Cracking a skill-specific interview, like one for Biomedical Device Innovation and Commercialization, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Biomedical Device Innovation and Commercialization Interview
Q 1. Explain the design control process for medical devices.
Design control in medical device development is a systematic process ensuring a device meets its intended use and required performance. It’s essentially a roadmap guiding the entire design process from initial concept to final product release, ensuring safety and efficacy. This process is meticulously documented and auditable.
- Planning: This initial phase defines the device’s intended use, target users, and performance requirements. It also establishes the overall design and development plan.
- Input: Gathering necessary information, including user needs, market research, and technological feasibility studies. For example, gathering data on the effectiveness of different materials or investigating alternative design approaches.
- Design Output: Creating detailed design specifications, drawings, and protocols. This ensures clarity and consistency throughout the process. Think of it as constructing a blueprint for the device.
- Design Review: Regular reviews are conducted to assess the design’s progress, identify potential risks, and ensure compliance with regulatory requirements. This involves multi-disciplinary teams that can identify blind spots.
- Verification & Validation: Verification confirms the design meets the pre-defined specifications, while validation demonstrates the finished device functions as intended in its intended use environment. This often involves rigorous testing.
- Design Transfer: This crucial step transfers the approved design to manufacturing, ensuring the final product consistently meets the design specifications.
- Design Changes: A well-defined change control process ensures any modifications to the design are thoroughly reviewed, documented, and approved before implementation. This prevents deviations from the validated design.
A real-world example might involve the design of a new insulin pump. The design control process would meticulously outline the required accuracy of insulin delivery, safety features to prevent overdoses, material compatibility with the human body, and user interface considerations. Each step would be meticulously documented, meeting stringent regulatory requirements.
Q 2. Describe your experience with FDA regulations (e.g., 510(k), PMA).
I have extensive experience navigating FDA regulations, particularly 510(k) premarket notifications and Premarket Approvals (PMAs). My work has involved numerous submissions, including devices ranging from Class II to Class III. The process is significantly different depending on the device’s classification and intended use.
For 510(k) submissions, the focus is on demonstrating substantial equivalence to a legally marketed predicate device. This requires a thorough comparison of the design, performance characteristics, and intended use. I’ve personally handled numerous 510(k) submissions, working closely with the FDA to address any questions or concerns and ensuring a smooth regulatory pathway.
PMA submissions are far more rigorous, requiring extensive clinical data demonstrating the safety and effectiveness of the device. My experience includes participating in the design and execution of clinical trials, compiling the necessary data packages for the submission, and managing interactions with the FDA review team. I am very familiar with the required documentation and the thorough review process involved in securing a PMA. This process is significantly more complex and time-consuming but essential for higher-risk devices.
Q 3. How do you manage risk in the development of a biomedical device?
Risk management is paramount in biomedical device development. We employ a systematic approach using tools like Failure Modes and Effects Analysis (FMEA) and Hazard Analysis and Risk Control (HARC) to identify, assess, and mitigate potential hazards throughout the product lifecycle. This involves proactively identifying potential failures, evaluating their severity, likelihood of occurrence, and developing mitigation strategies.
For instance, during the design phase, we might identify a risk of the device overheating. Through FMEA, we would evaluate the severity of overheating (potentially causing burns), the likelihood of it occurring (based on simulations and testing), and the detectability of the problem (through temperature sensors). Based on this analysis, we would implement mitigation strategies such as adding thermal protection mechanisms or implementing alerts to notify users of high temperatures. We maintain a comprehensive risk management plan throughout the development, and post-market surveillance continuously monitors for risks. Effective risk management minimizes negative health outcomes and ensures patient safety.
Q 4. What are the key factors to consider when commercializing a new medical device?
Commercializing a new medical device is a complex process requiring careful consideration of several key factors:
- Market Analysis: Thoroughly understanding the target market, identifying unmet needs, and analyzing the competitive landscape is crucial. This includes considering market size, potential customer segments, and regulatory hurdles.
- Reimbursement Strategy: Securing reimbursement from healthcare payers is vital for long-term market success. This involves preparing clinical and economic data to support coverage decisions.
- Manufacturing & Supply Chain: Establishing a reliable manufacturing process and supply chain is essential for ensuring consistent product quality and availability. This needs to be scaled to meet anticipated demand.
- Sales & Marketing: Developing a robust sales and marketing strategy to effectively reach the target market is essential. This includes building a strong sales team and creating marketing materials targeted at healthcare professionals and potential patients.
- Regulatory Strategy: A well-defined regulatory strategy that ensures timely approvals and compliance with all relevant standards is crucial for market access.
- Intellectual Property (IP): Protecting the intellectual property associated with the device is critical to maintaining a competitive edge. This involves patents and trade secrets.
- Financial Projections & Funding: Secure sufficient funding and develop realistic financial projections to manage the commercialization process. This may involve securing venture capital or seeking strategic partnerships.
A successful commercialization plan requires a holistic view, integrating these elements into a cohesive and well-executed strategy. Ignoring any of these aspects can significantly impact the device’s market success.
Q 5. Explain your understanding of Design Failure Mode and Effects Analysis (DFMEA).
Design Failure Mode and Effects Analysis (DFMEA) is a systematic approach to identify potential failure modes in a design, evaluate their effects, and determine the severity and probability of each failure. It’s a proactive risk management tool that helps prevent failures before they occur, focusing on designing for reliability and safety.
The DFMEA process typically involves a team brainstorming potential failure modes in each component or subsystem of the device. For each failure mode, the team assesses the severity (how bad the consequences would be), the occurrence (how likely the failure is to happen), and the detection (how likely the failure would be detected before reaching the end-user). These values are typically ranked on a numerical scale, and the resulting Risk Priority Number (RPN) helps prioritize mitigation efforts. A high RPN indicates a high-risk failure mode needing immediate attention.
For example, in a pacemaker, a potential failure mode might be the battery failing prematurely. The team would assess the severity (potentially life-threatening), the occurrence (based on historical data and battery testing), and the detection (could be detected via monitoring systems or patient symptoms). Based on the RPN, they might implement strategies such as using a higher-capacity battery or incorporating redundant battery systems. The results of the DFMEA are documented and reviewed throughout the product lifecycle.
Q 6. Describe your experience with ISO 13485.
ISO 13485 is an internationally recognized standard for quality management systems (QMS) specific to medical devices. It provides a framework for organizations to demonstrate their ability to consistently provide medical devices that meet customer and regulatory requirements. Compliance with ISO 13485 is often a prerequisite for obtaining regulatory approvals in many countries, including the U.S. and the European Union.
My experience with ISO 13485 encompasses implementing, maintaining, and auditing quality management systems in several medical device companies. This includes establishing documented procedures, conducting internal audits, implementing corrective and preventive actions (CAPA), and managing risk. I’m familiar with all the key requirements of the standard, including requirements for design and development, risk management, purchasing, production, and post-market surveillance. Successfully obtaining and maintaining ISO 13485 certification demonstrates a commitment to quality and regulatory compliance. It builds trust and credibility with regulators, customers, and partners.
Q 7. How do you balance innovation with regulatory compliance?
Balancing innovation with regulatory compliance is a constant challenge in medical device development. It’s not a trade-off but rather a synergistic relationship. Regulatory compliance shouldn’t stifle innovation; instead, it should guide and shape it to ensure safety and effectiveness.
To achieve this balance, we incorporate regulatory requirements early in the design process. We don’t wait until the end to address compliance issues. Instead, we actively incorporate regulatory considerations throughout the entire design and development lifecycle. This includes thorough risk assessments, rigorous testing protocols, and meticulous documentation. We leverage design control processes that inherently incorporate regulatory needs. This proactive approach ensures the device meets all necessary requirements while allowing for creativity and flexibility in design and functionality. Continuous monitoring of evolving regulations and technologies is also important to remain compliant and competitive.
For example, incorporating feedback from early regulatory interactions helps shape the design and testing plans, ensuring the device meets the necessary requirements without compromising its innovative features. It’s about designing for both patient safety and market acceptance.
Q 8. What are the different types of medical device classifications and their implications?
Medical devices are classified based on their risk to the patient, with classifications dictating the regulatory pathway and requirements for approval. The higher the risk, the more stringent the regulations. In the US, the Food and Drug Administration (FDA) uses a system generally categorized as Class I, II, and III.
- Class I: These are low-risk devices, often requiring only general controls like good manufacturing practices. Examples include bandages, hand-held surgical instruments, and some diagnostic tools. The regulatory burden is minimal.
- Class II: These devices present moderate risk and require special controls in addition to general controls. This might include performance standards, labeling requirements, or post-market surveillance. Examples include powered wheelchairs, infusion pumps, and many diagnostic imaging systems. This category involves more rigorous testing and documentation.
- Class III: These are high-risk devices that support or sustain human life, or present a potential for unreasonable risk of illness or injury. They require premarket approval (PMA) from the FDA, the most stringent regulatory process. Examples include implantable pacemakers, heart valves, and certain types of software used in medical devices. This requires extensive clinical trials and rigorous documentation of safety and efficacy.
Understanding these classifications is critical because it impacts the time and cost involved in bringing a device to market, as well as the required testing, documentation, and ongoing surveillance. A Class III device will require significantly more resources than a Class I device.
Q 9. Explain your experience with clinical trials and data analysis.
My experience spans the entire clinical trial process, from protocol design and IRB submissions to data collection, analysis, and reporting. I’ve worked on multiple trials for various medical devices, including a pivotal study for a novel drug-eluting stent.
Data analysis is a key component of this work. I am proficient in statistical software like R and SAS, and use these tools to analyze clinical trial data, assess device safety and efficacy, and prepare reports for regulatory submissions. For the stent trial, for instance, we used Kaplan-Meier analysis to compare event rates (e.g., restenosis) between the experimental and control groups, and Cox proportional hazards models to adjust for confounding variables. This analysis was crucial in demonstrating the superiority of the novel stent.
Beyond statistical analysis, I understand the importance of data integrity, regulatory compliance, and clear communication of findings. A rigorous approach is crucial to ensuring that results are credible and can be used to support regulatory approvals.
Q 10. How do you identify and evaluate market opportunities for medical devices?
Identifying market opportunities requires a multifaceted approach combining market research, clinical need assessment, and competitive analysis. I typically start by analyzing unmet clinical needs and current treatment limitations. This involves reviewing medical literature, conducting physician interviews, and attending industry conferences.
Next, I delve into market research to gauge the size and potential of a target market. This includes examining market reports, analyzing sales data, and understanding reimbursement scenarios.
Finally, competitive analysis helps determine a device’s unique selling points and potential competitive advantage. This involves identifying key competitors, analyzing their strengths and weaknesses, and understanding the competitive landscape. For example, when we were developing a new minimally invasive surgical tool, we identified a large unmet need for less-invasive procedures and a competitive landscape dominated by larger, more complex devices. Our device focused on simplicity and ease of use, targeting a niche within the existing market.
This three-pronged approach – unmet need, market analysis, and competitive landscape – is essential in ensuring that a medical device can successfully enter the market and achieve commercial success.
Q 11. Describe your experience with intellectual property protection for medical devices.
Protecting intellectual property (IP) is critical for any medical device company. My experience encompasses various IP strategies, including patent filings, trade secret protection, and trademark registration. I’ve worked with patent attorneys to draft and file patent applications for novel device designs, manufacturing processes, and software algorithms.
For example, when developing a novel sensor technology, we filed patents on both the device’s unique design and the underlying signal-processing algorithm. This provided broad protection for our innovation. Furthermore, maintaining meticulous records detailing inventions and their development is crucial for supporting IP claims and ensuring trade secret protection.
Understanding the IP landscape and the strategic application of various IP protection mechanisms is vital to safeguarding a company’s investment and ensuring market exclusivity for its products.
Q 12. How do you develop a marketing strategy for a medical device?
Developing a marketing strategy for a medical device requires a deep understanding of the target audience – clinicians, hospitals, and patients – as well as regulatory requirements. A successful strategy incorporates several key elements:
- Target Audience Segmentation: Defining specific target audiences (e.g., cardiologists, orthopedic surgeons, etc.) allows for tailored messaging and marketing materials.
- Value Proposition: Clearly articulating the device’s clinical benefits, economic advantages, and ease of use.
- Marketing Channels: Utilizing appropriate channels, including medical journals, conferences, direct sales representatives, and digital marketing. For example, a minimally invasive device might benefit from video demonstrations shown at surgical conferences.
- Regulatory Compliance: Adhering to all advertising and promotional regulations, ensuring truthful and non-misleading information.
- Key Performance Indicators (KPIs): Defining metrics for success, such as market share, sales figures, and customer satisfaction.
A well-defined marketing strategy, aligned with the overall business objectives, is essential for successful commercialization of a medical device. It’s not enough to have a good product; you need a strategy to effectively communicate its value to the target audience.
Q 13. Explain your understanding of cost-effectiveness analysis in healthcare.
Cost-effectiveness analysis (CEA) in healthcare assesses the value of a medical intervention relative to its cost. It aims to determine whether a particular treatment, like a new medical device, provides a greater benefit per dollar spent than alternative treatments.
CEA typically involves comparing different treatment options based on their effectiveness (measured by relevant clinical outcomes) and their costs (including acquisition, implementation, and ongoing maintenance). The results are often expressed as an incremental cost-effectiveness ratio (ICER), which shows the additional cost per unit of additional benefit gained by choosing one option over another. For example, an ICER might show the extra cost per additional year of life gained using a new device versus a standard treatment.
Understanding CEA is vital for medical device companies to demonstrate the value proposition of their products to healthcare providers and payers. Demonstrating cost-effectiveness can significantly improve market access and adoption.
Q 14. How do you build a strong business case for a new medical device?
Building a strong business case for a new medical device requires a compelling narrative demonstrating its clinical value, market potential, and financial viability. It should include:
- Clinical Need & Value Proposition: Clearly articulating the unmet clinical need the device addresses and its advantages over existing solutions. This section often includes clinical trial data.
- Market Analysis: Detailed market research showing the target market’s size, growth potential, and competitive landscape. This includes projections of revenue and market share.
- Financial Projections: Realistic financial forecasts encompassing development costs, manufacturing costs, marketing expenses, and projected revenues. This also includes return-on-investment (ROI) analysis.
- Regulatory Strategy: Outline of the regulatory pathway and timeline for obtaining necessary approvals.
- Team & Management: Highlighting the experience and capabilities of the management team and key personnel.
- Risk Assessment & Mitigation: Identifying potential risks and outlining strategies for mitigating them.
A well-structured business case serves as a roadmap for investors and potential partners, demonstrating the device’s potential for both clinical and commercial success. It’s essentially a persuasive argument for investment and adoption.
Q 15. Describe your experience with supply chain management in the medical device industry.
Supply chain management in the medical device industry is incredibly complex, demanding meticulous oversight across the entire product lifecycle. It’s not just about sourcing raw materials; it’s about ensuring the consistent availability of high-quality components, managing manufacturing processes, and delivering finished devices to end-users reliably and efficiently, all while adhering to stringent regulatory requirements.
My experience encompasses all these aspects. In a previous role, I was responsible for optimizing the supply chain for a novel cardiac implant. This involved identifying and qualifying reliable suppliers for critical components like sensors and microprocessors, negotiating contracts to secure favorable pricing and delivery terms, and implementing robust inventory management systems to minimize stockouts and prevent obsolescence. We leveraged lean manufacturing principles and predictive analytics to forecast demand accurately, preventing costly shortages and ensuring timely delivery to hospitals and distribution centers. Furthermore, I actively participated in risk mitigation strategies, building relationships with secondary suppliers to ensure business continuity in case of unforeseen disruptions such as natural disasters or supplier issues.
A significant challenge was managing the global nature of the supply chain. We had components sourced from multiple countries, each with its own regulations and logistical complexities. Addressing these required close coordination with international partners, careful planning for customs clearance, and proactive management of potential shipping delays.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the ethical considerations in the development and commercialization of medical devices?
Ethical considerations in medical device development and commercialization are paramount. The safety and well-being of patients must always be the top priority. This translates into several key areas:
- Transparency and Honesty: Clearly and accurately representing the device’s capabilities and limitations in marketing materials and regulatory submissions is crucial. Exaggerated claims or misleading information are ethically unacceptable.
- Data Integrity: Rigorous and unbiased clinical trials are essential to demonstrate the safety and efficacy of the device. Manipulating data or selectively reporting results compromises the integrity of the entire process and can have severe consequences for patients.
- Accessibility and Affordability: While innovation is key, ensuring that life-saving devices are accessible to all patients, regardless of their socioeconomic status, is an important ethical responsibility. Pricing strategies should be transparent and fairly reflect the value proposition without exploiting patients’ vulnerabilities.
- Privacy and Data Security: Many modern medical devices collect patient data. Protecting this data’s confidentiality and security is an ethical imperative. This includes adhering to relevant data privacy regulations like HIPAA and GDPR.
- Conflicts of Interest: Maintaining transparency and avoiding conflicts of interest in all stages of development and commercialization is critical. For example, disclosing financial relationships with researchers or regulatory bodies is essential to preserve trust and credibility.
In practice, this means establishing robust ethical review boards, adhering to stringent internal guidelines, and fostering a culture of ethical conduct throughout the organization.
Q 17. How do you handle conflicts between engineering, marketing, and regulatory requirements?
Conflicts between engineering, marketing, and regulatory requirements are common in medical device development. A proactive, collaborative approach is essential to navigate these tensions effectively.
My strategy typically involves establishing a cross-functional team with representatives from each department. We use a structured decision-making process, emphasizing open communication and data-driven discussions. We begin by clearly defining the device’s core functionalities and target market. Engineering defines the technical specifications, considering manufacturability and cost-effectiveness. Marketing outlines the desired features and clinical claims. Regulatory affairs identifies the necessary compliance requirements and potential hurdles. Then, we work collaboratively to find solutions that satisfy all three imperatives. This might involve compromises or iterations in design, marketing messaging, or clinical study design. For instance, a particular engineering feature might need to be simplified for improved manufacturability while still meeting regulatory standards. Similarly, marketing claims might need to be refined to reflect the actual device performance data and comply with regulatory requirements.
Ultimately, mediation and consensus building are key to resolving conflicts fairly and efficiently, always prioritizing patient safety and regulatory compliance.
Q 18. Describe your experience with project management methodologies in the context of medical device development.
I have extensive experience utilizing various project management methodologies in medical device development, primarily Agile and Waterfall. The choice of methodology depends on the project’s nature, complexity, and regulatory requirements.
For projects with well-defined requirements and minimal anticipated changes, a Waterfall approach can be effective. This involves a sequential process with clearly defined phases (requirements, design, development, testing, deployment). For projects with evolving requirements, greater uncertainty, or a need for rapid iteration, an Agile approach is often more suitable. This involves iterative development cycles (sprints) with frequent feedback loops, allowing for flexibility and adaptation throughout the development process. In practice, a hybrid approach, combining elements of both methodologies, is often most effective in medical device development.
Irrespective of the chosen methodology, rigorous risk management is crucial. This involves identifying potential risks early on, assessing their likelihood and impact, and developing mitigation strategies. Detailed documentation and traceability throughout the project lifecycle are also essential for regulatory compliance and auditability.
I routinely use project management tools like Jira and MS Project to track progress, manage tasks, and ensure accountability. Effective communication is critical; I regularly hold team meetings to review progress, address roadblocks, and ensure everyone is aligned on goals and deadlines.
Q 19. Explain your understanding of biocompatibility testing.
Biocompatibility testing is a crucial aspect of medical device development, aimed at ensuring that the device doesn’t elicit harmful biological reactions when it comes into contact with living tissues, blood, or bodily fluids. It’s a rigorous process involving a series of tests to evaluate the device’s compatibility with the body.
These tests are guided by international standards like ISO 10993, which outlines different tests based on the device’s intended use and duration of contact with the body. Common tests include cytotoxicity (assessing cell death), genotoxicity (evaluating DNA damage), sensitization (detecting allergic reactions), and irritation (measuring inflammation). The selection of tests depends on the material, the intended application, and the duration of contact with the body. For instance, a short-term contact device like a bandage might require fewer tests compared to a long-term implantable device.
The results of biocompatibility testing are crucial for regulatory submissions, demonstrating that the device is safe for its intended use. Any adverse effects identified must be addressed through material modification or design changes. Failure to conduct adequate biocompatibility testing can lead to product recalls or regulatory rejection.
Q 20. How do you define success in the development and launch of a new medical device?
Defining success in medical device development and launch is multifaceted and goes beyond just achieving regulatory approval or market entry. It requires a holistic perspective encompassing several factors.
- Patient Benefit: Ultimately, success hinges on demonstrably improving patient outcomes. This could involve improved treatment efficacy, reduced complications, enhanced quality of life, or increased longevity.
- Regulatory Approval: Securing regulatory clearance from bodies like the FDA (in the US) or the EMA (in Europe) is a critical milestone, demonstrating the device’s safety and effectiveness.
- Commercial Success: Achieving sustainable market adoption and generating positive revenue streams are essential for long-term viability. This involves effective marketing, strategic pricing, and efficient distribution channels.
- Clinical Utility: The device should be effectively used by healthcare professionals, integrated into existing clinical workflows, and provide demonstrable value within the healthcare system.
- Return on Investment (ROI): The development and commercialization process must demonstrate a financially viable return for investors.
For example, the success of a new minimally invasive surgical device wouldn’t be measured solely by sales figures but also by its impact on reducing hospital stay duration, improving patient recovery time, and minimizing complications. The entire process needs to be assessed across all these factors.
Q 21. What are the key performance indicators (KPIs) used to track the success of a medical device?
Key Performance Indicators (KPIs) used to track the success of a medical device vary depending on the stage of the product lifecycle and the specific goals. Some common KPIs include:
- Pre-launch KPIs: Development costs, time to market, regulatory approval timelines, and the number of patents secured.
- Post-launch KPIs: Market share, sales revenue, gross margin, customer satisfaction scores (CSAT), net promoter score (NPS), device utilization rates, and patient reported outcome measures (PROMs) like quality of life scores.
- Safety and Efficacy KPIs: Post-market surveillance data, including adverse event rates, device failures, and overall effectiveness in clinical practice. This is extremely important and often under-appreciated.
- Manufacturing KPIs: Production yield, defect rates, and cost of goods sold (COGS).
- Return on Investment (ROI) and payback period: These track the financial performance of the device and help assess its long-term viability.
The choice of KPIs should be strategic and aligned with the overarching goals of the company and the specific device. Regular monitoring and analysis of these KPIs are essential for making informed decisions, identifying areas for improvement, and ensuring the continued success of the medical device.
Q 22. Describe a situation where you had to troubleshoot a technical problem during device development.
During the development of a minimally invasive surgical tool, we encountered significant challenges with the actuator mechanism. The initial prototype, designed for precise tissue manipulation, exhibited inconsistent force delivery and occasional jamming. This directly impacted the device’s efficacy and safety.
Our troubleshooting process began with a systematic review of the design specifications and manufacturing process. We meticulously analyzed the CAD models, paying close attention to tolerances and material properties. We then conducted a series of controlled experiments, systematically varying parameters such as actuation pressure, lubricant viscosity, and component materials. We utilized high-speed cameras to visualize the mechanism’s movement during operation, pinpointing the source of the jamming to friction between the actuator shaft and its housing.
The solution involved a multi-pronged approach: refining the surface finish of the components, optimizing the lubricant composition, and slightly modifying the housing design to reduce contact pressure. We also implemented a sensor to monitor the actuator’s force and detect potential jamming in real-time. Through these iterative steps, we eliminated the jamming issue and significantly improved the consistency of force delivery, leading to a much safer and more effective device.
Q 23. How do you manage competing priorities and deadlines in a fast-paced environment?
Managing competing priorities and deadlines in the fast-paced medical device industry requires a structured approach. I utilize a combination of project management methodologies, like Agile, and prioritization techniques, such as the MoSCoW method (Must have, Should have, Could have, Won’t have). This helps to clearly define what’s crucial and what can be deferred.
I begin by breaking down large projects into smaller, manageable tasks, assigning realistic timelines to each. This allows for better tracking of progress and identification of potential bottlenecks early on. I use tools like Jira or Asana to manage tasks and track progress, ensuring transparency and accountability among team members. Regular stand-up meetings are critical for quick problem identification and collaborative solution-finding. Furthermore, open communication and clear expectations are paramount to ensure everyone understands the priorities and deadlines.
In situations with unavoidable conflicts, I prioritize based on risk assessment and regulatory requirements. For example, a delay in software validation might pose a higher risk than a minor cosmetic change to the device housing. Prioritization requires proactive communication with stakeholders to manage expectations and, when necessary, adjust timelines based on shared understanding.
Q 24. Explain your experience with different manufacturing processes used in the medical device industry.
My experience encompasses a range of manufacturing processes commonly used in the medical device industry, including injection molding, machining, casting, and additive manufacturing (3D printing).
- Injection molding is extensively used for high-volume production of plastic components, offering cost-effectiveness and precision. I’ve worked on projects using this method to manufacture housings and disposable parts for various devices.
- Machining, particularly CNC machining, is essential for creating complex metal components with high accuracy. My experience includes overseeing the production of precision surgical instruments using this technique.
- Casting, such as investment casting, provides a versatile way to create intricate metal parts. I’ve worked with this method to fabricate components requiring specific surface finishes and internal geometries.
- Additive manufacturing, or 3D printing, is particularly valuable for prototyping and producing small batches of customized parts. I’ve used this technology for rapid prototyping of new designs and creating customized jigs and fixtures.
My understanding extends beyond the manufacturing processes themselves to encompass material selection, quality control procedures, and regulatory compliance within each process. I understand the importance of selecting biocompatible materials and ensuring sterilization processes are rigorously followed to maintain safety and efficacy.
Q 25. How do you stay up-to-date with the latest technologies and regulations in the biomedical device field?
Staying current in the dynamic biomedical device field requires a multi-faceted approach. I actively participate in industry conferences and webinars, such as those hosted by AdvaMed and the FDA, to learn about emerging technologies and regulatory changes. I subscribe to leading industry publications like Medical Device & Diagnostic Industry (MD&DI) and regularly read peer-reviewed scientific journals.
Furthermore, I maintain a professional network through participation in industry associations and online forums. Engaging with colleagues and experts allows me to share knowledge, learn about new developments, and gain insights into different perspectives. I also utilize online resources such as the FDA website and various regulatory databases to stay abreast of evolving guidelines and regulations. Finally, continuous professional development, including participation in relevant workshops and training programs, is crucial to maintaining my expertise.
Q 26. Describe your experience with different sales and marketing channels for medical devices.
My experience with sales and marketing channels for medical devices spans various approaches, reflecting the diverse needs of different products and target audiences.
- Direct Sales Force: I’ve worked with teams that directly engage with healthcare providers, hospitals, and clinics, building strong relationships and providing technical expertise. This approach is particularly effective for complex devices requiring detailed demonstrations and technical support.
- Distribution Networks: I understand the importance of leveraging established distribution networks to reach a wider customer base, especially for high-volume products. This involves collaborating with distributors to ensure effective market penetration and customer service.
- Digital Marketing: I recognize the significant role of digital marketing in today’s landscape. This includes targeted online advertising, search engine optimization (SEO), and the utilization of social media platforms to reach key decision-makers and raise brand awareness.
- Trade Shows and Conferences: Participation in industry events is crucial for showcasing new products, networking with potential customers and partners, and staying informed about market trends.
Selecting the right mix of sales and marketing channels depends on various factors, including the product’s characteristics, target market, budget constraints, and competitive landscape. A tailored strategy is crucial for success.
Q 27. How do you ensure data integrity and traceability throughout the medical device lifecycle?
Data integrity and traceability are paramount throughout the medical device lifecycle, from design and development to manufacturing, distribution, and post-market surveillance. Ensuring these aspects requires a comprehensive quality management system (QMS) compliant with regulations like ISO 13485 and 21 CFR Part 820.
We use a combination of strategies:
- Unique Device Identification (UDI): Implementing UDI systems ensures traceability of devices throughout their lifecycle, enabling efficient recall management and post-market surveillance.
- Electronic Data Capture (EDC): Utilizing EDC systems for all stages of development and manufacturing ensures data integrity and minimizes errors through automated data collection and validation.
- Version Control: Employing version control systems for software and design documents preserves a complete audit trail, enabling traceability of changes and ensuring that the final product adheres to approved specifications.
- Validation and Verification: Rigorous validation and verification protocols are crucial to ensuring the software and hardware function as designed and meet the required performance criteria.
- Auditable Paper Trails: Maintaining meticulous records, including test results, manufacturing logs, and quality control reports, provides a comprehensive audit trail and ensures regulatory compliance.
Regular internal audits and external inspections help identify gaps and ensure compliance with regulations and industry best practices. Proactive measures are essential to build a robust system that guarantees data integrity and traceability.
Q 28. What are your salary expectations for this position?
My salary expectations for this position are commensurate with my experience and skills, as well as the responsibilities and compensation range typical for this role within the industry and geographic location. I’m confident that my contributions will significantly benefit your company and am open to a discussion about the specific compensation package.
Key Topics to Learn for Biomedical Device Innovation and Commercialization Interview
- Regulatory Landscape: Understand FDA regulations (510k, PMA), ISO standards, and the complexities of navigating the approval process for medical devices. Consider the ethical implications of device development and commercialization.
- Market Analysis & Competitive Landscape: Analyze market needs, identify unmet clinical needs, and understand the competitive dynamics within the biomedical device industry. Practice conducting thorough market research and developing compelling value propositions.
- Intellectual Property (IP) Strategy: Learn about patent protection, trade secrets, and licensing agreements. Understand how to protect your innovations and navigate IP challenges in collaborations.
- Design Control & Development Process: Familiarize yourself with the design control process, risk management (FMEA), and verification and validation techniques used in biomedical device development. Be prepared to discuss your experience with design iterations and improvements based on testing results.
- Manufacturing & Supply Chain: Understand the challenges and considerations involved in manufacturing medical devices, including quality control, sterilization, and supply chain management. Discuss your knowledge of different manufacturing processes and materials.
- Commercialization Strategies: Learn about different go-to-market strategies, including direct sales, distribution partnerships, and marketing to healthcare providers and patients. Practice articulating the unique selling points of a device and its potential market impact.
- Financial Modeling & Business Planning: Understand how to build financial models for new medical devices, including forecasting revenues, costs, and profitability. Be able to discuss business planning, investment strategies, and return on investment.
- Teamwork and Collaboration: Biomedical device innovation often involves multidisciplinary teams. Prepare to discuss your experience working collaboratively with engineers, clinicians, regulatory affairs specialists, and business professionals.
Next Steps
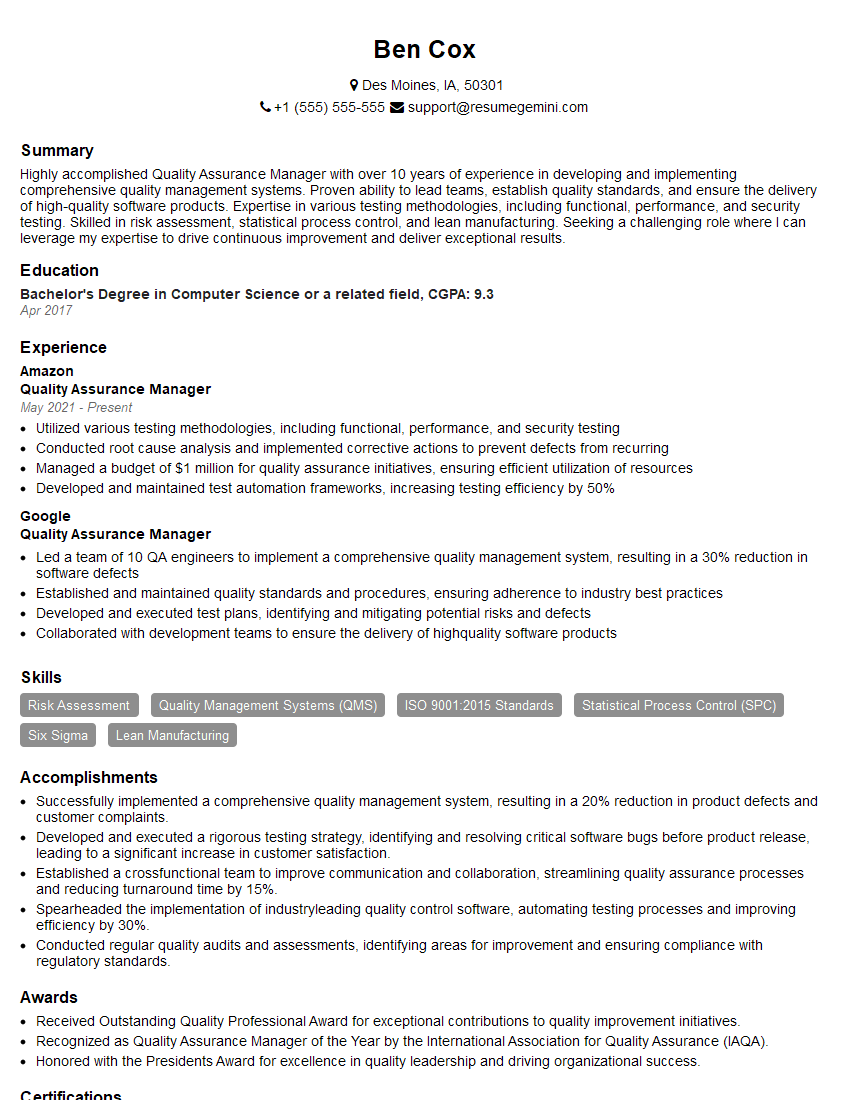
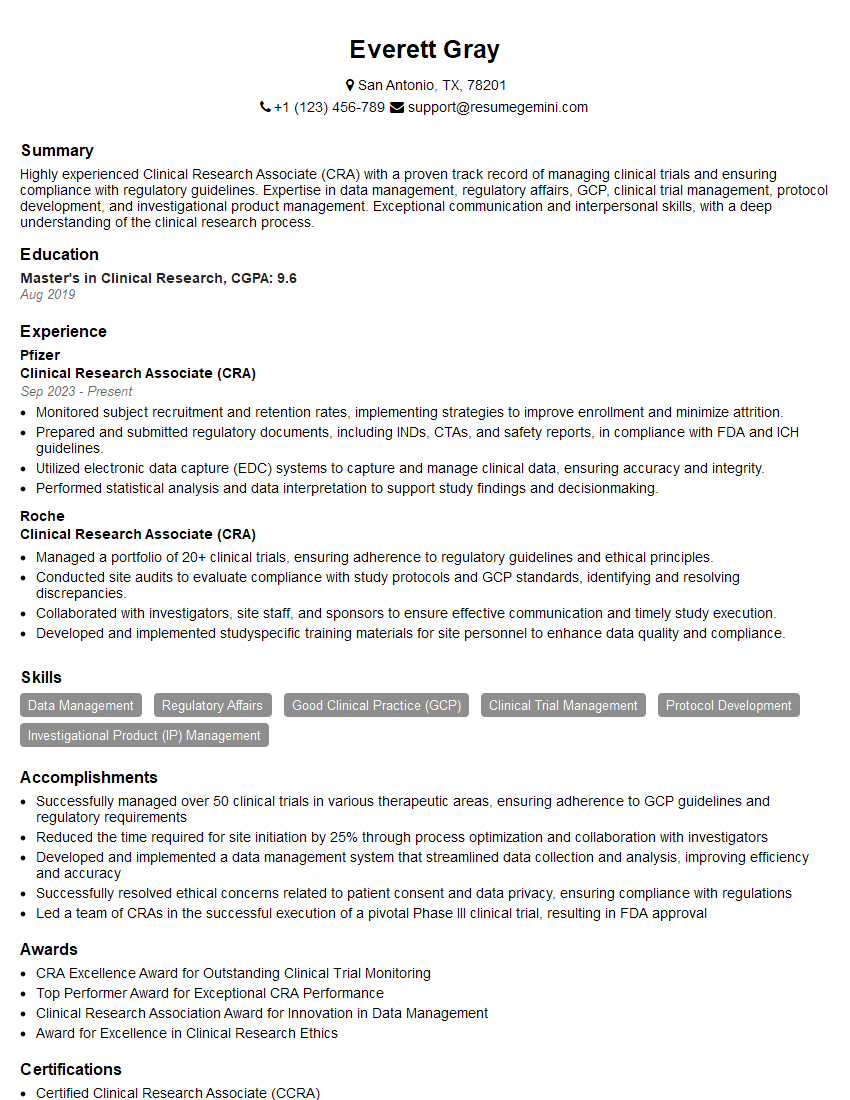
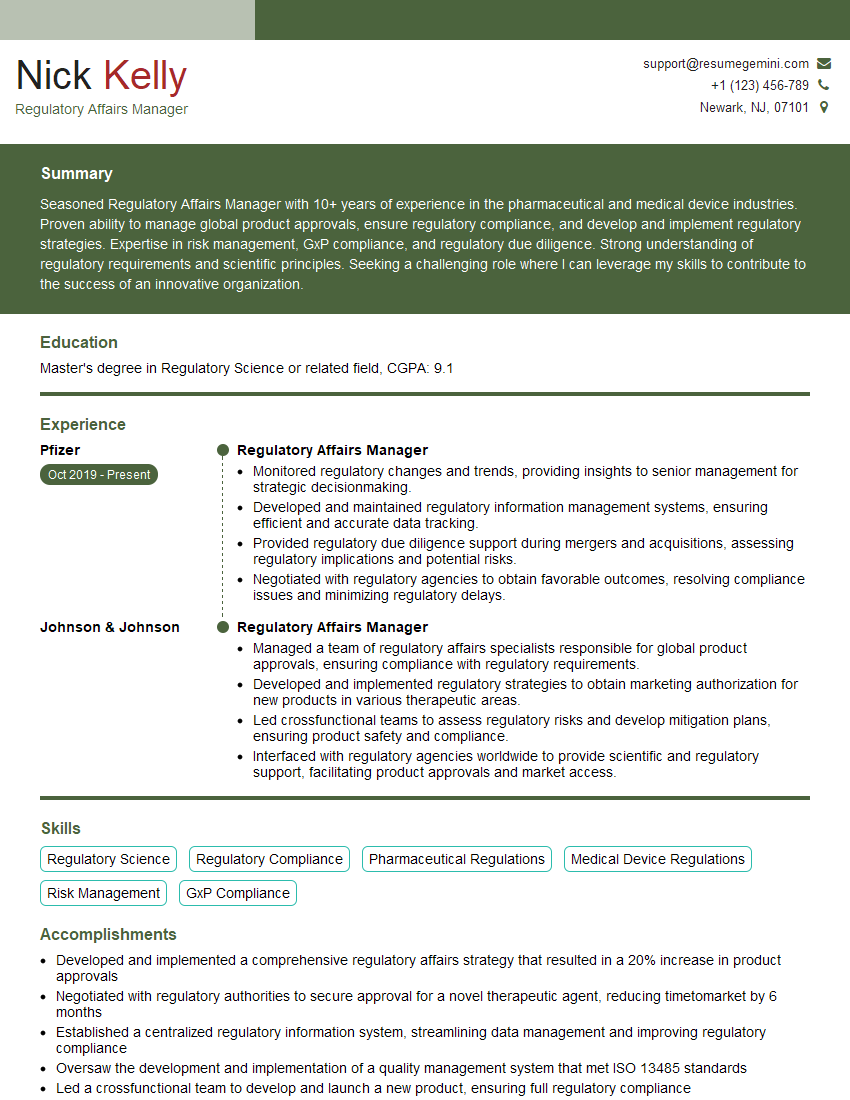
Mastering Biomedical Device Innovation and Commercialization is crucial for a successful and rewarding career in this dynamic field. It allows you to contribute meaningfully to improving healthcare and significantly impacts your earning potential and career progression opportunities. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource for building professional, impactful resumes. They provide examples of resumes specifically tailored to Biomedical Device Innovation and Commercialization, helping you present your qualifications in the best possible light. Take advantage of these resources to stand out from the competition and secure your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good