Preparation is the key to success in any interview. In this post, we’ll explore crucial Disinfection Techniques interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Disinfection Techniques Interview
Q 1. Explain the difference between sterilization, disinfection, and sanitation.
Sterilization, disinfection, and sanitation are all crucial processes aimed at reducing microbial contamination, but they differ significantly in their level of microbial reduction.
Sterilization is the complete elimination or destruction of all forms of microbial life, including bacteria, viruses, fungi, and spores. Think of it like completely wiping a hard drive – nothing is left behind. This is essential in situations where absolute sterility is required, such as in surgical instruments or injectable medications.
Disinfection reduces the number of viable microbes on a surface or in a substance to a safe level, but it doesn’t necessarily eliminate all microorganisms. It’s like decluttering a room; you’ve removed a lot, but not everything. Disinfection targets vegetative bacteria, viruses, and fungi, but often doesn’t kill resistant spores. Disinfecting a countertop after preparing food is a good example.
Sanitation is a process that reduces the microbial load to a level considered safe by public health standards. It’s a lower level of microbial reduction than disinfection. Think of it as light cleaning—reducing the overall microbial load to an acceptable level, but not necessarily killing all harmful microbes. Washing dishes in soapy water is an example of sanitation.
Q 2. What are the different methods of sterilization?
Sterilization can be achieved through various methods, each with its own advantages and disadvantages:
Heat Sterilization: This is a widely used and highly effective method. It includes:
Autoclaving (Moist Heat): Uses pressurized steam to achieve high temperatures, effectively killing all microorganisms including spores. It’s the gold standard for sterilizing many medical instruments and lab equipment.
Dry Heat Sterilization: Uses high temperatures in the absence of moisture. It’s slower than autoclaving but suitable for materials that can’t withstand steam.
Radiation Sterilization: Uses ionizing (gamma or X-rays) or non-ionizing (UV) radiation to kill microorganisms. Ionizing radiation is effective against all types of microbes, including spores. It’s often used for sterilizing single-use medical products.
Chemical Sterilization: Employs chemicals such as ethylene oxide gas or glutaraldehyde to kill microorganisms. Ethylene oxide is effective but is a toxic gas and requires special handling. Glutaraldehyde is used for sterilizing heat-sensitive medical instruments.
Filtration Sterilization: Uses membrane filters with pore sizes small enough to remove bacteria and other microorganisms. This method is suitable for sterilizing heat-sensitive liquids such as some medications.
Q 3. Describe the principles of effective disinfection.
Effective disinfection hinges on several key principles:
Contact Time: The disinfectant must remain in contact with the surface for a sufficient length of time to effectively kill or inactivate microorganisms. This time varies depending on the disinfectant and the type of microorganism.
Concentration: The correct concentration of the disinfectant is critical. Too low a concentration may be ineffective, while too high a concentration may be hazardous.
Temperature: Temperature influences the efficacy of many disinfectants. Higher temperatures often enhance their activity.
pH: The pH of the surface being disinfected and the disinfectant itself can influence effectiveness. Some disinfectants work best at a specific pH range.
Bioburden: The initial level of microbial contamination (bioburden) will influence the time and concentration needed for effective disinfection. A higher bioburden requires more stringent treatment.
Surface Material: The surface material can affect the disinfectant’s action. Porous surfaces may require more prolonged treatment.
Organic Matter: The presence of organic matter (blood, feces, etc.) can interfere with the action of many disinfectants. It’s crucial to clean surfaces thoroughly before disinfection.
Q 4. What factors influence the choice of a disinfectant?
Several factors influence the choice of disinfectant:
Target Microorganisms: The type and level of microbial contamination dictate the choice of disinfectant. Some disinfectants are more effective against certain types of microorganisms than others.
Surface Material: Certain disinfectants may damage specific materials. Compatibility with the surface being disinfected is crucial.
Toxicity: The safety of the disinfectant for humans, animals, and the environment must be considered. Less toxic options are preferred whenever possible.
Cost: The cost of the disinfectant and its application must be taken into account.
Ease of Use: The ease of application and disposal of the disinfectant should also be a factor in decision-making.
Environmental Considerations: The environmental impact of the disinfectant should be considered, particularly its potential to cause pollution.
Q 5. How do you assess the efficacy of a disinfection process?
Assessing the efficacy of a disinfection process often involves a combination of methods:
Challenge Testing: This involves inoculating a surface with a known number of microorganisms, applying the disinfectant, and then counting the surviving microorganisms after a specified contact time. This provides quantitative data on the disinfectant’s effectiveness.
Surveillance Cultures: Regularly sampling surfaces after disinfection to monitor microbial levels helps ensure the process remains effective. This can include swabbing surfaces and culturing the samples.
ATP Bioluminescence Testing: This rapid method measures adenosine triphosphate (ATP), a molecule found in all living cells. Lower ATP levels indicate reduced microbial contamination. This provides quick feedback but doesn’t specify the type of microorganisms.
Proper documentation of the disinfection process, including the disinfectant used, concentration, contact time, and results of efficacy testing, is vital for quality control and regulatory compliance.
Q 6. Explain the concept of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC).
Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) are crucial measures in evaluating the effectiveness of antimicrobial agents.
MIC: The MIC is the lowest concentration of an antimicrobial substance that prevents visible growth of a microorganism in vitro. It assesses the inhibitory effect of an agent. Imagine it as the minimum amount of medicine needed to stop the bacteria from multiplying.
MBC: The MBC is the lowest concentration of an antimicrobial substance that kills 99.9% of a bacterial population in vitro. It measures the bactericidal effect, assessing killing capability. This is the minimum amount needed to actually kill off the bacteria.
Determining MIC and MBC values is important for selecting appropriate antimicrobial agents and dosages in clinical settings and in industrial applications. For example, a higher MBC compared to MIC suggests that the agent may primarily inhibit growth without killing a significant portion of bacteria. This information is critical for treatment strategies.
Q 7. Describe the mechanism of action of chlorine-based disinfectants.
Chlorine-based disinfectants, such as hypochlorite (bleach), exert their antimicrobial action primarily through the formation of hypochlorous acid (HOCl).
When chlorine is dissolved in water, it forms hypochlorous acid (HOCl) and hypochlorite ions (OCl–). The equilibrium between these two species is pH-dependent: HOCl predominates at lower pH values (acidic), while OCl– is more prevalent at higher pH values (alkaline). HOCl is generally considered the more potent antimicrobial agent.
The mechanism involves the disruption of microbial cell structures and processes:
Oxidation: HOCl is a strong oxidizing agent. It oxidizes essential cellular components, such as proteins, lipids, and DNA, leading to cell death.
Protein Modification: HOCl reacts with amino acid residues in proteins, altering their structure and function, rendering them inactive.
DNA Damage: HOCl can damage microbial DNA, interfering with replication and cell survival.
It’s crucial to remember that the effectiveness of chlorine-based disinfectants is affected by factors such as pH, organic matter, and contact time, as discussed earlier. The presence of organic matter consumes chlorine, reducing its available concentration and its efficacy.
Q 8. What are the advantages and disadvantages of using alcohol-based disinfectants?
Alcohol-based disinfectants, primarily ethanol and isopropanol, are widely used due to their rapid action and broad-spectrum efficacy against many bacteria and viruses. However, their effectiveness is influenced by factors like concentration, contact time, and the presence of organic matter.
- Advantages: Rapid action, broad-spectrum activity against many microorganisms, relatively low toxicity compared to other disinfectants, ease of use, and readily available.
- Disadvantages: Flammability (especially ethanol), potential for skin irritation or dryness with frequent use, reduced effectiveness in the presence of organic matter (blood, feces), and ineffectiveness against certain resistant microorganisms like bacterial spores.
For example, a 70% isopropyl alcohol solution is more effective than a 90% solution because the water in the 70% solution helps the alcohol penetrate the microorganism’s cell wall more effectively. However, using too low a concentration may be ineffective.
Q 9. How do you handle a spill of a hazardous chemical?
Handling a hazardous chemical spill requires a prompt and controlled response to minimize risks. The first step is always to ensure your own safety. Never attempt to clean up a spill without appropriate PPE.
- Isolate the area: Prevent further spread by cordoning off the spill area and restricting access. This could involve closing doors, setting up barriers, and warning others.
- Assess the situation: Identify the chemical spilled, refer to its Safety Data Sheet (SDS) for handling instructions and appropriate cleanup procedures. The SDS contains crucial information regarding the hazards of the chemical and the recommended response measures.
- Don appropriate PPE: This typically includes gloves, eye protection, a respirator (if necessary, depending on the chemical), and potentially a full body suit depending on the severity and chemical’s hazards.
- Contain the spill: Use absorbent materials like spill pads or kitty litter to soak up the liquid. Avoid spreading the spill further. Carefully collect the contaminated materials in appropriate containers for disposal, according to local regulations.
- Clean and disinfect the area: After the spill is contained, thoroughly clean the affected area using a suitable disinfectant, again referring to the SDS for recommendations. Proper ventilation is crucial during the entire process.
- Dispose of waste properly: All contaminated materials must be disposed of according to local regulations and waste management guidelines.
For instance, if a spill of bleach occurs, one must use gloves and eye protection, and properly ventilate the room before starting the clean up. The SDS will provide specific guidance on the appropriate neutralizing agent and cleanup procedures for the particular bleach concentration.
Q 10. What are the safety precautions to take when handling disinfectants?
Safety is paramount when handling disinfectants. These chemicals are designed to kill microorganisms, but they can also pose risks to human health if not handled properly.
- Always read and follow the label instructions: This is the single most important safety precaution. The label provides vital information on usage, dilution rates, precautions, and first aid measures.
- Wear appropriate PPE: This is crucial to protect skin, eyes, and respiratory system from exposure. The type of PPE will depend on the disinfectant being used.
- Work in a well-ventilated area: Many disinfectants release fumes that can be irritating or harmful. Good ventilation helps to minimize exposure to these fumes.
- Avoid skin contact: Disinfectants can cause skin irritation, dryness, or allergic reactions. Wash hands thoroughly after each use.
- Avoid ingestion: Keep disinfectants out of reach of children and pets. Never ingest them.
- Proper storage: Store disinfectants in their original containers, in a cool, dry place, away from incompatible substances.
- Emergency preparedness: Know the location of safety data sheets (SDS) for all chemicals and have a spill response plan in place.
For example, never mix different disinfectants together unless explicitly stated as safe on the product label. Mixing incompatible disinfectants can create dangerous reactions.
Q 11. Explain the importance of proper personal protective equipment (PPE) when working with disinfectants.
Personal Protective Equipment (PPE) is non-negotiable when working with disinfectants. It’s the primary barrier between you and potentially harmful chemicals. Failure to use appropriate PPE can result in a range of health problems, from skin irritation to severe chemical burns or respiratory issues.
Think of PPE as your armor. Just as a knight wouldn’t go into battle without his armor, you shouldn’t handle disinfectants without the proper protection. PPE minimizes exposure risks, ensuring your safety and well-being during disinfection processes. Proper PPE use prevents accidental contact with skin, eyes, or mucous membranes which can lead to serious health consequences. The right PPE reduces the risk of long term health problems, allowing you to continue performing this important work safely.
Q 12. What are the different types of PPE used in disinfection procedures?
The specific PPE needed depends on the disinfectant and the task. Common PPE items include:
- Gloves: Nitrile or other chemical-resistant gloves are essential to protect hands from direct contact.
- Eye protection: Safety glasses or goggles prevent splashes from entering the eyes.
- Respiratory protection: A mask or respirator might be necessary when working with disinfectants that release harmful fumes, especially in poorly ventilated areas.
- Aprons or gowns: These protect clothing and skin from splashes or spills.
- Boot covers: These prevent contamination of shoes and protect feet from spills.
For instance, when disinfecting a large area with a spray disinfectant that produces aerosols, you might wear a respirator in addition to gloves, goggles, and an apron to fully protect yourself from exposure.
Q 13. How do you monitor and control the effectiveness of your disinfection program?
Monitoring and controlling the effectiveness of a disinfection program is crucial to ensure its success. It involves a multi-pronged approach:
- Environmental monitoring: Regularly collect samples from high-touch surfaces and test them for microbial contamination using appropriate microbiological methods. This provides evidence of the program’s success in reducing microbial counts.
- Efficacy testing of disinfectants: Periodically test the disinfectants used to ensure they maintain their efficacy. Factors such as concentration, contact time, and presence of organic matter can affect disinfection performance.
- Staff training and competency assessment: Regularly train staff on proper disinfection techniques and assess their competency through observations and practical evaluations. Effective disinfection relies on correct procedures.
- Record keeping: Meticulously document all disinfection activities, including dates, times, areas disinfected, disinfectants used, and results of monitoring activities. This documentation is crucial for program evaluation and audits.
- Regular review and updates: Regularly review the effectiveness of the program and make adjustments as needed. The program should be adapted to address emerging pathogens or identified deficiencies.
For example, if environmental monitoring reveals a persistent high level of a specific bacteria on a particular surface, the disinfection protocol for that area might need adjustment, possibly involving a change in disinfectant, contact time, or frequency of cleaning.
Q 14. What are the regulatory requirements for disinfection in your industry?
Regulatory requirements for disinfection vary significantly depending on the industry and geographic location. However, common themes include adherence to relevant standards, proper labeling and handling of chemicals, appropriate record-keeping, and compliance with environmental regulations regarding waste disposal. For healthcare settings, regulatory bodies like the Centers for Disease Control and Prevention (CDC) provide detailed guidelines. Food processing facilities face stringent regulations from agencies like the Food and Drug Administration (FDA). In other sectors, local or national health and safety regulations will dictate specific requirements. Consulting relevant standards and regulatory documents appropriate to your specific industry and locale is essential for compliance.
It is crucial to stay abreast of changes in regulations and adapt disinfection procedures accordingly. Failure to comply with regulations can result in penalties, fines, and even legal action.
Q 15. Describe your experience with different types of disinfection equipment.
My experience encompasses a wide range of disinfection equipment, from traditional methods to cutting-edge technologies. I’ve extensively worked with:
- Autoclaves: These steam sterilizers are crucial for high-heat sterilization of surgical instruments and other heat-resistant materials. I’m proficient in operating various models, including those with pre-programmed cycles and advanced monitoring systems.
- Ultraviolet (UV) disinfection systems: UV-C light is highly effective against a broad spectrum of microorganisms. I have experience using both high-intensity UV lamps for room disinfection and lower-intensity systems for surface disinfection in controlled environments, like cleanrooms.
- Chemical disinfection systems: I’m familiar with various automated chemical disinfection systems that utilize solutions like chlorine dioxide or hydrogen peroxide for large-scale applications. I understand the importance of proper chemical handling, concentration control, and safety protocols.
- High-pressure washers and sprayers: These are employed for initial cleaning and disinfection of large areas, especially in industrial settings. Proper technique and understanding of surface contact time are critical for effectiveness.
Furthermore, I possess knowledge of the maintenance, calibration, and troubleshooting procedures for all the mentioned equipment, ensuring optimal performance and safety.
Career Expert Tips:
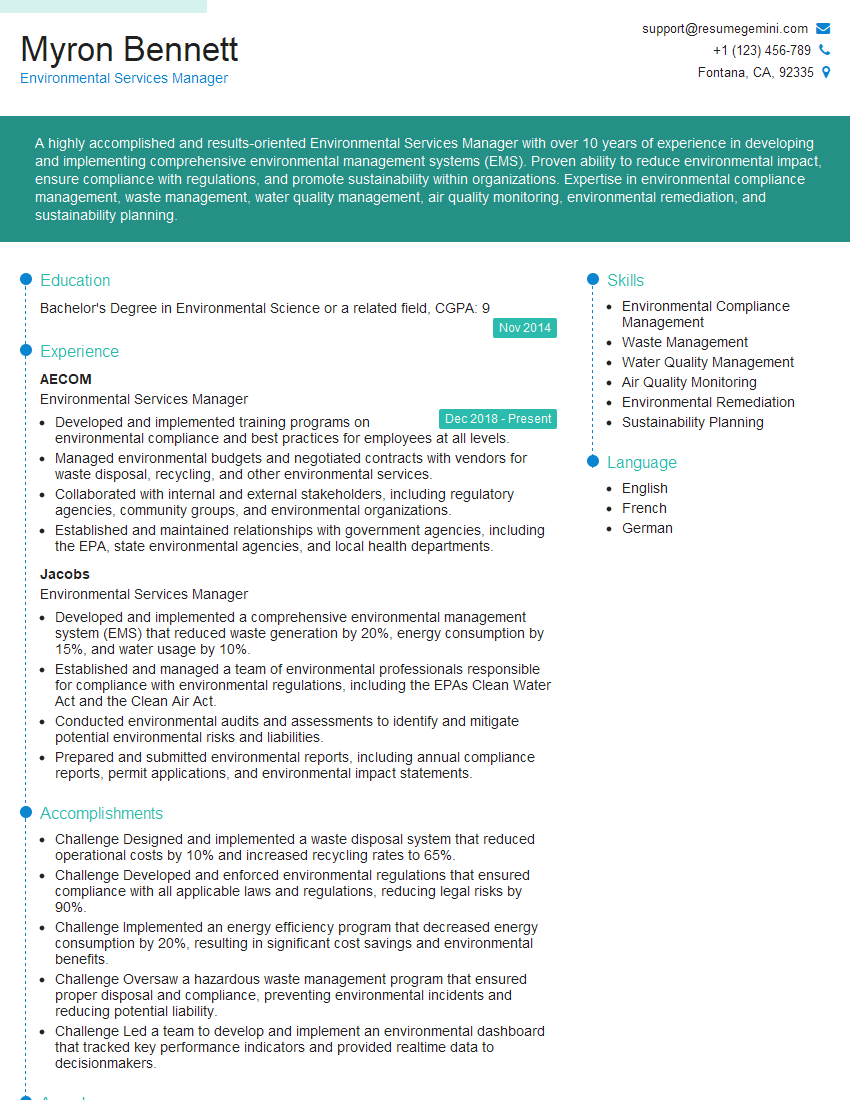
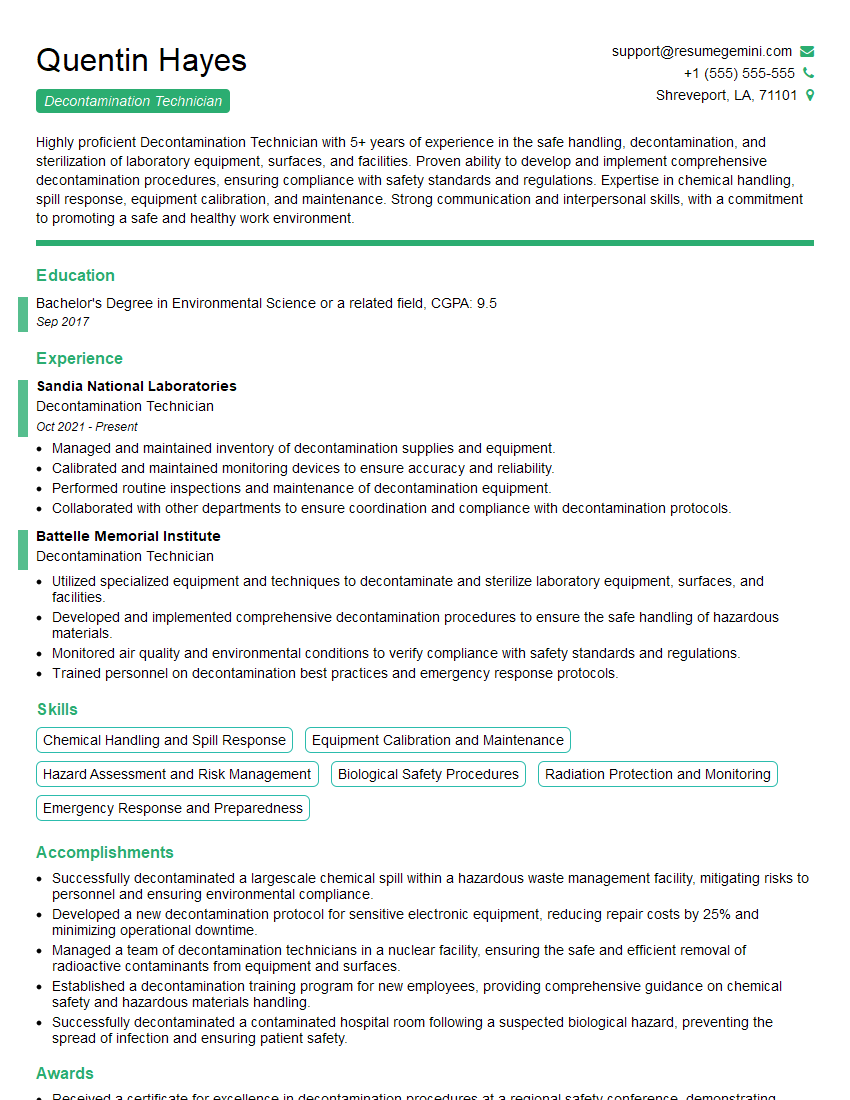
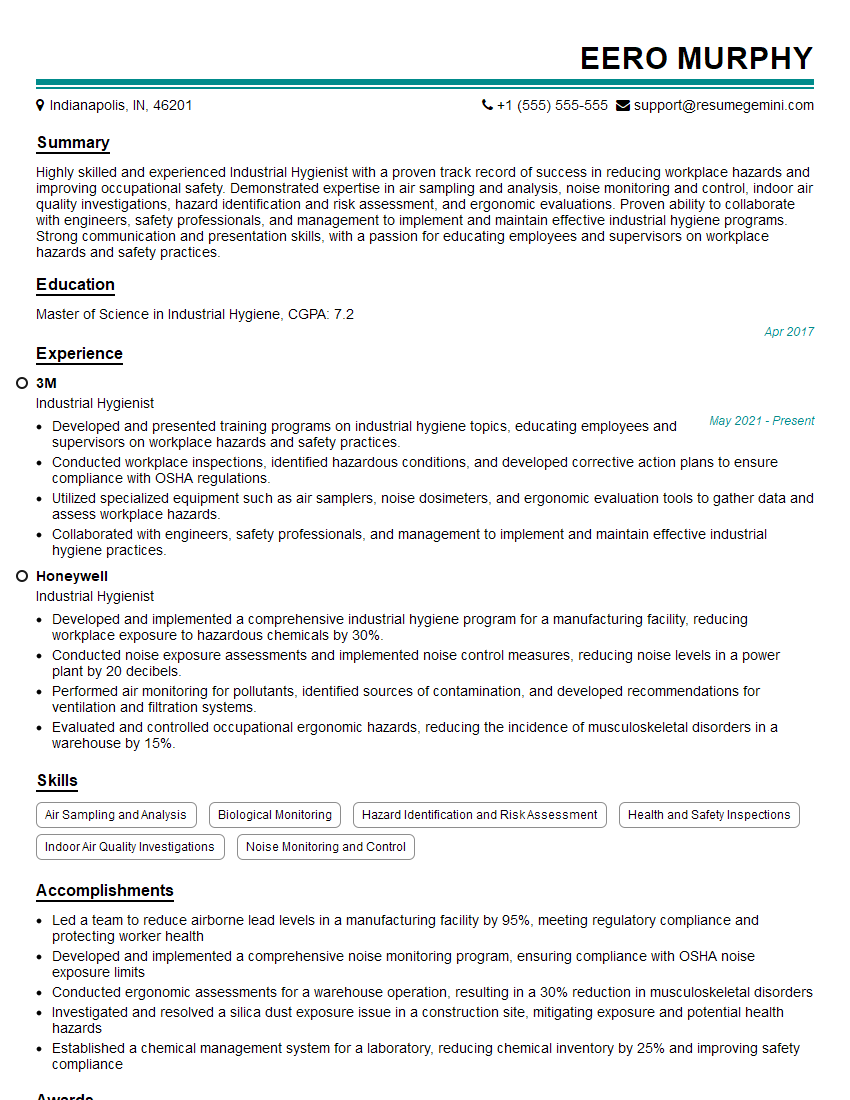
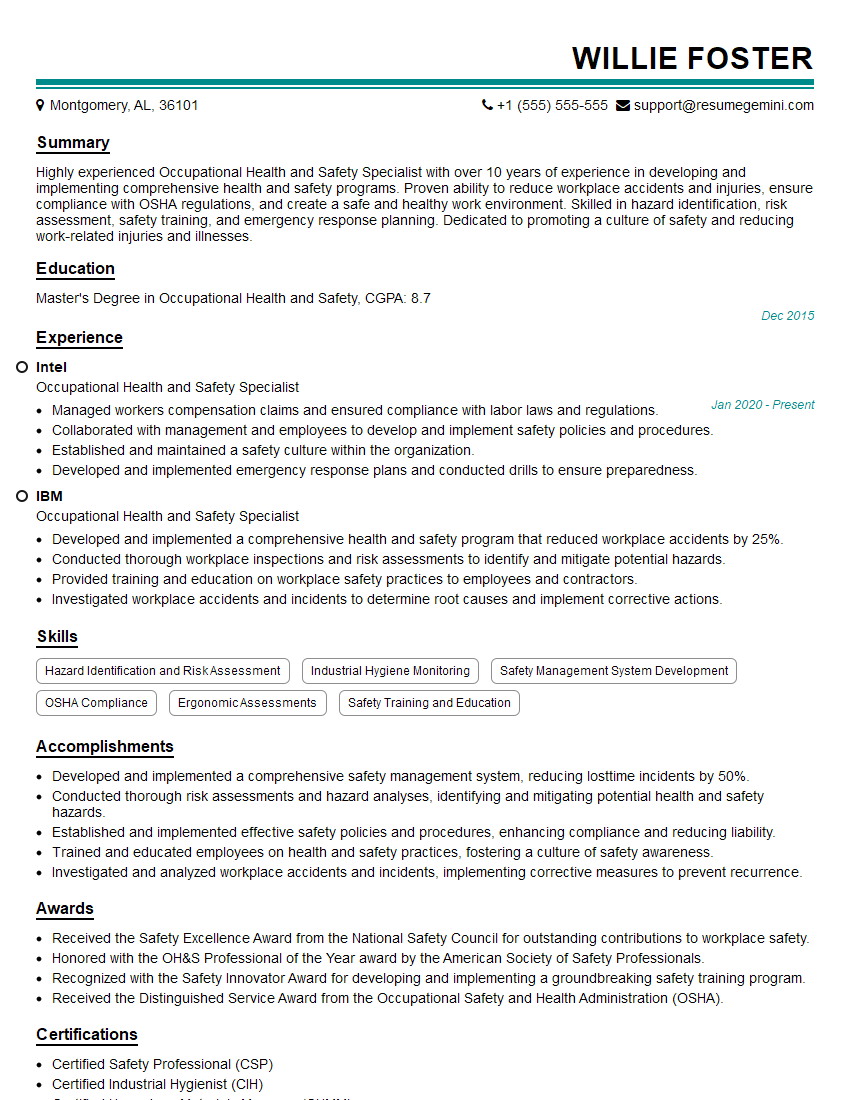
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you validate the sterilization process?
Validating sterilization involves proving that the process consistently eliminates all viable microorganisms. This is typically achieved through a combination of methods:
- Biological Indicators (BIs): These are spore-containing strips placed within the sterilization load. After the cycle, the strips are cultured to verify the spores’ inactivation, confirming the effectiveness of the process. A negative result indicates successful sterilization.
- Physical Indicators (PIs): These are external and internal indicators that provide visual confirmation that the sterilization parameters (e.g., temperature, time, pressure) have been met. They don’t guarantee sterility but provide valuable process monitoring.
- Chemical Indicators (CIs): CIs change color when exposed to specific sterilization parameters, offering an additional check on process validity. They are often integrated into packaging.
Regular validation testing, including both routine and periodic sterility tests, is vital to maintain confidence in the sterilization process. Any deviation requires thorough investigation and corrective actions.
Q 17. What are some common indicators of improper disinfection?
Indicators of improper disinfection can be subtle or obvious, depending on the situation. Some common signs include:
- Persistent unpleasant odors: This can suggest incomplete removal of organic matter or inadequate disinfection.
- Visible microbial growth: This is a clear sign of disinfection failure and should trigger immediate corrective action. Mold, mildew, and bacterial colonies are easily observable.
- Increased infection rates: A rise in infections among patients or staff in a healthcare setting, or a higher incidence of contamination in an industrial setting, indicates a potential problem with disinfection protocols.
- Positive culture results: Environmental swabs taken from surfaces after disinfection should yield negative or low microbial counts. High counts reveal inadequate disinfection.
- Damaged or malfunctioning equipment: Faulty autoclaves, UV lamps, or chemical dispensers will compromise disinfection effectiveness.
It’s crucial to regularly monitor for these indicators and implement robust monitoring programs to proactively identify and address issues.
Q 18. How do you address a situation where disinfection procedures have failed?
When disinfection procedures fail, a structured approach is necessary. The steps typically involve:
- Immediate Containment: Isolate the affected area to prevent further spread of contamination.
- Thorough Investigation: Identify the root cause of the failure. This might involve reviewing disinfection protocols, equipment functionality, environmental factors, or personnel training.
- Remediation: Implement thorough cleaning and re-disinfection of the affected area, utilizing appropriate methods and validated protocols. This may involve increased concentration of disinfectants or longer contact times.
- Corrective Actions: Address the root cause of the failure. This could involve equipment repair or replacement, staff retraining, modification of protocols, or improved cleaning practices.
- Documentation: Meticulously document all steps of the process, including the cause of the failure, corrective actions, and verification of successful remediation.
A post-incident review is crucial to prevent recurrence. This involves a multidisciplinary team analyzing the event and implementing preventative measures.
Q 19. Describe your experience with different types of microbial contaminants.
My experience encompasses a wide range of microbial contaminants, including:
- Bacteria: Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa are examples of common bacterial contaminants that require different disinfection strategies.
- Viruses: Norovirus, influenza viruses, and coronaviruses present unique challenges due to their resilience to some disinfectants.
- Fungi: Candida albicans and Aspergillus species are common fungal contaminants found in various environments. Their elimination requires specialized fungicides.
- Spores: Bacterial endospores (like those of Bacillus and Clostridium species) are highly resistant to many disinfectants, requiring rigorous sterilization methods.
Understanding the specific type of contaminant is critical for selecting the appropriate disinfection method. For example, a virus might require a different approach than a bacterial spore.
Q 20. What are some emerging disinfection technologies?
Several emerging disinfection technologies offer promising solutions for various applications:
- Pulsed Light (PL): PL systems use short bursts of intense light to inactivate microorganisms. This technology is advantageous for its rapid action and minimal environmental impact.
- Plasma Technology: Plasma-based systems generate reactive oxygen and nitrogen species that can effectively eliminate microorganisms. These are particularly useful for delicate surfaces.
- Electrochemical disinfection: This method utilizes electrodes to generate disinfecting agents, offering on-site generation of disinfectants and reducing storage and handling risks.
- Nanotechnology-based disinfectants: Nanoparticles of silver or copper, for example, exhibit antimicrobial properties and are being investigated for their potential in various applications.
These technologies are continuously being refined and optimized for broader applications, promising increased effectiveness and reduced environmental burden compared to traditional methods.
Q 21. How do you select the appropriate disinfectant for a specific application?
Selecting the appropriate disinfectant involves considering several crucial factors:
- Type of Microorganism: The chosen disinfectant should be effective against the target microorganisms (bacteria, viruses, fungi, spores).
- Surface Material: Some disinfectants can damage specific materials (e.g., wood, plastics). Compatibility is paramount.
- Environmental Conditions: Temperature, humidity, and pH can influence a disinfectant’s efficacy.
- Toxicity: Safety for humans and the environment is crucial. The disinfectant’s toxicity profile and potential health effects must be considered.
- Contact Time: The disinfectant must remain in contact with the surface for the recommended time to achieve adequate disinfection.
- Cost-effectiveness: Balancing efficacy with cost is vital. More expensive options are not always necessary.
For instance, choosing a broad-spectrum disinfectant suitable for use on stainless steel surfaces in a food processing facility requires careful consideration of all these factors. A risk assessment often forms the basis for this selection process.
Q 22. Explain the importance of surface contact time in disinfection.
Surface contact time is crucial in disinfection because it dictates how long a disinfectant needs to remain in contact with a surface to effectively kill or inactivate microorganisms. Think of it like this: you wouldn’t expect a single drop of bleach to instantly sterilize a heavily contaminated countertop. The disinfectant needs sufficient time to penetrate the microbial cell walls and disrupt their essential functions. A shorter contact time might only reduce the microbial load, while a longer contact time, as specified by the disinfectant’s label, is necessary for complete disinfection.
The required contact time varies significantly depending on several factors: the specific disinfectant used (some are faster-acting than others), the type and concentration of microorganisms present (e.g., bacterial spores are notoriously resistant), the surface material (porous surfaces require longer contact times), the presence of organic matter (blood, bodily fluids, etc., can interfere with disinfection), and the temperature and humidity of the environment. For example, a high-level disinfectant might require a contact time of 10 minutes, while a low-level disinfectant may only need 5 minutes, but these are just examples; you must always refer to the manufacturer’s instructions.
Insufficient contact time can lead to incomplete disinfection, resulting in persistent microbial contamination and potential health risks. Always follow the manufacturer’s instructions precisely regarding the contact time to ensure effective disinfection.
Q 23. What are the limitations of using disinfectants?
While disinfectants are invaluable tools in infection control, they do have limitations. One major limitation is their specificity; a disinfectant effective against one type of microorganism might be ineffective against others. For instance, a disinfectant that readily kills Gram-positive bacteria might be less effective against Gram-negative bacteria or viruses. Another significant limitation is the influence of environmental factors. The presence of organic matter like blood or feces can significantly reduce a disinfectant’s efficacy, creating a protective barrier around microorganisms.
Furthermore, material compatibility is a key concern. Some disinfectants can damage or corrode certain materials, limiting their use in specific environments. For example, strong acids or chlorine-based disinfectants can damage certain plastics and metals. Residue issues can also occur. Some disinfectants leave behind residues that might interfere with subsequent procedures or pose a health risk if not properly cleaned. Lastly, disinfectant resistance is an increasing concern. Overuse and improper application of disinfectants can lead to the development of resistant strains of microorganisms, rendering those disinfectants useless.
Q 24. How do you ensure the compatibility of disinfectants with different materials?
Ensuring compatibility between disinfectants and different materials is paramount to prevent damage and ensure effective disinfection. This involves a multi-step approach:
- Consult the disinfectant label and Safety Data Sheet (SDS): The label and SDS provide crucial information about the disinfectant’s compatibility with various materials. Always check for specific recommendations and warnings before applying it to any surface.
- Perform small-scale testing: Before widespread application, test the disinfectant on an inconspicuous area of the material to assess its impact. This helps to identify any potential discoloration, damage, or reactions.
- Consider material properties: Porous materials (like wood or fabric) can absorb disinfectants, making them less effective and potentially causing damage. Non-porous materials (like stainless steel or glass) generally tolerate disinfectants better. Understand the material’s composition and properties to predict its compatibility.
- Use appropriate disinfectant: Select a disinfectant known for its compatibility with the materials in your setting. For instance, alcohol-based disinfectants are generally compatible with a wide range of materials, while chlorine-based disinfectants require careful consideration.
- Proper dilution and application: Using the correct dilution as per manufacturer’s instructions is crucial. Too concentrated a solution can damage materials; too dilute a solution might not disinfect effectively. The method of application (spraying, wiping, immersion) should also be appropriate for the material.
In my experience, careful attention to these steps is essential to prevent costly damage and ensure the efficacy of your disinfection program.
Q 25. Describe your experience with implementing and maintaining a disinfection program.
In my previous role at a large hospital, I was responsible for designing, implementing, and maintaining a comprehensive hospital-wide disinfection program. This involved developing detailed Standard Operating Procedures (SOPs) for various areas, including operating rooms, patient rooms, and common areas. The program incorporated a combination of high-level and low-level disinfectants, selected based on their efficacy against prevalent pathogens and compatibility with different surfaces. We employed a rigorous cleaning schedule, monitored disinfectant usage, and tracked any adverse events or equipment damage. Regular training and competency assessments for staff ensured consistent and effective implementation.
One of the biggest challenges was maintaining consistent adherence to protocols. To overcome this, we implemented a system of regular audits and feedback, along with ongoing training sessions to reinforce correct techniques. We also incorporated visual aids, checklists, and color-coded systems to simplify procedures and ensure compliance. The success of the program was measurable through reduced healthcare-associated infections (HAIs) and improved patient safety.
Q 26. How do you train personnel on proper disinfection techniques?
Training personnel on proper disinfection techniques is critical to ensure a safe and effective infection control program. My approach uses a multi-faceted strategy:
- Initial didactic training: This involves classroom sessions or online modules covering the theory of disinfection, different disinfectant types, their uses and limitations, and proper application techniques. I use visual aids, videos, and interactive exercises to enhance understanding.
- Hands-on practical training: Following theory, practical demonstrations and supervised practice sessions allow staff to gain practical experience in applying disinfectants correctly. This includes proper donning and doffing of personal protective equipment (PPE).
- Regular competency assessments: Periodic assessments—both theoretical and practical—ensure staff maintain proficiency and identify any knowledge gaps. These assessments are documented to track performance and identify areas for further training.
- Ongoing reinforcement: We use regular refresher training, posters, checklists, and team briefings to maintain awareness and compliance. This prevents complacency and ensures adherence to best practices.
- Feedback and improvement: Regular feedback sessions allow us to adapt training to address specific challenges or emerging issues. Open communication and a supportive environment encourage staff participation and questions.
The success of any disinfection program rests heavily on well-trained and motivated personnel.
Q 27. How do you document and record disinfection procedures?
Meticulous documentation and record-keeping are essential for demonstrating compliance, identifying trends, and improving the disinfection program. Our system incorporates several key elements:
- Disinfectant inventory and usage logs: Detailed records track disinfectant type, quantity used, date of application, area treated, and personnel involved. This information is crucial for replenishing supplies and identifying any potential usage issues.
- Cleaning and disinfection checklists: Checklists ensure all steps in the cleaning and disinfection process are completed correctly. Completed checklists are signed and dated by the staff member performing the task.
- Incident reports: Any spills, equipment malfunction, or issues with disinfectant efficacy are documented in incident reports. These reports allow us to investigate root causes and implement corrective actions.
- Training records: A central repository maintains records of all staff training, including attendance, competency assessment results, and continuing education. This ensures all staff members are adequately trained and up-to-date on best practices.
- Audits and inspections: Regular audits and inspections ensure compliance with protocols, and findings are documented and used to improve the program.
This comprehensive documentation system provides a complete audit trail, ensuring accountability, supporting compliance with regulations, and facilitating continuous improvement of our infection control strategies.
Key Topics to Learn for Disinfection Techniques Interview
- High-Level Disinfection Strategies: Understanding the differences between sterilization, disinfection, and sanitation; choosing appropriate methods based on the application and risk level.
- Chemical Disinfection Methods: Mechanism of action of various disinfectants (e.g., chlorine, alcohols, quaternary ammonium compounds); selecting appropriate disinfectants for different surfaces and organisms; understanding the limitations and safety precautions associated with each.
- Physical Disinfection Methods: Principles and applications of heat (moist and dry), radiation (UV, ionizing), and filtration techniques; evaluating the effectiveness and practicality of each method.
- Disinfection Monitoring and Validation: Methods for monitoring the effectiveness of disinfection procedures (e.g., microbial testing, ATP bioluminescence); understanding validation protocols and regulatory requirements.
- Infection Prevention and Control: Applying disinfection techniques within the broader context of infection prevention and control; understanding standard precautions and transmission-based precautions.
- Practical Application & Problem Solving: Analyzing case studies of disinfection failures; troubleshooting common issues in disinfection protocols; adapting disinfection strategies to different environments (e.g., healthcare, food processing).
- Emerging Technologies in Disinfection: Familiarizing yourself with advancements in disinfection technologies, such as antimicrobial coatings and plasma disinfection.
- Regulatory Compliance and Safety: Understanding relevant safety regulations and guidelines pertaining to the handling and use of disinfectants; implementing appropriate personal protective equipment (PPE).
Next Steps
Mastering disinfection techniques is crucial for career advancement in various fields, opening doors to specialized roles and increased earning potential. A well-crafted resume is your key to unlocking these opportunities. An ATS-friendly resume ensures your qualifications are effectively communicated to hiring managers, maximizing your chances of landing an interview. ResumeGemini is a trusted resource to help you build a professional and impactful resume, tailored to highlight your skills and experience in Disinfection Techniques. Examples of resumes tailored specifically to this field are available to guide you through the process. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good