Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Goniometry interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Goniometry Interview
Q 1. Explain the purpose of goniometry in clinical settings.
Goniometry, in a clinical setting, is the precise measurement of angles created at joints. It’s a fundamental tool for assessing a patient’s range of motion (ROM), a critical factor in diagnosing and monitoring musculoskeletal conditions. Think of it as a ruler for joint movement. By quantifying joint angles, clinicians can objectively track progress during rehabilitation, identify limitations, and develop tailored treatment plans. For example, measuring the knee flexion angle after a knee replacement helps determine the effectiveness of physical therapy.
Q 2. Describe the different types of goniometers and their applications.
Several types of goniometers exist, each with specific applications:
- Standard Universal Goniometer: This is the most common type, featuring two arms connected at a central protractor. It’s versatile and suitable for most joints. Think of it as the ‘workhorse’ of goniometry.
- Circular Goniometer: Used for measuring rotation, particularly in the spine or hip. It offers a 360-degree measurement range.
- Inclinometer: A small, handheld device that measures angles using an internal bubble level. It’s often preferred for assessing spinal curvature and trunk flexion.
- Digital Goniometers: These electronic devices offer increased accuracy and often have data logging capabilities for easy record-keeping. They are increasingly common due to improved precision and efficient data management.
The choice of goniometer depends on the specific joint and type of movement being measured. For instance, a standard goniometer is ideal for measuring elbow flexion, while a circular goniometer is better suited for measuring spinal rotation.
Q 3. What are the standard anatomical positions for goniometric measurements?
Accurate goniometric measurements rely on establishing consistent anatomical positions as a baseline. The standard anatomical position is crucial for comparability and accuracy across different assessments. It’s defined as the body standing erect, arms at the sides, palms facing forward, and feet together. From this position, joint angles are measured relative to the body’s alignment. For example, measuring shoulder flexion involves starting with the arm positioned alongside the body (0 degrees) and then measuring the angle as the arm is raised.
Q 4. How do you ensure accurate and reliable goniometric measurements?
Ensuring accurate and reliable goniometric measurements requires careful attention to detail and standardized procedures:
- Proper Patient Positioning: The patient should be positioned comfortably and correctly to avoid influencing the measurement. Proper support can be crucial for accurate readings.
- Stabilizing the Proximal Segment: One clinician should firmly but gently stabilize the proximal (stationary) limb segment while the other measures movement.
- Accurate Alignment of Goniometer Arms: The stationary arm should be aligned with the proximal segment, and the moving arm should be aligned with the distal segment. This precise alignment is vital for accurate angles.
- Clear Visual Reference Points: Identify and utilize clear bony landmarks to position the goniometer accurately. Using incorrect anatomical landmarks can lead to significant errors.
- Multiple Measurements: Taking multiple measurements and averaging them minimizes the impact of slight inconsistencies.
- Calibration and Maintenance of Goniometers: Ensure the goniometer is properly calibrated and maintained. This ensures the accuracy of your assessments.
By following these steps, clinicians can minimize error and enhance the reliability of their goniometric assessments.
Q 5. Explain the procedure for measuring range of motion (ROM) in the shoulder joint.
Measuring shoulder range of motion requires a systematic approach:
- Patient Positioning: The patient should be sitting or standing, with the shoulder relaxed.
- Goniometer Placement: The stationary arm of the goniometer is aligned with the midline of the trunk, and the moving arm is aligned with the lateral aspect of the arm.
- Landmarks: Common landmarks include the acromion process (stationary) and the lateral epicondyle of the humerus (moving).
- Measurements: Measure flexion (raising the arm forward), abduction (raising the arm to the side), external rotation (rotating the arm outward), and internal rotation (rotating the arm inward). Each movement should be measured from its respective starting point (0 degrees).
- Recording: Note each angle separately, clearly indicating the direction of movement.
For example, when measuring shoulder flexion, the patient raises their arm forward until they feel a comfortable stretch. The angle created between the trunk and the humerus is the flexion angle. Repeating this process for other movements ensures a complete picture of the shoulder’s ROM.
Q 6. How do you document goniometric measurements in a patient’s chart?
Goniometric measurements should be meticulously documented in the patient’s chart to ensure continuity of care and facilitate treatment planning. Documentation should be clear, concise, and consistent. Include:
- Date and Time of Assessment: This ensures accurate tracking of progress over time.
- Joint Assessed: Clearly specify the joint being measured, such as the right or left knee, elbow etc.
- Type of Movement: Indicate the specific movement measured, for example, flexion, extension, abduction, adduction, etc.
- Angle Measured: Record the measured angle in degrees. For example, ‘Right knee flexion: 110 degrees’.
- Any Pain or Limitation: Document any pain or limitations experienced by the patient during the measurement. This information is essential for assessing the patient’s condition and guiding treatment decisions. For example: ‘Right shoulder abduction limited to 90 degrees due to pain.’
- Clinician’s Name: Include the clinician who performed the assessment. This ensures accountability and facilitates communication.
Using a standardized format, such as a template, will improve consistency and make it easier to compare measurements over time.
Q 7. What are the common errors to avoid during goniometric assessments?
Common errors to avoid during goniometric assessments include:
- Improper Patient Positioning: Incorrect positioning can significantly affect the accuracy of measurements.
- Inaccurate Alignment of Goniometer Arms: Misalignment of the goniometer arms leads to inaccurate angle readings.
- Incorrect Identification of Anatomical Landmarks: Using the wrong bony landmarks can introduce substantial error into the measurement.
- Insufficient Stabilization of the Proximal Segment: Allowing movement in the proximal segment makes the measurement invalid.
- Applying Excessive Pressure: Applying excessive pressure to the joint or surrounding muscles can restrict movement and lead to an underestimation of the ROM.
- Ignoring Pain: Pushing a patient beyond their pain tolerance can result in injury and inaccurate measurements.
- Failing to Perform Multiple Measurements: Taking only one measurement increases the risk of error.
- Lack of Standardization: Lack of standardized procedures across clinicians can lead to inconsistencies in measurements and interpretations.
By diligently avoiding these errors, clinicians can ensure more accurate and meaningful goniometric assessment results.
Q 8. How do you handle a patient with pain or discomfort during goniometry?
Patient comfort is paramount during goniometry. If a patient expresses pain or discomfort, immediately stop the measurement. The key is to proceed slowly and gently, explaining each step of the process. We need to identify the source of the pain – is it muscular, articular, or due to the positioning? We might need to adjust the patient’s position, using pillows or supports to ensure proper alignment and reduce strain. In some cases, we may need to modify the measurement technique to avoid exacerbating the pain. For example, if pain is limiting range of motion in the knee, we might utilize a different goniometer placement or modify the patient’s posture to reduce the discomfort while still obtaining useful data. Always communicate with the patient; encourage them to verbally signal any discomfort. If pain persists despite adjustments, the examination might need to be postponed, and the cause of pain investigated further.
Q 9. How do you interpret goniometric measurements in relation to normal values?
Interpreting goniometric measurements requires comparing the obtained values to established normative data. These norms vary depending on factors such as age, gender, and activity level. A reliable source for these values is crucial. Significant deviations from the normative range (generally more than 10-15 degrees depending on the joint) can suggest limitations in joint mobility. For instance, a 25-year-old male presenting with a knee flexion range of 100 degrees when the normal range is 135-145 degrees suggests a potential impairment. However, it’s crucial to consider the patient’s overall clinical presentation and medical history. A seemingly low range of motion might be normal for an individual with pre-existing conditions or past injuries. It’s never just about the numbers; context is key.
Q 10. Explain the difference between active and passive range of motion.
Active range of motion (AROM) refers to the movement a patient can perform independently, while passive range of motion (PROM) is the movement achieved by the examiner when the patient is relaxed and offers no resistance. The difference highlights the patient’s ability to actively control the joint compared to the potential range present in the absence of muscular limitations. For example, a patient might have an AROM of 90 degrees of knee flexion due to hamstring tightness, but a PROM of 120 degrees when the examiner moves the leg passively. This disparity indicates muscle weakness or tightness limiting active movement. Both AROM and PROM are important for assessing the extent of impairment and guiding treatment strategies.
Q 11. How do you assess end-feel during range of motion testing?
Assessing end-feel involves the examiner’s palpation of the resistance felt at the end of the passive range of motion. It’s crucial to feel the quality of the resistance, not just the limitation in movement. The assessment should be conducted gently and smoothly to avoid misinterpretations. It involves a systematic approach: I first move the joint through its full passive range and then gently apply a slight overpressure to note the resistance. The quality and character of this resistance are described using specific terms such as normal, abnormal, or empty. I always document both the range and the quality of the end-feel, describing it with terminology such as firm, soft, hard, or bony.
Q 12. Describe the various types of end-feels and their significance.
Several types of end-feels exist, each indicating different underlying conditions.
- Normal end-feels: These include bony (hard, abrupt stop, e.g., elbow extension), soft tissue approximation (soft, yielding stop, e.g., knee flexion), and capsular (firm, springy stop, e.g., shoulder external rotation).
- Abnormal end-feels: These indicate pathology. Examples include muscle spasm (sudden, abrupt stop with muscle guarding), springy block (rebound effect due to internal derangement, e.g., meniscus tear), empty (pain prevents the completion of the ROM), and boggy (soft, spongy, often indicative of edema).
Q 13. How does goniometry help in the diagnosis and treatment planning?
Goniometry plays a vital role in diagnosis and treatment planning. It provides objective data on joint mobility, quantifying impairments. This objective data is used to formulate a diagnosis and create a tailored treatment plan. For instance, a patient with limited shoulder abduction may receive targeted physical therapy exercises to improve range of motion based on the degree of limitation identified through goniometry. Goniometry is used to set measurable goals for treatment, such as increasing shoulder abduction by 20 degrees in four weeks. It helps monitor the treatment’s effectiveness. Repeated measurements show progress or identify areas requiring adjustment in the treatment plan.
Q 14. Explain how goniometry contributes to the overall rehabilitation process.
Goniometry is integral to the rehabilitation process. It establishes a baseline of the patient’s joint mobility before initiating interventions. This baseline allows for monitoring progress and measuring the effectiveness of treatment. It guides exercise prescription by providing data on specific areas needing improvement. Goniometry helps to identify limitations, which helps in crafting specific exercise programs targeting those areas. Progress tracking via repeated goniometric measurements provides motivation and shows the patient tangible evidence of their improvement. Finally, it’s a crucial tool in evaluating the overall outcome of the rehabilitation process and determining whether the goals have been met. For example, measuring improvements in wrist flexion post-surgery quantifies successful recovery.
Q 15. What are the limitations of goniometry as a diagnostic tool?
Goniometry, while a valuable tool for measuring joint range of motion (ROM), has limitations. It provides a static measurement at a single point in time and doesn’t account for the dynamic complexities of movement. For instance, it doesn’t assess muscle strength, joint stability, or the quality of movement. A goniometer reading of 100 degrees of knee flexion doesn’t tell us if that flexion is achieved smoothly or with pain and compensation. Furthermore, patient cooperation is crucial; pain, fear, or lack of understanding can significantly affect the accuracy of the measurement. Finally, the measurement is highly dependent on the skill and experience of the examiner, leading to potential inter-rater variability.
Think of it like measuring the height of a tree with a tape measure; it tells you how tall the tree is, but it doesn’t tell you about the health of the tree, the condition of its branches, or if it’s leaning. Similarly, goniometry gives us a numerical value for ROM, but it’s just one piece of a much larger clinical picture.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you incorporate goniometry into a comprehensive patient assessment?
Goniometry is just one component of a comprehensive patient assessment. It should be integrated with other assessment methods, such as observation of functional movements, palpation for muscle tone and joint play, and thorough patient history. For example, a patient reports difficulty climbing stairs. Observation might reveal a limp. Goniometry would then quantify the limitations in hip flexion and knee extension. Palpation might reveal tight hamstring muscles. This integrated approach helps identify the underlying cause of the movement limitation, leading to a more accurate diagnosis and effective treatment plan. A solely goniometric assessment would be incomplete and potentially misleading.
- Patient History: Understanding the onset, duration, and character of symptoms provides context for the goniometric findings.
- Observation: Watching the patient perform functional activities (e.g., walking, reaching) reveals movement patterns and compensations.
- Palpation: Assessing muscle tone, joint integrity, and presence of tenderness adds to the overall picture.
- Goniometry: Quantifies the ROM limitations and provides objective data.
Q 17. Discuss the importance of proper patient positioning during goniometric measurements.
Proper patient positioning is critical for accurate goniometric measurements. Inconsistent positioning introduces significant error. The patient should be relaxed and positioned so the joint being measured is in a neutral position and the body segments being aligned with the axes of the goniometer. For instance, measuring knee flexion requires the patient to lie supine with their leg extended and the hip in neutral rotation. Any deviation from this could influence the result. Similarly, for shoulder abduction, the patient’s trunk must remain upright and the shoulder blades must be stabilized to avoid scapular compensation. Landmarks for the goniometer must be identified accurately; incorrect landmark selection can lead to a substantial error in measurements.
Imagine trying to measure the angle of a triangle if its sides are not properly aligned. The same principle applies to goniometry; precise positioning ensures accurate measurements.
Q 18. How do you ensure inter-rater reliability when using goniometry?
Ensuring inter-rater reliability—meaning consistent results among different examiners—is crucial for goniometry. This involves standardization of procedures. Examiners should receive thorough training on proper techniques, including patient positioning, landmark identification, and goniometer placement. Using a standardized protocol helps reduce variations in technique and improves consistency among clinicians. Regular calibration of goniometers and practice with each other assessing the same patients are essential for improving inter-rater reliability. For example, before starting a study, the research team could perform several test measurements on the same patients to establish a baseline level of agreement between assessors. This helps identify any inconsistencies early and allows for adjustments in technique before the study is in full swing.
In clinical practice, regular internal quality checks and peer reviews can enhance the reliability of assessments. The adoption of a universally accepted protocol also ensures better inter-rater reliability across different healthcare settings.
Q 19. Describe the use of goniometry in specific joint assessments (e.g., knee, hip, elbow).
Goniometry’s application varies across joints. For the knee, we measure flexion and extension. For the hip, we assess flexion, extension, abduction, adduction, internal and external rotation. For the elbow, flexion and extension are primary. Each joint has specific anatomical landmarks used for alignment and measurement. For example, the lateral epicondyle and the styloid process of the radius are key landmarks for measuring elbow flexion and extension. The use of anatomical landmarks is crucial in maintaining consistency and accuracy across different assessors. Different axes of rotation are used according to the joint being assessed and the movement being measured.
- Knee: Flexion (0-140°), Extension (0°)
- Hip: Flexion (0-120°), Extension (0-30°), Abduction (0-45°), Adduction (0-30°), Internal Rotation (0-45°), External Rotation (0-45°)
- Elbow: Flexion (0-150°), Extension (0°)
Note: These are approximate ranges; normal values vary slightly with age, gender, and individual variation.
Q 20. How do you adapt goniometry techniques for patients with specific conditions (e.g., arthritis, fractures)?
Adapting goniometry techniques for patients with specific conditions requires careful consideration. With arthritis, pain may limit the patient’s ability to achieve full ROM. In such cases, gentle movements are necessary, and the assessment should be performed with care to avoid causing further discomfort. The examiner should document any pain experienced by the patient during the assessment. With fractures, the injured area is protected, and measurements are adjusted accordingly; sometimes, measuring ROM might not even be advisable in the immediate post-fracture phase. We focus on other methods of assessing progress, such as observing any edema or signs of inflammation.
For patients with limited ROM due to pain or immobility, we might focus on measuring the amount of pain associated with different ranges of movement rather than focusing solely on the absolute ROM values. Modifying positions, using alternative measurement techniques, or focusing on functional ROM might also be considered.
Q 21. Explain the concept of capsular pattern in joint ROM limitations.
A capsular pattern refers to a characteristic pattern of limited ROM in a joint that is consistent with restriction of the joint capsule itself. It’s not a random limitation but rather a specific pattern that helps determine the structures involved. For example, the classic capsular pattern for the knee is limited flexion greater than extension; this suggests a restriction of the posterior aspect of the knee joint capsule. Each joint has a typical capsular pattern; deviations from this pattern suggest other issues, such as ligamentous involvement or muscle contractures. Understanding capsular patterns helps to differentiate between intrinsic joint problems (e.g., arthritis) and other causes of ROM limitation.
Identifying the capsular pattern is crucial for making a differential diagnosis. For example, if a patient presents with limited knee flexion and extension but the limitation in extension is much greater than the limitation in flexion, it is less likely to be a capsular pattern and might suggest other issues, such as a ligamentous restriction or muscular contracture.
Q 22. How can goniometry data be used for progress tracking and treatment outcomes?
Goniometry, the measurement of joint angles, is crucial for tracking progress and evaluating treatment outcomes. By repeatedly measuring a patient’s range of motion (ROM) at specific joints, we can objectively monitor improvements or deteriorations over time. This allows us to tailor interventions and assess the effectiveness of therapies.
For example, a patient recovering from a knee injury might have their ROM measured initially, then weekly, using a goniometer. If their flexion (bending) increases from 90 degrees to 110 degrees over several weeks, it indicates positive progress. Conversely, a lack of improvement or a decrease in ROM might necessitate a change in the treatment plan.
Data is often charted, allowing for visual representation of changes over time. This visual data aids communication with the patient and other healthcare professionals, clearly demonstrating the effectiveness of treatment and progress toward established goals.
Q 23. What software or technology are you familiar with for recording and analyzing goniometry data?
I’m proficient with several methods for recording and analyzing goniometry data. This includes using both traditional manual goniometers and digital goniometers, which often interface with software for data storage and analysis.
I have experience with software packages that allow for direct input of goniometry measurements, automated calculation of ROM, and the generation of comprehensive reports. These typically offer features like patient databases, customizable reports, and the ability to graph changes in ROM over time. Furthermore, some newer electronic goniometers offer wireless data transmission, reducing manual data entry and increasing efficiency.
In addition to dedicated goniometry software, I have used spreadsheets (like Excel) for data organization and basic analysis when more sophisticated software wasn’t immediately available, but such programs do not offer the same level of data management or visual capabilities as specialized goniometry software.
Q 24. How do you maintain and calibrate your goniometers?
Maintaining and calibrating goniometers is vital for accurate measurements. Manual goniometers should be regularly inspected for damage to the arms or protractor. Any looseness in the joints needs to be addressed to maintain accuracy. Calibration involves checking the zero point of the goniometer against a known flat surface. It’s crucial that the arms lie flat against the anatomical landmarks to avoid measurement errors.
Digital goniometers often require calibration through built-in routines that should be performed per the manufacturer’s instructions, generally involving the measurement of a known angle. Regular checks of battery life and sensor performance are also necessary for these devices.
Proper maintenance and calibration procedures are documented and followed diligently to ensure the reliability and validity of the goniometric data collected.
Q 25. Describe your experience using goniometry in different patient populations.
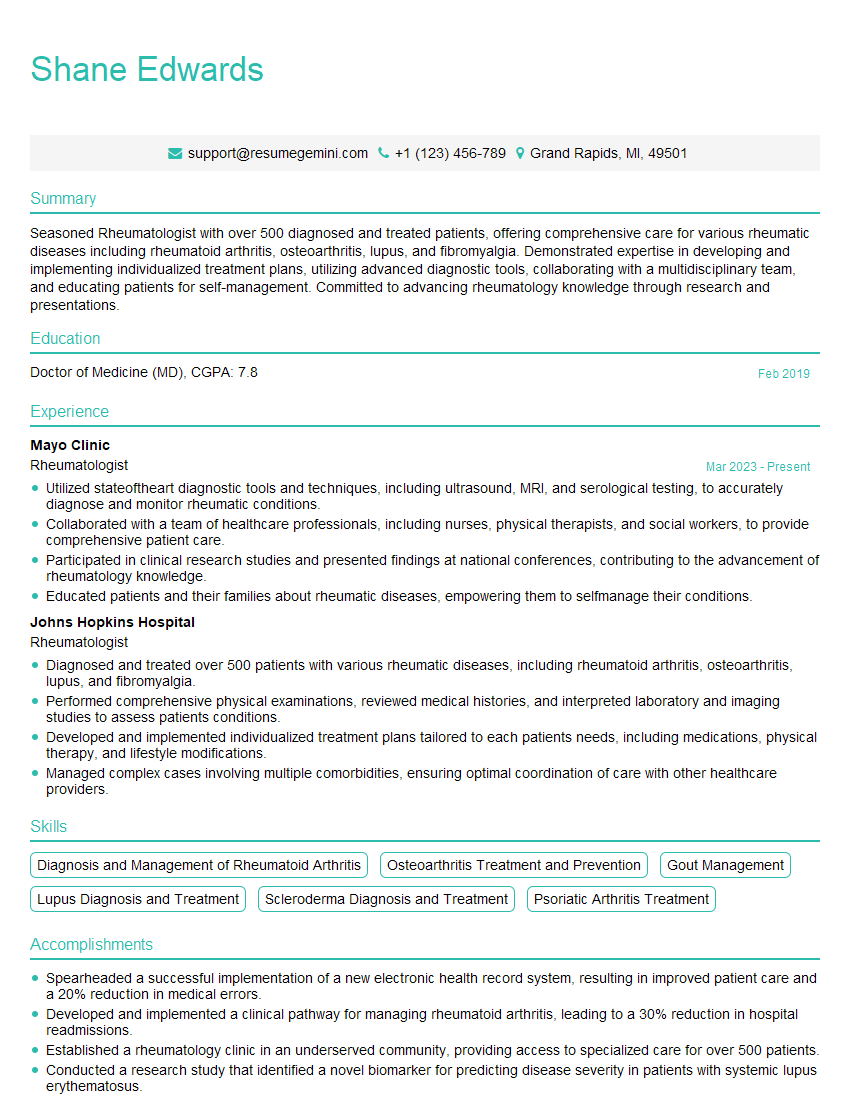
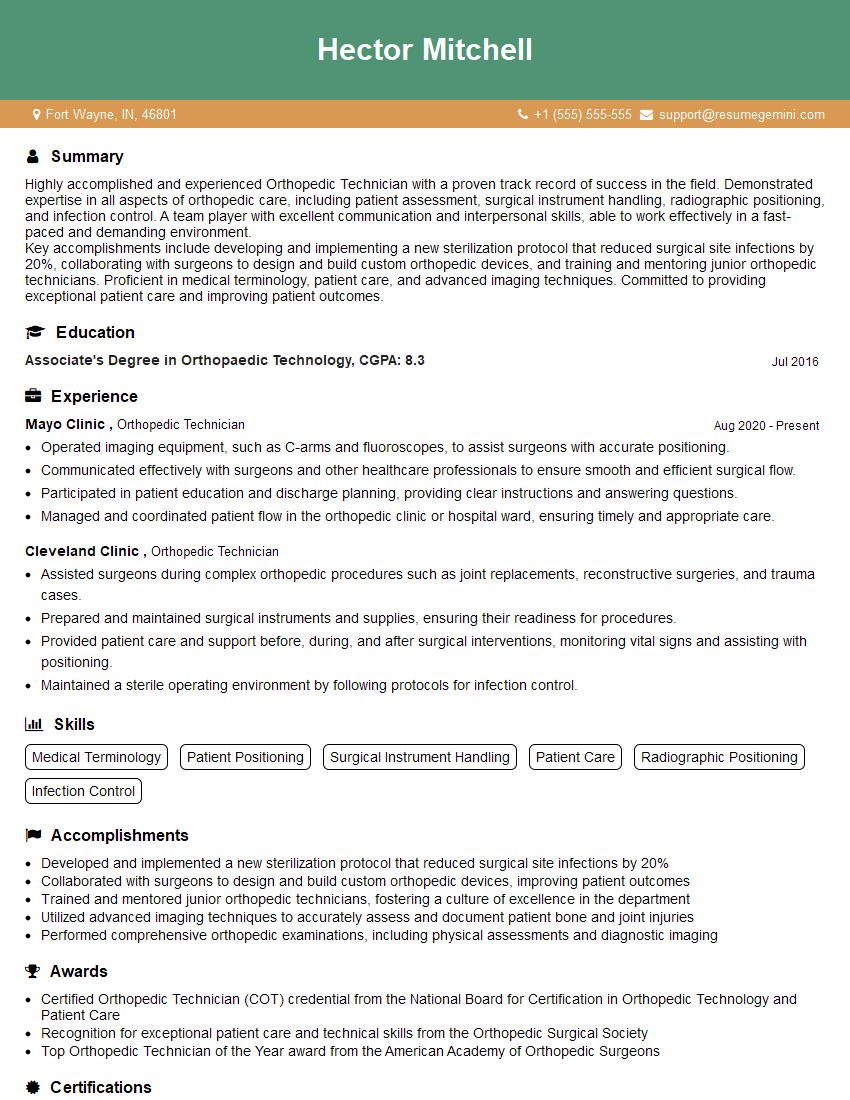
My experience with goniometry spans various patient populations, including those with musculoskeletal injuries, neurological conditions, and post-surgical rehabilitation needs. For instance, I’ve used goniometry extensively with patients recovering from strokes to assess their range of motion in affected limbs, tracking progress and adjusting physiotherapy accordingly. In orthopedic settings, I’ve used goniometry to monitor the recovery of patients after knee replacements, shoulder surgeries, or other joint procedures.
I’ve also worked with patients with rheumatoid arthritis, where goniometry helps track disease progression and the effectiveness of treatments aimed at preserving joint function. My experience across these diverse patient populations highlights the versatility and importance of goniometry in assessing and managing diverse conditions.
Q 26. What are some alternative methods to goniometry for assessing joint mobility?
While goniometry is a valuable tool, other methods exist for assessing joint mobility. These include:
- Visual observation: A skilled clinician can often visually estimate joint range of motion, although this is subjective and less precise than goniometry.
- Inclinometry: This electronic device provides objective measurement of joint angles, often used in research settings.
- Photography and video analysis: Advanced techniques like video analysis can objectively quantify movement, though equipment and expertise are often more demanding.
- Patient self-report: While not as precise, patient-reported outcome measures can provide valuable insights into functional limitations.
The choice of method depends on the clinical context, the availability of resources, and the level of precision needed. Often, a combination of methods is beneficial to obtain a comprehensive assessment.
Q 27. How do you communicate goniometric findings to other healthcare professionals?
Communicating goniometric findings effectively involves clear, concise documentation and verbal reporting. I always use standardized terminology and units of measurement (degrees). Written reports include the date, specific joints measured, ROM values (both active and passive), and comparisons to previous measurements whenever available. I also include any observations of pain, muscle spasms, or other limitations impacting ROM.
When communicating with other professionals, I use clear and non-technical language where appropriate, while ensuring the accuracy of the data presented. For example, instead of saying “Patient demonstrates limited flexion,” I might say, “Patient’s knee flexion is currently 100 degrees, significantly below the expected 135 degrees for their age and activity level.”
Visual aids, such as graphs or charts showing trends in ROM over time, enhance understanding and facilitate informed decision-making.
Q 28. Describe a situation where goniometric measurement was crucial in determining a diagnosis or treatment plan.
A patient presented with persistent shoulder pain following a fall. Initial X-rays were unremarkable. However, goniometric assessment revealed significantly reduced abduction and external rotation compared to the unaffected shoulder. This disparity, coupled with the patient’s reported pain during specific movements, strongly suggested a rotator cuff tear. The goniometric data was crucial in identifying the need for further investigations (MRI) that confirmed the diagnosis and led to appropriate surgical intervention.
In this instance, the objective goniometric measurements helped differentiate between generalized shoulder pain and a more specific diagnosis, guiding the treatment pathway and ultimately leading to improved patient outcomes. Without those precise measurements, the diagnosis might have been delayed or missed entirely.
Key Topics to Learn for Goniometry Interview
- Range of Motion (ROM) Measurement: Understanding different goniometer types, proper positioning techniques, and accurate measurement protocols for various joints.
- Anatomical Landmarks: Mastering the identification and palpation of key bony landmarks necessary for precise goniometric assessments.
- Normal ROM Values: Familiarize yourself with age- and population-specific normative data for joint ROM and interpreting deviations.
- Clinical Applications: Discuss the role of goniometry in diagnosing musculoskeletal disorders, tracking progress in rehabilitation, and evaluating treatment effectiveness.
- Error Reduction Techniques: Understand and be prepared to discuss potential sources of error during goniometric measurements and strategies to minimize them (e.g., patient positioning, consistent measurement techniques).
- Interpreting Goniometric Data: Practice analyzing goniometry results in conjunction with other clinical findings to form a comprehensive assessment.
- Goniometry in Specific Populations: Consider the unique challenges and considerations for performing goniometry on pediatric, geriatric, or special needs populations.
- Documentation and Reporting: Understand appropriate methods for recording and reporting goniometric data in a clear and concise manner.
Next Steps
Mastering goniometry is crucial for advancing your career in healthcare professions requiring precise musculoskeletal assessments. A strong understanding of goniometry demonstrates clinical competency and attention to detail, highly valued by employers. To significantly boost your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. We strongly recommend using ResumeGemini, a trusted resource for building professional resumes. ResumeGemini provides examples of resumes tailored to Goniometry professionals, enabling you to showcase your qualifications in the best possible light. Take the next step towards your dream career—build a powerful resume today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good