The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Animal Health and Disease Control interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Animal Health and Disease Control Interview
Q 1. Describe the pathogenesis of bovine tuberculosis.
Bovine tuberculosis (TB), caused by Mycobacterium bovis, is a chronic infectious disease primarily affecting cattle but also impacting other mammals. Its pathogenesis is complex and involves several stages.
Initial Infection: After inhalation or ingestion of M. bovis, the bacteria are initially phagocytosed by alveolar macrophages in the lungs or by cells within the gut. However, M. bovis is adept at surviving and multiplying within these macrophages, preventing their destruction. This leads to the formation of early lesions called granulomas.
Granuloma Formation: These granulomas are characteristic of TB and consist of a central core of infected macrophages surrounded by a wall of lymphocytes and other immune cells. The granulomas contain caseous (cheesy) material, which is composed of dead cells and bacteria. The size and number of granulomas vary depending on the immune response and the bacterial load.
Dissemination: From the primary infection site, M. bovis can spread via the lymphatic system to regional lymph nodes and then through the bloodstream to other organs, such as the liver, spleen, and kidneys. This dissemination often results in secondary lesions and further granuloma formation.
Clinical Disease: The clinical signs of bovine TB are varied and may include weight loss, reduced milk production, coughing, and lymph node enlargement. The severity of clinical disease depends on the extent of bacterial dissemination and the host’s immune response. Some animals remain sub-clinically infected, shedding the bacteria without showing overt symptoms.
Example: A farmer might notice a cow with enlarged lymph nodes and reduced milk yield, prompting suspicion of TB. Further investigation, including diagnostic tests, would be needed to confirm the diagnosis.
Q 2. Explain the different types of animal vaccines and their mechanisms of action.
Animal vaccines are biological preparations that stimulate an immune response against specific infectious agents, protecting the animal from subsequent disease. Different types exist, categorized by their composition and mechanism of action:
- Live-attenuated vaccines: These vaccines contain weakened (attenuated) forms of the pathogen. They elicit a strong and long-lasting immune response as the pathogen replicates in the host, mimicking a natural infection but without causing serious illness. Examples include modified-live vaccines for canine parvovirus and feline panleukopenia.
- Inactivated vaccines: These vaccines use killed pathogens. They are generally safer than live-attenuated vaccines, as they cannot cause disease, but they usually require multiple doses and may produce a less robust or shorter-lived immune response. Examples include rabies vaccines.
- Subunit vaccines: These vaccines use specific components of the pathogen, such as proteins or polysaccharides, rather than the whole pathogen. They are highly safe but often require adjuvants (substances that enhance the immune response) to be effective. Examples include some vaccines against bovine respiratory syncytial virus.
- Recombinant vaccines: These are produced using recombinant DNA technology. A gene encoding an immunogenic protein from the pathogen is inserted into a vector (e.g., another virus or bacteria), which is then used to produce the vaccine. This allows for precise control over the antigens produced and enhances safety. Examples include some vaccines against avian influenza.
- DNA vaccines: These vaccines introduce DNA encoding pathogen antigens directly into the animal’s cells. The cells then produce the antigens, triggering an immune response. They are still under development for many animal diseases but hold promise for their ease of production and ability to induce both humoral and cell-mediated immunity.
The mechanisms of action involve the stimulation of both humoral (antibody-mediated) and cell-mediated immunity. Humoral immunity involves the production of antibodies that neutralize the pathogen, while cell-mediated immunity involves the activation of cytotoxic T cells that kill infected cells.
Q 3. What are the key biosecurity measures to prevent the spread of avian influenza?
Avian influenza (AI), or bird flu, poses a significant threat to poultry and can have implications for human health. Robust biosecurity measures are crucial for prevention:
- Quarantine and Isolation: New birds should be quarantined for a period before introduction to the flock. This isolates them from existing birds, reducing the risk of disease transmission.
- Hygiene and Sanitation: Regular and thorough cleaning and disinfection of poultry houses, equipment, and vehicles are essential. Appropriate disinfectants should be used, focusing on areas prone to contamination like water sources and feeders.
- Rodent and Wild Bird Control: Rodents and wild birds can act as reservoirs of AI viruses. Implementing measures to exclude them from poultry farms is essential.
- Biosecurity Personnel: People entering the farm should follow strict hygiene protocols. This includes changing clothes and footwear, and hand sanitization before and after interaction with poultry. Footwear disinfection is particularly important.
- Visitor Control: Restricting access to the farm to essential personnel minimizes the risk of introducing the virus.
- Waste Management: Proper disposal of poultry manure and other waste products is essential to prevent the spread of the virus into the environment.
- Vehicle and Equipment Sanitation: Any vehicles or equipment entering the farm should be thoroughly cleaned and disinfected. Dedicated equipment and vehicles for each farm help avoid cross-contamination.
- Surveillance and Monitoring: Regular surveillance of the flock for signs of AI is vital for early detection and response.
Example: A farm implementing strict biosecurity protocols may designate specific entry and exit points, equip these with foot dips and hand sanitizing stations, and meticulously clean and disinfect all surfaces daily. This layered approach greatly minimizes the risk of an AI outbreak.
Q 4. How would you diagnose and treat parvovirus in a canine patient?
Canine parvovirus (CPV) is a highly contagious viral disease affecting dogs. Diagnosis and treatment are crucial for survival.
Diagnosis: CPV is diagnosed through a combination of clinical signs and laboratory tests.
- Clinical Signs: These include lethargy, vomiting, diarrhea (often bloody), dehydration, and fever. Severe cases can lead to death.
- Laboratory Tests: The most common diagnostic test is an ELISA (enzyme-linked immunosorbent assay) test on a fecal sample, which detects the presence of CPV antigens. A complete blood count (CBC) and serum biochemistry profile are used to assess the severity of dehydration and organ damage.
Treatment: Treatment is supportive and focuses on managing the clinical signs and preventing complications.
- Fluid Therapy: Intravenous (IV) fluid therapy is crucial to correct dehydration, which is a major threat in CPV.
- Anti-emetic Medications: Drugs to reduce vomiting (anti-emetics) are used to reduce the severity of the vomiting.
- Antibiotics: Antibiotics may be prescribed to prevent secondary bacterial infections, which are common in dogs with CPV due to immune suppression.
- Nutritional Support: Once the vomiting and diarrhea subside, careful reintroduction of food is vital. Often, bland diets are offered initially.
- Monitoring: Close monitoring of the patient’s hydration status, vital signs, and overall clinical condition is crucial to determine the need for adjusting the treatment strategy.
Example: A veterinarian diagnosing CPV would perform a fecal ELISA to confirm the diagnosis, run blood work, and initiate IV fluid therapy, anti-emetic medication, and supportive care. The severity of the case would determine the length and intensity of treatment.
Q 5. Outline the steps involved in a disease outbreak investigation on a farm.
Investigating a disease outbreak on a farm requires a systematic approach:
- Preliminary Investigation: This involves confirming the existence of an outbreak, defining the affected population, and collecting initial data on the disease’s characteristics (e.g., symptoms, mortality rate). This step might include interviews with farm personnel and preliminary observations.
- Case Definition: A clear case definition is crucial for identifying affected animals consistently. This involves specifying the diagnostic criteria and the timeframe for inclusion.
- Data Collection: Detailed data are collected on the affected animals, including their age, breed, sex, and any relevant history. This also involves collecting epidemiological data, such as the number of affected animals, the incubation period, and the pattern of disease spread.
- Hypothesis Formulation: Based on the collected data, several hypotheses regarding the outbreak’s cause are formulated. This involves considering potential infectious agents, environmental risk factors, and management practices.
- Laboratory Testing: Samples from affected animals are sent for laboratory analysis to identify the causative agent. This might involve bacteriological, virological, or parasitological tests.
- Data Analysis: Collected data are analyzed to test the hypotheses and identify risk factors associated with the outbreak. Statistical methods are useful for this.
- Control Measures: Based on the findings, appropriate control measures are implemented to prevent the further spread of disease. This might include quarantine, vaccination, treatment, and culling.
- Report Writing and Follow-up: A detailed report summarizing the investigation and its findings is written, providing recommendations for preventing future outbreaks. Follow-up monitoring is essential to assess the effectiveness of control measures.
Example: An outbreak of salmonellosis on a poultry farm would require detailed case definitions (clinical signs, diagnostic test results), investigation into feed sources, water sanitation, and biosecurity protocols. Laboratory analysis would confirm the presence of Salmonella, and appropriate control measures would be implemented, including disinfection and potentially antibiotic treatment for affected birds.
Q 6. What are the zoonotic diseases of concern in your region?
(This answer requires specifying a region. I will provide a general example using a temperate North American region.)
In a temperate North American region, zoonotic diseases of concern include:
- Rabies: A viral disease transmitted through the saliva of infected animals (e.g., raccoons, skunks, bats). Transmission to humans typically occurs through bites.
- Lyme Disease: A bacterial disease transmitted through the bite of infected blacklegged ticks. Symptoms include fever, rash, and joint pain.
- West Nile Virus: A viral disease transmitted to humans through the bite of infected mosquitoes. Symptoms can range from mild fever to severe neurological illness.
- Q Fever: A bacterial disease transmitted through contact with infected animals or their products (e.g., milk, meat). Symptoms can include fever, fatigue, and pneumonia.
- Brucellosis: A bacterial disease transmitted through contact with infected animals or their products. It can cause debilitating symptoms in humans.
These diseases highlight the interconnectedness of human and animal health. Effective surveillance and prevention strategies, including animal vaccination and public health education, are crucial to minimize zoonotic transmission risk.
Q 7. Explain the concept of herd immunity and its relevance in animal health.
Herd immunity refers to the indirect protection from an infectious disease conferred upon susceptible individuals within a population due to a sufficiently high proportion of immune individuals. Imagine a population of animals like a flock of sheep. If a significant portion of the sheep are vaccinated or have recovered from the disease, they are immune. This reduces the chances of the disease spreading through the entire population even if some sheep are susceptible. This is because the virus or bacteria has difficulty finding a susceptible host to infect.
Relevance in Animal Health: Herd immunity is highly relevant in preventing and controlling the spread of infectious diseases in livestock and companion animals. A high vaccination rate within a herd reduces the probability of outbreaks and minimizes the economic impact of disease. It’s particularly important for diseases where complete eradication is not feasible.
Practical Application: Herd immunity is achieved through vaccination programs, often mandated by government regulations for certain diseases (e.g., brucellosis, foot-and-mouth disease). The required percentage of immune animals for effective herd immunity varies depending on the disease’s characteristics and the herd’s size and structure. Factors such as contact rates between animals, the duration of immunity, and the virulence of the pathogen will affect the threshold for herd immunity.
Example: A high vaccination rate against bovine viral diarrhea (BVD) in a cattle herd can prevent significant economic losses due to abortions and reduced productivity, even if some animals remain unvaccinated. The immunity of the vaccinated animals prevents widespread transmission and protects the vulnerable animals.
Q 8. Describe the role of diagnostic testing in animal disease control.
Diagnostic testing is the cornerstone of effective animal disease control. It allows us to identify the presence, nature, and extent of disease in individual animals or populations. Accurate diagnosis is crucial for implementing targeted interventions, preventing outbreaks, and protecting animal welfare and public health.
This involves a range of techniques, from simple clinical examinations (like observing symptoms and taking temperature) to sophisticated laboratory tests. For example, we might use serological tests to detect antibodies against specific pathogens, PCR (polymerase chain reaction) to detect the genetic material of viruses or bacteria, or microbiological culture to isolate and identify microorganisms. The choice of test depends on the suspected disease, the available resources, and the urgency of the situation. Imagine a dairy farm experiencing a sudden drop in milk production: diagnostic testing might reveal mastitis, allowing for prompt treatment and prevention of further spread.
Beyond individual animals, diagnostic testing is essential for surveillance and monitoring disease prevalence within a population. This enables early detection of emerging diseases and facilitates targeted control measures. Think of national avian influenza surveillance programs; regular testing of poultry flocks helps to quickly identify and contain outbreaks, minimizing economic and public health impacts.
Q 9. What are the ethical considerations in euthanasia of animals?
Euthanasia in animals raises complex ethical considerations. The primary ethical principle is to minimize suffering and ensure a humane death. This means employing methods that are swift, painless, and cause minimal distress to the animal. The choice of method depends on factors like the species, size, and condition of the animal, as well as the availability of trained personnel and equipment.
- Minimizing Distress: The process should be conducted in a calm and controlled environment, with the animal handled gently and respectfully. Prior sedation can help reduce anxiety.
- Appropriate Method Selection: Different methods, such as intravenous barbiturate overdose or captive bolt stunning, have varying levels of acceptability and suitability, depending on the situation. The method chosen should be the most appropriate for the specific circumstances, minimizing pain and distress.
- Competence and Training: Euthanasia should only be performed by trained and qualified personnel who are competent to use the selected method effectively and humanely.
- Legal and Regulatory Compliance: Many jurisdictions have regulations and guidelines regarding the humane euthanasia of animals. These must be strictly adhered to. Furthermore, there must be a clear and justifiable reason for the euthanasia.
Ultimately, the ethical justification for euthanasia is a careful balancing of minimizing suffering and preserving animal welfare with other considerations, such as public health and safety.
Q 10. How do you handle animal cruelty cases?
Handling animal cruelty cases requires a systematic and compassionate approach. It’s crucial to act swiftly and effectively to ensure the immediate safety and well-being of the affected animals. The process usually involves the following steps:
- Assessment and Evidence Gathering: This involves documenting the situation comprehensively, taking photos and videos as evidence, and collecting any relevant information, such as witness statements or veterinary reports.
- Animal Seizure and Care: If necessary, animals are seized to remove them from the harmful environment and provide emergency veterinary care. Temporary housing is arranged for safekeeping.
- Investigation: A thorough investigation is undertaken to ascertain the facts, identify the perpetrator, and gather evidence to support legal action.
- Legal Action: Depending on the severity and jurisdiction, legal action may be taken against the perpetrator. Charges can include animal cruelty, neglect, or abuse.
- Rehabilitation and Rehoming: After the legal process, abused animals may require rehabilitation before being rehomed. Efforts are made to find them appropriate and safe new homes.
The handling of animal cruelty cases often requires collaboration among various agencies, including animal welfare organizations, law enforcement, and veterinary professionals. This collaboration is vital in ensuring effective investigation, prosecution, and rehabilitation.
Q 11. Explain different methods of animal restraint.
Animal restraint is vital for safe and effective handling during examinations, treatments, and procedures. The method chosen should always prioritize the animal’s safety and well-being, minimizing stress and injury. Different restraint techniques are used depending on the species, size, temperament, and procedure. Here are a few common methods:
- Physical Restraint: This involves manually holding or securing the animal using various techniques. For example, a large dog might be restrained by multiple handlers, while a cat might be gently wrapped in a towel.
- Chemical Restraint: This involves using sedatives or tranquilizers to calm and immobilize the animal. This is particularly helpful with aggressive or agitated animals.
- Mechanical Restraint: This uses equipment, such as leads, halters, or specialized crates, to confine the animal and prevent movement. Examples include stocks for cattle and head catches for sheep.
- Environmental Restraint: This utilizes the animal’s natural behavior to minimize stress. Creating a quiet and secure environment, and using positive reinforcement techniques, can reduce the need for physical restraint.
It’s essential to choose the least stressful and most effective restraint method for each situation, considering the individual animal’s needs and the procedure to be performed. Improper restraint can cause injury or increase the risk of aggressive behavior. Proper training is crucial for anyone involved in animal handling.
Q 12. Describe the lifecycle of a common parasitic worm affecting livestock.
Let’s take Haemonchus contortus, the barber’s pole worm, a common parasitic nematode affecting livestock, particularly sheep and goats. Its lifecycle is a good example of the complexity of parasitic infections.
- Egg Stage: The life cycle begins when infected animals pass eggs in their feces. These eggs are microscopic and require favorable conditions (moisture, temperature) to develop.
- Larval Stages (L1-L3): Within the egg, a larva develops. After hatching, the larva undergoes several molts (L1, L2, L3) in the environment. The L3 stage is infective.
- Infection: Animals become infected by ingesting infective L3 larvae while grazing on contaminated pasture. The larvae penetrate the intestinal wall.
- Immature Adult Stage: Larvae mature into adult worms within the animal’s abomasum (the fourth stomach compartment in ruminants).
- Adult Stage: Adult worms feed on the host’s blood, causing anemia and other health problems. They reproduce, producing more eggs that are passed in the feces, continuing the cycle.
Understanding this lifecycle is critical for effective control. Strategies such as pasture rotation, anthelmintic treatment (drenching), and improved grazing management can interrupt the parasite’s life cycle and reduce infection rates.
Q 13. What are the common causes of mastitis in dairy cows?
Mastitis, an inflammation of the mammary gland, is a major problem in dairy cows, significantly impacting milk production and animal welfare. Several factors contribute:
- Bacterial Infection: This is the most common cause. Bacteria such as Staphylococcus aureus, Escherichia coli, and Streptococcus agalactiae are frequently implicated. Infection can occur through the teat canal during milking or through skin abrasions.
- Environmental Factors: Poor hygiene during milking, damp and muddy conditions, and inadequate ventilation in the barn all increase the risk of infection.
- Teat Injuries: Teat injuries caused by rough handling during milking or by physical trauma can create entry points for bacteria.
- Genetic Predisposition: Some cows have a greater susceptibility to mastitis due to genetic factors that influence udder conformation and immune response.
- Milking Management Practices: Inefficient milking procedures, including incomplete milk removal and insufficient teat disinfection, can facilitate bacterial growth and infection.
Control strategies focus on improving hygiene, proper milking techniques, timely treatment of infected animals, and selective breeding for mastitis resistance.
Q 14. How do you differentiate between viral and bacterial infections in animals?
Differentiating between viral and bacterial infections in animals requires a multifaceted approach combining clinical observation with laboratory diagnostics. While symptoms can sometimes overlap, key differences exist:
- Clinical Signs: Viral infections often present with more systemic symptoms, like fever, lethargy, and generalized weakness, while bacterial infections may exhibit more localized signs such as abscesses, pneumonia, or diarrhea.
- Duration and Course of Disease: Viral infections tend to be more acute, often resolving more quickly, while bacterial infections can be either acute or chronic, sometimes persisting for longer periods.
- Laboratory Diagnostics: This is essential for definitive diagnosis. Viral infections are typically diagnosed using PCR, ELISA (enzyme-linked immunosorbent assay), or virus isolation techniques. Bacterial infections are identified by microbiological culture, Gram staining, and sensitivity testing.
- Response to Treatment: Antiviral medications are generally less effective than antibiotics against bacterial infections. A positive response to antibiotics is highly suggestive of a bacterial infection.
However, some diseases are co-infections with both bacteria and viruses which complicate diagnostic processes. A complete clinical picture and several diagnostic tests are needed for accurate identification. For example, a respiratory disease in a cat might present with coughing, fever, and lethargy. Further investigation using tests such as PCR for feline viral rhinotracheitis virus and bacterial culture might reveal the cause to be a co-infection of both.
Q 15. What are the symptoms and treatment of rabies?
Rabies is a deadly viral disease affecting the central nervous system, primarily transmitted through the saliva of infected animals, most commonly through a bite. Symptoms can vary depending on the incubation period and the animal species but generally progress through three stages.
- Prodromal stage: This initial stage may involve non-specific symptoms like fever, headache, malaise, and unusual fatigue. The animal may also exhibit behavioral changes such as restlessness or unusual aggression.
- Excitation stage: This phase is characterized by increased excitability, aggression, excessive salivation (often described as ‘foaming at the mouth’), and fear of water (hydrophobia). Animals may bite at anything in their path.
- Paralytic stage: In this final, often fatal stage, the animal experiences paralysis, progressing from the site of the bite to the whole body. Coma and death usually follow.
Unfortunately, there is no cure for rabies once clinical signs develop. Treatment focuses on supportive care to manage symptoms and prevent secondary infections. Post-exposure prophylaxis (PEP) is crucial for individuals bitten by a potentially rabid animal and involves a series of rabies vaccine injections and rabies immunoglobulin administration. PEP is highly effective in preventing the disease if administered promptly.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe different methods of animal identification.
Animal identification is crucial for traceability, disease control, and managing animal populations. Several methods exist, each with its advantages and disadvantages.
- Microchipping: A small, passive transponder is injected under the skin, containing a unique identification number. It requires a scanner to read the chip. This is commonly used in companion animals and is considered a permanent identification method.
- Tattooing: A permanent ink tattoo is applied to the skin, usually on the inner ear or inner thigh. Although visible, it can be difficult to read if the tattoo fades or the animal is heavily pigmented.
- Branding: A hot iron is used to create a mark on the animal’s skin. This method is less common due to animal welfare concerns and the potential for scarring.
- Ear Tagging: Plastic or metal tags, bearing identification numbers, are attached to the animal’s ears. These can be lost or damaged.
- Electronic Identification (EID): More sophisticated than microchipping, EID systems involve RFID (radio-frequency identification) tags that can be read remotely. These are increasingly used in livestock management and disease tracking.
The choice of identification method depends on the animal species, the purpose of identification, and practical considerations like cost and ease of application.
Q 17. Explain the importance of quarantine in disease prevention.
Quarantine is a crucial tool in preventing the spread of infectious diseases. It involves isolating animals suspected of carrying or exposed to a contagious disease to prevent transmission to healthy animals or humans. The duration of quarantine varies greatly depending on the specific disease and its incubation period.
Imagine a situation where a new livestock shipment arrives with symptoms suggestive of a highly contagious disease. Implementing quarantine immediately prevents potential widespread infection by isolating the suspected animals and preventing their interaction with other animals. This buys time for diagnosis and treatment while preventing the spread into the herd. Similarly, quarantining pets newly adopted from shelters ensures they are not carrying any diseases before being introduced to other animals in a home.
Effective quarantine requires careful monitoring, stringent hygiene protocols, and appropriate biosecurity measures to prevent the entry and exit of disease vectors.
Q 18. Discuss the role of antimicrobial stewardship in animal health.
Antimicrobial stewardship (AMS) in animal health is a coordinated program to promote the appropriate use of antimicrobials (antibiotics, antivirals, antifungals, and antiparasitics), maximizing their effectiveness and minimizing the development of antimicrobial resistance (AMR).
AMR is a significant threat to both animal and human health. The overuse or misuse of antimicrobials in animals leads to the selection and proliferation of resistant bacteria, making infections harder to treat. AMS programs focus on several key areas:
- Diagnosis before treatment: Prioritizing laboratory tests to confirm infections before prescribing antimicrobials.
- Targeted antimicrobial selection: Using the most appropriate drug for a specific infection based on antibiotic sensitivity testing.
- Appropriate dosage and duration: Ensuring correct administration of antimicrobials to achieve effective treatment while limiting potential side effects and AMR development.
- Vaccination and biosecurity: Emphasis on preventative measures to reduce the need for antimicrobials in the first place.
- Surveillance and monitoring: Tracking antimicrobial use and AMR patterns to identify areas for improvement.
Effective AMS requires collaboration between veterinarians, farmers, and regulatory authorities, emphasizing responsible antimicrobial use to preserve the efficacy of these vital drugs for future generations.
Q 19. What are the regulations surrounding the use of antibiotics in livestock?
Regulations surrounding the use of antibiotics in livestock vary widely depending on the country or region. However, there are common themes driven by the global concern over AMR.
Generally, regulations aim to:
- Restrict the use of critically important antimicrobials: These drugs are essential for treating human infections and their use in livestock is often severely limited or prohibited.
- Require veterinary oversight: Antibiotics in livestock should be prescribed by a veterinarian following a proper diagnosis, not given freely by farmers.
- Promote responsible use: Regulations often incorporate best practices guidelines for antibiotic administration and storage.
- Implement withdrawal periods: There is a period of time after administering antibiotics to livestock before meat or dairy products can be consumed to ensure no antibiotic residues remain.
- Monitor antimicrobial sales and use: Data collection is crucial for tracking trends and identifying potential problems.
Non-compliance can result in penalties, fines, and product recalls. The goal is to protect both animal and public health by minimizing the emergence and spread of AMR.
Q 20. Explain the One Health approach to disease control.
The One Health approach recognizes that human, animal, and environmental health are interconnected. Disease outbreaks often cross boundaries between these three domains, making a holistic approach vital for effective control.
For example, avian influenza (bird flu) can affect poultry, wild birds, and potentially humans. A One Health strategy would involve collaboration between veterinarians, human health professionals, wildlife biologists, and environmental agencies to monitor the spread of the virus in birds, protect poultry flocks, and educate the public on risk mitigation. This collaborative approach encompasses surveillance, prevention, preparedness, and response, utilizing combined expertise and resources for better outcomes.
By working together across disciplines, One Health enhances our ability to anticipate and address emerging health threats more effectively than a fragmented approach could achieve.
Q 21. Describe the challenges in controlling wildlife diseases.
Controlling wildlife diseases presents unique challenges compared to managing diseases in domestic animals or humans.
- Accessibility: Wildlife populations are often difficult to access and monitor, making surveillance and intervention challenging.
- Mobility: Wildlife can move freely across vast geographical areas, making it difficult to contain disease outbreaks.
- Biodiversity: Different wildlife species can act as reservoirs or vectors for various diseases, creating complex epidemiological patterns.
- Ethical and logistical limitations: Intervention methods are limited by ethical concerns about animal welfare and practical difficulties in administering treatments or vaccines to wild populations.
- Disease surveillance: Detecting and monitoring disease in wildlife often relies on passive surveillance methods such as post-mortem examinations of carcasses or observing clinical signs in affected animals, which can be unreliable.
Strategies often involve a combination of surveillance, vaccination of select populations (where feasible), habitat management to reduce disease transmission, and public health education to limit human-wildlife interaction and potential transmission.
Q 22. How would you manage a situation where a potentially rabid animal bites a person?
Managing a potential rabies exposure requires immediate and decisive action. Rabies is a fatal zoonotic disease, meaning it can spread from animals to humans. The first step is to thoroughly wash the wound with soap and water for at least 15 minutes. This helps remove any potential virus particles. Then, seek immediate medical attention. The individual should contact their doctor or a public health official immediately. They will likely receive post-exposure prophylaxis (PEP), which involves a series of rabies vaccine shots and possibly rabies immune globulin. This treatment is highly effective in preventing the disease if administered promptly.
Meanwhile, the animal involved, if possible, should be captured and observed for signs of rabies (such as changes in behavior, aggression, paralysis, or excessive salivation). If the animal is deceased, its head should be submitted to a laboratory for rabies testing. This helps confirm the diagnosis and provides crucial information for public health officials to manage further potential exposures.
Imagine a scenario where a child is bitten by a stray dog. Immediate washing of the wound, followed by a trip to the emergency room for PEP, would be critical. The dog would ideally be captured and monitored, or its head sent for testing. This proactive approach minimizes the risk of the virus developing into a fatal disease.
Q 23. Discuss the role of vaccination programs in preventing disease outbreaks.
Vaccination programs are the cornerstone of preventative animal health. They work by stimulating the animal’s immune system to produce antibodies against specific diseases, providing protection against future infection. This herd immunity protects not only vaccinated individuals but also those who cannot be vaccinated (like very young or sick animals). Effective vaccination programs are crucial in preventing disease outbreaks and controlling their spread, reducing morbidity (illness) and mortality (death). For example, mass vaccination campaigns have effectively eradicated diseases like rinderpest (a devastating cattle disease) and are making significant progress against others, such as rabies.
Consider the impact of a successful canine rabies vaccination program. By vaccinating a significant portion of the dog population, the risk of rabies transmission to both dogs and humans is drastically reduced. This public health intervention protects human lives and saves significant economic resources associated with disease treatment and prevention. Successful vaccination programs hinge on factors like vaccine availability, cost-effectiveness, accessibility to veterinary services, public awareness and engagement, and robust surveillance systems to monitor vaccine efficacy and disease incidence.
Q 24. Explain the importance of record-keeping in animal health management.
Record-keeping is paramount in animal health management. It provides a comprehensive history of each animal, tracking health events, treatments, vaccinations, and other critical data. This information is crucial for making informed management decisions, monitoring the health status of individual animals and the herd/flock as a whole, and facilitating effective disease surveillance and control. Accurate records aid in identifying disease trends, implementing preventive strategies, and responding effectively to outbreaks. Moreover, detailed record-keeping is essential for complying with regulations, supporting disease traceability, and facilitating biosecurity measures.
Imagine a dairy farm maintaining detailed records of each cow’s milk production, health status, and reproductive cycles. These records allow the farmer to identify cows with low milk yields, early signs of disease, or reproductive problems, enabling timely interventions and improving overall herd productivity and profitability. Thorough record-keeping ensures traceability, preventing the spread of disease from an affected animal to the rest of the herd. In addition, farm management software, with features for tracking vaccination schedules, animal movements and treatments, greatly simplifies and improves the accuracy of record keeping.
Q 25. Describe different types of animal housing and their impact on animal health.
Animal housing significantly impacts animal health and welfare. Different housing systems cater to various animal species and production systems. For instance, intensive systems, such as battery cages for laying hens or indoor confinement for pigs, offer efficient production but may compromise animal welfare if not managed carefully. Extensive systems, like free-range poultry or pasture-raised livestock, provide animals with more space and opportunities for natural behaviors but may pose challenges in terms of disease control and biosecurity. Intermediate systems combine elements of both intensive and extensive systems, seeking to optimize both productivity and animal welfare.
The choice of housing system depends on several factors including the animal species, climate, available resources, and production goals. For example, pigs raised outdoors in a muddy environment are more susceptible to certain types of parasites and diseases. In contrast, well-managed indoor systems can minimize parasite exposure, offering better biosecurity and protecting the animals from adverse weather conditions. The key is finding the balance that promotes good animal health, welfare, and efficient production.
Q 26. How would you assess the nutritional needs of a group of animals?
Assessing the nutritional needs of a group of animals requires a multifaceted approach. Factors such as species, age, breed, sex, physiological status (e.g., pregnancy, lactation), and activity level all influence nutrient requirements. Nutritional needs are typically determined using published standards and guidelines or through nutrition modeling software. These provide recommendations for essential nutrients such as protein, carbohydrates, fats, vitamins, and minerals. A thorough assessment of the animals’ current diet is essential to identify any deficiencies or excesses. This may involve feed analysis, observation of animal behavior (e.g., appetite, body condition), and measurement of key physiological parameters (e.g., weight, blood values). Changes to the diet may be made gradually to minimize digestive upset.
Let’s say you are assessing the nutritional needs of dairy cows in peak lactation. You would consider their higher energy requirements due to milk production. Feed analysis would be crucial to ensure they receive enough protein, calcium, and phosphorus to support milk production and bone health. Regular monitoring of body condition scores, milk production, and blood parameters ensures that the feeding regime is meeting the animals’ needs and that adjustments are made as needed. Failure to meet nutritional needs can lead to reduced productivity, impaired immunity, and various health problems. Professional consultation with a veterinary nutritionist is highly recommended for such assessments.
Q 27. Explain the principles of biosecurity in a veterinary practice.
Biosecurity in a veterinary practice involves implementing procedures and protocols to minimize the risk of infectious disease transmission between animals, from animals to humans, and vice versa. This includes strict hygiene practices, such as handwashing and disinfection of equipment and surfaces. Implementing traffic control measures, like restricting access to the facility and using appropriate protective clothing (e.g., gowns, gloves, masks), is critical. Proper waste disposal procedures, segregation of animals by health status (e.g., isolating sick animals), and routine disinfection of premises are all key biosecurity elements. Effective biosecurity protocols should be tailored to the specific veterinary practice and the types of animals being treated.
For example, a veterinary clinic seeing multiple species would need strict cleaning and disinfection protocols between patients. Designated areas for different species would minimize cross-contamination. Separate clothing and footwear would be designated for staff working with different animal groups or entering high-risk areas. Implementing a strict vaccination policy for clinic staff against zoonotic diseases would also significantly enhance biosecurity. The cost-effectiveness of such measures is easily offset by reduced likelihood of outbreaks, decreased disease treatment costs and potentially improved patient outcomes.
Q 28. What are the current challenges facing animal health professionals?
Animal health professionals face numerous challenges in today’s world. The emergence and spread of antimicrobial resistance (AMR) is a major concern, limiting treatment options for bacterial infections. Climate change poses significant threats, impacting animal health through altered weather patterns and increased disease vector prevalence. Globalization and international trade increase the risk of introducing exotic diseases. The growing demand for animal products places pressure on animal welfare and intensifies the risk of disease outbreaks in intensive farming systems. Furthermore, limited resources and access to veterinary services in many parts of the world hinder disease prevention and control efforts. In addition, evolving public expectations regarding animal welfare, increasing complexity of regulatory frameworks and the need for better communication and collaboration with farmers, stakeholders and the public remain significant challenges.
Addressing AMR requires a multi-pronged approach, including responsible antibiotic use, improved hygiene and sanitation, and development of new antimicrobial agents and vaccines. Mitigating the impacts of climate change needs global collaboration and investment in sustainable agricultural practices. Strengthening biosecurity measures and improving surveillance systems are vital in preventing the introduction and spread of exotic diseases. Addressing these challenges requires a holistic approach involving collaboration among animal health professionals, policymakers, and the public.
Key Topics to Learn for Animal Health and Disease Control Interview
- Epidemiology and Surveillance: Understanding disease outbreaks, transmission dynamics, and implementing effective surveillance programs. Practical application: Analyzing disease data to identify trends and predict future outbreaks.
- Disease Diagnosis and Control: Mastering diagnostic techniques (clinical examination, laboratory tests), and implementing appropriate control measures (vaccination, biosecurity). Practical application: Developing and implementing a control plan for a specific disease in a given population.
- Animal Welfare and Biosecurity: Balancing animal health with ethical considerations and implementing robust biosecurity protocols to prevent disease introduction and spread. Practical application: Designing and implementing a biosecurity plan for a farm or veterinary clinic.
- Veterinary Public Health: Understanding the interface between animal and human health, including zoonotic diseases and food safety. Practical application: Assessing the risk of a zoonotic disease transmission and developing strategies for mitigation.
- Regulatory Frameworks and Policy: Familiarity with relevant regulations, guidelines, and policies related to animal health and disease control. Practical application: Interpreting and applying relevant legislation to specific scenarios.
- Data Analysis and Interpretation: Ability to collect, analyze, and interpret data related to disease prevalence, risk factors, and control program effectiveness. Practical application: Presenting findings from an epidemiological investigation to stakeholders.
- Communication and Collaboration: Effective communication with colleagues, farmers, and the public to promote animal health and disease control. Practical application: Explaining complex scientific information to a non-technical audience.
Next Steps
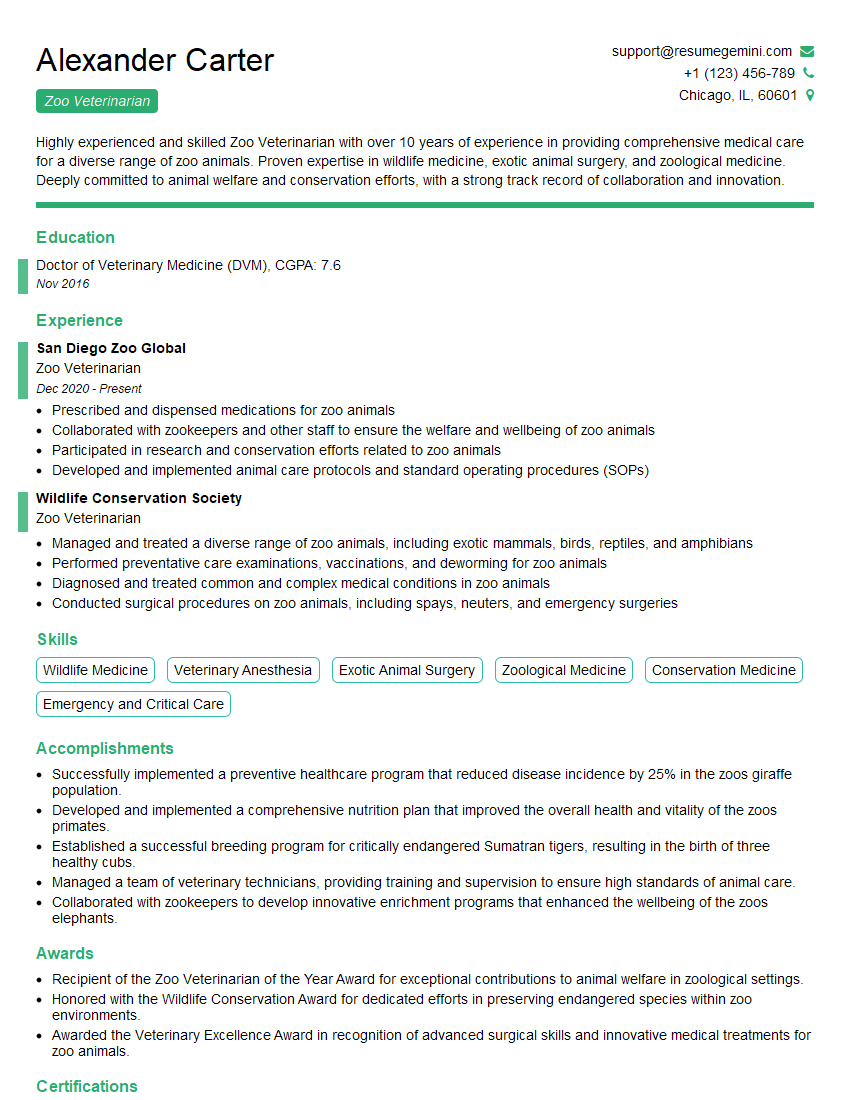
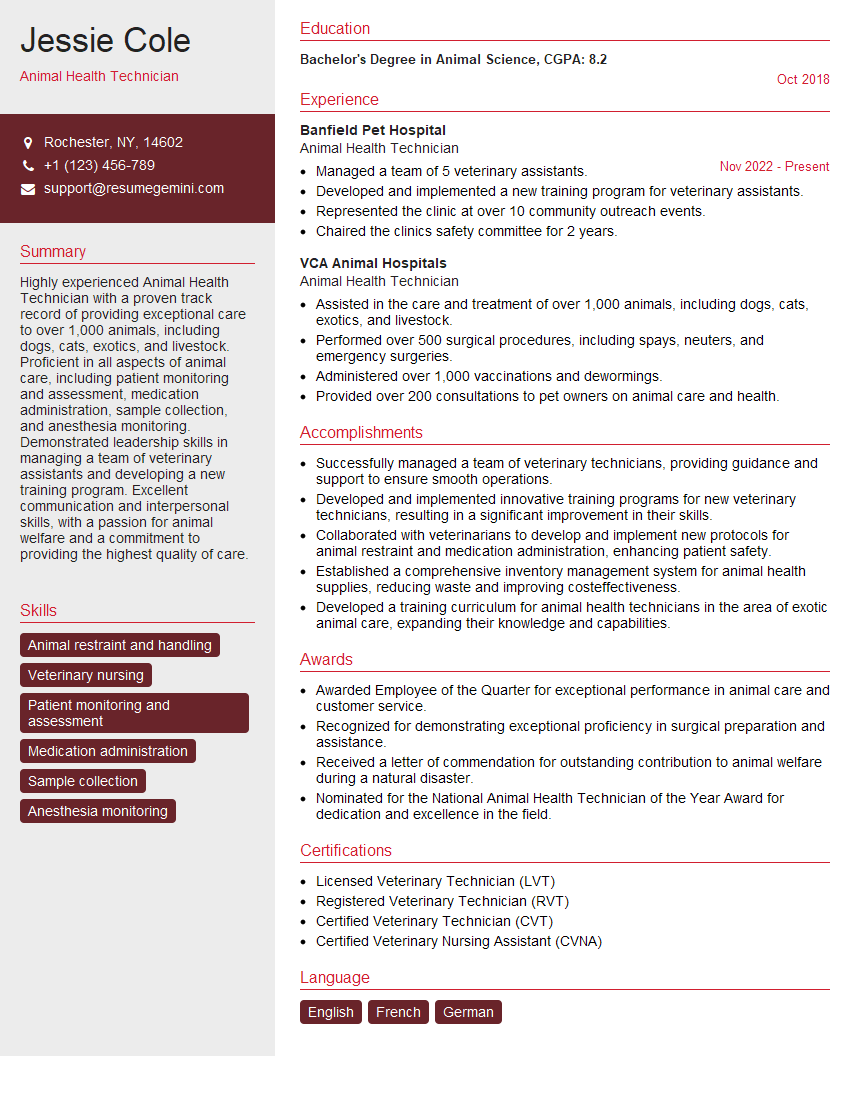
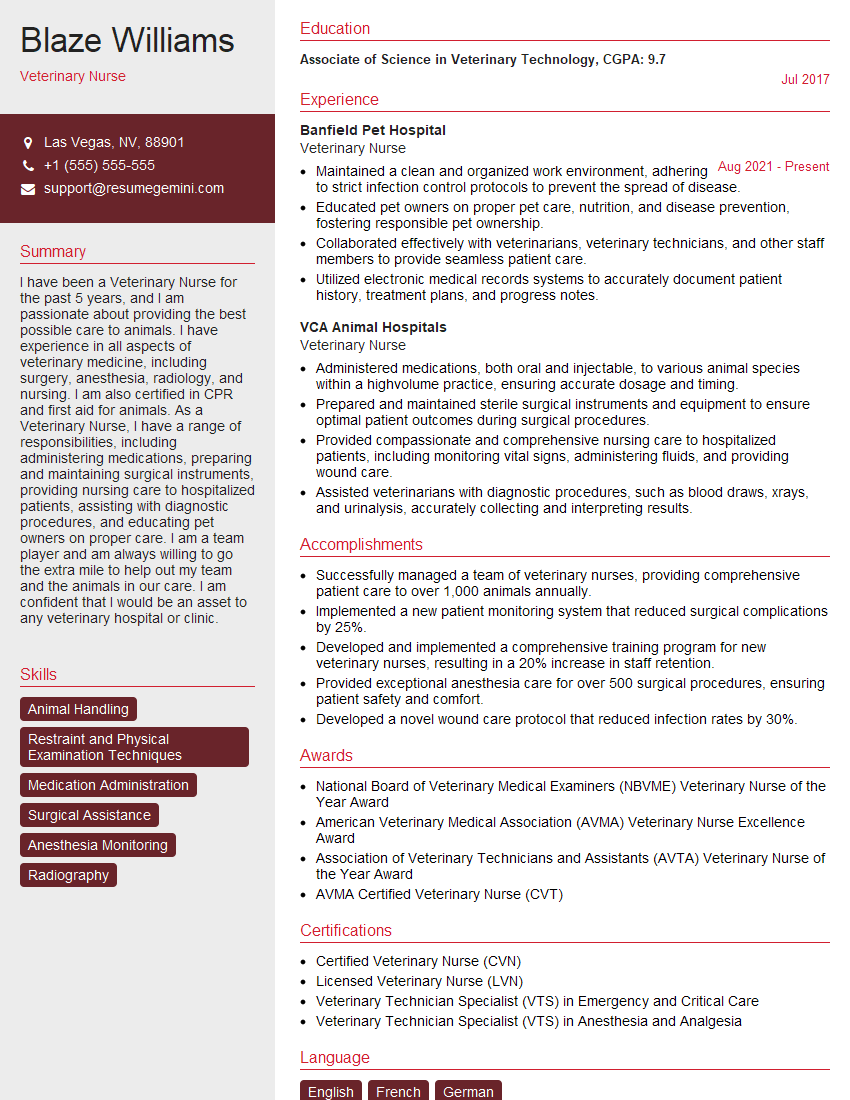
Mastering Animal Health and Disease Control opens doors to a rewarding career with significant impact on animal welfare and public health. To maximize your job prospects, creating a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional and effective resume tailored to highlight your skills and experience. ResumeGemini provides examples of resumes specifically designed for Animal Health and Disease Control professionals, guiding you through the process and ensuring your application stands out. Invest time in crafting a compelling resume; it’s your first impression and a vital step towards securing your dream role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good