The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Biomedical Device Infection Control interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Biomedical Device Infection Control Interview
Q 1. Describe the process of sterilizing endoscopes.
Sterilizing endoscopes is a critical process to prevent infections. It involves a multi-step procedure, starting with pre-cleaning to remove visible debris and organic matter. This is typically done manually using enzymatic detergents and brushes designed to reach all lumens and channels within the endoscope. Then, the endoscope undergoes a high-level disinfection or sterilization process. The choice depends on the specific endoscope type and the level of contamination risk.
For sterilization, methods like steam sterilization (autoclaving), liquid chemical sterilization (e.g., glutaraldehyde), and ethylene oxide (EtO) sterilization might be used. Steam sterilization is preferred when compatible, but certain endoscopes with heat-sensitive components might require liquid or EtO sterilization. Following sterilization, the endoscope undergoes a thorough rinse and drying process before being stored in a clean, dry environment. The entire process is rigorously documented to ensure compliance with infection control protocols and regulatory requirements. For example, a gastroenterology department might use automated endoscope reprocessors (AERs) that integrate cleaning, disinfection, and high-level disinfection or sterilization steps for improved efficiency and consistency. Regular maintenance of AERs and adherence to manufacturer’s instructions are vital.
Q 2. What are the different sterilization methods and their applications?
Several sterilization methods exist, each with its own strengths and limitations.
- Steam Sterilization (Autoclaving): This is the most common and preferred method when applicable. It uses saturated steam under pressure to achieve high temperatures that effectively kill microorganisms. It’s effective against a wide range of microorganisms, including spores, but not suitable for heat-sensitive devices.
- Ethylene Oxide (EtO) Sterilization: Used for heat-sensitive instruments and devices that cannot withstand steam sterilization. EtO is a gas that penetrates packaging and kills microorganisms through alkylation. However, it’s a carcinogenic substance, requiring specialized equipment and handling procedures. Aeration is crucial after EtO sterilization to remove residual gas.
- Liquid Chemical Sterilization: This involves immersing devices in a sterilizing liquid, such as glutaraldehyde or peracetic acid, for a specific duration. It’s effective for heat-sensitive items but requires careful handling due to potential toxicity and environmental concerns. Strict adherence to contact times and proper disposal are critical.
- Hydrogen Peroxide Gas Plasma Sterilization: This method uses low-temperature hydrogen peroxide plasma to kill microorganisms. It’s suitable for heat-sensitive and moisture-sensitive devices, and it’s environmentally friendly compared to EtO. However, it has limitations with certain materials and might not be suitable for all devices.
The choice of method depends on the device’s material compatibility, the required sterilization level (e.g., high-level disinfection versus sterilization), and the availability of resources and expertise.
Q 3. Explain the principles of aseptic technique.
Aseptic technique is a set of practices designed to minimize the risk of contamination by infectious agents. It’s crucial in healthcare settings to protect both patients and healthcare workers. The core principles include:
- Maintaining a sterile field: Creating a designated area where only sterile objects are allowed.
- Hand hygiene: Frequent and thorough handwashing is essential, using soap and water or an alcohol-based hand rub.
- Proper gowning and gloving: Wearing appropriate personal protective equipment (PPE) to prevent contamination.
- Sterile instrument handling: Using sterile instruments and supplies correctly, avoiding touching non-sterile surfaces.
- Environmental control: Maintaining a clean and disinfected environment to minimize the risk of contamination.
Think of it like preparing a delicate dish – you wouldn’t want to contaminate it during the cooking process. Similarly, aseptic technique is vital to prevent infection during medical procedures. A surgeon meticulously scrubbing before an operation exemplifies this. Any deviation from the established aseptic techniques compromises patient safety significantly.
Q 4. How do you identify and manage a potential outbreak related to medical devices?
Managing a potential outbreak linked to medical devices requires a swift and coordinated response. The process involves:
- Surveillance and detection: Monitoring infection rates and identifying potential clusters of infections associated with the use of specific medical devices.
- Investigation: Conducting a thorough investigation to determine the source and cause of the outbreak, including examining device processing procedures, sterilization methods, and patient records.
- Confirmation: Using microbiological testing to confirm the presence of the infectious agent and its link to the devices.
- Control measures: Implementing immediate control measures, such as removing suspect devices from service, enhancing disinfection or sterilization protocols, and initiating contact tracing.
- Communication: Communicating with relevant stakeholders, including healthcare professionals, patients, regulatory agencies, and the public.
- Prevention: Implementing long-term preventive measures to prevent future outbreaks, such as reviewing and updating infection control protocols, enhancing staff training, and improving device tracking systems.
Imagine a scenario where several patients who underwent a particular procedure using a specific catheter developed similar infections. A thorough investigation might reveal flaws in the sterilization process for that catheter, leading to a recall and revised protocols.
Q 5. What are the key regulatory requirements for medical device sterilization?
Regulatory requirements for medical device sterilization vary across countries but generally focus on ensuring safety and efficacy. Key aspects include:
- Compliance with standards: Adherence to relevant international and national standards (e.g., ISO 11135, ISO 11137) for sterilization methods and validation.
- Sterility assurance: Demonstrating a high level of assurance that the sterilization process reliably achieves sterility.
- Validation and verification: Performing rigorous validation studies to demonstrate the effectiveness of the sterilization process and regular verification to confirm ongoing efficacy.
- Documentation and record-keeping: Maintaining detailed records of the sterilization process, including parameters, results, and any deviations.
- Quality management system (QMS): Implementing a robust QMS that encompasses all aspects of the sterilization process, from design and development to manufacturing and distribution.
- Post-market surveillance: Monitoring the performance of sterilized devices in the field and addressing any issues that may arise.
These requirements ensure that medical devices are sterilized effectively, minimizing the risk of infection. Non-compliance can lead to severe consequences, including product recalls, regulatory penalties, and legal actions.
Q 6. Describe the role of high-level disinfection in infection control.
High-level disinfection (HLD) is a crucial process that reduces the bioburden (number of microorganisms) on medical devices to a very low level. While it doesn’t achieve sterility (eliminate all microorganisms, including spores), it significantly reduces the risk of infection. HLD is used for semi-critical and non-critical medical devices.
Semi-critical items (e.g., endoscopes) come into contact with mucous membranes but do not penetrate sterile tissues. Non-critical items (e.g., blood pressure cuffs) touch only intact skin. HLD is often achieved using liquid chemical germicides such as glutaraldehyde or ortho-phthalaldehyde (OPA), or by using automated endoscope reprocessors with advanced disinfection cycles. HLD is essential for items that cannot withstand sterilization methods, ensuring a high level of safety for patients.
It’s important to differentiate between disinfection and sterilization. Disinfection reduces the number of microorganisms, but sterilization eliminates all of them. HLD sits between these extremes, providing a balance between safety and practicality for various medical devices.
Q 7. What are the different types of biological indicators used in sterilization?
Biological indicators (BIs) are used to validate the effectiveness of sterilization processes. They contain a known number of resistant microorganisms (usually spores) that are killed if the sterilization process is successful. Different types of BIs exist:
- Geobacillus stearothermophilus spores: Used for steam sterilization and some liquid chemical sterilization processes. These spores are highly resistant to heat and are killed only under appropriate sterilization conditions.
- Bacillus atrophaeus spores: Used for EtO sterilization and dry heat sterilization. These spores are more resistant to EtO and dry heat than Geobacillus stearothermophilus.
- Spores of Bacillus subtilis: Used for validating some low-temperature sterilization methods such as hydrogen peroxide gas plasma.
After the sterilization cycle, BIs are incubated, and the absence of growth indicates successful sterilization. The presence of growth signals a failure of the sterilization process, necessitating investigation and corrective actions. BIs are vital for ensuring the efficacy of sterilization and patient safety, providing objective evidence that the process is working as intended.
Q 8. How do you interpret the results of biological indicators?
Biological indicators (BIs) are self-contained devices that contain a known population of resistant microorganisms, typically Geobacillus stearothermophilus for steam sterilization or Bacillus atrophaeus for dry heat or ethylene oxide sterilization. They’re used to verify the lethality of a sterilization cycle. Interpreting the results involves checking for growth or no growth after incubation.
No growth indicates successful sterilization; the BI was killed, proving the sterilization process was effective. Growth, however, signifies a failure in the sterilization process. The spores survived, implying inadequate sterilization parameters (temperature, time, or exposure). This necessitates investigation into equipment malfunction, procedural errors, or inadequate cycle parameters.
For example, imagine a steam sterilization cycle for surgical instruments. If the BI shows no growth after incubation, we know the cycle achieved sterility. But if growth is observed, we immediately quarantine all instruments processed in that cycle and investigate potential issues – was the steam generator functioning correctly? Was the chamber properly loaded, ensuring steam penetration? Were the parameters set correctly? A thorough investigation is crucial to prevent further incidents and ensure patient safety.
Q 9. What are the common causes of medical device-related infections?
Medical device-related infections (MDRIs) stem from a complex interplay of factors. They’re not usually caused by a single source but rather a combination of issues.
- Contamination of the device: This can occur during manufacturing, processing, or handling before use. Improper sterilization or disinfection techniques are major culprits.
- Biofilm formation: Biofilms are communities of microorganisms encased in a self-produced matrix that’s highly resistant to antimicrobial agents. Once formed on a medical device’s surface, they are extremely difficult to eradicate.
- Patient factors: Immunocompromised patients are inherently more vulnerable to infections. Existing infections or chronic diseases further increase susceptibility.
- Improper device handling and insertion: Aseptic techniques during device implantation or use are crucial; failure here directly introduces microorganisms.
- Device design and material: Certain materials may be more susceptible to biofilm formation or harbor microorganisms more readily.
For instance, a contaminated catheter can lead to bloodstream infection, while improper sterilization of an arthroscopy instrument can cause a joint infection. Understanding the multifactorial nature of MDRIs is critical for effective prevention strategies.
Q 10. Describe the process of cleaning and disinfecting reusable medical devices.
Cleaning and disinfecting reusable medical devices is a critical, multi-step process aimed at removing gross soil and reducing microbial load before sterilization. It involves several key stages:
- Pre-cleaning: Removing visible soil and organic matter using mechanical methods, like brushing, wiping, or ultrasonic cleaning. This step is crucial as residual organic matter can interfere with subsequent disinfection and sterilization.
- Washing: Thorough rinsing with detergent and water to remove remaining debris. Appropriate detergents are selected based on the device material and type of soil.
- Disinfection: Application of a disinfectant solution appropriate for the device and its intended use to kill or inactivate remaining microorganisms. This step usually involves immersion, spraying, or wiping, followed by a thorough rinse.
- Drying: Complete drying of the device is necessary to prevent microbial growth and to ensure proper sterilization.
Consider endoscopes, for example. Pre-cleaning involves removing any visible tissue or debris from the channels. Then, enzymatic detergents are used to break down organic material before high-level disinfection. The entire process must be meticulously documented to ensure traceability and accountability.
Q 11. What are the different types of disinfectants and their effectiveness?
Different disinfectants have varying levels of effectiveness against different microorganisms. Selection depends on the type of device, level of contamination, and regulatory guidelines. Here are a few examples:
- High-level disinfectants: These inactivate vegetative bacteria, fungi, viruses, and mycobacteria, but may not reliably kill bacterial spores. Examples include glutaraldehyde and ortho-phthalaldehyde.
- Intermediate-level disinfectants: Inactivate vegetative bacteria, most fungi, and some viruses, but not mycobacteria or bacterial spores. Iodophors and some phenolic compounds fall into this category.
- Low-level disinfectants: Inactivate vegetative bacteria and some enveloped viruses, but not mycobacteria, fungi, or bacterial spores. Quaternary ammonium compounds are a common example.
The effectiveness of a disinfectant is influenced by factors such as contact time, concentration, temperature, and the presence of organic matter. It’s crucial to follow manufacturer’s instructions precisely to ensure optimal efficacy. Using a high-level disinfectant on an item only requiring low-level disinfection is wasteful and may unnecessarily damage the device.
Q 12. How do you ensure the proper functioning of sterilization equipment?
Ensuring proper functioning of sterilization equipment is paramount for patient safety. This involves a multifaceted approach:
- Regular preventative maintenance: This includes scheduled inspections, cleaning, and calibration by qualified technicians. Following the manufacturer’s instructions for maintenance is non-negotiable.
- Biological indicator testing: Regular use of BIs ensures the equipment is effectively sterilizing items. Results must be documented and reviewed regularly.
- Mechanical monitoring: Sterilizers incorporate mechanical monitors (pressure gauges, temperature recorders) that provide real-time data during cycles. These need to be checked for accuracy.
- Chemical indicators: These change color to indicate exposure to specific sterilization parameters (e.g., steam, heat). While not as comprehensive as BIs, they provide an immediate visual check.
- Documentation and record keeping: Meticulous documentation of all maintenance, testing, and cycle parameters is essential for traceability and quality assurance.
Ignoring maintenance could lead to equipment malfunction, resulting in ineffective sterilization and increased risk of infection. A well-maintained sterilizer is a cornerstone of a safe and effective sterilization department.
Q 13. What are the key performance indicators (KPIs) for a sterilization department?
Key performance indicators (KPIs) for a sterilization department reflect its effectiveness and efficiency. They should be regularly monitored and analyzed to identify areas for improvement:
- Sterilization cycle failure rate: Percentage of cycles failing BI testing, indicating potential equipment issues or procedural errors.
- Turnaround time: Time taken to process devices from receipt to release, reflecting efficiency.
- Device damage rate: Percentage of damaged devices during processing, indicating potential handling or equipment issues.
- Compliance with sterilization protocols: Assessment of adherence to established procedures, ensuring consistent quality.
- Infection rates related to sterilized devices: Tracking post-sterilization infections linked to the devices processed; a high rate indicates a significant problem.
These KPIs help monitor the overall quality and safety of the sterilization process and guide decision-making regarding improvements. For instance, a consistently high sterilization cycle failure rate might indicate a need for equipment repair or retraining of staff.
Q 14. How do you manage and track medical device recalls?
Managing and tracking medical device recalls is crucial for patient safety. The process typically involves:
- Receipt of recall notification: The department must have a system for receiving official recall notices from manufacturers or regulatory bodies.
- Inventory check: Immediately check the department’s inventory to identify affected devices.
- Quarantine: Isolate and quarantine all recalled devices to prevent their use.
- Return and disposal: Follow the manufacturer’s instructions for returning and disposing of recalled devices. This often involves specialized procedures.
- Documentation: Maintain meticulous records of the entire recall process, including notification, inventory check, quarantine, and return/disposal. This documentation is crucial for audits and regulatory compliance.
- Staff notification and training: Keep staff updated on recall procedures and provide appropriate training.
Recall management requires a well-defined procedure and proactive monitoring of recalls. Failure to promptly address recalls puts patients at risk and can have serious legal and ethical implications. Imagine a recall for a faulty heart valve; effective recall management prevents potentially life-threatening consequences.
Q 15. What are the risks associated with improper medical device reprocessing?
Improper medical device reprocessing carries significant risks, primarily the transmission of healthcare-associated infections (HAIs). These infections can range from minor skin irritations to life-threatening sepsis. The risks stem from inadequate cleaning, disinfection, or sterilization, leaving behind bioburden (the number and type of microorganisms present) that can infect the next patient. This is especially concerning with invasive devices like catheters and surgical instruments.
- Patient harm: Infections can lead to prolonged hospital stays, increased morbidity and mortality, and substantial added healthcare costs.
- Legal ramifications: Hospitals and staff can face legal action from patients suffering from HAIs acquired through improperly reprocessed devices.
- Reputational damage: Outbreaks of HAIs can severely damage a healthcare facility’s reputation and erode public trust.
- Antimicrobial resistance: The overuse of disinfectants can contribute to the development of antimicrobial-resistant microorganisms, further complicating infection control.
Imagine a scenario where a surgical instrument isn’t properly sterilized. Residual bacteria or viruses can then infect the patient during the next procedure, causing a potentially serious infection. This highlights the critical importance of meticulous reprocessing procedures.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with implementing infection control protocols.
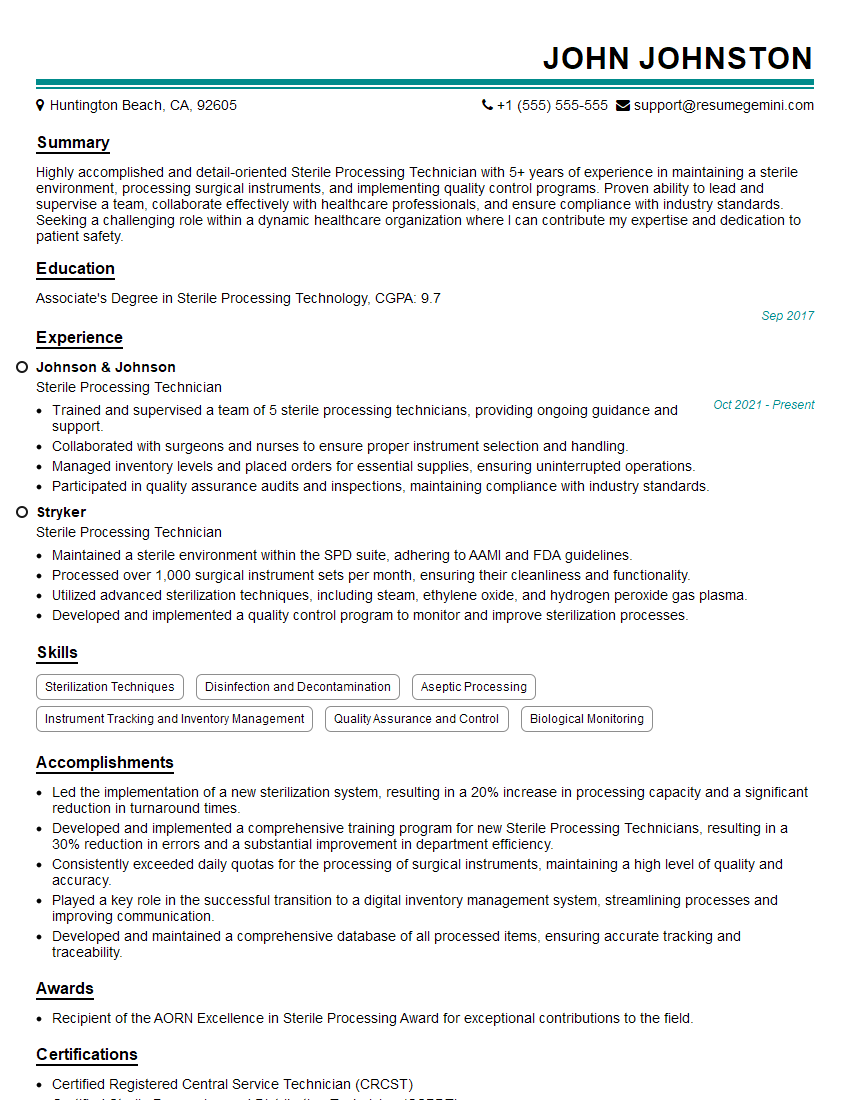
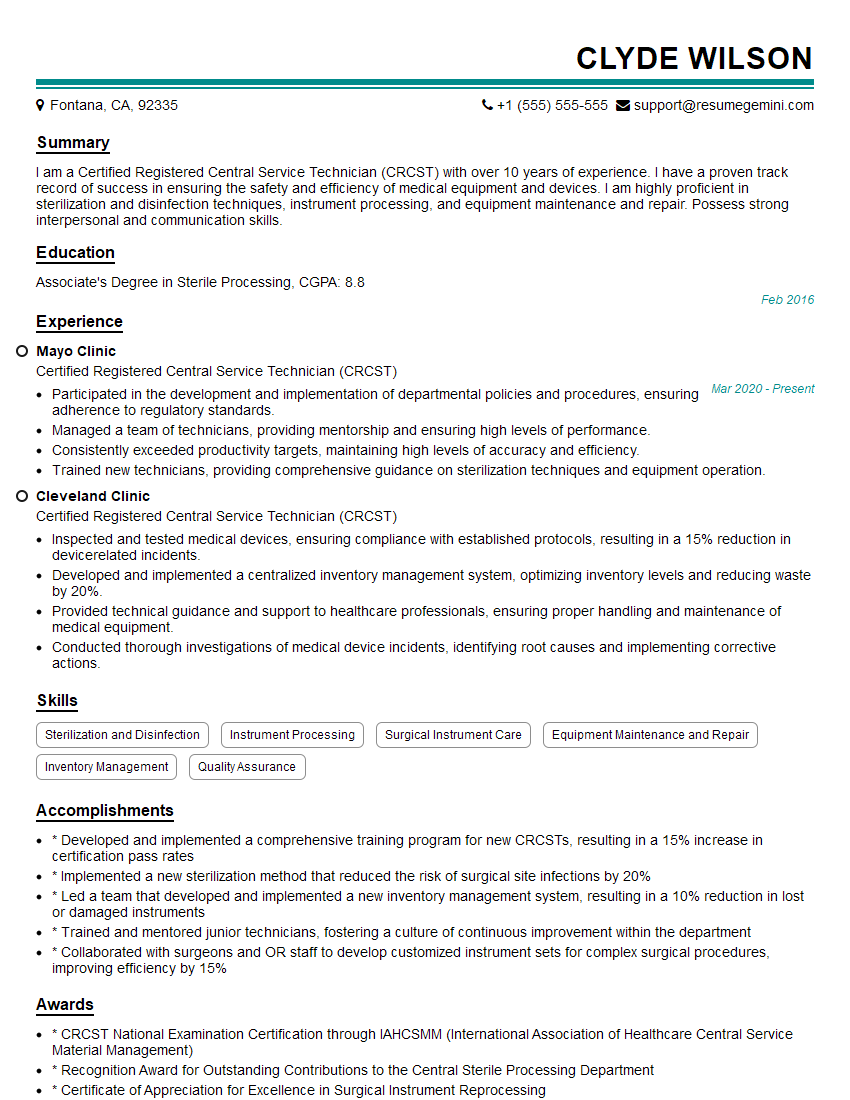
Throughout my career, I’ve been actively involved in implementing and improving infection control protocols across various healthcare settings. This has involved the development and execution of comprehensive training programs for healthcare professionals on proper reprocessing techniques, including meticulous cleaning, appropriate disinfection or sterilization methods, and safe handling procedures. For example, in one hospital, I spearheaded a project to standardize the reprocessing procedures for endoscopes, leading to a significant reduction in HAI rates. This involved not just training but also a complete review of the equipment, workflows and documentation processes to ensure compliance with national standards. We employed a multi-pronged approach, including staff training, updated protocols, and regular audits, leading to a demonstrable decrease in post-procedure infections.
Another significant experience involved the implementation of a new automated endoscope reprocessor. My role included the validation of the reprocessing cycle, staff training on its use, and ongoing monitoring of its effectiveness. This highlighted the importance of embracing new technology while ensuring appropriate training and validation to guarantee safety and effectiveness.
Q 17. How do you monitor and evaluate the effectiveness of infection control measures?
Monitoring and evaluating infection control measures is crucial for continuous improvement. We use a multi-faceted approach. This involves:
- Surveillance data: Tracking HAIs through infection surveillance programs provides vital information on trends, allowing for early detection of potential outbreaks. This involves actively monitoring rates of specific HAIs.
- Environmental monitoring: Regularly testing the environment for the presence of microorganisms helps identify potential sources of contamination. This includes sampling surfaces, air, and water.
- Audits and inspections: Regular audits ensure that protocols are being followed correctly. This includes checking staff competency, equipment maintenance records, and reprocessing documentation.
- Key performance indicators (KPIs): Using relevant metrics, such as HAI rates, sterilization failure rates, and staff compliance, allows for objective evaluation.
- Process capability analysis: Statistical methods can help quantify the consistency and effectiveness of reprocessing procedures.
For example, we might track the rate of post-operative surgical site infections (SSIs) to assess the efficacy of our sterilization techniques. If we see an increase, this triggers a root cause analysis to identify and address the contributing factors.
Q 18. What are the challenges in maintaining infection control in a healthcare setting?
Maintaining infection control in a healthcare setting presents numerous challenges:
- Staffing shortages and workload pressures: Time constraints and high workloads can lead to shortcuts and compromises in infection control practices.
- Resource limitations: Lack of funding for appropriate equipment, training, and supplies can hinder effective infection control.
- Adherence to protocols: Ensuring consistent adherence to complex infection control procedures requires ongoing education, training and reinforcement.
- Emerging pathogens: The constant emergence of new and drug-resistant microorganisms requires continuous adaptation of infection control strategies.
- Complexity of healthcare environments: The diverse range of patients, procedures, and equipment makes maintaining consistent infection control a complex undertaking.
For instance, a busy emergency department may face challenges in ensuring adequate cleaning and disinfection between patient encounters due to high patient volume. Similarly, ensuring consistent compliance with hand hygiene protocols across all staff requires a robust education and reinforcement program.
Q 19. What is your experience with medical device cleaning validation?
Medical device cleaning validation is a critical component of ensuring the safety and efficacy of reprocessing. It’s a rigorous process to demonstrate that the chosen cleaning methods effectively remove bioburden from medical devices. This involves a multi-step process:
- Defining cleaning requirements: Establishing specific requirements for acceptable levels of bioburden remaining after cleaning.
- Selecting cleaning methods: Choosing appropriate cleaning agents and techniques based on the device type and bioburden.
- Developing a cleaning protocol: Creating a detailed step-by-step procedure for cleaning the device.
- Validation testing: Performing rigorous testing to demonstrate that the cleaning process consistently meets the predefined requirements. This may involve using ATP bioluminescence, microbiological testing, and visual inspection.
- Documentation: Maintaining comprehensive documentation of the entire validation process.
I have extensive experience in this area, having led numerous cleaning validation studies for a variety of medical devices. A recent example involved validating a new automated cleaning system for surgical instruments. This process involved rigorous testing using various bioburden simulants, ensuring the system consistently met the required cleanliness levels before implementation.
Q 20. What are your strategies for continuous improvement in infection control?
Continuous improvement in infection control requires a proactive and data-driven approach. My strategies include:
- Regular review of protocols: Periodic review and updates of infection control procedures to incorporate best practices and address emerging challenges.
- Staff education and training: Providing regular, ongoing training to staff on infection control principles and techniques, particularly emphasizing new technologies or changing guidelines.
- Data analysis and trend monitoring: Continuously monitoring HAI rates and other KPIs to identify areas for improvement and track the effectiveness of implemented changes.
- Benchmarking: Comparing performance against similar healthcare facilities to identify best practices and areas for improvement.
- Participation in professional organizations and conferences: Staying abreast of the latest research, guidelines, and advancements in infection control.
For example, if we see a rise in catheter-related bloodstream infections, we would perform a root cause analysis to identify potential problems in our catheter insertion or maintenance protocols. This might involve reviewing staff training, improving adherence to hand hygiene guidelines, or implementing new catheter types with improved infection prevention features.
Q 21. How do you communicate effectively with healthcare professionals regarding infection control?
Effective communication is paramount for successful infection control. My approach centers on:
- Clear and concise messaging: Using plain language, avoiding jargon, and tailoring communication to the audience’s level of understanding.
- Multimodal communication: Utilizing a range of communication channels, such as training sessions, written materials, posters, and regular updates, to reach all healthcare professionals effectively.
- Interactive communication: Encouraging questions and feedback to ensure comprehension and address concerns.
- Collaboration and teamwork: Working collaboratively with healthcare professionals across different departments to ensure a cohesive approach to infection control.
- Feedback mechanisms: Establishing systems for providing and receiving feedback on infection control practices to identify areas for improvement.
For instance, I might present a short, informative session on hand hygiene techniques to a group of nurses, followed by a Q&A session to address any specific questions or concerns. Regular updates and reminders through emails, posters and staff meetings, ensures consistent engagement.
Q 22. Describe your knowledge of relevant industry standards and guidelines (e.g., AAMI, CDC).
My understanding of biomedical device infection control is deeply rooted in adherence to key industry standards and guidelines. I’m intimately familiar with the standards published by the Association for the Advancement of Medical Instrumentation (AAMI), and the Centers for Disease Control and Prevention (CDC). AAMI provides detailed guidance on sterilization, disinfection, and the overall management of medical devices, offering specific standards for various sterilization methods (like steam sterilization in autoclaves, ethylene oxide sterilization, and others) and process validation. The CDC, on the other hand, focuses on the broader aspects of infection prevention and control within healthcare settings, providing guidelines on hand hygiene, environmental cleaning, and outbreak management. Their recommendations directly influence how we approach device handling and patient safety protocols. For example, AAMI TIR30:2008 gives specific guidance on steam sterilization, while CDC guidelines on hand hygiene are vital before and after handling any medical device, even after cleaning and sterilization. My professional experience ensures I apply these standards rigorously in practice, constantly updating my knowledge to reflect the latest recommendations and advancements in the field.
Q 23. Explain the difference between sterilization and disinfection.
Sterilization and disinfection are both crucial for infection control, but they achieve different levels of microbial reduction. Think of it like this: disinfection is like cleaning your kitchen counter—it removes most germs, leaving it safe for food preparation. Sterilization is like sterilizing surgical instruments—it eliminates all forms of microbial life, including bacteria, viruses, fungi, and spores. Disinfection uses chemical agents or physical methods (like heat) to reduce the number of microorganisms to a safe level. Common disinfectants include alcohols, chlorine-based solutions, and quaternary ammonium compounds. Sterilization, however, employs more rigorous methods to achieve complete microbial inactivation. This typically includes steam sterilization (autoclaving), ethylene oxide (EtO) gas sterilization, or radiation sterilization. The choice between sterilization and disinfection depends on the intended use of the device and the level of microbial control required. A reusable surgical instrument needs sterilization, while a non-critical item may only need disinfection.
Q 24. How do you handle a situation where a contaminated device is discovered?
Discovering a contaminated device is a serious event requiring immediate and decisive action. My response follows a structured protocol to mitigate risk and prevent further contamination. First, I would immediately isolate the contaminated device to prevent accidental contact or spread. Then, I would thoroughly document the incident, including details such as the type of device, the suspected source of contamination, and the time of discovery. Next, I would initiate a thorough investigation to determine the root cause of the contamination. This might involve reviewing sterilization logs, examining cleaning and handling procedures, and interviewing personnel who handled the device. Based on the investigation, corrective actions will be implemented to prevent recurrence. These actions could involve retraining staff, modifying procedures, or replacing equipment. Finally, I would report the incident to the appropriate authorities and initiate any necessary recall procedures if the contamination poses a significant risk to patient safety. For instance, if a contaminated catheter was identified post-surgery, immediate action would be taken to inform the surgical team and initiate patient monitoring, in accordance with established protocols.
Q 25. What are your experience with different types of sterilization equipment (e.g., autoclaves, EtO sterilizers)?
I have extensive experience with various sterilization equipment, including autoclaves (steam sterilizers) and EtO sterilizers. Autoclaves use high-pressure steam to kill microorganisms, and I am proficient in operating and maintaining different types of autoclaves, ensuring proper temperature and pressure parameters are met for validated sterilization cycles. I understand the critical role of appropriate packaging materials, loading procedures and cycle validation in guaranteeing effective sterilization. With EtO sterilizers, I’m familiar with the process of using ethylene oxide gas to sterilize heat-sensitive medical devices. This involves understanding the need for aeration to remove residual EtO gas to safe levels. My experience includes validating sterilization cycles for both autoclaves and EtO sterilizers, ensuring compliance with AAMI standards and regulatory requirements. I also understand the limitations of each technology and how to select the appropriate method based on the device’s characteristics and materials. For instance, heat-sensitive implants necessitate EtO sterilization, while reusable surgical instruments are ideal for autoclaving.
Q 26. What is your understanding of the role of environmental monitoring in infection control?
Environmental monitoring is paramount in infection control. It provides a comprehensive assessment of the cleanliness and sterility of the environment where medical devices are handled and used. This involves regularly monitoring various surfaces for microbial contamination, using techniques such as surface sampling, air sampling, and water testing. The data generated from environmental monitoring helps identify potential sources of contamination, enabling proactive measures to reduce infection risks. For example, consistent high counts of a specific bacteria on a particular work surface indicate a problem with cleaning practices, requiring immediate remediation and staff retraining. Analysis of the data allows us to assess the effectiveness of infection control measures and inform modifications to protocols, further strengthening the overall infection control program. Regular environmental monitoring serves as an early warning system, allowing for swift interventions to prevent the spread of infections and safeguard patient safety.
Q 27. Describe your experience with performing risk assessments related to medical device infection control.
Risk assessment in medical device infection control is a crucial process I’ve been involved in many times. It systematically identifies potential hazards associated with the use of medical devices and evaluates the likelihood and severity of infection risks. This involves considering various factors, including the type of device, the procedure in which it’s used, and the patient population. I utilize a structured approach, often using Failure Mode and Effects Analysis (FMEA) or Hazard Analysis and Critical Control Points (HACCP), to systematically identify potential risks. For example, a risk assessment for a catheter would consider factors such as the material, sterilization method, insertion procedure, and patient susceptibility to infection. Based on the assessment, preventive measures such as modifying procedures, selecting appropriate materials, or providing additional training can be implemented to mitigate these risks. Effective risk assessments contribute to a more robust infection control program and proactively reduce the chances of device-related infections.
Q 28. How would you handle a conflict with a colleague regarding infection control practices?
Conflict resolution is a vital skill in any collaborative environment, especially in infection control where adherence to strict protocols is paramount. If a conflict arises regarding infection control practices, I would first approach the situation with professionalism and respect, aiming to understand my colleague’s perspective. I’d actively listen to their concerns and explain my reasoning based on established guidelines and best practices. If a compromise can’t be reached through discussion, I would involve a supervisor or manager to mediate the conflict. My goal would always be to find a solution that ensures patient safety while fostering a positive working relationship. The focus is on finding common ground and upholding the highest standards of infection prevention, even if it means revisiting and revising a procedure in consultation with senior members of the team. Ultimately, patient safety should always be the driving force behind any decision in this crucial area.
Key Topics to Learn for Biomedical Device Infection Control Interview
- Sterilization Techniques: Understand the principles and applications of various sterilization methods (e.g., steam sterilization, ethylene oxide, gamma irradiation) and their impact on device integrity and efficacy.
- Aseptic Processing: Master the principles and practices of aseptic processing and cleanroom environments, including environmental monitoring and contamination control strategies.
- Infection Control Policies and Regulations: Familiarize yourself with relevant regulations (e.g., FDA guidelines, ISO standards) and hospital infection control policies related to biomedical devices.
- Risk Assessment and Management: Learn how to conduct thorough risk assessments for biomedical devices to identify and mitigate potential infection risks throughout the device lifecycle.
- Bioburden and Endotoxin Testing: Understand the methods used to quantify microbial contamination (bioburden) and endotoxins in biomedical devices and their interpretation.
- Disinfection and Decontamination: Know the difference between disinfection and decontamination procedures and their appropriate applications for various devices and situations.
- Material Selection and Compatibility: Understand how material choices impact device sterilization and durability, and the importance of material compatibility with sterilization processes.
- Quality Assurance and Regulatory Compliance: Learn about quality control procedures, documentation requirements, and regulatory compliance crucial for maintaining infection control standards.
- Case Studies and Problem-Solving: Prepare to discuss real-world scenarios and apply your knowledge to solve problems related to device contamination or infection prevention.
- Emerging Technologies and Trends: Stay updated on the latest advancements in sterilization technologies and infection control strategies within the biomedical device field.
Next Steps
Mastering Biomedical Device Infection Control is crucial for a successful and rewarding career in this vital field. A strong understanding of these principles opens doors to advanced roles and leadership opportunities within medical device companies, healthcare facilities, and regulatory agencies. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to your specific experience and career goals. We provide examples of resumes specifically designed for Biomedical Device Infection Control professionals, giving you a head start in presenting your qualifications effectively. Invest the time to create a powerful resume – it’s your first impression with potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good