Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top ISO 13485:2016 Medical Devices Quality Management Systems interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in ISO 13485:2016 Medical Devices Quality Management Systems Interview
Q 1. Explain the key differences between ISO 9001 and ISO 13485.
While both ISO 9001 and ISO 13485 are quality management system (QMS) standards, ISO 13485 is specifically tailored for the medical device industry and builds upon the principles of ISO 9001. The key difference lies in the level of regulatory oversight and the emphasis on patient safety.
- Focus: ISO 9001 focuses on general customer satisfaction, while ISO 13485 prioritizes patient safety and regulatory compliance for medical devices.
- Risk Management: ISO 13485 has more stringent requirements for risk management, demanding a proactive approach throughout the product lifecycle. ISO 9001 includes risk-based thinking but doesn’t mandate the same level of detail.
- Regulatory Compliance: ISO 13485 explicitly addresses regulatory requirements specific to medical devices, including post-market surveillance and vigilance reporting, which are absent in ISO 9001.
- Traceability: ISO 13485 places a stronger emphasis on traceability of materials, processes, and devices throughout the entire supply chain to ensure product quality and safety.
- Validation and Verification: ISO 13485 is more rigorous in demanding design verification and validation to ensure devices meet their intended use and specifications.
Think of it this way: ISO 9001 is a broad framework for quality, while ISO 13485 is a specialized, more stringent version designed for the higher stakes involved in medical device manufacturing.
Q 2. Describe your experience with CAPA (Corrective and Preventive Action) investigations.
My experience with CAPA (Corrective and Preventive Action) investigations involves a structured approach emphasizing thorough root cause analysis and effective preventive measures. I’ve led numerous investigations, ranging from minor deviations to major non-conformances. My process typically includes:
- Immediate Containment: The first step is to isolate and contain the problem to prevent further incidents.
- Investigation: A thorough investigation is conducted to identify the root cause using tools like 5 Whys, fishbone diagrams, and fault tree analysis. This often involves interviewing involved personnel, reviewing documentation, and analyzing data.
- Corrective Action: Once the root cause is identified, effective corrective actions are implemented to resolve the immediate problem. For example, if a faulty component caused the non-conformance, we’d replace the component and potentially retrain staff on its proper handling.
- Preventive Action: Crucially, we implement preventive actions to prevent recurrence. This might involve process improvements, updated SOPs, enhanced training, or improved quality checks.
- Verification and Validation: We verify the effectiveness of both corrective and preventive actions. This could involve monitoring key metrics or conducting additional testing to ensure the problem is truly resolved and won’t reoccur.
- Documentation: Meticulous documentation throughout the entire process is crucial, ensuring traceability and transparency. This forms a valuable record for continuous improvement.
In one specific instance, we identified a recurring calibration error in a critical testing instrument. Through a thorough CAPA, we found the root cause to be inadequate training on the instrument’s operation. Corrective actions included immediate recalibration and retraining, while preventive actions included updated training materials and more frequent proficiency checks. This approach significantly reduced the frequency of calibration errors.
Q 3. How do you ensure traceability of medical devices throughout the supply chain?
Ensuring traceability of medical devices throughout the supply chain is paramount for patient safety and regulatory compliance under ISO 13485. This involves a robust system of identification and tracking. Key elements include:
- Unique Device Identification (UDI): Utilizing UDI systems allows for unambiguous identification of devices at every stage, from manufacturing to patient use. This assists in tracking devices in case of recalls or adverse events.
- Lot Number/Batch Tracking: Tracking devices by lot or batch number allows for rapid identification and isolation of problematic units if a defect is discovered.
- Supplier Control: Rigorous control of suppliers is vital. This involves assessing their quality management systems, verifying their materials and processes, and requiring them to maintain appropriate traceability records for the components they supply.
- Internal Tracking Systems: Maintaining internal systems for tracking device movement, from production to storage to distribution, is essential. This often involves barcodes, RFID tags, or other technologies.
- Documentation: Comprehensive documentation at each stage is essential. This includes purchase orders, manufacturing records, shipping documents, and distribution records. All documentation must be readily accessible and auditable.
For example, in a previous role, we implemented a barcode scanning system throughout our manufacturing and distribution processes. This allowed for real-time tracking of every device, enabling us to quickly locate and isolate devices in the event of a recall or quality issue.
Q 4. What are the requirements for risk management according to ISO 13485?
ISO 13485 mandates a robust risk management process throughout the entire lifecycle of a medical device, from design and development to post-market surveillance. This involves:
- Risk Identification: Systematically identifying potential hazards associated with the device and its use. This could involve brainstorming sessions, hazard analysis, and failure mode and effects analysis (FMEA).
- Risk Analysis and Evaluation: Determining the likelihood and severity of identified risks. This often uses a risk matrix to prioritize risks based on their potential impact.
- Risk Control: Implementing control measures to mitigate or eliminate identified risks. This could involve design modifications, process improvements, warnings in the instructions for use, or other measures.
- Risk Acceptance: Documenting any remaining risks that are considered acceptable after the implementation of control measures. This needs to be justified and accepted by management.
- Risk Review: Periodically reviewing and updating the risk management plan throughout the device’s lifecycle, especially when changes are made to the design or manufacturing process.
The risk management process should be documented and auditable, demonstrating a commitment to patient safety and regulatory compliance. A failure to adequately address risks can lead to serious consequences, including product recalls and potential harm to patients.
Q 5. Explain your understanding of Design Verification and Validation.
Design Verification and Validation are critical processes in ensuring that a medical device meets its intended use and performs as expected. They are distinct but complementary activities:
- Design Verification: This confirms that the design outputs meet the design inputs. It verifies that the design meets pre-defined specifications and requirements. This involves various methods such as inspections, reviews, tests, and analyses.
- Design Validation: This confirms that the finished design actually meets the intended use. It involves demonstrating that the device works as intended in its intended clinical setting. This often involves clinical trials or simulated use studies.
Analogy: Think of building a house. Verification checks that the house is built according to the blueprints (e.g., correct materials, dimensions, etc.). Validation confirms that the house is actually habitable and meets the needs of the occupants (e.g., it’s weatherproof, functional, etc.).
Both verification and validation require meticulous documentation. A comprehensive design history file is essential for demonstrating compliance with regulatory requirements.
Q 6. How would you handle a non-conformance identified during an audit?
Handling a non-conformance identified during an audit requires a prompt and systematic approach focused on corrective and preventive action. My steps would be:
- Immediate Assessment: Immediately assess the severity and scope of the non-conformance. Determine if it poses an immediate risk to patient safety.
- Containment: Take immediate action to contain the problem and prevent further non-conformances. This might involve stopping a production process, quarantining affected products, or implementing temporary corrective actions.
- Root Cause Analysis: Conduct a thorough investigation to determine the root cause of the non-conformance, using appropriate tools and techniques.
- Corrective Action: Implement corrective actions to rectify the immediate problem and address the root cause.
- Preventive Action: Develop and implement preventive actions to prevent recurrence of the non-conformance.
- Documentation: Document all actions taken, including the non-conformance, investigation, corrective actions, and preventive actions.
- Verification: Verify the effectiveness of corrective and preventive actions. This could involve monitoring key process parameters, conducting additional inspections or testing.
- Communication: Clearly communicate the findings and actions to relevant parties, including management and regulatory authorities if necessary.
This systematic approach ensures that the non-conformance is properly addressed and that steps are taken to prevent it from happening again. Effective communication is key to maintaining transparency and building trust with auditors and regulatory bodies.
Q 7. Describe your experience with internal audits of a QMS based on ISO 13485.
My experience with internal audits of ISO 13485-based QMSs involves a structured and systematic approach that ensures compliance and continuous improvement. I have:
- Developed and implemented audit plans: These plans outline the scope, objectives, and methodology of the audit, ensuring all critical areas of the QMS are covered.
- Conducted audits: I have conducted numerous internal audits, assessing the effectiveness of the QMS against the requirements of ISO 13485 and relevant regulations. This involves reviewing documents, interviewing personnel, observing processes, and evaluating records.
- Identified and documented non-conformances: During audits, I have identified non-conformances and documented them clearly and objectively, including their severity and potential impact.
- Prepared audit reports: I have prepared detailed audit reports summarizing the findings, including identified non-conformances and recommendations for corrective and preventive action.
- Followed up on corrective actions: I have followed up to ensure that appropriate corrective and preventive actions are implemented and effective.
In one instance, during an internal audit, we identified a gap in our document control process. This led to a non-conformance that was addressed through process improvements and retraining. The subsequent audit showed that the corrective actions had effectively closed the gap, highlighting the value of the internal audit process in maintaining compliance and continually improving our QMS.
Q 8. What are the essential elements of a robust document control system?
A robust document control system is the backbone of any ISO 13485 compliant Quality Management System (QMS). It ensures that all documents are current, accurate, readily available, and appropriately controlled throughout their lifecycle. Think of it as a meticulously organized library for all your critical company information.
- Identification and Control: Each document must be uniquely identified (e.g., document number, revision level) and controlled to prevent unauthorized changes. This often involves version control systems or document management software.
- Review and Approval: A clear process for reviewing and approving documents before release is crucial. This ensures accuracy, completeness, and alignment with regulatory requirements. Consider a formal approval workflow with designated approvers and audit trails.
- Distribution and Access: Controlled distribution ensures only authorized personnel have access to relevant documents. This could involve access control lists in a document management system or a controlled distribution list.
- Change Management: A well-defined change management process is vital. Any changes to a document must be formally proposed, reviewed, approved, and implemented, with clear traceability and version history. This prevents using obsolete documents and ensures everyone works with the latest version.
- Obsolete Document Control: Procedures to effectively remove obsolete documents from circulation and prevent their unintended use are essential. This might involve archiving and a process for physically destroying outdated hard copies.
- Storage and Retrieval: A system for storing and easily retrieving documents is crucial for efficiency and audit readiness. This could be a physical filing system or a digital repository.
For example, imagine a design specification for a medical device. A robust system ensures that only the approved version is used in manufacturing, and any changes are documented and communicated to all relevant parties. Without this control, there’s a high risk of manufacturing the wrong product, leading to potential patient harm and regulatory non-compliance.
Q 9. How do you ensure compliance with regulatory requirements like FDA 21 CFR Part 820?
Compliance with regulatory requirements like FDA 21 CFR Part 820, the Quality System Regulation (QSR), is paramount in the medical device industry. It demands a comprehensive QMS that covers every aspect of design, production, and post-market surveillance. Compliance isn’t a one-time achievement but an ongoing process requiring continuous monitoring and improvement.
To ensure compliance, we need a multi-pronged approach:
- Gap Analysis: Conduct a thorough gap analysis to compare our existing QMS against the requirements of 21 CFR Part 820. This identifies areas needing improvement.
- Implementation and Documentation: Develop and implement procedures and work instructions to address identified gaps. Thorough documentation of these procedures is essential for demonstrating compliance.
- Training: Train all personnel on the relevant regulations and their application within the QMS. Regular refresher training is important to maintain awareness and competency.
- Internal Audits: Conduct regular internal audits to assess the effectiveness of the QMS and identify any deviations from the requirements. These should follow a documented audit plan with qualified auditors.
- Corrective and Preventive Actions (CAPA): Implement a robust CAPA system to address any non-conformances, root causes of problems, and preventing their recurrence. This involves a well-defined process with documented steps.
- Management Review: Regularly review the QMS’s effectiveness through management reviews, addressing performance indicators and continuous improvement. This includes looking at key metrics like CAPA effectiveness, customer complaints, and audit findings.
- Supplier Management: Ensure that suppliers meet our quality requirements through rigorous supplier audits and quality agreements.
For example, our document control system directly addresses 21 CFR Part 820.80, which requires that design controls be established and maintained to ensure that devices are safe and effective. Our CAPA system addresses 21 CFR Part 820.100, ensuring that problems are investigated and corrected to prevent recurrence.
Q 10. What is your experience with post-market surveillance?
Post-market surveillance (PMS) is critical for monitoring the safety and performance of medical devices after they’ve been released to the market. It’s a proactive approach, not just reactive to complaints. My experience with PMS encompasses several key aspects:
- Planning and Implementation: Developing and implementing a PMS plan that defines the methods, scope, and timelines for monitoring devices. This typically involves defining key performance indicators (KPIs) and data collection methods.
- Data Collection and Analysis: Gathering data from various sources, including post-market reports, customer complaints, field safety notices, and literature reviews, and analyzing this data to identify potential problems or trends.
- Risk Management: Assessing the risks associated with identified problems and implementing appropriate risk mitigation strategies. This may include issuing field safety notices, conducting investigations, or modifying the product.
- Reporting and Regulatory Compliance: Reporting any identified safety issues to the relevant regulatory authorities (like the FDA) in a timely manner, complying with all reporting requirements.
- Continuous Improvement: Using the PMS data to improve the design, manufacturing, and performance of the devices and the PMS system itself.
In a previous role, I led a team that implemented a PMS system for a new implantable cardiac device. We established a comprehensive database to track reported events and leveraged statistical analysis to identify trends and correlations, allowing for proactive risk mitigation and ultimately, improved patient safety.
Q 11. Describe your understanding of the product lifecycle in medical devices.
The medical device product lifecycle is a structured series of stages, from initial concept to eventual retirement. Understanding this lifecycle is crucial for effective QMS management.
- Research and Development (R&D): This includes defining the device’s intended use, designing it, and verifying that the design meets the requirements.
- Design and Development: This is a critical stage involving detailed design specifications, prototyping, testing, and validation to ensure that the device meets safety, efficacy, and performance criteria.
- Manufacturing and Production: This stage involves establishing and validating manufacturing processes, ensuring consistent product quality and compliance with regulatory requirements.
- Quality Control (QC): Implementing rigorous QC checks at various stages of manufacturing to ensure that products meet specifications and regulatory standards.
- Packaging and Labeling: Ensuring that the device is appropriately packaged and labeled to meet regulatory requirements and to provide clear instructions for use.
- Distribution and Sales: Distributing the product to customers, ensuring that appropriate storage and handling procedures are followed.
- Post-Market Surveillance (PMS): As discussed earlier, monitoring the device’s performance and safety after it’s been released to the market.
- Product Retirement: Managing the end-of-life phase, including procedures for handling product recalls and disposal.
A thorough understanding of each stage allows for proactive identification and management of potential risks throughout the device’s lifespan, ensuring patient safety and regulatory compliance.
Q 12. How do you manage changes to the quality management system?
Managing changes to the QMS is crucial for maintaining compliance and adapting to evolving business needs. A structured change control process is essential.
- Change Proposal: Any proposed change to the QMS must be formally documented as a change proposal, detailing the proposed changes, rationale, and impact assessment.
- Review and Approval: The change proposal should be reviewed by relevant stakeholders and approved by authorized personnel. This might involve a change control board.
- Implementation: Changes must be implemented in a controlled manner, with clear documentation of the implementation steps.
- Verification and Validation: After implementation, the effectiveness of the changes should be verified and validated to ensure that they achieve the intended results and don’t introduce new risks.
- Documentation Update: All relevant QMS documentation should be updated to reflect the implemented changes, with clear version control.
- Communication: Stakeholders must be informed of the changes and their impact.
For instance, if we implement a new software for managing CAPA, the change control process ensures that all relevant procedures are updated, personnel are trained, and the effectiveness of the new software is verified. This prevents confusion and maintains the integrity of the QMS.
Q 13. Explain your experience with supplier management and quality agreements.
Effective supplier management is crucial for ensuring the quality and safety of medical devices. This includes selecting qualified suppliers, establishing robust quality agreements, and monitoring their performance.
- Supplier Selection: Selecting suppliers based on their capabilities, quality systems, and past performance. This often involves a pre-qualification process with audits.
- Quality Agreements: Establishing formal quality agreements with suppliers that clearly define quality requirements, responsibilities, and inspection criteria. These agreements outline expectations and compliance requirements.
- Supplier Audits: Conducting regular audits of suppliers to verify their compliance with the quality agreements and applicable regulatory requirements.
- Performance Monitoring: Continuously monitoring supplier performance using key performance indicators (KPIs) such as defect rates, on-time delivery, and compliance to specifications.
- Corrective Actions: Working with suppliers to address any non-conformances or quality issues that arise.
For example, a supplier providing critical components for a heart valve would be subject to rigorous audits, including on-site inspections of their facilities and manufacturing processes. The quality agreement would specify precise materials, tolerances, and testing requirements. Any deviations would trigger corrective actions and potential supplier replacement if necessary.
Q 14. What are the key requirements for managing records in a medical device QMS?
Managing records within a medical device QMS is critical for demonstrating compliance with ISO 13485 and other relevant regulations. This requires a systematic approach.
- Identification and Control: Each record must be uniquely identified and controlled to prevent loss, damage, or unauthorized alteration. This might involve numbering, version control, and storage in a secure location.
- Protection and Retention: Records must be protected from damage, loss, or unauthorized access and retained for a defined period, meeting regulatory requirements. This could involve secure digital storage and a defined record retention policy.
- Accessibility: Records must be readily accessible to authorized personnel when needed. This might involve a searchable database or well-organized filing system.
- Accuracy and Completeness: Records must be accurate, complete, and legible. This means using proper documentation techniques and ensuring accurate data entry.
- Integrity: Maintaining the integrity of records, preventing any changes or alterations that compromise their validity. This might involve version control and audit trails.
For example, records related to device design, testing, manufacturing, and complaints must be maintained for a specific period, often several years, and readily accessible during audits. Failure to properly manage these records could lead to non-compliance and serious consequences.
Q 15. How do you ensure the effectiveness of your quality management system?
Ensuring the effectiveness of a Quality Management System (QMS) compliant with ISO 13485:2016 is a continuous process, not a one-time event. It requires a robust approach encompassing several key aspects. Think of it like maintaining a finely tuned machine – regular checks, adjustments, and proactive maintenance are crucial.
- Regular Internal Audits: We conduct regular internal audits to assess compliance with the QMS, identify gaps, and ensure processes are functioning as intended. These audits follow a pre-defined schedule and checklist, focusing on critical aspects like document control, risk management, and corrective actions.
- Management Review: A management review meeting is held periodically to evaluate the QMS’s performance, effectiveness, and suitability. This is where we analyze audit findings, customer feedback, and key performance indicators (KPIs) to identify areas for improvement. It’s a high-level strategic review, ensuring alignment with business objectives.
- Corrective and Preventive Actions (CAPA): A robust CAPA system is essential. When a nonconformity occurs (a deviation from established procedures), a thorough investigation is performed to identify the root cause. Corrective actions address the immediate issue, while preventive actions aim to prevent similar problems from happening again. We track CAPA effectiveness to ensure lasting solutions.
- Continuous Improvement: ISO 13485 emphasizes a culture of continuous improvement. We utilize methods like Plan-Do-Check-Act (PDCA) cycles to systematically identify opportunities for improvement, implement changes, and monitor their effectiveness. This ensures the QMS is constantly evolving to meet changing needs and regulations.
- Monitoring and Measurement: We monitor key performance indicators (KPIs) relevant to product quality and QMS effectiveness. This includes metrics such as defect rates, customer complaints, and audit findings. Regular monitoring helps identify trends and potential problems early on.
For example, during an internal audit, if we discovered a deficiency in our document control process, we would immediately initiate a CAPA to address the issue. This might involve revising our document control procedures, providing additional training to personnel, and implementing a stricter document approval process. The effectiveness of the corrective actions would be verified through subsequent audits.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with statistical process control (SPC).
Statistical Process Control (SPC) is a crucial tool for monitoring and improving manufacturing processes in medical device production. It involves using statistical methods to identify variations and trends in processes, allowing us to proactively address potential problems before they lead to nonconformances. I have extensive experience applying SPC techniques in various contexts.
- Control Charts: I’m proficient in using various control charts, such as X-bar and R charts, p-charts, and c-charts, to monitor key process parameters. These charts help identify when a process is operating outside its normal limits, indicating potential problems needing investigation. For example, we might monitor the weight of a particular component using an X-bar and R chart to detect any variations that could impact product performance or safety.
- Process Capability Analysis: I have experience conducting process capability analyses (Cpk, Ppk) to determine whether a process is capable of consistently producing products that meet pre-defined specifications. This analysis helps determine whether process improvements are necessary.
- Data Analysis: My experience includes using statistical software packages to analyze process data, identify trends, and determine the root cause of variations. This analysis helps us make data-driven decisions related to process improvements.
In one instance, we used control charts to monitor the sterilization cycle time for a specific medical device. By analyzing the data, we identified a trend towards increasing cycle times, indicating potential issues with the sterilization equipment. A timely investigation revealed a malfunctioning component, which was promptly replaced, preventing potential product contamination and ensuring patient safety.
Q 17. What is your understanding of process validation in a medical device context?
Process validation in a medical device context is a critical step demonstrating that a manufacturing process consistently produces a product meeting predefined specifications and quality attributes. It’s not a one-time activity, but an ongoing process of verification and monitoring.
- Design Qualification: This phase ensures that the equipment and processes are designed correctly to produce the medical device according to the design specifications. This includes evaluating the suitability of the equipment and facilities.
- Installation Qualification: This involves verifying that the equipment is installed correctly and operates as intended in its intended environment.
- Operational Qualification: This verifies that the equipment operates within predetermined parameters and meets the process requirements. This might involve testing the equipment at different operating ranges.
- Performance Qualification: This demonstrates that the entire process, including equipment, materials, and personnel, consistently produces the expected product quality and performance. This often involves running multiple production batches under normal operating conditions.
Imagine validating the sterilization process for a surgical instrument. Design qualification would involve reviewing the design of the autoclave, operational qualification would involve verifying that the temperature and pressure parameters are maintained within acceptable ranges, and performance qualification would involve demonstrating that the process consistently achieves sterility as confirmed by microbiological testing.
Q 18. Explain your knowledge of quality planning and control methods.
Quality planning and control methods are fundamental to ensuring consistent product quality and compliance with regulatory requirements. They involve proactive planning and ongoing monitoring of processes.
- Quality Planning: This involves defining quality objectives, identifying potential risks, and developing strategies to ensure that products meet requirements. This is often achieved using tools like Failure Mode and Effects Analysis (FMEA).
- Design Control: This ensures that the product design meets its intended use and user needs. This includes design reviews, risk assessments, and verification and validation activities.
- Process Control: This involves monitoring and controlling the manufacturing processes to ensure consistency and prevent defects. This often utilizes SPC techniques.
- Inspection and Testing: This includes conducting inspections and tests at various stages of the manufacturing process to identify and address defects early on.
- Corrective and Preventive Actions (CAPA): This is a systematic approach to address nonconformities and prevent future occurrences.
For instance, during quality planning, we might use an FMEA to identify potential failure modes during the manufacturing of a medical device, assess the severity and likelihood of each failure, and implement controls to mitigate the risks. Regular process controls then ensure these mitigations remain effective.
Q 19. How do you conduct a risk analysis for a new medical device?
Risk analysis for a new medical device is crucial to identify and mitigate potential hazards that could affect patient safety and product quality. We typically use a risk management process based on ISO 14971.
- Hazard Identification: We systematically identify potential hazards associated with the device, considering its intended use, foreseeable misuse, and the device’s lifecycle. This often involves brainstorming sessions, hazard checklists, and fault tree analysis.
- Risk Analysis: We analyze the identified hazards to determine their severity, probability of occurrence, and the detectability of any resulting harm. This may use a risk matrix to visually represent the levels of risk.
- Risk Evaluation: We evaluate the overall level of risk associated with each hazard, comparing it to predetermined acceptance criteria. This determines whether the risk is acceptable or requires mitigation.
- Risk Control: We implement risk controls to mitigate unacceptable risks. These controls can be technical (design modifications), administrative (improved training), or procedural (changes to operating instructions).
- Risk Monitoring: After implementation, we continuously monitor the effectiveness of the implemented controls throughout the device’s lifecycle. This includes post-market surveillance.
For example, if a hazard analysis identified a risk of electrical shock from a device, risk control measures might include adding insulation, incorporating a ground fault circuit interrupter, and providing clear warnings in the user manual. Post-market surveillance would then monitor any incidents related to electrical shock.
Q 20. What is your experience with implementing and maintaining a quality management system?
My experience with implementing and maintaining a QMS encompasses all stages, from initial planning and documentation to ongoing maintenance and improvement. I have been involved in implementing ISO 13485:2016 QMS in multiple medical device companies.
- Gap Analysis: I begin by conducting a gap analysis to compare the existing QMS with the requirements of ISO 13485:2016, identifying areas needing improvement.
- Documentation Development: This involves developing or revising various QMS documents, including quality policy, procedures, work instructions, and records. These documents must be accurate, complete, and readily accessible to all relevant personnel.
- Training and Communication: I ensure all employees receive appropriate training on the QMS requirements and their responsibilities. Effective communication is essential to ensure everyone understands and adheres to the system.
- Internal Audits: I conduct and participate in internal audits to assess QMS compliance and identify areas needing improvement.
- Management Review: I actively participate in management reviews to evaluate QMS performance and ensure its effectiveness in achieving quality objectives.
- Continuous Improvement: I foster a culture of continuous improvement through the implementation of PDCA cycles, addressing nonconformities, and proactively seeking opportunities for enhancement.
In a recent implementation, we used a phased approach, starting with the core elements of the QMS and progressively implementing more complex aspects. This allowed us to demonstrate early successes, build confidence, and gather valuable feedback from our staff.
Q 21. How do you handle customer complaints related to medical devices?
Handling customer complaints related to medical devices is a critical process requiring a systematic approach. Our objective is to investigate the complaint thoroughly, resolve the issue promptly, and learn from the experience to prevent recurrence.
- Complaint Receipt and Recording: All complaints are received, documented, and logged in a complaint management system. Key details such as the nature of the complaint, the affected device, and the customer’s contact information are meticulously recorded.
- Investigation and Analysis: A thorough investigation is undertaken to determine the root cause of the complaint. This may involve reviewing device history records, conducting testing, and interviewing relevant personnel.
- Corrective Actions: Based on the investigation, appropriate corrective and preventive actions (CAPA) are implemented to resolve the immediate issue and prevent similar complaints in the future. This may involve repairing or replacing the device, updating instructions for use, or improving manufacturing processes.
- Customer Communication: We promptly communicate with the customer throughout the complaint handling process, providing updates and addressing their concerns.
- Closeout: The complaint is closed only after the corrective actions have been verified to be effective and the customer is satisfied.
- Data Analysis: Trends in customer complaints are analyzed to identify recurring issues and to highlight areas for improvement in the design, manufacturing, or post-market surveillance processes.
For example, if we received a complaint about a malfunctioning component in a medical device, we would investigate the complaint, identify whether it was a design or manufacturing issue, implement corrective actions (e.g., replacing defective parts, improving the manufacturing process), and inform the customer of our findings and resolution.
Q 22. Describe your experience with root cause analysis techniques.
Root cause analysis (RCA) is a systematic process for identifying the underlying causes of problems, not just the symptoms. My experience encompasses several techniques, including the 5 Whys, Fishbone diagrams (Ishikawa diagrams), Fault Tree Analysis (FTA), and Failure Mode and Effects Analysis (FMEA).
For example, using the 5 Whys, if a surgical instrument malfunctions during a procedure (the problem), we’d repeatedly ask ‘why’ to uncover the root cause. Why did it malfunction? (e.g., due to a faulty latch). Why was the latch faulty? (e.g., insufficient testing during manufacturing). Why was the testing insufficient? (e.g., lack of proper training for inspectors). Why was there a lack of training? (e.g., inadequate training budget). This final ‘why’ often reveals the true systemic issue needing correction.
Fishbone diagrams provide a visual representation of potential causes, categorized by factors like people, materials, methods, and machines. This helps in brainstorming and identifying potential failure points. FTA helps visualize complex systems and identify the combinations of events that lead to failure. Finally, FMEA proactively identifies potential failure modes and their effects, allowing us to mitigate risks before they materialize.
Q 23. What is your understanding of the different types of audits (e.g., internal, external, supplier)?
In the context of ISO 13485, audits are crucial for ensuring compliance. There are several types:
- Internal Audits: Conducted by the organization itself to assess its compliance with the QMS and identify areas for improvement. Think of this as a self-check, identifying weaknesses before an external audit.
- External Audits: Performed by an independent, accredited certification body to verify the effectiveness of the QMS. This is a formal assessment that determines whether the organization meets ISO 13485 requirements.
- Supplier Audits: These audits assess the quality management systems of suppliers who provide materials or services that impact the safety and effectiveness of our medical devices. This ensures that our supply chain maintains appropriate quality standards.
Each audit type has different scopes and objectives, but they all aim to ensure product quality, patient safety, and regulatory compliance.
Q 24. How would you address a significant non-conformance identified during an external audit?
Addressing a significant non-conformance from an external audit requires a prompt and systematic response. First, we’d acknowledge the non-conformance and its severity. Then, we’d conduct a thorough investigation using root cause analysis techniques (as described earlier) to understand why it occurred.
Next, we would implement corrective actions to eliminate the root cause and prevent recurrence. These actions might involve revising procedures, updating training materials, improving equipment calibration processes, or changing supplier relationships. We’d also implement preventative actions to avoid similar issues in the future.
All actions taken would be documented, and their effectiveness verified. We’d then report our findings and the corrective and preventative actions taken to the external auditor, demonstrating commitment to improvement and regulatory compliance. The effectiveness of the corrective actions would be monitored through key performance indicators (KPIs) to ensure lasting improvement.
Q 25. What are the key performance indicators (KPIs) you would track for a medical device QMS?
Key Performance Indicators (KPIs) for a medical device QMS should focus on both the effectiveness of the system and the quality of the product. Some examples include:
- Number of non-conformances: Tracks the frequency of quality issues, indicating areas needing attention.
- Customer complaints: Monitoring customer feedback provides insights into product performance and satisfaction.
- Effectiveness of corrective and preventative actions: Measures the success rate of actions taken to address identified problems.
- Supplier performance: Tracks the quality of materials and services received from suppliers.
- On-time delivery performance: Measures adherence to production schedules.
- Training completion rates: Indicates the effectiveness of employee training programs.
- Internal audit findings: Tracks the number and severity of non-conformances identified during internal audits.
The specific KPIs selected should align with the organization’s strategic goals and risk profile. Regular monitoring and analysis of these KPIs are crucial for continuous improvement.
Q 26. How do you ensure that your QMS is continually improved?
Continual improvement is a cornerstone of ISO 13485. We use several approaches to ensure ongoing improvement of our QMS. This includes:
- Regular management reviews: Senior management reviews the performance of the QMS at set intervals, identifying opportunities for improvement.
- Data analysis: Analyzing KPIs (as mentioned above) helps pinpoint areas needing attention.
- Internal audits: Regularly scheduled internal audits identify weaknesses in the system.
- Employee feedback: Encouraging and acting upon employee suggestions for improvement is vital.
- Benchmarking: Comparing our performance to industry best practices allows us to identify areas for enhancement.
- Process optimization: Continuously refining our processes to eliminate waste and enhance efficiency.
By actively implementing these methods, we ensure our QMS remains robust, efficient, and effective in producing high-quality, safe medical devices.
Q 27. Describe your experience with training employees on quality management system requirements.
Training is essential for a successful QMS. My experience includes developing and delivering training programs covering various aspects of ISO 13485. This includes creating engaging training materials, such as presentations, workbooks, and interactive exercises.
I tailor training to different roles and responsibilities within the organization, ensuring that employees receive the specific knowledge and skills needed to perform their jobs effectively and in compliance with the QMS. For example, production staff receives training on specific quality control procedures, while management is trained on management review processes and internal auditing techniques. Training effectiveness is assessed through regular evaluations, such as quizzes and practical assessments, to ensure understanding and competency. Records of all training activities are meticulously maintained to demonstrate compliance.
Q 28. How would you explain ISO 13485 requirements to someone with no prior knowledge of the standard?
ISO 13485:2016 is an international standard that specifies requirements for a quality management system (QMS) for organizations involved in the design, development, production, installation, and servicing of medical devices. Think of it as a detailed instruction manual for consistently producing safe and effective medical devices.
It’s designed to ensure that these organizations have the processes and controls in place to manage risks, meet regulatory requirements, and consistently deliver products that meet patient needs and safety standards. Compliance helps ensure the quality, safety and efficacy of medical devices which is paramount for patient health and safety. Failure to meet these requirements can lead to serious consequences including product recalls and regulatory action.
Key Topics to Learn for ISO 13485:2016 Medical Devices Quality Management Systems Interview
- Scope and Application: Understand the standard’s applicability to different medical device types and organizations. Consider how the requirements adapt to various organizational structures and product lifecycles.
- Risk Management: Explore the implementation of risk management processes throughout the product lifecycle, including hazard analysis and risk control. Practice applying risk management methodologies to hypothetical scenarios.
- Quality Management System (QMS) Requirements: Master the core elements of a QMS, such as document control, record management, internal audits, and management review. Think about practical challenges in maintaining a robust QMS and how to solve them.
- Design and Development: Understand the requirements for design control, including design verification and validation activities. Be prepared to discuss the practical aspects of designing medical devices according to ISO 13485 principles.
- Production and Service Provision: Familiarize yourself with the control of production processes, including purchasing, manufacturing, and distribution. Consider how to address potential production-related issues and ensure product traceability.
- Corrective and Preventive Actions (CAPA): Understand the process of investigating nonconformities, implementing corrective actions, and preventing recurrence. Practice applying the CAPA process to case studies.
- Post-Market Surveillance: Know the importance of monitoring device performance after market release, including handling complaints and adverse events. Think about effective strategies for post-market surveillance and vigilance.
- Management Responsibility: Understand the role of top management in establishing and maintaining the QMS. Consider the importance of leadership commitment to quality and regulatory compliance.
Next Steps
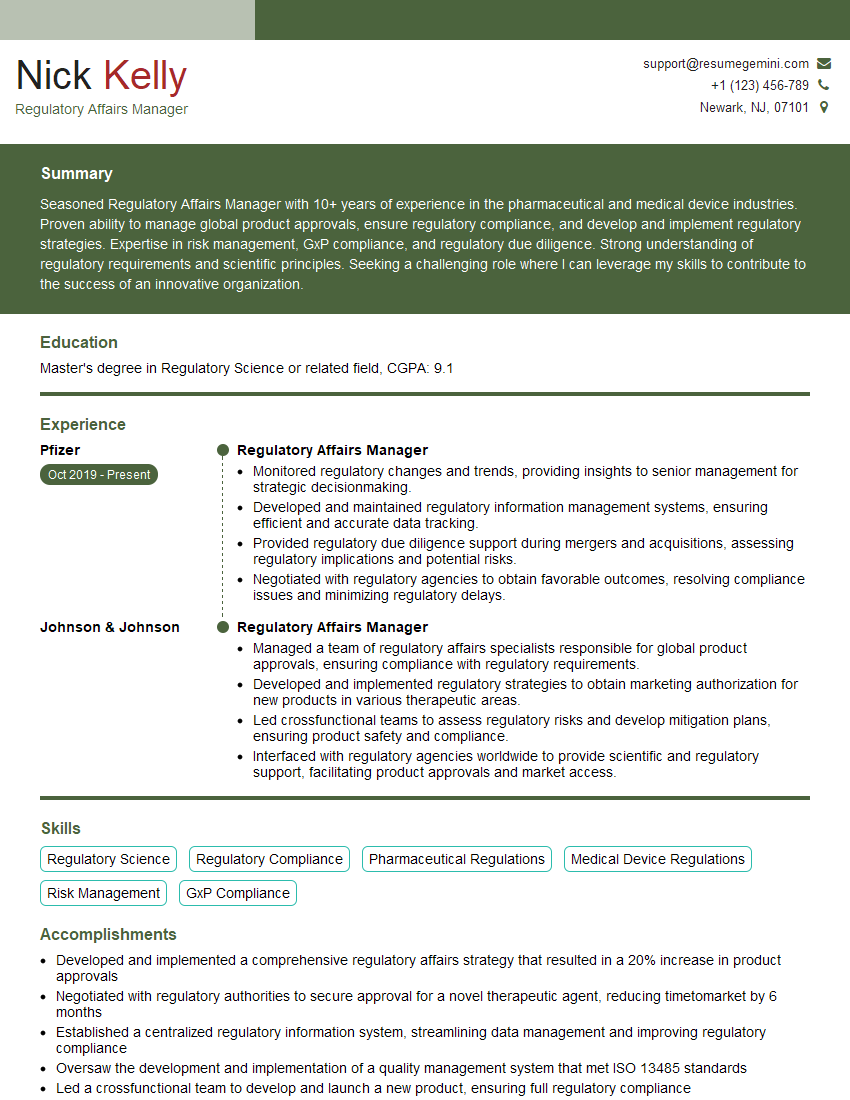
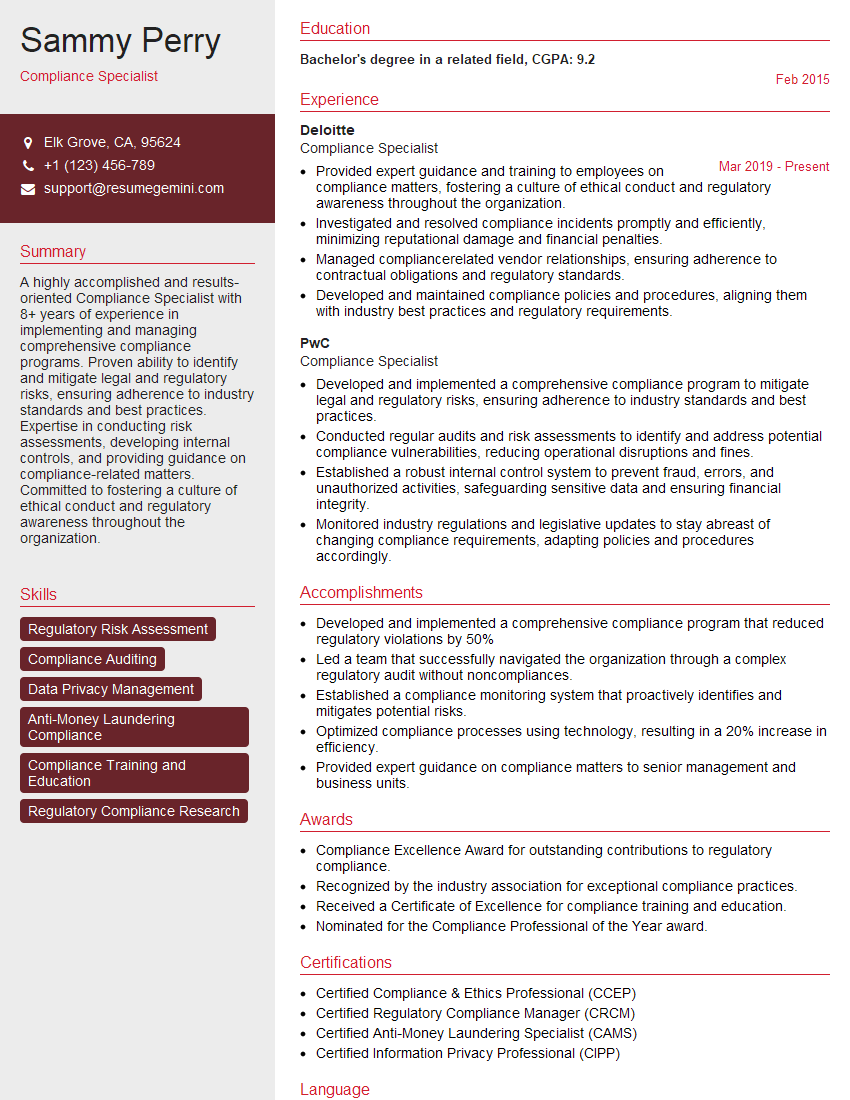
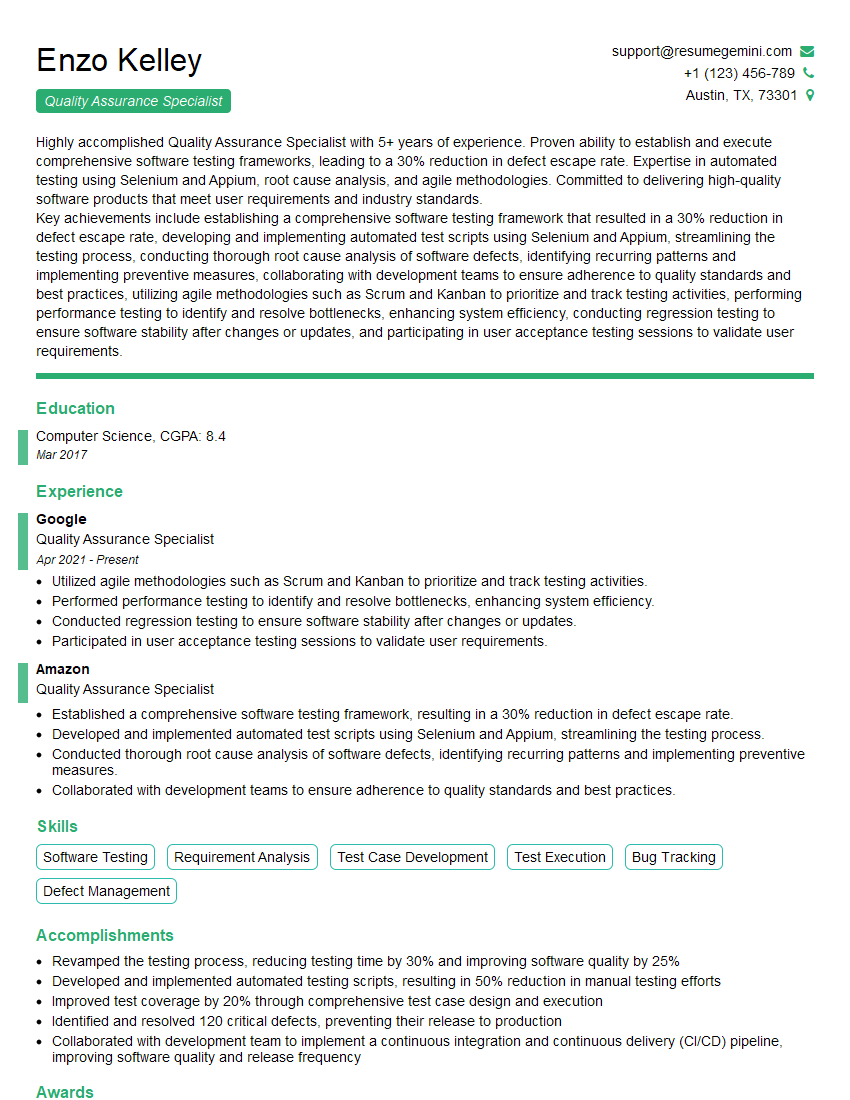
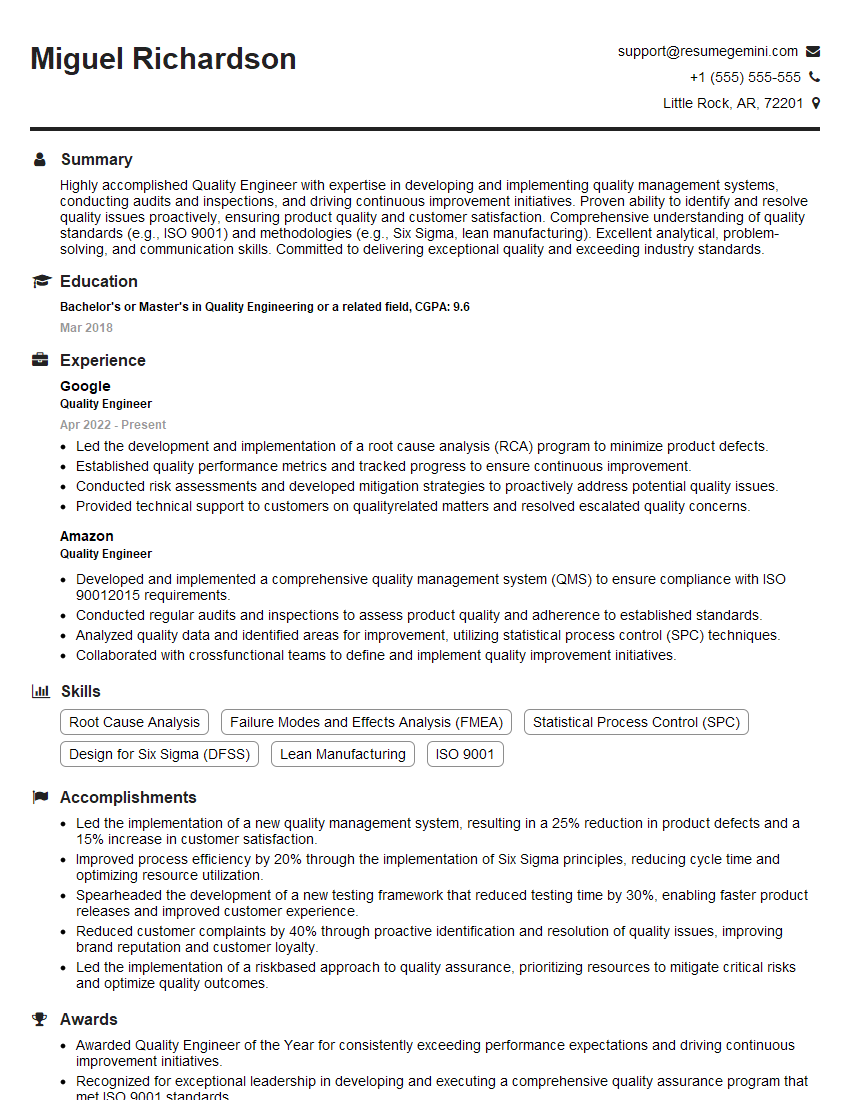
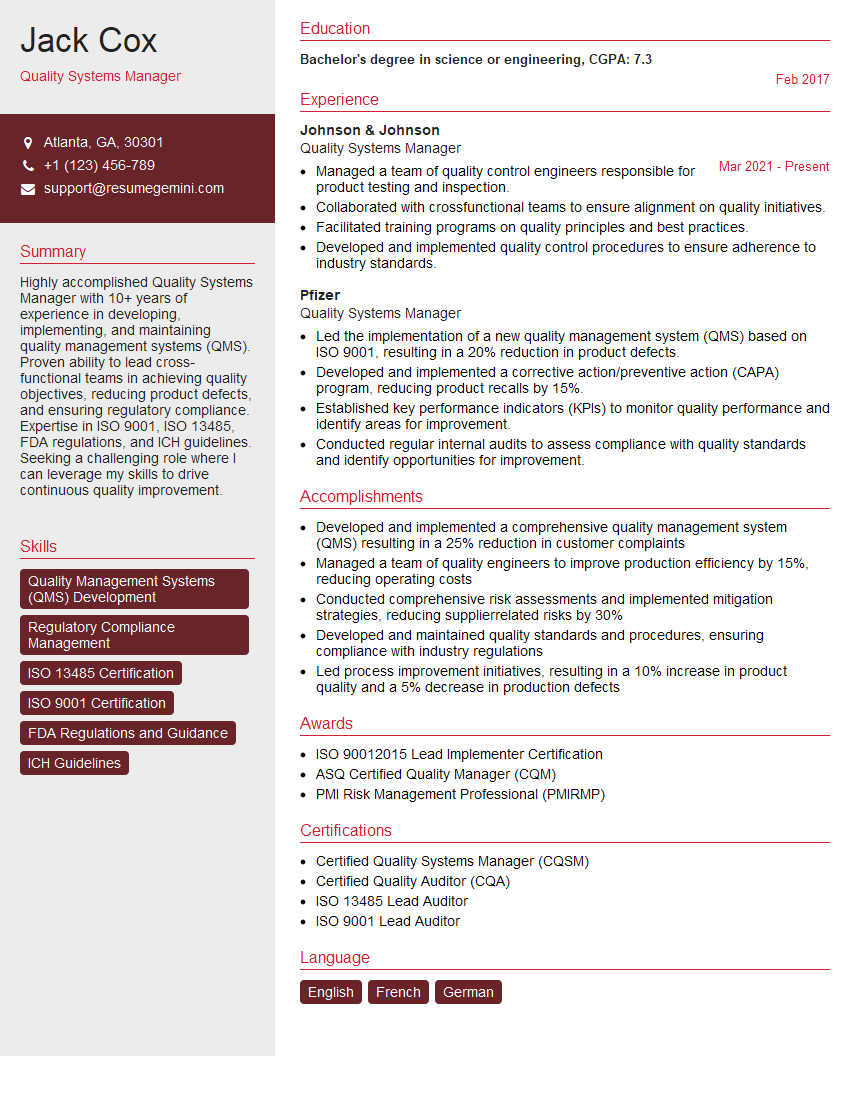
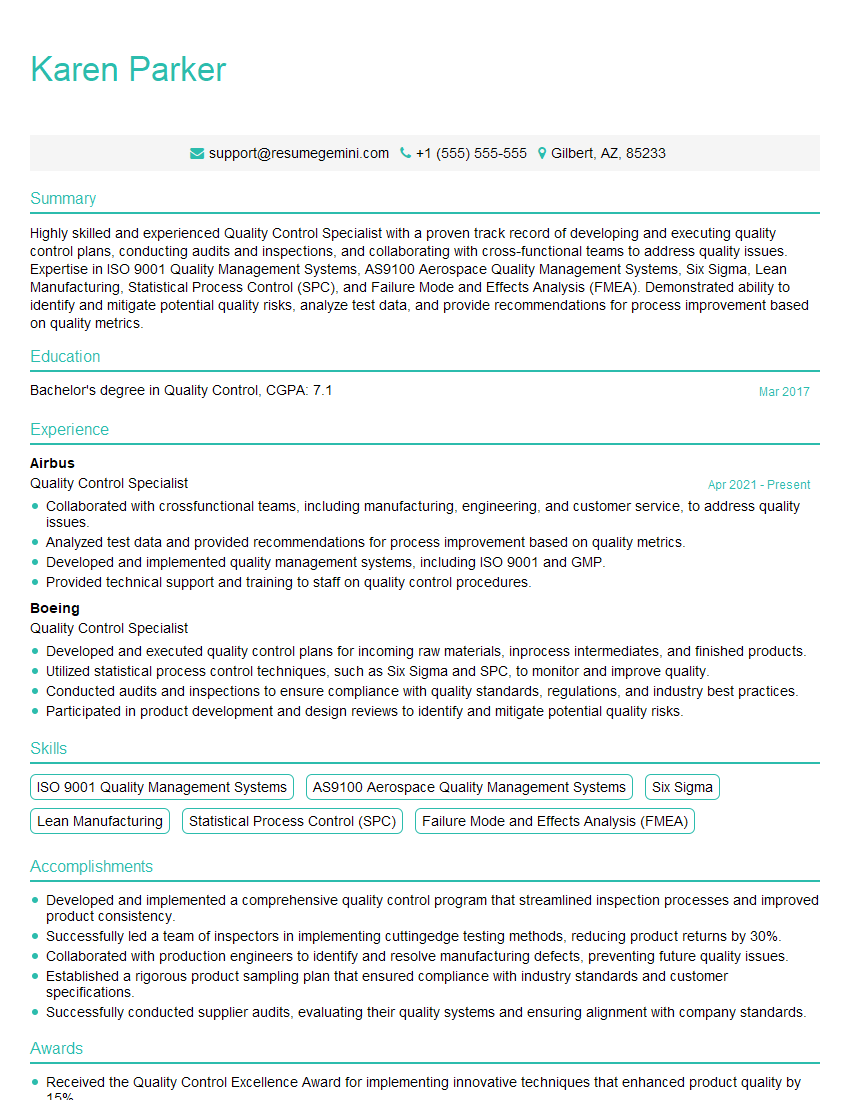
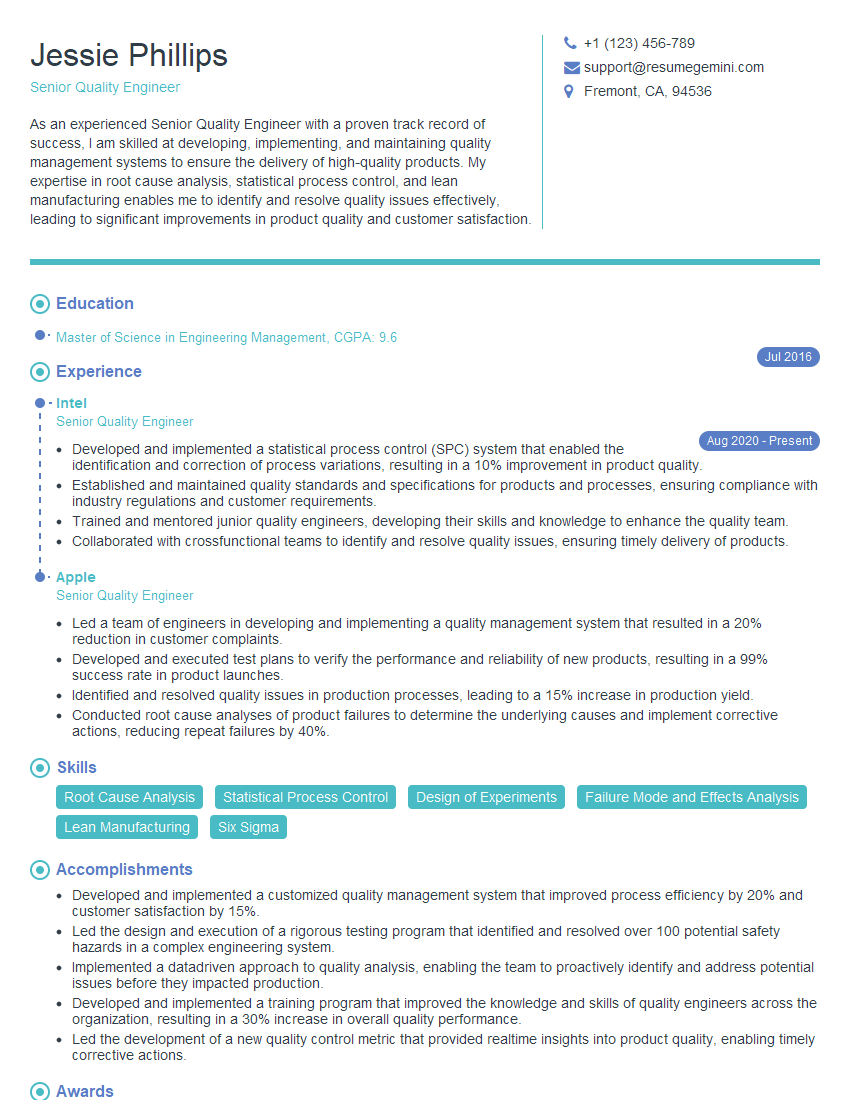
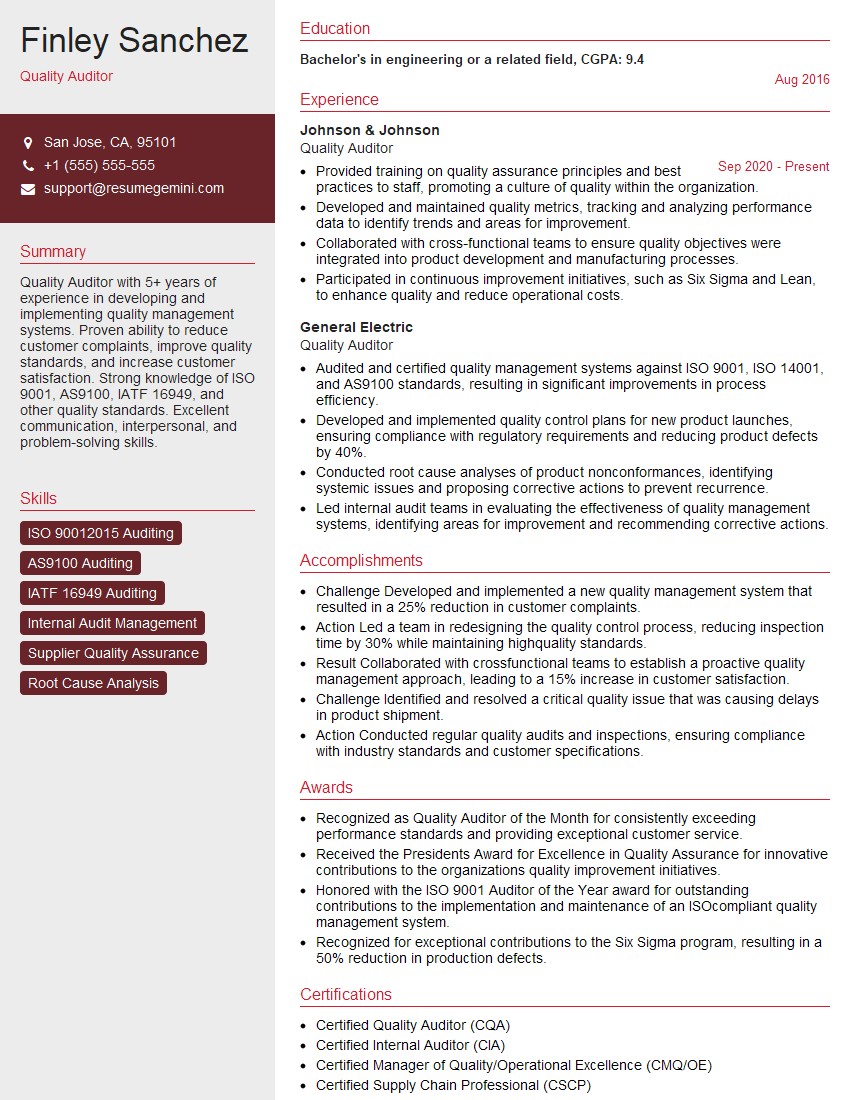
Mastering ISO 13485:2016 is crucial for career advancement in the medical device industry, opening doors to exciting opportunities and higher responsibilities. A strong understanding of this standard demonstrates your commitment to quality and patient safety. To significantly boost your job prospects, focus on crafting an ATS-friendly resume that highlights your skills and experience relevant to ISO 13485. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to ISO 13485:2016 Medical Devices Quality Management Systems to guide you. Take the next step toward your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good