The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Familiarity with medical imaging techniques (e.g., MRI, CT scans) interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Familiarity with medical imaging techniques (e.g., MRI, CT scans) Interview
Q 1. Explain the principles behind Magnetic Resonance Imaging (MRI).
Magnetic Resonance Imaging (MRI) leverages the principles of nuclear magnetic resonance to create detailed anatomical images. It works by placing the patient in a powerful magnetic field. The magnetic field aligns the protons (hydrogen nuclei) within the body’s water molecules. Then, radiofrequency pulses are emitted, temporarily disrupting this alignment. As the protons realign, they release energy which is detected by the MRI machine. The strength and timing of this signal vary depending on the tissue type, creating a contrast that allows different structures to be visualized.
Think of it like this: imagine tiny magnets (protons) all pointing in the same direction. The radio waves are like a gust of wind that knocks them over. As they settle back down, they emit a signal that’s unique to their surroundings (tissue type). The MRI machine listens to this signal to build the image.
Q 2. Describe the differences between T1-weighted and T2-weighted MRI images.
T1-weighted and T2-weighted images represent different aspects of tissue relaxation times after the radiofrequency pulse. T1 weighting shows how quickly protons return to their original alignment (longitudinal relaxation). Fat appears bright, and water appears dark. T2 weighting shows how quickly protons lose coherence in their alignment (transverse relaxation). Water appears bright, and fat appears dark. This difference is crucial in differentiating various pathologies. For example, T1-weighted images are excellent for visualizing anatomy, while T2-weighted images are more sensitive to edema (swelling) and inflammation.
Imagine two buckets of water. In a T1 sequence, the bucket that empties quickly (fat) appears brighter than the one that takes longer (water). In a T2 sequence, the opposite occurs.
Q 3. What are the contraindications for MRI scans?
Several contraindications exist for MRI scans. The most significant is the presence of ferromagnetic materials within the body. This includes certain types of aneurysm clips, pacemakers, and some types of metallic implants. The strong magnetic field can cause these objects to move, potentially causing injury or malfunction. Claustrophobia is another major concern, as patients are enclosed within the MRI machine. Patients with certain kidney conditions may also need precautions due to the use of contrast agents (gadolinium).
Always conduct a thorough screening interview with the patient before scheduling an MRI to identify any potential contraindications.
Q 4. Explain the principles behind Computed Tomography (CT) scanning.
Computed Tomography (CT) scanning uses X-rays to create cross-sectional images of the body. A rotating X-ray tube emits a thin beam of X-rays that passes through the patient. Detectors on the opposite side measure the amount of X-rays that pass through. Denser tissues (like bone) attenuate (absorb) more X-rays, appearing brighter on the image, while less dense tissues (like air) appear darker. A computer then processes this data to reconstruct a series of cross-sectional images.
Think of it like shining a flashlight through an object. The thicker parts block more light, creating shadows that represent denser material.
Q 5. What is the role of contrast agents in CT scans?
Contrast agents in CT scans are iodine-based substances that enhance the visibility of certain structures. They are injected intravenously and increase the attenuation of X-rays in blood vessels and other tissues, allowing for better visualization of subtle abnormalities. This is particularly useful in evaluating blood vessels, tumors, and inflammatory processes. For example, in a CT scan of the abdomen, contrast helps to clearly delineate blood vessels within the liver or identify the presence of a tumor.
The contrast essentially makes the area of interest ‘light up’ on the image, enhancing its visibility.
Q 6. Describe the differences between helical and multislice CT.
Helical (spiral) CT is a significant advancement over traditional CT, where the X-ray tube rotates continuously while the table moves through the scanner. This allows for faster scan times and better image quality, particularly for dynamic processes like blood flow. Multislice CT further enhances this by incorporating multiple detectors, allowing even faster scan times and thinner slice thicknesses. The improved resolution and faster acquisition reduce motion artifacts and provide a greater level of detail.
Imagine taking a movie instead of still photos. Helical CT is like taking a continuous film, while multislice CT takes a higher resolution, faster movie.
Q 7. What are the radiation risks associated with CT scans?
The primary risk associated with CT scans is radiation exposure. CT scans deliver a significantly higher dose of radiation compared to X-rays. This radiation exposure increases the risk of developing cancer in the long term. The exact risk depends on several factors, including the number of scans, the specific scan protocol, and the patient’s age. The benefits of the scan must always be carefully weighed against these risks. For pediatric patients or those requiring multiple scans, minimizing radiation dose is especially critical.
While the benefit often outweighs the risk, it’s crucial to always employ the ALARA (As Low As Reasonably Achievable) principle, using the lowest radiation dose that provides adequate diagnostic information.
Q 8. Explain the ALARA principle in medical imaging.
The ALARA principle, which stands for ‘As Low As Reasonably Achievable,’ is a fundamental guideline in medical imaging. It emphasizes minimizing radiation exposure to patients and personnel while still obtaining diagnostically useful images. This isn’t about eliminating radiation entirely – that would render the technology useless – but about optimizing the balance between image quality and radiation dose. We achieve this through various methods, including selecting the lowest possible radiation settings that still provide adequate image quality, optimizing scan parameters, using appropriate shielding, and employing techniques like iterative reconstruction in CT to reduce noise while lowering dose.
For example, if a chest X-ray is required, we wouldn’t use a CT scan, which involves significantly higher radiation. Within CT itself, we’d adjust parameters like tube current and kVp to obtain a sufficient signal while keeping the dose as low as possible. ALARA is not just a technical consideration; it’s deeply rooted in ethical responsibility to protect patients from unnecessary radiation exposure.
Q 9. Describe the process of image acquisition in MRI.
MRI image acquisition is a complex process relying on the interaction between strong magnetic fields, radio waves, and the hydrogen atoms within the body. It begins with the patient being placed inside a powerful magnet. The magnetic field aligns the hydrogen protons. Next, radiofrequency (RF) pulses are emitted, temporarily knocking the protons out of alignment. As the protons realign, they emit signals that are detected by the MRI machine’s coils. These signals are incredibly weak and require sophisticated signal processing. The strength and timing of these signals vary depending on the tissue type and its environment, producing the contrast we see in the final image. Different pulse sequences (e.g., T1-weighted, T2-weighted, FLAIR) are used to highlight different tissue properties.
Think of it like striking a tuning fork: different materials resonate at different frequencies. The MRI machine ‘listens’ to these resonances to create a map of the body’s composition. The process is then repeated many times from different angles to construct a 3D image. This is why MRI scans can take a considerable amount of time.
Q 10. Describe the process of image reconstruction in CT.
CT image reconstruction involves transforming the raw data acquired by the CT scanner into a diagnostically useful image. The scanner rotates around the patient, taking multiple X-ray projections from various angles. Each projection represents the attenuation of X-rays as they pass through the body. These projections are mathematically processed using sophisticated algorithms, often involving Filtered Back Projection (FBP) or iterative reconstruction techniques. The algorithms work backwards from the projections to estimate the attenuation coefficient of each voxel (a 3D pixel) within the patient’s body.
Imagine shining a flashlight through an object from multiple angles. You’d get different shadow patterns. The reconstruction algorithm uses those patterns to build a 3D representation of the object. Iterative reconstruction methods refine this process to improve image quality and reduce noise, leading to lower radiation doses. The final output is a series of cross-sectional images that can be viewed and manipulated in different ways to evaluate the anatomy and pathology.
Q 11. How do you ensure patient safety during MRI and CT procedures?
Ensuring patient safety during MRI and CT procedures involves a multi-faceted approach. For MRI, screening for contraindications is crucial. Patients with certain metallic implants (e.g., some pacemakers, aneurysm clips) or claustrophobia may not be suitable candidates. Careful monitoring during the scan is essential. For CT, the primary concern is radiation safety. We adhere strictly to ALARA principles, optimizing scan parameters, using appropriate shielding when possible, and ensuring proper patient positioning. Both modalities require clear communication with the patient, explaining the procedure and addressing any concerns.
In practice, this means detailed questionnaires, verifying patient information against screening criteria, and having emergency procedures in place. For MRI, regular checks are needed to ensure that the patient isn’t experiencing any adverse effects. In CT, we always consider whether the clinical need justifies the radiation dose, exploring alternative imaging modalities if appropriate. Continuous professional development and adherence to safety protocols are key.
Q 12. What are the artifacts commonly encountered in MRI and CT images?
Artifacts are image distortions that detract from the accuracy and diagnostic value of MRI and CT scans. In MRI, common artifacts include motion artifacts (blurring due to patient movement), susceptibility artifacts (caused by variations in magnetic susceptibility of different tissues near metallic objects), chemical shift artifacts (caused by differences in the resonance frequencies of fat and water), and truncation artifacts (incomplete data acquisition). In CT, common artifacts include beam hardening (differential attenuation of X-rays by different materials), ring artifacts (caused by detector malfunction), and motion artifacts.
Imagine taking a photo of a moving object – it’ll be blurry. That’s motion artifact. In CT, metallic objects can cause streaks. Recognizing these artifacts is crucial because they can mimic pathology, leading to misdiagnosis. Understanding the origin of artifacts helps radiologists interpret images more accurately. We use various techniques to minimize artifacts, including patient positioning, scan parameters optimization, and using specialized sequences.
Q 13. How do you identify and troubleshoot common equipment malfunctions?
Troubleshooting equipment malfunctions requires systematic problem-solving. It begins with identifying the specific problem – is it an image quality issue, a system error, or a safety concern? A checklist approach is helpful. We would first check for obvious issues: are there any error messages displayed? Are the machine’s vital signs (temperature, pressure, etc.) within normal range? Then, we move to more detailed checks, which may involve reviewing the logs for potential errors, verifying signal strength, testing the coils and detectors, and checking the calibration settings.
For instance, if images appear excessively noisy, we might check the coil performance, the RF settings, or the reconstruction parameters. If the system is not powering on, we’d check the power supply, fuses, and any other relevant components. If there’s a safety issue, we’d prioritize immediate shutdown and call for engineering support. Regular preventative maintenance is key in minimizing equipment malfunctions and ensuring optimal performance.
Q 14. Explain the difference between axial, coronal, and sagittal imaging planes.
Axial, coronal, and sagittal planes represent different ways of slicing a three-dimensional object like the human body for imaging. Think of it like cutting a loaf of bread:
- Axial (Transverse): This is a horizontal slice, like cutting the loaf of bread horizontally. It shows a cross-section of the body, dividing it into superior (upper) and inferior (lower) portions.
- Coronal: This is a vertical slice that divides the body into anterior (front) and posterior (back) portions. Imagine slicing the bread vertically from front to back.
- Sagittal: This is also a vertical slice, but it divides the body into left and right portions. It’s like slicing the bread vertically from side to side. A midsagittal plane passes directly through the midline of the body.
These different planes provide complementary views of the anatomy, allowing for a comprehensive assessment of structures and pathologies. Radiologists often utilize images from all three planes to obtain a complete understanding of a patient’s condition.
Q 15. How would you explain a complex medical image to a patient?
Explaining a complex medical image to a patient requires empathy and clear communication. I start by acknowledging that medical images can be intimidating. I then explain the type of image (e.g., MRI of the brain, CT scan of the abdomen) and what it shows in simple terms, avoiding jargon. I use analogies to help them understand. For example, if showing a brain MRI, I might say, “Think of this as a detailed map of your brain. The different colors and shades represent different tissues. This bright area here is the part of your brain responsible for…” I’ll point out relevant features, such as tumors or areas of inflammation, but I always explain their significance in a way that’s easy to grasp. Visual aids, like diagrams or simplified versions of the images, can significantly improve understanding. Finally, I encourage the patient to ask questions and ensure they leave feeling informed and comfortable.
For instance, if a patient has a CT scan showing a lung nodule, instead of saying ‘there is a 1cm nodule in the right upper lobe’, I’d explain it as, ‘The scan shows a small spot on your lung, like a tiny pebble. We need to do further tests to see if it’s anything to worry about.’
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with PACS (Picture Archiving and Communication Systems)?
I have extensive experience with PACS, using it daily for image viewing, storage, retrieval, and distribution. My expertise includes proficiency in accessing and interpreting images from different modalities (MRI, CT, X-ray, Ultrasound), using various PACS workstations and integrating with other hospital systems like EMRs (Electronic Medical Records). I am familiar with DICOM (Digital Imaging and Communications in Medicine) standards and understand their importance in ensuring image interoperability and quality control. I’ve also participated in PACS system upgrades and troubleshooting, resolving issues relating to image display, storage limitations, and connectivity problems. This experience includes managing user accounts, archiving studies, and ensuring compliance with HIPAA regulations regarding patient data privacy and security.
Q 17. Describe your proficiency with various medical imaging software.
My proficiency extends to several medical imaging software packages. I am highly skilled in using advanced image processing software such as Osirix, Horos, and 3D Slicer. These tools allow for detailed image manipulation, including MPR (Multiplanar Reconstruction), volume rendering, and 3D modeling, which significantly improves diagnostic accuracy. I’m also proficient in vendor-specific software associated with different imaging modalities, such as those provided by Siemens, GE, and Philips. My experience includes using these software packages for both routine image interpretation and advanced analysis techniques such as quantitative image analysis. For instance, I’ve used Horos to perform 3D reconstructions of CT scans to better visualize complex anatomical structures, and Osirix for advanced measurements in MRI scans.
Q 18. How do you maintain quality control in medical imaging?
Maintaining quality control in medical imaging is paramount. It involves a multifaceted approach encompassing equipment calibration, image acquisition protocols, image processing techniques, and quality assurance testing. We regularly perform quality control tests on our imaging equipment, such as phantom imaging for CT and MRI, to ensure consistent performance. We adhere strictly to established protocols for image acquisition, including proper patient positioning and scan parameters. Image processing involves careful review for artifacts and ensuring appropriate windowing and leveling. Our department participates in regular quality assurance programs, using standardized tools and techniques to monitor the quality of our work and identify any trends or issues that need to be addressed. This includes regular internal audits and external quality assurance inspections.
For instance, we use quality assurance phantoms with known characteristics to verify the accuracy and precision of our MRI and CT scanners. If the results deviate from the expected values, we investigate the causes and take corrective action.
Q 19. What is your experience with radiation safety protocols?
Radiation safety is a critical aspect of my work, and I’m thoroughly trained in ALARA principles (As Low As Reasonably Achievable). This involves optimizing scan parameters to minimize radiation dose while maintaining diagnostic image quality. I’m proficient in using radiation dosimetry equipment and interpreting the results. My understanding extends to regulatory compliance regarding radiation safety, such as adhering to guidelines set by regulatory bodies. I always ensure proper shielding for patients and staff during procedures. I routinely check equipment for safety compliance and participate in ongoing safety training to stay updated on best practices and emerging technologies. Furthermore, I’m knowledgeable about the safe handling and disposal of radioactive materials. Before each scan, I inform the patient about the risks and benefits of the procedure and ensure they understand the radiation dose involved, emphasizing the importance of ALARA.
Q 20. Describe a time you had to troubleshoot a technical issue during a scan.
During a busy afternoon, we encountered a problem with a CT scanner—an error message indicating a communication issue with the image reconstruction software. The patient was already positioned and ready for the scan. Initially, I tried restarting the system, a common troubleshooting step. When that failed, I checked the network connection, verifying cables and ensuring the server was operational. The problem persisted. I then consulted the system’s troubleshooting manual, systematically working through the suggested steps. It turned out a critical software update was needed. After contacting IT and coordinating with them to complete the update quickly and safely, the issue was resolved. The scan was successfully completed with minimal delay, minimizing patient discomfort and disruption to the department’s workflow. This situation highlighted the importance of methodical troubleshooting, teamwork, and having access to up-to-date documentation.
Q 21. How do you handle stressful situations in a fast-paced environment?
The medical imaging environment is often fast-paced and demanding. I handle stressful situations by prioritizing tasks, focusing on the immediate needs of the patients, and calmly assessing the situation. Effective communication with my team is vital; collaboration helps us manage workload efficiently and support each other under pressure. Prioritization ensures that urgent cases are addressed promptly while maintaining a consistent level of care for all patients. I also employ stress-reduction techniques outside of work, such as exercise and mindfulness, to maintain my overall well-being and resilience. Maintaining a calm demeanor helps to de-escalate tense situations and allows me to focus on finding solutions effectively, reducing errors and ensuring patient safety.
Q 22. What are the ethical considerations in medical imaging?
Ethical considerations in medical imaging are paramount, encompassing patient privacy, informed consent, radiation safety, and resource allocation. Patient privacy involves protecting sensitive medical information, adhering to HIPAA regulations (in the US) or equivalent legislation elsewhere. Informed consent requires patients to understand the procedure, its benefits, risks, and alternatives before undergoing imaging. Radiation safety necessitates minimizing radiation exposure to patients and staff by optimizing scan parameters and utilizing appropriate shielding. Finally, responsible resource allocation involves ensuring efficient use of expensive imaging equipment and personnel to maximize healthcare access.
For example, a patient’s MRI scan results should only be accessed by authorized personnel, and any dissemination of these results needs explicit consent. Similarly, when performing CT scans, utilizing the lowest effective radiation dose while achieving diagnostic quality is crucial. The ethical implications extend to ensuring equitable access to advanced imaging technologies, preventing disparities based on socioeconomic status or geographical location.
Q 23. What is your understanding of image interpretation?
Image interpretation is the process of analyzing medical images (like X-rays, CT scans, or MRIs) to identify anatomical structures and detect abnormalities. It’s a multi-step process involving careful observation, pattern recognition, and integration of clinical information. This involves comparing the image findings with the patient’s clinical history, symptoms, and other diagnostic tests to reach a conclusive diagnosis or suggest further investigations.
For instance, identifying a fracture on an X-ray requires recognizing the disrupted bone continuity, analyzing the fracture type and location, and considering the patient’s mechanism of injury. Similarly, interpreting a brain MRI involves identifying anatomical structures, looking for changes in signal intensity that could indicate lesions, edema or hemorrhage and correlating those findings with the patient’s neurological symptoms.
Effective image interpretation requires a strong understanding of anatomy, physiology, pathology, and the technical aspects of the imaging modality used. It’s a skill honed through extensive experience and continuous learning.
Q 24. What is your experience with different types of image post-processing techniques?
My experience with image post-processing techniques is extensive, covering a range of modalities. I’m proficient in techniques like image enhancement (e.g., adjusting brightness, contrast, and sharpness), which improve visualization of subtle details. I regularly use image reconstruction algorithms, particularly in CT and MRI, to optimize image quality and reduce noise. I’m also adept at utilizing 3D rendering techniques to create detailed anatomical models, crucial for surgical planning and complex case analysis.
Furthermore, I have experience with advanced post-processing techniques like maximum intensity projection (MIP) and minimum intensity projection (MinIP) for visualizing vascular structures, and volume rendering for creating 3D representations. I am familiar with software such as Osirix, 3D Slicer, and commercially available PACS systems. A specific example involves using MIP on a CT angiogram to clearly visualize the extent of a blood clot in a patient’s pulmonary artery, aiding in timely diagnosis and treatment.
Q 25. Describe your experience with different types of imaging modalities (e.g., fluoroscopy, ultrasound).
My experience encompasses various imaging modalities. I’ve worked extensively with MRI, CT, and X-ray, developing expertise in their respective applications and limitations. For example, MRI excels in visualizing soft tissues, making it ideal for neurological and musculoskeletal imaging. CT, with its speed and excellent bone detail, is frequently used in trauma and oncology. X-ray provides quick, readily available imaging, essential for initial assessment of fractures or pneumonias.
Beyond these, I possess experience with fluoroscopy, a real-time imaging technique often used during interventional procedures such as angioplasty or stent placement. This allows for immediate feedback during the procedure. I also have experience with ultrasound, a non-ionizing technique used in various applications, including obstetrics, cardiology, and abdominal imaging. The ability to differentiate between various modalities and selecting the appropriate exam based on clinical question is a key aspect of my expertise.
Q 26. How do you stay current with advancements in medical imaging technology?
Staying current in the rapidly evolving field of medical imaging requires a multi-pronged approach. I actively participate in continuing medical education (CME) courses and conferences, focusing on new techniques and technologies. I regularly read peer-reviewed journals and stay informed about the latest research findings published in prominent medical imaging publications.
I also engage with professional organizations like the American College of Radiology (ACR) or similar societies, leveraging their resources, webinars, and online communities. Online learning platforms offer further opportunities to enhance my knowledge in specific areas. Furthermore, actively collaborating with colleagues and experts in the field through case discussions and knowledge sharing remains a vital part of my professional development. This continuous learning ensures that my skills and knowledge remain up-to-date and relevant.
Q 27. What are your salary expectations?
My salary expectations are commensurate with my experience, skills, and the responsibilities of this position. I am open to discussing a competitive salary range based on the specifics of the role and compensation package offered.
Q 28. Why are you interested in this position?
I’m highly interested in this position because it aligns perfectly with my career goals and passion for medical imaging. The opportunity to contribute to a team dedicated to providing high-quality patient care using cutting-edge technology is very appealing. I am particularly drawn to [mention specific aspects of the role or organization that excite you – e.g., the research opportunities, the use of specific technology, the organization’s reputation]. I am confident that my skills and experience will allow me to make a significant contribution to your team and I am eager to learn and grow within this challenging yet fulfilling environment.
Key Topics to Learn for Familiarity with Medical Imaging Techniques (e.g., MRI, CT scans) Interview
- Basic Principles of MRI: Understand the fundamental physics behind MRI, including magnetic fields, radio waves, and nuclear magnetic resonance. Explore different MRI pulse sequences and their applications.
- CT Scan Fundamentals: Grasp the principles of X-ray computed tomography, including data acquisition, image reconstruction, and the differences between helical and multislice CT.
- Image Interpretation Basics: Learn to identify common anatomical structures on both MRI and CT scans. Practice recognizing normal vs. abnormal findings and understanding the implications of different image characteristics (e.g., density, signal intensity).
- Contrast Agents: Understand the role and mechanism of action of contrast agents used in MRI and CT scans. Be prepared to discuss potential side effects and contraindications.
- Clinical Applications: Discuss the practical applications of MRI and CT scans in various medical specialties (e.g., neurology, oncology, cardiology). Be ready to provide examples of how these imaging modalities are used to diagnose and manage specific conditions.
- Radiation Safety: Familiarize yourself with the principles of radiation safety related to CT scans, including ALARA principles and patient protection measures.
- Image Artifacts: Understand the causes and appearance of common artifacts in MRI and CT scans, and how these can affect image interpretation.
- Comparison of MRI and CT: Be able to compare and contrast the strengths and limitations of MRI and CT in different clinical scenarios.
- Emerging Technologies: Stay updated on the latest advancements in medical imaging techniques, such as perfusion imaging, diffusion tensor imaging, and advanced CT reconstruction techniques.
Next Steps
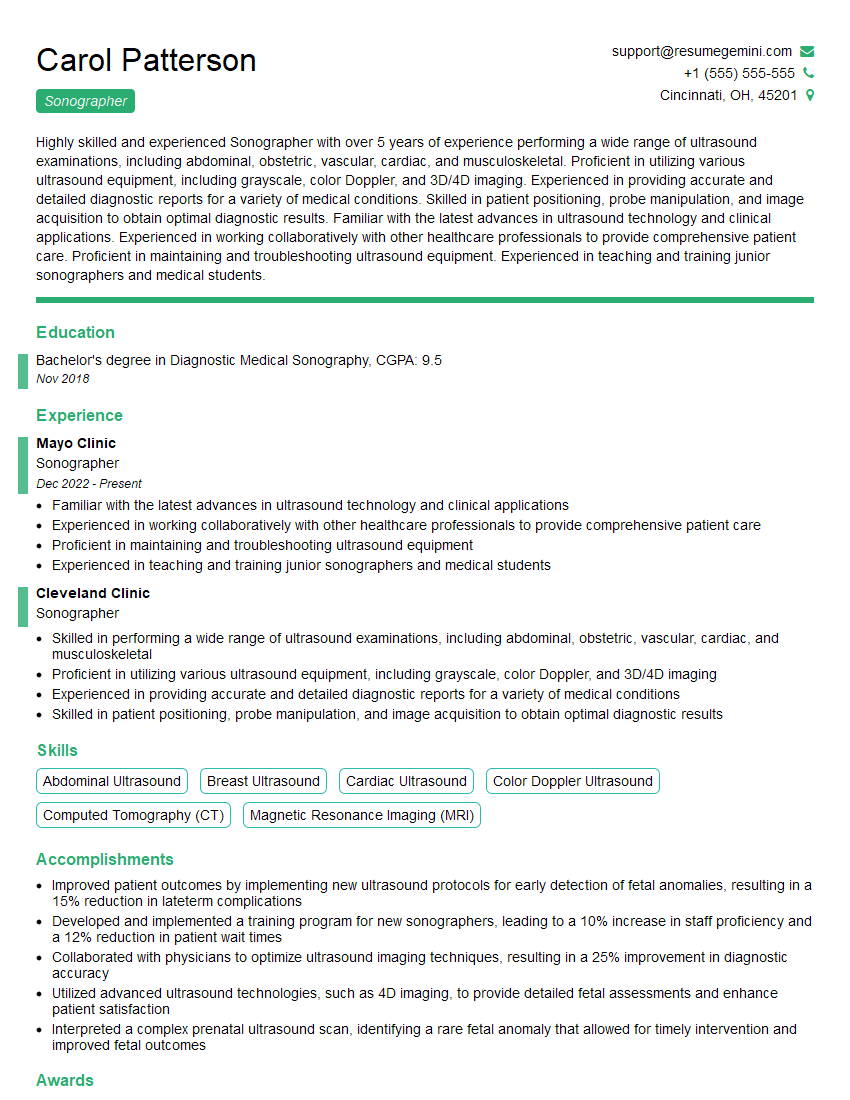
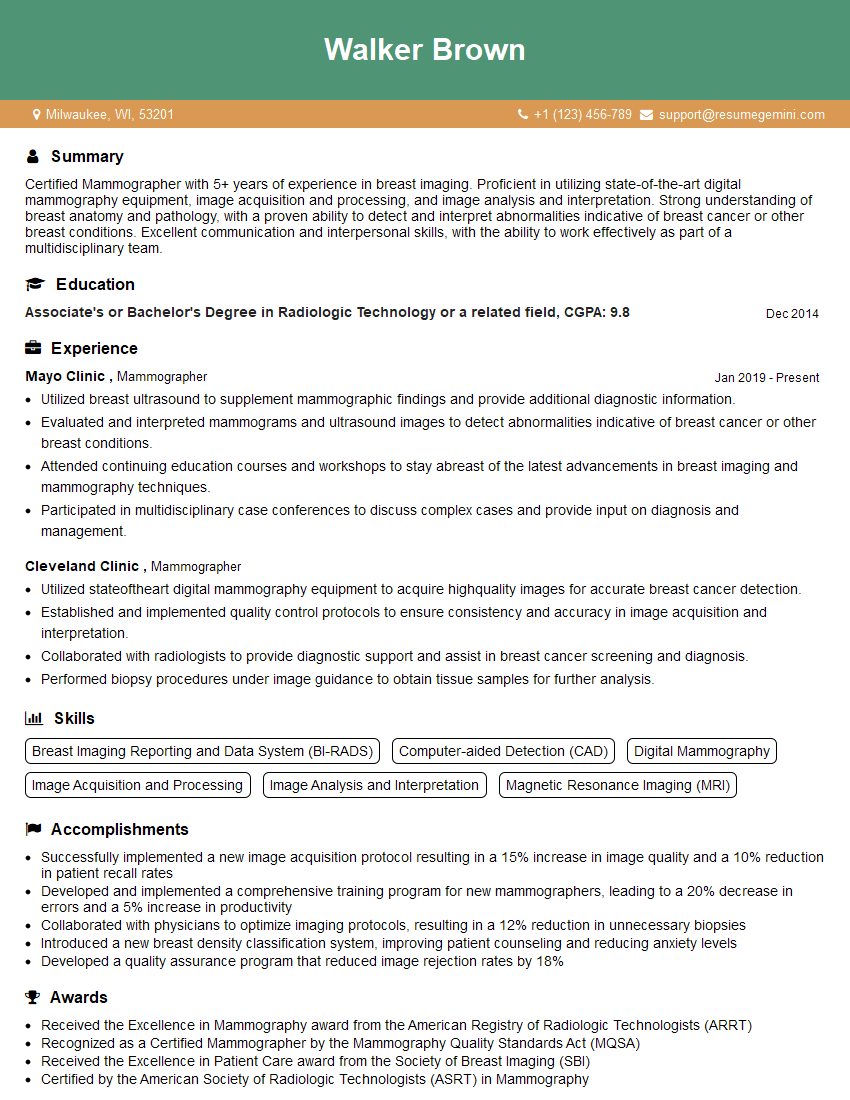
Mastering medical imaging techniques is crucial for career advancement in many healthcare fields. A strong understanding of MRI and CT scans demonstrates technical expertise and problem-solving abilities highly valued by employers. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to showcase expertise in medical imaging techniques like MRI and CT scans, giving you a head start in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good