The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Escharotomy interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Escharotomy Interview
Q 1. Describe the indications for performing an escharotomy.
Escharotomy is a surgical procedure performed to relieve circumferential full-thickness burns that constrict underlying tissues. The primary indication is the presence of circumferential burns, particularly on the extremities or torso, causing compartment syndrome. This means the burn eschar (the dead, leathery tissue) acts like a tourniquet, reducing blood flow and potentially leading to irreversible tissue damage.
Specifically, escharotomy is indicated when there’s evidence of compromised circulation distal to the burn, such as: decreased or absent pulses, pain disproportionate to the burn, pallor or cyanosis of the skin distal to the burn, swelling, paresthesia (numbness or tingling), and paralysis.
For example, a patient with a circumferential burn on their leg might experience intense pain, swelling, and loss of feeling in their toes. This is a clear sign that the constricting eschar is compromising circulation and necessitates an escharotomy.
Q 2. Explain the contraindications of escharotomy.
While escharotomy is life-saving in many instances, there are some contraindications. These are primarily situations where the procedure’s risks outweigh the potential benefits. The most significant contraindication is the absence of signs of compromised circulation. Performing an escharotomy without clear evidence of compartment syndrome is unnecessary and increases the risk of bleeding and infection.
Other relative contraindications include unstable patient hemodynamics (low blood pressure, rapid heart rate) where the added stress of the procedure could be detrimental, the presence of a significant coagulopathy (bleeding disorder) making bleeding difficult to control, and lack of appropriate surgical resources and personnel.
Imagine a patient with a circumferential burn but good distal pulses and no significant pain. An escharotomy wouldn’t be necessary in this scenario, as the eschar is not yet causing circulatory compromise.
Q 3. What are the different types of escharotomy incisions?
Escharotomy incisions are typically longitudinal, following the long axis of the limb or body part involved. This approach minimizes damage to blood vessels and nerves. They are designed to relieve the circumferential constriction.
While longitudinal incisions are the most common, other approaches might be used based on the specific location and severity of the burn. Occasionally, transverse incisions may be used in conjunction with longitudinal incisions, particularly on the chest or abdomen, for optimal decompression. The goal is always to make the shortest incisions necessary to release the constricting forces.
- Longitudinal incisions: These run parallel to the long axis of the limb or body part.
- Transverse incisions: These are less common and run perpendicular to the long axis.
Choosing the appropriate incision pattern involves careful clinical judgment and consideration of the underlying anatomy.
Q 4. How do you choose the appropriate incision depth for an escharotomy?
Incision depth for an escharotomy is crucial. The goal is to completely divide the eschar, relieving the constriction, but not to penetrate into viable tissue. Penetration into viable tissue increases the risk of bleeding and infection, and delays healing. The incision should go through the full thickness of the eschar, down to the underlying subcutaneous fat. One can usually easily visualize the fat layer once the eschar is completely divided.
The depth is judged visually and by tactile feedback. You’ll feel the resistance of the eschar give way as you incise through to the underlying fat. Using sharp instruments, such as a #10 or #15 blade, facilitates precise incision and reduces trauma to surrounding tissue. Careful attention to avoid deep penetration, especially near nerves and vessels, is vital.
Think of it like cutting through a tough piece of leather – you need to cut through the leather but stop before damaging the material underneath.
Q 5. What are the potential complications of escharotomy?
Escharotomy, despite being a life-saving procedure, carries potential complications. The most significant is bleeding. The incisions are deep, and significant blood vessels may be damaged. Infection is another serious risk because the eschar is a breeding ground for bacteria, and the incision creates an entry point for infection. Although rare, damage to underlying nerves and vessels can occur.
- Bleeding: This can range from minor oozing to significant hemorrhage.
- Infection: Wound infections can be serious and lead to sepsis (body-wide infection).
- Nerve injury: Injury to nerves can result in impaired sensation or motor function.
- Delayed wound healing: The wounds may be slow to heal due to the presence of underlying burn injury and potential infection.
Minimizing these complications requires careful surgical technique, meticulous hemostasis (control of bleeding), and appropriate post-operative care.
Q 6. How do you manage bleeding during an escharotomy?
Managing bleeding during an escharotomy is critical. Direct pressure is often sufficient for controlling minor bleeding. However, for more significant bleeding, surgical techniques may be necessary. This might involve electrocautery (using heat to seal blood vessels), or the use of ligatures (surgical ties) to stop bleeding from larger vessels.
Before the procedure, assessing the patient’s coagulation profile is important to anticipate potential bleeding problems. If there is an underlying coagulopathy, the risk of bleeding is significantly increased and needs to be addressed with the proper treatments or consultations before the escharotomy.
Having readily available hemostatic agents, such as surgical sponges and clotting factors, is essential. A thorough knowledge of anatomical landmarks allows the surgeon to avoid major blood vessels whenever possible.
Q 7. What are the post-operative care considerations following an escharotomy?
Post-operative care following an escharotomy is crucial for preventing complications and promoting healing. This involves close monitoring of the patient’s vital signs, wound assessment for signs of bleeding and infection, and pain management. The wounds need to be dressed regularly to prevent infection, with appropriate topical antimicrobial agents and dressings.
Debridement (removal of dead tissue) may be necessary in the later stages. Intravenous fluids and nutritional support are often required to maintain hydration and support healing. Close monitoring for signs of compartment syndrome recurrence is vital. Early mobilization and physiotherapy may be helpful in preventing contractures (scar tissue tightening) in the later stages.
Regular wound care, pain management, and nutritional support are essential to optimize patient recovery and minimize scarring. The patient will need frequent follow-up appointments for wound care and assessment.
Q 8. How do you assess the effectiveness of an escharotomy?
Assessing the effectiveness of an escharotomy centers around evaluating its impact on tissue perfusion and relieving circumferential constrictions caused by eschar (the leathery, dead tissue formed by a deep burn).
- Improved perfusion: Post-escharotomy, we observe for improved capillary refill, skin color (moving from dusky or cyanotic to pink), and palpable pulses distal to the incision. A return to normal or near-normal perfusion indicates success.
- Decreased compartment pressure: In cases of circumferential burns on extremities, compartment pressures should be monitored before and after the procedure. A significant drop in compartment pressure, ideally below 30 mmHg, demonstrates effective pressure relief.
- Improved motor and sensory function: We assess for improved movement and sensation in the affected area. Restoration of function reflects successful decompression.
- Absence of further complications: We monitor for signs of infection, excessive bleeding, or other complications. The absence of these signifies successful escharotomy.
For example, a patient with a circumferential burn on their leg might present with absent pulses and a pale, cool extremity. After escharotomy, the pulses should return, and the skin should become warm and pink. If these changes are observed, the procedure is deemed effective.
Q 9. Describe the anatomy relevant to performing an escharotomy on the extremities.
Escharotomy on the extremities requires a thorough understanding of the vascular and fascial compartments. The incisions are strategically placed to avoid major nerves and vessels.
- Superficial fascia: The superficial fascia is often incised along with the eschar. This layer is relatively avascular, minimizing bleeding.
- Deep fascia: The deep fascia is a more critical anatomical structure, housing major nerves and blood vessels. It’s essential to avoid excessive dissection to prevent injury.
- Compartments: Extremities, such as the forearm or leg, are divided into compartments containing specific muscle groups and neurovascular bundles. Escharotomies are designed to release pressure within these compartments, preventing compartment syndrome.
- Neurovascular bundles: Precise incision placement is crucial to prevent injury to nerves and arteries within the compartments. Anatomical knowledge guides incision positioning to minimize this risk.
Imagine the leg like a garden hose with a tight band around it – the escharotomy acts like cutting the band to restore blood flow. Knowing the precise location of the ‘hose’ (neurovascular bundle) is critical for success.
Q 10. Describe the anatomy relevant to performing an escharotomy on the torso.
Escharotomy on the torso requires understanding the layers of the chest wall and abdomen, including muscles, ribs, and underlying organs. Unlike the extremities, compartmentalization is less defined but the principles of releasing circumferential pressure remain.
- Chest wall: Incisions are carefully planned to avoid damaging ribs and intercostal muscles. These incisions often follow the intercostal spaces to minimize damage.
- Abdominal wall: Abdominal escharotomies may involve incisions in a longitudinal or transverse fashion, depending on the location and extent of the burn. Care must be taken to avoid damaging abdominal organs.
- Fascia: The underlying fascia of the chest and abdomen is incised to relieve the constricting force of the eschar.
- Vascular supply: Although less compartmentalized than extremities, maintaining blood supply to the underlying tissues is a crucial consideration.
Think of the torso as a tightly wrapped package. The escharotomy strategically ‘unwraps’ the package, releasing pressure and allowing for better breathing or blood flow, but always taking care not to damage the contents (organs).
Q 11. Explain the difference between a fasciotomy and an escharotomy.
While both fasciotomy and escharotomy are surgical procedures to release pressure from a confined space, they differ significantly in their targets and indications.
- Escharotomy: Incision through eschar (dead, leathery burn tissue) to relieve circumferential constriction caused by burn injury. It’s performed in the presence of full-thickness burns that restrict blood flow.
- Fasciotomy: Incision through the fascia (the tough connective tissue surrounding muscle groups) to relieve compartment syndrome. This condition occurs when pressure within a compartment builds up to dangerous levels, compromising blood supply to tissues. It may be done regardless of burn depth in cases of significant pressure increase.
In essence, escharotomy addresses pressure from dead tissue, while fasciotomy addresses pressure from swelling within living tissue. A patient could need both, for instance, if they have a circumferential burn causing eschar constriction and subsequent compartment syndrome.
Q 12. How do you differentiate between superficial and deep partial-thickness burns?
Differentiating between superficial and deep partial-thickness burns relies primarily on clinical assessment, including depth of injury, pain response, and appearance.
- Superficial partial-thickness (1st degree): Involves only the epidermis (outer skin layer). Characterized by redness, mild swelling, and pain. Blanches (turns white) with pressure and recovers quickly.
- Deep partial-thickness (2nd degree): Extends deeper into the dermis (underlying skin layer). Presents with blisters, significant edema, and intense pain. Blanches with pressure but recovery takes longer, sometimes involving scarring.
Imagine a sunburn: a mild sunburn is superficial partial thickness – red, painful but heals quickly. A severe sunburn with large blisters is deep partial thickness – painful, blisters, and healing may result in some scarring. This is mainly assessed by clinical examination; biopsy isn’t routinely needed.
Q 13. How do you assess for compartment syndrome following an escharotomy?
Assessing for compartment syndrome after escharotomy involves meticulous monitoring of the affected limb.
- Pain: Disproportionate pain that’s not relieved by analgesia is a key indicator.
- Pallor: The skin appears pale or dusky, indicating poor blood supply.
- Paresthesia: Numbness or tingling sensation distal to the site.
- Pulselessness: Absence or diminished pulses in the affected extremity.
- Paralysis: Impaired or absent movement of the affected extremity.
- Pressure measurement: Direct compartment pressure measurement using a Stryker pressure monitor provides objective data. Pressure above 30 mmHg is concerning.
The mnemonic ‘5 Ps’ (Pain, Pallor, Paresthesia, Pulselessness, Paralysis) helps remember the critical signs. If these signs appear, it means the escharotomy might not have completely decompressed the area, or a fasciotomy might be needed.
Q 14. What is the role of fluid resuscitation in patients requiring escharotomy?
Fluid resuscitation is paramount before, during, and after escharotomy in burn patients. Massive fluid shifts occur in burn injuries, leading to hypovolemic shock. The goal is to maintain adequate tissue perfusion and prevent organ dysfunction.
- Pre-operative resuscitation: Aggressive fluid resuscitation begins immediately after the burn injury to stabilize the patient’s circulatory system. This is typically calculated using Parkland formula.
- Intra-operative resuscitation: Fluid administration continues throughout the escharotomy procedure to maintain blood pressure and prevent hypotension.
- Post-operative resuscitation: Fluid management continues post-escharotomy to address ongoing fluid losses and support tissue healing. Monitoring urine output and hemodynamic parameters is crucial.
Think of it like this: the body is losing fluids like a leaking bucket. Fluid resuscitation is like constantly refilling the bucket to prevent the bucket (the body) from drying out, especially during the ‘repair’ process (the escharotomy).
Q 15. Discuss the importance of meticulous wound care post-escharotomy.
Meticulous wound care after escharotomy is paramount to prevent infection and promote healing. Escharotomy creates a large, deep wound that’s highly susceptible to bacterial colonization. Our post-operative care focuses on several key areas:
- Debridement: Regular removal of necrotic tissue (dead tissue) is crucial. This can be done surgically, or using enzymatic debridement methods. This prevents a breeding ground for infection and allows healthy tissue to regenerate.
- Wound cleansing: Gentle cleansing with sterile saline is essential. We avoid harsh antiseptic solutions that can damage the new tissue. The goal is to remove debris without causing further trauma.
- Dressing selection: The type of dressing depends on the wound characteristics. We often use moist dressings to encourage healing and prevent desiccation. Negative pressure wound therapy (NPWT) may be employed for larger, complex wounds to improve healing and manage exudate.
- Monitoring for infection: Close monitoring for signs of infection, including redness, swelling, pain, purulent drainage, and fever, is absolutely vital. Frequent wound assessments and lab tests (e.g., blood cultures) are part of our routine.
- Pain management: Post-escharotomy pain can be significant. We utilize a multimodal analgesic approach including analgesics, local anesthetic infiltration, and nerve blocks as needed.
For example, I recently managed a patient with a circumferential escharotomy on their leg. We used NPWT combined with topical antibiotics and regular wound debridement. The patient healed well, demonstrating the effectiveness of our multi-pronged approach.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the signs and symptoms of infection following escharotomy?
Recognizing infection after escharotomy is crucial for timely intervention. Signs and symptoms can range from subtle to severe and include:
- Increased pain and tenderness: Pain significantly exceeding the expected post-operative discomfort.
- Erythema (redness): Spreading redness around the incision site.
- Edema (swelling): Increased swelling beyond the immediate post-operative edema.
- Purulent drainage: Thick, yellow or green discharge from the wound.
- Fever and chills: Systemic signs of infection.
- Local warmth: The skin around the wound feels noticeably warmer than the surrounding area.
- Halitosis (foul odor): A bad smell emanating from the wound.
It’s important to note that some of these signs may be masked by the existing burn injury, making early and frequent clinical assessment essential. For instance, a subtle increase in purulent drainage might be easily missed if not carefully examined.
Q 17. How would you manage a post-escharotomy infection?
Management of a post-escharotomy infection requires a prompt and aggressive approach. Our strategy involves:
- Wound culture and sensitivity testing: Identifying the specific pathogen allows us to prescribe targeted antibiotics.
- Intravenous antibiotics: Broad-spectrum antibiotics are initially administered intravenously, followed by targeted antibiotics based on the culture results.
- Surgical debridement: Further surgical removal of infected and necrotic tissue may be necessary to control the infection.
- Wound irrigation: Regular irrigation of the wound with antiseptic solutions helps to remove bacteria and debris.
- Appropriate dressings: Dressings are chosen to manage exudate and support wound healing, potentially including NPWT.
- Monitoring vital signs: Close monitoring of temperature, heart rate, and blood pressure is essential.
- Supportive care: Fluid management, nutritional support, and pain control are crucial.
For example, a patient presenting with fever, increasing purulent drainage, and local erythema would necessitate immediate intravenous antibiotics, wound cultures, and potential surgical debridement.
Q 18. Describe your experience with different types of surgical instruments used in escharotomy.
Escharotomy requires sharp dissection through the eschar (the thick, leathery layer of dead tissue). The choice of instrument depends on the location and thickness of the eschar. Commonly used instruments include:
- No. 11 blade scalpel: Provides precision for superficial escharotomy.
- No. 15 blade scalpel: Suitable for thicker eschar, allowing deeper penetration.
- Surgical scissors: Used for blunt dissection and separating tissues.
- Electrocautery: Provides hemostasis (stops bleeding) and can be used for deeper escharotomy.
- Metzenbaum scissors: Excellent for dissecting delicate tissues adjacent to the eschar.
My experience shows that the selection of instruments depends largely on the clinical scenario. In thicker eschars, the No. 15 blade offers better penetration, whilst in more superficial cases, the No. 11 blade is more precise and minimizes tissue damage. The use of electrocautery is crucial in managing bleeding during the procedure, particularly in areas with rich vascular supply.
Q 19. What are the benefits of using a Z-plasty technique in escharotomy?
The Z-plasty technique in escharotomy is primarily used to improve wound closure and reduce tension across the scar. This is particularly useful in areas with significant contracture or limited skin mobility, such as circumferential burns. The benefits include:
- Improved scar pliability: The Z-plasty breaks up the linear scar, making it less prone to contracture and improving range of motion.
- Reduced tension on the wound: By altering the orientation of the incision, tension on the wound edges is redistributed, leading to improved healing.
- Better cosmetic outcome: The Z-plasty results in a more aesthetically pleasing scar.
It’s important to consider the depth and location of the burn injury when planning to incorporate this technique. It’s not always appropriate and requires careful surgical planning.
Q 20. Explain your approach to managing a patient who develops a fasciotomy complication after escharotomy.
A fasciotomy complication following escharotomy is a serious event, indicating compromised muscle perfusion and potentially limb-threatening ischemia. Management involves immediate action:
- Urgent surgical exploration: This is crucial to assess the extent of muscle damage and confirm the diagnosis.
- Extensive fasciotomy: This involves further incision of the fascia to relieve compartment pressure.
- Wound debridement: Removal of any necrotic muscle tissue is essential.
- Intravenous antibiotics: To prevent infection, broad-spectrum antibiotics are administered immediately.
- Monitoring vital signs: Close observation for signs of sepsis or multi-organ dysfunction is necessary.
- Supportive care: Fluid resuscitation, nutritional support, and pain management are essential.
- Referral to a plastic surgeon: For potential skin grafting or flap coverage once the infection is controlled.
In one case, a patient developed compartment syndrome in their forearm after an escharotomy. Immediate fasciotomy was performed, followed by aggressive wound care. Thankfully, early intervention prevented limb loss.
Q 21. How would you explain the procedure and potential risks to a patient prior to escharotomy?
Explaining escharotomy to a patient requires empathy and clear communication. My approach involves:
- Detailed explanation of the procedure: Using simple terms, I explain why the procedure is necessary to improve blood flow to compromised tissues. I describe what the procedure involves, emphasizing the need to relieve pressure and prevent limb loss. Analogies may be useful to illustrate the concept (e.g., comparing the eschar to a tight band restricting blood flow).
- Discussion of potential risks: These include infection, bleeding, nerve damage, scarring, and the possibility of further procedures (e.g., fasciotomy). I explain the rarity of serious complications and stress the urgency of the procedure.
- Addressing patient concerns: Creating a safe space for questions and concerns is crucial. I encourage them to write down questions before our discussion. I also ensure family members are included in the explanation, especially for patients who are heavily sedated.
- Reassurance and support: I reaffirm my commitment to their care and recovery, providing a sense of hope and positivity.
I always ensure that informed consent is obtained before proceeding with the procedure, documenting the discussion thoroughly.
Q 22. How do you document your work during and after an escharotomy?
Meticulous documentation is paramount in escharotomy. It begins pre-procedure with a clear indication for the procedure, including the location, depth, and extent of the burn. We record vital signs, pain scores (using a validated scale like the Numeric Rating Scale or Visual Analog Scale), and the patient’s overall condition. During the procedure, the surgical team documents the exact location and extent of the incisions, the depth of the eschar, any complications encountered (e.g., bleeding), and the type of instruments used. Post-procedure, we document the type and amount of fluid used for irrigation, the type of dressing applied, and any pain medication administered. Photographs are crucial for visual documentation of the burn, incisions, and healing progress. We note the patient’s response to the procedure, including changes in vital signs and pain levels. Finally, we document any plans for ongoing wound care, follow-up appointments, and further surgical interventions. This comprehensive record serves as a critical component for continuity of care, legal protection, and future research.
Q 23. What are the different types of dressings used following escharotomy and their purposes?
The choice of dressing after escharotomy depends on several factors, including the depth and location of the burn, the presence of infection, and the patient’s overall condition. Common dressings include:
- Hydrocolloids: These dressings provide a moist wound healing environment, protecting the wound from external contamination and promoting autolytic debridement. They are often suitable for superficial partial-thickness burns.
- Alginates: Highly absorbent dressings derived from seaweed, alginates are excellent for managing wounds with significant exudate (fluid). They are commonly used in deeper burns and are effective at absorbing drainage.
- Foam dressings: These dressings provide cushioning and protection, managing exudate while maintaining a moist wound environment. They can be used for various wound depths and are particularly useful in areas subject to friction or movement.
- Silver-containing dressings: These possess antimicrobial properties and can help prevent or manage wound infections. They are frequently used in burns at high risk of infection.
- Biological dressings (e.g., skin grafts): In many cases, escharotomy is a prelude to skin grafting. Autografts (from the patient) or allografts (from a donor) are often used for deeper burns to promote healing and closure.
The specific dressing choice is always individualized and based on the wound’s specific needs and the surgeon’s experience.
Q 24. Explain the role of debridement in the context of escharotomy.
Debridement plays a crucial role in the management of burns after escharotomy. Eschar, the thick, leathery necrotic tissue resulting from a burn, impedes healing and can create a breeding ground for infection. Debridement is the process of removing this necrotic tissue, allowing for healthy granulation tissue to form and facilitating wound healing. Different debridement techniques are employed: surgical debridement (sharp excision), enzymatic debridement (using topical enzymes), autolytic debridement (allowing the body’s natural processes to remove the eschar), and mechanical debridement (using wet-to-dry dressings or specialized tools). The type of debridement is chosen based on the extent and location of the burn and the patient’s overall health status. Adequate debridement is essential for preventing infection and promoting healing after escharotomy.
Q 25. Describe your experience in managing patients with circumferential burns.
Circumferential burns, which encircle a limb or body segment, pose a significant challenge due to the risk of compartment syndrome. This occurs when swelling within the confined space of the affected area compromises blood supply to the tissues. Early recognition and treatment are critical. My approach involves continuous monitoring of pulses distal to the burn, capillary refill, and sensation. Regular assessment of compartment pressures using a Stryker pressure monitor is crucial. If compartment syndrome is suspected, urgent escharotomy is performed. This procedure involves making incisions through the constricting eschar to relieve pressure and restore blood flow. The incisions are strategically placed to avoid major nerves and blood vessels. Post-escharotomy, close monitoring for infection and adequate pain management are vital. In severe cases, fasciotomy (surgical release of the fascia) may be required. Successful management requires a multidisciplinary team approach, involving surgeons, nurses, and intensivists.
Q 26. How do you monitor the effectiveness of pain management post-escharotomy?
Post-escharotomy pain management is a critical aspect of patient care. We use a multimodal approach, combining different modalities to optimize pain control. We regularly assess pain using validated scales and consider the patient’s subjective report. Pharmacological interventions, including analgesics (opioids and non-opioids), nerve blocks, and potentially epidurals are commonly employed. Non-pharmacological strategies, such as positioning, splinting to minimize movement, and wound care techniques designed to minimize pain, are also implemented. Regular reassessment of pain levels ensures effectiveness and allows adjustments to the pain management plan as needed. The goal is to provide comfort and promote mobility. In some cases, pain management specialist consultation may be beneficial.
Q 27. Describe a challenging escharotomy case you have managed and how you approached it.
One particularly challenging case involved a young adult with a full-thickness circumferential burn to the left upper extremity following a house fire. The eschar was extremely tight, restricting blood flow and causing significant swelling. Initial attempts to assess compartment pressures were unsuccessful due to the depth and thickness of the eschar. We decided on immediate escharotomy under general anesthesia. The procedure required careful dissection to avoid damaging underlying vessels and nerves. Post-operatively, despite meticulous wound care and aggressive pain management, the patient developed a significant wound infection. We initiated IV antibiotics and performed frequent wound debridements under local anesthesia. Ultimately, the patient required a skin graft. The case highlighted the importance of early intervention in circumferential burns, meticulous surgical technique, and diligent post-operative monitoring. It also reinforced the unpredictable nature of severe burns and the necessity of an adaptable treatment plan.
Key Topics to Learn for Escharotomy Interview
- Anatomy and Physiology of Burn Wounds: Understanding the depth, classification, and physiological consequences of burns is fundamental. Focus on how these factors influence escharotomy decisions.
- Indications and Contraindications for Escharotomy: Master the criteria for performing an escharotomy, including compartment syndrome assessment and the recognition of situations where it’s not appropriate.
- Escharotomy Techniques: Familiarize yourself with different incision techniques, including the location, depth, and direction of incisions. Consider the impact of different surgical approaches on patient outcomes.
- Compartment Syndrome: Develop a deep understanding of compartment syndrome, its pathophysiology, and its relationship to escharotomy. Practice diagnosing and managing this critical complication.
- Post-Escharotomy Management: Know the post-operative care, including wound management, pain control, and monitoring for complications. Understanding potential risks and preventative measures is crucial.
- Surgical Instruments and Equipment: Be prepared to discuss the tools and equipment used during escharotomy. This demonstrates practical surgical knowledge.
- Case Studies and Problem Solving: Prepare to analyze hypothetical scenarios and discuss decision-making processes related to escharotomy. This shows your critical thinking abilities.
Next Steps
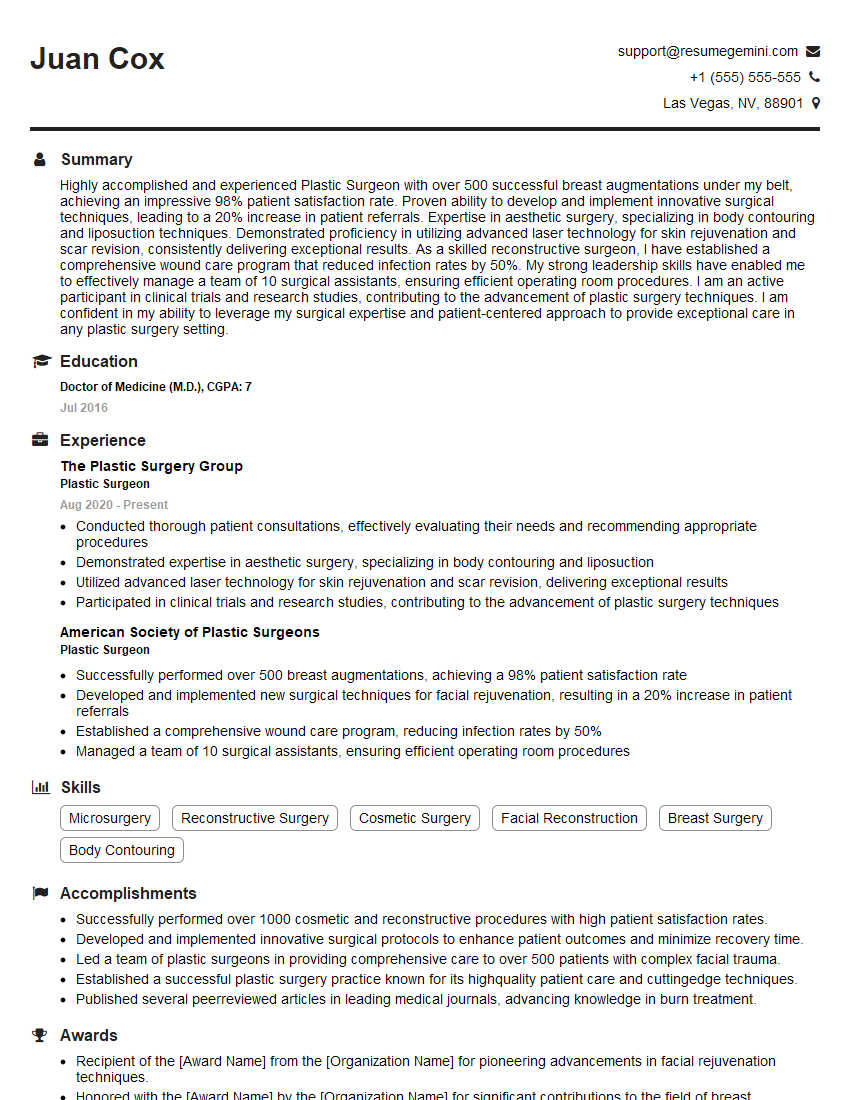
Mastering Escharotomy significantly enhances your career prospects in surgical specialties and demonstrates a high level of surgical skill and judgment. A strong grasp of this procedure is highly valued by employers. To maximize your chances of securing your dream role, it’s crucial to create an ATS-friendly resume that highlights your expertise. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, tailored to showcase your skills and experience in Escharotomy. Examples of resumes specifically designed for Escharotomy professionals are available within ResumeGemini to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good