Are you ready to stand out in your next interview? Understanding and preparing for Cell Culture and Microbiology interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Cell Culture and Microbiology Interview
Q 1. Describe the different types of cell cultures.
Cell cultures are broadly classified into three main types based on their origin and characteristics: primary, secondary, and cell lines.
- Primary cell cultures: These are cultures derived directly from a tissue or organ. They retain the characteristics of the original tissue, making them ideal for studying specific cell types in their native environment. However, they have a limited lifespan and are prone to senescence (aging). Think of them as freshly harvested fruit – delicious but with a short shelf life. Example: Fibroblasts isolated directly from a skin biopsy.
- Secondary cell cultures: These are cultures derived from a primary culture by subculturing (passaging) the cells. They possess some characteristics of the original tissue but may exhibit some changes due to the subculturing process. They have a longer lifespan than primary cultures but still have a limited number of passages before senescence. Imagine these as fruit that has been carefully processed and preserved to extend its lifespan, though it may not be quite as fresh as the primary harvest. Example: A second generation of fibroblasts grown from a primary culture.
- Cell lines: These are immortalized cell cultures capable of unlimited proliferation. They are often derived from primary cultures that have undergone transformation (e.g., spontaneous or induced by viral infection). Cell lines are convenient for research because of their unlimited lifespan, but their characteristics may differ significantly from the original tissue due to the transformation process. They’re like fruit that’s been genetically modified to last indefinitely, though it might taste a little different. Example: HeLa cells (immortalized cervical cancer cells).
Q 2. Explain the principles of aseptic technique in cell culture.
Aseptic technique is paramount in cell culture to prevent contamination by unwanted microorganisms (bacteria, fungi, yeast, mycoplasma). It involves a series of practices aimed at maintaining sterility throughout the entire cell culture process. Think of it as creating a sterile micro-environment within the lab to protect your precious cells.
- Sterile workspace: Using a laminar flow hood or biosafety cabinet to provide a clean air environment.
- Sterile materials: Using only sterile media, reagents, and equipment. This often involves autoclaving (high-pressure steam sterilization) or using pre-sterilized disposables.
- Proper hand hygiene: Washing hands thoroughly with soap and water before and after handling cell cultures, and wearing gloves.
- Sterile procedures: Performing all cell culture manipulations in a careful and controlled manner to avoid introducing contaminants. This includes techniques like flaming the necks of bottles and using sterile pipettes.
- Regular monitoring: Closely inspecting cell cultures for any signs of contamination (e.g., turbidity, change in media color, unusual morphology).
Failure to maintain aseptic techniques can lead to significant problems, including loss of valuable cell cultures, compromised experimental results and potential health hazards.
Q 3. What are the common contaminants found in cell cultures and how are they controlled?
Common contaminants in cell cultures include bacteria, yeast, fungi, and mycoplasma. Bacterial contamination is often readily visible as cloudiness or turbidity in the culture medium, along with a change in pH. Yeast and fungi may present as clumps or filaments. Mycoplasma contamination, however, is insidious because it’s often undetectable without specific testing. The consequences of contamination can range from subtle changes in cell behavior to complete loss of the culture.
- Control strategies: Aseptic techniques are the first line of defense. Additional measures include regular visual inspection of cell cultures, routine testing for mycoplasma contamination, and using antibiotics (although this should be done cautiously and only when necessary due to the risk of antibiotic resistance and masking of subtle contamination). Discarding contaminated cultures immediately and thoroughly cleaning the work area is crucial.
Remember, prevention is far better than cure. Strict adherence to aseptic techniques is the most effective way to control contaminants.
Q 4. How do you assess cell viability?
Assessing cell viability is critical to ensure the health and functionality of your cell cultures. Several methods exist, each with its strengths and weaknesses. A combination of techniques is often employed for the most accurate assessment.
- Trypan blue exclusion assay: This is a widely used method based on the principle that live cells with intact membranes exclude the dye trypan blue, while dead cells with compromised membranes take up the dye. Cells are stained with trypan blue, and the percentage of live (unstained) cells is determined using a hemocytometer.
- MTT assay: This colorimetric assay measures cell metabolic activity, indirectly reflecting viability. Live cells reduce MTT (a yellow tetrazolium dye) to formazan (a purple formazan dye), the amount of which can be quantified using a spectrophotometer.
- Resazurin assay: Similar to MTT assay, this measures cell metabolic activity. Resazurin (a non-fluorescent blue dye) is reduced by metabolically active cells to resorufin (a pink fluorescent dye), allowing for quantification using fluorescence or absorbance.
- Automated cell counters: These instruments provide faster and more objective cell counts and viability assessment compared to manual hemocytometer methods.
The choice of method depends on the specific application and resources available. For instance, trypan blue is simple and inexpensive, but less precise than automated cell counters.
Q 5. Describe different cell culture media and their applications.
Cell culture media provide essential nutrients and growth factors for cell survival and proliferation. Different cell types have different nutritional requirements, necessitating a variety of media formulations.
- Basal media: These provide basic nutrients like amino acids, vitamins, and salts. Examples include DMEM (Dulbecco’s Modified Eagle Medium) and RPMI 1640, commonly used for many cell types.
- Serum-supplemented media: Basal media are often supplemented with serum (typically fetal bovine serum or FBS), which provides growth factors, hormones, and attachment factors. The serum concentration varies depending on cell type and experimental requirements.
- Serum-free media: These are designed to eliminate the variability associated with serum. They are more defined and reproducible, but often more expensive and require specific growth supplements.
- Specialty media: Some cells require specific media formulations to support their growth. For example, neurobasal media is specifically designed for neuronal cells.
The choice of media is crucial for successful cell culture. Using the wrong media can lead to poor cell growth, altered cell behavior, and experimental artifacts. It’s important to research and select the appropriate media for your specific cell type and experimental objectives.
Q 6. Explain the process of subculturing cells.
Subculturing, also known as passaging, is the process of transferring cells from a confluent (overgrown) culture to a new vessel with fresh medium. This is necessary to provide cells with enough space to grow and prevent contact inhibition. It’s akin to giving your plants a larger pot when they outgrow their current one.
- Trypsinization: Cells are detached from the culture vessel using trypsin, a protease enzyme that breaks down cell-to-cell and cell-to-substrate adhesion. This step is crucial for cells grown as monolayers (attached to the surface of a flask or dish).
- Centrifugation (optional): Cells are spun down to create a pellet, allowing for removal of the trypsin and other media components.
- Resuspension: The cell pellet is resuspended in fresh medium.
- Counting and Dilution: The cell suspension is counted (e.g., using a hemocytometer) to determine cell density, and then appropriately diluted to the desired seeding density in new culture vessels.
- Incubation: The cells are placed in an incubator to allow for attachment and growth.
The frequency of subculturing depends on the growth rate of the cell type and the desired cell density. Over-confluent cultures are stressed and may exhibit altered behavior.
Q 7. What are the different methods for cryopreservation of cells?
Cryopreservation is the process of storing cells at ultra-low temperatures (-80°C or lower) to maintain their viability and prevent degradation. This is essential for long-term storage of cell lines and primary cultures.
- Slow freezing: This method involves a controlled rate of freezing (typically 1-2°C per minute) using a controlled-rate freezer or a freezing container with isopropyl alcohol. This slow freezing minimizes ice crystal formation, which can damage cells. A cryoprotective agent (CPA), such as DMSO or glycerol, is added to the cell suspension to prevent ice crystal formation and protect cell membranes.
- Vitrification: This method involves extremely rapid freezing, often using liquid nitrogen vapor, resulting in a glassy or “vitrified” state. Vitrification bypasses ice crystal formation, potentially preserving cells with higher viability than slow freezing but often requiring specialized equipment.
After freezing, cells are stored in liquid nitrogen (-196°C) for long-term preservation. Proper thawing procedures are equally important to maintain cell viability. The choice between slow freezing and vitrification depends on cell type, available resources and desired preservation efficiency.
Q 8. How do you maintain a sterile environment in a cell culture laboratory?
Maintaining sterility in a cell culture lab is paramount to prevent contamination and ensure reliable experimental results. It’s like preparing a pristine operating room for surgery – every detail matters. We achieve this through a multi-pronged approach:
Environmental Control: Laminar flow hoods provide a sterile work area by filtering air to remove particles and microorganisms. Regular cleaning and UV sterilization of the hood are crucial. The entire lab is kept clean and disinfected regularly using appropriate disinfectants like 70% ethanol.
Aseptic Techniques: Proper hand hygiene, sterile gloves, and meticulous work practices are essential. This includes working near the flame of a Bunsen burner to create an upward air current, minimizing airborne contamination. All materials and equipment coming into contact with the cells must be sterile.
Sterilization of Media and Equipment: Growth media are sterilized using autoclaving (high-pressure steam sterilization), while other equipment (e.g., glassware, instruments) can be autoclaved or sterilized using dry heat or filtration (for heat-sensitive materials).
Regular Monitoring: We routinely monitor the sterility of our cultures through visual inspection and sometimes through sterility testing using appropriate media. Any sign of contamination necessitates immediate action, which might include discarding contaminated cultures and thoroughly decontaminating the work area.
Q 9. What are the different types of microbial growth media?
Microbial growth media are carefully formulated nutrient solutions that support the growth of microorganisms. The type of media used depends on the specific organism being cultured and the purpose of the experiment. Think of it like providing a tailored diet for your microbial guests!
Defined Media: The exact chemical composition is known. They’re great for studying specific metabolic pathways because you control every ingredient.
Complex Media: The exact chemical composition is unknown, typically containing extracts like yeast extract or beef extract, which provide a rich source of nutrients. They’re more versatile and easier to prepare, perfect for general cultivation.
Selective Media: Contains components that inhibit the growth of certain organisms while allowing others to grow. Imagine a bouncer at a club, letting only certain ‘guests’ inside.
Differential Media: Allows the distinction of different organisms based on their growth characteristics. For example, some bacteria might produce a color change in the media, making identification easier.
Enrichment Media: Provides specific nutrients to support the growth of a particular organism that might be present in low numbers in a sample.
Q 10. Explain the principles of microbial identification.
Microbial identification involves a systematic approach to determine the species or strain of a microorganism. It’s like a detective investigation, using various clues to pinpoint the identity of the ‘suspect.’
Morphological Characteristics: Observing the shape, size, arrangement, and staining properties of the microorganism under a microscope.
Physiological and Biochemical Tests: Assessing metabolic capabilities, such as the ability to ferment specific sugars, produce enzymes, or grow under different environmental conditions. Think of it as testing the microbe’s ‘skills’ and preferences.
Genetic Analysis: Utilizing techniques such as 16S rRNA sequencing (for bacteria) to analyze the organism’s genetic material, providing a highly accurate identification. This is like examining the microbe’s DNA ‘fingerprint.’
Immunological Methods: Employing antibody-based techniques (e.g., ELISA) to detect specific microbial antigens, essentially using antibodies to ‘recognize’ the microorganism.
Often, a combination of these methods is used to ensure accurate identification.
Q 11. Describe different methods for sterilization.
Sterilization is the complete removal or destruction of all forms of microbial life. It’s a critical step in maintaining sterility in any microbiology or cell culture laboratory. Think of it as eliminating all potential contaminants.
Autoclaving: Uses high-pressure saturated steam to achieve sterilization. It’s highly effective for most materials except those that are heat-sensitive.
Dry Heat Sterilization: Uses high temperatures in the absence of moisture. It’s useful for materials that cannot be autoclaved, such as glassware and metal instruments, but requires longer exposure times.
Filtration: Passes liquids or gases through a membrane filter with pores small enough to trap microorganisms. This is ideal for heat-sensitive materials like some media or solutions.
Gas Sterilization (Ethylene Oxide): Uses ethylene oxide gas to sterilize heat-sensitive medical equipment and other materials. It’s effective but requires special safety precautions because it’s a toxic gas.
Radiation Sterilization: Uses ionizing radiation (gamma or electron beams) to sterilize medical supplies and other items. Very effective but requires specialized equipment.
Q 12. What are the common bacterial staining techniques?
Bacterial staining techniques are essential for visualizing bacteria under a microscope, enhancing our ability to observe their morphology, size, and arrangement. It’s like highlighting the bacteria to make them easier to see.
Gram Staining: A differential staining technique that classifies bacteria into Gram-positive and Gram-negative based on differences in their cell wall structure. This is arguably the most important staining technique in microbiology.
Acid-Fast Staining: Identifies bacteria with a waxy cell wall, like Mycobacterium tuberculosis. These bacteria resist conventional staining methods.
Endospore Staining: Detects endospores, resistant structures formed by some bacteria under adverse conditions.
Capsule Staining: Visualizes the capsule, a polysaccharide layer surrounding some bacteria.
Flagella Staining: Visualizes flagella, the structures responsible for bacterial motility.
Q 13. Explain the process of Gram staining and its significance.
Gram staining is a crucial differential staining technique that distinguishes between Gram-positive and Gram-negative bacteria based on their cell wall composition. It’s like using a special dye to reveal hidden structural differences. The process involves several steps:
Crystal violet (primary stain): Both Gram-positive and Gram-negative cells stain purple.
Gram’s iodine (mordant): Forms a complex with crystal violet, trapping it inside the cell wall.
Alcohol (decolorizer): This is the crucial step. Gram-positive cells retain the crystal violet-iodine complex, while Gram-negative cells lose it, decolorizing.
Safranin (counterstain): Stains the decolorized Gram-negative cells pink or red.
Significance: Gram staining provides essential information for bacterial identification and guides treatment decisions. Gram-positive and Gram-negative bacteria often have different sensitivities to antibiotics, making this a critical tool for clinical microbiology.
Q 14. How do you perform a bacterial culture?
Performing a bacterial culture involves growing bacteria in a controlled environment to obtain a visible colony, allowing for identification and further study. It’s like providing a suitable environment for bacteria to thrive and multiply.
Sample Collection: Obtain a sample containing the bacteria of interest. This could be from various sources, such as a clinical specimen, environmental sample, or a pure culture.
Inoculation: Introduce the sample onto an appropriate growth medium (e.g., agar plate, broth). This can be done using various techniques, including streaking, spreading, or pouring.
Incubation: Place the inoculated medium under optimal conditions for bacterial growth (temperature, humidity, and atmosphere). The incubator provides a stable and controlled environment to promote bacterial growth.
Incubation: Place the inoculated medium under optimal conditions for bacterial growth (temperature, humidity, and atmosphere). The incubator provides a stable and controlled environment to promote bacterial growth.
Observation and Isolation: After incubation, observe the growth characteristics (colony morphology, pigmentation, etc.). If necessary, perform further isolation techniques to obtain pure cultures.
Identification: Employ various identification methods (staining, biochemical tests, molecular methods) to identify the bacteria.
Q 15. What are the different types of microbial metabolism?
Microbial metabolism encompasses all the biochemical processes within a microorganism that allow it to acquire and utilize energy and nutrients for growth and reproduction. It’s essentially how microbes ‘eat’ and ‘live’. These processes are incredibly diverse, depending on the organism and its environment.
- Chemoorganotrophs: Obtain energy from organic compounds. Think of E. coli fermenting sugars in your gut to produce energy for itself. This can involve fermentation (anaerobic) or respiration (aerobic or anaerobic).
- Chemolithotrophs: Obtain energy from inorganic compounds, like ammonia or hydrogen sulfide. These are often found in extreme environments, like deep-sea vents, where they play a crucial role in nutrient cycling.
- Phototrophs: Obtain energy from light. Cyanobacteria, for example, are photosynthetic microbes that produce oxygen as a byproduct – incredibly important for our planet’s atmosphere.
- Heterotrophs: Obtain carbon from organic compounds. Many bacteria and fungi fall under this category, needing to consume pre-formed organic molecules for their carbon source.
- Autotrophs: Obtain carbon from inorganic sources like carbon dioxide. This is characteristic of plants and certain bacteria (like cyanobacteria) that can synthesize organic molecules from CO2 through photosynthesis or chemosynthesis.
Understanding microbial metabolism is crucial in various fields, from developing new antibiotics that target specific metabolic pathways to designing bioremediation strategies where microbes are utilized to clean up pollutants.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the different types of microbial infections.
Microbial infections can be broadly classified based on several factors, including the site of infection, the type of microorganism, and the host’s immune response.
- Localized Infections: Confined to a specific area of the body, such as a skin boil (caused by Staphylococcus aureus) or a urinary tract infection (UTI, often caused by E. coli).
- Systemic Infections: Spread throughout the body via the bloodstream. Sepsis, a life-threatening condition, is a classic example of a systemic infection caused by the body’s overwhelming response to infection.
- Primary Infections: The initial infection in a previously healthy individual.
- Secondary Infections: Occur as a consequence of a primary infection, often due to weakened immunity. For example, a viral respiratory infection can weaken the lungs, making them susceptible to a secondary bacterial pneumonia.
- Acute Infections: Develop rapidly and have a relatively short course, such as strep throat.
- Chronic Infections: Develop slowly and persist for a long time, such as tuberculosis.
The classification helps in understanding the severity and appropriate treatment strategies for various microbial infections. For instance, a localized infection might be treatable with topical antibiotics, whereas a systemic infection would require intravenous antibiotics and possibly intensive care.
Q 17. Explain the principles of antimicrobial susceptibility testing.
Antimicrobial susceptibility testing (AST) determines the effectiveness of antimicrobial agents (antibiotics, antifungals, etc.) against a specific microorganism. It’s vital for guiding appropriate treatment decisions and preventing the development of antimicrobial resistance.
The most common method is the disk diffusion test (Kirby-Bauer test). A bacterial lawn is inoculated on an agar plate, and antibiotic disks are placed on the surface. After incubation, the zones of inhibition (areas around the disks where bacterial growth is inhibited) are measured. Larger zones indicate greater susceptibility to the antibiotic.
Minimum Inhibitory Concentration (MIC) testing determines the lowest concentration of an antimicrobial agent that inhibits visible bacterial growth. This can be done using broth microdilution or other automated methods. MIC values provide a quantitative measure of susceptibility.
Minimum Bactericidal Concentration (MBC) testing determines the lowest concentration of an antimicrobial agent that kills a predetermined percentage (e.g., 99.9%) of the bacterial population. This method is typically used to assess the bactericidal activity of an antimicrobial agent, distinguishing it from bacteriostatic agents that only inhibit growth.
AST results are interpreted using standardized guidelines to categorize organisms as susceptible, intermediate, or resistant to specific antimicrobial agents. These results are crucial for guiding clinical decisions and ensuring effective treatment of bacterial infections while minimizing the contribution to antibiotic resistance.
Q 18. What are the safety precautions to be taken while handling microbial cultures?
Handling microbial cultures requires strict adherence to safety protocols to prevent accidental exposure and contamination. The key is to treat all cultures as potentially harmful.
- Biosafety Cabinets (BSCs): Work within a BSC to contain aerosols and protect both the user and the environment.
- Personal Protective Equipment (PPE): Always wear lab coats, gloves, and eye protection. Depending on the biosafety level, additional PPE might be needed (e.g., respirators).
- Sterile Techniques: Employ proper aseptic techniques to prevent contamination of cultures and work surfaces. This includes sterilizing equipment and working near a flame to create an upward air current.
- Waste Disposal: Dispose of contaminated materials properly according to institutional guidelines. This often involves autoclaving or chemical disinfection before discarding.
- Training and Competency: Ensure adequate training on safety procedures and handling techniques before working with microbial cultures. Always follow established protocols and procedures.
- Decontamination: Regularly decontaminate work surfaces and equipment using appropriate disinfectants.
Failure to follow these safety precautions can lead to serious health consequences for the laboratory personnel and potential environmental contamination.
Q 19. Describe the importance of quality control in microbiology.
Quality control (QC) in microbiology is essential for ensuring the accuracy, reliability, and reproducibility of laboratory results. It involves a systematic approach to monitoring and verifying all aspects of the laboratory process, from sample collection to reporting.
- Media QC: Testing sterility and functionality of growth media before use. This is done through sterility checks (incubation) and growth promotion tests (inoculation with known organisms).
- Reagent QC: Verification of the quality and purity of reagents and chemicals.
- Equipment QC: Regular calibration and maintenance of equipment like autoclaves, incubators, and microscopes to ensure consistent and accurate performance.
- Personnel QC: Implementing training programs and proficiency testing to maintain the competence of laboratory personnel.
- Strain Identification QC: Using well-characterized control strains to verify the accuracy of identification methods.
- External QC: Participation in proficiency testing programs to compare results with other laboratories and ensure consistent quality.
Robust QC measures are crucial for ensuring the reliability of diagnostic tests, preventing misdiagnosis, and maintaining the integrity of research findings. Inaccurate results can have serious implications for patient care and public health.
Q 20. How do you troubleshoot common problems in cell culture?
Troubleshooting cell culture problems often involves a systematic approach. It’s like detective work – you need to identify clues and systematically eliminate possibilities.
Common Problems and Troubleshooting Steps:
- Contamination (bacterial, fungal, yeast):
- Visual Inspection: Look for turbidity, unusual color changes, or unusual morphology under the microscope.
- Microbial Tests: Perform Gram staining and/or culture to identify the contaminant.
- Prevention: Sterile technique, proper aseptic handling, regular cleaning and disinfection.
- Low Cell Growth:
- Check Media: Ensure proper nutrients, pH, and sterility of the culture media.
- Assess Cell Viability: Use trypan blue exclusion test to assess the percentage of viable cells.
- Incubation Conditions: Ensure appropriate temperature, CO2 concentration, and humidity.
- Cell Death/Detachment:
- Check for Mycoplasma: Mycoplasma contamination can cause cell death and detachment; test regularly.
- Culture Conditions: Ensure proper media, temperature, and passage frequency.
- Substratum: Check the suitability of the culture flask or plates.
- High Cell Density:
- Passage Cells: Subculture to lower the cell density.
- Media Changes: Replace the media more frequently.
Keeping detailed records is crucial. This helps in identifying trends and patterns, which can facilitate faster troubleshooting in the future.
Q 21. Explain the concept of cell cycle and its regulation.
The cell cycle is an ordered series of events that culminates in cell growth and division into two daughter cells. It’s a highly regulated process with checkpoints to ensure accuracy.
The main phases are:
- G1 (Gap 1): Cell growth and preparation for DNA replication. A critical checkpoint (restriction point) ensures the cell is ready to proceed.
- S (Synthesis): DNA replication occurs.
- G2 (Gap 2): Cell continues to grow and prepares for mitosis. Another checkpoint ensures DNA replication is complete and accurate.
- M (Mitosis): The process of nuclear division, followed by cytokinesis (cytoplasmic division). Further checkpoints ensure proper chromosome segregation.
Regulation is achieved primarily through cyclin-dependent kinases (CDKs) and cyclins. CDKs are enzymes that require cyclins (regulatory proteins) to become active. Different cyclins are expressed at different stages of the cell cycle, driving the progression through each phase. Tumor suppressor proteins, like p53, act as checkpoints, halting the cycle if errors are detected.
Dysregulation of the cell cycle is a hallmark of cancer. Mutations affecting CDKs, cyclins, or tumor suppressors can lead to uncontrolled cell growth and division, ultimately forming tumors.
Q 22. Describe the different stages of mitosis and meiosis.
Mitosis and meiosis are both types of cell division, but they serve very different purposes. Mitosis is responsible for cell growth and repair, producing two identical daughter cells from a single parent cell. Meiosis, on the other hand, is involved in sexual reproduction, generating four genetically diverse haploid gametes (sperm or egg cells) from a single diploid parent cell.
- Mitosis: This process occurs in four main stages:
- Prophase: Chromosomes condense and become visible, the nuclear envelope breaks down, and the mitotic spindle forms.
- Metaphase: Chromosomes align at the metaphase plate (the center of the cell).
- Anaphase: Sister chromatids separate and move to opposite poles of the cell.
- Telophase: Chromosomes decondense, the nuclear envelope reforms, and cytokinesis (division of the cytoplasm) occurs, resulting in two identical daughter cells.
- Meiosis: This process involves two rounds of cell division – Meiosis I and Meiosis II.
- Meiosis I: This is a reductional division, reducing the chromosome number by half. Key events include homologous chromosome pairing (synapsis), crossing over (exchange of genetic material between homologous chromosomes), and separation of homologous chromosomes.
- Meiosis II: This is an equational division, similar to mitosis, where sister chromatids separate. The result is four haploid daughter cells, each with a unique combination of genetic material due to crossing over and independent assortment of chromosomes.
Think of it like this: mitosis is like photocopying a document – you get two identical copies. Meiosis is like shuffling a deck of cards and dealing out four unique hands – each hand (gamete) is different from the others.
Q 23. What is the difference between prokaryotic and eukaryotic cells?
The primary difference between prokaryotic and eukaryotic cells lies in the presence or absence of a membrane-bound nucleus and other organelles. Prokaryotic cells, such as bacteria and archaea, are simpler and lack a defined nucleus; their genetic material is located in a region called the nucleoid. Eukaryotic cells, including plant, animal, fungal, and protist cells, are more complex and possess a true nucleus containing their DNA, as well as various membrane-bound organelles that perform specific functions.
- Prokaryotic Cells: Generally smaller, simpler, lack membrane-bound organelles, have a single circular chromosome, and reproduce asexually through binary fission.
- Eukaryotic Cells: Generally larger, more complex, have membrane-bound organelles like mitochondria, endoplasmic reticulum, Golgi apparatus, etc., have multiple linear chromosomes, and reproduce sexually or asexually.
For example, a bacterium (prokaryotic) has a single circular chromosome in its cytoplasm, whereas a human cell (eukaryotic) has multiple linear chromosomes neatly packaged within its nucleus.
Q 24. Describe the structure and function of different organelles in eukaryotic cells.
Eukaryotic cells are highly organized, with various organelles working in coordination. Here are a few key examples:
- Nucleus: The control center of the cell, containing the genetic material (DNA).
- Mitochondria: The powerhouses of the cell, responsible for cellular respiration and ATP production.
- Endoplasmic Reticulum (ER): A network of membranes involved in protein synthesis (rough ER) and lipid metabolism (smooth ER).
- Golgi Apparatus: Processes and packages proteins and lipids for secretion or transport within the cell.
- Ribosomes: Sites of protein synthesis, found free in the cytoplasm or attached to the rough ER.
- Lysosomes: Contain enzymes that break down waste materials and cellular debris.
- Peroxisomes: Involved in lipid metabolism and detoxification.
Imagine a factory: the nucleus is the management office, mitochondria are the power generators, the ER is the assembly line, the Golgi apparatus is the packaging department, and lysosomes are the waste disposal system.
Q 25. Explain the principles of PCR and its applications in microbiology.
Polymerase Chain Reaction (PCR) is a revolutionary technique that allows for the amplification of specific DNA sequences. It’s based on the principles of DNA replication, using a heat-stable DNA polymerase enzyme to repeatedly copy a target DNA fragment.
- Principles: PCR involves cycles of heating and cooling, each cycle consisting of three main steps:
- Denaturation: The DNA template is heated to separate the double strands.
- Annealing: Short DNA sequences called primers bind to the target DNA sequence.
- Extension: The DNA polymerase enzyme synthesizes new DNA strands complementary to the template strands.
- Applications in Microbiology: PCR has numerous applications in microbiology, including:
- Detection of pathogens: Identifying specific bacteria, viruses, or parasites in clinical samples.
- Genetic fingerprinting: Analyzing microbial genomes for identification and typing purposes.
- Gene cloning: Amplifying specific genes for further study or manipulation.
- Quantitative PCR (qPCR): Measuring the amount of a specific DNA sequence, useful in studying gene expression.
For example, in a clinical setting, PCR can quickly detect the presence of a specific viral DNA in a patient’s blood sample, enabling timely diagnosis and treatment.
Q 26. What are the different types of microscopy techniques used in cell biology and microbiology?
Various microscopy techniques are used to visualize cells and microbes, each with its own advantages and limitations. Here are some examples:
- Light Microscopy: Uses visible light to illuminate the sample. Different types include bright-field, dark-field, phase-contrast, and fluorescence microscopy.
- Electron Microscopy: Uses a beam of electrons instead of light, providing much higher resolution. Transmission electron microscopy (TEM) allows for visualization of internal structures, while scanning electron microscopy (SEM) provides high-resolution images of the surface.
- Confocal Microscopy: Uses lasers and a pinhole to eliminate out-of-focus light, creating sharp images of thick samples.
- Atomic Force Microscopy (AFM): Scans the surface of a sample with a sharp tip to create a three-dimensional image at a very high resolution. It’s particularly useful for visualizing surface details of cells and molecules.
Choosing the right technique depends on the type of sample, the desired resolution, and the specific features to be visualized. For instance, to visualize the internal structure of a bacterium, TEM would be a suitable choice, while to examine the surface of a cell, SEM would be preferred.
Q 27. Describe your experience with flow cytometry.
I have extensive experience with flow cytometry, a powerful technique used to analyze and sort cells based on their physical and chemical characteristics. In my previous role, I routinely used flow cytometry to analyze immune cell populations. I was responsible for sample preparation, instrument operation, data acquisition, and analysis. For example, I used flow cytometry to identify and quantify different types of immune cells (e.g., T cells, B cells, NK cells) in blood samples and tissue homogenates. This involved staining cells with fluorescent antibodies specific for cell surface markers, running the samples on the flow cytometer, and then analyzing the data using specialized software to identify and quantify the various cell populations. I have also used this technique to study cell apoptosis and cell cycle analysis.
Specifically, I am proficient in using various flow cytometry software packages for data analysis, including the compensation and gating of various cell subsets. I also have experience in troubleshooting common flow cytometry issues and maintaining the instrument.
Q 28. Explain your experience working with biosafety cabinets.
Biosafety cabinets (BSCs) are critical for working with biological agents that pose a risk to the researcher and the environment. Throughout my career, I’ve consistently adhered to strict safety protocols while working with BSCs, particularly Class II BSCs which provide personnel, product, and environmental protection. My experience includes operating, maintaining, and troubleshooting different models of BSCs.
Before commencing any work, I always ensure proper decontamination of the BSC using a 70% ethanol solution. I understand the importance of proper airflow and HEPA filtration to maintain a sterile environment. I have experience in performing various microbiological procedures inside the BSC, such as cell culture work, inoculation of plates, and handling infectious agents. I am also trained in the proper techniques to minimize the risk of aerosol generation and contamination. Regular maintenance, including filter integrity checks, are crucial; I’m familiar with standard operating procedures for both routine and preventative maintenance.
Furthermore, I am well-versed in the proper procedures for dealing with spills and other accidents inside the BSC. Safety is always my top priority when handling any biological material.
Key Topics to Learn for Cell Culture and Microbiology Interview
- Aseptic Techniques: Understanding and applying sterile techniques to prevent contamination in cell culture and microbiological experiments. This includes proper handling of equipment, media preparation, and environmental control.
- Cell Culture Fundamentals: Mastering cell culture techniques such as cell seeding, passaging, cryopreservation, and maintaining cell lines. This also encompasses understanding cell growth kinetics and media optimization.
- Microbial Growth and Metabolism: Understanding bacterial growth curves, metabolic pathways, and the factors influencing microbial growth (e.g., temperature, pH, oxygen). Practical application includes interpreting growth data and designing experiments to control microbial growth.
- Sterilization Methods: Knowledge of various sterilization methods (autoclaving, filtration, UV irradiation) and their appropriate applications in cell culture and microbiology labs. This includes understanding the principles behind each method and their limitations.
- Microscopy and Staining Techniques: Proficiency in using microscopes to visualize cells and microorganisms. Understanding different staining techniques (Gram staining, fluorescence microscopy) and their applications in identification and analysis.
- Troubleshooting Common Issues: Developing problem-solving skills to address common challenges in cell culture and microbiology, such as contamination, cell death, and unexpected experimental results. This includes understanding root causes and implementing corrective actions.
- Molecular Techniques (Optional, depending on the role): Depending on the specific job, familiarity with techniques like PCR, ELISA, or flow cytometry might be beneficial. Understanding the principles and applications of these techniques would be a significant advantage.
- Good Laboratory Practices (GLP): Understanding and adhering to GLP principles for maintaining accuracy, reproducibility, and safety in the laboratory. This includes proper record-keeping and data management.
Next Steps
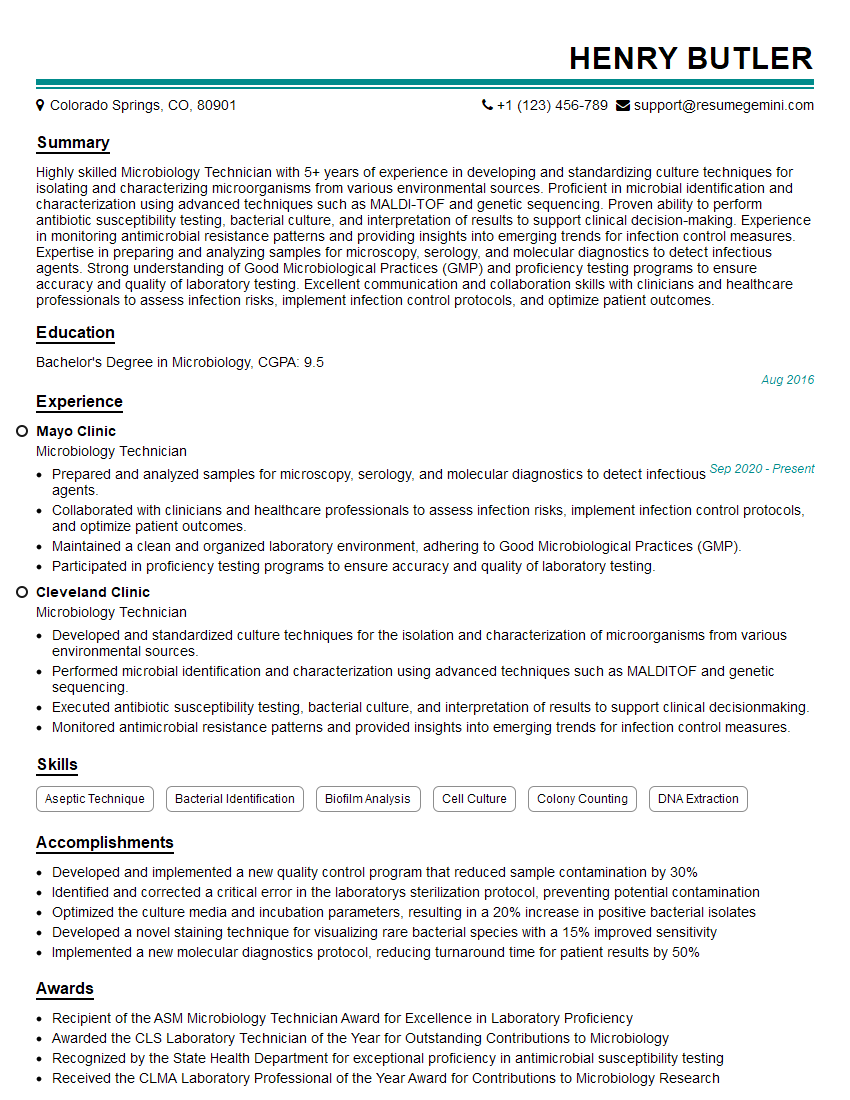
Mastering Cell Culture and Microbiology is crucial for a successful career in many exciting fields, from pharmaceutical research and development to biotechnology and diagnostics. A strong foundation in these areas opens doors to diverse and rewarding opportunities. To significantly increase your chances of landing your dream role, it’s vital to create a resume that effectively showcases your skills and experience to Applicant Tracking Systems (ATS). ResumeGemini is a trusted resource that can help you build a professional and ATS-friendly resume. We provide examples of resumes tailored to Cell Culture and Microbiology roles to guide you in creating a compelling application that highlights your expertise. Invest in your future – craft a resume that stands out.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good