Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Hemovac Placement interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Hemovac Placement Interview
Q 1. Describe the procedure for Hemovac placement.
Hemovac placement is a surgical procedure involving the insertion of a closed-suction drainage system to remove fluid, blood, or air from a surgical site or body cavity. It’s a relatively straightforward procedure but requires meticulous attention to sterile technique to prevent infection. Think of it like a mini-vacuum cleaner for your body, helping the healing process.
The procedure generally involves:
- Surgical incision: A small incision is made near the surgical site or drain location.
- Drain placement: The Hemovac drain, which is a flexible tube with a reservoir, is carefully inserted into the desired location guided by the surgeon.
- Securement: The drain is sutured in place to prevent dislodgement. A dressing is then applied to cover the incision site.
- Activation: The Hemovac reservoir is compressed to create a vacuum, initiating the drainage process. The amount of suction is pre-set and should not be altered without a physician’s order.
- Post-operative monitoring: Regular monitoring of the drainage amount, color, and consistency is essential.
The exact steps may vary depending on the specific surgical site and the surgeon’s preferences, but the core principles remain the same.
Q 2. What are the indications for Hemovac drainage?
Hemovac drainage is indicated in various surgical situations where the removal of fluid or blood is necessary for optimal healing. Some common indications include:
- Post-surgical drainage: Following procedures like mastectomies, abdominal surgeries, orthopedic surgeries, and trauma surgery where significant fluid or blood collection is expected.
- Prevention of hematoma or seroma formation: Preventing the buildup of blood (hematoma) or serum (seroma) that can impede healing and potentially lead to infection.
- Management of infected wounds: Though not the primary treatment, Hemovacs can assist in removing pus and other infectious material from wounds.
- Pleural effusion: Removal of excess fluid from the pleural space (the area between the lungs and the chest wall).
In essence, Hemovac drainage aids in maintaining a clean surgical site, promoting faster healing, and reducing the risk of complications.
Q 3. What are the contraindications for Hemovac placement?
While Hemovac placement is generally safe, there are certain contraindications which means it shouldn’t be used. These include:
- Active bleeding: A Hemovac should not be placed in an area with uncontrolled bleeding, as it can exacerbate the bleeding.
- Presence of an arteriovenous fistula: This vascular abnormality can lead to complications if a drain is placed nearby.
- Patient allergy to the drain material: Rare, but an allergic reaction to the drain material (usually silicone) could occur.
- Conditions that contraindicate surgery in general: For example, a severely compromised coagulation profile would make surgical drainage too risky.
Careful assessment of the patient’s condition is crucial before placing a Hemovac to avoid potential complications.
Q 4. Explain the different types of Hemovac drains available.
Hemovac drains primarily differ in their capacity (how much fluid they can hold). They are essentially all made of flexible silicone tubing with a collection reservoir. The main difference lies in the reservoir size, commonly ranging from 200mL to 1000mL. Larger volume drains are chosen for surgeries generating greater amounts of fluid. Although not always explicitly different “types”, the selection is driven by patient specific needs rather than distinct drain “types”.
Q 5. How do you select the appropriate size of Hemovac drain?
Selecting the appropriate Hemovac size is crucial for effective drainage. Too small a drain can lead to overflow and potential complications; too large a drain can be uncomfortable for the patient. The selection is largely determined by the anticipated amount of drainage based on the type of surgery and the patient’s individual characteristics. For example, a mastectomy might necessitate a smaller drain compared to a large abdominal surgery. The surgeon’s judgement and surgical plan plays a key role in the selection of the drain.
Q 6. Describe the steps for preparing the patient for Hemovac placement.
Preparing the patient for Hemovac placement involves several crucial steps to ensure patient safety and a successful procedure. This includes:
- Informed consent: The patient needs to understand the procedure, its benefits, risks, and alternatives.
- Preoperative assessment: The patient’s medical history, coagulation profile, and allergy status should be carefully evaluated.
- Skin preparation: The surgical site needs to be thoroughly cleaned and disinfected to minimize the risk of infection. This is critical for preventing contamination of the area where the Hemovac will be placed.
- Positioning: The patient is positioned appropriately for the surgery, often with the surgical site exposed for ease of access.
- Monitoring: Vital signs, such as blood pressure, heart rate, and oxygen saturation, are continuously monitored throughout the procedure.
Proper preparation significantly contributes to a smooth and complication-free Hemovac placement.
Q 7. What are the potential complications of Hemovac placement?
While generally safe, Hemovac placement carries potential complications. It’s essential to be aware of these to provide appropriate monitoring and intervention.
- Infection: This is a significant concern, and strict sterile technique is vital to prevent it. Signs include redness, swelling, increased pain, and purulent drainage.
- Bleeding: Though less common after the initial surgical hemostasis, excessive bleeding can occur, requiring intervention.
- Drain blockage: Blood clots or tissue can block the drain, necessitating repositioning or replacement.
- Dislodgement: The drain can become dislodged, requiring surgical reattachment or replacement.
- Skin irritation or erosion: Prolonged contact between the drain and the skin can cause irritation or erosion at the insertion site.
- Seromas or hematomas (despite the drain): While the drain’s purpose is to minimize this, it may not completely eliminate them.
Regular monitoring of the patient’s condition and the drainage characteristics is crucial for early detection and management of potential complications. A proactive approach minimizes the impact of these possibilities.
Q 8. How do you monitor a patient with a Hemovac drain?
Monitoring a patient with a Hemovac drain involves vigilant observation and meticulous documentation. We need to assess several key factors regularly.
- Drainage Output: This is the most crucial aspect. We meticulously measure the amount of drainage at regular intervals (usually every shift, or more frequently if there’s a significant change), noting the color, consistency (serous, serosanguinous, sanguineous, purulent), and odor. A sudden increase in drainage could indicate bleeding or infection, while a decrease might signify a drain blockage. For example, a patient post-abdominal surgery might initially have 200ml of serosanguinous drainage, which should gradually decrease over time. Anything deviating from this expected pattern warrants immediate attention.
- Patient’s Condition: We closely monitor vital signs (heart rate, blood pressure, respiratory rate, temperature, oxygen saturation) for signs of hypovolemia (low blood volume) or infection (fever, tachycardia, increased white blood cell count). Changes in these readings, especially in context with the drainage output, need prompt investigation.
- Drain Site: The site itself is assessed for signs of infection (redness, swelling, warmth, pain, purulent drainage), leakage around the insertion site, or displacement of the drain. We inspect for any signs of inflammation or irritation of the surrounding skin. Any redness or tenderness around the insertion site could indicate infection, a serious complication that needs immediate medical attention.
- Drain Patency: We ensure the Hemovac drain is functioning correctly. We check for kinks in the tubing, ensuring it’s appropriately connected and patent. A blocked drain can lead to fluid accumulation, increasing the risk of infection or complications. Gentle palpation along the tubing can help detect any obstructions.
These observations are critically important because they provide valuable insights into the patient’s healing process and can help us identify potential complications early on.
Q 9. What are the signs and symptoms of Hemovac drain malfunction?
Signs and symptoms of Hemovac drain malfunction vary but often include:
- Decreased or absent drainage: This is a major red flag, often indicating a blockage in the tubing or within the drainage system itself.
- Increased drainage: A sudden, significant increase in drainage volume can signify postoperative hemorrhage.
- Change in drainage characteristics: A shift from serous or serosanguinous drainage to purulent (pus-like) drainage suggests infection. A foul odor is also a strong indicator of infection.
- Pain or tenderness at the insertion site: This can indicate infection, inflammation, or perhaps even a dislodged drain.
- Leakage around the insertion site: Leakage suggests that the drain isn’t properly sealed, increasing the risk of infection.
- Visible kinks or obstructions in the tubing: This can cause the drain to become blocked.
- Patient experiencing signs of shock (hypotension, tachycardia, pale skin): This is indicative of significant blood loss.
Any of these signs warrants immediate attention and further investigation to determine the cause and take appropriate action. For instance, if we observe purulent drainage and a fever, we’d immediately alert the physician and anticipate antibiotic administration.
Q 10. How do you manage a Hemovac drain malfunction?
Managing a Hemovac drain malfunction depends on the specific problem. It’s crucial to:
- Assess the situation: Carefully examine the drain, the tubing, and the insertion site. Measure the drainage output and note its characteristics. Check the patient’s vital signs.
- Address the cause: If the drain is blocked, gentle manipulation of the tubing might resolve the issue (always within the scope of practice and following established protocols; never force). If there’s leakage, we might need to reinforce the dressing. If the issue is significant bleeding, immediate physician notification is critical. Infection requires prompt physician notification and likely antibiotic therapy.
- Notify the physician: For any significant changes in drainage, patient’s condition or suspected malfunction, the physician should be immediately informed. This is not to be delayed; early intervention is key to optimal outcomes.
- Document findings: Precise documentation of all assessments, interventions, and responses is vital for ongoing patient care and risk management.
For example, if we suspect a blockage, we might attempt gentle milking of the tubing (towards the collection chamber). However, we should never force anything or introduce contamination. If this fails, it’s essential to alert the physician as it could be a serious problem that requires intervention, such as the insertion of a new drain.
Q 11. How do you maintain the sterility of a Hemovac drain?
Maintaining the sterility of a Hemovac drain is paramount to prevent infection. This involves several crucial steps:
- Aseptic technique during drainage: When emptying the drain, meticulous aseptic technique is critical. We use clean gloves and maintain a sterile field.
- Proper dressing changes: Dressings should be changed as per protocol, usually every 24 hours or if soiled. We should use sterile gloves and materials.
- Monitoring for signs of infection: Regular assessment of the drainage site is crucial for early detection of infection (redness, swelling, warmth, pain, purulent drainage).
- Maintaining a closed system: Any manipulation of the Hemovac system must preserve its integrity to prevent entry of microorganisms.
- Hand hygiene: Meticulous hand hygiene before and after any contact with the patient or drainage system is essential.
Imagine handling the Hemovac like you would handle a surgical instrument. Every step must be approached with utmost care to avoid contamination.
Q 12. Describe the procedure for emptying a Hemovac drain.
Emptying a Hemovac drain is a crucial nursing procedure requiring strict adherence to sterile technique:
- Hand hygiene: Perform thorough handwashing with soap and water, or use an alcohol-based hand sanitizer.
- Gather supplies: Assemble necessary supplies, including clean gloves, antiseptic solution (e.g., chlorhexidine), measuring device (graduated cylinder), and clean absorbent material.
- Assess the patient: Assess the patient’s comfort level and explain the procedure. Ensure proper patient positioning for comfort and access.
- Don gloves: Put on clean gloves.
- Clean the port: Clean the Hemovac drainage port with antiseptic solution using circular motions, moving from the center outward.
- Open the valve: Open the Hemovac drainage port valve using the proper technique.
- Empty the drainage: Gently pour the contents into the measuring device, carefully documenting the amount.
- Close the valve: Close the Hemovac port valve, ensuring it’s securely closed.
- Measure and record drainage: Record the amount of drainage, noting the time, color, and consistency. Document any notable odors.
- Clean and replace dressing (if indicated): If the dressing is soiled or needs changing, perform a sterile dressing change.
- Discard supplies: Dispose of used supplies properly according to hospital policy.
- Reassess the patient: Assess the patient’s condition and comfort.
It is extremely important to maintain a closed system during this procedure to avoid contaminating the drain. Each step must be performed with precision and care.
Q 13. How do you document Hemovac drain output?
Documentation of Hemovac drain output is critical for accurate assessment of the patient’s recovery and early detection of complications. It’s usually recorded in the patient’s chart and electronic health record. The documentation should include:
- Date and time: Precise timing of each measurement is essential.
- Amount of drainage: The volume of drainage should be recorded in milliliters (mL).
- Color and consistency: Descriptive terms like serous, serosanguinous, sanguineous, or purulent should be used. Any change from previous measurements should be highlighted.
- Odor: Any unusual or offensive odor should be noted.
- Patient’s condition: Any associated symptoms such as fever, pain, or discomfort should be documented.
- Interventions taken: Any actions taken in response to the drainage (e.g., repositioning the drain, changing the dressing) should be recorded.
A typical entry might look like this: “10/26/2024, 0800: Hemovac drain emptied, 150 mL serosanguinous drainage, slight musty odor noted. Patient reports mild discomfort at the insertion site.”
Q 14. What are the nursing interventions for a patient with a Hemovac drain?
Nursing interventions for a patient with a Hemovac drain are multifaceted and aim to prevent complications and promote healing. These include:
- Monitoring drainage output: Frequent monitoring, as previously discussed, is crucial.
- Maintaining drain patency: Regular assessment for kinks or blockages.
- Preventing infection: Strict aseptic technique during dressing changes and drainage.
- Pain management: Administer analgesics as needed to manage pain at the insertion site.
- Patient education: Educate the patient and family on the purpose of the drain, signs of malfunction, and proper care.
- Promoting mobility: Encourage deep breathing and coughing exercises to prevent pulmonary complications.
- Nutritional support: Ensure adequate nutrition to support wound healing.
- Wound care: Provide routine wound care as directed by the physician.
- Frequent reassessment: Regularly assess the patient’s overall condition and note any changes.
Remember, providing holistic care for the patient involves addressing both their physical and psychological needs. Regular communication with the patient and their family is also vital for providing effective nursing care.
Q 15. How do you teach a patient about Hemovac drain care?
Teaching a patient about Hemovac drain care involves breaking down the process into manageable steps and using clear, simple language. I always start by explaining what a Hemovac drain is: a closed-suction system that helps remove fluid from the surgical site, promoting healing and preventing complications. Then, I visually show them the drain and its components. I explain the importance of maintaining a sterile environment to avoid infection.
- Emptying the drain: I demonstrate how to empty the drain, emphasizing hand hygiene and the use of sterile gloves. I show them how to measure the drainage accurately and record it. I use a visual aid like a diagram if needed.
- Cleaning the insertion site: I explain the importance of keeping the insertion site clean and dry. I detail the proper technique: gentle cleaning with soap and water, followed by patting dry – no scrubbing! I’ll provide examples of suitable cleansing solutions. I emphasize avoiding the use of alcohol or hydrogen peroxide, as these can damage the skin.
- Monitoring for complications: I educate the patient about signs of infection (redness, swelling, increased pain, purulent drainage) or other complications (excessive bleeding, unusual drainage). I clearly explain when to contact their physician or nurse.
- Maintaining the system’s integrity: I highlight the importance of keeping the drain and tubing free of kinks and ensuring the drainage system remains closed to prevent air leaks. This might involve showing them how to gently reposition the drain without pulling or tugging on the tubing.
Finally, I answer any questions they have, repeat key instructions, and ensure they understand the process thoroughly. I provide them with written instructions and contact information in case of any concerns or questions. I often relate this to something familiar, like emptying a container, to make it easier for them to grasp the concept.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the discharge instructions for a patient with a Hemovac drain?
Discharge instructions for a patient with a Hemovac drain are crucial for a successful recovery. These instructions are tailored to the individual patient and their specific surgical procedure. However, some common elements always include:
- Drain care instructions: Detailed instructions on how to empty, clean, and monitor the drain, as explained above.
- Wound care instructions: Specific instructions on how to care for the surgical incision, including keeping it clean and dry and recognizing signs of infection.
- Activity restrictions: Guidance on appropriate physical activity levels to prevent complications. This could range from complete bed rest to limited movement.
- Medication instructions: Information on any prescribed pain relievers, antibiotics, or other medications, including dosage, timing, and potential side effects.
- Follow-up appointments: Scheduling of necessary follow-up appointments with the surgeon or healthcare provider for drain removal and wound assessment.
- Signs and symptoms to watch for: A comprehensive list of concerning signs, including increased pain, excessive bleeding, fever, redness, swelling, or foul-smelling drainage, and what steps to take if they occur. I emphasize the importance of immediately reporting any concerning symptoms.
The discharge instructions are always provided in both written and verbal formats, ensuring clear understanding and facilitating easier recall. I take the time to answer all their questions, ensuring they feel confident managing their care at home.
Q 17. How do you assess the effectiveness of Hemovac drainage?
Assessing the effectiveness of Hemovac drainage involves several key steps. Primarily, we monitor the quantity and character of the drainage. The amount of drainage should gradually decrease over time as the wound heals. A sudden increase in drainage could indicate a complication, such as a hematoma or infection.
- Drainage volume: Regularly measuring the volume of drainage (in mL) and documenting it helps monitor the healing process. A steady decline indicates effective drainage.
- Drainage color and consistency: The color and consistency of the drainage provide clues about the healing process. Serous drainage (clear, watery) is generally a good sign of healing. Serosanguineous (pinkish or pale red) indicates a mix of serum and blood and can be normal early in the healing process, but if it persists or increases, it might indicate a problem. Sanguineous (bright red) drainage indicates active bleeding and requires immediate attention.
- Patient assessment: In addition to the objective measures of drainage, we consider subjective indicators like the patient’s pain level, incision site appearance (redness, swelling), and overall well-being. A patient who feels well and whose incision appears healing is a good indicator of effective drainage.
By combining objective measurements of drainage with a careful patient assessment, we gain a comprehensive understanding of the effectiveness of the Hemovac drain and the healing process.
Q 18. How do you differentiate between serous, serosanguineous, and sanguineous drainage?
Differentiating between serous, serosanguineous, and sanguineous drainage is essential for effective wound management. It’s all about the appearance:
- Serous drainage: Clear, watery, and pale yellow in appearance. It’s mostly serum, the liquid component of blood. This is usually a good sign in the later stages of healing.
- Serosanguineous drainage: This is a mixture of serum and blood. It typically appears light pink to pale red, and it’s slightly thicker than serous drainage. It’s common in the early stages of healing but should gradually decrease in volume and color.
- Sanguineous drainage: Bright red and indicates active bleeding. This requires immediate attention as it could signal a serious complication, like a haematoma or vessel injury. It is a clear sign of a problem requiring immediate intervention.
Think of it like this: serous is like plain water, serosanguineous is like water with a little pink food coloring, and sanguineous is like bright red paint.
Q 19. What are the normal values for Hemovac drainage output?
There isn’t a single “normal” value for Hemovac drainage output, as it varies greatly depending on the type of surgery, the size of the surgical site, and the individual patient. However, we generally expect drainage to decrease gradually over time as the wound heals.
Early on, higher volumes might be expected. The crucial aspect is the trend: a steady decrease is a positive sign. A sudden increase warrants further investigation. We also consider the overall context: a small volume of bright red drainage is far more concerning than a large volume of clear or serosanguineous drainage.
For example, a patient on post-operative day one might have 200-300 mL of drainage, while by day three, the volume might be reduced to 50-100 mL, which shows improvement. Specific expected values are determined based on the individual patient, type of surgery, and physician’s preferences.
Q 20. When should you notify the physician about Hemovac drainage?
You should notify the physician about Hemovac drainage under several circumstances:
- Excessive drainage: A sudden and significant increase in drainage volume compared to previous days, regardless of color.
- Change in drainage character: Appearance of bright red (sanguineous) drainage, cloudy or foul-smelling drainage, or a change from serous to serosanguineous or vice-versa.
- Persistent drainage: Drainage that continues beyond the expected time frame of healing.
- Signs of infection: Appearance of redness, swelling, increased pain at the incision site, fever, or chills.
- Drain dislodgment: If the drain is accidentally pulled out or becomes dislodged, immediate medical attention is required.
- Patient discomfort: If the patient experiences significant pain or discomfort, especially if accompanied by other concerning symptoms.
Prompt communication is crucial in preventing serious complications. The early detection and prompt management of any change can lead to better patient outcomes.
Q 21. Describe the proper technique for removing a Hemovac drain.
Removing a Hemovac drain is a sterile procedure performed by a qualified healthcare professional. The exact technique may vary slightly depending on institutional protocols but generally involves:
- Assessment: The patient’s condition and the drainage amount are assessed beforehand.
- Preparation: The site is cleansed with antiseptic solution, and sterile gloves and other equipment are used.
- Drain removal: The drainage system is disconnected, and the drain itself is gently removed while applying slight pressure to the insertion site. This helps to minimize bleeding and potential air entry.
- Wound closure: The insertion site is assessed, and a sterile dressing is applied.
- Post-removal assessment: The patient is monitored for any signs of bleeding or other complications.
The entire process is carefully performed to ensure patient comfort and minimize any risks of infection or complications. The removed drain and its contents are disposed of properly according to hospital waste management policies. The patient is then educated on post-removal wound care instructions.
Q 22. What are the post-removal care instructions for a Hemovac drain site?
Post-removal care for a Hemovac drain site focuses on preventing infection and promoting healing. The area should be kept clean and dry. We instruct patients to gently wash the area with soap and water once a day, patting it dry, rather than rubbing. Any dressings should be changed as prescribed, typically using sterile technique. We’ll monitor the site closely for signs of infection, such as increased redness, swelling, pain, warmth, or purulent drainage. Patients are educated to report any of these signs immediately. Sometimes, a small amount of serosanguinous drainage (a mixture of serum and blood) is normal for a day or two, but anything beyond that needs assessment. We also advise patients to avoid strenuous activity to minimize stress on the incision site and promote healing.
For example, a patient might be instructed to use a sterile dressing pad over the site and change it if it becomes wet or soiled. The patient would then be advised to monitor for signs of infection and contact their healthcare provider immediately if any symptoms develop.
Q 23. What are the different types of surgical drains besides Hemovac?
Besides the Hemovac, several other surgical drains are commonly used, each with its own advantages and disadvantages. These include:
- Jackson-Pratt (JP) drain: This is a smaller, self-contained drain that uses suction to remove fluid. It’s often preferred for smaller incisions.
- Penrose drain: This is a passive drain, meaning it doesn’t use suction. It relies on gravity to drain fluid. It’s simpler than other drains but less effective at removing fluid.
- Blake drain: Similar to a Penrose drain, but with a fenestrated (perforated) tip for better fluid collection.
- Wound Vacuum Assisted Closure (VAC) therapy: This is a more advanced system that applies negative pressure to the wound bed to promote healing and remove fluid. It’s used for larger wounds and more complex cases.
The choice of drain depends on several factors, including the type of surgery, the amount of expected drainage, and the patient’s overall condition. For instance, a patient undergoing a large abdominal surgery might require a Hemovac or VAC therapy, while a patient with a smaller incision might only need a Jackson-Pratt drain.
Q 24. How do you address patient anxiety related to Hemovac drainage?
Addressing patient anxiety related to Hemovac drainage involves open communication, education, and empathy. Many patients are unfamiliar with drains and find them unsettling. I begin by explaining the purpose of the drain in simple terms, emphasizing that it’s a temporary measure to help prevent complications and promote healing. I’ll show them the drain, explaining how it works, and reassure them that it’s not painful. I’ll address specific concerns they may have, such as the appearance of the drainage or the feeling of the drain itself. Providing visual aids, like diagrams or pictures, can also be helpful.
For example, I might say something like, “The Hemovac drain is like a tiny vacuum cleaner that helps remove excess fluid from your surgery site. It’s designed to make your recovery smoother and faster.” I’d also emphasize the importance of monitoring the drainage and reporting any changes to the healthcare team. In some cases, involving a family member or support person in the education process can ease anxieties.
Q 25. What are the legal and ethical considerations related to Hemovac placement?
Legal and ethical considerations surrounding Hemovac placement are primarily focused on informed consent and proper technique. Patients must provide informed consent before any procedure, including drain placement. This means they need to understand the risks and benefits of the procedure, as well as any alternatives. The procedure itself must be performed according to established protocols and standards of care to minimize risks and complications. Accurate documentation of the placement, care, and removal of the drain is crucial for both legal and clinical reasons. This ensures that the patient’s care is well-documented and that any issues can be addressed appropriately. Maintaining patient confidentiality and adhering to HIPAA regulations are paramount.
For instance, failure to obtain informed consent could lead to legal action. Similarly, improper drain placement or management could lead to malpractice claims. Meticulous documentation serves as a protection against these risks.
Q 26. How do you ensure patient safety during Hemovac drain management?
Ensuring patient safety during Hemovac drain management involves several key steps. Strict adherence to sterile technique during dressing changes is crucial to prevent infection. Regular monitoring of drainage output, noting the amount, color, and consistency, is vital to detect potential complications early. We educate patients to watch for signs of infection at the insertion site and to promptly report any concerning changes. Properly securing the drain to prevent accidental dislodgement is also essential. We thoroughly explain the process and provide the patient with appropriate contact information for any questions or concerns. Frequent assessment of the patient’s overall condition is crucial to address any related complications.
For instance, if a patient experiences a sudden increase in drainage or shows signs of infection, this necessitates immediate medical attention. The timely detection of such changes allows for prompt intervention and better patient outcomes.
Q 27. Describe your experience with troubleshooting Hemovac drain issues.
I’ve encountered various Hemovac drain issues throughout my career. One common problem is clogged drains. This can be due to kinking of the tubing, clots in the tubing, or the presence of thick drainage. To troubleshoot this, I’d first gently milk the tubing toward the collection chamber, starting at the insertion site. If this doesn’t work, I may need to reposition the tubing to remove any kinks. If clots are suspected, I may need to flush the drain with sterile saline (following facility protocol). Another issue can be a significant increase in drainage, which may suggest a postoperative complication like a hematoma or seroma (a collection of blood or serum). This necessitates further assessment, potentially including imaging studies. Finally, any signs of infection require prompt intervention with antibiotics and possible surgical debridement.
In one instance, a patient presented with a significant decrease in Hemovac drainage. This turned out to be a blockage due to clotting, which we addressed through careful assessment and flushing of the drainage system. The patient’s post-operative care, including regular monitoring of drainage, ensured prompt detection and successful resolution.
Q 28. Explain how you would educate a patient and family member on Hemovac care.
Educating patients and family members about Hemovac care involves a multi-faceted approach. I begin with a clear explanation of the drain’s purpose, using simple language and avoiding medical jargon. I’ll show them the drain and its components, explaining how it works. We review proper hygiene practices, emphasizing the importance of handwashing before touching the drain site. I’ll demonstrate how to empty the collection chamber and record the amount of drainage, highlighting the importance of accurate documentation. We’ll discuss signs and symptoms of infection and what steps to take if these occur. Finally, we’ll provide clear and readily available contact information for any questions or concerns. Involving the family allows for shared understanding and support during the recovery process.
For instance, I might provide a written instruction sheet, reinforced with a verbal explanation, and even offer a demonstration on how to monitor and empty the drain. Clear communication, reinforced with visual aids and written instructions, increases understanding and promotes patient safety and recovery.
Key Topics to Learn for Hemovac Placement Interview
- Hemovac System Anatomy and Function: Understand the components of the Hemovac drainage system, including the canister, tubing, and drainage port. Comprehend its mechanism for fluid collection and its role in wound management.
- Placement Technique and Procedures: Master the proper techniques for inserting and securing a Hemovac drain, including patient positioning, incision site preparation, and suture management. Be prepared to discuss variations in placement depending on surgical site and patient condition.
- Post-Placement Care and Monitoring: Detail the crucial aspects of post-operative Hemovac care, such as monitoring drainage volume and character, assessing for complications (e.g., infection, dislodgement), and providing patient education.
- Troubleshooting and Problem-Solving: Discuss common Hemovac-related issues, such as leaks, kinks in tubing, or inadequate drainage. Explain your approach to diagnosing and resolving these problems safely and effectively.
- Safety Protocols and Infection Control: Demonstrate a thorough understanding of infection control measures related to Hemovac placement and management, emphasizing sterile technique and proper disposal procedures.
- Patient Assessment and Communication: Be ready to discuss your approach to assessing patient comfort and potential complications, and how you would communicate effectively with patients and healthcare team members regarding Hemovac management.
Next Steps
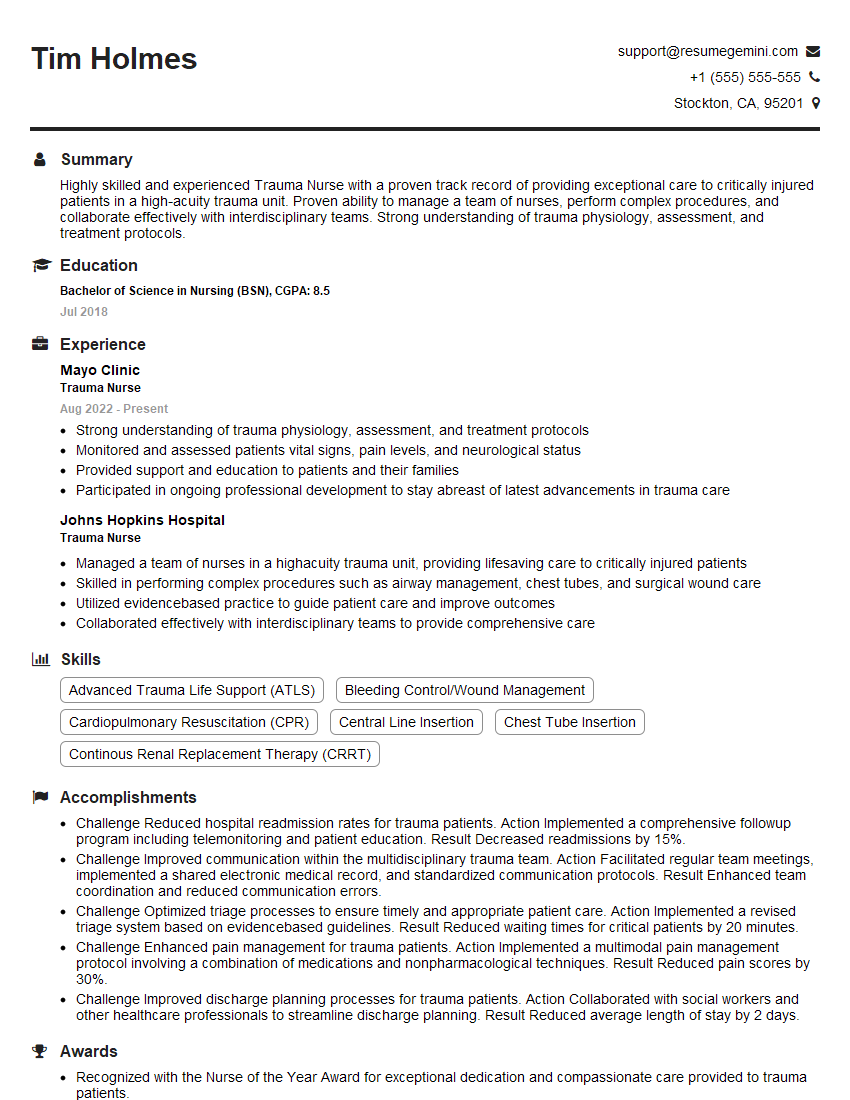
Mastering Hemovac placement demonstrates valuable surgical skills and attention to detail, significantly enhancing your career prospects in healthcare. An ATS-friendly resume is crucial for getting your application noticed. To build a compelling and effective resume that highlights your Hemovac expertise and other skills, we strongly recommend using ResumeGemini. ResumeGemini provides a user-friendly platform for creating professional resumes, and we offer examples of resumes tailored to Hemovac Placement to help you get started. Take the next step in your career journey – build a resume that gets results.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good