Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Knowledge of Pharmaceutical Industry Standards interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Knowledge of Pharmaceutical Industry Standards Interview
Q 1. Explain the significance of Good Manufacturing Practices (GMP) in the pharmaceutical industry.
Good Manufacturing Practices (GMP) are a set of guidelines that ensure the consistent production of high-quality pharmaceutical products. Think of it as a recipe for making medicine that’s meticulously followed to guarantee safety and efficacy. These regulations cover every aspect of drug manufacturing, from the sourcing of raw materials to the final packaging and distribution. Compliance with GMP is not just a suggestion; it’s a legal requirement in most countries and is crucial for protecting public health.
- Raw Material Control: GMP ensures that all raw materials used meet strict quality standards. This includes proper identification, testing, and storage.
- Manufacturing Process: The manufacturing process itself must be validated and controlled to ensure consistency and prevent contamination. This includes environmental controls, equipment calibration, and meticulous documentation.
- Quality Control: Rigorous testing is performed at various stages of production to verify the quality of the finished product. This involves both in-process and final product testing.
- Personnel Training: GMP emphasizes the importance of well-trained personnel who understand the procedures and are capable of following them accurately.
- Record Keeping: Meticulous record-keeping is essential for traceability and accountability. Any deviations from established procedures must be thoroughly documented and investigated.
Failure to comply with GMP can result in serious consequences, including product recalls, regulatory sanctions, and damage to a company’s reputation. For example, a pharmaceutical company that doesn’t properly validate its manufacturing process might produce batches of medication with inconsistent potency, leading to ineffective treatment or even harm to patients.
Q 2. Describe your experience with FDA regulations, specifically 21 CFR Part 11.
21 CFR Part 11, a section of the FDA’s Code of Federal Regulations, sets forth rules and regulations for electronic records and electronic signatures in the pharmaceutical industry. In essence, it ensures the integrity and authenticity of electronic data. My experience with 21 CFR Part 11 includes implementing and maintaining systems that comply with these regulations. This involved everything from software validation and audit trails to user access control and data backup procedures.
For instance, I was involved in the validation of a new laboratory information management system (LIMS) to ensure it met the requirements of 21 CFR Part 11. This included a comprehensive review of the system’s functionalities, development of validation protocols, and execution of testing to verify compliance with regulations. We had to ensure the system had robust audit trails, secure user access controls, and mechanisms for preventing unauthorized modification of data. A key aspect was establishing and implementing a system for electronic signatures that meet the regulatory requirements for authenticity and non-repudiation. Proper documentation and change control processes were crucial components to demonstrate compliance.
Q 3. What are the key differences between ICH guidelines and FDA guidelines?
ICH (International Council for Harmonisation) guidelines and FDA guidelines both aim to improve the quality and safety of pharmaceuticals, but they have key differences. ICH guidelines are internationally harmonized standards developed through a collaborative effort by regulatory authorities from different countries, including the FDA. They provide a common framework for regulatory requirements, aiming to reduce redundancy and streamline the drug development and approval process. The FDA, on the other hand, issues its own guidelines specific to the United States, which may incorporate or expand upon the ICH guidelines. Think of ICH as a broad agreement and FDA guidelines as the US-specific implementation of that agreement, sometimes with added nuances.
- Scope: ICH guidelines are international and broader in scope, applying to multiple regulatory jurisdictions. FDA guidelines are specific to the United States.
- Enforceability: FDA guidelines are legally binding in the United States, while ICH guidelines are not legally binding but provide a strong recommendation.
- Specificity: FDA guidelines often provide more detailed and specific requirements than ICH guidelines.
For example, while both might address Good Clinical Practice (GCP), the FDA might have more stringent requirements concerning documentation or data handling specific to US clinical trials.
Q 4. How do you ensure data integrity within a pharmaceutical quality system?
Data integrity is paramount in the pharmaceutical industry. It refers to the completeness, consistency, and accuracy of data throughout its lifecycle. Ensuring data integrity within a pharmaceutical quality system involves a multi-faceted approach. It’s like building a strong foundation for a building – you need every component to be perfectly aligned and secure to ensure stability.
- ALCOA+ Principles: Adherence to the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate + Complete, Enduring, Available) is fundamental. This ensures that all data is properly documented, traceable, and reliable.
- Validation of Systems: All computerized systems used for data generation, storage, and processing must be validated to ensure they function as intended and produce accurate and reliable results.
- Access Control: Restricting access to data based on roles and responsibilities minimizes the risk of unauthorized modification or deletion.
- Audit Trails: Implementing comprehensive audit trails tracks all changes to data, allowing for the identification and investigation of any discrepancies.
- Data Backup and Recovery: Regular backups and disaster recovery plans ensure data protection against loss or corruption.
- Training: Thorough training of personnel on data integrity principles and procedures is crucial.
For example, a system for recording manufacturing parameters must have appropriate audit trails showing who made changes, when they were made, and what those changes were. This ensures that any issues can be investigated and resolved.
Q 5. Explain the process of validating a new analytical method.
Method validation is a crucial process in analytical chemistry, proving that an analytical method is suitable for its intended purpose. It’s like testing a new recipe before serving it to guests – you need to ensure it consistently produces the desired result. A comprehensive validation typically involves several stages:
- Specificity: Demonstrating that the method measures only the analyte of interest and doesn’t interfere with other components in the sample.
- Linearity: Verifying that the response of the method is directly proportional to the concentration of the analyte over a specific range.
- Range: Determining the concentration range over which the method provides accurate and precise results.
- Accuracy: Assessing the closeness of the measured value to the true value.
- Precision: Evaluating the reproducibility of the method, measuring how close the results are to each other when repeated multiple times.
- Limit of Detection (LOD) and Limit of Quantification (LOQ): Determining the lowest concentration that can be reliably detected and quantified.
- Robustness: Evaluating the method’s resistance to small variations in experimental conditions.
Each of these parameters requires detailed documentation and statistical analysis. For example, to assess linearity, you might run a series of samples at different known concentrations and plot the results. The R-squared value obtained from the regression analysis should be close to 1 to demonstrate good linearity. A properly validated method assures confidence in the accuracy and reliability of analytical data used for quality control.
Q 6. Describe your experience with deviation investigations and CAPA (Corrective and Preventive Action).
Deviation investigations and Corrective and Preventive Actions (CAPA) are essential components of a robust quality system. Deviations are any unplanned events that occur during manufacturing or testing that deviate from established procedures. CAPA is the systematic process of investigating deviations, identifying root causes, implementing corrective actions to prevent recurrence, and preventing similar problems in the future.
My experience involves conducting thorough deviation investigations, documenting findings, and proposing and implementing CAPAs. This often includes interviewing personnel, reviewing production records, and analyzing data to determine the root cause of the deviation. For example, if a batch of tablets fails to meet weight specifications, a thorough investigation would be launched to identify if the issue stemmed from faulty equipment, incorrect weighing procedures, or raw material variation. This would then guide corrective actions like equipment calibration, employee retraining, or tighter raw material specifications. The CAPA process would ensure documentation of the root cause analysis, the corrective actions taken, and verification that the actions effectively prevented recurrence of the problem. This would be followed by preventative actions to eliminate the possibility of similar problems occurring in future batches.
Q 7. How do you handle out-of-specification (OOS) results in a pharmaceutical laboratory?
Out-of-specification (OOS) results are analytical test results that fall outside the pre-defined acceptance criteria. Handling OOS results requires a systematic and thorough investigation to determine the root cause and ensure the integrity of the product. It’s like finding a flaw in a perfectly crafted piece of art – you need to carefully examine every detail to understand what went wrong.
The process typically involves:
- Immediate Actions: Quarantine the affected batch. This prevents any further distribution of potentially sub-standard product.
- Investigation: A detailed investigation is conducted to determine the root cause of the OOS result. This might involve repeating the test, reviewing laboratory records, investigating potential equipment malfunctions, and reviewing raw materials.
- Root Cause Analysis: Techniques such as fishbone diagrams or 5 Whys can be used to identify the underlying cause of the OOS result.
- Corrective Actions: Corrective actions are implemented to address the identified root cause. This might involve recalibrating equipment, retraining personnel, or implementing new procedures.
- Preventive Actions: Preventive actions are taken to prevent similar OOS results from occurring in the future. This may involve improving existing procedures, implementing additional quality checks, or strengthening training programs.
- Documentation: The entire process, from the initial OOS result to the implementation of corrective and preventive actions, is meticulously documented.
OOS investigations require a scientific approach and a strong emphasis on data integrity. The goal is not only to explain the OOS result but also to prevent similar issues from occurring in the future and ensure that patients receive safe and effective medication.
Q 8. What is your understanding of change control in a GMP environment?
Change control in a GMP (Good Manufacturing Practices) environment is a systematic process for managing and approving any alterations that impact the manufacturing process, equipment, materials, or documentation. Think of it as a carefully orchestrated dance to ensure that any changes, no matter how small, don’t compromise the quality, safety, and efficacy of the final product. It’s all about preventing unintended consequences.
The process typically involves:
- Identifying the need for change: This could be anything from a minor equipment adjustment to a major process modification. For example, changing a supplier of a raw material or upgrading a software system.
- Submitting a change control request: A formal request, often documented through a specific form, details the proposed change, its rationale, and its potential impact.
- Review and approval: A cross-functional team, including quality control, manufacturing, and potentially regulatory affairs, evaluates the change request. They assess the potential risks and benefits and ensure compliance with GMP guidelines.
- Implementation: Once approved, the change is implemented under controlled conditions, often with enhanced monitoring and validation to confirm effectiveness.
- Verification and documentation: Post-implementation, the effectiveness of the change is verified, and all actions are meticulously documented. This documentation serves as an audit trail.
A well-defined change control system ensures consistency, reduces the risk of errors, and supports regulatory compliance. Imagine a scenario where a crucial parameter in a manufacturing process is inadvertently changed without proper control – the results could be disastrous, leading to product recalls or regulatory actions.
Q 9. Explain the importance of document control in pharmaceutical manufacturing.
Document control in pharmaceutical manufacturing is paramount; it’s the backbone of a robust quality system. Documents, including SOPs (Standard Operating Procedures), batch records, specifications, and training materials, are the lifeblood of the operation, ensuring that everything is done correctly and consistently. Without proper control, you’re building a house on sand.
Effective document control includes:
- Version control: Tracking and managing different versions of documents to avoid confusion and ensure everyone is using the most up-to-date version.
- Distribution and access control: Ensuring that only authorized personnel have access to specific documents.
- Change management: A formal process for approving and implementing changes to documents (often integrated with the overall change control system).
- Record keeping: Maintaining a complete and accurate record of all documents, including their creation, revisions, and approvals.
- Retention and archiving: Storing documents securely and for the required duration, complying with regulatory guidelines and industry standards.
Poor document control can lead to inconsistencies in manufacturing, deviations from approved procedures, and ultimately, product quality issues. For example, if an outdated SOP is used, it could result in a batch failure, necessitating a recall.
Q 10. How do you ensure compliance with current Good Distribution Practices (GDP)?
Ensuring compliance with Current Good Distribution Practices (GDP) requires a comprehensive approach focusing on maintaining the quality and integrity of pharmaceutical products throughout the distribution chain. It’s like running a relay race; each handoff needs to be seamless and accurate to ensure the final product reaches the patient in perfect condition.
Key aspects of GDP compliance include:
- Qualified personnel: Employing trained staff who understand GDP requirements and their responsibilities.
- Appropriate facilities and storage conditions: Maintaining storage facilities with controlled temperature and humidity to protect product quality.
- Effective transportation: Using appropriate transport methods (e.g., temperature-controlled vehicles) to prevent product degradation during shipment.
- Inventory management: Implementing systems to track product location, expiry dates, and batch numbers, preventing the distribution of outdated or compromised products.
- Complaint handling: Establishing procedures to investigate and address any complaints related to product quality or distribution.
- Documentation and record keeping: Meticulous documentation of all distribution activities, including product movement, storage conditions, and any deviations.
Failure to comply with GDP can lead to product recalls, regulatory sanctions, and reputational damage. For instance, improper storage temperature leading to product degradation can render a batch ineffective or even harmful.
Q 11. Describe your experience with auditing pharmaceutical manufacturing facilities.
My experience in auditing pharmaceutical manufacturing facilities involves a systematic and rigorous process to evaluate compliance with GMP regulations and internal standards. It’s akin to a detective investigating a crime scene, meticulously examining each piece of evidence to uncover any inconsistencies or potential risks.
My approach typically involves:
- Planning and scoping: Defining the objectives of the audit, identifying the areas to be reviewed, and developing a detailed audit plan.
- On-site assessment: Conducting on-site visits to observe processes, review documentation, and interview personnel.
- Data collection and analysis: Gathering evidence, such as batch records, SOPs, and test results, to verify compliance and identify areas for improvement.
- Reporting and communication: Preparing a comprehensive audit report that summarizes the findings, identifies non-conformances, and provides recommendations for corrective and preventive actions (CAPA).
- Follow-up: Monitoring the implementation of CAPAs to ensure effectiveness.
I’ve conducted audits covering various aspects of pharmaceutical manufacturing, from raw material handling to finished product testing, always striving for a balanced approach that recognizes both strengths and areas for improvement. A particular challenge I remember was identifying and resolving a discrepancy in a critical process parameter during an audit, which required collaborative efforts with the facility’s management to implement effective corrective actions.
Q 12. What is your understanding of risk assessment in pharmaceutical quality management?
Risk assessment in pharmaceutical quality management is a proactive approach to identify, analyze, and mitigate potential hazards that could affect product quality, safety, or efficacy. It’s about anticipating potential problems and taking steps to prevent them, rather than reacting to them after they’ve occurred. Imagine it like a ship’s captain charting a course, carefully considering weather patterns and potential obstacles to ensure a safe voyage.
Common risk assessment methodologies include:
- Failure Mode and Effects Analysis (FMEA): A systematic approach to identify potential failure modes and their effects on the product or process.
- Hazard Analysis and Critical Control Points (HACCP): A preventive approach to identify and control biological, chemical, or physical hazards in food and drug manufacturing.
- Risk Matrix: A tool that helps prioritize risks based on their likelihood and potential impact.
These methodologies are essential for maintaining product quality and ensuring regulatory compliance. For example, a risk assessment might reveal a vulnerability in a specific process step; consequently, implementing appropriate control measures such as enhanced monitoring or process validation can significantly reduce the risk of product failure.
Q 13. How do you manage and resolve conflicts concerning quality standards?
Managing and resolving conflicts concerning quality standards requires a collaborative and objective approach. It’s about finding common ground and solutions that benefit both the organization and the patient. Think of it as mediating a dispute, guiding everyone towards a mutually agreeable outcome.
My approach involves:
- Open communication: Creating a safe space for all parties to express their concerns and perspectives.
- Objective assessment: Reviewing the facts and evidence without bias to understand the root cause of the conflict.
- Collaborative problem-solving: Working with all parties involved to identify solutions that meet quality standards and address concerns.
- Documentation: Maintaining a detailed record of the conflict, the steps taken to resolve it, and the outcome.
- Escalation if necessary: If resolution is not possible at a lower level, escalating the conflict to higher management for further action.
A memorable situation involved a disagreement between two departments regarding the interpretation of a quality standard. By facilitating open dialogue and collaboration, we were able to clarify the standard, and consequently, the conflict was resolved, reinforcing a stronger collaborative culture.
Q 14. Explain your understanding of the lifecycle of a pharmaceutical product.
The lifecycle of a pharmaceutical product encompasses all stages from initial research and development to its eventual discontinuation. It’s a long and complex journey, demanding meticulous planning and execution at every stage. Imagine it as a marathon, requiring endurance, strategy, and precise execution.
The key stages include:
- Discovery and pre-clinical development: Identifying potential drug candidates and conducting laboratory and animal studies.
- Clinical development: Conducting clinical trials in humans to assess safety and efficacy.
- Regulatory approval: Submitting the drug for approval to regulatory agencies like the FDA or EMA.
- Manufacturing and commercialization: Producing and marketing the drug to patients.
- Post-marketing surveillance: Monitoring the drug’s safety and efficacy after it’s launched.
- Product lifecycle management: Ongoing management and potential reformulation or discontinuation of the drug.
Understanding the entire lifecycle is crucial for effective product management. Each stage presents unique challenges and opportunities; thorough planning and rigorous quality control are essential at every point to ensure the safe and effective use of the pharmaceutical product.
Q 15. Describe your experience with quality system certifications, such as ISO 9001.
My experience with ISO 9001 and other quality system certifications is extensive. I’ve been directly involved in implementing, maintaining, and auditing these systems across various pharmaceutical companies. This includes leading internal audits, preparing for external audits from certification bodies, and driving continuous improvement initiatives. Think of ISO 9001 as the foundation of a robust quality management system; it provides a framework for consistently meeting customer requirements and enhancing customer satisfaction. In practice, this translates to meticulously documented procedures, rigorous internal controls, and proactive risk management. For example, in my previous role, we successfully transitioned to a new ERP system while maintaining ISO 9001 certification. This involved extensive process mapping, training, and validation to ensure a seamless transition and adherence to the quality management system. We also implemented a robust corrective and preventive action (CAPA) system to identify and rectify any non-conformances swiftly.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure the accuracy and reliability of analytical testing data?
Ensuring the accuracy and reliability of analytical testing data is paramount in the pharmaceutical industry. We achieve this through a multi-faceted approach. First, we meticulously validate all analytical methods to demonstrate their accuracy, precision, specificity, and linearity. This validation process often involves rigorous statistical analysis and the generation of detailed validation reports. Think of it as proving the testing method itself is reliable before it’s used. Second, we employ robust quality control measures, such as the use of certified reference standards, regular instrument calibration and maintenance, and participation in proficiency testing programs to compare our results with those of other accredited labs. For example, we might use a certified reference standard to verify the concentration of a drug substance, and then participate in inter-laboratory comparisons to assess the accuracy of our results. Third, we implement a robust data management system including electronic laboratory notebooks (ELNs) and LIMS (Laboratory Information Management System) to ensure data integrity and traceability, preventing data manipulation and loss. Finally, comprehensive training for laboratory personnel is crucial in upholding data quality.
Q 17. Explain your understanding of stability testing and its importance.
Stability testing is crucial for determining the shelf life and storage conditions of pharmaceutical products. It involves storing samples of the drug product under various environmental conditions (e.g., different temperatures, humidity, and light exposure) and analyzing them periodically over time to assess changes in its quality attributes like potency, purity, and appearance. This ensures the product remains safe and effective throughout its intended shelf life. Imagine you’re making a cake; stability testing is like checking if your cake remains fresh and palatable after a week, a month, or even longer under different storage conditions (room temperature vs. refrigerator). The results obtained from stability testing are used to determine the expiration date and storage recommendations for the drug product, ensuring patient safety and product efficacy.
For example, we recently conducted a stability study on a new drug formulation to determine its shelf life under different temperature conditions. This involved regular testing for degradation products and potency, ultimately allowing us to define optimal storage conditions and provide an accurate expiration date.
Q 18. Describe your experience with the design and execution of validation studies.
My experience in designing and executing validation studies is broad. Validation is the process of demonstrating that equipment, processes, and systems consistently perform as expected. This involves defining acceptance criteria, developing a validation protocol, executing the study, analyzing the data, and generating a comprehensive validation report. I have been involved in validating various aspects of pharmaceutical manufacturing, such as cleaning validation (demonstrating the effectiveness of cleaning procedures to prevent cross-contamination), analytical method validation (as discussed previously), and computer system validation (ensuring the reliability and security of software used in pharmaceutical operations). A real-world example includes validating a new high-performance liquid chromatography (HPLC) system. This involved meticulously documenting every step of the process, from system suitability testing to linearity and accuracy assessments, ensuring the system met all regulatory requirements before its use in routine testing.
Q 19. What are some common challenges in maintaining compliance with pharmaceutical regulations?
Maintaining compliance with pharmaceutical regulations presents ongoing challenges. Some common issues include keeping up with ever-evolving regulations (e.g., changes in GMPs, new guidances), managing data integrity across multiple systems, ensuring adequate resources for training and compliance programs, and navigating the complexities of global regulations for multinational pharmaceutical companies. For instance, maintaining data integrity can be difficult due to the large amounts of data generated in the pharmaceutical industry, including electronic laboratory notebooks and manufacturing batch records. It requires robust data management systems, thorough training, and appropriate audit trails. Another challenge is adapting to new technologies; the industry is rapidly embracing new technologies, requiring personnel training and system validation, posing a significant challenge to compliance.
Q 20. How do you stay updated on changes in pharmaceutical regulations and industry standards?
Staying updated on changes in pharmaceutical regulations and industry standards is a continuous process. I actively participate in industry conferences and webinars, subscribe to regulatory newsletters and journals (such as FDA announcements, EMA updates, and PhRMA publications), and engage with regulatory agencies and industry experts. Membership in professional organizations like the PDA (Parenteral Drug Association) or ISPE (International Society for Pharmaceutical Engineering) also provides access to valuable updates and networking opportunities. I also leverage online resources and databases to track changes to regulatory guidelines and best practices. This proactive approach ensures my knowledge and practices remain current and compliant.
Q 21. Describe your experience with quality metrics and reporting.
My experience with quality metrics and reporting is extensive. I’ve been responsible for designing, implementing, and analyzing key performance indicators (KPIs) relevant to various aspects of pharmaceutical quality, including manufacturing yield, product quality, and compliance. This involves collecting and analyzing data from diverse sources, using statistical methods to identify trends and areas for improvement, and creating clear and concise reports for management and regulatory agencies. The reporting must clearly communicate the effectiveness of quality systems and highlight any areas requiring immediate attention. For example, I’ve used statistical process control (SPC) charts to monitor manufacturing processes and identify potential deviations from expected performance. I then use these charts and other data to construct comprehensive quality reports illustrating our performance and areas where we’re excelling or need improvement. These reports are essential for making data-driven decisions to enhance efficiency and quality.
Q 22. Explain your understanding of the role of quality control in preventing product defects.
Quality Control (QC) in the pharmaceutical industry is a critical function designed to prevent product defects and ensure the safety and efficacy of medications. It’s like a diligent gatekeeper, meticulously examining every step of the manufacturing process to identify and eliminate any potential problems before they reach the patient.
QC encompasses a wide range of activities, including:
- Raw material testing: Ensuring the raw materials used meet predefined specifications for purity, identity, and quantity. For example, testing the potency of active pharmaceutical ingredients (APIs).
- In-process testing: Monitoring critical parameters during the manufacturing process to ensure consistent product quality. This might involve checking the pH level of a solution at various stages.
- Finished product testing: Rigorous testing of the final product to verify it conforms to all established specifications, including potency, purity, stability, and appearance. Think of this as the final quality check before the medication is released.
- Environmental monitoring: Maintaining a clean and controlled manufacturing environment to prevent contamination. This involves regular monitoring of air, water, and surface cleanliness.
- Calibration and maintenance of equipment: Ensuring that all equipment used in the manufacturing process is properly calibrated and maintained to deliver accurate and reliable results.
By proactively identifying and addressing potential defects at each stage, QC minimizes the risk of releasing substandard products and safeguards patient safety. A failure to implement robust QC measures can lead to significant financial losses, reputational damage, and even harm to patients.
Q 23. How would you approach a situation where a regulatory inspector finds a non-compliance issue?
Discovering a non-compliance issue during a regulatory inspection is a serious event requiring a swift and methodical response. My approach would be based on transparency, immediate corrective action, and thorough root cause analysis.
- Acknowledge and document the issue: Immediately acknowledge the finding to the inspector and document it accurately. This sets the tone of cooperation and professionalism.
- Implement immediate corrective action: Take immediate steps to correct the non-compliance issue. This might involve stopping the affected process, quarantining potentially affected products, or implementing temporary process changes.
- Conduct a thorough investigation: Initiate a root cause analysis to determine the underlying reasons for the non-compliance. This could involve interviewing personnel, reviewing records, and analyzing data.
- Develop a comprehensive corrective and preventive action (CAPA) plan: Develop a detailed CAPA plan to prevent recurrence of the issue. This plan should include specific actions, timelines, responsibilities, and verification measures.
- Communicate findings and CAPA plan to the regulatory agency: Communicate the findings of the investigation and the CAPA plan to the regulatory agency. This shows proactive engagement and commitment to compliance.
- Monitor effectiveness of CAPA plan: Monitor the effectiveness of the CAPA plan to ensure that it is successful in preventing future occurrences.
Throughout this process, maintaining open communication with the regulatory inspector is crucial. Transparency and a commitment to addressing the issue effectively are key to mitigating the impact of the non-compliance finding.
Q 24. Describe your experience with implementing and maintaining a quality management system (QMS).
I have extensive experience in implementing and maintaining Quality Management Systems (QMS), primarily based on ISO 9001 and GMP (Good Manufacturing Practices) principles. My experience includes leading the implementation of QMS in several pharmaceutical manufacturing facilities.
The process typically involves:
- Gap analysis: Assessing the current state of the organization’s quality system against the requirements of the chosen standard (e.g., ISO 9001, GMP).
- Development of procedures and documentation: Creating detailed Standard Operating Procedures (SOPs) and other documentation to define processes and ensure consistency.
- Training and communication: Providing comprehensive training to personnel on the QMS requirements and procedures.
- Implementation of the system: Implementing the QMS across the organization, including the establishment of quality metrics and KPIs.
- Internal audits: Conducting regular internal audits to ensure the effectiveness of the QMS.
- Management review: Regularly reviewing the QMS’s performance and making necessary improvements.
- Continuous improvement: Continuously monitoring and improving the QMS to ensure its ongoing effectiveness.
For instance, in a previous role, I led the implementation of a new ERP system integrated with our QMS, leading to a 20% reduction in documentation errors and a 15% increase in audit efficiency. This demonstrates the tangible benefits of a well-implemented QMS.
Q 25. Explain your understanding of the principles of quality by design (QbD).
Quality by Design (QbD) is a proactive approach to pharmaceutical development and manufacturing that focuses on understanding the science behind the product and process, leading to greater product quality and consistency. It’s about building quality into the product from the very beginning, rather than inspecting it in at the end.
Key principles of QB include:
- Understanding the product’s critical quality attributes (CQAs): Identifying the characteristics of the product that are essential for its safety and efficacy (e.g., potency, purity, dissolution rate).
- Identifying critical process parameters (CPPs): Pinpointing the manufacturing process steps that have the most significant impact on CQAs.
- Establishing design space: Defining the range of CPPs within which consistent CQAs can be achieved. This provides flexibility while maintaining quality.
- Risk assessment and management: Systematically evaluating and mitigating potential risks to product quality throughout the development and manufacturing processes.
QbD facilitates better control over the manufacturing process, leading to reduced variability and higher product quality. Imagine baking a cake – QbD would involve understanding how each ingredient (CPP) affects the final product’s taste and texture (CQA). This allows for better control over the baking process and a more consistent outcome.
Q 26. How would you handle a situation where a critical supplier fails to meet quality standards?
A critical supplier failing to meet quality standards is a serious situation that requires immediate action. My approach would involve a structured process:
- Immediate communication: Contact the supplier immediately to understand the cause of the non-compliance and their proposed corrective actions.
- Assessment of impact: Assess the potential impact of the non-compliance on product quality and patient safety.
- Implementation of corrective actions: Work with the supplier to implement corrective actions and verify their effectiveness. This might involve additional testing, process improvements, or supplier audits.
- Consider alternative suppliers: If the supplier consistently fails to meet standards, evaluate alternative qualified suppliers to mitigate risk. This involves a thorough qualification process of any new supplier.
- Documentation: Thoroughly document all communication, actions taken, and results achieved.
- Long-term preventative measures: Implement long-term measures to prevent future occurrences, such as more frequent supplier audits, enhanced quality agreements, or improved supplier relationship management.
In my experience, a collaborative approach with the supplier, combined with clear expectations and consequences for non-compliance, is the most effective way to manage such situations. For instance, implementing a robust supplier performance management system can greatly minimize the risk of future failures.
Q 27. Describe your experience with root cause analysis techniques used in quality investigations.
Root cause analysis (RCA) is a crucial tool for investigating quality deviations and preventing future occurrences. I’m proficient in several RCA techniques, including the ‘5 Whys,’ Fishbone diagrams (Ishikawa diagrams), and Fault Tree Analysis (FTA).
The ‘5 Whys’ is a simple yet powerful technique. For example, if a batch failed potency testing, we might ask:
- Why did the batch fail? Because the API potency was low.
- Why was the API potency low? Because the supplier provided sub-standard material.
- Why was the material sub-standard? Because their manufacturing process was not properly validated.
- Why wasn’t the process validated? Because they lacked appropriate quality control procedures.
- Why were these procedures lacking? Because of inadequate training and oversight.
Fishbone diagrams provide a more visual representation of potential causes, categorizing them into different groups (e.g., people, methods, materials, environment). FTA provides a structured approach to identifying potential causes of a system failure, useful for complex situations. The choice of technique depends on the complexity of the issue. No matter the method, a thorough investigation, involving relevant personnel and a commitment to objectivity, is critical to uncovering the true root cause.
Key Topics to Learn for Knowledge of Pharmaceutical Industry Standards Interview
- Good Manufacturing Practices (GMP): Understand the principles and applications of GMP across different pharmaceutical manufacturing stages, including documentation, quality control, and deviation management. Consider practical scenarios involving non-compliance and corrective actions.
- Quality by Design (QbD): Explore the theoretical framework of QbD and its practical application in pharmaceutical development and manufacturing. Focus on understanding how risk assessment and process understanding contribute to product quality and consistency.
- Regulatory Compliance (FDA, EMA, etc.): Familiarize yourself with the key regulatory agencies and their respective guidelines for drug development and approval. Practice analyzing hypothetical scenarios to assess regulatory compliance.
- Pharmaceutical Quality Systems (PQS): Learn about the implementation and maintenance of effective PQS, encompassing aspects like change control, CAPA (Corrective and Preventative Actions), and quality audits. Be prepared to discuss real-world examples of PQS challenges and solutions.
- Data Integrity: Understand the principles of ALCOA+ (Attributable, Legible, Contemporaneous, Original, Accurate + Complete, Consistent, Enduring) and its importance in maintaining accurate and reliable data throughout the pharmaceutical lifecycle. Consider the consequences of data integrity breaches.
- Validation and Qualification: Learn about the various types of validation (process, cleaning, equipment) and qualification (installation, operational, performance) and their role in ensuring consistent product quality and regulatory compliance. Prepare to discuss practical examples and challenges.
Next Steps
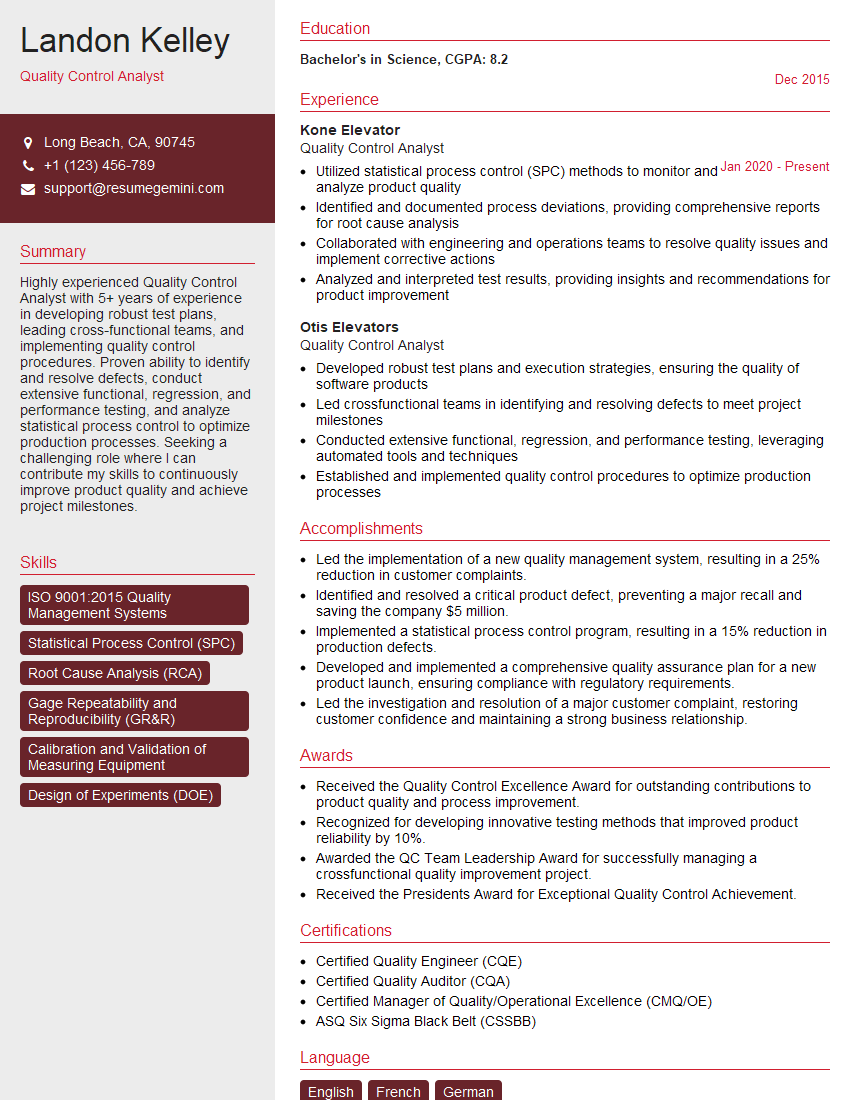
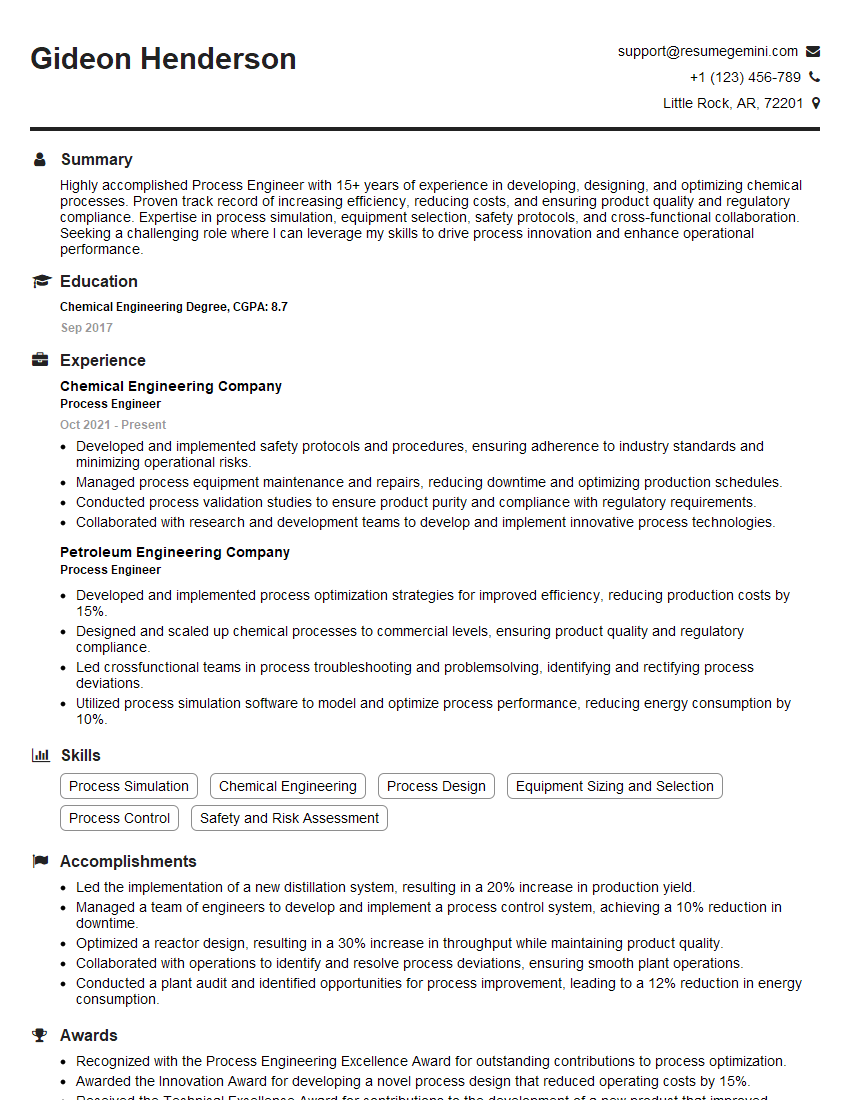
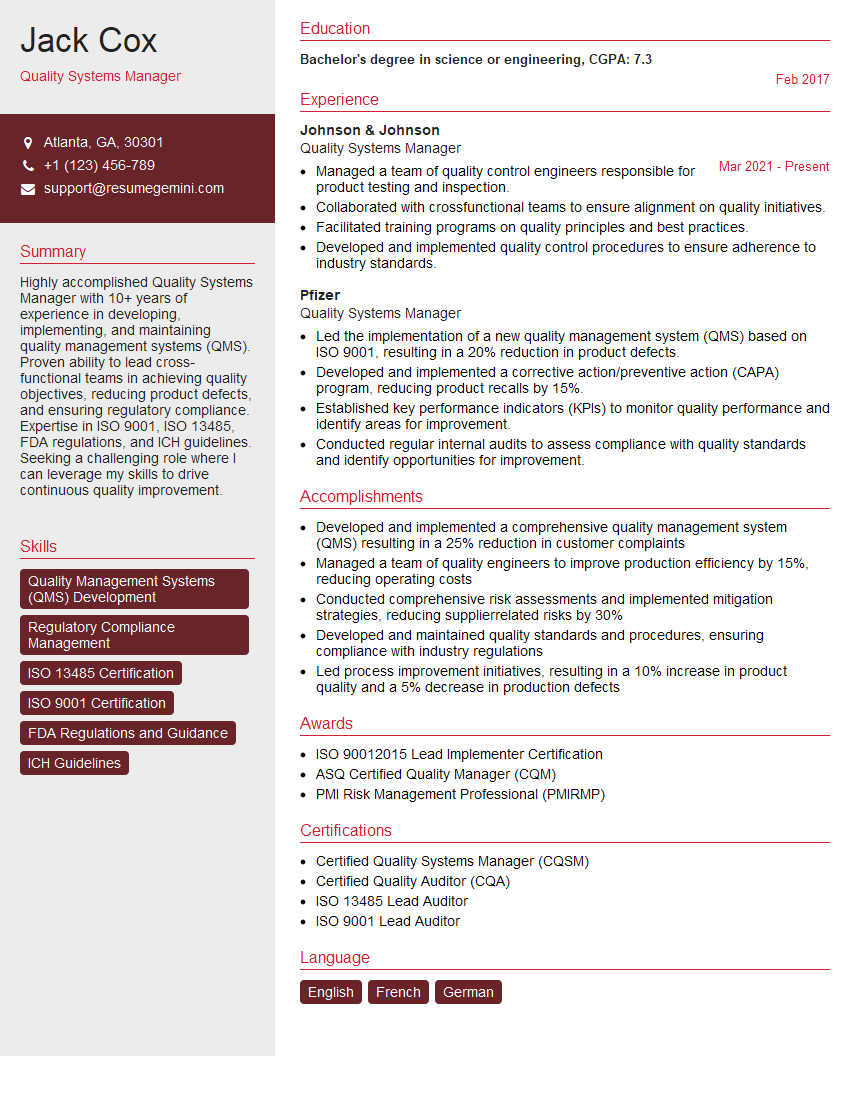
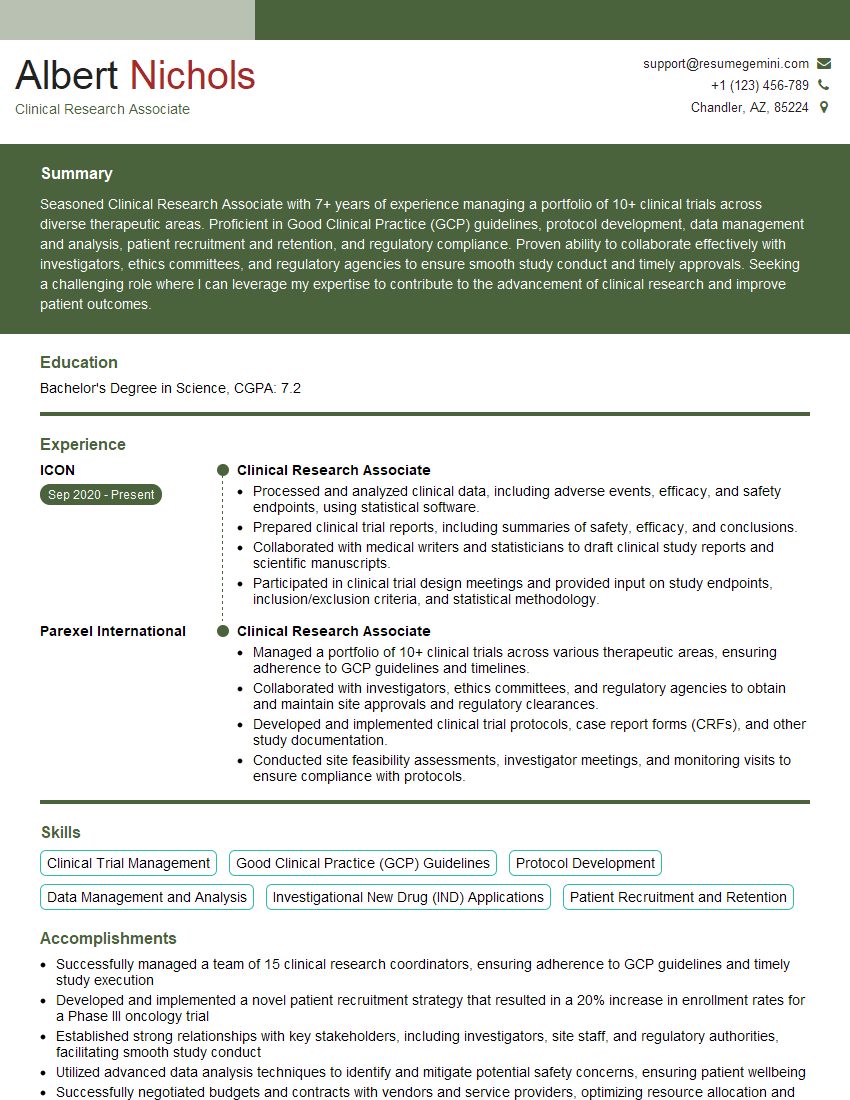
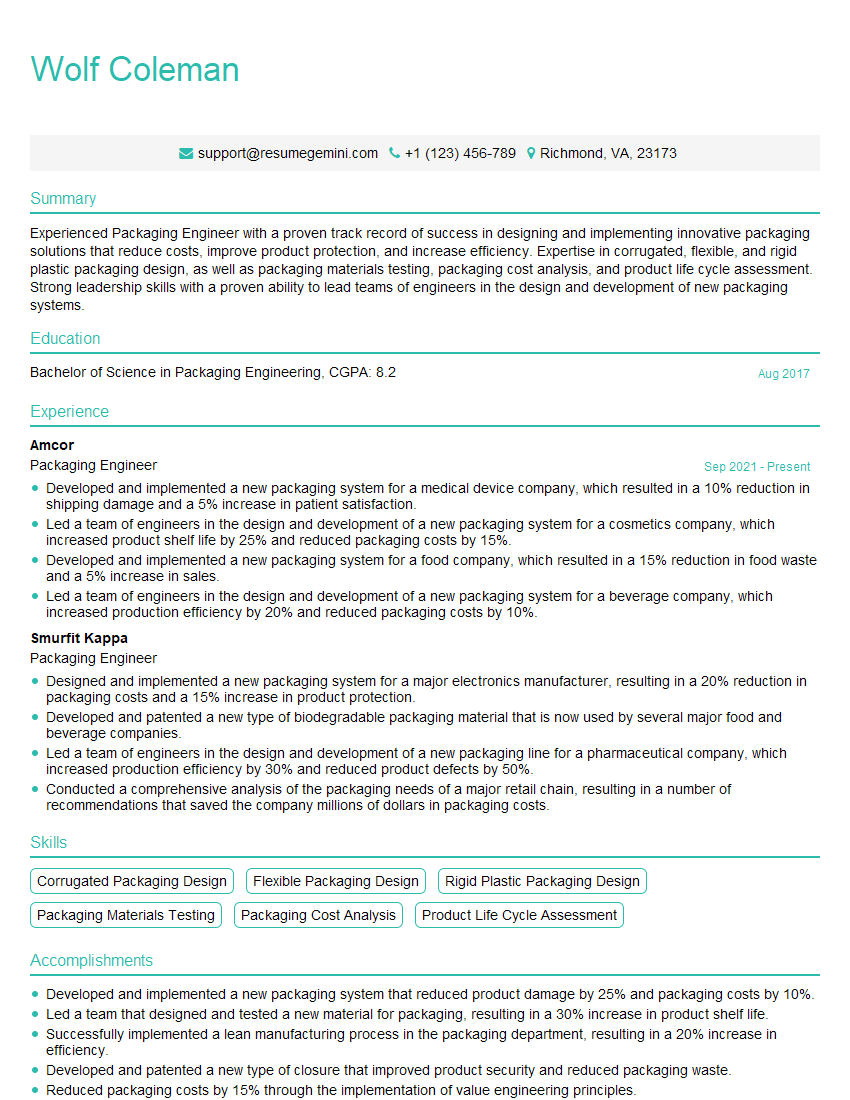
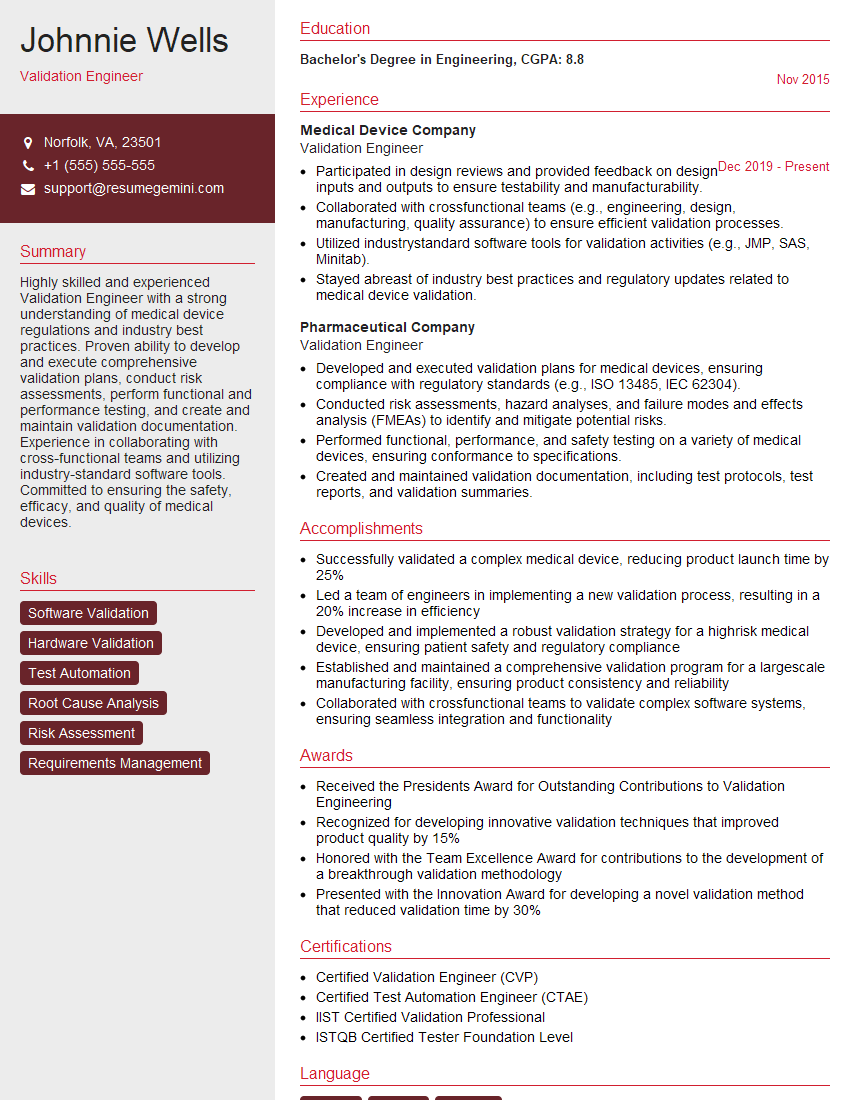
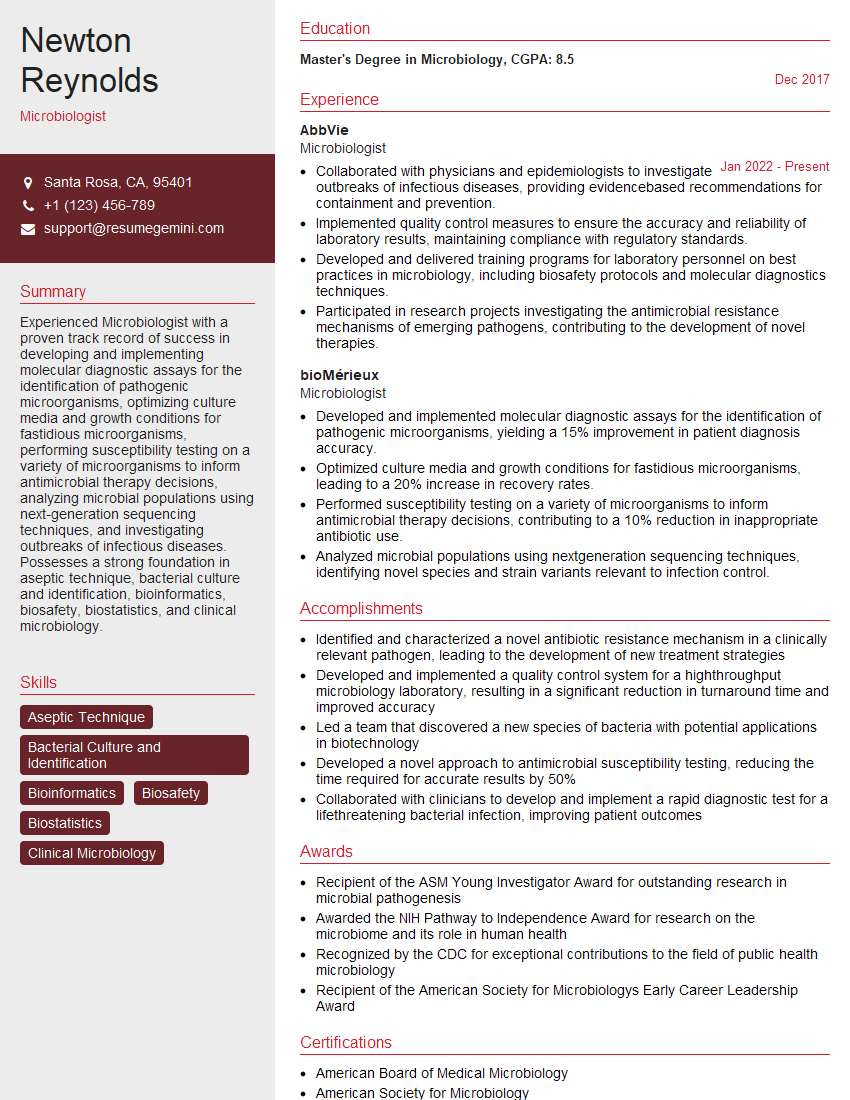
Mastering Knowledge of Pharmaceutical Industry Standards is crucial for career advancement in this highly regulated field. A strong understanding of these concepts demonstrates your commitment to quality and compliance, making you a valuable asset to any pharmaceutical organization. To significantly boost your job prospects, create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini can be a trusted resource to help you build a professional and impactful resume that gets noticed by recruiters. Examples of resumes tailored to showcasing expertise in Knowledge of Pharmaceutical Industry Standards are available through ResumeGemini to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good