The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to First Aid and Emergency Medical Response interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in First Aid and Emergency Medical Response Interview
Q 1. Describe the steps you would take to control severe bleeding.
Controlling severe bleeding is a critical first aid skill that can be lifesaving. The key is to apply direct pressure to the wound, elevate the injured limb (if possible), and seek immediate medical attention.
- Direct Pressure: This is the most important step. Use a clean cloth or dressing and apply firm, consistent pressure directly to the wound. Don’t remove the cloth even if it becomes soaked with blood; add more layers on top. Imagine you’re trying to stop a water leak with a sponge – you need to maintain pressure to be effective.
- Elevation: If the bleeding is from an arm or leg, elevate the injured limb above the heart. This helps to slow the flow of blood by reducing blood pressure in that area. Think of it like tilting a container of water – the water flows more slowly when it’s tilted.
- Pressure Points: As a last resort, if direct pressure and elevation aren’t enough, you can apply pressure to pressure points. These are locations where major arteries are close to the surface of the skin, allowing you to compress the artery and reduce blood flow. However, this should only be done if direct pressure isn’t effective and requires specialized knowledge.
- Seek Medical Attention: Call emergency services immediately. Severe bleeding requires professional medical care to ensure the wound is properly cleaned and closed, and to assess for any underlying injuries or complications.
Example: Imagine someone has a deep laceration on their leg from a fall. You would immediately apply direct pressure to the wound with a clean cloth, elevate their leg, and then call emergency medical services.
Q 2. Explain the difference between stable and unstable side positioning.
Stable and unstable side positioning both involve placing an unconscious patient on their side to help maintain an open airway and prevent choking on vomit or other secretions. However, the key difference lies in the level of spinal stabilization.
- Stable Side Positioning: Used when there is no suspected spinal injury. The patient is gently rolled onto their side, creating a recovery position. This ensures that any fluids can drain and the airway remains clear. Imagine tilting a cup to pour out any excess water.
- Unstable Side Positioning: Used when a spinal injury is suspected. This requires specialized techniques, and often involves stabilizing the spine before carefully moving the patient to a side. This aims to prevent further injury to the spine. Think of it as carefully moving a delicate object.
In essence, stable side positioning is a simple maneuver focused on airway management. Unstable side positioning incorporates spinal precautions and necessitates additional training and expertise. Improper handling in suspected spinal injury cases can cause irreversible harm.
Q 3. How would you assess a patient’s airway, breathing, and circulation (ABCs)?
Assessing a patient’s ABCs – Airway, Breathing, and Circulation – is the cornerstone of initial trauma assessment. It’s a systematic approach to quickly identify life-threatening conditions.
- Airway: Check if the airway is open and clear. Look for signs of obstruction like swelling, blood, or foreign bodies. Listen for abnormal breathing sounds. Feel for air movement at the mouth and nose. If obstructed, gently tilt the head and lift the chin (unless a spinal injury is suspected).
- Breathing: Assess the rate, depth, and quality of breathing. Observe the chest rise and fall. Look for signs of respiratory distress like gasping, cyanosis (blue discoloration of skin), or abnormal breathing patterns.
- Circulation: Check the pulse for rate and strength. Assess skin color for pallor (pale), cyanosis, or flushed appearance. Check for bleeding. Assess for capillary refill (press on a fingernail and see how quickly it returns to normal color).
This assessment should be done quickly and efficiently. Remember the mnemonic ABC; prioritize immediate life-threatening issues and address them accordingly. For instance, an obstructed airway must be cleared before addressing other concerns.
Q 4. What are the signs and symptoms of a stroke?
Stroke is a medical emergency caused by a disruption of blood flow to the brain. Recognizing the signs and symptoms quickly is crucial for timely treatment. The acronym FAST is helpful in remembering key symptoms:
- F – Face: Ask the person to smile. Does one side of their face droop?
- A – Arms: Ask the person to raise both arms. Does one arm drift downward?
- S – Speech: Ask the person to repeat a simple sentence. Is their speech slurred or strange?
- T – Time: If you observe any of these signs, call emergency services immediately. Time is brain!
Other symptoms can include sudden numbness or weakness, especially on one side of the body; confusion; trouble seeing; sudden severe headache with no known cause; dizziness or loss of balance and coordination. It’s important to remember that stroke symptoms can vary; any sudden neurological change warrants immediate medical attention.
Q 5. How do you treat a suspected spinal injury?
Suspected spinal injury requires utmost caution. The goal is to prevent further damage to the spinal cord.
- Stabilization: Do not move the patient unless absolutely necessary. If they must be moved, it should be done by trained professionals using a spinal board and collar. Imagine the spine as a delicate stack of building blocks; any jarring movement could cause further damage.
- Manual Stabilization: If moving is unavoidable before professional help arrives, carefully support the head and neck, keeping them aligned with the spine. Avoid any twisting or jerking movements. This requires proper training and shouldn’t be attempted without it.
- Monitoring: Monitor the patient’s breathing, level of consciousness, and any changes in their condition. Record the time of injury and any symptoms observed.
Improper handling of a suspected spinal injury can lead to permanent paralysis or death. Prioritize safety and wait for trained emergency medical personnel to handle the situation.
Q 6. Describe the proper procedure for using an AED.
Using an AED (Automated External Defibrillator) can be lifesaving in cases of sudden cardiac arrest. Follow these steps carefully:
- Turn on the AED: The device will give clear, voice-prompted instructions.
- Attach Pads: Apply the adhesive pads to the patient’s bare chest, as indicated on the pads themselves.
- Analyze: Allow the AED to analyze the patient’s heart rhythm.
- Shock (if advised): If a shock is advised, ensure no one is touching the patient and deliver the shock by pressing the button.
- CPR: After the shock (or if no shock is advised), immediately begin CPR (chest compressions and rescue breaths) as instructed by the AED.
- Continue: Continue CPR and follow the AED’s instructions until emergency medical services arrive.
It’s critical to follow the AED’s instructions precisely. These devices are designed to be user-friendly, even for individuals with minimal medical training. However, proper training is recommended for effective and confident use.
Q 7. How would you manage a patient experiencing a seizure?
Managing a patient experiencing a seizure requires a focus on safety and preventing injury.
- Protect from Injury: Move any nearby objects that could cause harm. Do not restrain the person, but gently guide them to the ground to prevent falls or impact injuries. Think of cushioning their fall with pillows or clothing.
- Airway: Once the seizure has subsided, check their airway and ensure clear breathing.
- Positioning: Turn the patient onto their side to prevent choking on vomit or secretions (unless a spinal injury is suspected).
- Monitor: Monitor vital signs and be prepared to assist with breathing if necessary.
- Post-ictal State: After the seizure, the individual may be drowsy, confused, or disoriented (post-ictal state). Provide comfort and reassurance until they regain consciousness.
- Seek Medical Attention: If this is their first seizure, if the seizure lasts longer than 5 minutes, or if there are repeated seizures, seek immediate medical help.
Remember to stay calm and provide a safe environment. Avoid putting anything in their mouth and do not attempt to restrain their movements during the seizure.
Q 8. Explain how to treat a diabetic emergency.
Treating a diabetic emergency, often a hypoglycemic episode (low blood sugar) or hyperglycemic episode (high blood sugar), requires swift action. Hypoglycemia is far more common and life-threatening in the short term.
Hypoglycemic Emergency (Low Blood Sugar): Symptoms include confusion, dizziness, sweating, shakiness, rapid heartbeat, and even loss of consciousness. Treatment focuses on rapidly raising blood glucose levels. If the patient is conscious and can swallow, give them 15-20 grams of fast-acting carbohydrates, such as glucose tablets, honey, or regular soda (avoid diet soda). Recheck blood glucose levels in 15 minutes. Repeat if still low. If the patient is unconscious, administer glucagon as trained and call emergency medical services (EMS) immediately.
Hyperglycemic Emergency (High Blood Sugar): This typically develops more slowly and symptoms include excessive thirst, frequent urination, blurred vision, fatigue, and fruity-smelling breath (due to ketones). Treatment requires medical attention, as hyperglycemia can lead to diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), both serious complications. The patient should be monitored closely and transported to the hospital for appropriate treatment. Never attempt to treat this at home without medical guidance.
Important Note: Always call EMS if you are unsure about the severity of a diabetic emergency or if the patient’s condition doesn’t improve after treatment.
Q 9. What are the signs and symptoms of anaphylaxis?
Anaphylaxis is a severe, life-threatening allergic reaction. It’s a rapid, systemic response to an allergen, often something the person has been exposed to before.
Signs and Symptoms: These can appear suddenly and rapidly progress. Common signs include:
- Swelling of the face, lips, tongue, or throat (angioedema)
- Difficulty breathing or wheezing
- Hives (urticaria) or widespread rash
- Lightheadedness or dizziness
- Rapid, weak pulse
- Nausea, vomiting, or abdominal cramps
- Loss of consciousness
The presence of two or more of these symptoms, especially involving the respiratory or cardiovascular systems, strongly suggests anaphylaxis. Even one symptom, especially respiratory distress, warrants immediate treatment.
Q 10. How would you treat a patient with a suspected heart attack?
Suspected heart attack (myocardial infarction) requires immediate action. Time is critical as heart muscle damage increases with each passing minute.
Treatment:
- Call EMS immediately (911 or your local emergency number). This is the most crucial step.
- Have the patient rest and sit or lie down. Avoid unnecessary exertion.
- Administer oxygen if available and trained to do so.
- Assess vital signs (pulse, breathing, blood pressure) as able.
- If the patient is conscious and has a prescription for nitroglycerin, and you are authorized to assist, help them take it as prescribed.
- Be prepared to perform CPR if the patient becomes unresponsive and stops breathing.
Important: Do not attempt to drive the patient to the hospital. EMS provides advanced life support and rapid transport to a suitable facility for definitive care.
Q 11. Describe the different types of shock and their management.
Shock is a life-threatening condition where the body’s tissues and organs aren’t getting enough oxygenated blood. There are several types:
- Hypovolemic Shock: Caused by significant blood or fluid loss (e.g., severe bleeding, dehydration). Management: Control bleeding, provide fluids (if trained), and maintain body temperature.
- Cardiogenic Shock: The heart isn’t pumping effectively (e.g., heart attack, heart failure). Management: Advanced medical intervention is crucial. Immediate EMS call.
- Anaphylactic Shock: An allergic reaction (discussed earlier). Management: Epinephrine injection (if trained and available), airway management, and EMS.
- Septic Shock: A severe infection. Management: Requires immediate medical attention; antibiotics are necessary.
- Neurogenic Shock: Damage to the nervous system (e.g., spinal cord injury). Management: Maintaining airway, stabilizing the spine (if applicable), and advanced medical care.
General Management of Shock: Regardless of the type, ensure the patient is lying flat with their legs elevated slightly. Maintain airway, provide oxygen if available, and control any external bleeding. Keep them warm and monitor their vital signs. EMS should be called immediately for all types of shock.
Q 12. How would you handle a situation with a combative patient?
Dealing with a combative patient requires a calm and measured approach. Your priority is safety—yours and the patient’s.
Strategies:
- Maintain a safe distance: Avoid getting too close, and be aware of your surroundings.
- Speak calmly and reassuringly: Use a calm, clear voice and attempt to de-escalate the situation.
- Identify the cause of combativeness: Is it pain, confusion, intoxication, mental illness, or something else?
- If possible, get help: Call for additional assistance from security or law enforcement as needed.
- Avoid physical restraints unless absolutely necessary and you are trained in appropriate techniques. Improper restraint can lead to injury.
- Prioritize patient safety: If the situation cannot be de-escalated, prioritize ensuring no one is injured and call for trained emergency personnel to intervene.
Remember: Your safety is paramount. If you feel unsafe, prioritize removing yourself from the situation and getting help.
Q 13. What are your skills in splinting and immobilizing injuries?
My splinting and immobilization skills include the application of various types of splints—rigid, soft, and traction splints—to stabilize fractures and dislocations of the extremities. I am proficient in the use of slings and swaths to support injuries to the upper extremities and am trained in the proper techniques for spinal immobilization using cervical collars and backboards, following established protocols. I understand the importance of proper padding to prevent further injury during splinting. My training includes practical application and assessment of neurovascular status before and after splinting, ensuring that circulation and nerve function are not compromised. I am aware of the limitations of my training and would always defer to medical professionals for definitive diagnosis and treatment.
Q 14. Explain the importance of maintaining a sterile environment during wound care.
Maintaining a sterile environment during wound care is crucial to prevent infection. Infection can lead to significant complications, including delayed healing, sepsis (a life-threatening condition), and even death.
Sterile Technique: This involves preventing the introduction of microorganisms into the wound. Key aspects include:
- Hand hygiene: Thorough handwashing with soap and water or using an alcohol-based hand rub before and after wound care.
- Use of sterile gloves, dressings, and instruments: These items are crucial to prevent contamination.
- Proper cleaning technique: Cleaning the wound with sterile saline or an appropriate antiseptic solution, working from the center outward.
- Appropriate wound closure techniques: Using sterile materials and adhering to proper procedures if closure is necessary (medical professionals usually do this).
- Disposal of contaminated materials: Properly disposing of used materials to prevent the spread of infection.
Real-World Example: Imagine cleaning a deep laceration without sterile gloves and using a dirty rag. This could introduce bacteria directly into the wound, significantly increasing the risk of infection. Proper sterile technique minimizes this risk and promotes optimal healing.
Q 15. Describe your experience with oxygen administration techniques.
Oxygen administration is crucial in emergency situations where a patient is experiencing respiratory distress or hypoxia (low blood oxygen levels). My experience encompasses various techniques, ensuring the safety and efficacy of oxygen delivery. This includes using:
Nasal Cannula: A simple, low-flow method delivering 1-6 liters per minute. I’ve used this extensively for patients with mild respiratory compromise, ensuring comfort and adequate oxygenation. For instance, I used a nasal cannula on a patient recovering from a minor asthma attack, carefully monitoring their oxygen saturation levels.
Simple Face Mask: Provides a higher flow rate (5-10 liters per minute) and a more concentrated delivery. I find this useful for patients requiring increased oxygen support, such as those experiencing moderate shortness of breath. During a recent traffic accident, I applied a simple face mask to a patient with chest trauma until paramedics arrived.
Non-Rebreather Mask: Delivers the highest oxygen concentration possible without intubation, typically around 90%. This is reserved for patients in severe respiratory distress. I’ve used this method in cases of severe trauma or cardiac arrest where maintaining adequate oxygenation is paramount.
Venturi Mask: Allows for precise oxygen delivery at a specific FiO2 (fraction of inspired oxygen). I use this when precise oxygen concentration is crucial, particularly for patients with chronic lung diseases like COPD, to avoid oxygen toxicity.
In each case, I prioritize patient assessment to determine the appropriate method and flow rate, constantly monitoring vital signs like oxygen saturation (SpO2) and respiratory rate. Safety procedures are strictly followed, including checking oxygen tank levels and ensuring proper equipment function.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you prioritize multiple patients with different injuries?
Prioritizing multiple patients involves a systematic approach using triage principles. The goal is to maximize the number of survivors and minimize casualties by addressing the most critical cases first. I utilize the START (Simple Triage and Rapid Treatment) method or a similar system, focusing on these steps:
Rapid Assessment: I quickly assess each patient’s breathing, circulation, and mental status (often referred to as the ABCs – Airway, Breathing, Circulation). I look for obvious signs of life-threatening injuries like severe bleeding, respiratory arrest, or absent pulse.
Categorization: Based on the initial assessment, patients are categorized into priority levels (e.g., immediate, delayed, minimal, expectant). Immediate patients require immediate life-saving interventions (e.g., controlling massive bleeding, opening an airway). Delayed patients have injuries requiring treatment but are not immediately life-threatening. Minimal patients have minor injuries. Expectant patients are unfortunately deemed unlikely to survive given the severity of their injuries.
Continuous Re-evaluation: Conditions can change rapidly. I continuously monitor all patients and reassess their status, adjusting priorities as needed. This is crucial as a patient’s condition could rapidly deteriorate or improve.
For example, imagine a scenario with three patients: one with severe bleeding, one with a broken arm, and one unconscious but breathing. The patient with severe bleeding takes immediate priority, followed by the unconscious patient. The broken arm is treated later. This ensures the most critical patients receive timely attention.
Q 17. Explain your understanding of triage protocols.
Triage protocols are systematic methods for sorting and prioritizing patients based on the urgency of their medical needs. The primary goal is to ensure the most critically injured patients receive prompt treatment while maximizing the number of survivors. Different triage systems exist, but they share common principles.
Rapid Assessment: A quick assessment of vital signs (breathing, pulse, mental status) is crucial for immediate prioritization.
Categorization: Patients are categorized based on their severity, allowing for efficient resource allocation.
Prioritization: Patients are prioritized based on their likelihood of survival and the potential impact of immediate intervention.
Systematization: Triage systems are structured and standardized to ensure consistency across different settings and providers.
Common protocols include START, SALT (Simple Algorithm for Life-Threatening injuries), and others tailored to specific environments (e.g., mass casualty incidents, disaster relief). Understanding these protocols is essential for effective management in high-pressure situations. The key is to act efficiently and systematically to provide the greatest possible benefit to the most patients.
Q 18. What are your skills in intravenous (IV) insertion (if applicable)?
As a certified [mention your certification, e.g., EMT, Paramedic], I am proficient in intravenous (IV) insertion. This is a critical skill allowing for rapid fluid administration, medication delivery, and blood draws. I understand the importance of sterile technique to prevent infection and complications. My training involved:
Venipuncture Techniques: I am adept at locating appropriate veins (typically in the antecubital fossa or hand) and performing venipuncture using various techniques.
Catheter Selection and Insertion: I am proficient in selecting the appropriate catheter size and inserting it smoothly, minimizing patient discomfort.
Fluid and Medication Administration: Following the prescription and maintaining aseptic techniques are essential aspects of post-insertion care.
Complications Management: Recognizing and managing potential complications such as hematoma formation, infiltration, and phlebitis are key parts of my skillset.
Each insertion is documented meticulously, noting the location, catheter size, and any complications. Maintaining asepsis and patient comfort are always top priorities. My competency in this procedure has been demonstrated consistently through practical assessments and real-world applications.
Q 19. Describe your experience with using various medical equipment.
My experience encompasses a wide range of medical equipment, including:
Monitoring Equipment: I am skilled in using ECG monitors, pulse oximeters, blood pressure cuffs, and other devices to assess vital signs. Accurate monitoring is crucial for making informed treatment decisions.
Respiratory Equipment: I’m proficient with bag-valve masks (BVMs), oxygen delivery systems, and other devices used to support respiration. I also have experience using advanced airway management techniques when necessary.
Trauma Equipment: I am familiar with the use of spinal boards, cervical collars, splints, and other equipment used to immobilize injuries and prevent further damage.
Other Equipment: I’m experienced using suction devices, defibrillators, and other life-saving equipment.
I regularly undertake continuing education and training to maintain my proficiency with new and evolving medical technologies. My understanding extends beyond basic operation; I’m knowledgeable about the principles of operation, maintenance, and potential limitations of each device.
Q 20. How do you document patient information accurately and thoroughly?
Accurate and thorough documentation is paramount in patient care. It serves as a legal record, assists in continuity of care, and supports effective communication among healthcare providers. My documentation practices follow these principles:
Timeliness: I record patient information immediately after assessment or intervention, ensuring accuracy and avoiding recall bias.
Objectivity: I focus on factual observations, avoiding subjective interpretations. For instance, instead of ‘patient was in pain,’ I’d record ‘patient reported pain level 8/10 on a numerical pain scale.’
Completeness: My notes include the date, time, patient identifiers, detailed assessment findings, interventions performed, and patient response.
Clarity and Legibility: I use clear, concise language, avoiding abbreviations unless universally understood. My handwriting is legible, or I use electronic documentation systems.
Compliance: I follow all relevant regulations and guidelines for record keeping, ensuring confidentiality and data security.
For example, when documenting an IV insertion, I’d note the time, vein used, catheter size, amount of fluid infused, and any complications encountered. This level of detail ensures clear communication and supports appropriate follow-up care.
Q 21. Explain your knowledge of medical terminology.
Medical terminology is essential for effective communication within the healthcare field. My knowledge encompasses a wide range of terms related to anatomy, physiology, pathology, pharmacology, and procedures. I understand the meaning and application of terms like:
Anatomical Terms: e.g., ‘anterior,’ ‘posterior,’ ‘proximal,’ ‘distal,’ ‘lateral,’ ‘medial’ – crucial for accurately describing injury locations.
Physiological Terms: e.g., ‘tachycardia,’ ‘bradycardia,’ ‘hypotension,’ ‘hypertension,’ ‘hypoxia’ – fundamental to understanding a patient’s physiological state.
Pathological Terms: e.g., ‘fracture,’ ‘laceration,’ ‘contusion,’ ‘infarction’ – essential for documenting and understanding injury types.
Pharmacological Terms: e.g., ‘analgesic,’ ‘antibiotic,’ ‘antihypertensive’ – necessary for understanding medication administration and effects.
Procedure-Specific Terms: e.g., ‘intubation,’ ‘defibrillation,’ ‘CPR’ – critical for documenting interventions.
My understanding allows me to read and interpret medical charts, accurately communicate with other healthcare professionals, and provide the best possible patient care. Continued learning and access to medical dictionaries ensures my terminology remains up-to-date and comprehensive.
Q 22. How do you maintain confidentiality and patient privacy?
Maintaining confidentiality and patient privacy is paramount in emergency medical response. It’s not just about following regulations like HIPAA (in the US), but about building trust with patients who are often vulnerable and distressed. This involves several key strategies:
- Strict adherence to HIPAA regulations (or equivalent in your region): This includes only accessing information relevant to the emergency, securely storing patient data, and limiting access to authorized personnel only.
- Never discussing patient information with unauthorized individuals: This includes family members, friends, or even colleagues who are not directly involved in the patient’s care. If family members inquire, I direct them to the appropriate channels, such as hospital staff or designated representatives.
- Using appropriate methods of communication: I use secure messaging systems and avoid discussing sensitive information in public places or on unsecured devices.
- Properly securing and disposing of patient records: This includes shredding paper records and following established procedures for electronic data disposal.
- Maintaining professional boundaries: It is crucial to avoid any form of personal relationship with patients, even after the emergency is over, to protect both their privacy and my professional integrity.
For example, I once responded to an accident where a patient’s identity was initially unknown. I ensured all information gathered during the emergency care was carefully documented and only shared with the appropriate authorities after their identity was confirmed and consent was obtained to share information with family or legal representatives.
Q 23. Describe a situation where you had to make a critical decision under pressure.
During a multi-vehicle accident, I faced a critical decision. We had multiple patients with varying injuries – some critical, some less so. We were significantly short-staffed, and resources were limited. I had to quickly assess the situation, prioritize patients based on the severity of their injuries (using triage techniques like START), and delegate tasks effectively to the available personnel. One patient, a young child, had a severe head injury and needed immediate attention. While others were seriously injured, their injuries were less immediately life-threatening. I made the difficult decision to immediately prioritize the child, assigning the most skilled team members to stabilize him while simultaneously providing appropriate care to the other patients based on their need. This was a high-pressure situation demanding rapid assessment, strategic resource allocation, and decisive leadership to ensure the best possible outcome for everyone involved.
Q 24. How do you handle stressful situations in an emergency?
Handling stress in emergencies relies on a combination of training, preparation, and self-care. My approach involves:
- Maintaining situational awareness: Staying focused on the immediate tasks and avoiding being overwhelmed by the overall chaos.
- Controlled breathing techniques: Deep, slow breaths help regulate my heart rate and calm my nerves.
- Effective communication: Clearly and concisely communicating with my team members helps maintain order and coordination. This ensures we work cohesively to provide the most efficient and effective response.
- Prioritization: Focusing on what needs to be done first, one step at a time, rather than getting bogged down by the enormity of the situation.
- Post-incident debriefing: Talking through the incident with colleagues helps process emotions and learn from the experience. This is crucial for both mental health and professional growth.
Think of it like a fire: you don’t try to put out the entire blaze at once; you focus on containing the flames and extinguishing them strategically, section by section. In an emergency, it’s a similar process—controlled, methodical actions, and effective teamwork lead to the best results.
Q 25. Describe your teamwork skills in an emergency setting.
Teamwork in emergency settings is essential for effective and efficient patient care. My approach emphasizes:
- Clear communication: I use concise and unambiguous language to convey information to my team, ensuring everyone understands their roles and responsibilities.
- Active listening: Paying close attention to what others are saying and responding appropriately allows me to identify issues and adapt our approach.
- Respectful collaboration: I value the input of all team members, acknowledging individual strengths and expertise. This builds trust and morale, which is crucial during stressful situations.
- Delegation: I efficiently delegate tasks based on team members’ skill sets, ensuring optimal utilization of resources and minimizing workload bottlenecks.
- Conflict resolution: Addressing disagreements constructively, focusing on the patient’s needs above individual preferences.
For example, during a mass casualty incident, I coordinated a team of paramedics, EMTs, and firefighters, effectively delegating tasks based on individual skills, ensuring timely care for all patients. The effective collaboration, stemming from clear communication and trust, ensured the successful management of a complex situation.
Q 26. How do you stay up-to-date with current medical protocols?
Staying current with medical protocols is critical in this field. I use a multi-pronged approach:
- Continuing Medical Education (CME): I actively participate in CME courses, workshops, and conferences to learn about the latest advancements in emergency medical care.
- Professional journals and publications: I regularly read peer-reviewed journals and publications such as The Journal of Emergency Medical Services to stay abreast of new research and evidence-based practices.
- Professional organizations: Membership in organizations like the National Association of Emergency Medical Technicians (NAEMT) provides access to resources, updates, and networking opportunities.
- Online resources and databases: I leverage reputable online platforms offering medical information and updates, while carefully evaluating the source’s credibility.
- Regular review of protocols and guidelines: I ensure my understanding aligns with the latest guidelines issued by relevant governing bodies.
Regularly updating my knowledge is like updating software on a computer. It’s crucial to ensure I’m using the latest and most effective methods to deliver optimal patient care.
Q 27. What are your personal strengths and weaknesses relevant to this role?
My strengths include my strong decision-making skills under pressure, my ability to remain calm and focused in stressful situations, and my excellent teamwork abilities. I’m also highly adaptable, capable of quickly assessing situations and adjusting my approach as needed.
As for weaknesses, I strive to improve my time management skills in particularly hectic situations, ensuring that I consistently prioritize the most critical tasks and allocate time effectively.
While perfection isn’t achievable, ongoing self-reflection and continuous learning help me proactively address potential shortcomings and maintain a high standard of care.
Q 28. What are your salary expectations?
My salary expectations are commensurate with my experience and qualifications in this field, and align with the industry standards for this role. I am open to discussing a competitive compensation package that reflects the value I bring to the organization. I am more interested in a role that offers a challenging and rewarding environment where I can utilize my skills to their full potential and contribute to a team that prioritizes patient care.
Key Topics to Learn for First Aid and Emergency Medical Response Interview
- Primary Assessment: Understanding the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) and its practical application in various emergency scenarios. This includes recognizing and managing life-threatening conditions.
- Secondary Assessment: Performing a systematic head-to-toe examination to identify injuries and collect vital information. Practical application includes documenting findings accurately and prioritizing treatment based on assessment results.
- CPR and AED Use: Mastering the techniques of cardiopulmonary resuscitation (CPR) for adults, children, and infants, including proper hand placement, compression depth, and rescue breaths. Understanding AED operation and troubleshooting common issues.
- Bleeding Control: Different types of bleeding and appropriate control methods (direct pressure, elevation, tourniquet application). Understanding the limitations and potential complications of each technique.
- Shock Management: Recognizing the signs and symptoms of shock and implementing appropriate management strategies, including maintaining body temperature and positioning the patient.
- Trauma Management: Understanding different types of trauma (blunt force, penetrating) and initial assessment and management procedures. This includes spinal immobilization techniques and recognizing potential complications.
- Emergency Medical Services (EMS) System: Knowing the roles and responsibilities of different members of the EMS system (dispatchers, EMTs, paramedics) and the process of requesting emergency assistance. Understanding patient handoff procedures.
- Legal and Ethical Considerations: Understanding the legal aspects of providing first aid and emergency medical response, including consent, confidentiality, and reporting requirements. Ethical decision-making in challenging situations.
- Specific Emergency Situations: Preparation for questions about managing specific emergencies such as strokes, heart attacks, seizures, and allergic reactions. Understanding the signs, symptoms, and appropriate interventions for each condition.
- Teamwork and Communication: Understanding the importance of effective communication and teamwork within an emergency response team. Practicing clear and concise reporting of patient information.
Next Steps
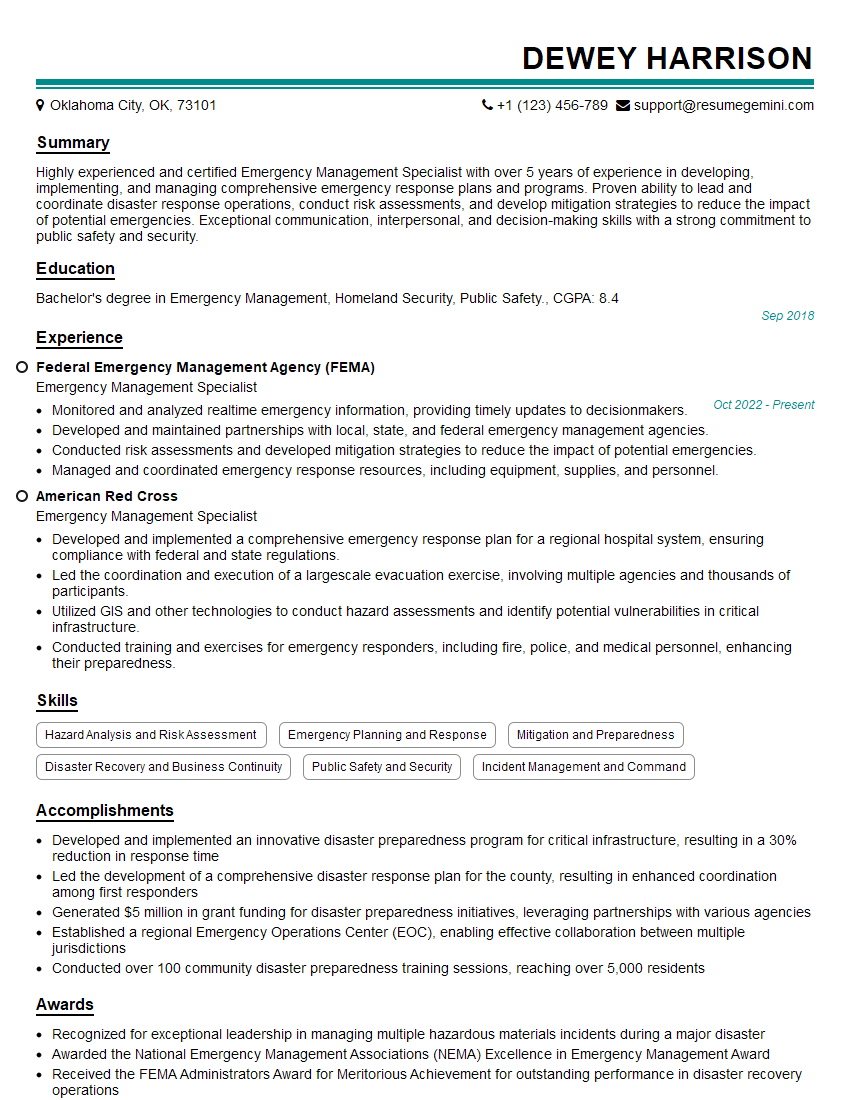
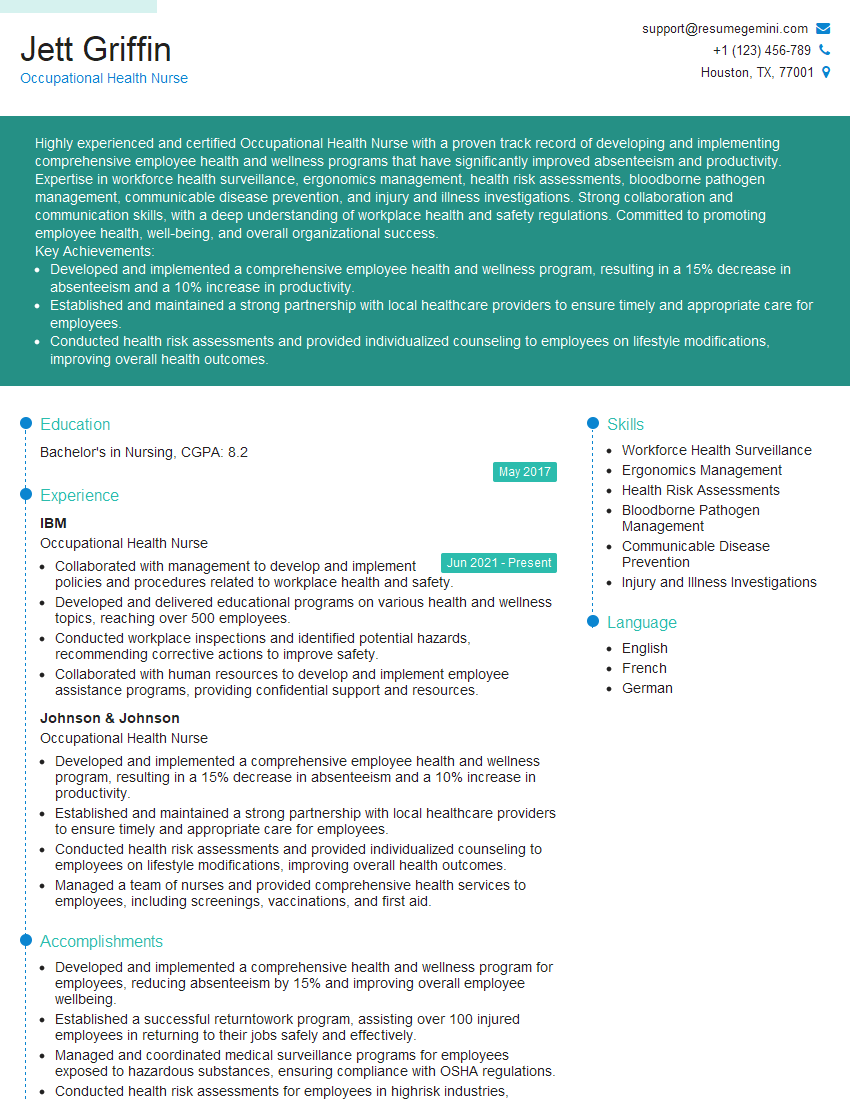
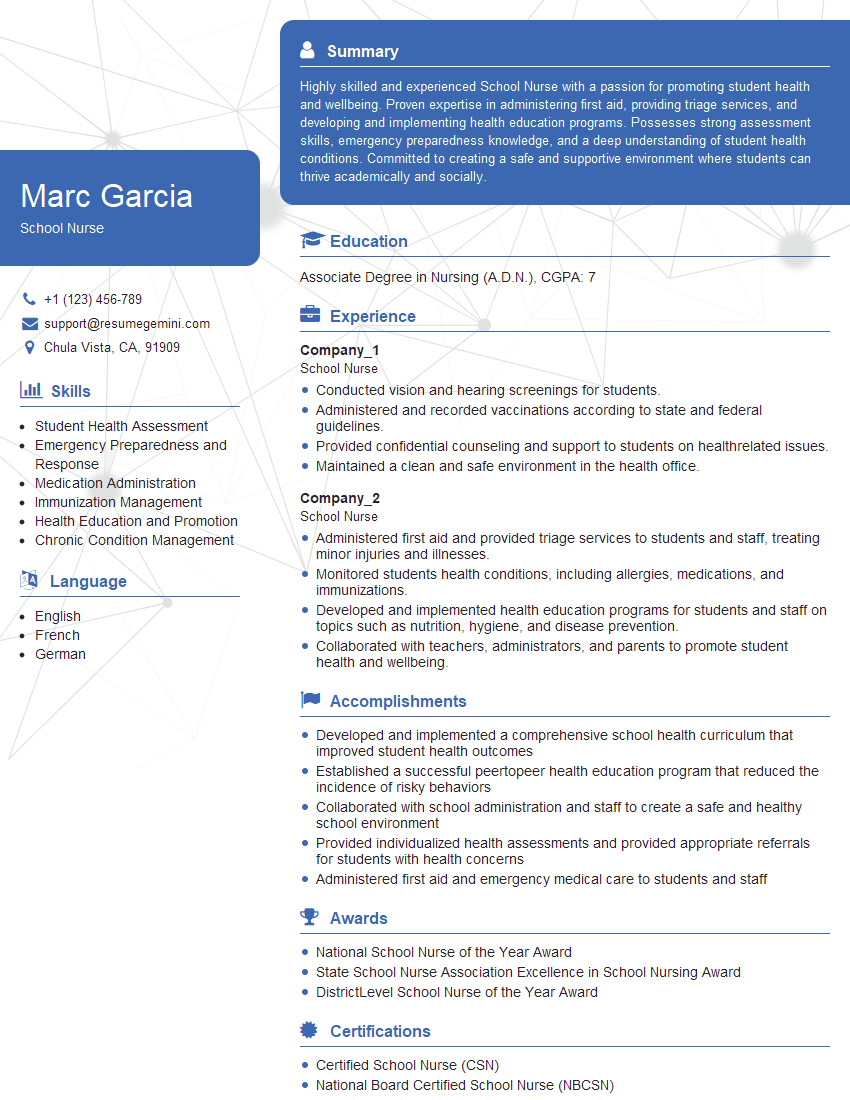
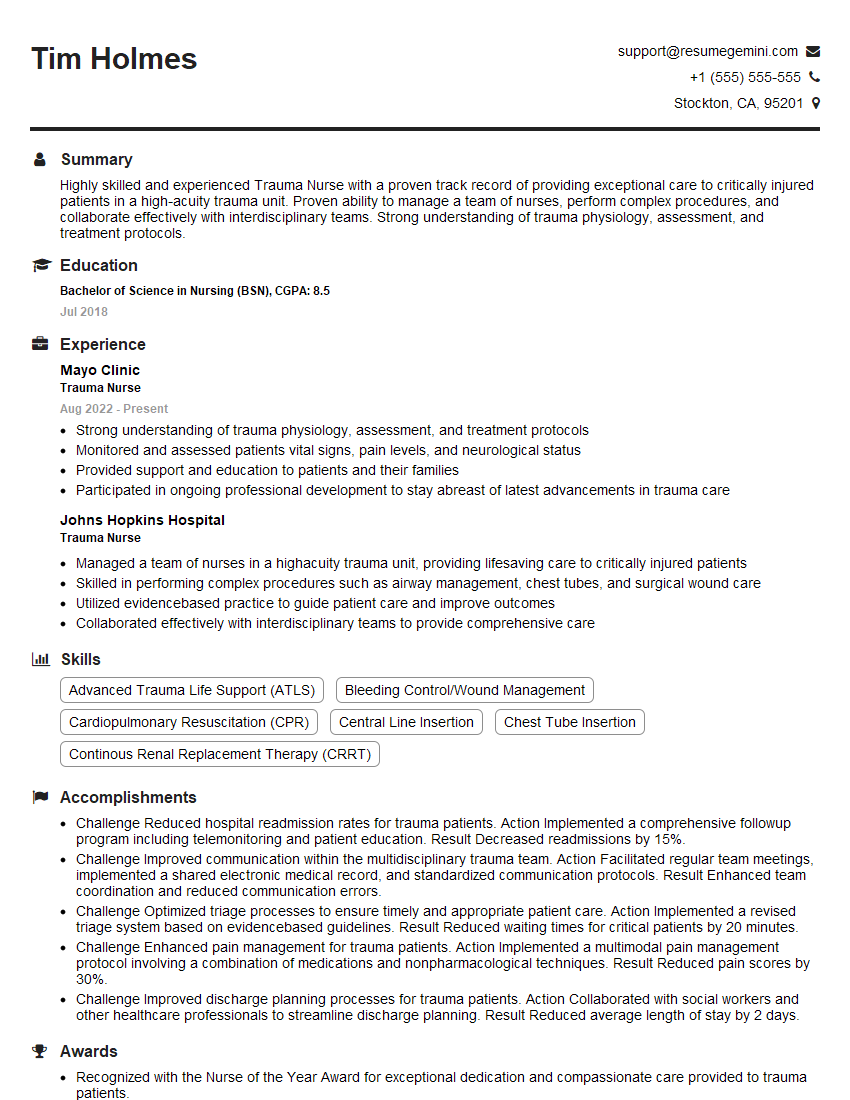
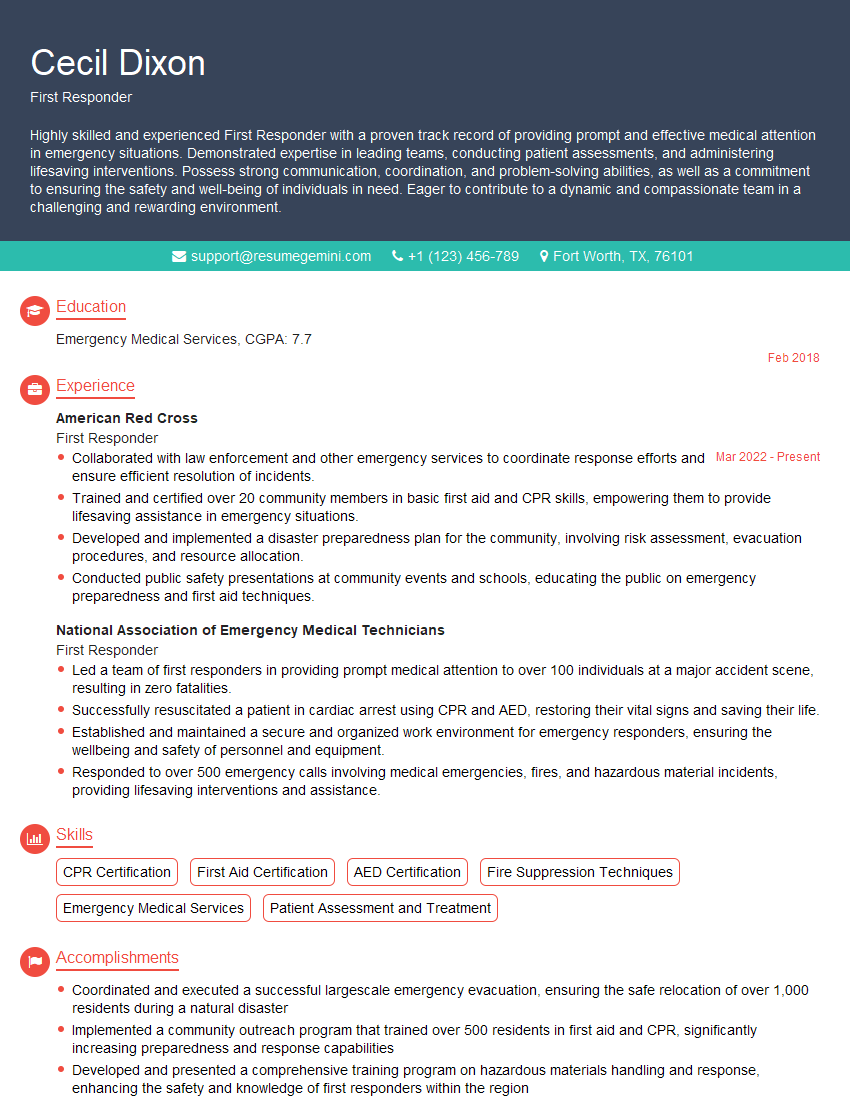
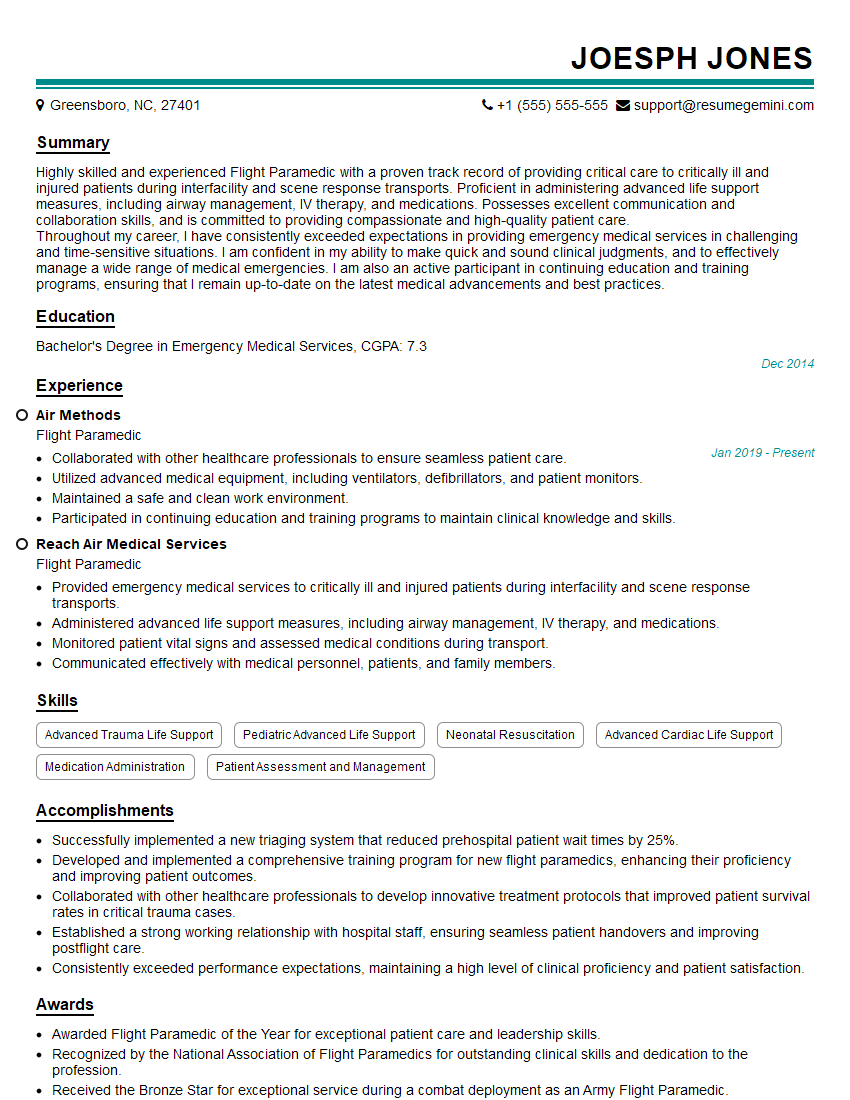
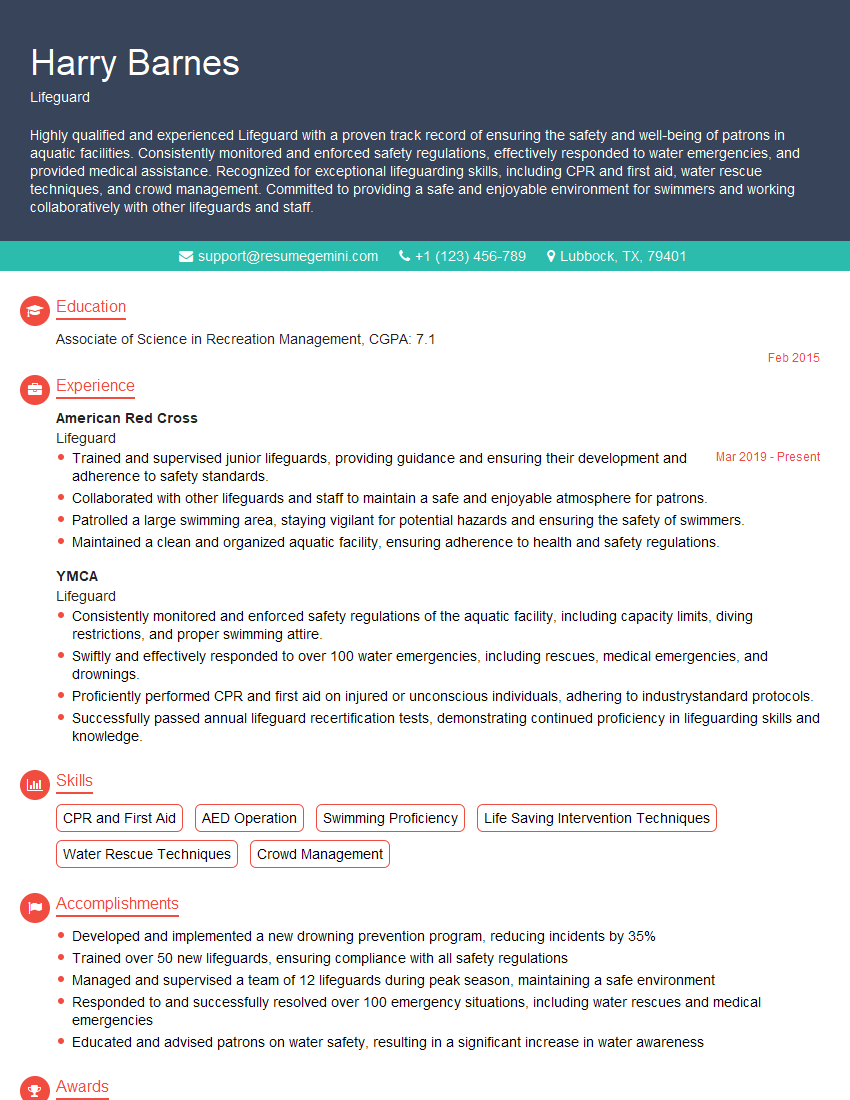
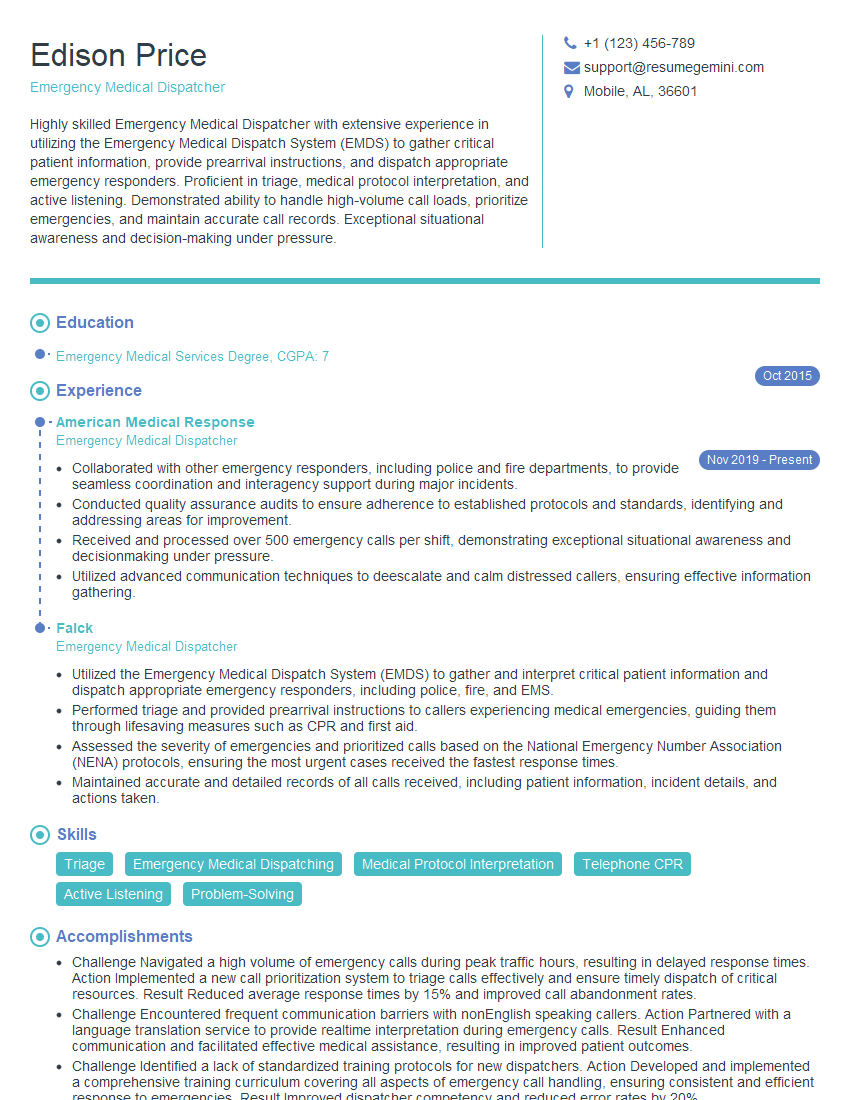
Mastering First Aid and Emergency Medical Response skills significantly enhances your career prospects in healthcare and related fields, opening doors to various roles with increased responsibility and earning potential. To stand out, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume that gets noticed. They provide examples of resumes tailored to First Aid and Emergency Medical Response positions, giving you a head start in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good