Unlock your full potential by mastering the most common Physical Therapy and Rehabilitation interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Physical Therapy and Rehabilitation Interview
Q 1. Explain the difference between Type I and Type II muscle fibers.
Type I and Type II muscle fibers are the two main types of skeletal muscle fibers, differing significantly in their contractile and metabolic properties. Think of it like this: Type I fibers are the marathon runners, while Type II fibers are the sprinters.
- Type I (Slow-twitch): These fibers are slow to contract but highly resistant to fatigue. They rely primarily on aerobic metabolism (using oxygen) for energy production. They are rich in mitochondria (the powerhouses of the cell) and myoglobin (which stores oxygen). We use these fibers for endurance activities like long-distance running or maintaining posture.
- Type II (Fast-twitch): These fibers contract rapidly but fatigue quickly. They primarily use anaerobic metabolism (without oxygen) for energy. Type II fibers are further subdivided into Type IIa (intermediate) and Type IIb (fastest), with Type IIa having some aerobic capacity. We use these fibers for powerful, short bursts of activity like sprinting or weightlifting.
Understanding this distinction is crucial in physical therapy. For example, a patient recovering from a lower extremity injury might require a program emphasizing Type I fiber training for improved endurance and functional mobility, while a patient aiming to regain strength after surgery might benefit from Type II fiber-focused exercises.
Q 2. Describe the process of gait analysis.
Gait analysis is a comprehensive assessment of a person’s walking pattern. It involves a systematic evaluation of various aspects of locomotion to identify any deviations from a normal gait, which may indicate underlying musculoskeletal or neurological impairments. Imagine it as a detailed ‘walk report’ for the body.
The process typically involves:
- Observation: Visual assessment of the patient’s walking pattern, noting posture, stride length, step width, and limb movements.
- Kinematic Analysis: Using motion capture technology (cameras or sensors) to quantify joint angles, displacement, and velocity during walking. This provides objective data on gait parameters.
- Kinetic Analysis: Measuring ground reaction forces (forces exerted by the foot on the ground) and joint moments (torques acting at joints) using force plates. This helps assess the efficiency and mechanics of movement.
- Electromyography (EMG): Recording the electrical activity of muscles during walking to identify patterns of muscle activation and coordination. This helps us determine which muscles are doing the work during specific stages of walking.
The data gathered from these methods is then analyzed to identify potential problems, such as muscle weakness, joint stiffness, or neurological deficits. This information is essential for designing an appropriate physical therapy intervention to improve gait efficiency and reduce pain or risk of falls.
Q 3. What are the contraindications for ultrasound therapy?
Ultrasound therapy, while generally safe and effective, has several contraindications, meaning situations where it should be avoided. These precautions are in place to prevent potential harm to the patient.
- Over Pregnant Uterus or Gonads: Ultrasound energy can potentially harm developing fetuses or reproductive organs.
- Malignancy: Applying ultrasound to cancerous tissues may stimulate tumor growth or spread.
- Active Hemorrhage: The heat generated by ultrasound can exacerbate bleeding.
- Deep Vein Thrombosis (DVT): The heat can increase the risk of clot dislodgement and pulmonary embolism (blood clot in the lung).
- Impaired Sensation/Cognition: Patients who cannot feel or communicate may not be able to report discomfort from the treatment.
- Infection: Applying ultrasound to an infected area can increase inflammation and spread the infection.
- Areas Over Implants: Certain implants may be affected by ultrasound energy and could malfunction or overheat.
A thorough assessment of the patient’s medical history and current condition is essential before initiating ultrasound therapy. Ignoring these contraindications could lead to serious adverse effects.
Q 4. How do you assess muscle strength?
Assessing muscle strength involves determining the maximal force a muscle or muscle group can generate. There are several methods, ranging from simple subjective assessments to more objective quantitative measures.
- Manual Muscle Testing (MMT): This is a subjective assessment where the therapist applies resistance to a patient’s voluntary movement, grading the strength on a scale of 0 to 5 (0 being no contraction, 5 being normal strength). It’s a common method, but prone to variability between testers.
- Dynamometry: Using a dynamometer (a device that measures force) provides a more objective measure of muscle strength. Different types of dynamometers exist, measuring grip strength, isometric force (static force), or isokinetic strength (force during movement at a constant speed).
- Isokinetic Testing: This involves using specialized equipment to assess strength during movement at a constant speed. It provides detailed information about muscle performance throughout the range of motion.
- Functional Strength Assessments: These assess strength in the context of functional tasks, such as sit-to-stand, stair climbing, or carrying objects. This reflects real-world strength capacity.
The choice of method depends on the patient’s condition, the specific muscle being assessed, and the available resources. It’s critical to select an assessment that aligns with the therapeutic goals and provides reliable information for guiding treatment.
Q 5. Explain the stages of wound healing.
Wound healing is a complex process involving several overlapping stages, aiming to restore tissue integrity. It’s a bit like a well-orchestrated construction project.
- Hemostasis (Immediately after injury): The body’s initial response involves controlling bleeding through blood clot formation. This stops the blood loss and creates a scaffold for the healing process.
- Inflammation (1-10 days): This phase involves vasodilation (widening of blood vessels), attracting immune cells to the wound site. Inflammation is characterized by redness, swelling, pain, and heat. It is essential for removing debris and preparing the wound for repair.
- Proliferation (3-21 days): New tissue is formed during this stage. Fibroblasts (cells that produce collagen) build a granulation tissue, which forms the base for new skin. Epithelial cells migrate to cover the wound surface.
- Maturation/Remodeling (21 days to 2 years): Collagen fibers are reorganized, increasing wound strength. Scar tissue forms, although it is never as strong as original tissue. The wound gradually fades and heals completely.
Understanding these stages is vital for physical therapists because our interventions must consider the phase of healing. For instance, early mobilization might be contraindicated during the inflammation phase, whereas gentle range of motion and wound care are appropriate. During the proliferation stage, exercises promoting collagen synthesis can be implemented.
Q 6. What are the common causes of shoulder impingement syndrome?
Shoulder impingement syndrome, often referred to as subacromial impingement, occurs when the structures within the subacromial space (the space under the acromion bone) become compressed. This compression can lead to inflammation and pain. Think of it like a crowded hallway – if too many things try to pass through a narrow space, they get pinched.
Common causes include:
- Poor Posture: Rounded shoulders (kyphosis) and forward head posture can narrow the subacromial space, increasing the risk of impingement.
- Repetitive Overhead Activities: Repeated overhead movements, as seen in sports (like swimming or baseball) or occupational tasks, can gradually irritate the rotator cuff tendons and bursa.
- Rotator Cuff Tears: Tears in the rotator cuff tendons can lead to instability and subsequent impingement of the remaining structures.
- Acromial Morphology: A hooked or curved acromion bone can reduce the space available for the tendons and bursa.
- Weakness in Scapular Stabilizers: Weakness in the muscles around the shoulder blade (scapula) can disrupt normal shoulder mechanics, increasing stress on the subacromial space.
It’s important for physical therapists to consider these various contributing factors in their assessment and treatment plan. A comprehensive approach might include posture correction exercises, strengthening exercises for the rotator cuff and scapular muscles, and manual therapy to address joint mobility restrictions.
Q 7. Describe your experience with manual therapy techniques.
My experience with manual therapy techniques is extensive. I’m proficient in a range of techniques, using them as part of a holistic approach to patient care. I always prioritize a thorough assessment to determine the most appropriate technique for each individual.
Some of the techniques I regularly employ include:
- Soft Tissue Mobilization: Techniques like massage, myofascial release, and trigger point therapy are used to address muscle tightness and fascial restrictions. This can improve range of motion and reduce pain.
- Joint Mobilization and Manipulation: These techniques are used to improve joint mobility and address joint dysfunction. These techniques are high-velocity low-amplitude movements performed safely only after a thorough assessment.
- Neural Mobilization: These techniques address nerve gliding and tension, commonly used for nerve pain, such as sciatica or carpal tunnel syndrome.
- Muscle Energy Techniques: These techniques use isometric muscle contractions to improve joint mobility and decrease pain by resetting musculotendinous junctions.
I adapt my approach based on the patient’s response and progress. For example, a patient with acute pain might benefit from gentle soft tissue mobilization and joint mobilization, while a patient with chronic pain might require a combination of techniques, including strengthening and neuromuscular re-education. The integration of manual therapy with other interventions like exercise prescription and patient education is key to achieving optimal outcomes.
Q 8. How do you treat plantar fasciitis?
Plantar fasciitis, a common cause of heel pain, involves inflammation of the plantar fascia, a thick band of tissue on the bottom of the foot. Treatment focuses on reducing inflammation, improving flexibility, and strengthening supporting muscles. My approach is multi-pronged:
Conservative Management: This forms the cornerstone of treatment and often yields excellent results. It includes rest, ice application (15-20 minutes at a time, several times a day), stretching exercises (especially the calf muscles and plantar fascia), and wearing supportive footwear with good arch support. I often guide patients through specific stretches like towel stretches and plantar fascia rolling with a frozen water bottle or massage ball.
Orthotics: Custom or over-the-counter orthotics can help redistribute pressure and support the arch, reducing strain on the plantar fascia. I’ll assess the patient’s foot structure to determine the most appropriate type.
Physical Therapy Modalities: I may utilize modalities like ultrasound therapy to reduce inflammation and promote tissue healing. Low-level laser therapy (LLLT) can also be beneficial for pain relief and tissue regeneration.
Night Splints: These keep the foot in a dorsiflexed position overnight, stretching the plantar fascia and preventing it from tightening during sleep. This is particularly useful in cases where nighttime pain is significant.
Medication: In some cases, I may recommend over-the-counter anti-inflammatory drugs (NSAIDs) like ibuprofen to manage pain and inflammation. Corticosteroid injections are considered only after other conservative measures have failed, as they can have potential side effects.
Surgical Intervention: Surgery is rarely necessary and is considered only as a last resort when all other treatment options have been exhausted.
For example, I recently treated a runner with plantar fasciitis. We started with a combination of rest, ice, stretching, and supportive shoes. We gradually progressed to incorporate strengthening exercises and night splints. Within 8 weeks, her pain was significantly reduced, and she was able to resume running with minimal discomfort.
Q 9. What is your experience with neurological rehabilitation?
I have extensive experience in neurological rehabilitation, working with patients recovering from a wide range of conditions, including stroke, traumatic brain injury (TBI), multiple sclerosis (MS), and spinal cord injury (SCI). My expertise spans across the various phases of rehabilitation, from acute care to long-term management.
My approach is patient-centered and goal-oriented, focusing on functional recovery. This involves a thorough assessment of the patient’s neurological deficits, including motor skills, balance, coordination, cognition, and communication. Based on this assessment, I develop an individualized treatment plan incorporating various therapeutic interventions:
Motor Learning Techniques: These techniques, such as task-specific training and constraint-induced movement therapy (CIMT), aim to improve motor control and function by engaging in repetitive practice of functional tasks. CIMT, for example, focuses on retraining the affected limb through repetitive practice while the unaffected limb is temporarily restrained.
Balance and Gait Training: Improving balance and gait is crucial for independence. This involves exercises to enhance postural stability, improve gait symmetry, and use assistive devices if necessary.
Cognitive Rehabilitation: Cognitive deficits are common after neurological injury. I collaborate with other specialists, such as speech-language pathologists and occupational therapists, to address cognitive impairments such as attention, memory, and executive function.
Adaptive Strategies: I work with patients to develop adaptive strategies to compensate for neurological deficits and enhance their participation in daily activities.
For instance, I worked with a patient recovering from a stroke who experienced significant weakness on one side of her body. Through intensive motor learning techniques, balance training, and adaptive strategies, she regained enough function to walk independently and return to her daily activities.
Q 10. Explain the principles of therapeutic exercise.
Therapeutic exercise is a cornerstone of physical therapy, employing planned and structured movement to improve physical function and well-being. The principles underpinning effective therapeutic exercise are multifaceted:
Specificity: Exercises must target specific impairments and functional limitations. For example, strengthening exercises for weak quadriceps are crucial for improving gait after knee surgery.
Overload: Gradual increases in the intensity or duration of exercise challenge the body to adapt and improve. This might involve increasing repetitions, weight, or resistance over time.
Progression: Exercises should progress in difficulty as the patient improves. Starting with simple movements and gradually advancing to more complex activities ensures a safe and effective approach.
Individualization: Exercises are tailored to each patient’s unique needs, abilities, and goals. A treatment plan for a marathon runner will differ significantly from that of an elderly individual recovering from a fall.
Adaptation: Treatment plans must be adaptable to the patient’s response. This requires regular monitoring and adjustments based on the patient’s progress and any setbacks.
Pain Management: Exercises should be performed within a pain-free or tolerable range to avoid exacerbating injury or discouraging the patient.
For example, when designing a program for someone recovering from a rotator cuff tear, exercises must initially focus on pain management and range of motion, before progressing to strengthening and functional activities like reaching overhead.
Q 11. How do you adapt treatment plans for patients with cognitive impairments?
Adapting treatment plans for patients with cognitive impairments requires a nuanced and patient approach. Understanding the nature and severity of the impairment is crucial. For example, someone with mild cognitive impairment will require a different approach than someone with severe dementia. Key adaptations include:
Simplified Instructions: Break down instructions into short, clear, and concise steps. Use visual aids like pictures or diagrams whenever possible. Avoid jargon.
Repetition and Reinforcement: Frequent repetition of exercises and positive reinforcement are essential to enhance learning and retention. Frequent positive feedback is key.
Environmental Modifications: Adjust the treatment environment to minimize distractions and enhance focus. A quiet, well-lit space can greatly improve a patient’s concentration.
Task-Oriented Approach: Focus on functional tasks relevant to the patient’s daily life. This makes the exercises more engaging and motivating. For example, practicing reaching for objects can be more effective than isolated range of motion exercises.
Caregiver Involvement: Involve caregivers in the treatment process to ensure consistency and support outside the therapy sessions. Home exercise programs should be easy for caregivers to implement.
Patience and Understanding: Recognize that progress may be slower and require more patience and understanding. Celebrate even small achievements to maintain motivation.
For example, when working with a patient with Alzheimer’s disease, I might use simple verbal cues combined with visual demonstrations. I would focus on functional activities like getting dressed or preparing a simple meal, breaking them down into smaller steps, and providing positive reinforcement throughout the process.
Q 12. Describe your experience with electrical stimulation modalities.
Electrical stimulation modalities are valuable tools in physical therapy, offering various therapeutic effects depending on the type of current used. My experience encompasses several modalities:
Transcutaneous Electrical Nerve Stimulation (TENS): TENS uses low-voltage electrical currents to stimulate nerves, reducing pain by releasing endorphins and altering nerve signals. I often use TENS for acute pain management, particularly in conditions like musculoskeletal pain and post-surgical pain.
Neuromuscular Electrical Stimulation (NMES): NMES uses higher-voltage currents to cause muscle contractions, improving muscle strength, reducing muscle atrophy, and improving range of motion. I utilize NMES in patients recovering from injuries, surgeries, or neurological conditions leading to muscle weakness.
Functional Electrical Stimulation (FES): FES is more sophisticated, using electrical stimulation to restore functional movement, such as assisting with walking or improving hand function. This is especially useful in patients with spinal cord injuries or stroke.
It is crucial to understand the contraindications and precautions for each modality. For example, electrical stimulation should be avoided in patients with pacemakers, over pregnant abdomens, or in areas of active bleeding. Precise electrode placement is paramount for optimal therapeutic effects and to avoid unintended stimulation. I always carefully assess each patient before using electrical stimulation, tailoring the parameters to their specific needs and carefully monitor their response during treatment.
Q 13. What are the benefits and risks of using traction therapy?
Traction therapy involves applying a pulling force to the spine, aiming to widen the intervertebral spaces, reducing pressure on nerve roots and potentially alleviating pain. However, it’s essential to weigh the benefits against the risks:
Benefits: Traction can provide temporary pain relief in conditions such as lumbar disc herniations, sciatica, and spinal stenosis by decreasing pressure on the spinal nerves and joints. It can also improve range of motion and reduce muscle spasms.
Risks: Traction is not without potential risks. These include muscle soreness, headaches, dizziness, and, in rare cases, more serious complications such as nerve damage or exacerbation of spinal instability. Certain conditions, like osteoporosis, pregnancy, or recent spinal surgery, make traction contraindicated.
Before recommending traction, I conduct a thorough examination to assess the patient’s suitability. I carefully consider their medical history, the nature of their pain, and any potential contraindications. Moreover, I explain the potential benefits and risks in detail, ensuring the patient is fully informed and consents to the procedure. The type of traction (mechanical, manual, or positional) and the parameters (duration, weight, and angle) are meticulously adjusted based on individual needs and ongoing assessment.
For example, I might recommend mechanical traction for a patient with lumbar disc herniation causing radiating leg pain, but only after ruling out contraindications and explaining the possible side effects. It would be part of a broader treatment plan also including exercises, manual therapy, and patient education.
Q 14. How do you assess and manage pain in patients?
Pain assessment and management are fundamental to physical therapy. My approach involves a comprehensive evaluation using several methods:
Subjective Assessment: I begin by carefully listening to the patient, documenting the location, quality, intensity (using a numerical rating scale – NRS or visual analogue scale – VAS), duration, and any aggravating or relieving factors of their pain.
Objective Assessment: Physical examination involves assessing range of motion, muscle strength, posture, and palpation to identify specific areas of tenderness or dysfunction.
Pain-Specific Questionnaires: Standardized questionnaires, such as the Oswestry Disability Index for back pain, may be used to objectively quantify pain and its impact on daily activities.
Pain management strategies are highly individualized. They might include:
Manual Therapy: Techniques like soft tissue mobilization, joint mobilization, and spinal manipulation can help to reduce pain and restore joint mobility.
Therapeutic Exercise: Exercises are tailored to address specific pain generators and improve overall function, including strengthening, stretching, and postural correction exercises.
Modalities: Thermotherapy, cryotherapy, ultrasound, and electrical stimulation can be used to manage pain and inflammation.
Patient Education: Educating patients about their condition, pain mechanisms, and self-management strategies is crucial for long-term pain control.
Referral: In cases of chronic or severe pain that doesn’t respond to conservative management, referral to a pain specialist or other healthcare professionals might be necessary.
For example, a patient with chronic neck pain might receive a combination of manual therapy to address joint restrictions, specific exercises to strengthen deep neck flexor muscles, and education on proper posture and ergonomics to alleviate pain and prevent recurrence.
Q 15. Describe your experience working with patients with stroke.
My experience with stroke patients spans over eight years, encompassing both inpatient and outpatient rehabilitation settings. I’ve worked with individuals experiencing a wide spectrum of stroke severity, from mild hemiparesis (weakness on one side of the body) to severe impairments affecting motor function, speech, and cognition. My approach is highly individualized, focusing on a thorough assessment to understand the patient’s specific deficits and functional goals. This involves evaluating motor skills, balance, coordination, speech, and swallowing. Based on this assessment, I develop a customized rehabilitation program targeting areas like:
- Motor recovery: Utilizing techniques such as constraint-induced movement therapy (CIMT), task-specific training, and progressive resistance exercises to improve strength, range of motion, and motor control.
- Balance and gait training: Employing various strategies, from simple balance exercises to the use of assistive devices and gait training to improve mobility and reduce fall risk.
- Cognitive rehabilitation: Incorporating exercises to improve attention, memory, and problem-solving skills, crucial for independent living.
- Activities of daily living (ADL) training: Focusing on retraining patients to perform everyday tasks like dressing, eating, and bathing independently.
I collaborate closely with other members of the healthcare team, including physicians, occupational therapists, speech-language pathologists, and nurses, to ensure a holistic and integrated approach to patient care. Success is measured not just by improvements in objective measures, but also by the patient’s ability to return to meaningful activities and improve their quality of life.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you incorporate patient education into your treatment plans?
Patient education is an integral part of my treatment philosophy. I believe that informed patients are more empowered and engaged in their recovery. My approach incorporates several strategies:
- Initial education session: At the outset of treatment, I dedicate time to explain the patient’s diagnosis, prognosis, and the overall treatment plan in clear, non-medical language. I also encourage questions and answer them thoroughly.
- Ongoing education during sessions: I integrate education seamlessly into each therapy session. For example, while practicing exercises, I explain the rationale behind each movement and the expected benefits. I also provide visual aids, such as diagrams or videos, to enhance understanding.
- Home exercise programs (HEP): I always provide patients with a written HEP that details the exercises they need to perform at home. I demonstrate each exercise correctly and ensure they understand the proper technique before sending them home. This sheet includes pictures and frequency of exercise to aid the patient.
- Resource provision: I direct patients to relevant websites, support groups, and community resources to continue learning and connect with others facing similar challenges.
- Verbal and written reinforcement: I regularly check the patient’s understanding through questions and provide written and verbal reminders and reinforcements.
My goal is to equip patients with the knowledge and skills they need to manage their condition effectively, even after their formal therapy concludes.
Q 17. What is your experience with documentation and electronic health records?
I am proficient in using electronic health records (EHR) systems and consider accurate and timely documentation crucial for effective patient care and interprofessional communication. My experience includes using various EHR platforms, including [mention specific EHR systems if comfortable, e.g., Epic, Meditech]. I am adept at accurately recording patient assessments, treatment plans, progress notes, and discharge summaries. My documentation consistently reflects the patient’s functional status, response to interventions, and goals. I understand the importance of adhering to HIPAA regulations and maintaining patient confidentiality. I am also familiar with using telehealth platforms and documentation practices in a virtual setting.
Beyond simply inputting data, I utilize the EHR system to track patient progress effectively, allowing for data-driven adjustments to the treatment plan. This facilitates efficient communication with other healthcare providers, ensuring that everyone is aligned on the patient’s care. For example, I utilize the charting system to flag any urgent situations requiring immediate attention from other medical professionals.
Q 18. Describe a challenging patient case and how you addressed it.
One challenging case involved a 72-year-old patient who suffered a severe stroke resulting in significant left-sided hemiparesis and aphasia (difficulty with speech). He was initially very discouraged and unmotivated to participate in therapy. His frustration with his communication difficulties and limited mobility was palpable.
My approach involved a multi-faceted strategy:
- Building rapport: I spent extra time in the initial sessions getting to know him and understanding his personality and preferences, focusing on active listening and empathy.
- Modifying treatment: I adjusted my treatment plan to focus on small, achievable goals initially, rather than overwhelming him with extensive exercises. I utilized alternative communication methods, such as picture cards and writing, to enhance communication.
- Incorporating family: I actively involved his family in the treatment process, educating them on how to support him at home and encouraging their active participation in therapy sessions.
- Celebrating small victories: We celebrated every milestone, however small, reinforcing his progress and boosting his confidence. This positive reinforcement was crucial for motivation.
- Utilizing technology: We incorporated assistive technology, such as communication apps, to aid in communication and independence.
Through patience, individualized adaptation, and collaborative efforts, this patient made significant progress in motor function and communication. He regained some independence in activities of daily living and showed marked improvement in mood and motivation. This case highlighted the importance of adapting treatment to the unique needs of each patient and emphasizes the power of a holistic, collaborative approach.
Q 19. How do you prioritize patient care in a busy clinical setting?
Prioritizing patient care in a busy clinical setting requires efficient time management and organizational skills. I utilize several strategies:
- Effective scheduling: I utilize the EHR system’s scheduling tools to optimize patient appointments, allocating adequate time for each patient based on their needs and treatment plan complexity.
- Prioritization matrix: I use a prioritization matrix to categorize patients based on their urgency and level of need. This ensures that patients with critical needs receive timely attention.
- Time blocking: I allocate specific blocks of time for documentation, patient interaction, and administrative tasks, minimizing interruptions and ensuring sufficient time for each activity.
- Delegation and teamwork: Where appropriate, I delegate tasks to support staff and collaborate effectively with other members of the healthcare team. For example, certain aspects of the treatment plan may be implemented by an aide while I focus on higher level interventions.
- Efficient communication: I utilize the EHR system’s messaging function for efficient communication with other healthcare providers and staff, reducing time spent on phone calls or in-person consultations.
Despite the demands of a busy setting, I remain committed to providing individualized and high-quality care to every patient.
Q 20. What are your strategies for managing patient expectations?
Managing patient expectations is crucial for a positive therapeutic alliance. I employ these strategies:
- Realistic goal setting: I work collaboratively with patients to set realistic, achievable goals that are tailored to their individual circumstances, abilities, and medical history. This involves open and honest communication about potential limitations and challenges.
- Regular progress updates: I provide regular feedback to patients regarding their progress, using both quantitative data and qualitative observations to illustrate their improvements. This helps them stay motivated and informed.
- Open communication: I maintain open communication with patients, addressing any concerns or questions they may have promptly and honestly. This fosters trust and helps manage expectations.
- Shared decision-making: I involve patients in the decision-making process, empowering them to take ownership of their treatment and recovery. This includes offering options and allowing them to participate in modifying the treatment plan if necessary.
- Realistic timelines: I avoid making promises that I cannot keep and set realistic timelines for achieving goals. It’s important to acknowledge that recovery is a journey, not a race.
By setting clear expectations from the start, maintaining open communication, and collaboratively working towards achievable goals, I aim to foster a positive and productive therapeutic relationship and ensure patient satisfaction.
Q 21. Explain the difference between active and passive range of motion exercises.
Active and passive range of motion (ROM) exercises both aim to maintain or improve joint mobility, but they differ significantly in how the movement is achieved.
- Active ROM exercises: Involve the patient actively moving their joint through its full range of motion, using their own muscle power. These exercises improve muscle strength, coordination, and neuromuscular control. Examples include actively bending and straightening the elbow, lifting the leg, or rotating the shoulder.
- Passive ROM exercises: Involve the therapist or another person moving the patient’s joint through its range of motion without the patient’s active participation. These exercises are used to maintain joint mobility, prevent contractures (shortening or tightening of muscles and tendons), and reduce pain. Passive ROM exercises are particularly useful when the patient is unable to actively move their joint due to weakness, paralysis, or pain. An example is a therapist gently moving a patient’s paralyzed leg through a range of motions.
The choice between active and passive ROM exercises depends on the patient’s specific condition and abilities. Ideally, a combination of both is used, starting with passive ROM to maintain mobility and then gradually progressing to active ROM exercises to promote strength and functional recovery.
Q 22. What is your experience with assistive devices?
My experience with assistive devices spans a wide range, from basic mobility aids like canes and walkers to more complex equipment such as wheelchairs, prosthetic limbs, and orthotics. I’m proficient in assessing a patient’s needs to determine the most appropriate device, fitting and adjusting them for optimal comfort and function, and providing thorough instruction on safe and effective use. For example, I recently worked with a patient recovering from a stroke who needed a customized wheelchair. I collaborated with an occupational therapist to assess her specific needs, considering factors such as her upper body strength, seating tolerance, and home environment. We selected a chair with adjustable features that catered to her evolving needs and provided comprehensive training to her and her caregiver on wheelchair propulsion and safety. I also have experience with instructing patients on the use of adaptive eating utensils, reaching aids, and other devices to enhance their independence in daily living activities.
Q 23. How do you assess functional mobility?
Assessing functional mobility involves a holistic approach, integrating various assessment tools and observation techniques. I typically begin with a thorough patient history, reviewing their medical records and understanding their presenting complaints. Then, I perform a physical examination, assessing range of motion, muscle strength, balance, and coordination. Functional mobility tests are crucial; these might include the Timed Up and Go (TUG) test, the Berg Balance Scale, or the Functional Gait Assessment (FGA). These tests objectively measure how quickly a patient can stand up from a chair, walk a short distance, and turn around, providing a quantitative measure of their mobility. I also observe the patient during functional tasks such as transferring from bed to chair, walking, and stair climbing, to gain insight into their functional capacity in real-world settings. The results from the assessment are used to create a personalized treatment plan targeted at improving their functional abilities. For example, if a patient struggles with balance, I might incorporate exercises to enhance proprioception and strength.
Q 24. Describe your understanding of the ICF model.
The International Classification of Functioning, Disability and Health (ICF) model provides a comprehensive framework for understanding health and disability. It moves beyond the traditional medical model by considering not only the disease or impairment but also the impact on the individual’s body functions, activities, and participation in society. The ICF model uses two main aspects: body functions and structures (impairments), and activity and participation (limitations). It also considers environmental factors and personal factors that influence the individual’s overall functioning. For example, a patient with a knee injury (body structure/function impairment) might experience difficulty walking (activity limitation) and be unable to participate in their favorite sport (participation restriction). The ICF model helps us to consider the environmental factors, such as access to appropriate assistive devices, and personal factors, such as their motivation and social support system, to develop a more holistic and effective treatment plan.
Q 25. How do you ensure patient safety during treatment sessions?
Patient safety is my utmost priority. I ensure a safe environment by properly setting up the treatment area, removing any potential hazards, and ensuring adequate lighting. I always explain the treatment procedures clearly and obtain informed consent before starting any intervention. During the treatment sessions, I monitor the patient’s vital signs, paying close attention to any signs of discomfort or distress. For instance, if a patient reports dizziness during an exercise, I immediately cease the activity and assess their condition. I regularly assess their ability to perform exercises safely and adjust the intensity and type of exercises as needed. I also utilize appropriate safety equipment like gait belts when assisting patients with ambulation or transfers. Post-treatment, I provide clear instructions on how to safely manage their condition and prevent further injuries. I also document any adverse events meticulously.
Q 26. What are your professional development goals?
My professional development goals focus on enhancing my expertise in neurological rehabilitation and expanding my knowledge of evidence-based practices. I plan to pursue advanced certification in neuro-rehabilitation techniques and stay updated on the latest advancements in technology and treatment modalities. I’m also keen on improving my skills in interprofessional collaboration by actively participating in continuing education courses and workshops focusing on teamwork and communication within the healthcare setting. I’m particularly interested in exploring the applications of virtual reality technology in physical therapy and integrating this into my clinical practice to enhance patient engagement and outcomes. Finally, I aim to become a mentor for junior physical therapists, sharing my knowledge and experience to foster the next generation of clinicians.
Q 27. Describe your experience with interprofessional collaboration.
Interprofessional collaboration is essential in providing comprehensive patient care. I regularly collaborate with physicians, occupational therapists, speech therapists, and social workers to ensure a coordinated approach. For example, I frequently work with occupational therapists to address a patient’s functional needs and activities of daily living (ADL) skills. A recent case involved a patient with a spinal cord injury. I worked closely with the occupational therapist to design an adaptive exercise program to strengthen upper body strength for transfers and ADLs. The collaboration ensured that the rehabilitation plan was holistic and addressed all the patient’s needs. We also routinely share progress notes and treatment plans to ensure everyone is on the same page. Clear communication and mutual respect are crucial for effective interprofessional collaboration. I actively participate in team meetings and case conferences, contributing my expertise and perspectives to help optimize patient outcomes.
Q 28. How do you handle conflict with colleagues or patients?
Conflict resolution is a vital skill for effective teamwork and patient care. My approach emphasizes open communication, active listening, and empathy. If a conflict arises with a colleague, I address it directly and professionally. I strive to understand their perspective, find common ground, and reach a mutually acceptable solution through respectful dialogue. If the conflict cannot be resolved internally, I will seek mediation from a supervisor or other appropriate personnel. With patients, I address concerns empathetically and clearly, explaining the rationale behind my recommendations and considering their perspectives and preferences. For instance, if a patient is hesitant to perform a particular exercise, I will try to understand their concerns, allay their anxieties, and perhaps modify the exercise to make it more comfortable and achievable. My goal is always to create a collaborative relationship built on trust and mutual respect, ensuring the best possible treatment experience for the patient.
Key Topics to Learn for Physical Therapy and Rehabilitation Interview
- Musculoskeletal System: Understanding anatomy, biomechanics, and common pathologies affecting the musculoskeletal system. Consider practical application in assessing range of motion, muscle strength, and identifying movement impairments.
- Neuromuscular Rehabilitation: Explore the principles of neurological rehabilitation, including techniques for managing conditions like stroke, spinal cord injury, and multiple sclerosis. Focus on practical application in designing individualized treatment plans.
- Cardiopulmonary Rehabilitation: Understand the principles of cardiopulmonary rehabilitation and their application to patients with cardiovascular and respiratory conditions. Consider how you would assess a patient’s functional capacity and design a safe and effective exercise program.
- Therapeutic Exercise and Modalities: Master the application of various therapeutic exercises and modalities, including manual therapy techniques, electrotherapy, and thermotherapy. Be prepared to discuss the rationale for your choices and potential contraindications.
- Patient Assessment and Treatment Planning: Demonstrate a thorough understanding of the patient assessment process, including subjective and objective data collection. Practice formulating evidence-based treatment plans tailored to individual patient needs and goals.
- Ethical and Legal Considerations: Discuss professional ethics, patient confidentiality, and legal implications relevant to physical therapy practice. Consider scenarios involving informed consent and documentation.
- Evidence-Based Practice: Showcase your ability to critically appraise research and apply evidence-based principles to clinical decision-making. Be ready to discuss how you stay updated on the latest research and clinical guidelines.
Next Steps
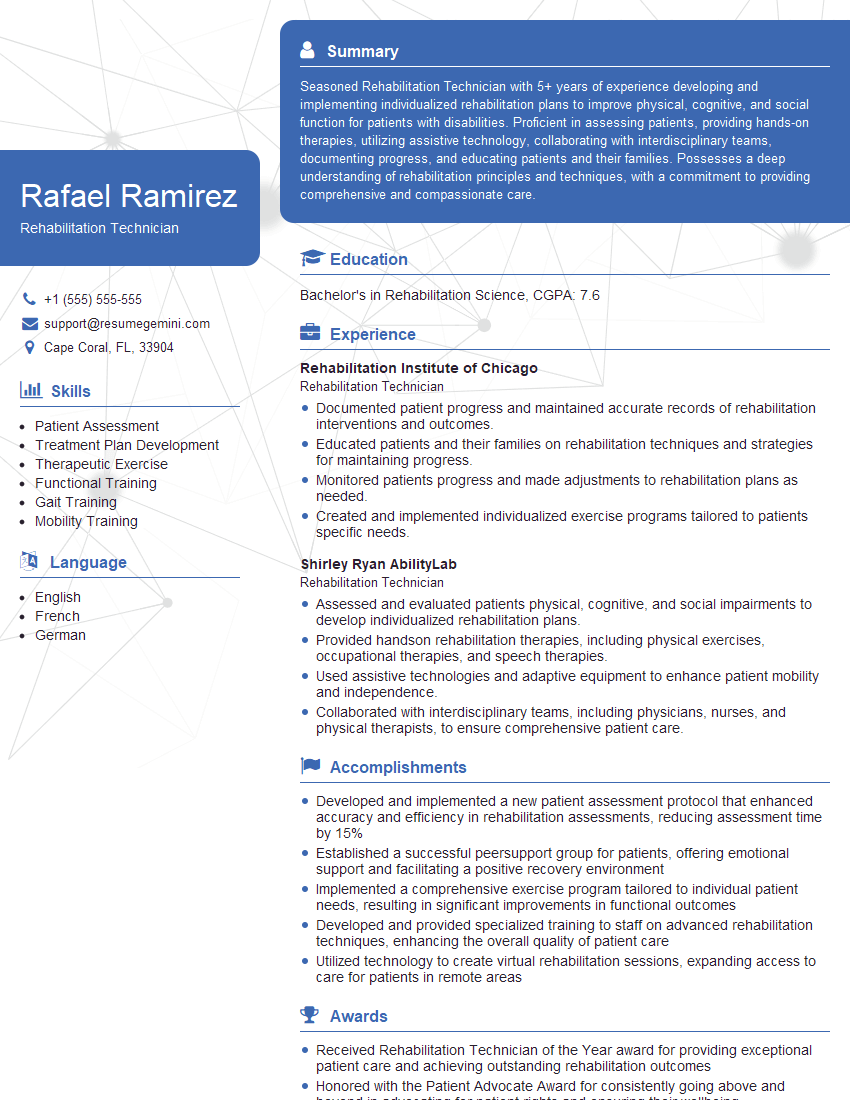
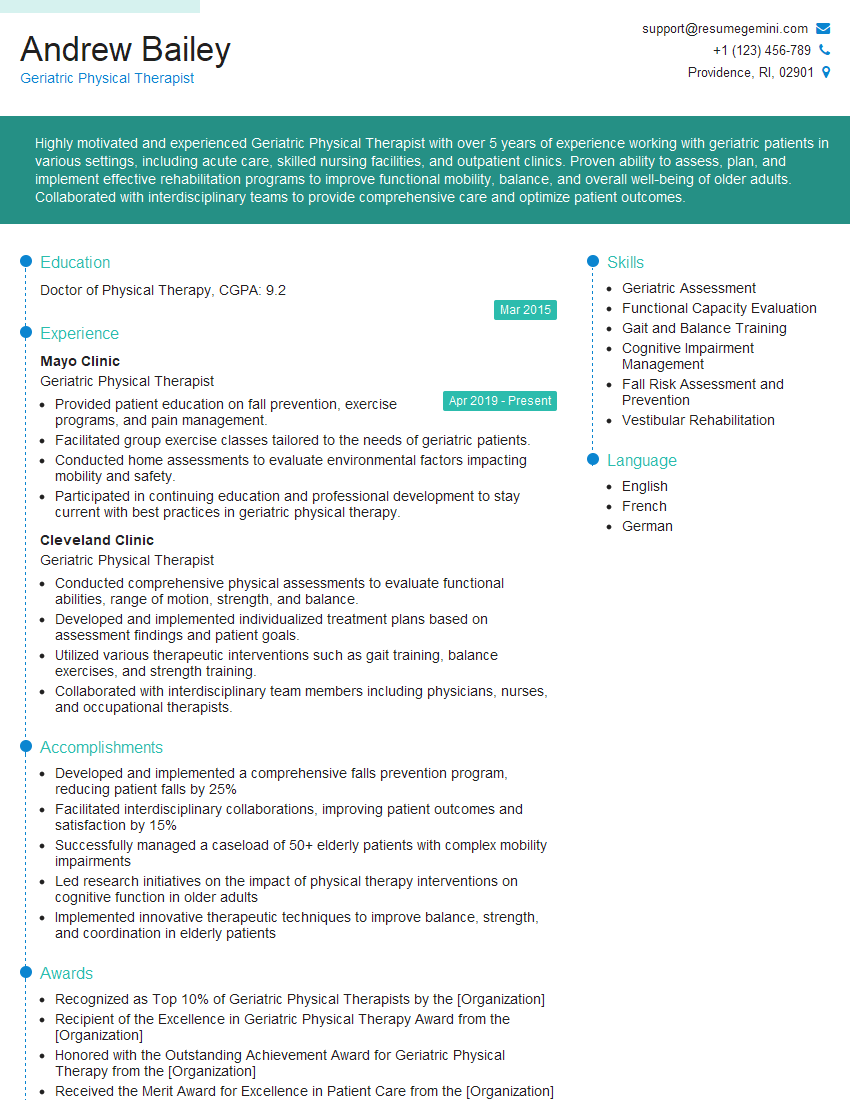
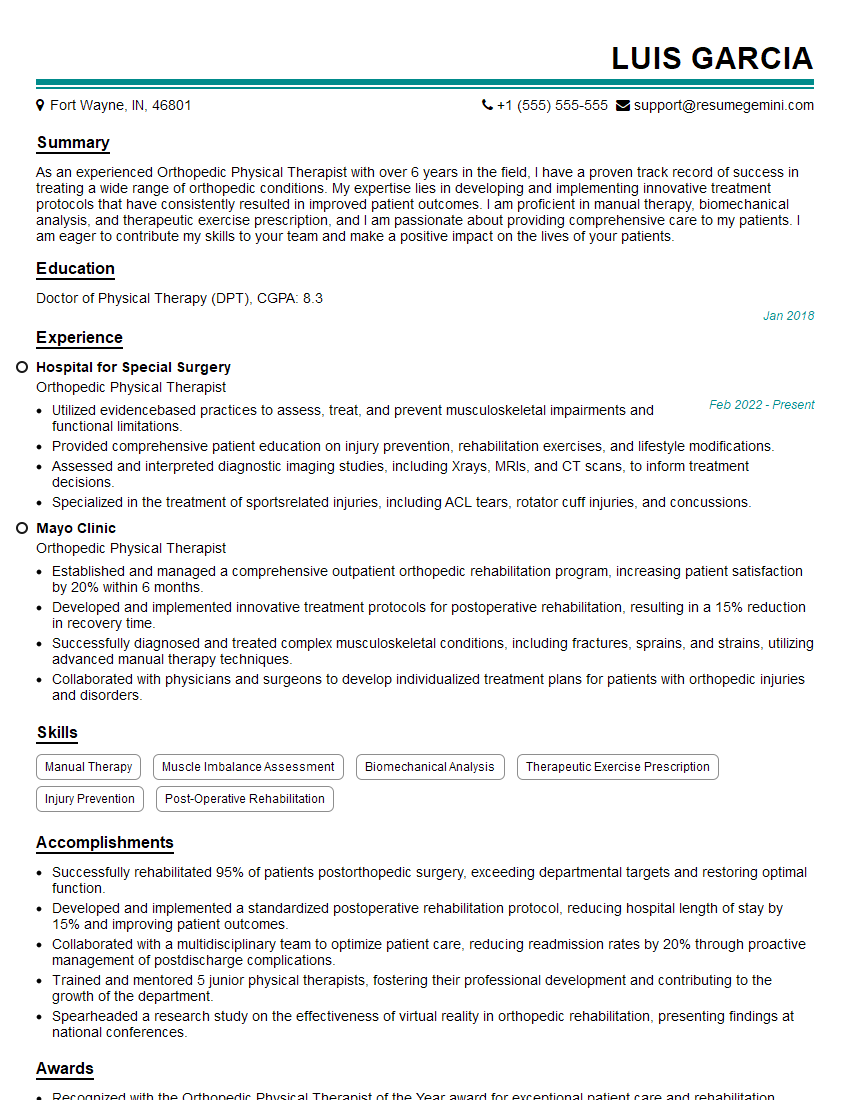
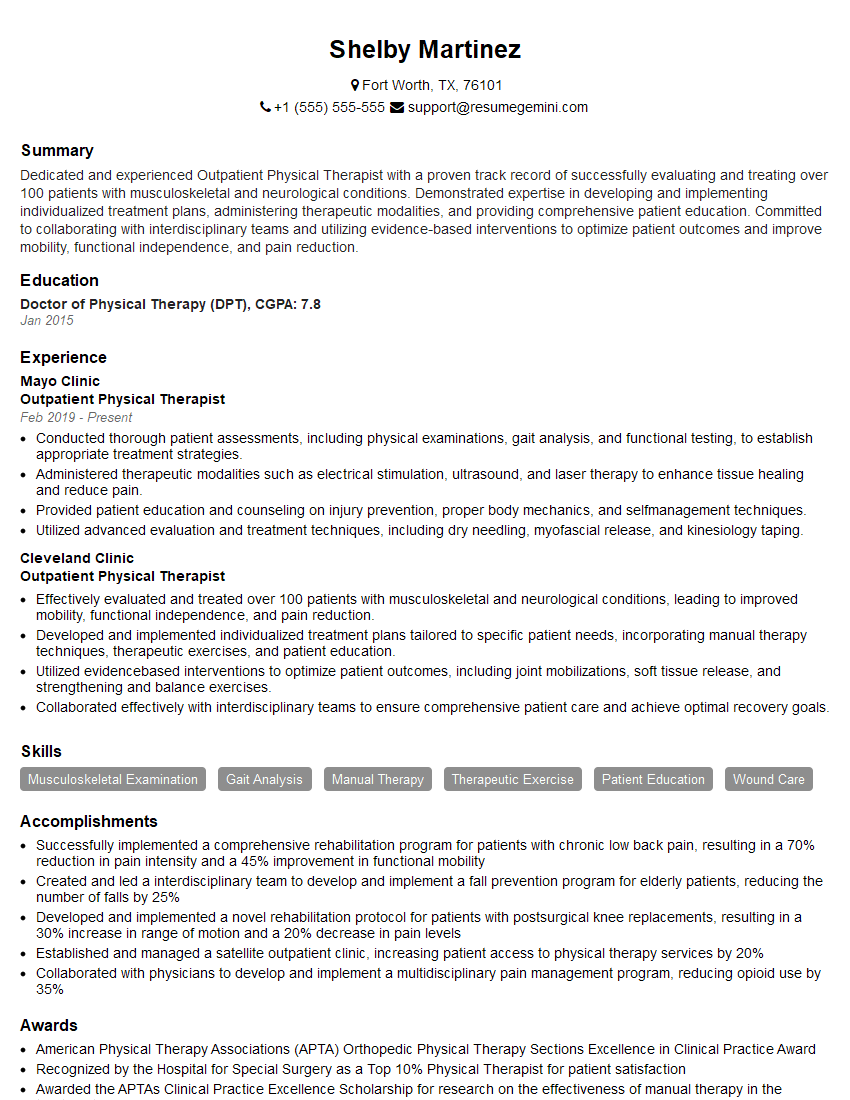
Mastering these key areas in Physical Therapy and Rehabilitation is crucial for a successful and rewarding career. A strong foundation in these topics will not only impress potential employers but will also equip you with the skills to provide exceptional patient care. To significantly boost your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that gets noticed by recruiters. We offer examples of resumes tailored specifically to Physical Therapy and Rehabilitation to help you get started. Invest time in crafting a compelling resume – it’s your first impression and a key to unlocking your career potential.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good