Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Veterinary Care and Emergency Procedures interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Veterinary Care and Emergency Procedures Interview
Q 1. Describe your experience with advanced cardiac life support (ACLS) in veterinary medicine.
Advanced Cardiac Life Support (ACLS) in veterinary medicine involves a coordinated, multi-step approach to managing life-threatening cardiac emergencies. My experience encompasses years of practical application, from initial assessment and stabilization to advanced interventions like cardiopulmonary resuscitation (CPR), defibrillation, and administration of emergency medications. I’m proficient in using various monitoring devices, interpreting ECGs to identify arrhythmias, and selecting appropriate treatment protocols based on the underlying cause of cardiac arrest.
For instance, I recall a case involving a Great Dane with sudden cardiac arrest. Using the principles of ACLS, we immediately initiated CPR, placing an IV catheter for rapid fluid and drug administration. Concurrent ECG monitoring allowed us to identify ventricular fibrillation, prompting immediate defibrillation. Post-defibrillation, we administered epinephrine and other supportive medications while carefully monitoring vital signs. Successful resuscitation required a team effort, and understanding the precise sequence and rationale behind each intervention was crucial for achieving a positive outcome. I regularly participate in continuing education courses to stay updated on the latest ACLS guidelines and techniques, ensuring my skills are optimized for handling these critical situations.
Q 2. Explain your approach to stabilizing a patient in respiratory distress.
Stabilizing a patient in respiratory distress requires a systematic approach focused on ensuring adequate oxygenation and ventilation. The first step is a thorough assessment, including observation of respiratory rate and effort, auscultation of lung sounds for any abnormalities (wheezing, crackles), and assessment of mucus membrane color for signs of cyanosis. Once the underlying cause is identified (e.g., pneumonia, pneumothorax, aspiration), treatment is tailored accordingly. This might involve supplemental oxygen therapy, using an oxygen cage or mask depending on the patient’s condition and cooperation.
For more severe cases, mechanical ventilation may be necessary. This involves placing an endotracheal tube and using a ventilator to support breathing. In certain cases, medications like bronchodilators (for airway constriction) or mucolytics (for excessive mucus) may be required. For example, a cat with severe asthma might require nebulized bronchodilators alongside supplemental oxygen. Throughout the process, continuous monitoring of respiratory parameters and oxygen saturation levels is paramount to ensure effective stabilization and prevent further complications.
Q 3. How do you assess and manage hypovolemic shock in a canine patient?
Hypovolemic shock, caused by significant blood or fluid loss, is a life-threatening emergency in canines. Assessment involves careful evaluation of the patient’s vital signs – a rapid, weak pulse, pale gums, low blood pressure, and signs of dehydration (sunken eyes, dry mucous membranes) are all indicative. We also assess the potential cause (e.g., trauma, internal bleeding, severe vomiting/diarrhea).
Management begins with immediate fluid resuscitation using intravenous (IV) fluids like crystalloids (e.g., lactated Ringer’s solution) or colloids (e.g., plasma). The fluid rate is carefully calculated based on the animal’s weight and the degree of dehydration. For example, a dog with a significant blood loss will require a faster fluid rate. Simultaneously, we address the underlying cause, which may involve surgical intervention for internal bleeding or treatment for gastrointestinal disorders. Careful monitoring of urine output, heart rate, and blood pressure is crucial to guide fluid therapy and ensure the shock is effectively reversed. In some cases, blood transfusions may be needed to replace lost blood components.
Q 4. What are the key differences in managing trauma in small vs. large animals?
Managing trauma in small and large animals presents distinct challenges. Small animals (e.g., cats, dogs) are often more easily handled, and their injuries can be more readily assessed. However, their smaller size and delicate anatomy present difficulties in stabilizing fractures and performing complex surgical procedures. Large animals (e.g., horses, cows) pose significant challenges related to restraint, handling, and the scale of injuries. Their larger size requires specialized equipment and techniques for immobilization, resuscitation, and surgery.
For instance, while a fracture in a small dog may be managed with external coaptation, a horse with a limb fracture requires more complex techniques including casting, external skeletal fixation, or surgical repair. Assessing and treating internal injuries such as organ damage also requires specialized expertise and equipment depending on the size of the patient. Additionally, the weight and bulk of large animals can make simple procedures like intravenous catheter placement challenging. A good understanding of species-specific anatomy and physiology is vital in tailoring the approach to trauma management.
Q 5. Describe your experience with administering intravenous fluids and calculating fluid rates.
I have extensive experience administering intravenous (IV) fluids and calculating fluid rates. Accurate fluid therapy is critical in various veterinary emergencies and routine procedures. The process starts with selecting the appropriate fluid type and catheter size depending on the animal’s size and condition. Aseptic technique is essential to prevent infection. Once the catheter is placed, the fluid rate is calculated using established formulas, considering the animal’s weight, dehydration level, and ongoing fluid losses (e.g., vomiting, diarrhea).
For example, the maintenance fluid rate for a dog is often calculated as 60ml/kg/day. However, this needs to be adjusted depending on several factors. A dog that is severely dehydrated might require a much higher rate initially (e.g., bolus administration). Fluid administration needs constant monitoring. We check for swelling at the infusion site, monitor urine output, and observe the patient’s response. Continuous monitoring of vital signs helps adjust the fluid rate and prevents over- or under-hydration. I use various infusion pumps to precisely control the fluid rate, ensuring safe and effective administration.
Q 6. How do you interpret arterial blood gas results and make necessary adjustments to treatment?
Interpreting arterial blood gas (ABG) results provides crucial insights into a patient’s respiratory and acid-base balance. Key parameters include pH (reflecting acidity/alkalinity), PaCO2 (partial pressure of carbon dioxide, indicating ventilation), and PaO2 (partial pressure of oxygen, reflecting oxygenation). Bicarbonate (HCO3-) and base excess values reflect the metabolic component of acid-base balance.
For example, a low pH with a high PaCO2 suggests respiratory acidosis (inadequate ventilation). Treatment might involve assisted ventilation or bronchodilators. A low pH with a low HCO3- indicates metabolic acidosis (excess acid production or bicarbonate loss). Treatment might include fluid therapy or administration of sodium bicarbonate. I use this information to guide therapy, adjusting fluid rates, oxygen supplementation, and medication as needed. For instance, if a patient is hypoxic (low PaO2), we would increase oxygen flow. Careful monitoring of ABG results allows for dynamic adjustments to treatment, optimizing patient outcome.
Q 7. Explain your understanding of pain management protocols for emergency cases.
Pain management protocols in emergency cases are crucial for patient well-being and successful treatment. The approach is multifaceted and depends on the type and severity of the injury or condition. A thorough pain assessment is essential, taking into account both physiological and behavioral signs. The choice of analgesics depends on several factors, including the species, age, overall health of the patient, and the nature of the pain (acute vs. chronic).
Commonly used analgesics include opioids (e.g., morphine, butorphanol), NSAIDs (non-steroidal anti-inflammatory drugs, e.g., meloxicam), and local anesthetics. The choice and route of administration (oral, intravenous, intramuscular) depend on the individual patient and the urgency of the situation. Multimodal analgesia, combining different types of analgesics, often provides more effective pain relief with fewer side effects. For instance, a post-operative patient might receive opioids for immediate post-surgical pain, followed by NSAIDs for ongoing pain management. Regular assessment of pain levels and careful monitoring for any adverse effects are vital for ensuring effective and safe pain control.
Q 8. What are the common causes of seizures in dogs and how do you manage them?
Seizures in dogs, also known as convulsions, are episodes of abnormal brain activity causing involuntary muscle contractions. Common causes are diverse and range from relatively benign to life-threatening conditions.
- Idiopathic Epilepsy: This is the most common cause, where seizures occur without an identifiable underlying cause. We often manage this with anticonvulsant medications tailored to the individual dog’s needs and seizure frequency.
- Brain Tumors: Growing tumors can compress brain tissue, leading to seizures. Diagnosis often involves advanced imaging like MRI. Treatment focuses on managing the tumor, which might involve surgery, radiation, or chemotherapy, along with anticonvulsant medication for seizure control.
- Infections: Infections of the brain (encephalitis) or its coverings (meningitis) can trigger seizures. Treatment involves aggressive antimicrobial therapy guided by culture and sensitivity results.
- Metabolic Disorders: Conditions like hypoglycemia (low blood sugar), hypocalcemia (low calcium), and liver or kidney disease can disrupt brain function and cause seizures. Addressing the underlying metabolic imbalance is crucial; this might involve intravenous fluids, electrolyte correction, or dietary changes.
- Trauma: Head injuries can cause seizures, sometimes delayed. Management involves careful monitoring for neurological deterioration, supportive care, and potential anticonvulsant therapy.
Managing a seizure involves ensuring the dog’s safety by protecting them from injury during the episode. We would carefully monitor vital signs, providing supportive care such as intravenous fluids and oxygen if necessary. Once the seizure subsides, a thorough neurological examination and diagnostic testing are crucial to identify the underlying cause and implement appropriate treatment.
Q 9. Describe your experience with performing endotracheal intubation and mechanical ventilation.
Endotracheal intubation and mechanical ventilation are critical life-saving procedures in veterinary emergency medicine. I have extensive experience performing both, having intubated and ventilated hundreds of patients across a range of species and sizes.
Endotracheal intubation involves inserting a tube into the trachea (windpipe) to secure an airway and allow for assisted ventilation. My approach follows a standardized procedure, beginning with careful preoxygenation, selection of the appropriate size endotracheal tube, and visualization of the larynx using either direct laryngoscopy or a fiberoptic scope, depending on the patient’s anatomy and the situation. I always confirm proper placement by auscultation (listening for breath sounds), capnography (monitoring carbon dioxide levels), and chest rise and fall.
Mechanical ventilation involves using a ventilator to deliver breaths to the patient. I’m proficient in setting various ventilator parameters, including tidal volume, respiratory rate, and inspiratory pressure, based on the patient’s specific needs and physiological status. I carefully monitor the patient’s response to mechanical ventilation, adjusting the settings as needed to maintain adequate oxygenation and ventilation. This often involves close monitoring of blood gases and other vital signs. For example, in a patient with severe pneumonia and respiratory distress, I may utilize positive end-expiratory pressure (PEEP) to improve oxygenation. In a patient with pneumothorax, I would need to address that issue first before placing the patient on mechanical ventilation.
Q 10. How do you assess and treat toxicities in animals?
Assessing and treating toxicities in animals requires a systematic approach, beginning with a thorough history – what the animal ingested, when, and how much. Physical examination findings are crucial, identifying any clinical signs.
The approach depends on the suspected toxin. For example, if chocolate toxicity is suspected, we’d consider the amount ingested and the dog’s size; treatment may involve inducing vomiting, administering activated charcoal to absorb the toxin, and supportive care such as intravenous fluids. For rodenticide ingestion, specific antidotes might be needed depending on the type of rodenticide ingested. Similarly, for plant toxicities, a detailed description of the plant is essential.
Laboratory tests are often necessary, including blood work to assess organ function and urine tests. Depending on the clinical picture and the suspected toxin, more specialized tests such as toxicology screens may be required. Treatment might involve decontamination (e.g., inducing emesis, administering activated charcoal), administering antidotes, supportive care (fluid therapy, oxygen support), and monitoring organ function. In some cases, referral to a veterinary toxicologist is crucial for complex cases.
Q 11. What is your experience with using diagnostic imaging (radiography, ultrasound) in emergency situations?
Diagnostic imaging plays a vital role in veterinary emergency medicine. My experience includes extensive use of radiography (X-rays) and ultrasound in various emergency situations.
Radiography is invaluable for assessing fractures, pneumothorax (collapsed lung), foreign bodies in the abdomen or airway, and other internal injuries. I routinely interpret radiographic images to guide treatment decisions, for instance, deciding whether a fracture requires surgical repair or splinting.
Ultrasound allows for real-time assessment of internal organs, crucial in cases of suspected abdominal trauma or internal bleeding. It enables rapid evaluation of the heart, lungs, abdomen, and other areas. For instance, I’ve used ultrasound to identify free fluid in the abdomen (indicative of internal bleeding) and to guide fluid administration during resuscitation. Combining both modalities provides a comprehensive view. For example, an initial radiograph could show a foreign body, then ultrasound could reveal associated injury to the adjacent organs.
Q 12. Describe your experience with performing blood transfusions.
Performing blood transfusions is a complex procedure requiring meticulous attention to detail. My experience includes numerous blood transfusions in various critical care scenarios.
Before initiating a transfusion, I always ensure thorough cross-matching to minimize the risk of adverse reactions. This involves careful blood typing of both the donor and recipient animals to ensure compatibility. The transfusion is carefully monitored for any signs of allergic or adverse reactions, such as increased heart rate, vomiting, or respiratory distress. Vital signs such as heart rate, blood pressure, and oxygen saturation are monitored continuously, and blood work is done before and after transfusions to observe changes in hemoglobin and hematocrit.
Proper administration involves maintaining a slow infusion rate to avoid complications. I’ve managed transfusions in situations ranging from post-surgical anemia to trauma patients experiencing severe blood loss, often in combination with fluid resuscitation and other supportive care.
Q 13. How do you approach a patient with suspected internal bleeding?
Suspected internal bleeding is a critical emergency requiring immediate action. My approach involves a rapid assessment of the patient’s condition, focusing on identifying the source and extent of bleeding.
Initial steps include assessing the patient’s vital signs (heart rate, respiratory rate, blood pressure, mucous membrane color), and evaluating for signs of shock (pale gums, rapid weak pulse, etc.). Abdominal palpation (gently feeling the abdomen) can sometimes provide clues. Diagnostic imaging such as ultrasound and radiography are crucial to identify the source of the bleeding (e.g., ruptured spleen, liver laceration). Laboratory tests such as complete blood count to check for anemia, and coagulation profile are imperative.
Treatment depends on the identified source and severity. Immediate measures often include fluid resuscitation (IV fluids) to maintain blood pressure and tissue perfusion. In cases of severe, ongoing bleeding, blood transfusions might be necessary. Surgical intervention is frequently required to control the bleeding source, such as repairing a lacerated liver or splenectomy (surgical removal of the spleen). Post-surgical care often involves close monitoring of vital signs, pain management, and continued supportive care.
Q 14. What is your experience with managing patients with heat stroke?
Heat stroke is a life-threatening emergency characterized by an extremely elevated body temperature. My experience encompasses managing numerous cases, often involving dogs left in hot cars or during strenuous activity in hot weather.
Immediate treatment focuses on rapid cooling to lower the body temperature. This might involve immersing the animal in cool (not ice-cold) water, applying cool packs, or using fans. Intravenous fluids are crucial to replace lost fluids and support vital organ function. Monitoring vital signs is paramount; I frequently use a rectal thermometer to monitor temperature closely and monitor for cardiac arrhythmias.
Laboratory tests may include blood work to evaluate organ function. Additional supportive care includes oxygen therapy if needed and treatment for any associated complications such as seizures or organ damage. The prognosis depends on the severity of the heat stroke and the success of rapid cooling and supportive care; early intervention is key to improving outcome.
Q 15. Explain your understanding of different types of shock and their management.
Shock is a life-threatening condition where the body isn’t getting enough blood flow to its organs. Different types of shock result from various causes, each requiring a unique approach to management.
- Hypovolemic Shock: This is caused by a significant loss of blood volume, often due to hemorrhage (severe bleeding), dehydration, or burns. Management focuses on rapid fluid resuscitation with intravenous fluids (crystalloids like lactated Ringer’s solution or colloids like plasma) to restore blood volume. We also address the underlying cause, such as surgically controlling hemorrhage.
- Cardiogenic Shock: This occurs when the heart is unable to pump enough blood to meet the body’s demands. This often results from conditions like heart failure or myocardial infarction (heart attack). Management involves supportive care with oxygen, medications to improve heart function (inotropes and vasopressors), and potential interventions like surgery.
- Distributive Shock: This happens when blood vessels dilate excessively, leading to a decrease in blood pressure. Septic shock (caused by infection), anaphylactic shock (allergic reaction), and neurogenic shock (nerve damage) fall under this category. Treatment involves addressing the underlying cause (e.g., antibiotics for sepsis, epinephrine for anaphylaxis), fluid resuscitation, and vasopressors to constrict blood vessels and raise blood pressure.
- Obstructive Shock: This type of shock is due to something physically blocking blood flow, such as a pulmonary embolism (blood clot in the lungs), pericardial effusion (fluid around the heart), or tension pneumothorax (collapsed lung). Immediate intervention is crucial, often requiring surgery or other procedures to relieve the obstruction.
In all cases of shock, monitoring vital signs (heart rate, blood pressure, respiratory rate, temperature, and capillary refill time) is crucial. Early recognition and prompt intervention are key to improving survival rates.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with wound management and surgical techniques.
My experience with wound management and surgical techniques is extensive, encompassing a wide range of procedures from simple laceration repairs to complex abdominal surgeries. I’m proficient in techniques like wound debridement (removing damaged tissue), suturing, and the use of various wound closure materials like staples and surgical glue.
For example, I recently managed a dog with a deep laceration to its leg requiring extensive debridement to remove contaminated tissue before closure. I’ve also performed numerous surgeries including splenectomies (removal of the spleen), gastropexies (surgical fixation of the stomach), and fracture repairs using both intramedullary pins and external fixators. I am well-versed in sterile surgical techniques, including proper draping, instrument handling, and aseptic practices. Maintaining meticulous surgical technique is paramount to minimizing infection risk and optimizing healing. Post-operative care, including pain management and monitoring for complications, is equally important.
Q 17. How do you prioritize multiple emergency cases simultaneously?
Prioritizing multiple emergency cases involves a systematic approach based on the severity and urgency of each case, using a triage system. I use a combination of factors to determine the order of treatment:
- ABCs: Airway, Breathing, Circulation. Cases with immediate threats to these basic life functions are always top priority.
- Severity of condition: A patient in respiratory distress or hemorrhagic shock takes precedence over a patient with a less critical injury.
- Potential for rapid deterioration: Cases with conditions likely to worsen rapidly (e.g., severe internal bleeding) require immediate attention.
I communicate clearly with the team, delegating tasks effectively, to ensure all patients receive appropriate and timely care. Using a whiteboard or similar system to keep track of patients and their status can be invaluable in a fast-paced emergency setting. Effective team communication, combined with a systematic triage approach, ensures that resources are allocated efficiently to provide the best possible care for all patients.
Q 18. Explain your knowledge of common emergency drugs and their dosages.
My knowledge of emergency drugs and their dosages is comprehensive and in line with current veterinary standards. Dosage calculations are always based on the patient’s weight and condition. Here are a few examples:
- Epinephrine: Used in anaphylaxis and cardiac arrest. Dosage varies depending on the route of administration and the specific indication. Always consult the drug’s package insert.
- Fluid therapy (Lactated Ringer’s solution): Used to treat hypovolemic shock and dehydration. Dosage is calculated based on the degree of dehydration and ongoing losses.
- Analgesics (e.g., buprenorphine, fentanyl): Essential for pain management post-surgery and in trauma cases. Dosage is carefully calculated based on species, weight, and pain level.
- Dobutamine: A positive inotrope used to increase cardiac contractility in cardiogenic shock. Dosage is carefully titrated based on the patient’s response.
I always follow established protocols, consult with veterinary colleagues if needed, and double-check dosages before administering any medications. Maintaining a detailed record of medications administered is vital for both the patient’s safety and legal compliance.
Q 19. Describe your experience with monitoring vital signs and interpreting changes.
Monitoring vital signs and interpreting changes is a fundamental aspect of veterinary emergency care. I use various methods to continuously monitor vital signs, including:
- Heart rate and rhythm: Assessed using auscultation (listening with a stethoscope) and ECG (electrocardiogram).
- Blood pressure: Measured using a Doppler ultrasound or oscillometric device.
- Respiratory rate and effort: Observed visually and by auscultation.
- Temperature: Measured using a rectal thermometer.
- Capillary refill time (CRT): An indicator of peripheral perfusion.
- Pulse oximetry: Measures blood oxygen saturation.
Changes in vital signs, particularly a drop in blood pressure or an increase in heart rate, indicate a possible deterioration in the patient’s condition, requiring immediate intervention. For example, a sudden decrease in blood pressure could signify internal bleeding, while an increase in heart rate might suggest pain, hypoxia (low oxygen), or shock. Careful observation and interpretation of vital sign changes are critical in guiding treatment decisions.
Q 20. How do you communicate effectively with clients during emergency situations?
Effective communication with clients during emergencies is crucial. I strive to remain calm and empathetic, recognizing that they are often experiencing high levels of stress and anxiety.
My approach involves providing clear and concise updates on the patient’s condition, explaining the diagnostic and treatment plan in understandable terms (avoiding excessive veterinary jargon), and answering their questions patiently. I maintain regular communication, updating them on progress or changes in the patient’s condition. Transparency and honest communication build trust and reduce anxiety. Should the situation warrant it, I am also able to discuss difficult options such as euthanasia with compassion and sensitivity.
Q 21. What are your strategies for handling stressful or difficult situations?
Handling stressful or difficult situations requires a combination of preparation, effective coping mechanisms, and teamwork. I maintain a calm demeanor under pressure, focusing on the immediate task at hand. Prioritization and systematic approach are key.
I regularly debrief with colleagues after challenging cases to process the experience, learn from mistakes and celebrate successes. Maintaining work-life balance and utilizing personal stress-reduction techniques (exercise, mindfulness etc.) are crucial for long-term well-being. Seeking help when needed, whether from supervisors or mental health professionals is a sign of strength and demonstrates commitment to personal and professional health.
Q 22. Describe your experience with emergency surgery.
My experience with emergency surgery spans over ten years, encompassing a wide range of procedures. I’ve performed hundreds of surgeries, from life-saving interventions like trauma repair (e.g., splenectomies for ruptured spleens, thoracotomies for penetrating chest wounds) to more specialized procedures like gastrointestinal surgeries (e.g., intestinal resection and anastomosis for volvulus or foreign body ingestion) and cardiopulmonary resuscitation (CPR). I’m proficient in advanced surgical techniques and comfortable managing critical patients, including those with significant blood loss or compromised organ systems. My experience includes working in high-volume emergency veterinary hospitals, where rapid assessment and efficient surgical intervention are crucial.
I’m also experienced in utilizing various surgical equipment and monitoring technologies, ensuring optimal patient outcomes during and after the procedures. This includes the use of advanced imaging (ultrasound, fluoroscopy) to guide minimally invasive surgeries, reducing post-operative complications.
Q 23. How do you maintain a sterile surgical field?
Maintaining a sterile surgical field is paramount to preventing surgical site infections. It’s a multi-step process that starts well before the incision. We begin with meticulous pre-surgical preparation of the patient, including thorough scrubbing and clipping of the surgical site. The surgical team, including myself and the veterinary technicians, then scrub their hands and arms rigorously using a surgical scrub, adhering to strict protocols. Sterile gowns, gloves, and masks are donned, ensuring no non-sterile material comes into contact with the operative field.
The surgical area is draped with sterile drapes, creating a barrier between the sterile and non-sterile zones. Instruments and supplies are meticulously prepared and maintained in sterile packs or containers. Throughout the procedure, we constantly monitor the sterility of the field, replacing any contaminated materials promptly. We also employ strategies such as minimizing movement and conversation around the surgical site to reduce airborne contamination. Continuous monitoring during and after the surgery is important to assess the sterility of the area and prevent any potential infection. Even the slightest breach of sterility could have life-threatening consequences.
Q 24. What is your experience with post-operative care of emergency patients?
Post-operative care of emergency patients is just as critical as the surgery itself. It involves close monitoring of vital signs (heart rate, respiratory rate, blood pressure, temperature), pain management, fluid therapy to maintain hydration and electrolyte balance, and nutritional support. We regularly assess the surgical site for signs of infection, hemorrhage, or dehiscence (wound separation). Patients often require continuous monitoring for several hours after surgery, sometimes requiring intensive care unit (ICU) admission.
The specifics of post-operative care are tailored to each patient’s condition and the nature of the surgery. For example, a patient who underwent a major abdominal surgery might require pain medication, intravenous fluids, and close monitoring for ileus (intestinal paralysis), while a patient with a simple laceration repair may only require analgesics and regular wound checks. We always provide detailed instructions to owners regarding medication administration, wound care, and when to seek further medical attention.
Q 25. How do you handle difficult or unusual cases?
Difficult or unusual cases require a systematic and multidisciplinary approach. First, I thoroughly review the patient’s history, physical examination findings, and any diagnostic tests (bloodwork, radiographs, ultrasound). I often consult with specialists in relevant fields (e.g., internal medicine, cardiology, oncology) to obtain expert opinions and consider various treatment options. Collaboration is key – discussing the case with other veterinarians, veterinary technicians, and even specialists from human medicine can often shed new light on the problem.
When faced with a rare or unknown condition, a thorough literature review and research of relevant medical databases becomes crucial. I might also consider referral to a university teaching hospital for advanced diagnostics and treatment options. The key is remaining flexible and adaptable, while maintaining a calm and rational approach that prioritizes the patient’s welfare.
For example, I once encountered a dog with an unusual presentation of heart failure. The typical diagnostic methods initially yielded inconclusive results. Through collaboration with a cardiology specialist and extensive research, we were able to identify a rare congenital heart defect that was successfully treated, improving the patient’s quality of life. This reinforced my commitment to continuous learning and utilizing all available resources to provide the best possible care.
Q 26. What are the legal and ethical considerations surrounding emergency veterinary care?
Legal and ethical considerations in emergency veterinary care are significant and multifaceted. Legally, we must follow established protocols for informed consent, obtaining owner authorization for procedures and treatment plans. Accurate and detailed record-keeping is crucial for legal protection, should disputes arise. We are also bound by professional standards of care, meaning we must provide the same level of skill and competence as a reasonably prudent veterinarian in similar circumstances. Failing to meet this standard could lead to malpractice claims.
Ethically, we are obligated to act in the best interest of the animal, even when facing difficult decisions, such as whether to provide extensive and potentially costly treatment or to humanely euthanize a suffering animal. Transparency and honest communication with owners are crucial to navigating these ethical dilemmas. We must balance the financial considerations with the animal’s welfare, ensuring decisions are driven by veterinary medical judgment, not financial constraints. The principles of beneficence (acting in the best interest of the animal) and non-maleficence (avoiding harm) are central to ethical decision-making.
Q 27. Describe a challenging emergency case you’ve handled and what you learned from it.
One particularly challenging case involved a dog hit by a car that arrived in critical condition. The dog had severe internal injuries, including a ruptured diaphragm, pneumothorax (collapsed lung), and liver lacerations. The initial stabilization was extremely complex, requiring immediate chest tube placement to address the pneumothorax and fluid resuscitation to counteract blood loss. The subsequent surgery was lengthy and technically demanding, necessitating coordination between multiple surgical teams.
The patient’s condition remained precarious in the post-operative period, requiring intensive care and careful monitoring of vital signs. Despite the challenges, through the collaborative efforts of the team and meticulous post-operative care, the dog eventually made a remarkable recovery. The experience reinforced the importance of rapid assessment, efficient teamwork, and persistent vigilance in managing critically ill patients. It taught me the necessity of patience, resilience, and the rewards of seeing a seemingly hopeless case achieve a favorable outcome.
Q 28. What are your continuing education plans related to emergency and critical care?
My continuing education plans are focused on staying abreast of the latest advancements in emergency and critical care. This includes attending conferences, workshops, and seminars, and actively participating in professional organizations such as the American College of Veterinary Emergency and Critical Care (ACVECC). I also regularly review veterinary journals and online resources to keep my knowledge current on new techniques, diagnostic tools, and treatment protocols. I’m particularly interested in advanced surgical techniques, pain management protocols, and the utilization of advanced imaging in emergency situations.
Furthermore, I actively participate in case reviews with colleagues, fostering a collaborative learning environment. This helps me refine my clinical skills and learn from diverse experiences. Continuing education is vital for providing high-quality emergency veterinary care and ensuring the best possible outcomes for my patients.
Key Topics to Learn for Veterinary Care and Emergency Procedures Interview
- Animal Emergency Triage: Understanding the prioritization of patients based on severity of illness or injury. This includes assessing vital signs, recognizing life-threatening conditions, and initiating immediate stabilization protocols.
- Cardiopulmonary Resuscitation (CPR) and Advanced Life Support: Practical application of CPR techniques in various animal species, including intubation, chest compressions, and medication administration. Understanding the physiological rationale behind these procedures is crucial.
- Trauma Management: Assessing and managing injuries such as fractures, lacerations, and internal bleeding. This involves proper wound care, splinting techniques, and fluid resuscitation strategies.
- Shock Management: Recognizing the different types of shock (hypovolemic, septic, etc.) and implementing appropriate treatment plans, including fluid therapy and medication administration.
- Pharmacology in Emergency Medicine: Understanding the use of common emergency drugs, their dosages, routes of administration, and potential side effects. This includes analgesics, anesthetics, and fluids.
- Fluid Therapy: Calculating fluid deficits and administering intravenous fluids to maintain hydration and blood pressure. Understanding different types of fluids and their indications is essential.
- Monitoring Techniques: Competence in using and interpreting data from various monitoring devices, such as ECGs, pulse oximeters, and blood pressure cuffs.
- Surgical Assistance in Emergencies: Understanding the role of a veterinary technician in assisting with emergency surgeries, including preparing the surgical field and providing instrument assistance.
- Disease Recognition and Treatment: Identifying common emergency conditions such as seizures, heatstroke, and poisoning, and implementing effective treatment protocols.
- Client Communication: Effectively communicating with clients about their pet’s condition, treatment plan, and prognosis during stressful emergency situations.
Next Steps
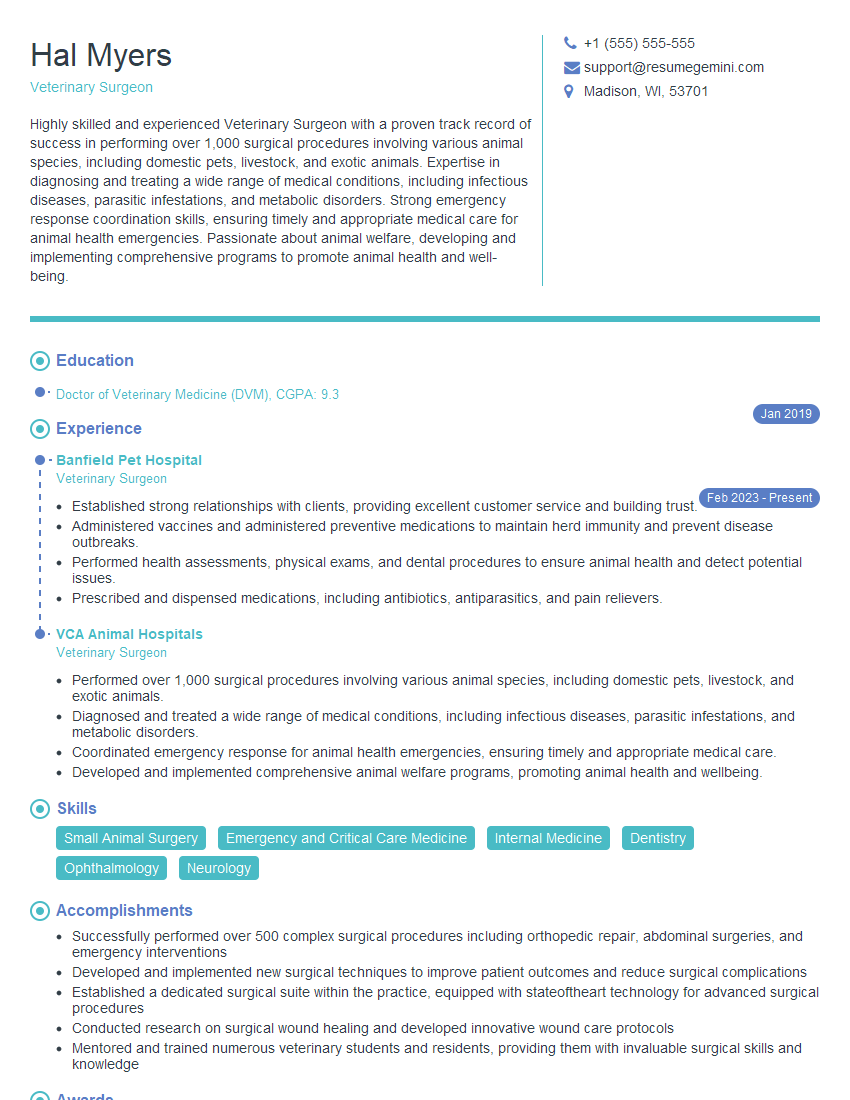
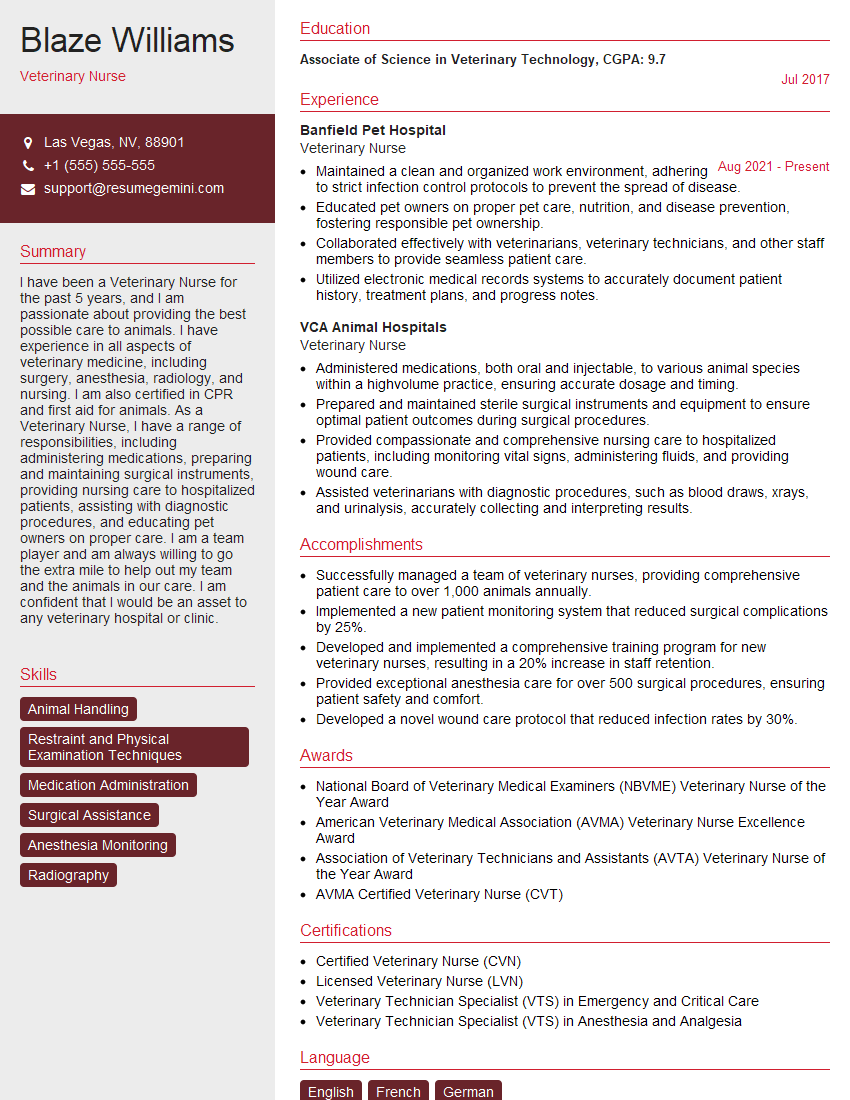
Mastering Veterinary Care and Emergency Procedures is paramount for career advancement in this demanding yet rewarding field. A strong understanding of these critical skills opens doors to specialized roles and leadership opportunities. To maximize your job prospects, creating an ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. Examples of resumes tailored to Veterinary Care and Emergency Procedures are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good