Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Nasogastric Tube Placement interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Nasogastric Tube Placement Interview
Q 1. Describe the steps involved in performing nasogastric tube placement.
Nasogastric (NG) tube placement is a common procedure involving inserting a flexible tube through the nose, down the esophagus, and into the stomach. It’s crucial to remember patient comfort and safety are paramount throughout the process.
- Assessment: Assess the patient’s nasal passages for patency, checking for any obstructions or deformities. Consider the patient’s gag reflex and level of consciousness.
- Preparation: Gather necessary supplies: NG tube of appropriate size and length, lubricant, measuring tape, syringe, gloves, antiseptic solution, suction equipment (optional), pH testing strips or imaging device (for verification). Explain the procedure to the patient, obtaining informed consent if necessary.
- Measurement: Measure the distance from the tip of the nose to the earlobe, and then to the xiphoid process. This measurement helps determine the appropriate insertion depth, preventing accidental lung placement. This measurement is a guideline and may need adjustments based on the individual patient.
- Lubrication and Insertion: Lubricate the NG tube generously. Gently insert the tube through the nostril, following the anatomical pathway. Advise the patient to swallow sips of water to facilitate passage, or tilt their head slightly back.
- Securing the Tube: Once the tube is in place (verified using the methods discussed later), secure it to the patient’s nose with tape. Avoid applying excessive pressure, which can cause skin breakdown. Document the procedure, including tube size, insertion time, and verification method.
- Post-Insertion Care: Regularly assess the tube placement, monitor for any signs of complications, and provide ongoing patient education on the importance of keeping the tube patent and clean.
Q 2. What are the indications for nasogastric tube placement?
NG tube placement is indicated for various reasons, all centering on the need to bypass the normal oral route for feeding, medication administration, or gastric decompression.
- Gastric Decompression: Removing stomach contents in cases of bowel obstruction, ileus, or post-operative situations.
- Enteral Feeding: Providing nutrition when the patient cannot swallow or needs supplementary caloric intake, such as in cases of stroke, trauma, or severe illness.
- Medication Administration: Administering medications, especially those that may cause esophageal irritation or are difficult to swallow.
- Gastric Lavage: Washing out the stomach, for example, after ingestion of poison.
- Sampling Gastric Contents: Obtaining samples for analysis (e.g., pH measurement or aspirating for blood).
The specific indication will always be determined by the patient’s clinical presentation and the healthcare provider’s assessment.
Q 3. What are the contraindications for nasogastric tube placement?
Contraindications are situations where NG tube placement is either not advisable or outright dangerous. These include:
- Severe facial trauma or nasal deformity: Insertion may be difficult or impossible, and may cause further damage.
- Recent nasal surgery or significant nasal bleeding: Insertion could cause bleeding or disrupt the healing process.
- Esophageal strictures or obstructions: The tube may not be able to pass, or could cause injury.
- Coagulopathy (bleeding disorder): Increased risk of bleeding during insertion or afterward.
- Severe gastroesophageal reflux disease (GERD): The tube may exacerbate GERD symptoms.
- Inability to obtain patient consent (when applicable): Ethical considerations require informed consent, except in emergency situations.
Careful assessment of the patient’s condition is vital to determine the suitability of NG tube placement. When in doubt, alternative methods such as a nasojejunal tube or percutaneous endoscopic gastrostomy (PEG) should be considered.
Q 4. Explain the different types of nasogastric tubes and their uses.
Several types of NG tubes are available, each suited to a particular need. The choice depends on factors like the patient’s condition, the purpose of placement, and the duration of use.
- Standard NG tubes: These are the most common type, made of soft, pliable material, available in various diameters (French sizes). They’re used for general feeding, medication administration, and gastric decompression.
- Levin tubes: A single-lumen tube with several holes near the distal end, suitable for both suctioning and feeding.
- Salem sump tubes: Double-lumen tubes; one lumen for suction and the other for venting to prevent pressure build-up in the stomach.
- Dobbhoff tubes: Small-diameter, flexible tubes, ideal for long-term feeding; their smaller size is gentler on the nasal passages.
The choice of tube size and type needs careful consideration for patient comfort and effectiveness of the procedure. For instance, larger diameter tubes may be easier for feeding but can be less comfortable for the patient, while smaller tubes may be more comfortable but may clog easily.
Q 5. How do you verify the placement of a nasogastric tube?
Verification of NG tube placement is critically important to prevent life-threatening complications like aspiration pneumonia. There are several methods:
- Aspiration of Gastric Contents: Aspirating stomach contents and testing their pH (pH should be less than 5.5). This is a widely used method, but isn’t always foolproof, particularly with patients who have gastroesophageal reflux.
- X-ray confirmation: This is the gold standard, providing definitive confirmation of the tube’s position. An X-ray clearly shows the tube’s location in relation to the stomach and other anatomical structures.
- Auscultation: Injecting air into the tube while auscultating over the epigastric region (the upper abdomen). Hearing a whooshing sound indicates the tube’s placement in the stomach. However, this method has a high false-positive rate and should not be solely relied upon.
- Colorimetric Methods: Some tubes have a color-changing marker that indicates the presence of specific substances, for example, changes color when it comes in contact with stomach acid.
Multiple methods are often used to ensure accuracy. Incorrect NG tube placement can have serious consequences, thus confirmation is not a step to be skipped or taken lightly.
Q 6. What are the potential complications associated with nasogastric tube placement?
Several complications can arise during and after NG tube placement.
- Nasal or esophageal trauma: Bleeding, irritation, or perforation of the nasal mucosa or esophagus.
- Aspiration pneumonia: Accidental introduction of gastric contents into the lungs.
- Sinusitis: Infection of the sinuses.
- Tube displacement or blockage: The tube can move out of place or become obstructed by food or secretions.
- Nausea and vomiting: Common side effects, often related to tube irritation or the type of material being administered.
- Diarrhea or constipation: Changes in bowel habits can be associated with the type of formula being used or the tube’s presence.
- Electrolyte imbalances: Can occur in some cases, particularly with long-term enteral nutrition.
Preventive measures, such as proper tube insertion technique, regular monitoring, and adequate patient education, play a crucial role in minimizing these risks.
Q 7. How do you manage a patient experiencing complications from an NG tube?
Managing complications depends on the specific problem.
- Bleeding: If bleeding occurs, remove the tube and apply direct pressure. Consult a physician for further evaluation and management.
- Aspiration: Immediate treatment may include suctioning, oxygen administration, and intravenous fluids. Antibiotics may be prescribed if an infection develops.
- Tube Displacement: Re-insert the tube following proper procedure. If unable to reinsert, consult physician.
- Blockage: Try flushing the tube with warm water (unless contraindicated). If the blockage persists, consider replacing the tube.
- Infection: Administer antibiotics as prescribed by the physician. Monitor for signs of sepsis.
- Electrolyte imbalances: May require intravenous fluid correction and close monitoring of electrolyte levels.
Prompt assessment and appropriate intervention are key to effectively managing complications and improving patient outcomes. Continuous monitoring and communication among healthcare professionals are crucial for positive results.
Q 8. Describe the procedure for removing a nasogastric tube.
Removing a nasogastric (NG) tube is a relatively straightforward procedure, but safety and patient comfort are paramount. First, we verify the physician’s order for removal. Then, we explain the process to the patient, reassuring them and answering any questions. We then perform hand hygiene and don gloves. The patient is positioned comfortably, usually sitting upright. Gently, we remove the tape securing the tube to the patient’s nose. While supporting the tube near the nares, we slowly and steadily withdraw the tube, advising the patient to take slow, deep breaths to minimize discomfort. Once the tube is removed, we inspect it for intactness, noting the length removed to verify correct placement originally. Next, we assess the patient’s nares for any signs of irritation or bleeding. Finally, we document the time and date of removal, the patient’s tolerance of the procedure, and any observations made. In some cases, a small amount of saline flush is performed prior to removal to ensure the tube remains patent and free of obstruction.
Q 9. How do you assess a patient’s suitability for nasogastric tube placement?
Assessing a patient’s suitability for NG tube placement involves a comprehensive evaluation. We first check the physician’s order and ensure the rationale for NG tube placement is documented (e.g., feeding, medication administration, gastric decompression). We then assess the patient’s overall condition, looking for contraindications such as nasal obstruction, recent nasal surgery, facial trauma, or bleeding disorders. A thorough assessment of the patient’s gag reflex is crucial; a severely impaired gag reflex increases the risk of aspiration. We also consider the patient’s ability to cooperate during the procedure. For patients who are combative or unable to cooperate, alternative feeding methods may be more appropriate. Finally, we assess the patient’s airway and breathing to minimize the risk of complications during the procedure. A properly performed assessment minimizes complications and ensures patient safety.
Q 10. What are the nursing considerations for patients with NG tubes?
Nursing considerations for patients with NG tubes are multifaceted and focus on preventing complications. Regular monitoring of tube placement is crucial; this often involves checking the pH of aspirated gastric contents and/or obtaining an X-ray. We carefully monitor fluid balance, intake and output, and the patient’s weight. We regularly assess for signs of aspiration (e.g., coughing, shortness of breath, fever). Nasal care is essential to prevent irritation and infection. Regular oral hygiene is performed as well, to maintain comfort and minimize bacterial growth in the mouth and throat. Patient education regarding the purpose and care of the NG tube is vital. We also assess for signs of complications like diarrhea, constipation, or electrolyte imbalances which can result from the use of NG tubes.
- Regular assessment of tube placement: This is crucial to prevent medication or feedings from entering the lungs.
- Careful monitoring of fluid balance: Prevents dehydration or fluid overload.
- Regular nasal and oral hygiene: Reduces the risk of infection.
Q 11. What are the signs and symptoms of NG tube misplacement?
Misplacement of an NG tube can have serious consequences, including aspiration pneumonia. Signs and symptoms of misplacement include coughing, choking, cyanosis (bluish discoloration of the skin), respiratory distress, and the presence of excessive air bubbles in the aspirate. If the tube is in the lungs, the aspirate pH will be close to 7. If it is correctly positioned in the stomach, the pH should be less than 5. A significant change in patient status, like sudden respiratory distress, after NG tube insertion or medication administration, should immediately raise suspicion of misplacement. It’s also important to note that the patient might experience discomfort or report a burning sensation if the tube is in an incorrect location. Immediate action is necessary to correct any suspected misplacement; typically the physician is notified and an X-ray is obtained to verify positioning.
Q 12. How do you prevent complications during NG tube insertion?
Preventing complications during NG tube insertion involves meticulous attention to detail and adherence to strict protocols. Before insertion, we confirm the physician’s order and verify the patient’s identity. Thorough hand hygiene and the use of gloves are essential. Lubricating the tube with a water-soluble lubricant reduces friction and discomfort. Proper measurement and positioning techniques are critical. Aspirating the contents and checking pH helps confirm proper placement. Continuous monitoring of the patient’s vital signs and respiratory status during and after insertion is vital. Careful attention to the patient’s comfort level throughout the process minimizes anxiety and promotes cooperation. Following all agency policies and procedures minimizes risk and maintains quality care.
Q 13. How do you maintain the patency of a nasogastric tube?
Maintaining the patency of an NG tube is critical for effective feeding and medication administration. Regular flushing with sterile water or saline is crucial; this prevents clogging. The amount and frequency of flushing are determined by the type of feeding or medication administered. We should observe the aspirate for any signs of obstruction or change in color, consistency, or amount, which could indicate blockage. If blockage is suspected, we should attempt to clear it with the appropriate method, such as gentle irrigation with sterile water. We should also monitor for signs of tube displacement, and if any signs of tube dislodgement are observed, we must validate its placement.
Q 14. Explain the process of administering medications through an NG tube.
Administering medications through an NG tube requires precision and careful technique. Before administering any medication, we confirm the order and check for any contraindications. We crush tablets into a fine powder, if applicable. We reconstitute the medication with the appropriate amount of water. We flush the tube with water before and after administering the medication to prevent clogging and ensure proper delivery. We always verify tube placement before each medication administration. We check medication compatibility before administering multiple medications through an NG tube to prevent reactions. Never administer medications that cannot be crushed or will not dissolve in water. We meticulously document each medication administered, including the time, dose, and patient response. The nurse must be knowledgeable on incompatibilities and proper techniques.
Q 15. What are the safety precautions to take during NG tube placement?
Nasogastric (NG) tube placement, while a common procedure, demands strict adherence to safety protocols to minimize risks to the patient. These precautions are crucial because incorrect placement can lead to serious complications such as lung injury (aspiration pneumonia), esophageal perforation, or bleeding.
- Patient Identification and Verification: Always confirm the patient’s identity using two identifiers (e.g., name and date of birth) before starting the procedure. This prevents medication errors and ensures the right patient receives the correct treatment.
- Hand Hygiene: Meticulous hand hygiene is paramount to reduce the risk of infection. Wash your hands thoroughly with soap and water or use an alcohol-based hand rub before and after the procedure.
- Proper Equipment Preparation: Ensure all equipment is sterile and functional. This includes the NG tube itself, lubricant, gloves, measuring tape, and any necessary suction apparatus. Check the NG tube for any kinks or damage before use.
- Patient Positioning: The patient should be in a high-Fowler’s position (sitting upright) to facilitate tube insertion and minimize the risk of aspiration. A comfortable position is also crucial to reduce patient anxiety.
- Monitoring Patient Response: Throughout the procedure, carefully observe the patient for signs of distress, such as coughing, choking, cyanosis (bluish discoloration of the skin), or difficulty breathing. Stop immediately if any of these occur.
- Post-Insertion Verification: After insertion, it’s crucial to confirm proper placement using methods such as chest x-ray and aspirating gastric contents. This helps to verify that the tube is in the stomach and not in the lungs.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you calculate the appropriate length for NG tube insertion?
Calculating the appropriate NG tube length is crucial to ensure correct placement and prevent complications. An inaccurate measurement can lead to the tube ending up in the lungs (aspiration) or not reaching the stomach, rendering it ineffective.
The standard method involves measuring from the tip of the nose to the earlobe, and then to the xiphoid process (the bottom of the sternum). This measurement provides an estimate of the required tube length. However, this is just an estimate, and final placement verification with a chest x-ray is mandatory.
Example: Let’s say the measurement from the nose to the earlobe is 10cm and from the earlobe to the xiphoid process is 40cm. The total estimated length would be 50cm. However, it’s important to remember that this is only an estimate, and the actual length required might vary depending on the individual’s anatomy.
Q 17. What are the key points for documenting NG tube placement and care?
Accurate and thorough documentation is essential for maintaining patient safety and providing continuity of care. The documentation should clearly reflect the entire process, from pre-insertion assessment to post-insertion monitoring.
- Pre-procedure Assessment: Record the patient’s vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation before beginning.
- Procedure Details: Document the type and size of the NG tube used, the measurement used for insertion, the method used to verify placement (e.g., x-ray, pH testing, aspiration of gastric contents), and the time of insertion.
- Post-procedure Assessment: Document the patient’s vital signs and any complications or adverse events after insertion. Note the amount and characteristics of any aspirated gastric contents.
- Ongoing Care: Document the ongoing care provided, including flushing of the tube, medication administration, and any drainage or output.
- Complications or Adverse Events: Any issues, such as discomfort, bleeding, coughing, or aspiration, should be clearly documented along with interventions taken.
Using a standardized documentation format helps prevent errors and ensures that all relevant information is readily available to healthcare professionals involved in the patient’s care.
Q 18. Describe your experience with different sizes and types of NG tubes.
I have extensive experience with various sizes and types of NG tubes, recognizing that the appropriate choice depends on the individual patient’s needs and clinical circumstances. Factors such as age, anatomy, and the purpose of the tube (feeding, medication administration, or decompression) influence the selection.
Size: Tube sizes are expressed in French gauge (Fr), ranging from 8 Fr to 18 Fr. Smaller sizes (8-10 Fr) are often preferred for children or individuals with small esophageal openings, while larger sizes (14-18 Fr) might be used for feeding or gastric decompression.
Types: Different types include:
- Standard Polyvinyl Chloride (PVC) tubes: These are commonly used, relatively inexpensive, and easy to use.
- Silicone tubes: More comfortable for long-term use, biocompatible, and less likely to cause irritation or adhere to the mucosa.
- Dobbhoff tubes: These have a smaller diameter and are less likely to cause irritation during long-term use.
Example: A frail elderly patient with dysphagia might benefit from a smaller, softer silicone tube for long-term feeding, whereas a patient requiring gastric decompression after surgery might need a larger PVC tube. The selection requires careful consideration of the patient’s specific needs.
Q 19. How would you handle resistance during NG tube insertion?
Encountering resistance during NG tube insertion is common and often indicates an anatomical obstruction. It is crucial to handle this situation carefully and avoid forcing the tube, which could cause significant damage.
Approach:
- Assess the Situation: Stop immediately and try to identify the cause of resistance. Is it an anatomical issue (e.g., stricture, tumor), improper positioning, or a kink in the tube?
- Re-evaluate Technique: Check the patient’s position, and ensure the tube is not coiled or kinked. Sometimes, slight adjustments in the angle of insertion can help overcome the obstruction.
- Lubrication: Apply additional water-based lubricant to the tube to ease insertion.
- Avoid Force: Never force the tube, as this can lead to esophageal perforation or trauma.
- Alternative Methods: In some cases, alternate techniques, such as using a different size or type of NG tube, might be needed.
- Seek Assistance: If resistance persists, consult a more experienced colleague, and consider radiologic guidance.
It is paramount to prioritize patient safety and never compromise this for the sake of quick completion of the procedure.
Q 20. What are the common causes of NG tube blockage?
NG tube blockage is a common complication, particularly with long-term use, compromising the patient’s nutrition and medication delivery. Several factors contribute to blockages:
- Medication Residue: Some medications, particularly crushed tablets or those with a high binding capacity, can adhere to the tube walls, causing a blockage.
- Formula Thickening: Using formulas that are too thick can lead to solidification within the tube.
- Dehydration: Dehydration can increase the viscosity of gastric contents, making them more prone to clumping and blockage.
- Food Particles: In some cases, particulate matter or improperly mixed feeding formulas might inadvertently enter the tube and cause blockages.
- Tube Material: Certain tube materials can be more prone to clogging than others.
Prevention Strategies: Frequent flushing with water, using appropriately sized tubes for the viscosity of the feeding solution, and meticulous attention to preparing feeding solutions can all reduce the risk of blockage.
Q 21. What is your approach to managing a patient who is coughing or choking during NG tube placement?
Coughing or choking during NG tube insertion indicates that the tube may be in the airway (trachea) or has stimulated the airway reflex. This is a serious complication that needs to be addressed immediately.
Immediate Actions:
- Stop the Procedure: Immediately stop the insertion process to prevent further injury.
- Remove the Tube: Gently withdraw the tube to remove it from the airway.
- Assess the Patient: Check the patient’s vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) to ensure there’s no respiratory compromise or other adverse events.
- Oxygen Support: Provide supplementary oxygen if necessary.
- Suction: If needed, use suction to clear the airway of any secretions.
- Reassess and Restart (if necessary): After addressing the airway issue, the NG tube placement can be attempted again only after appropriate reassessment and, potentially, a change of technique or with additional assistance.
If the coughing and choking are severe or persistent, it’s crucial to seek immediate assistance from a colleague or respiratory therapist. Documentation of the event and the steps taken is essential.
Q 22. How do you address patient discomfort during NG tube procedures?
Addressing patient discomfort during NG tube placement is paramount. It’s a procedure that can cause anxiety and physical distress. My approach is multifaceted, starting with thorough pre-procedure education. I explain the process step-by-step, using simple language and visuals, answering all questions patiently. I also emphasize the benefits of the procedure to alleviate any concerns. During the procedure, I use topical anesthetic sprays or gels to numb the nasal passages, minimizing discomfort. I employ slow, gentle insertion techniques, frequently pausing to check the patient’s comfort level and adjust as needed. I reassure and distract patients with calming conversation or music, depending on their preference. Post-procedure, I provide analgesics as prescribed and monitor for any complications, such as nasal irritation or bleeding. Continuous assessment and patient-centered communication are key to managing discomfort effectively.
Q 23. Explain the role of radiology in verifying NG tube placement.
Radiology plays a crucial role in verifying NG tube placement. While techniques like checking pH or aspirating gastric contents offer initial indications, they aren’t foolproof. Chest X-ray is the gold standard for confirming that the tube is in the stomach and not in the lungs (a potentially life-threatening complication). The X-ray clearly shows the position of the tube relative to anatomical landmarks. If the image shows the tip of the NG tube in the esophagus or trachea, immediate corrective action is required. I always order a chest X-ray to verify placement, especially for patients at higher risk of complications or if there’s any doubt using other methods. This helps avoid potential complications and ensures patient safety.
Q 24. How do you manage a patient with an accidental dislodgement of their NG tube?
Accidental NG tube dislodgement requires immediate action to prevent complications and restore feeding or medication administration. First, I assess the patient’s condition for any signs of distress, such as respiratory compromise or discomfort. Then, I would attempt to reinsert the existing tube if it is still available and intact, following the same procedure as initial placement. If re-insertion isn’t possible or deemed unsafe, I will order a new NG tube. In either case, confirmation of proper placement is essential via chest X-ray. Close monitoring of the patient’s vital signs, hydration status, and overall well-being is critical post-dislodgement. Depending on the patient’s condition and the reason for the NG tube, I’d consult with the physician to determine the appropriate course of action. Documentation of the entire event, including the cause of dislodgement and subsequent actions, is essential.
Q 25. Describe your experience with providing patient and family education about NG tube care.
Patient and family education is a significant part of my practice. I believe that informed patients are better equipped to manage their care. When placing an NG tube, I always take the time to explain the purpose, procedure, and potential complications in a clear, concise manner. I use simple, non-medical terms, and I answer questions patiently and thoroughly. I provide written instructions and visual aids demonstrating proper NG tube care, including cleaning, flushing, and preventing blockage. I emphasize the importance of reporting any issues to the healthcare team promptly. I involve family members in the educational process, empowering them to support the patient’s recovery. I check for understanding and provide ongoing support as needed. For instance, I’ve had several patients and their families express concerns about aspiration. I address this by thoroughly explaining the risk and how we mitigate it through proper placement verification and careful feeding techniques.
Q 26. How do you prioritize patient safety during NG tube placement and maintenance?
Prioritizing patient safety during NG tube placement and maintenance involves a multi-pronged approach. Strict adherence to aseptic techniques minimizes infection risk. Thorough verification of tube placement through X-ray is essential. Regular monitoring of the patient’s respiratory status, hydration, and bowel sounds prevents complications. Using the correct size and type of NG tube for the patient’s anatomy and condition is important. Proper tube anchoring prevents accidental dislodgement. Regular flushing of the tube maintains patency and prevents blockages. Careful medication and feeding administration avoids aspiration and other complications. The entire team’s involvement is crucial; open communication and timely reporting of any issues are critical for ensuring patient safety.
Q 27. What are the legal and ethical considerations related to NG tube placement?
Legal and ethical considerations surrounding NG tube placement are complex. Informed consent is paramount – patients must understand the procedure, its risks and benefits, and alternative options. Documentation of the consent process is crucial. The procedure must be medically indicated and proportionate to the patient’s needs. Patient autonomy and dignity must be respected throughout the process. Confidentiality is crucial, protecting patient information. Proper training and competency in NG tube placement are essential for healthcare professionals. Any adverse events must be reported and documented thoroughly. Legal issues might arise from negligence or lack of informed consent. Ethical considerations might involve end-of-life care decisions where NG tube placement is relevant. Maintaining high ethical standards and adhering to legal regulations ensures patient well-being and avoids potential legal repercussions.
Q 28. Describe a time you had to troubleshoot a problem with an NG tube.
I once encountered a situation where an NG tube became completely blocked despite regular flushing. The patient was experiencing significant discomfort and was unable to receive necessary medications or nutrition. Initially, I tried various flushing techniques with saline and other solutions, but the blockage persisted. I suspected a medication residue build-up. I carefully reviewed the medication administration record and discovered that the patient had been receiving several medications known to have high viscosity. I then used an enzymatic solution to break down the residue, followed by repeated flushing with warm water. This successfully cleared the blockage. The chest X-ray confirmed that the tube was still correctly positioned. Post-incident, we adjusted the medication administration protocol to reduce the risk of future blockages. This situation underscored the importance of thorough medication reconciliation and problem-solving approaches in managing NG tubes.
Key Topics to Learn for Nasogastric Tube Placement Interview
- Anatomy and Physiology: Thorough understanding of the nasal cavity, pharynx, esophagus, and stomach; potential anatomical variations and their implications for tube placement.
- Indications and Contraindications: Mastering the criteria for appropriate NG tube insertion and recognizing situations where it’s contraindicated, including patient-specific considerations.
- Procedure Techniques: Detailed knowledge of different NG tube insertion methods, including the use of various sizes and types of tubes. Practice explaining the steps clearly and concisely.
- Verification of Placement: Comprehensive understanding of methods for confirming correct tube placement, including X-ray confirmation, aspiration of gastric contents, and pH testing. Be prepared to discuss the pros and cons of each method.
- Potential Complications and Management: Familiarity with potential complications such as nasal trauma, esophageal perforation, and misplacement. Demonstrate your ability to troubleshoot and manage complications effectively.
- Post-Placement Care: Knowledge of appropriate post-insertion care, including securing the tube, monitoring for complications, and providing patient education.
- Legal and Ethical Considerations: Understanding informed consent, patient rights, and documentation requirements related to NG tube placement.
- Troubleshooting and Problem-Solving: Be prepared to discuss scenarios involving tube displacement, blockage, or patient discomfort, and how you would address these situations.
Next Steps
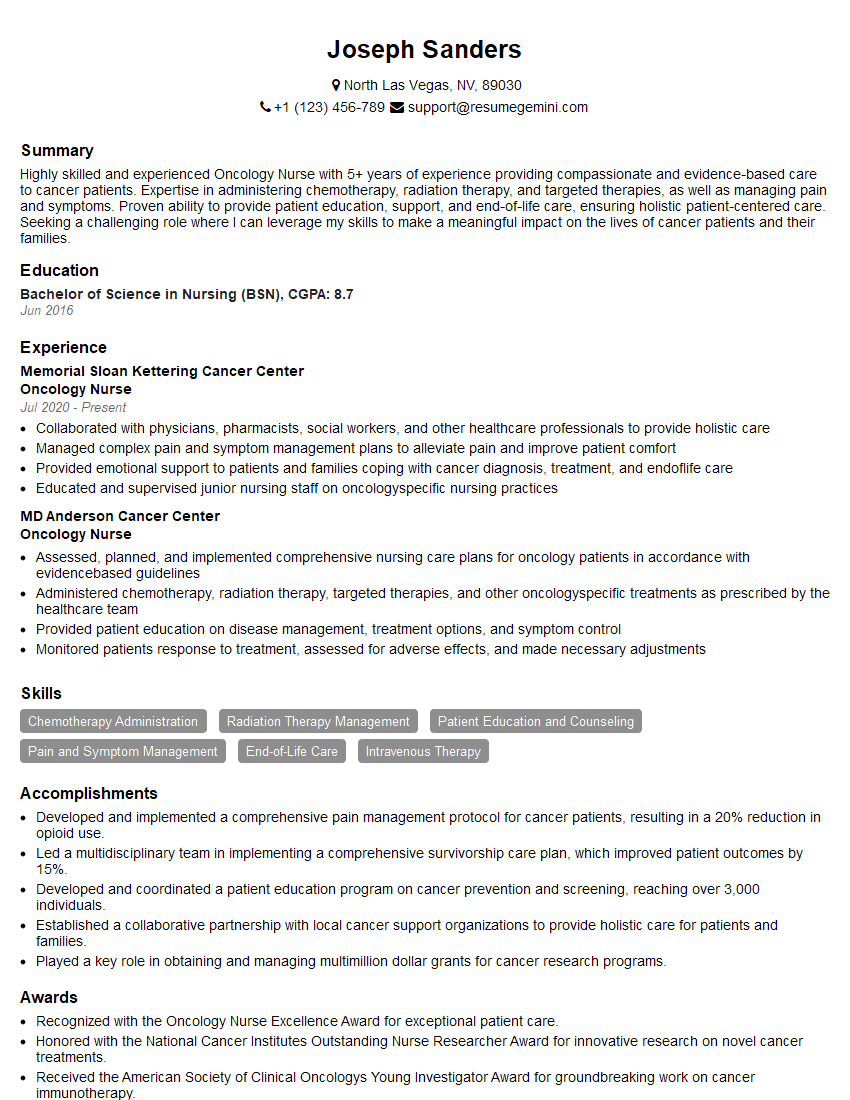
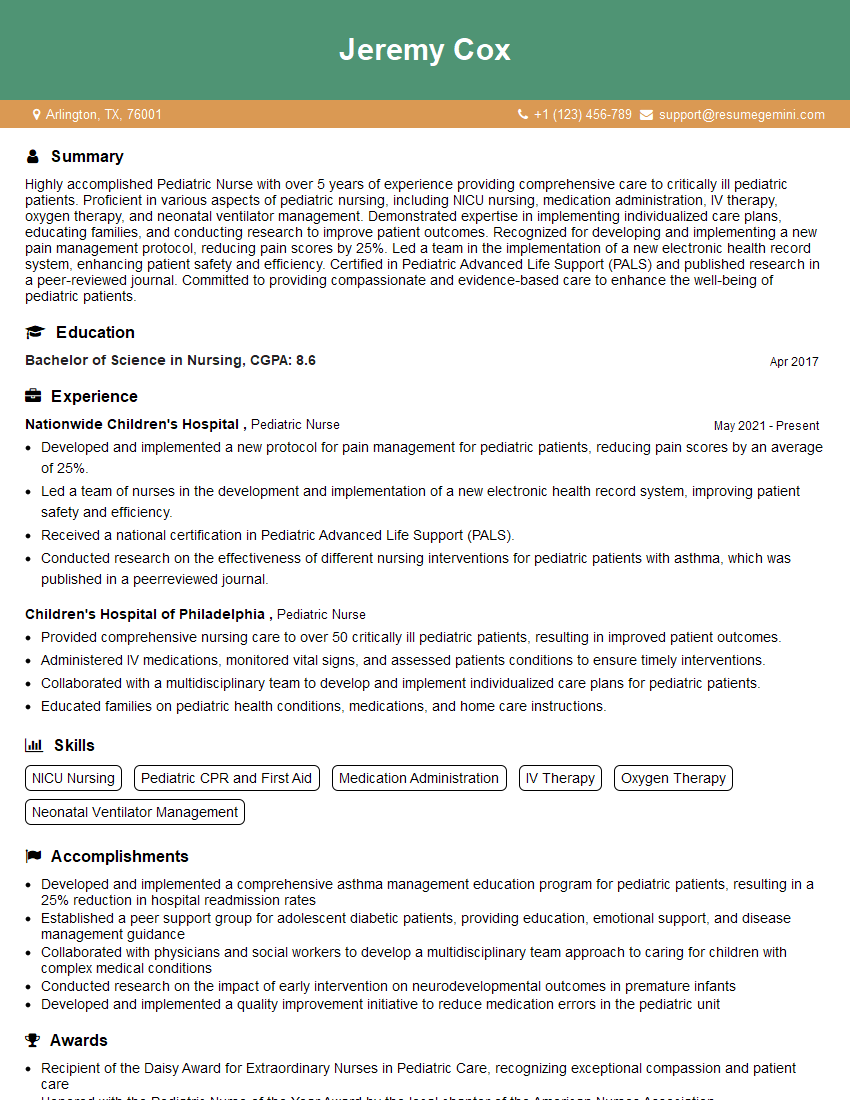
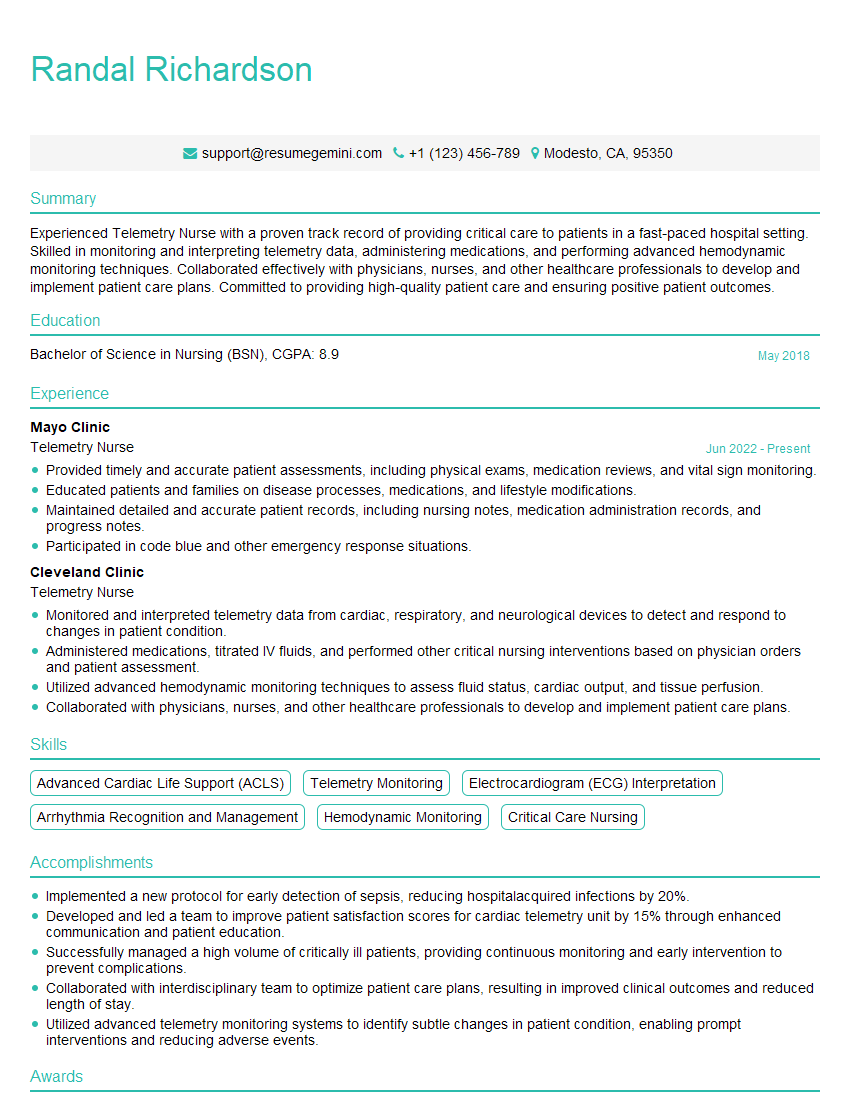
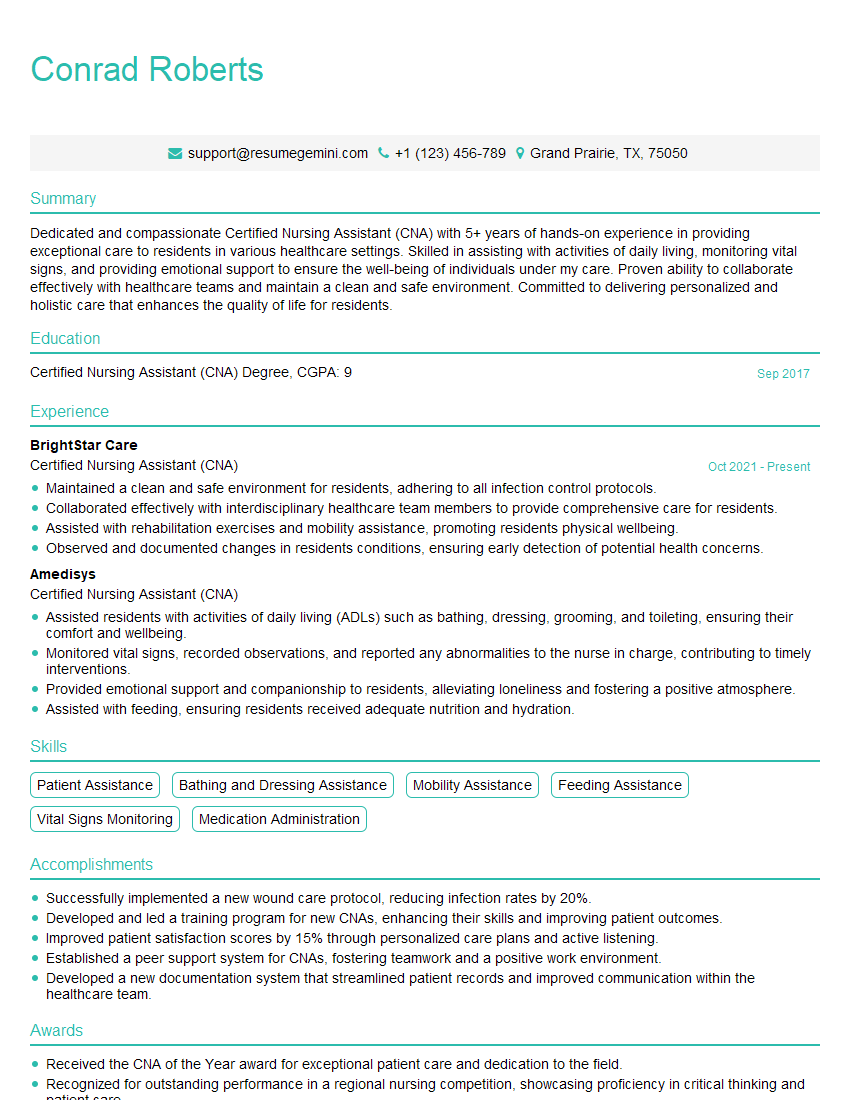
Mastering Nasogastric Tube Placement demonstrates crucial clinical skills highly valued by employers in healthcare settings. This expertise significantly enhances your career prospects and opens doors to various advanced roles. To further strengthen your job application, focus on creating an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your qualifications stand out to recruiters. Examples of resumes tailored to Nasogastric Tube Placement professionals are available to guide you through this process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good