The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Pin Plating interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Pin Plating Interview
Q 1. Describe the different types of pins used in pin plating.
Pin plating utilizes various pin types, each chosen based on the fracture’s specifics and the surgeon’s preference. The core distinction lies in their material and design.
- Stainless Steel Pins: These are the most common, offering good strength and biocompatibility. They’re readily available and relatively inexpensive.
- Titanium Pins: Titanium pins are stronger and lighter than stainless steel, making them ideal for certain situations. Their biocompatibility is excellent, minimizing the risk of allergic reactions. However, they are more expensive.
- Kirschner Wires (K-wires): These are thin, smooth pins primarily used for smaller bones or temporary fixation. They’re easily inserted but can be less rigid than other pins.
- Steinmann Pins: These are larger diameter pins than K-wires, offering greater stability for larger fractures. They are often used for longer bone segments.
- Cancellous Screws: While not strictly ‘pins’, cancellous screws are sometimes used in conjunction with plating, especially in areas where purchase in cancellous bone (spongy bone) is needed.
The choice of pin material and diameter is crucial for successful fracture healing and depends on factors like bone density, fracture pattern, and the patient’s overall health.
Q 2. Explain the indications and contraindications for pin plating.
Pin plating is indicated for a variety of fractures, particularly those that are unstable and require rigid fixation to allow for proper healing. Suitable cases include comminuted fractures (fractures with multiple bone fragments), displaced fractures (fractures where the bone ends are not aligned), and fractures in areas where adequate bone stock is present for pin purchase.
Contraindications include situations where the bone quality is severely compromised (e.g., osteoporotic bone), significant soft tissue injury which might compromise healing, or in cases where infection is present at the fracture site. Furthermore, pin plating might not be suitable for certain pediatric patients whose bones are still growing rapidly.
The decision of whether or not to use pin plating is made on a case-by-case basis, taking into account the individual patient’s anatomy, fracture pattern, and overall health.
Q 3. What are the steps involved in the surgical procedure of pin plating?
The surgical procedure for pin plating generally follows these steps:
- Preoperative planning: This involves imaging studies (X-rays, CT scans) to assess the fracture, plan the incision, and determine the appropriate number, size, and placement of pins and plate.
- Incision and exposure: A surgical incision is made over the fracture site to expose the fractured bone.
- Reduction: The fractured bone fragments are carefully manipulated back into their anatomical position (reduction).
- Pin insertion: Pins are strategically inserted into the bone fragments, aiming for stable fixation. The surgeon may use image intensifier guidance for precise pin placement.
- Plate application: An appropriate plate is chosen and secured to the bone, further stabilizing the fracture.
- Screw insertion: Screws are used to secure the plate to the bone.
- Wound closure: The incision is closed in layers, using sutures or staples.
- Postoperative care: This includes pain management, wound care, and monitoring for any complications.
The exact steps may vary depending on the fracture’s complexity and the surgeon’s technique. A surgical assistant plays a crucial role in many of these steps to facilitate the process.
Q 4. How do you select the appropriate size and number of pins for a fracture?
Selecting the appropriate size and number of pins is critical for successful fracture healing. It’s a balance between providing sufficient stability and minimizing damage to the surrounding tissues. The surgeon considers several factors:
- Fracture type and location: A complex fracture might need more pins for stability compared to a simple fracture.
- Bone density: Osteoporotic bones may require larger or more pins to achieve adequate purchase.
- Bone size: Pin diameter should be appropriately sized relative to the bone’s diameter. Too large a pin risks weakening the bone, whereas too small a pin may lead to inadequate fixation.
- Surgical approach: The available space for pin insertion might influence pin selection and positioning.
Generally, the goal is to achieve a stable fixation with minimal pin-related trauma. Preoperative planning utilizing imaging studies is crucial in guiding this decision.
For instance, a small, stable fracture in a child’s wrist might only require one or two small K-wires, while a severely comminuted femur fracture in an adult might necessitate multiple Steinmann pins and a large plate for sufficient stability.
Q 5. Describe the different techniques used for pin insertion.
Several techniques are employed for pin insertion. The choice depends on the pin type, bone characteristics, and surgeon preference:
- Freehand technique: This involves manually drilling the pin into the bone using a drill guide. It’s relatively straightforward for simple fractures but relies heavily on the surgeon’s skill and experience.
- Image intensifier guidance: Fluoroscopy (real-time X-ray imaging) allows for precise pin placement, particularly important in complex fractures or cases where the pin’s trajectory needs careful consideration. This ensures the pin is appropriately placed within the bone fragment without causing iatrogenic injury.
- Drill guides: Various drill guides are used to ensure accurate and safe pin insertion. These guides help prevent slippage and ensure proper depth of penetration.
Regardless of the chosen method, meticulous technique is essential to prevent soft tissue injury and iatrogenic fractures.
Q 6. What are the potential complications associated with pin plating?
Potential complications associated with pin plating include:
- Pin tract infection: This is a common complication, often presenting as local pain, swelling, and purulent drainage around the pin sites. Early detection and prompt treatment are crucial.
- Non-union: Failure of the fracture to heal properly. This can result from inadequate fixation, poor bone quality, or infection.
- Malunion: Healing of the fracture in a malaligned position, leading to deformity and functional limitations.
- Implant failure: Fracture of the plate or pins. This usually results from stress shielding.
- Nerve or vessel injury: Injury to nearby nerves or blood vessels during the surgical procedure.
- Pin breakage: Pins can break, especially under stress.
- Allergic reaction to implant material: This is relatively rare but can be a significant concern.
Careful surgical technique, appropriate patient selection, and diligent postoperative monitoring can minimize the risks of these complications.
Q 7. How do you manage pin tract infections?
Pin tract infection management begins with prompt recognition. Signs include local pain, swelling, redness, warmth, and purulent drainage at the pin site. Early treatment is crucial to prevent serious complications.
Management strategies typically include:
- Oral antibiotics: Broad-spectrum antibiotics are usually prescribed initially, adjusted based on culture results.
- Local wound care: Careful cleaning and dressing of the wound to remove debris and promote healing. Regular dressing changes are essential.
- Pin removal: In cases of persistent infection, pin removal may be necessary. This facilitates drainage and improves the effectiveness of antibiotic treatment. Often, the surgeon will remove the pin, debride infected tissue, and possibly culture the wound site for sensitive antibiotics.
- Surgical debridement: In severe cases, surgical removal of infected tissue may be needed.
Regular monitoring and follow-up are essential to ensure successful treatment and prevent recurrence. The decision on which treatment method to use depends on the severity of the infection, and the patient’s overall health.
Q 8. How do you assess the stability of a fracture after pin plating?
Assessing fracture stability after pin plating involves a multi-faceted approach combining clinical examination and imaging. Initially, we assess the patient’s pain levels and range of motion. Significant pain or limited movement suggests instability. More objectively, we rely on radiographic imaging – post-operative X-rays are crucial. We look for things like:
- Alignment: Is the fracture reduced (bones properly aligned) and maintained? Any significant displacement suggests instability.
- Apposition: Are the fracture fragments in close contact? Gaps indicate potential instability and delayed healing.
- Pin placement: Are the pins adequately placed to provide sufficient fixation? Pins that are too short, poorly positioned, or that have loosened are indicative of instability.
For example, if we see significant overriding of the fracture fragments on X-ray, despite the presence of pins, we know there is instability. This might require additional fixation, like a longer plate or supplementary screws. We might also employ computed tomography (CT) scans for a more detailed three-dimensional assessment of the fracture and the pin placement, particularly in complex cases.
Q 9. What are the post-operative instructions for patients undergoing pin plating?
Post-operative instructions for patients who have undergone pin plating are critical for successful healing and minimizing complications. These are usually tailored to the specific fracture and patient condition, but generally include:
- Pain management: Patients are prescribed analgesics (pain medication) to manage postoperative pain. We also teach them non-pharmacological pain management techniques like ice application.
- Wound care: Meticulous wound care is essential to prevent infection. Patients are instructed on proper cleaning and dressing changes, and they are advised to keep the area clean and dry.
- Elevation and immobilization: The affected limb should be elevated to reduce swelling. A cast or splint may be used to provide initial immobilization, depending on the location and type of fracture. The extent of immobilization is dictated by the fracture pattern and the stability of the fixation.
- Physical therapy: Early mobilization is important to prevent stiffness and muscle atrophy. Patients are referred to physical therapy for customized exercises to gradually regain range of motion and strength. The therapy commences after the initial healing phase.
- Follow-up appointments: Regular follow-up appointments are crucial to monitor healing progress, assess stability, and detect any complications like infection or malunion.
- Activity restrictions: Patients are typically restricted from weight-bearing on the affected limb initially, with gradual progression as healing occurs. Specific instructions about activity levels will be given depending upon the healed bone’s strength and the type of fracture.
For example, a patient with a tibial fracture might be non-weight-bearing for 6-8 weeks initially, gradually increasing weight-bearing under the guidance of their physician and physical therapist.
Q 10. Explain the use of image intensifiers during pin plating.
Image intensifiers are fluoroscopic devices that provide real-time X-ray imaging during surgery. In pin plating, they’re indispensable for several reasons:
- Accurate pin placement: The image intensifier allows the surgeon to visualize the bone and pin in real-time, ensuring precise placement to achieve optimal fracture reduction and fixation. This minimizes the risk of injuring nearby nerves, blood vessels, or other structures.
- Intraoperative assessment: During the procedure, the surgeon can continually assess the reduction (alignment) of the fracture and adjust pin placement as needed. This ensures accurate alignment is maintained throughout the process.
- Minimizing radiation exposure: While using radiation, the image intensifier’s pulsed mode minimizes exposure to the surgical team and patient, only utilizing the X-ray when necessary.
- Confirmation of fixation: After pin placement, the image intensifier helps confirm that the fracture is adequately stabilized and that the pins are secure. We can see if the fracture fragments remain perfectly aligned and whether the pins have adequately penetrated the bone fragments.
Imagine trying to assemble a complex jigsaw puzzle blindfolded. The image intensifier is like having X-ray vision – it provides the necessary guidance to ensure every piece (pin) is positioned correctly.
Q 11. How do you address malreduction during pin placement?
Malreduction, or improper alignment of the fracture fragments, during pin placement requires immediate corrective action. The approach depends on the extent of malreduction and the surgical stage.
- Minor adjustments: If the malreduction is minor, we might attempt manipulation under image intensification. This involves using specialized instruments to gently reposition the bone fragments while continuously monitoring alignment using the image intensifier.
- Revision: If manipulation fails, revision of the pin placement might be necessary. This could involve removing some pins and repositioning them or adding additional pins for better stabilization. In some cases, the surgeon might use bone reduction forceps or other instruments to improve the fracture fragments’ alignment.
- Alternative fixation: In cases of severe malreduction where pin placement alone is insufficient, the surgeon may consider additional fixation methods such as the addition of screws or a different plate.
For instance, if a fracture is angulated (bent) after several pins have been placed, we might use a small, specialized device called a bone reduction clamp to gently straighten it under fluoroscopic guidance before placing additional pins. In severe cases, a different type of plate might be necessary to provide more rigid fixation.
Q 12. Describe the different types of plates used in conjunction with pins.
Various plates are used in conjunction with pins, each designed for specific fracture patterns and bone types. Common types include:
- Dynamic Compression Plates (DCP): These plates have angled holes to allow for compression across the fracture site, promoting bone healing. The compression helps to hold the fracture fragments together tightly.
- Locking Compression Plates (LCP): These plates have locking screws that engage directly into the plate, providing more stable fixation, even in osteoporotic bone (weak bone). They’re particularly useful in situations where bone quality is poor.
- Reconstruction Plates: These are designed for complex fractures requiring more extensive reconstruction. They often have multiple holes and different angles, offering greater versatility.
- Buttress Plates: These provide support to a fracture at a specific location or angle and are often used in conjunction with pins. They are particularly useful for fractures that have a tendency to slide along a specific plane.
The choice of plate depends on factors such as fracture morphology, bone quality, and the surgeon’s preference. A DCP might be ideal for a simple, stable fracture in a healthy bone, whereas an LCP might be preferred for an osteoporotic bone or a more complex fracture requiring enhanced stability.
Q 13. What are the advantages and disadvantages of pin plating compared to other fracture fixation techniques?
Pin plating, like any surgical technique, has advantages and disadvantages compared to other fracture fixation methods like intramedullary nailing or external fixation:
- Advantages:
- Anatomical reduction: Allows for precise anatomical reduction and stable fixation.
- Versatility: Applicable to various fracture patterns and locations.
- Early mobilization: Often allows for earlier weight-bearing and mobilization compared to external fixation.
- Lower risk of pin tract infection (compared to external fixation): Pins are less exposed to the environment.
- Disadvantages:
- Surgical invasiveness: Requires an open surgical approach, leading to more extensive soft tissue damage compared to intramedullary nailing.
- Potential for hardware complications: Risk of pin breakage, loosening, or irritation.
- Lengthy surgical time: Can be a relatively lengthy procedure, particularly in complex fractures.
- Post-operative rehabilitation required: Requires significant post-operative rehabilitation to regain full function.
For example, pin plating may be preferred over intramedullary nailing for a comminuted (fragmented) fracture of the distal radius because it allows for precise fragment reduction and stabilization, while intramedullary nailing might not offer the same level of control in such cases. However, intramedullary nailing might be better suited for a long bone fracture (like a femur) where it can achieve robust stabilization with less soft tissue disturbance.
Q 14. How do you manage a broken pin during surgery?
A broken pin during surgery is an infrequent but potentially serious complication. Management depends on the location of the break and the extent of the damage.
- Minor break near the surface: If the break is minor and near the skin surface, the broken portion might be left in place if it’s not interfering with fixation. It’s often left, as removal might cause more soft tissue damage.
- Significant break or deep break: For a significant break or if the broken portion is deep within the bone and interfering with fixation, it needs to be carefully removed using appropriate instruments under image intensification. We carefully evaluate if repositioning and further fixation with other pins is required.
- Additional fixation: After the broken pin is removed, we assess the stability of the fracture. If deemed necessary, additional pins or screws might be added to maintain adequate fixation.
Imagine a supporting beam breaking in a building. If it’s a small, non-critical piece, leaving it in place might be acceptable. However, if a major beam is broken, it necessitates immediate attention and replacement/repair. Similarly, with a broken pin, the course of action hinges upon the situation’s severity and impact on fracture stability.
Q 15. How do you handle pin migration?
Pin migration, the movement of a fixation pin from its original position within the bone, is a serious complication in pin plating. It can lead to further injury, impaired healing, and the need for revision surgery. Handling pin migration involves a multi-pronged approach, starting with prevention.
- Proper Pin Placement: Precise placement of pins, ensuring they are deeply seated within the bone’s cortical layer and avoiding critical neurovascular structures, is paramount. We use image guidance (fluoroscopy) to confirm accurate pin placement.
- Appropriate Pin Diameter and Number: Selecting the right pin diameter relative to bone density and the fracture pattern minimizes the risk of breakage and migration. More robust fractures may need more pins for secure fixation.
- Stable Fixation: The fixation construct itself must be stable to reduce stress on the pins. Adequate reduction (alignment) of the fracture fragments before pin placement is crucial.
If migration does occur, we assess the clinical significance. Minor migration may be monitored clinically and radiographically. Significant migration, causing pain, instability, or compromising healing, necessitates surgical intervention. This might involve pin removal and replacement, or alternative fixation methods like plate and screw fixation.
Career Expert Tips:
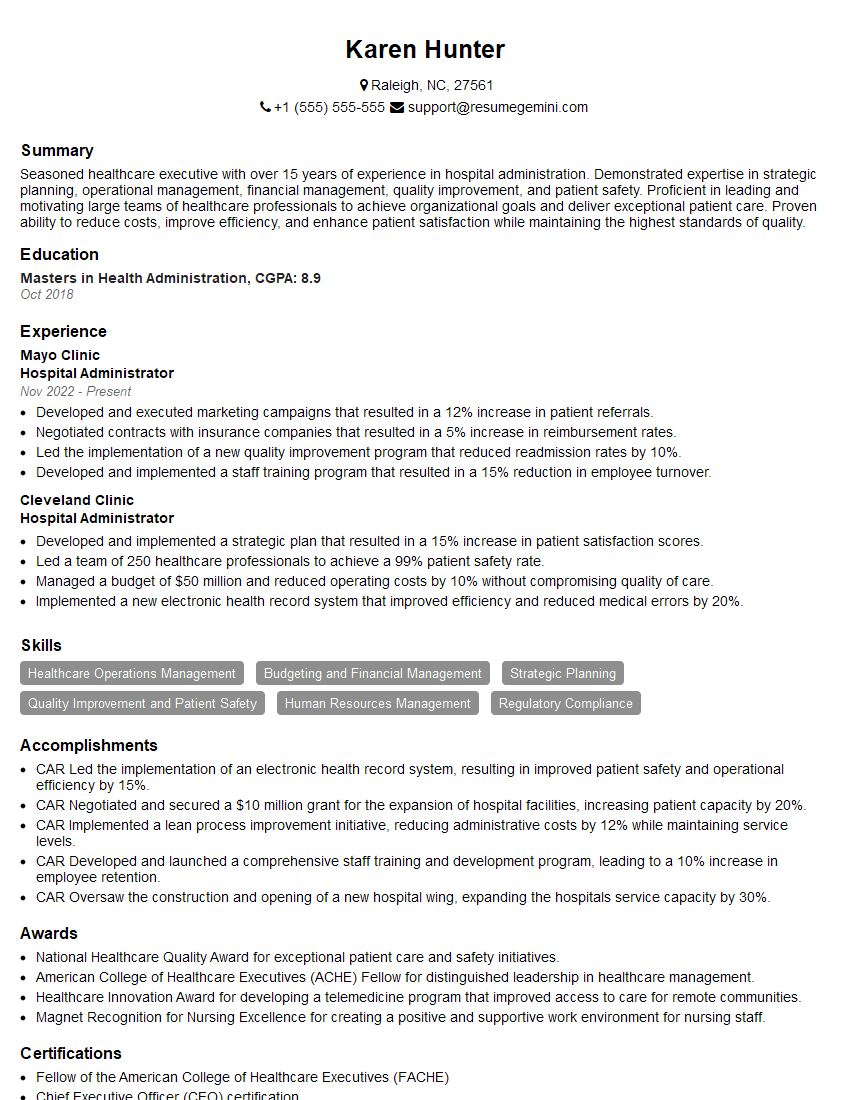
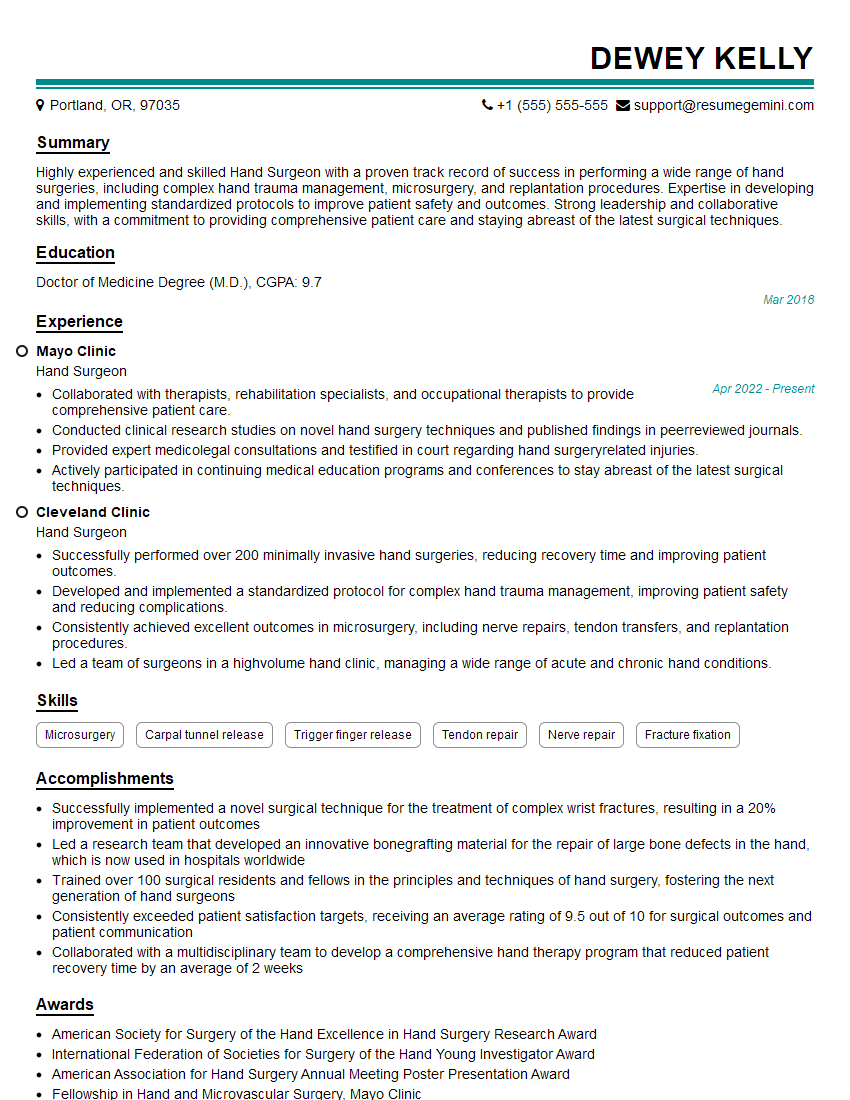
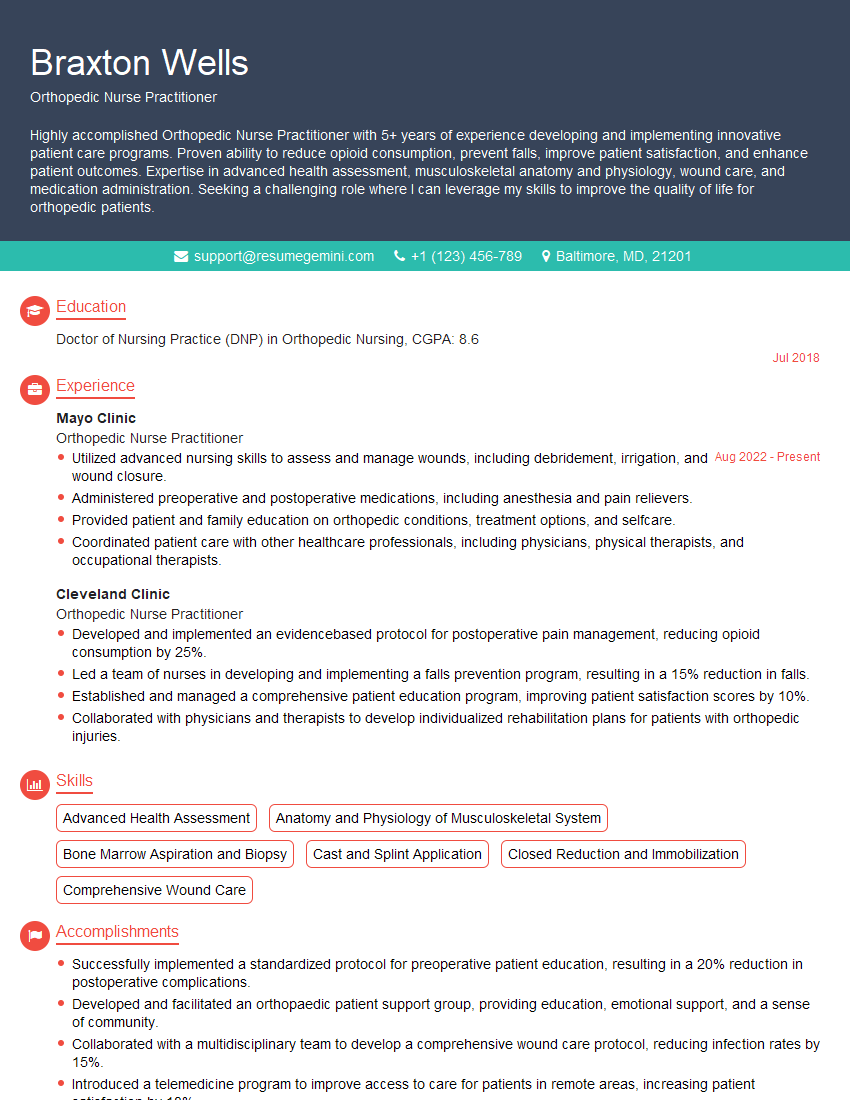
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the biomechanics of pin fixation.
The biomechanics of pin fixation center around the principle of compression and immobilisation. Pins provide stability by transmitting forces across a fracture site, thereby reducing movement and allowing for bone healing. Think of it like scaffolding for a building under construction. The pins act as the scaffolding, holding the fractured bone fragments (the building) in place until the bone heals (the building is finished).
When a force is applied to the bone, the pins distribute that force, preventing movement at the fracture site. This distribution relies on the pin’s material properties (strength, stiffness), its diameter, and its number and placement within the bone. The bone itself also plays a significant role, with stronger, denser bones providing more robust support for the pins.
The success of pin fixation is dependent on several factors: appropriate pin selection, accurate placement, adequate number of pins for the fracture, and the patient’s overall health and healing capacity.
Q 17. What are the factors that influence pin loosening?
Pin loosening is a common complication, often related to the dynamic forces experienced by the bone during healing and normal activity. Several factors contribute to this:
- Bone Resorption: The body’s natural bone remodeling process can lead to resorption (loss) of bone around the pin, creating space and loosening the pin’s hold.
- Infection: Infection at the pin site induces inflammation, leading to bone resorption and weakening the bond between the pin and the bone.
- Cyclic Loading: Repetitive forces acting on the bone during movement can cause gradual loosening.
- Pin Diameter and Material: Inadequate pin diameter or bioincompatible materials can increase the risk of loosening.
- Patient Factors: Osteoporosis (weakened bones), patient compliance, and smoking can all contribute.
Minimizing these factors through careful surgical technique, appropriate implant selection, and diligent post-operative care is vital in preventing pin loosening.
Q 18. Describe your experience with different types of bone screws.
My experience encompasses various bone screws, each with its specific applications and advantages. Common types include cortical screws (for dense cortical bone), cancellous screws (for less dense cancellous bone), and self-tapping screws (requiring less pre-drilling). I’ve also worked with locking screws, which provide more rigid fixation by engaging into a locking mechanism in the screw head, reducing the risk of pullout.
The choice of screw depends on several factors, including the bone quality, the type of fracture, and the desired level of stability. For example, locking screws are beneficial in osteoporotic bone or when dealing with comminuted fractures (fractures with multiple fragments). Cortical screws are generally stronger and more suited to strong, dense bone. Understanding the mechanical properties of each screw type is crucial for successful surgical planning.
Q 19. How do you choose between intramedullary nailing and pin plating?
The choice between intramedullary nailing and pin plating hinges on several key factors, primarily the fracture pattern and bone characteristics. Intramedullary nailing is preferred for long bone fractures, particularly those that are relatively stable and well-aligned. It provides excellent stability by residing within the medullary canal of the bone.
Pin plating is more versatile and often used for complex fractures, comminuted fractures (fractures with multiple bone fragments), or fractures that require precise reduction (alignment) of the fragments. It’s also suitable for metaphyseal and epiphyseal fractures (fractures in the ends of the bone). Pin plating offers more precise control over fracture fragments.
Ultimately, the choice is individualized to the patient’s specific needs and the fracture characteristics. Factors like bone quality, age of the patient, and the surgeon’s experience also play a role in the decision-making process.
Q 20. Describe the process of pin removal.
Pin removal is a relatively straightforward procedure, usually performed under local anesthesia, once the bone has sufficiently healed. This typically occurs several weeks to months post-surgery, depending on the fracture’s location and the patient’s healing progress. Radiographic imaging (X-rays) confirms adequate healing before pin removal.
The process involves making a small incision over the pin, using a specialized instrument to grasp and remove the pin. The incision is then closed, and the area is dressed. The procedure is minimally invasive and usually associated with minimal discomfort. Post-operative care includes keeping the area clean and dry. Occasional pain and minor swelling are expected, usually resolving within a few days.
Q 21. What are the signs and symptoms of pin site infection?
Pin site infection is a serious complication that requires prompt attention. Signs and symptoms can range from mild to severe. Early signs may include redness, swelling, warmth, and tenderness around the pin site. As the infection progresses, purulent (pus-like) drainage from the pin site may occur, along with increasing pain, fever, and malaise (general feeling of discomfort).
More severe signs could indicate a deep infection, potentially involving the bone (osteomyelitis). These could include significant swelling, persistent high fever, and systemic symptoms like chills and fatigue. If any signs of infection are suspected, immediate medical attention is crucial. Treatment typically involves antibiotics and possibly surgical debridement (removal of infected tissue) or pin removal to control the infection.
Q 22. How do you assess the healing progress of a fracture after pin plating?
Assessing fracture healing after pin plating involves a multi-faceted approach combining clinical examination and imaging. We look for signs of clinical union, such as the absence of pain and tenderness at the fracture site, the ability to bear weight (depending on the location and type of fracture), and the return of normal function. This is crucial, as it shows the bone is beginning to heal and bear load.
However, clinical examination alone isn’t enough. We rely heavily on imaging to confirm the healing process. Initially, there might be some widening of the fracture line. Over time, we expect to see progressive bridging of the fracture gap with callus formation, which is visible as increased density on X-rays. Eventually, the fracture line should disappear completely, indicating bony union.
For example, I had a patient with a tibial fracture who initially showed pain on weight-bearing. Over several months, we saw a gradual decrease in pain, an increase in weight-bearing capacity, and radiographic evidence of callus formation and eventual union. This whole process is carefully monitored and documented.
Q 23. What are the common imaging techniques used to monitor pin plating cases?
The primary imaging modalities used to monitor pin plating cases are X-rays and, less frequently, CT scans. X-rays provide a readily available and cost-effective way to visualize the fracture site, assess alignment, and monitor callus formation. We typically take serial X-rays at regular intervals (e.g., every 4-6 weeks) to track progress.
CT scans offer better visualization of the bone and surrounding tissues, which can be helpful in complex cases or when there’s suspicion of complications like non-union or infection. However, due to the increased radiation exposure and cost, they’re typically reserved for specific situations. In essence, X-rays are our workhorse and CT scans are the specialized tool.
Q 24. What are your strategies for preventing complications during pin plating?
Preventing complications during and after pin plating requires a meticulous approach, starting with meticulous surgical technique. This includes precise reduction of the fracture (aligning the broken bone fragments), secure fixation with appropriately sized pins and plates, and meticulous soft tissue handling to minimize damage and promote healing.
Beyond the surgery itself, careful post-operative management is crucial. This includes:
- Infection prophylaxis: Administering prophylactic antibiotics to reduce the risk of infection.
- Pain management: Implementing an effective pain management strategy to promote patient comfort and mobility.
- Early mobilization: Encouraging early mobilization and range of motion exercises (as guided by the specific fracture and patient condition) to prevent stiffness and promote healing.
- Weight-bearing restrictions: Implementing appropriate weight-bearing restrictions to protect the healing fracture, which is often specific to the fracture location and type.
- Wound care: Maintaining meticulous wound care to prevent infection.
For instance, I always ensure proper surgical asepsis during pin plating, and closely monitor patients for signs of infection, ensuring prompt intervention if needed. This proactive strategy significantly reduces the risk of complications.
Q 25. How do you manage pain in patients after pin plating surgery?
Pain management after pin plating is a crucial aspect of patient care. We utilize a multimodal approach combining pharmacologic and non-pharmacologic methods. Initially, we often use intravenous opioids for acute pain relief. Once the patient’s condition stabilizes, we transition to oral analgesics, like NSAIDs or weaker opioids, titrated according to the patient’s response.
Non-pharmacologic methods are also important. These can include ice packs to reduce swelling, elevation of the limb to reduce edema, and physical therapy to improve mobility and reduce pain. We often involve pain management specialists to develop an individualized plan, ensuring the patient achieves adequate pain relief while minimizing potential side effects. For example, some patients respond well to nerve blocks which provide more targeted and longer lasting pain relief.
Q 26. Explain your experience with different types of bone.
My experience encompasses working with various bone types, each presenting unique challenges in pin plating. Cortical bone, the dense outer layer of most bones, is strong and requires more force for pin insertion. Cancellous bone, the spongy inner layer, is less dense and requires a different approach. The density and quality of the bone directly influence pin selection and placement.
For instance, osteoporotic bone, which is characteristically weak and brittle, requires more careful consideration and potentially different fixation techniques to avoid complications like pin loosening or pullout. Similarly, pediatric bone, still growing and more pliable, requires specialized plates and pins to accommodate growth and avoid growth plate damage. This knowledge directly informs my surgical decisions, such as pin diameter and placement.
Q 27. How do you determine the appropriate length of pins?
Determining the appropriate length of pins is critical to ensure secure fixation. It’s not a standardized measurement; instead, it’s based on several factors. First, we assess the length of the fracture and the surrounding bone. We need sufficient pin length to penetrate adequate bone beyond the fracture to provide stable fixation. The quality of the bone itself also matters. In osteoporotic bone, longer pins may be needed for better purchase.
Secondly, we consider the diameter of the pins. Thicker pins provide more strength but increase the risk of complications. The pin’s length is always balanced against its diameter and the bone’s characteristics. Finally, the type of plate used influences pin length as it has pre-drilled holes that dictate placement. Improper pin length can lead to loosening, pull-out, or even failure of fixation.
Pre-operative planning, including image analysis (X-rays, CT), is vital for accurate pin length determination. Intra-operative assessment further refines this determination. For example, sometimes we need to adjust based on the bone’s actual density and the effectiveness of the pin purchase.
Q 28. What are your experiences with revision pin plating surgery?
Revision pin plating surgery is unfortunately sometimes necessary. The most common reasons include pin loosening, infection, or failure of initial fixation. Pin loosening might result from inadequate initial bone purchase or bone resorption around the pin. Infection can necessitate pin removal, debridement (surgical removal of infected tissue), and sometimes replacement of the plating system.
Revision surgery is technically more challenging than initial surgery due to scar tissue and potential changes in bone density. The goal is to achieve stable fixation, address the underlying cause of the failure, and restore bone integrity. The challenges might include bone loss from the prior surgery, which needs to be addressed with bone grafts or other techniques. Careful preoperative planning and intra-operative assessment are crucial to successfully resolve the problem and improve the patient’s outcome.
Each case is carefully evaluated, and we consider various options including removing pins, replacing pins, using a different plate or technique, or even performing a different type of fixation altogether based on the individual situation. The long-term outcome of revision surgeries relies heavily on meticulous surgical technique and careful post-operative management.
Key Topics to Learn for Pin Plating Interview
- Anatomy and Biomechanics of Fractures: Understanding fracture types relevant to pin plating, bone healing processes, and the biomechanical principles influencing implant selection and placement.
- Pin Plating Techniques: Mastering various pin plating techniques, including different implant types (e.g., Kirschner wires, Steinmann pins), insertion methods, and considerations for bone density and fracture morphology.
- Surgical Planning and Instrumentation: Familiarize yourself with pre-operative planning (e.g., imaging interpretation, surgical approach selection), intra-operative techniques (e.g., drilling, pin placement, fixation), and the use of specialized surgical instruments.
- Implant Selection and Stabilization: Learn about the factors influencing implant selection (e.g., fracture pattern, bone quality, patient factors), achieving stable fixation, and minimizing complications.
- Post-Operative Care and Complications: Understand post-operative management (e.g., pain management, immobilization, rehabilitation), potential complications (e.g., infection, malunion, non-union), and their prevention and treatment.
- Troubleshooting and Problem-Solving: Develop your ability to identify and address intraoperative challenges, such as unexpected bone fragility or difficult fracture patterns. Consider how you would approach unexpected situations and adapt your techniques accordingly.
- Material Science of Implants: Gain a foundational understanding of the materials used in pin plating and their properties (e.g., biocompatibility, strength, stiffness).
Next Steps
Mastering Pin Plating techniques significantly enhances your career prospects in orthopedics and related fields. A strong understanding of these procedures demonstrates valuable surgical skills and problem-solving abilities highly sought after by employers. To maximize your job search success, create an ATS-friendly resume that effectively highlights your expertise. ResumeGemini is a trusted resource for building professional and impactful resumes. We provide examples of resumes tailored to Pin Plating to help you showcase your skills and experience effectively. Take the next step towards your dream career; start building your resume with ResumeGemini today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good