aspects of the workflow, including specimen tracking, test ordering, reporting, and quality control.
This multi-layered approach ensures that every specimen is correctly identified and tracked throughout its journey through the laboratory. It’s a vital component in preventing errors that could affect patient care.
Q 13. Describe your experience with different types of microscopes used in histology.
My experience encompasses various microscope types, each suited for specific tasks in histology. The workhorse is the brightfield microscope, essential for routine H&E and special stain examination. It provides detailed morphological information about tissue structure and cellular components.
Beyond brightfield, I’ve extensively used:
- Fluorescence microscopes: Used in IHC and ISH to visualize fluorescently labeled antibodies or probes. The sensitivity and specificity of fluorescence microscopy are invaluable for these techniques.
- Polarizing microscopes: Detect birefringent substances like amyloid or crystals, which exhibit unique optical properties under polarized light.
- Digital microscopes: These allow for image capture, storage, and analysis, improving efficiency and facilitating consultations with colleagues or remote experts. They also allow for image enhancement and measurement capabilities.
The choice of microscope depends on the specific application and the information required. My expertise encompasses selecting the appropriate microscopy technique to obtain optimal results for each diagnostic task.
Q 14. Explain the difference between routine H&E staining and special stains.
Routine H&E staining is the foundation of histopathology, providing a general overview of tissue architecture. Hematoxylin stains cell nuclei blue, while eosin stains cytoplasmic proteins pink. It gives a general overview of tissue structure and cellular morphology. Think of it as a general map of the tissue landscape.
Special stains, on the other hand, are more targeted. They’re used to highlight specific cellular components or structures, like collagen fibers, microorganisms, or specific proteins. They’re like specialized lenses that zoom in on particular aspects of interest that may not be visible in the broader context of the H&E stained section. For example, while H&E might show an inflammatory infiltrate, a special stain for fungi could pinpoint a fungal infection within that infiltrate.
In short, H&E provides a general overview, while special stains provide detailed information about specific components, working together to give a comprehensive understanding of the tissue.
Q 15. Describe your experience with automated staining systems.
My experience with automated staining systems encompasses several years of hands-on operation and maintenance of various platforms, including Leica ST5020 and Ventana Benchmark ULTRA. These systems significantly enhance efficiency and standardization in tissue processing. I’m proficient in programming and troubleshooting these systems, including managing reagent levels, calibrating instruments, and performing routine maintenance to ensure optimal staining quality and prevent downtime. For instance, I once resolved a recurring issue with inconsistent staining on the Leica ST5020 by identifying a minor leak in the reagent delivery system, a problem quickly rectified after a thorough inspection and replacement of a worn seal. This highlights the importance of preventative maintenance and proactive troubleshooting in maximizing the lifespan and performance of these valuable assets.
Furthermore, my experience extends to validating and implementing new staining protocols on automated systems, ensuring optimal results while adhering to stringent quality control measures. This often involves optimizing reagent concentrations and staining times for specific tissue types to achieve consistent and high-quality staining.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle discrepancies in staining results?
Discrepancies in staining results require a systematic approach to identify and rectify the root cause. My initial steps involve reviewing the entire staining process, from tissue fixation and processing to staining parameters. This includes checking the quality of reagents, verifying the correct application of protocols, and examining the staining equipment for any malfunctions. For example, inconsistent hematoxylin staining might indicate a problem with the hematoxylin solution itself (oxidation, concentration), the staining time, or even a faulty staining instrument.
I meticulously document all observations, including the batch numbers of reagents, staining times, and equipment settings. If the issue persists after these initial checks, I perform a comparison with control slides stained in parallel to isolate the variable. This process often involves repeating the staining procedure with fresh reagents and known-good controls to rule out systematic errors. If the problem continues, I consult relevant literature and may even conduct further testing, such as assessing reagent pH, to pinpoint the exact cause. Through this methodical approach, I’ve successfully resolved numerous staining inconsistencies, ensuring the delivery of accurate and reliable diagnostic results.
Q 17. What are the safety precautions you follow when handling hazardous chemicals in the histology lab?
Safety is paramount in a histopathology laboratory, especially when handling hazardous chemicals like formalin, xylene, and various stains. My adherence to safety protocols begins with proper personal protective equipment (PPE), including lab coats, gloves (nitrile or neoprene depending on the chemical), eye protection, and sometimes respirators, depending on the concentration and volatility of the chemicals. I always work under a well-ventilated fume hood when handling volatile chemicals such as xylene.
We maintain detailed safety data sheets (SDS) for all chemicals and follow the recommended handling and disposal procedures. Proper waste segregation and disposal are strictly adhered to, following local and institutional regulations. Regular safety training and refresher courses ensure everyone in the lab remains updated on best practices. Furthermore, we conduct regular equipment checks and maintain emergency response plans to handle spills or other unforeseen incidents. In short, safety isn’t just a protocol; it’s an ingrained part of our daily laboratory practice.
Q 18. Describe your experience with maintaining histology equipment.
Maintaining histology equipment is crucial for optimal performance and longevity. My experience involves routine maintenance tasks such as cleaning, lubricating, and calibrating various instruments, including microtomes, tissue processors, embedding stations, and stainers. I’m familiar with the preventative maintenance schedules for each piece of equipment and adhere to these schedules rigorously. This includes regularly checking reagent levels, cleaning and replacing filters, and performing routine checks to identify potential problems before they escalate into major malfunctions.
For instance, I regularly clean and lubricate the microtome knife holder to ensure smooth sectioning and prevent damage to the blades. I also perform regular checks on the tissue processor’s heating and vacuum systems to ensure efficient and optimal tissue processing. Proactive maintenance minimizes downtime and ensures the consistent production of high-quality histological sections. Furthermore, I am adept at troubleshooting minor technical issues and documenting all maintenance activities in a logbook for easy tracking and reference.
Q 19. Explain your understanding of quality assurance procedures in a histopathology laboratory.
Quality assurance (QA) is fundamental to the reliability of histopathology results. Our laboratory adheres to strict QA protocols to ensure the accuracy and consistency of our work. This starts with meticulous sample tracking and handling, ensuring proper labeling and accessioning of each tissue sample. We employ standardized operating procedures (SOPs) for all processes, from tissue fixation and processing to staining and sectioning. Regular quality controls (QCs) are implemented at each stage, including monitoring reagent quality, checking section thickness and staining quality, and performing proficiency testing to assess technician competency.
We use quality control slides with known characteristics to monitor the consistency of staining procedures. Regular instrument calibration and maintenance are crucial aspects of our QA program. We also participate in external quality assurance programs to compare our performance with other laboratories and identify areas for improvement. All discrepancies are thoroughly investigated, and corrective actions are documented and implemented to maintain the high quality of our results and ensure patient safety.
Q 20. What are the different types of tissue cassettes used in histology, and when would you use each?
Various types of tissue cassettes are used in histology, each suited to specific needs. The most common type is the standard plastic cassette, typically made of hard, durable plastic with a hinged lid. These are used for most routine tissue processing. Larger cassettes accommodate larger tissue specimens. Some cassettes feature embedded barcodes for automated tracking and identification, especially in high-throughput labs.
Other specialized cassettes include those with porous walls for optimal reagent exchange during processing, and cassettes designed for specific applications such as immunohistochemistry (IHC). The choice of cassette depends on factors such as the size and type of tissue, the processing method, and the need for automated tracking. For example, larger cassettes might be selected for whole organs, while cassettes with porous walls are ideal for ensuring complete infiltration of reagents during processing. Selecting the appropriate cassette is key to optimal tissue processing and maintaining sample integrity.
Q 21. How would you address a situation where you encounter a heavily calcified tissue sample?
Encountering heavily calcified tissue presents a challenge in histological processing, as it can hinder proper sectioning and staining. To address this, I would employ a decalcification process prior to routine histological processing. Several methods exist, including acid decalcification (using acids like formic acid or nitric acid) and chelation (using EDTA). The choice depends on the type and extent of calcification and the desired preservation of tissue morphology.
Acid decalcification is generally faster but can damage tissue morphology if not carefully controlled. Chelation is slower but generally considered gentler on the tissue. After decalcification, thorough washing is essential to remove residual decalcifying agent, which can interfere with subsequent staining. Careful monitoring during decalcification is vital to prevent over-decalcification, which can compromise tissue integrity. Once decalcification is complete, the tissue undergoes standard histological processing, embedding, sectioning, and staining procedures. The use of special microtome blades designed for hard tissue may also be necessary to ensure efficient sectioning of the decalcified tissue. Microscopic examination post-processing will then confirm the adequacy of the decalcification procedure.
Q 22. Describe your experience with troubleshooting problems related to tissue processing.
Troubleshooting tissue processing issues requires a systematic approach. I’ve encountered various problems, from inadequate fixation leading to poor tissue morphology to issues with paraffin infiltration resulting in incomplete embedding. My troubleshooting strategy involves first identifying the point of failure. For example, if sections are crumbling, this often indicates problems with either fixation (insufficient or prolonged) or paraffin infiltration (incomplete). If tissues are overly hard or brittle, it could suggest problems with processing times or reagent concentrations.
I’ll then methodically review the processing steps:
- Fixation: Checking fixation time, adequacy of fixative volume, and the fixative’s quality itself are key. If the fixative is old or improperly stored, it may not function correctly.
- Dehydration: I’ll verify that the graded alcohol series (e.g., 70%, 95%, 100%) is working correctly and that appropriate times are being used; inadequate dehydration can lead to poor paraffin infiltration.
- Clearing: I ensure that the clearing agent (e.g., xylene) is fresh and that sufficient time is allowed for the agent to remove the alcohol. The transition between alcohol and clearing agent must be smooth to avoid tissue damage.
- Infiltration: Problems here might manifest as incomplete paraffin infiltration. I examine the paraffin bath temperature and the infiltration times; longer times may be necessary for larger or denser tissues.
I meticulously document all steps and any deviations from standard protocols. This detailed record helps me identify patterns and prevent recurring issues. I also rely on quality control measures, such as routinely checking the quality of processed tissues through the use of control tissues.
Q 23. How familiar are you with different types of tissue fixatives and their applications?
I’m very familiar with various fixatives and their applications. The choice of fixative depends heavily on the type of tissue and the intended staining procedures. For example:
- Formalin (10% neutral buffered formalin): This is the most common fixative, suitable for routine histopathology. It’s relatively inexpensive and provides good preservation of cellular morphology for most tissues. However, prolonged exposure can cause artifacts, and it can be hazardous to handle.
- Formaldehyde-free fixatives: These are gaining popularity due to the safety concerns associated with formaldehyde. Options include glutaraldehyde (better for electron microscopy) and alcohol-based fixatives (better for cytology).
- Bouin’s solution: This is an excellent fixative for preserving the quality of nuclei, particularly beneficial for immunohistochemistry. However, it can make tissue brittle.
- Zenker’s solution: Excellent for preserving cellular detail, particularly good for bone marrow samples, but requires special handling and disposal.
- Microwaving fixation: This method accelerates the fixation process, saving time but requiring careful control to avoid tissue damage.
My experience allows me to select the optimal fixative based on the specific needs of each case. I understand the impact of fixation on subsequent staining procedures, choosing fixatives compatible with desired stains and immunohistochemical analyses.
Q 24. What is your experience with cryostat sectioning?
I have extensive experience with cryostat sectioning, a technique crucial for rapid processing of frozen tissues for immunofluorescence, enzyme histochemistry, and situations where rapid diagnosis is needed (e.g., frozen sections during surgery).
My expertise encompasses:
- Proper tissue preparation: This involves optimal freezing of the tissue using isopentane cooled by liquid nitrogen to minimize ice crystal formation, which can compromise tissue morphology.
- Cryostat operation and maintenance: I am proficient in operating a cryostat, setting the optimal temperature for sectioning, and maintaining the cryostat’s cleanliness and functionality. Regular maintenance, including cleaning the blade holder and adjusting the chuck, is crucial for quality sections.
- Sectioning techniques: I can produce high-quality sections of varying thicknesses (typically 4-10 µm), depending on the intended application. This includes handling different tissue types, some of which may require special handling (e.g., very soft or delicate tissues).
- Troubleshooting: I can identify and address common problems such as chatter (vibrations during cutting), compression artifacts, and ice crystal formation. For example, if I am getting ice crystal formation, it indicates the temperature is not low enough or the tissue is not being frozen optimally.
I’m adept at producing high-quality sections consistently, understanding that the quality of the sections directly affects the accuracy of the results.
Q 25. Explain your understanding of the importance of proper tissue orientation during embedding.
Proper tissue orientation during embedding is critical for obtaining appropriately oriented sections, ensuring accurate diagnosis, particularly in biopsies where specific tissue architecture is vital. Imagine trying to interpret a map that’s upside down – it would be difficult! Similarly, misoriented tissues can lead to misinterpretations.
For example, when embedding a skin biopsy, it’s crucial to orient the specimen so that the epidermis is facing upwards for proper examination of layers. In a muscle biopsy, orientation helps assess fiber arrangement and muscle architecture. During embedding, I carefully arrange the tissue cassette with the desired orientation in the mold using a dissecting microscope to improve precision. I use markers or labels to confirm the orientation for my own reference, and often also on the tissue block itself with an orientation arrow. This allows me to section the block in the correct plane to obtain sections with the appropriate anatomical representation.
Failing to properly orient the tissue can lead to a misdiagnosis or inaccurate interpretation of cellular relationships within the tissue.
Q 26. Describe your experience with maintaining accurate records and documenting procedures.
Maintaining accurate records and documenting procedures is paramount in histology. It ensures traceability, quality control, and compliance with regulations. My approach involves using a combination of electronic and paper-based records.
Electronic systems: I utilize laboratory information management systems (LIMS) to track specimens, record processing steps, staining procedures, and any related information. This ensures that data is easily accessible and organized.
Paper-based systems: While LIMS is the primary documentation method, I also use paper-based logs to record daily activities, equipment maintenance, and any anomalies. This serves as a backup and provides a quick reference point for immediate issues.
Detailed entries: I record all relevant information, including lot numbers of reagents, instrument settings, and any observed issues. Any deviations from standard operating procedures are meticulously noted, along with the corrective actions taken. The clarity and detail are extremely important to guarantee traceability, facilitate troubleshooting and allow for auditing and review.
Q 27. How do you maintain the quality of reagents and stains in the histology laboratory?
Maintaining reagent and stain quality is essential for reliable results. This involves several key strategies:
- Proper storage: Reagents and stains are stored according to manufacturer’s instructions, often in cool, dark places to prevent degradation. This might involve refrigeration or freezing in some cases.
- Inventory management: We employ a first-in, first-out (FIFO) system to ensure that older reagents are used before newer ones, minimizing the risk of degradation. Regular inventory checks prevent reagents from expiring.
- Quality control: Routine testing of reagents and stains is performed using positive and negative controls to verify their effectiveness. This might involve running test slides with tissues known to react positively with the reagent or stain, and others known not to react. The expected results are then compared to the obtained results.
- Appropriate disposal: Proper disposal of expired or contaminated reagents is crucial to maintain safety and environmental compliance.
- Regular maintenance of equipment: Stainers and other equipment are regularly maintained and calibrated to ensure accurate dispensing and consistent results.
By following these measures, I help ensure the quality of our staining procedures and maintain the reliability of our histological results.
Q 28. What are your strategies for managing a high volume of specimens in a busy histology lab?
Managing a high volume of specimens efficiently in a busy histology lab requires a well-organized workflow and effective teamwork. My strategies include:
- Prioritization: Urgent cases (e.g., frozen sections during surgery) are prioritized to ensure rapid turnaround times. A system to flag urgent cases at the point of accessioning is crucial.
- Workflow optimization: We utilize automated processing and staining equipment whenever feasible. This increases throughput and reduces manual labor. Lean methodology principles can be applied to identify and eliminate bottlenecks in the workflow.
- Teamwork and communication: Effective communication among team members is crucial for efficient sample tracking and problem-solving. Clear roles and responsibilities help streamline tasks.
- Regular maintenance and preventative care of equipment: Prevents downtime and maximizes efficiency.
- Quality control: Implementing rigorous quality control measures throughout the process identifies and addresses any potential problems early on, avoiding delays and ensuring quality.
- Batch processing: Processing multiple specimens simultaneously in automated systems optimizes turnaround time and efficiency.
By combining technological advancements with a structured, efficient workflow and great teamwork, we can effectively manage a high volume of specimens while maintaining the high quality of our results.
Key Topics to Learn for Hands-on Experience with Histopathology and Tissue Staining Techniques Interview
- Tissue Processing: Understanding the principles and practical steps involved in tissue fixation, dehydration, clearing, and embedding. Be prepared to discuss troubleshooting common issues encountered during each stage.
- Microtomy and Sectioning: Mastering the techniques of sectioning paraffin-embedded tissues using a microtome. Discuss different types of microtomes and the challenges associated with obtaining high-quality sections from various tissue types.
- Staining Techniques: Demonstrate a thorough understanding of Hematoxylin and Eosin (H&E) staining, along with other special stains (e.g., PAS, Trichrome, Immunohistochemistry). Be prepared to explain the principles behind each stain, its applications, and interpretation of results.
- Microscopy and Image Analysis: Discuss the use of light microscopy for examining stained tissue sections. Explain how to identify different tissue types and cellular components. If applicable, mention experience with digital microscopy and image analysis software.
- Quality Control and Troubleshooting: Highlight your experience in identifying and resolving issues related to tissue processing, sectioning, and staining. This demonstrates a practical understanding and problem-solving skills crucial in a histopathology lab.
- Safety and Regulations: Demonstrate knowledge of laboratory safety protocols, including handling hazardous chemicals and disposing of biological waste according to regulations.
- Laboratory Information Systems (LIS): Familiarity with LIS software used for tracking samples, generating reports, and managing lab workflows is a valuable asset.
Next Steps
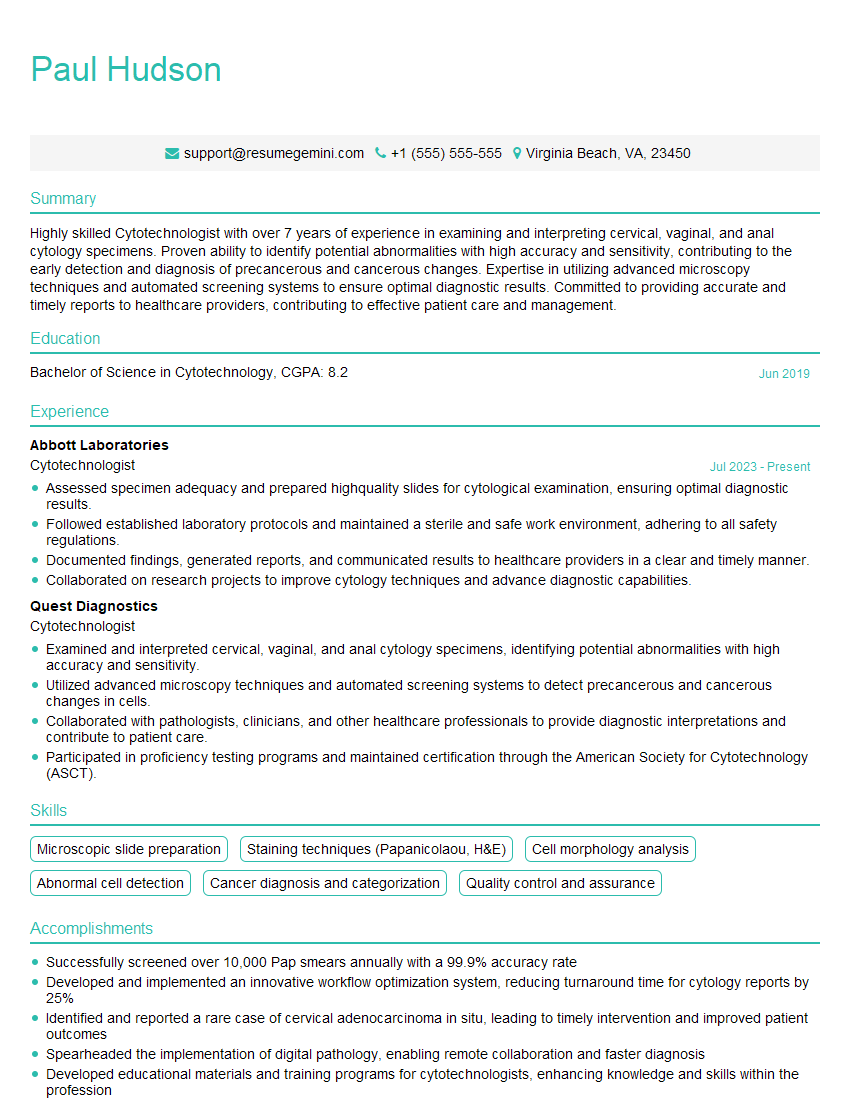
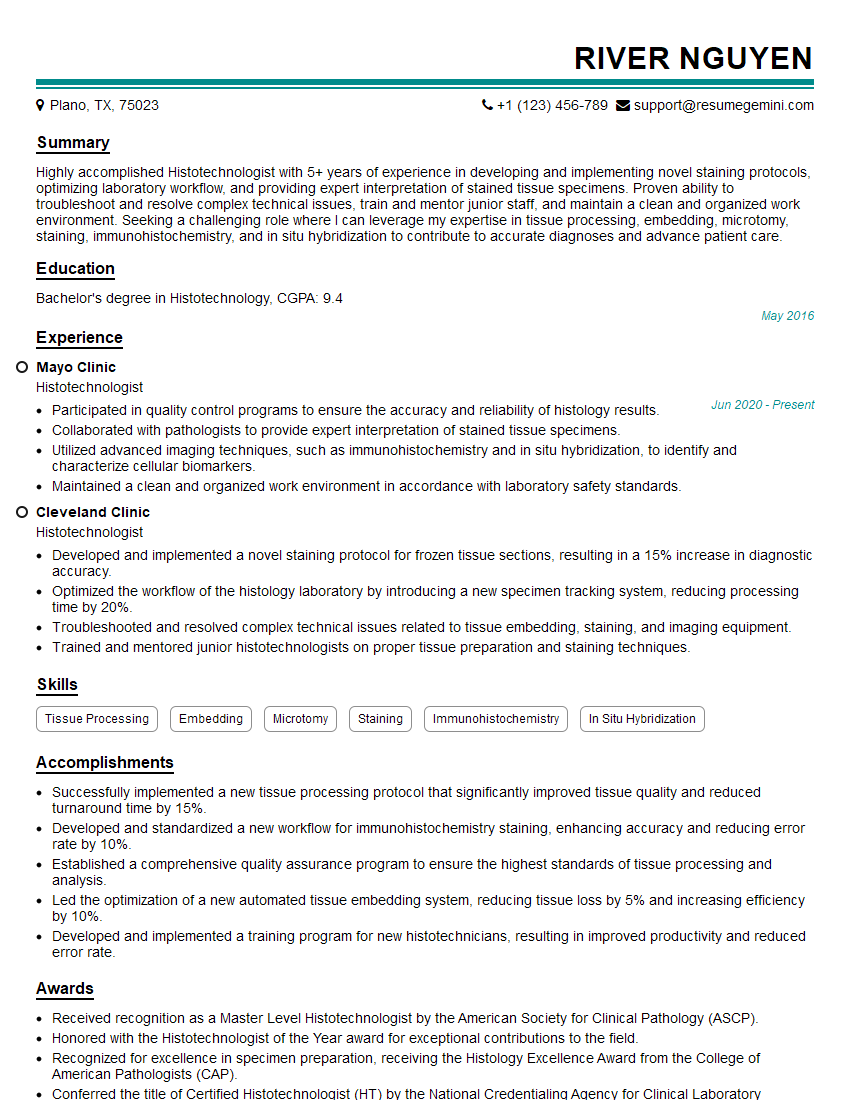
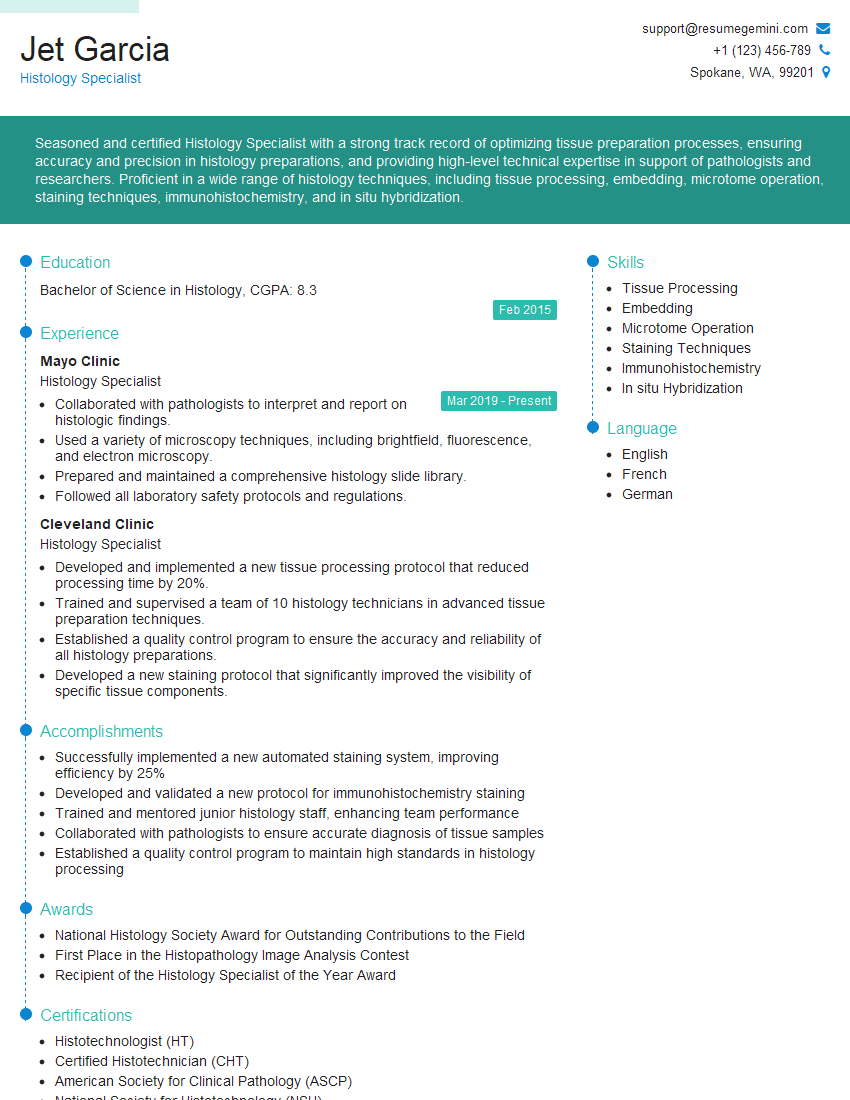
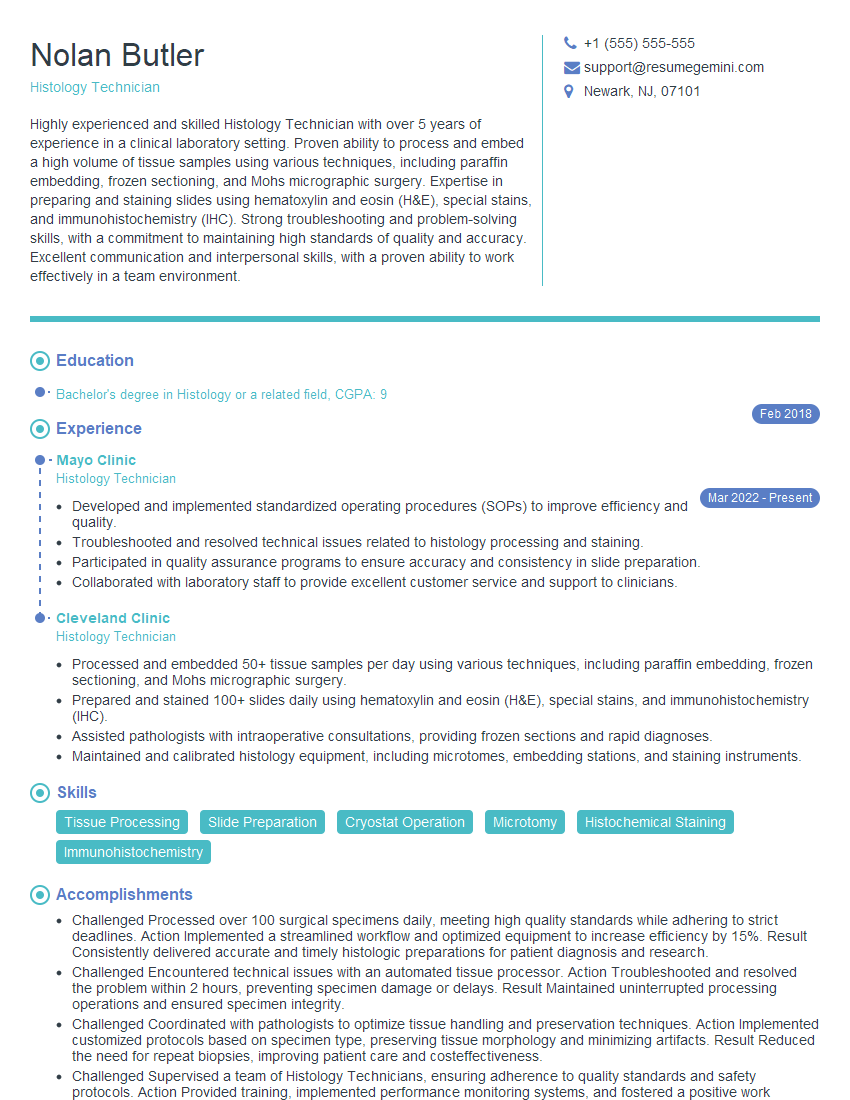
Mastering hands-on experience with histopathology and tissue staining techniques is crucial for career advancement in this specialized field. A strong understanding of these techniques will open doors to exciting opportunities and demonstrate your valuable expertise to potential employers. To increase your job prospects, creating a well-structured, ATS-friendly resume is paramount. We highly recommend using ResumeGemini to build a professional and impactful resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Hands-on Experience with Histopathology and Tissue Staining Techniques, helping you present your qualifications in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good