Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential First Aid and Medical Knowledge interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in First Aid and Medical Knowledge Interview
Q 1. Describe the steps you would take to assess a patient’s airway, breathing, and circulation (ABCs).
Assessing a patient’s airway, breathing, and circulation (ABCs) is the cornerstone of initial trauma care. It’s a systematic approach to quickly identify life-threatening conditions and prioritize treatment.
- Airway: First, check if the airway is open and clear. Look for obstructions like vomit, blood, or a loose object. If the airway is blocked, gently tilt the head back and lift the chin (head-tilt-chin-lift maneuver), unless a neck injury is suspected. In that case, use the jaw-thrust maneuver. Listen for breathing sounds.
- Breathing: Once the airway is secured, assess breathing. Look for chest rise and fall, listen for breath sounds, and feel for air movement against your cheek near the patient’s mouth and nose. Note the rate, depth, and ease of breathing. Is it labored, shallow, or absent?
- Circulation: Check for a pulse, typically at the carotid artery (neck) or femoral artery (groin). Assess the skin color (pale, cyanotic – bluish, flushed). Check for any signs of bleeding. Look for capillary refill – gently press a fingernail and note how quickly the color returns; prolonged refill indicates poor circulation.
Example: Imagine finding an unconscious person. You would first ensure their airway is open, then check for breathing. If they aren’t breathing, you would start CPR immediately. If they are breathing but have a weak pulse and pale skin, you’d suspect significant blood loss and manage that accordingly.
Q 2. Explain the procedure for controlling external bleeding.
Controlling external bleeding is crucial to prevent shock and potential death. The key steps involve:
- Direct Pressure: Apply firm, direct pressure to the wound using a clean cloth. Elevate the injured limb above the heart if possible (unless a fracture is suspected). This slows the bleeding by compressing blood vessels.
- Elevation: Elevating the bleeding extremity helps reduce blood flow to the area.
- Pressure Points: If direct pressure isn’t enough, apply pressure to a pressure point—a location where major arteries are close to the surface. For example, the brachial artery (inner arm) or femoral artery (groin). This technique requires specific knowledge and should be used cautiously.
- Tourniquet (Last Resort): A tourniquet should only be used as a last resort when severe, uncontrolled bleeding cannot be stopped by other means. It should be placed 2-3 inches above the wound, and tightened until bleeding stops. Mark the time of application on the tourniquet.
Important Note: Once bleeding is controlled, seek immediate medical attention. Even seemingly minor wounds can lead to complications.
Q 3. How would you treat a person experiencing a suspected stroke?
Suspected stroke requires immediate medical attention. The acronym FAST is a useful way to remember the key signs:
- Facial drooping: Ask the person to smile. Does one side of their face droop?
- Arm weakness: Ask the person to raise both arms. Does one arm drift downward?
- Speech difficulty: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- Time: If you observe any of these signs, call emergency services immediately. Time is critical in stroke treatment.
Treatment: The primary treatment involves getting the person to a hospital quickly for advanced medical care, including potential clot-busting medication (thrombolysis) if appropriate. Keep the person comfortable and monitor their vital signs until help arrives.
Q 4. What are the signs and symptoms of a heart attack?
Heart attack symptoms can vary, but common signs include:
- Chest pain or discomfort: This can feel like pressure, squeezing, fullness, or pain in the center of the chest lasting more than a few minutes.
- Discomfort in other areas: Pain or discomfort can spread to the shoulders, arms, back, neck, or jaw.
- Shortness of breath: Difficulty breathing may accompany the chest pain.
- Other symptoms: These might include breaking out in a cold sweat, nausea, lightheadedness, or sudden dizziness.
Important Note: Women may experience different symptoms than men, such as back pain, nausea, and fatigue. Don’t dismiss any unusual symptoms. Seek immediate medical attention if you suspect a heart attack.
Q 5. How would you respond to someone experiencing an allergic reaction?
Allergic reactions can range from mild to life-threatening. The severity depends on the allergen and the individual’s sensitivity.
Mild Reactions: These might include hives, itching, rash, or mild swelling. Treat with antihistamines (if available and the person isn’t allergic to them).
Severe Reactions (Anaphylaxis): This is a life-threatening emergency characterized by difficulty breathing, swelling of the face, lips, or tongue, dizziness, and a rapid, weak pulse. Immediate action is crucial.
- Call Emergency Services: Immediately call for emergency medical help.
- Administer Epinephrine (if trained and available): If the person has an epinephrine auto-injector (like an EpiPen), administer it as directed.
- Monitor Breathing and Circulation: Maintain the airway, assist breathing if necessary, and monitor vital signs.
- Maintain a Calm and Reassuring Demeanor: Anxiety can exacerbate the situation.
Q 6. Describe your approach to managing a seizure.
Managing a seizure involves protecting the person from injury and ensuring they receive appropriate medical care.
- Protect the person from injury: Gently move any nearby objects that could cause harm. Do not restrain the person during the seizure.
- Turn the person onto their side (recovery position): This helps prevent choking or aspiration if they vomit.
- Time the seizure: Note how long the seizure lasts.
- Do not put anything in their mouth: This is a common myth and can cause injury.
- After the seizure: Check for injuries. Stay with the person until they regain consciousness and are alert.
- Seek medical attention: Call emergency services if it’s the person’s first seizure, the seizure is prolonged (more than 5 minutes), or if the person doesn’t regain consciousness quickly.
Q 7. Explain the proper technique for performing CPR on an adult.
Performing CPR on an adult involves these steps:
- Check for responsiveness: Gently tap the person and shout, “Are you okay?”
- Call for help: Dial emergency services (911 or your local emergency number).
- Check for breathing: Look, listen, and feel for normal breathing for no more than 10 seconds.
- Start chest compressions: Position your hands on the center of the chest, interlacing your fingers and keeping your arms straight. Compress the chest at a rate of 100–120 compressions per minute and a depth of at least 2 inches.
- Give rescue breaths (if trained): After 30 compressions, give 2 rescue breaths, each lasting about 1 second.
- Continue CPR: Repeat cycles of 30 compressions and 2 breaths until help arrives or the person shows signs of life.
Important: Proper training is essential for performing CPR effectively and safely. Hands-on instruction from a certified instructor is crucial.
Q 8. What are the key differences between adult, child, and infant CPR?
The primary differences in CPR technique between adults, children, and infants center around the size and development of the victim’s body. These differences impact hand placement, compression depth, and the ratio of compressions to breaths.
- Adults (8 years and older): Two hands are placed on the center of the chest, just below the nipple line. Compressions should be at least 2 inches deep, delivered at a rate of 100-120 per minute. The compression-to-ventilation ratio is typically 30:2.
- Children (1-8 years): For children, you’ll use either one or two hands depending on the size of the child. Place your hands in the center of the chest, just below the nipple line. The compression depth should be about 2 inches (or one-third the depth of the chest). The rate remains 100-120 compressions per minute, and the ratio is typically 30:2. For smaller children, using only one hand might be necessary.
- Infants (less than 1 year): For infants, use only two fingers to perform compressions on the center of the chest, just below the nipple line. The compression depth should be about 1.5 inches (approximately one-third the depth of the chest). The rate is the same (100-120 compressions per minute), but the ratio is 30:2. Infants also require gentler breaths, ensuring you can see their chest rise.
Imagine trying to squeeze a grape versus an orange – the force and technique would differ significantly, and this analogy reflects the differences in CPR for varied age groups. Proper technique is crucial for effective circulation and oxygen delivery.
Q 9. How do you prioritize multiple patients in a mass casualty incident?
Prioritizing multiple patients in a mass casualty incident (MCI) requires a systematic approach using triage. The most common method is the START (Simple Triage and Rapid Treatment) method. This system categorizes patients based on their immediate need for care.
- Immediate (Red): These patients require immediate life-saving interventions. Examples include patients with airway obstruction, uncontrolled bleeding, or signs of shock.
- Delayed (Yellow): These patients have injuries that require treatment but are not immediately life-threatening. Examples include fractures with no major bleeding, minor burns, or moderate pain.
- Minimal (Green): These patients have minor injuries that can wait for treatment. They are often ambulatory and require minimal immediate intervention. Examples include abrasions and minor sprains.
- Expectant (Black): These patients are severely injured and have a very low chance of survival. Resources are not allocated to these patients, focusing instead on those with better chances of survival.
In practice, I would quickly assess each patient’s respiratory status, perfusion, and mental status, assigning them a category. This ensures that limited resources are effectively allocated, maximizing the number of lives saved. For instance, a patient bleeding profusely takes priority over one with a minor fracture.
Q 10. What are the limitations of your First Aid certification?
My First Aid certification, while providing valuable knowledge and skills, has inherent limitations. It’s crucial to understand these limitations to avoid exceeding my scope of practice and potentially harming a patient.
- Scope of Practice: My certification enables me to provide basic first aid; I am not a medical professional and cannot diagnose or treat illnesses or injuries beyond the scope of my training.
- Ongoing Training: Medical knowledge evolves continuously. My certification’s validity is time-limited, and continued professional development is vital to maintain proficiency.
- Limited Equipment: My ability to effectively treat a patient is limited by the available equipment and resources. I cannot perform procedures requiring specialized tools or medications.
- Emergency Medical Services (EMS) Responsibilities: My role is to stabilize the patient until professional medical care arrives. I cannot replace the expertise of paramedics or other healthcare professionals.
For example, while I can control bleeding and perform basic wound care, I cannot perform advanced procedures like intubation or administer medications.
Q 11. Describe your experience with automated external defibrillators (AEDs).
I have extensive experience with Automated External Defibrillators (AEDs). I am proficient in operating various AED models, and I understand the importance of early defibrillation in cases of sudden cardiac arrest.
My training includes recognizing signs of cardiac arrest, properly attaching the AED pads, ensuring the device is functioning correctly, and following the verbal prompts. I am also comfortable in assessing the scene for safety before using the AED.
I’ve utilized AEDs in training simulations and practiced with real-life scenarios. I understand the importance of teamwork in managing sudden cardiac arrest, efficiently coordinating actions with bystanders and ensuring a safe and effective procedure.
The use of an AED is a critical component of effective CPR and significantly increases survival chances. Remembering to follow the device’s instructions is paramount; the AED’s safety measures will ensure a safe procedure, even for a novice user.
Q 12. How would you handle a patient who is refusing treatment?
Handling a patient refusing treatment requires a delicate balance between respecting their autonomy and ensuring their safety. I would first attempt to understand the reason for their refusal, communicating calmly and respectfully.
I would explain the potential risks of not receiving treatment and the benefits of accepting my help, ensuring they are fully informed. I would document their refusal, clearly stating the reasons they provided. If the refusal poses a significant risk to their life or well-being and they lack the capacity to make informed decisions, I would seek guidance from emergency medical services (EMS) or other relevant authorities.
It’s imperative to approach the situation with empathy and understanding, acknowledging their right to refuse treatment and respecting their decision. My priority is to preserve their dignity and safety while acting within the boundaries of my legal and ethical obligations. The key here is to be an advocate for the patient, whether they accept treatment or not.
Q 13. Explain the importance of maintaining a sterile environment during wound care.
Maintaining a sterile environment during wound care is paramount to prevent infection. Infection can significantly complicate wound healing, leading to prolonged recovery times, scarring, and potentially life-threatening sepsis.
Sterile techniques include washing hands thoroughly, using sterile gloves, dressings, and instruments. The wound area should be cleaned gently with an antiseptic solution, moving from the center outwards to avoid spreading contaminants. Applying a sterile dressing helps protect the wound from further contamination.
For example, failing to use sterile gloves when changing a dressing could introduce bacteria into the wound, potentially leading to a serious infection. Similarly, using a contaminated dressing could have the same result. The importance of sterile technique cannot be overstated, as it significantly impacts the healing process and reduces the risk of complications.
Q 14. Describe your understanding of different types of shock.
Shock is a life-threatening condition characterized by inadequate blood flow to the body’s tissues and organs. Different types of shock have unique causes but share similar symptoms such as rapid, weak pulse; pale, cool, clammy skin; and altered mental status.
- Hypovolemic Shock: This occurs due to significant blood or fluid loss, such as from severe bleeding or dehydration. Think of it as your body’s plumbing system having insufficient fluid to keep functioning properly.
- Cardiogenic Shock: This is caused by the heart’s inability to pump enough blood to meet the body’s needs, often due to a heart attack or other heart conditions. This is like the pump in your system being faulty.
- Distributive Shock (e.g., Septic, Anaphylactic, Neurogenic): This results from abnormal dilation of blood vessels, reducing blood pressure and blood flow. Septic shock arises from severe infection; anaphylactic shock is a severe allergic reaction; and neurogenic shock is caused by damage to the nervous system. In these types, the vessels themselves malfunction, allowing blood to pool and become ineffective.
- Obstructive Shock: This is caused by obstruction to blood flow, such as a pulmonary embolism (blood clot in the lung) or cardiac tamponade (fluid buildup around the heart). This involves a physical blockage of the system.
Recognizing the type of shock is crucial for appropriate treatment. Addressing the underlying cause is essential, whether it involves controlling bleeding, administering fluids, or providing advanced cardiac life support. Each type requires a specific approach to improve circulation and oxygen delivery to the tissues.
Q 15. How would you manage a patient with a suspected spinal injury?
Managing a suspected spinal injury requires a systematic approach prioritizing the patient’s safety and minimizing further damage. The primary concern is to stabilize the spine to prevent movement that could worsen the injury. This is achieved through the principle of spinal immobilization.
Assessment: Begin by carefully assessing the patient’s level of consciousness, breathing, and circulation (ABCs). Look for any obvious deformities or signs of injury.
Manual Stabilization: Before moving the patient, manually stabilize their head and neck. This involves gently supporting the head and neck in a neutral position, preventing any rotation or flexion. This often requires multiple rescuers.
Immobilization: Use a rigid cervical collar to immobilize the neck. A long spine board is then used to immobilize the entire spine. Secure the patient to the board using straps, ensuring the head is properly aligned and stabilized. It is crucial to avoid unnecessary movement during this process.
Ongoing Monitoring: Continuously monitor the patient’s vital signs, level of consciousness, and respiratory status. Be aware of potential complications such as respiratory distress or shock.
Transport: Once immobilized, transport the patient to the hospital on a stretcher, maintaining spinal immobilization throughout. Avoid any jarring movements.
Example: Imagine you find a person lying unconscious after a car accident. You wouldn’t immediately try to move them. Instead, you’d call emergency services and carefully stabilize their head and neck before attempting any movement using the steps outlined above.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the potential complications of a fractured bone?
Fractured bones, or bone breaks, can lead to a range of complications, depending on the severity and location of the fracture. Some potential complications include:
Nonunion: The bone fragments fail to heal properly, leaving a gap between the broken ends.
Malunion: The bone heals in a misaligned position, leading to deformity and potential functional impairment.
Delayed Union: The bone takes longer to heal than expected.
Infection: Open fractures or fractures with poor blood supply are at higher risk of infection, which can be serious and potentially life-threatening.
Compartment Syndrome: Swelling and pressure build up within the muscle compartment surrounding the fracture, compromising blood supply to the tissues. This is a surgical emergency.
Nerve Damage: A fracture can damage nearby nerves, leading to loss of sensation, muscle weakness, or paralysis.
Blood Vessel Damage: A fracture can damage blood vessels, leading to bleeding, hematoma formation, and potentially life-threatening blood loss.
Fat Embolism: In certain fractures, fat globules can enter the bloodstream and travel to the lungs or brain, causing serious complications.
Chronic Pain: Even after healing, some patients experience persistent pain or stiffness at the fracture site.
Example: A severely displaced femur fracture could lead to compartment syndrome if not promptly treated, requiring immediate surgical intervention to alleviate the pressure and restore blood flow.
Q 17. How would you recognize and respond to signs of hypothermia or hyperthermia?
Hypothermia and hyperthermia represent opposite ends of the thermoregulation spectrum, both posing significant risks. Recognizing and responding promptly are crucial.
Hypothermia (low body temperature):
Recognition: Shivering (initially), confusion, slurred speech, drowsiness, slow heart rate, slow breathing, loss of coordination, and eventually loss of consciousness.
Response: Move the person to a warm environment, remove any wet clothing, provide warm blankets or clothing, offer warm fluids (if conscious), and seek medical attention. Do not rub the person’s extremities as this can damage tissues.
Hyperthermia (high body temperature):
Recognition: High body temperature (above 104°F or 40°C), flushed skin, rapid pulse, rapid breathing, headache, dizziness, nausea, vomiting, confusion, seizures, and loss of consciousness.
Response: Move the person to a cool environment, remove excess clothing, apply cool compresses or a cool bath (be cautious to avoid chilling), offer cool fluids (if conscious), and seek immediate medical attention. Heat stroke is a life-threatening emergency.
Example: An elderly person found unresponsive outdoors on a hot summer day could be suffering from heat stroke (hyperthermia). Conversely, a hiker lost in cold weather might develop hypothermia and need immediate warming measures.
Q 18. Describe your knowledge of different types of burns.
Burns are classified by depth and extent, impacting treatment significantly. We categorize them as follows:
First-degree burns (Superficial): These affect only the epidermis (outer skin layer). They cause redness, pain, and mild swelling. Sunburn is a common example.
Second-degree burns (Partial-thickness): These involve the epidermis and part of the dermis (the deeper skin layer). They cause redness, pain, swelling, and blistering. The skin may appear mottled.
Third-degree burns (Full-thickness): These destroy the entire epidermis and dermis and may extend into the subcutaneous tissue, muscle, or bone. The skin appears white, charred, or leathery; pain may be absent due to nerve damage.
Fourth-degree burns: These extend beyond the subcutaneous tissue to affect muscle, tendons, or bone. These are severe injuries requiring specialized care.
Treatment varies depending on the burn’s severity and size. First and second-degree burns can often be treated at home with cool water, pain relief, and keeping the area clean and covered. Third and fourth-degree burns require immediate medical attention, often involving hospitalization, wound care, and possibly skin grafts.
Example: A small scald from hot water is likely a first-degree or superficial second-degree burn. A burn from prolonged contact with a hot stove, however, could be deeper and require specialist care.
Q 19. How do you assess and manage a patient with a suspected concussion?
Assessing and managing a suspected concussion involves a careful evaluation of the patient’s symptoms and neurological status. A concussion is a traumatic brain injury causing temporary disruption of brain function.
Assessment: Use the Glasgow Coma Scale (GCS) to assess the level of consciousness. Ask about symptoms like headache, dizziness, nausea, vomiting, confusion, memory loss, balance problems, and sensitivity to light or noise. Observe for any neurological deficits.
Immediate Management: The immediate focus is on rest, monitoring for worsening symptoms, and preventing further injury. This includes keeping the patient still and avoiding any activities that could exacerbate the injury.
Monitoring: Monitor the patient closely for changes in consciousness, respiratory status, pupil size, and any new or worsening neurological symptoms. Seek immediate medical attention for any concerning changes.
Medical Evaluation: A medical professional should assess the patient, including a neurological exam. Imaging (CT scan) may be necessary to rule out other serious injuries.
Gradual Return to Activity: A gradual return to physical and mental activity is essential under medical supervision, following a graded protocol to minimize the risk of second-impact syndrome.
Example: If someone sustains a blow to the head during a sports game and exhibits symptoms like headache, dizziness, or confusion, immediate removal from play and subsequent medical assessment is crucial. Rushing them back into activity can have serious consequences.
Q 20. Explain the importance of documenting patient care.
Accurate and thorough documentation of patient care is paramount for several crucial reasons:
Legal Protection: Detailed records provide legal protection for healthcare providers, demonstrating adherence to standards of care and potentially avoiding malpractice claims.
Continuity of Care: Comprehensive documentation ensures seamless continuity of care. It allows healthcare professionals involved in the patient’s treatment to share information, preventing duplication of efforts and potential errors.
Quality Improvement: Data collected through patient records allows healthcare institutions to track trends, identify areas for improvement, and ultimately enhance the quality of care.
Research and Education: Aggregated, anonymized data from patient records contributes valuable information for medical research, advancing understanding and treatment of various conditions.
Billing and Reimbursement: Accurate documentation is crucial for insurance billing and reimbursement purposes. It ensures healthcare providers receive appropriate payment for services rendered.
Example: Imagine a patient with multiple health issues treated by different specialists over several years. Consistent and detailed documentation allows each practitioner to access a comprehensive history, enabling informed decisions and coordinating their efforts to optimize patient care.
Q 21. How familiar are you with different types of wound dressings and bandages?
I am familiar with a wide range of wound dressings and bandages, each designed for specific wound types and purposes.
Gauze pads: Highly absorbent, used for wound cleansing and covering.
Non-adherent dressings: Prevent sticking to the wound, minimizing pain during dressing changes. Examples include Telfa pads.
Hydrocolloids: Gel-forming dressings that maintain a moist wound environment, promoting healing and reducing pain. Useful for minor burns and abrasions.
Alginates: Highly absorbent dressings derived from seaweed, ideal for wounds with moderate to heavy exudate (discharge).
Hydrogel dressings: Gel-based dressings that hydrate the wound and provide pain relief. Used for burns, pressure ulcers, and dry wounds.
Foam dressings: Highly absorbent dressings that provide cushioning and protection, suitable for wounds with moderate to heavy exudate.
Bandages (e.g., elastic bandages, crepe bandages, roller gauze): Used to secure dressings, provide support, and control bleeding.
Example: A superficial wound with minimal drainage might be appropriately managed with a gauze pad and adhesive bandage. A deep wound with significant drainage would require a more absorbent dressing like an alginate, secured with a roller bandage.
Q 22. Describe your experience working under pressure in an emergency situation.
Working under pressure in emergency situations is commonplace for First Aiders. My experience has taught me the importance of remaining calm and focused amidst chaos. For instance, during a multi-vehicle accident, I had to rapidly assess multiple patients with varying injuries – from minor abrasions to severe limb trauma. My training kicked in, allowing me to prioritize victims based on the severity of their injuries using the triage system (START method, for example). I delegated tasks to other first responders efficiently, ensured airway maintenance and controlled bleeding where necessary, and maintained clear communication with emergency medical services (EMS) to ensure swift and effective patient transport. This experience highlighted the importance of systematic approach, clear communication and delegation under immense pressure.
Another example involved a sudden cardiac arrest where I had to perform CPR and use an AED while simultaneously coordinating with bystanders to clear the area and manage the patient’s family. The adrenaline was high, but my focus remained on the immediate life-saving actions, following established protocols precisely.
Q 23. How do you stay updated with current best practices in First Aid and emergency medical care?
Staying updated on best practices is crucial in the rapidly evolving field of emergency medical care. I accomplish this through several methods:
- Continuing Medical Education (CME) courses: I regularly participate in advanced first aid and emergency medical care courses offered by reputable organizations like the American Heart Association (AHA) and the American Red Cross. These courses cover the latest guidelines and techniques.
- Professional journals and publications: I subscribe to peer-reviewed journals and regularly read publications from leading medical organizations to keep abreast of new research and advancements.
- Conferences and workshops: Attending conferences and workshops allows me to network with other professionals and learn about new approaches and technologies in first aid and emergency medicine.
- Online resources: Reputable online platforms offer access to updated guidelines, protocols, and training modules. I utilize these resources to reinforce my knowledge and learn about emerging best practices.
This multi-pronged approach ensures I remain proficient and up-to-date with the most current and effective methods of providing emergency care.
Q 24. Explain your understanding of infection control protocols.
Infection control is paramount in first aid and emergency medical care to prevent the spread of infectious diseases. My understanding encompasses several key elements:
- Hand hygiene: This is the cornerstone of infection control. I meticulously wash my hands with soap and water or use an alcohol-based hand sanitizer before and after each patient interaction.
- Personal Protective Equipment (PPE): Appropriate PPE use is critical. This includes gloves, masks, eye protection, and gowns, depending on the situation and potential exposure to bodily fluids.
- Safe disposal of sharps and biohazardous waste: I am trained in the proper disposal of needles, syringes, and other potentially infectious materials to prevent accidental needlesticks and environmental contamination.
- Cleaning and disinfection of equipment and surfaces: Any equipment or surfaces that come into contact with a patient or their bodily fluids are thoroughly cleaned and disinfected according to established protocols.
- Standard precautions: I adhere strictly to universal precautions, treating all patients as potentially infectious regardless of their known health status.
These protocols are not merely guidelines; they are essential to protect both patients and healthcare providers from the transmission of infectious diseases.
Q 25. Describe your experience with patient communication and empathy.
Effective patient communication and empathy are vital components of providing excellent first aid. I strive to create a calm and reassuring environment for the patient, regardless of the circumstances. I achieve this through active listening, clear and concise explanations, and demonstrating genuine care and concern. For example, when assisting a child with a minor injury, I use age-appropriate language and a gentle approach to minimize fear and anxiety.
With adult patients, I employ a more detailed explanation of the procedures involved and ensure they understand the steps being taken. I actively seek their input and address their concerns, adapting my communication style based on their individual needs and emotional state. Building rapport through empathy helps build trust and reduces the patient’s stress, leading to more effective care.
Q 26. How would you handle a situation where you disagree with a colleague’s medical judgment?
Disagreements on medical judgment can arise, and addressing them professionally is critical. My approach involves a respectful and constructive dialogue. I would first privately express my concerns to my colleague, explaining my reasoning based on established protocols and current best practices. I would emphasize patient safety as the primary concern and aim for a collaborative solution. If a resolution cannot be reached through discussion, I would seek the advice of a senior medical professional or supervisor to ensure the best possible outcome for the patient. Documenting the disagreement and the steps taken to resolve it is also essential for maintaining accountability and transparency.
Q 27. What are your strengths and weaknesses as a First Aider?
Strengths: My strengths include a calm demeanor under pressure, systematic problem-solving skills, strong communication and interpersonal abilities, and a deep understanding of current first aid and emergency medical protocols. I am a quick learner, adaptable to various situations, and committed to continuous professional development.
Weaknesses: While I possess extensive knowledge, there’s always room for improvement. I am currently working on enhancing my skills in advanced trauma management, particularly in situations involving multiple casualties. I also aim to further refine my skills in crisis communication and debriefing techniques post-incident to improve my support of both patients and colleagues.
Q 28. Describe a time you had to make a critical decision under pressure in a medical setting.
During a hiking trip, a fellow hiker suffered a severe ankle injury resulting in significant swelling and pain. Determining whether to attempt an immediate splint and evacuation or wait for professional help presented a critical decision. I had to assess the severity of the injury, the terrain, the hiker’s overall condition, and the available resources (communication, access for rescue). Considering the remoteness, the potential for further injury during transport, and the limited communication, I decided to stabilize the ankle with a makeshift splint using readily available materials, prioritizing pain management, and then contacting emergency services for evacuation. This decision, made under time pressure and with limited resources, underscored the need for rapid assessment, resourcefulness, and prioritizing patient safety.
Key Topics to Learn for First Aid and Medical Knowledge Interview
- Emergency Response Procedures: Understanding the steps involved in assessing a scene, prioritizing injuries, and initiating appropriate actions. This includes recognizing life-threatening conditions and taking immediate steps to stabilize the patient.
- Wound Management: Practical application of cleaning, dressing, and bandaging various types of wounds, from minor cuts to more serious lacerations. Consider the importance of infection control and recognizing signs of infection.
- Cardiopulmonary Resuscitation (CPR): Mastering the techniques of chest compressions and rescue breaths, including variations for adults, children, and infants. Understanding the importance of early CPR and recognizing when it’s necessary.
- Shock Management: Recognizing the signs and symptoms of shock and implementing appropriate first aid measures, such as maintaining body temperature and positioning the patient.
- Bleeding Control: Different techniques for controlling external and internal bleeding, including direct pressure, elevation, and tourniquet application (when appropriate). Understanding the limitations and risks associated with each technique.
- Fracture and Sprain Management: Proper splinting techniques for suspected fractures and the management of sprains and dislocations. Understanding the principles of immobilization and pain management.
- Basic Anatomy and Physiology: A foundational understanding of the human body’s systems (respiratory, circulatory, nervous) will help you answer questions about the rationale behind first aid procedures.
- Legal and Ethical Considerations: Awareness of relevant legal and ethical implications of providing first aid, including consent, confidentiality, and limitations of scope of practice.
- Common Medical Conditions: Familiarity with recognizing symptoms of common medical emergencies, such as heart attack, stroke, diabetic emergencies, and allergic reactions.
- Communication and Teamwork: Demonstrating clear and effective communication skills, both in assessing the patient and relaying information to emergency medical services (EMS).
Next Steps
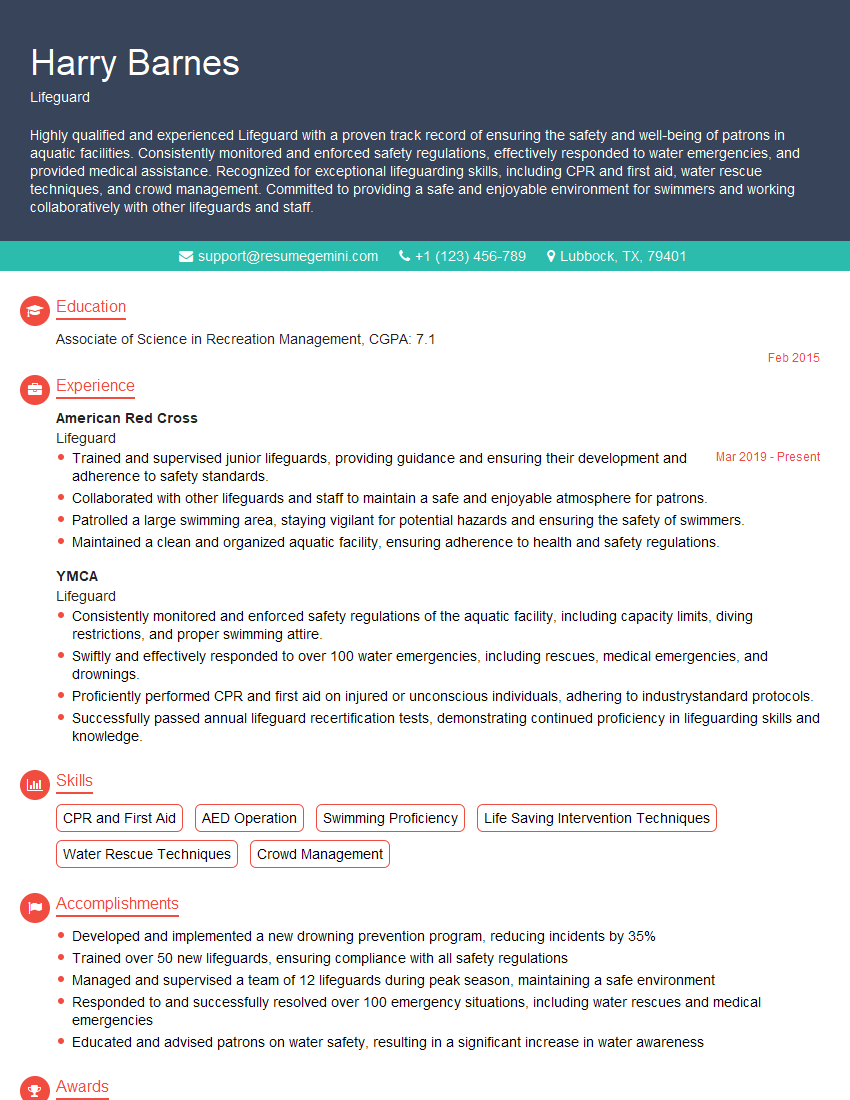
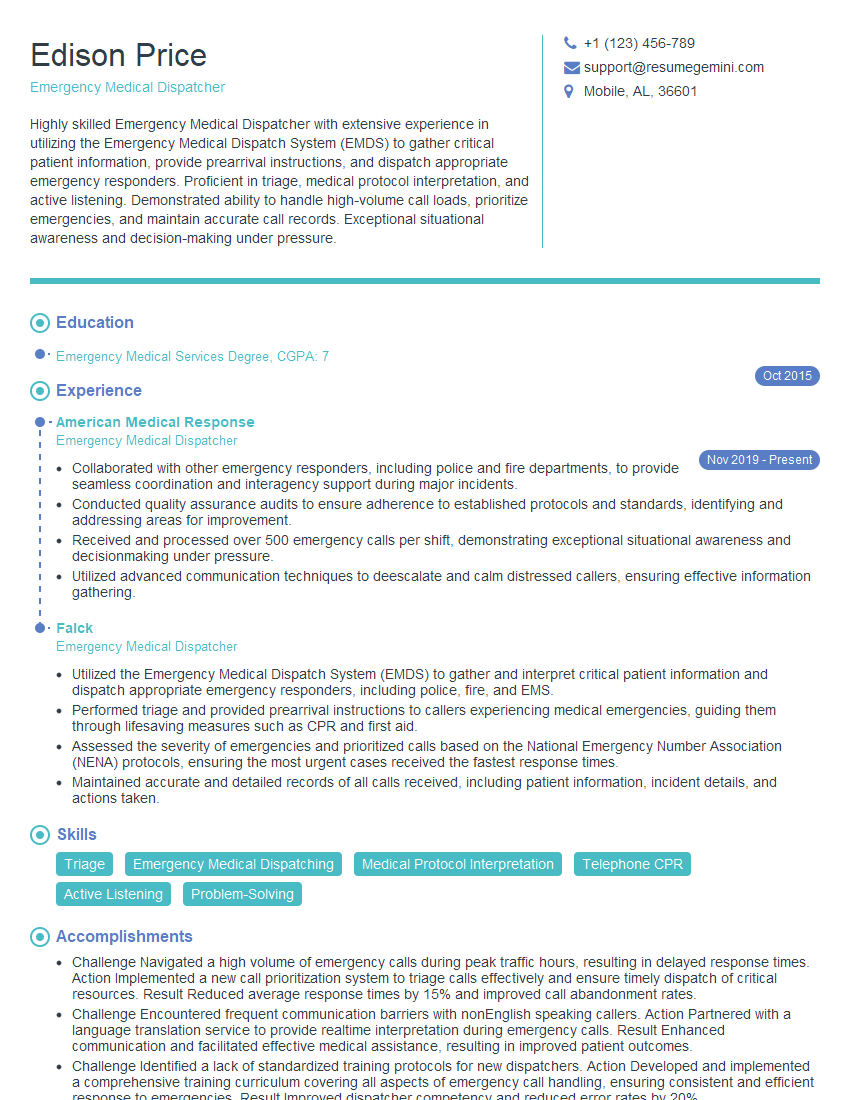
Mastering First Aid and Medical Knowledge is crucial for career advancement in many healthcare and safety-related fields. A strong foundation in these areas demonstrates competency, reliability, and a commitment to patient well-being. To maximize your job prospects, it’s essential to create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. They provide examples of resumes tailored to First Aid and Medical Knowledge positions, giving you a head start in creating a document that will get noticed.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good