Unlock your full potential by mastering the most common Needle Decompression interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Needle Decompression Interview
Q 1. Describe the indications for needle decompression.
Needle decompression, also known as needle thoracostomy, is a life-saving emergency procedure used primarily to relieve a tension pneumothorax. A tension pneumothorax is a life-threatening condition where air accumulates in the pleural space (the area between the lung and the chest wall), causing increased pressure that collapses the lung and compromises cardiovascular function. Indications for needle decompression include:
- Suspected tension pneumothorax: This is the primary indication, characterized by signs and symptoms like respiratory distress, decreased breath sounds on one side, tracheal deviation (shifting of the trachea away from the affected side), and hypotension.
- Rapidly deteriorating respiratory status: If a patient’s respiratory condition is worsening despite other interventions, needle decompression may be considered.
- Pre-hospital setting: In situations where rapid intervention is critical and definitive chest tube insertion is delayed, needle decompression provides immediate relief.
Essentially, if a patient exhibits signs of a tension pneumothorax and immediate relief is needed, needle decompression is indicated. Remember, it’s a temporary measure until definitive chest tube placement can be performed.
Q 2. What are the contraindications for needle decompression?
While needle decompression is a vital procedure, it’s not without contraindications. These are situations where the procedure shouldn’t be attempted or should be approached with extreme caution:
- Absence of clinical signs of tension pneumothorax: Performing the procedure without clear evidence of a tension pneumothorax is inappropriate and potentially harmful. A proper diagnosis is paramount.
- Presence of a clotting disorder: The risk of bleeding increases significantly in patients with clotting disorders.
- Patient with significant underlying lung pathology: Severe underlying lung disease may make needle decompression less effective or increase the risk of complications.
- Inability to adequately visualize anatomical landmarks: Obese patients or those with significant anatomical deformities may pose challenges in accurate needle placement.
Careful consideration of these contraindications is crucial to ensuring patient safety and the appropriate use of this life-saving procedure. Always prioritize proper diagnosis and consider the individual patient’s clinical circumstances before proceeding.
Q 3. Explain the anatomical landmarks used for needle decompression in a tension pneumothorax.
For needle decompression of a tension pneumothorax, accurate anatomical landmark identification is critical to avoid vital structures like the intercostal vessels and nerves. The procedure typically targets the second intercostal space in the mid-clavicular line on the affected side. Here’s a breakdown:
- Second intercostal space: This space is identified by palpation, counting down from the clavicle (collarbone). The second rib is a palpable bony structure, and the space between the second and third ribs is the target area.
- Mid-clavicular line: This line runs vertically downward from the midpoint of the clavicle. It’s crucial to locate this line accurately to guide needle placement.
Imagine drawing a horizontal line across the chest at the level of the second rib, and then a vertical line down the middle of the clavicle. The intersection of these lines represents the ideal entry point for the needle. Always double-check the landmarks before initiating the procedure.
Q 4. What size needle is typically used for needle decompression?
The needle size commonly used for needle decompression is typically a large-bore catheter, usually between 14 and 16 gauge. The larger bore allows for rapid decompression of the pleural space. While smaller needles *might* be used, the larger bore is preferred for quicker and more effective release of trapped air.
Q 5. Describe the procedure for performing needle decompression, step-by-step.
Needle decompression is a rapid procedure that should be performed quickly and efficiently in a life-threatening situation. The steps are as follows:
- Identify the landmarks: Locate the second intercostal space in the mid-clavicular line of the affected side.
- Prepare the skin: Cleanse the area with an antiseptic solution.
- Insert the needle: Insert the large-bore needle (14-16 gauge) superiorly, angled slightly towards the head, directed into the pleural space. Avoid directing the needle inferiorly to reduce the risk of injuring the intercostal vessels and nerves. The needle should be inserted quickly and decisively.
- Confirm proper placement: Listen for the escape of air (a hissing sound) and observe for the escape of air bubbles.
- Monitor the patient: Continuously monitor the patient’s respiratory status and vital signs after needle insertion.
- Prepare for chest tube insertion: Needle decompression is temporary. Arrange for immediate chest tube insertion.
The entire procedure should be carried out swiftly and efficiently in an emergency setting, keeping in mind that this is a temporary, life-saving maneuver and not a definitive treatment.
Q 6. What are the potential complications of needle decompression?
While needle decompression is a life-saving procedure, potential complications exist and should be kept in mind:
- Bleeding: Injury to intercostal vessels is possible.
- Pneumothorax worsening: Improper needle placement can worsen the pneumothorax.
- Lung injury: Direct lung puncture can occur.
- Infection: Risk of infection at the puncture site.
- Subcutaneous emphysema: Air leakage into the subcutaneous tissues.
These risks highlight the importance of proper training, precise technique, and close monitoring of the patient before, during, and after the procedure.
Q 7. How do you confirm successful needle decompression?
Confirmation of successful needle decompression involves several methods. Immediate improvement in the patient’s clinical status is the most important indicator, along with:
- Auscultation: Improved or return of breath sounds on the affected side suggests relief of pressure.
- Observation of air escape: Hearing or visually seeing air escaping from the needle insertion site confirms the release of trapped air.
- Reduction of respiratory distress: The patient’s breathing should become less labored.
- Improvement in vital signs: Blood pressure, heart rate, and oxygen saturation should improve.
These combined observations provide a strong indication of successful decompression, although definitive confirmation often comes after a chest x-ray following chest tube insertion.
Q 8. How do you manage a patient after needle decompression?
Post-needle decompression management focuses on stabilizing the patient and addressing the underlying cause of the pneumothorax. Immediate priorities include monitoring vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) closely for signs of recurrent respiratory distress. The patient’s oxygen saturation should be maintained at or above 95% using supplemental oxygen. The insertion site should be monitored for bleeding or signs of infection. A chest x-ray is crucial to confirm successful decompression and rule out any residual pneumothorax or complications. Further management depends on the underlying cause and the patient’s overall condition. This might involve admission for observation, further diagnostic tests (like a CT scan), or definitive treatment like a chest tube insertion if the pneumothorax recurs or doesn’t fully resolve with needle decompression.
For instance, a patient who experienced a pneumothorax due to a rib fracture might require pain management and close observation for several hours, while someone with a spontaneous pneumothorax may only need monitoring before discharge, provided their condition remains stable.
Q 9. What are the differences between needle decompression and chest tube insertion?
Needle decompression and chest tube insertion are both procedures used to treat a tension pneumothorax, but they differ significantly in their invasiveness and long-term management. Needle decompression is a rapid, life-saving intervention performed at the point of care to immediately relieve pressure. It involves inserting a large-bore needle into the pleural space to allow air to escape. It’s a temporary measure, often providing immediate relief but not definitively treating the underlying cause. Think of it as a quick fix, buying time for definitive treatment.
Chest tube insertion, on the other hand, is a more invasive procedure performed in a controlled setting (typically an operating room or emergency department) that involves inserting a chest tube into the pleural space connected to a drainage system. The chest tube drains air and fluid continuously and remains in place until the lung re-expands completely. It’s the definitive treatment for most pneumothoraces. Consider it like a thorough repair after the quick fix of needle decompression.
Essentially, needle decompression is a bridge to definitive care, while chest tube insertion is the long-term solution.
Q 10. Describe the equipment needed for needle decompression.
The equipment needed for needle decompression is minimal but crucial for ensuring a safe and effective procedure. It typically includes:
- A large-bore (14–16 gauge) catheter needle – this is critical for rapid decompression. Smaller needles are ineffective.
- Sterile gloves and appropriate personal protective equipment (PPE)
- Antiseptic solution (e.g., chlorhexidine or povidone-iodine) for skin preparation.
- Sterile dressing materials.
- Local anesthetic (optional, but recommended to reduce patient discomfort).
- Syringe (to potentially aspirate air, though this isn’t the primary goal).
- Adhesive tape or other securement device (to keep the needle in place, though removal is often immediate).
It’s critical to ensure all equipment is sterile to minimize the risk of infection. The procedure is performed rapidly, and speed is paramount in this potentially life-threatening situation.
Q 11. What are the signs and symptoms of a tension pneumothorax?
Tension pneumothorax is a life-threatening condition where air enters the pleural space but cannot escape, leading to a progressive increase in pressure. This pressure compromises cardiopulmonary function. The signs and symptoms are often dramatic and can include:
- Severe shortness of breath (dyspnea)
- Chest pain
- Hypotension (low blood pressure)
- Tachycardia (rapid heart rate)
- Distended neck veins (jugular venous distension)
- Tracheal deviation (the trachea, or windpipe, shifts away from the affected side)
- Absent or diminished breath sounds on the affected side
- Cyanosis (bluish discoloration of the skin and mucous membranes) due to hypoxia.
The key is the progressive nature of these symptoms, leading to rapid deterioration if untreated. A delay in diagnosis and treatment can be fatal.
Q 12. How do you differentiate a tension pneumothorax from other respiratory emergencies?
Differentiating a tension pneumothorax from other respiratory emergencies requires a careful clinical assessment. While other conditions like pulmonary embolism, cardiac tamponade, and severe asthma can present with similar symptoms (like shortness of breath and chest pain), several key features distinguish a tension pneumothorax:
- Progressive hemodynamic instability: Hypotension and tachycardia worsen rapidly in a tension pneumothorax.
- Tracheal deviation: The shift of the trachea away from the affected lung is a hallmark sign, rarely seen in other emergencies.
- Absent or markedly diminished breath sounds: This is due to the collapsed lung.
- Distended neck veins: Due to compromised venous return to the heart.
A high index of suspicion is crucial, particularly in trauma patients or those with underlying lung disease. Prompt assessment and imaging (chest x-ray) is crucial to confirm the diagnosis and guide treatment.
Q 13. What is the role of ultrasound in needle decompression?
Ultrasound plays an increasingly important role in the rapid diagnosis and management of tension pneumothorax. Lung ultrasound can quickly identify the presence of a pneumothorax by visualizing the characteristic ‘lung point’ – the edge of the collapsed lung – and assess its size and extent. This is particularly helpful in situations where a chest x-ray is unavailable or delayed. Real-time ultrasound guidance can significantly enhance the accuracy and safety of needle decompression. The sonographer can guide the needle directly into the pleural space, minimizing the risk of injuring other structures like blood vessels or nerves. It allows for confirmation of successful decompression by visualization of lung re-expansion.
In the hands of a skilled clinician, bedside ultrasound can be a crucial tool for early detection and definitive management, improving patient outcomes.
Q 14. Discuss the importance of sterile technique during needle decompression.
Strict adherence to sterile technique during needle decompression is paramount to prevent infection. The pleural space is normally sterile, and introducing bacteria can lead to serious complications like empyema (pus in the pleural space), which can be life-threatening. This requires meticulous attention to detail throughout the procedure. This starts with proper hand hygiene, followed by meticulous preparation of the skin at the insertion site using an antiseptic solution. All equipment must be sterile and handled aseptically. Gloves should be worn, and appropriate PPE, including eye protection, should be used if there’s a chance of splashing body fluids. Post-procedure, a sterile dressing is applied to the insertion site to minimize the risk of infection. If a subsequent chest tube is placed, similar sterile techniques are followed.
The focus is on maintaining a sterile field throughout the entire procedure to prevent any potential complications.
Q 15. How do you assess the effectiveness of needle decompression?
Assessing the effectiveness of needle decompression hinges on observing immediate clinical improvement in the patient’s respiratory status. We look for several key indicators.
- Improved respiratory rate and effort: A decrease in the respiratory rate, and less labored breathing are strong positive signs.
- Increased breath sounds: Auscultation (listening with a stethoscope) should reveal improved or clearer breath sounds on the affected side, indicating re-expansion of the lung.
- Resolution of cyanosis (bluish discoloration of the skin): Improved oxygenation, a direct result of lung re-expansion, will alleviate cyanosis.
- Increased SpO2 (oxygen saturation): A rise in SpO2 levels, typically measured with a pulse oximeter, shows improved oxygen uptake.
- Relief of chest pain: Many patients experience significant pain relief as the pressure on the lung subsides.
It’s crucial to remember that needle decompression is a temporary measure. Sustained improvement requires definitive management, usually with a chest tube.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the limitations of needle decompression?
Needle decompression, while a life-saving procedure, has limitations. It’s not a substitute for definitive chest tube placement, and its effectiveness depends heavily on the nature and extent of the pneumothorax (collapsed lung).
- Inability to remove large amounts of air: The needle’s small bore limits its ability to evacuate significant volumes of air. A large pneumothorax may not be adequately addressed by needle decompression alone.
- Risk of re-expansion pulmonary edema: Rapid re-expansion of a lung that’s been collapsed for a prolonged period can lead to pulmonary edema (fluid build-up in the lungs), a potentially serious complication.
- Potential for bleeding or lung injury: While rare, the procedure carries a small risk of injuring blood vessels or lung tissue.
- Not suitable for all types of pneumothorax: It’s less effective for tension pneumothorax when the air pressure inside the chest cavity is extremely high and compromises circulation.
- Temporary solution: Needle decompression only provides temporary relief; it doesn’t address the underlying cause of the pneumothorax.
Understanding these limitations is critical for making informed decisions about patient management.
Q 17. When should you consider converting needle decompression to a chest tube?
The decision to convert needle decompression to a chest tube is based on several factors. It’s not a rigid set of rules but rather a clinical judgment call.
- Persistent or recurrent pneumothorax: If the lung continues to collapse after needle decompression, or if air leaks back into the pleural space, a chest tube is necessary for ongoing drainage.
- Hemodynamic instability: If the patient shows signs of shock or circulatory compromise, a chest tube is needed for definitive management.
- Large or tension pneumothorax: Needle decompression is rarely sufficient for large pneumothoraces or tension pneumothoraces; chest tube insertion is the preferred method.
- Inability to adequately decompress with needle: If the needle decompression doesn’t provide sufficient relief of symptoms, a chest tube is necessary to fully drain the air and allow lung re-expansion.
- Presence of other injuries: If the patient has multiple injuries requiring intensive care, a chest tube provides more reliable and sustained management.
In essence, if needle decompression fails to provide sustained improvement or if the clinical situation worsens, immediate conversion to chest tube placement is warranted.
Q 18. How do you handle unexpected complications during needle decompression?
Unexpected complications during needle decompression are rare but require immediate attention. The key is to remain calm, assess the situation quickly, and take appropriate actions.
- Pneumothorax worsening: If the patient’s condition deteriorates after needle decompression, immediately cease the procedure, assess for tension pneumothorax, and prepare for chest tube insertion.
- Bleeding: Apply direct pressure to the insertion site. If bleeding is significant, consider surgical intervention.
- Lung injury: Monitor the patient closely for signs of respiratory distress or hemoptysis (coughing up blood). Supportive care and imaging may be necessary.
- Needle breakage: If the needle breaks, attempt retrieval if possible; otherwise, consult a surgeon for removal.
- Air embolism: This is extremely rare, but if suspected, immediately support the patient’s circulation and consider hyperbaric oxygen therapy.
A systematic approach, teamwork, and rapid access to advanced resources are paramount in managing unexpected complications.
Q 19. What are the legal and ethical considerations surrounding needle decompression?
Legal and ethical considerations surrounding needle decompression are centered on informed consent, proper technique, and documentation.
- Informed Consent: Patients (or their surrogates) must be fully informed about the procedure, including its benefits, risks, and alternatives. This must be documented thoroughly.
- Appropriate Indications: Needle decompression should only be performed when clinically indicated and by appropriately trained personnel. Improper use could lead to legal repercussions.
- Documentation: Detailed records, including patient assessment, procedure details, and the patient’s response, are essential for legal protection and quality improvement.
- Adherence to Standards: Following established guidelines and protocols minimizes risks and reduces the chance of legal complications.
- Competence: Only personnel with sufficient training and skills should perform needle decompression.
Careful attention to these aspects safeguards both the patient and the healthcare provider.
Q 20. Describe your experience with needle decompression in different clinical settings.
I have extensive experience with needle decompression in diverse clinical settings, including emergency departments, trauma bays, and pre-hospital care. In the emergency department, I’ve managed numerous cases of traumatic and spontaneous pneumothoraces, often under high-pressure situations. In the trauma bay, I’ve performed needle decompression as part of a multidisciplinary resuscitation effort for critically injured patients. My pre-hospital experience involved providing rapid needle decompression in remote locations, emphasizing resourcefulness and decision-making in challenging environments. Each setting demanded adaptation of techniques and resource management according to available resources and the patient’s condition.
One memorable instance involved a young motorcyclist with a tension pneumothorax at a remote accident site. Quickly performing needle decompression, while coordinating with paramedics for transport, proved vital in stabilizing him and preventing cardiorespiratory collapse before definitive care was available.
Q 21. How do you document the needle decompression procedure?
Thorough documentation of the needle decompression procedure is crucial. The documentation should follow a standardized format and include:
- Patient identification: Full name, date of birth, medical record number.
- Time and location: Precise time of the procedure and location (e.g., emergency department, trauma bay).
- Clinical indication: Reason for performing needle decompression (e.g., traumatic pneumothorax, spontaneous pneumothorax).
- Pre-procedure assessment: Vital signs, respiratory status, and physical examination findings.
- Procedure details: Site of needle insertion (e.g., 2nd intercostal space, midclavicular line), needle size, and amount of air aspirated.
- Post-procedure assessment: Changes in vital signs, respiratory status, and pain levels after the procedure.
- Disposition: Plan for further management (e.g., chest tube insertion, admission to hospital).
- Physician’s signature and credentials: Documentation must be signed by the physician who performed the procedure.
Detailed, accurate documentation protects both the patient and the healthcare provider. It serves as a crucial record for legal, quality improvement, and research purposes.
Q 22. What is your understanding of the pathophysiology of a tension pneumothorax?
A tension pneumothorax occurs when air enters the pleural space, the area between the lung and the chest wall, under pressure. This pressure builds up, collapsing the lung and compressing the heart and great vessels. Imagine a balloon inflated inside a rigid container; as more air is pumped in, the pressure increases, restricting the balloon’s expansion and potentially causing it to burst. Similarly, the increased pressure in the pleural space impairs venous return to the heart, leading to decreased cardiac output and potentially circulatory collapse. The pathophysiology involves a disruption in the integrity of the visceral pleura (the lining of the lung) or the parietal pleura (the lining of the chest wall), allowing air to enter the pleural space. This air can originate from a penetrating injury (like a stab wound) or a spontaneous rupture of a bleb or cyst in the lung. The resulting positive pressure prevents lung expansion, leading to hypoxemia (low blood oxygen) and potentially circulatory shock.
Q 23. How do you prioritize patients needing needle decompression in a busy emergency setting?
Prioritizing patients in a busy emergency setting needing needle decompression requires rapid assessment using a systematic approach. The ABCDEs of resuscitation are critical. Airway patency is paramount, followed by Breathing. Patients exhibiting signs of tension pneumothorax – such as severe respiratory distress, tracheal deviation, absent breath sounds on the affected side, and profound hypotension – take immediate priority. We use a simple triage system: patients with absent breath sounds on one side, hypotension, and altered mental status are immediately prioritized over those with less severe symptoms. Using a combination of clinical examination and pulse oximetry helps quickly identify patients who are critically compromised and require immediate intervention. Time is of the essence in these cases; even a few minutes of delay can be life-threatening.
Q 24. What are the different types of pneumothoraces and how do they affect your approach to decompression?
Pneumothoraces are categorized into several types, significantly influencing the approach to decompression. A tension pneumothorax, as discussed, requires immediate needle decompression due to the life-threatening nature of the increased intrathoracic pressure. A simple pneumothorax involves air in the pleural space but without significant pressure build-up. These patients may be managed conservatively with observation or small-bore chest tube placement depending on the size and the patient’s clinical status. A traumatic pneumothorax results from injury, often requiring aggressive management due to associated injuries. A spontaneous pneumothorax arises without apparent trauma, and treatment can range from observation to chest tube placement depending on the size and the patient’s clinical state. My approach to decompression is guided by the type of pneumothorax; tension pneumothoraces require immediate needle decompression, while others may be managed with less urgent interventions. The size of the pneumothorax, assessed via chest x-ray, further informs the treatment choice.
Q 25. Describe your experience with different needle decompression techniques.
I have extensive experience with various needle decompression techniques. The most common technique involves inserting a 14-16 gauge catheter over a needle into the second intercostal space in the mid-clavicular line on the affected side. This avoids the underlying neurovascular bundle. I’ve used this technique countless times with success. We utilize different needle sizes depending on the size and nature of the pneumothorax; smaller gauge needles may be employed for smaller pneumothoraces to minimize complications. In cases where a patient is in extremis, and immediate decompression is necessary, a larger-gauge needle may be considered. Critical to all techniques is rapid confirmation of the release of air with auscultation and immediate chest radiograph following the procedure. Thorough patient monitoring is vital during and after the procedure.
Q 26. Discuss the role of continuous monitoring after needle decompression.
Continuous monitoring after needle decompression is crucial to ensure its effectiveness and detect any potential complications. This includes close observation of the patient’s respiratory rate, oxygen saturation, blood pressure, and heart rate. Auscultation of lung sounds is repeated to assess the relief of tension. Pulse oximetry monitors oxygenation, and ongoing electrocardiography is beneficial to track cardiac rhythm. Any signs of persistent respiratory distress or hemodynamic instability warrant immediate attention. The placement of a chest tube is the definitive treatment and will often be performed following needle decompression. This allows for complete evacuation of the air from the pleural space and allows for continuous monitoring of pressure. Following needle decompression, a chest X-ray is taken to ascertain the presence of the pneumothorax.
Q 27. What post-procedure care instructions do you give the patient?
Post-procedure care instructions are tailored to the individual patient’s condition, but generally include advising patients to remain calm, monitor for any recurrence of symptoms (shortness of breath, chest pain), avoid strenuous activity, follow up with their physician as instructed (and often promptly for chest tube placement), and continue any prescribed medications. Patients are educated on the importance of recognizing signs of worsening respiratory distress and seeking immediate medical attention if such symptoms arise. Specific details regarding wound care and pain management are also discussed. Emphasis is placed on the importance of attending follow-up appointments to assess the healing process and ensure complete lung re-expansion.
Q 28. How do you stay current with the best practices in needle decompression?
Staying current with best practices in needle decompression is an ongoing process. I actively participate in continuing medical education courses and workshops focusing on trauma and critical care. I regularly review relevant medical literature, including peer-reviewed journals and guidelines published by organizations such as the American College of Surgeons and the American Heart Association. Membership in professional organizations allows access to the latest research and updates on best practices. Furthermore, participation in case reviews and discussions with colleagues enhances my understanding of current methodologies, allowing for continuous improvement of my skills and knowledge in this critical life-saving procedure.
Key Topics to Learn for Needle Decompression Interview
- Anatomy and Physiology: Thorough understanding of relevant anatomical structures and physiological processes affected by needle decompression procedures.
- Indications and Contraindications: Mastering the criteria for selecting appropriate candidates and identifying situations where the procedure is unsuitable.
- Procedure Techniques: Detailed knowledge of different needle decompression techniques, including variations and nuances in their application.
- Instrumentation and Equipment: Familiarity with the tools and technologies used in needle decompression procedures, including their proper handling and maintenance.
- Complications and Management: Understanding potential complications, their early recognition, and effective management strategies.
- Pre- and Post-operative Care: Comprehensive knowledge of patient preparation, monitoring, and post-procedure recovery protocols.
- Patient Assessment and Monitoring: Proficiency in evaluating patient status before, during, and after the procedure, utilizing relevant diagnostic tools and interpreting data.
- Ethical Considerations: Awareness of the ethical implications and decision-making processes involved in needle decompression.
- Case Studies and Problem-Solving: Ability to analyze case studies, identify challenges, and propose effective solutions based on best practices.
- Research and Current Trends: Keeping abreast of the latest research, advancements, and evolving best practices in needle decompression techniques.
Next Steps
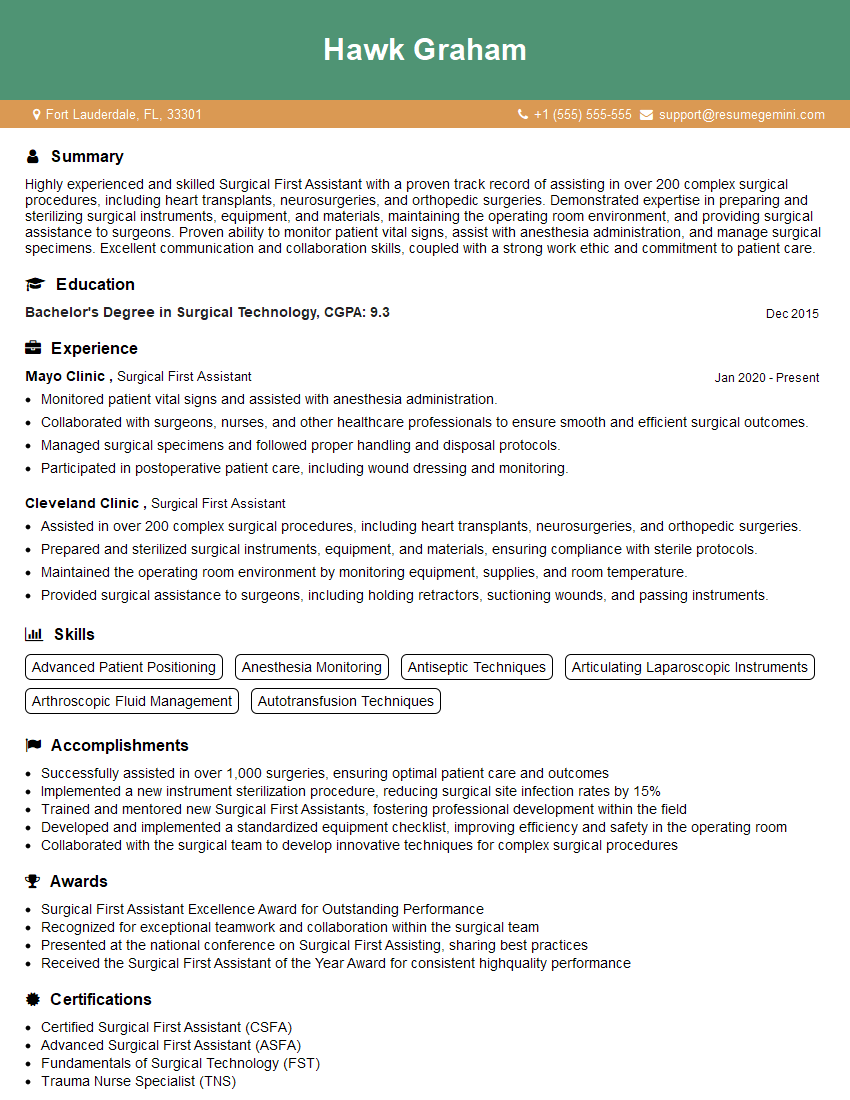
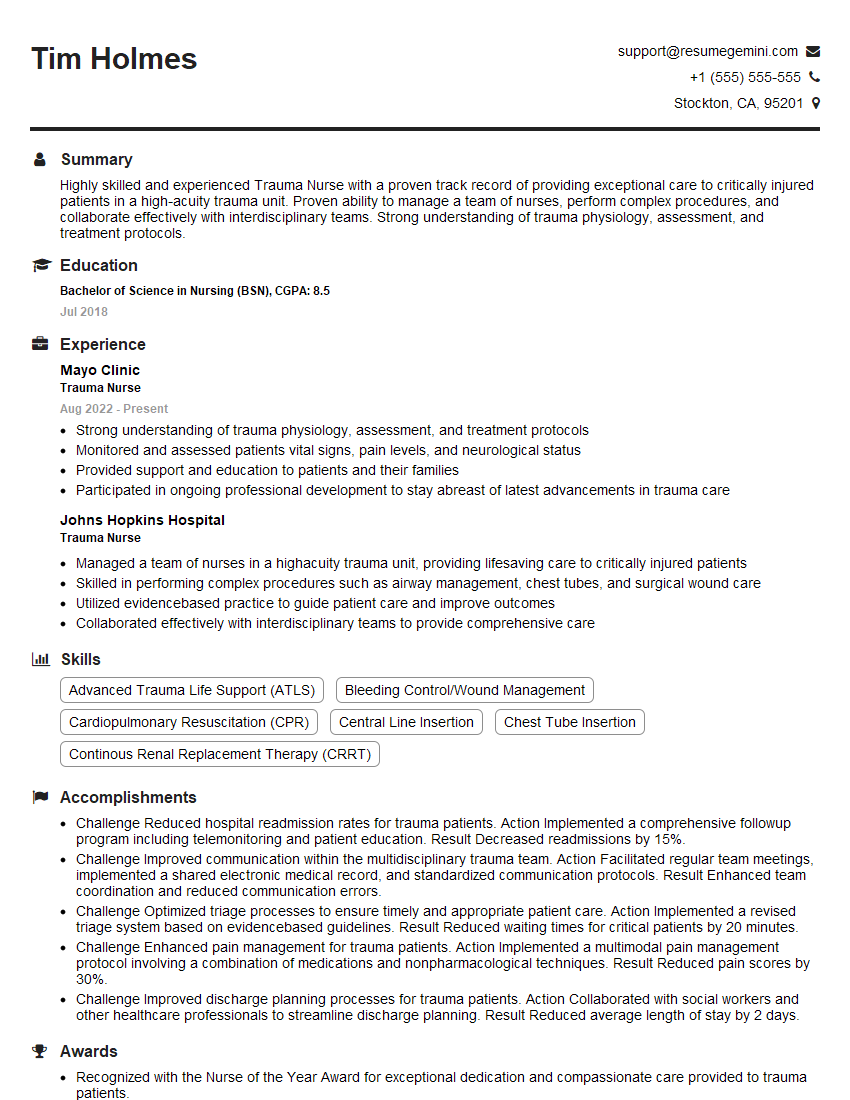
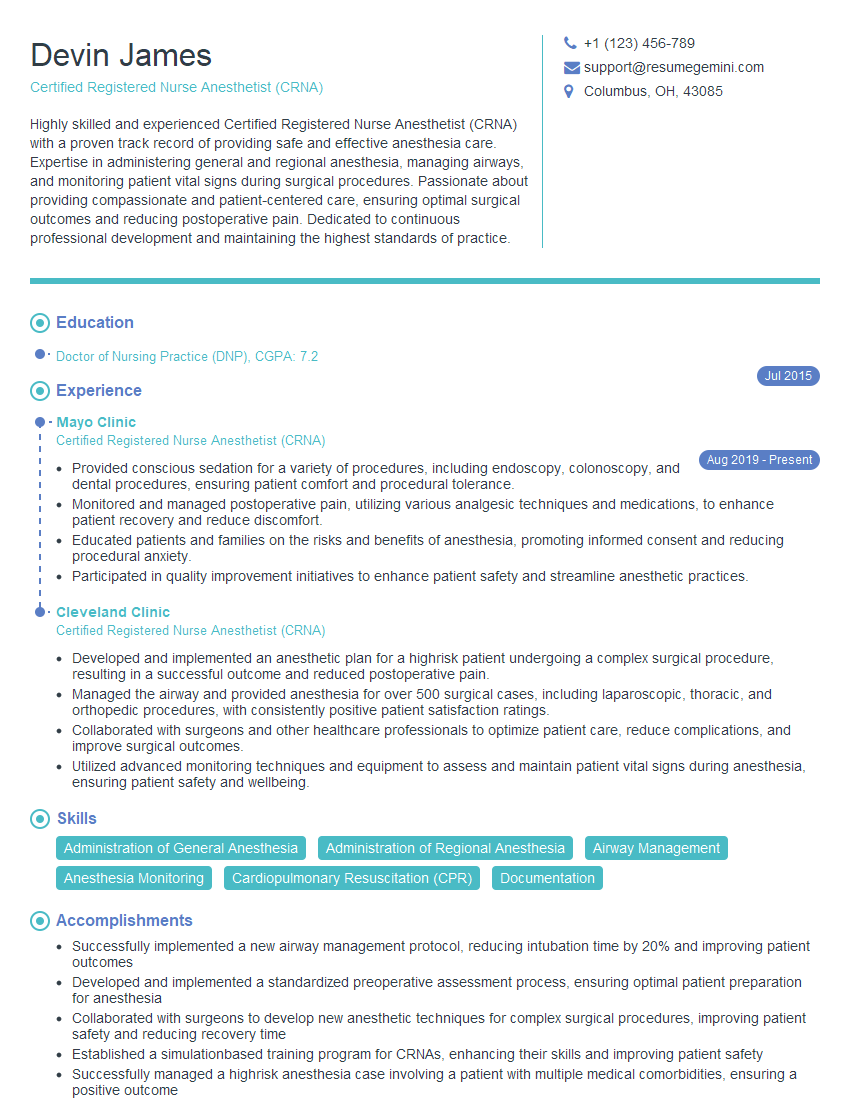
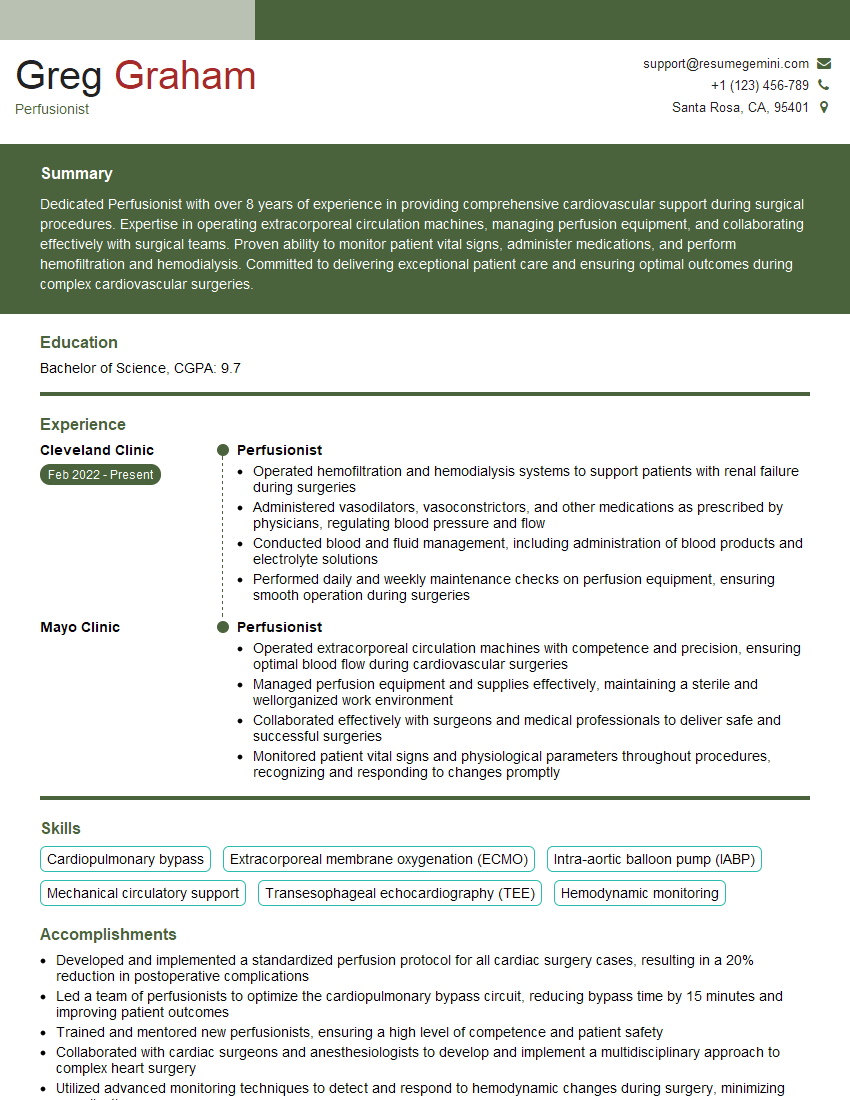
Mastering needle decompression techniques opens doors to exciting career opportunities in a specialized and in-demand field. To maximize your job prospects, it’s crucial to present your skills and experience effectively. Creating an ATS-friendly resume is key to getting your application noticed by recruiters. ResumeGemini can help you build a powerful, professional resume that showcases your expertise in needle decompression. Examples of resumes tailored to this specialization are available to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good