Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Basic Trauma Care interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Basic Trauma Care Interview
Q 1. Describe the primary survey in trauma assessment.
The primary survey in trauma assessment is a rapid initial assessment designed to identify and manage immediately life-threatening injuries. It follows a systematic approach, prioritizing interventions based on the severity of the threat. Think of it as a quick triage to stabilize the patient before moving on to a more detailed examination. It’s crucial to remember that this survey is not meant to be exhaustive; it’s about identifying and addressing the most critical problems first.
The primary survey typically follows the mnemonic ABCDE (Airway, Breathing, Circulation, Disability, Exposure), which we’ll discuss in more detail in the next question. Each letter represents a critical area needing immediate attention.
In a real-world scenario, imagine a car accident victim. The first step would be to quickly assess their airway to make sure they can breathe. If there’s significant bleeding, that would be addressed next before checking for spinal injury, etc. The speed and efficiency are vital to saving lives.
Q 2. Explain the ABCDEs of trauma resuscitation.
The ABCDEs of trauma resuscitation are a systematic approach to managing life-threatening injuries. It’s a structured way of thinking, ensuring no critical issue is missed in the chaos of a trauma scene.
- A – Airway and Cervical Spine Control: This is always the first priority. Ensure a patent airway while simultaneously protecting the cervical spine. This often involves manual in-line stabilization of the head and neck. If the airway is compromised, immediate intervention such as opening the airway using the jaw thrust maneuver may be necessary.
- B – Breathing and Ventilation: Assess respiratory rate, rhythm, and depth. Look for signs of respiratory distress like increased work of breathing, use of accessory muscles, or cyanosis (blue discoloration of the skin). Treatment may involve supplemental oxygen, assisted ventilation with a bag-valve mask, or advanced airway management like endotracheal intubation.
- C – Circulation: Control any external bleeding using direct pressure and elevation. Assess heart rate, blood pressure, and capillary refill. Administer intravenous fluids as needed to maintain adequate blood pressure and perfusion.
- D – Disability (Neurological Status): Briefly assess neurological status using the Glasgow Coma Scale (GCS). This measures level of consciousness, eye opening, verbal response, and motor response. This helps gauge the severity of brain injury.
- E – Exposure and Environmental Control: Completely expose the patient to allow a thorough assessment of injuries, while simultaneously maintaining normothermia (normal body temperature). This might involve removing clothing and covering the patient with blankets to prevent hypothermia.
Remember, the ABCDEs are a guideline, and the order may need to be adjusted based on the specific situation. For instance, if there’s massive external hemorrhage, addressing circulation (C) might temporarily take precedence over a full neurological exam (D).
Q 3. What are the indications for a rapid sequence intubation?
Rapid Sequence Intubation (RSI) is a technique used to rapidly secure an airway in patients who are critically ill or injured and at risk of airway compromise or respiratory arrest. It’s crucial to remember that this is an advanced procedure requiring specialized training and should only be performed by qualified personnel.
Indications for RSI include:
- Loss of protective airway reflexes: Such as in cases of severe head injury or drug overdose.
- Inadequate oxygenation or ventilation: When supplemental oxygen is insufficient to maintain adequate oxygen levels.
- Risk of aspiration: When there’s a high likelihood that the patient might aspirate gastric contents into the lungs.
- Need for controlled ventilation: In situations where the patient requires mechanical ventilation.
- Suspected or confirmed upper airway obstruction: RSI may be necessary to bypass the obstruction.
For example, a patient with a severe head injury and depressed level of consciousness may require RSI to prevent aspiration and ensure adequate ventilation. The procedure involves a sedative and paralytic agent to facilitate intubation. It needs to be carried out in a skilled and timely manner by a trained medical professional.
Q 4. How do you manage a patient with a suspected cervical spine injury?
Managing a patient with a suspected cervical spine injury requires a high degree of caution and a systematic approach. The primary goal is to prevent further injury to the spinal cord.
The initial steps are:
- Stabilize the cervical spine: Manual in-line stabilization (MILs) should be provided by a trained individual before moving the patient. This involves carefully supporting the head and neck in a neutral position, preventing any movement.
- Use a cervical collar: Once MILs is in place, a cervical collar should be applied to provide additional support and reduce movement.
- Careful log rolling: If the patient needs to be moved, this should be done using a log roll technique, ensuring the head, neck, and spine remain in alignment.
- Assess neurologic status: Regularly assess the patient’s motor and sensory function in all four extremities. This helps track any changes in neurological status.
- Obtain imaging: Cervical spine imaging, usually X-rays and/or CT scans, is crucial to definitively rule out or identify fractures or dislocations.
Consider this analogy: think of the spine as a stack of delicate blocks. Any sudden or forceful movement can cause displacement and damage. Careful handling is paramount to preventing further harm.
Q 5. Describe your approach to controlling external hemorrhage.
Controlling external hemorrhage is a critical step in trauma management. Prompt and effective control can prevent significant blood loss and improve patient survival. The approach involves a combination of direct pressure, elevation, and pressure points.
The steps are:
- Direct pressure: Applying direct pressure to the bleeding wound using a clean dressing. This is the most effective initial method.
- Elevation: Elevating the bleeding extremity above the heart helps reduce blood flow to the area.
- Pressure points: If direct pressure isn’t controlling the bleeding, applying pressure to the major arteries proximal to the wound can be used. For example, pressure on the brachial artery in the arm or the femoral artery in the leg.
- Tourniquet: As a last resort, a tourniquet can be applied proximal to the bleeding site to completely stop blood flow. This is a life-saving technique, but should be used judiciously and only when other methods have failed. Improper application can lead to limb loss.
Example: In a severe leg laceration, the first action would be to apply direct pressure to the wound with a sterile dressing. If this isn’t effective, elevating the leg and applying pressure to the femoral artery might be necessary. Only as a last resort, and with appropriate training, would a tourniquet be considered.
Q 6. Explain the different types of shock and their management.
Shock is a life-threatening condition characterized by inadequate tissue perfusion. This means that not enough oxygenated blood is reaching the body’s organs. There are different types of shock, each with its own cause and management strategy.
- Hypovolemic Shock: Caused by blood loss (e.g., hemorrhage, severe dehydration). Management involves fluid resuscitation (IV fluids) and addressing the source of bleeding.
- Cardiogenic Shock: Caused by the heart’s inability to pump sufficient blood (e.g., heart attack, heart failure). Management involves medications to support heart function and possibly mechanical circulatory support.
- Obstructive Shock: Caused by obstruction of blood flow (e.g., tension pneumothorax, pericardial tamponade). Management focuses on removing the obstruction. For example, a tension pneumothorax requires needle decompression or chest tube insertion.
- Distributive Shock: Caused by widespread vasodilation, resulting in decreased peripheral resistance (e.g., septic shock, anaphylactic shock, neurogenic shock). Management involves addressing the underlying cause (e.g., antibiotics for sepsis, epinephrine for anaphylaxis) and providing supportive care.
The management of shock always begins with stabilizing the airway, breathing, and circulation (ABCs). Identifying the type of shock is crucial, as treatment strategies differ significantly.
Q 7. What are the signs and symptoms of a tension pneumothorax?
A tension pneumothorax is a life-threatening condition where air accumulates in the pleural space (the space between the lung and chest wall), causing the lung to collapse and compromising cardiovascular function. It’s a true medical emergency requiring immediate intervention.
Signs and symptoms include:
- Severe respiratory distress: Shortness of breath, rapid and shallow breathing.
- Hypotension: Low blood pressure due to decreased venous return to the heart.
- Tachycardia: Rapid heart rate as the body compensates for low blood pressure.
- Tracheal deviation: The trachea (windpipe) may be shifted away from the affected side.
- Absent breath sounds: On the affected side.
- Distended neck veins: Due to increased pressure in the chest.
- Subcutaneous emphysema: A crackling sensation under the skin.
Imagine a balloon inside a rigid container. Air leaking into the container puts pressure on the balloon, preventing it from expanding. Similarly, air in the pleural space compresses the lung and impairs its function. Immediate needle decompression or chest tube insertion is necessary to relieve the pressure and restore lung function. Delaying treatment can be fatal.
Q 8. How do you manage an open pneumothorax?
An open pneumothorax, or sucking chest wound, is a life-threatening condition where air enters the pleural space (the space between the lung and the chest wall) through an open wound in the chest. This disrupts the negative pressure within the pleural space, causing the lung to collapse.
Management involves several key steps:
- Immediate Seal: The priority is to seal the wound to prevent further air entry. This is typically done using an occlusive dressing, such as a petroleum gauze pad, taped on three sides. This allows air to escape but prevents air from entering. Imagine it like a one-way valve for your lung.
- Supplemental Oxygen: Administer high-flow oxygen to improve oxygenation. The collapsed lung reduces the amount of oxygen the patient can take in.
- Monitor Vital Signs: Closely monitor heart rate, respiratory rate, blood pressure, and oxygen saturation levels to assess the patient’s stability.
- Transport to Definitive Care: Rapid transport to a hospital is crucial for definitive management, which might include chest tube insertion to remove air and re-expand the lung.
Example: Imagine a construction worker struck by a falling beam, creating a large open wound in his chest. Immediate application of an occlusive dressing, along with high-flow oxygen, would be vital to stabilize him before transport to the emergency room.
Q 9. Describe the treatment for a flail chest.
A flail chest occurs when multiple ribs fracture in two or more places, creating a segment of the chest wall that moves paradoxically (in the opposite direction) during breathing. This paradoxical movement hinders effective ventilation.
Treatment focuses on supporting ventilation and oxygenation:
- Pain Management: Adequate pain control is essential, as pain restricts breathing. Opioids are often used.
- Oxygen Supplementation: High-flow oxygen is crucial to compensate for impaired ventilation.
- Positive Pressure Ventilation: In severe cases, positive pressure ventilation, either through a bag-valve mask or mechanical ventilator, may be necessary to maintain adequate oxygenation and reduce the work of breathing. Think of it as a temporary support system for the lungs.
- Surgical Intervention: In some instances, surgical stabilization of the flail segment might be required, particularly if the paradoxical movement severely compromises ventilation.
Example: A patient involved in a motor vehicle accident sustains multiple rib fractures resulting in a flail segment. This patient would likely receive pain medication, oxygen, and potentially require mechanical ventilation to support their breathing until surgery to stabilize the chest wall could be performed.
Q 10. What are the signs and symptoms of a cardiac tamponade?
Cardiac tamponade is a life-threatening condition where blood or fluid accumulates in the pericardial sac (the sac surrounding the heart), compressing the heart and impairing its ability to pump blood effectively.
Signs and symptoms typically include:
- Hypotension (low blood pressure): Due to reduced cardiac output.
- Tachycardia (rapid heart rate): The heart attempts to compensate for decreased blood flow.
- Distended Neck Veins (JVD): Increased pressure in the veins due to impaired venous return to the heart.
- Muffled Heart Sounds: Fluid in the pericardium dampens the sounds of the heartbeat.
- Pulsus Paradoxus: A significant decrease in systolic blood pressure during inspiration.
Example: A patient arrives in the emergency room following a stabbing injury to the chest with signs of hypotension, tachycardia, distended neck veins, and muffled heart sounds – highly suggestive of cardiac tamponade, which requires immediate intervention such as pericardiocentesis (needle aspiration of the fluid).
Q 11. How do you manage a patient with a penetrating chest wound?
Penetrating chest wounds can cause significant damage, including pneumothorax, hemothorax (blood in the pleural space), and cardiac injury.
Management involves:
- Airway Management: Secure the airway and provide supplemental oxygen.
- Control Bleeding: If there is significant external bleeding, apply direct pressure to the wound.
- Occlusive Dressing (if needed): For suspected pneumothorax, apply an occlusive dressing as described in the open pneumothorax management.
- Fluid Resuscitation: Administer intravenous fluids to maintain blood pressure.
- Monitor Vital Signs: Continuously monitor vital signs, including heart rate, blood pressure, and oxygen saturation.
- Rapid Transport: Prompt transport to a trauma center is crucial.
Example: A patient presents with a gunshot wound to the chest. First responders would control external bleeding, assess for and manage respiratory compromise (potential pneumothorax), establish intravenous access for fluid resuscitation, monitor vital signs diligently, and immediately transport to a hospital for further evaluation and management such as surgery to repair damaged tissues.
Q 12. Describe the management of a patient with an abdominal injury.
Abdominal injuries encompass a wide spectrum of severity, from minor contusions to life-threatening organ damage. Management depends greatly on the mechanism of injury and the patient’s presentation.
General principles include:
- Assessment: Careful assessment is crucial, including a focused physical exam and imaging studies (CT scan) to identify injuries.
- Fluid Resuscitation: Aggressive fluid resuscitation is crucial to maintain blood pressure and tissue perfusion. Loss of blood in abdominal injuries can be significant.
- Pain Management: Manage pain with analgesics.
- Surgical Intervention: Laparotomy (open abdominal surgery) or laparoscopy (minimally invasive surgery) may be necessary to repair damaged organs or control bleeding.
- Monitor for Complications: Close monitoring for complications such as peritonitis (infection of the abdominal cavity), bleeding, and organ failure.
Example: A patient involved in a high-speed motor vehicle accident presents with abdominal pain and tenderness. This patient will need a comprehensive assessment, including blood tests, imaging studies, and potentially laparotomy to explore for internal bleeding or organ damage.
Q 13. Explain the principles of fluid resuscitation in trauma.
Fluid resuscitation is a critical component of trauma management. Its goal is to restore and maintain adequate tissue perfusion (blood flow to the tissues) following blood and fluid loss.
Principles include:
- Early Resuscitation: Start early and aggressively to avoid hypovolemic shock (shock due to low blood volume).
- Crystalloid Solutions: Lactated Ringer’s solution or normal saline are commonly used as initial fluids. Think of these as replenishing the body’s fluid balance.
- Blood Products: Packed red blood cells, fresh frozen plasma, and platelets are administered to replace blood loss in significant hemorrhage.
- Monitoring Response: Closely monitor vital signs, urine output, and level of consciousness to assess the effectiveness of resuscitation. Urine output is a good indication of kidney perfusion.
- Avoid Over-Resuscitation: Excessive fluid administration can be detrimental. The goal is to restore adequate tissue perfusion, not to overfill the circulatory system.
Example: A trauma patient with significant blood loss from a femur fracture will receive rapid fluid administration with crystalloids initially, followed by blood products as needed to restore blood volume and maintain blood pressure and organ perfusion.
Q 14. What are the common complications of trauma?
Trauma can lead to a wide range of complications, both immediate and long-term.
Common complications include:
- Infection: Wound infections, pneumonia, and sepsis are frequent occurrences, especially with significant injuries.
- Hemorrhage: Continued bleeding can lead to hypovolemic shock.
- Acute Respiratory Distress Syndrome (ARDS): Severe lung injury leading to respiratory failure.
- Compartment Syndrome: Increased pressure within a confined muscle compartment, compromising blood supply.
- Multiple Organ Dysfunction Syndrome (MODS): Failure of multiple organ systems.
- Post-traumatic Stress Disorder (PTSD): A psychological disorder that can develop following a traumatic experience.
- Chronic Pain: Persistent pain resulting from nerve damage or muscle injury.
Example: A patient with a severe head injury may develop ARDS and require prolonged mechanical ventilation, while a patient with a crush injury could develop compartment syndrome requiring fasciotomy (surgical incision to relieve pressure).
Q 15. How do you assess for and manage hypothermia in a trauma patient?
Hypothermia, a dangerously low body temperature, is a significant threat in trauma patients, often exacerbated by blood loss, exposure, and the effects of injury itself. Assessment begins with checking the patient’s core temperature using a rectal thermometer for the most accurate reading. Look for signs and symptoms like shivering (initially), then apathy, confusion, slowed breathing and heart rate, and eventually loss of consciousness. Management focuses on preventing further heat loss and rewarming the patient gradually.
- Passive Rewarming: Removing wet clothing, applying blankets, and moving the patient to a warm environment are initial steps. This is crucial as rapid rewarming can lead to dangerous cardiac arrhythmias.
- Active Rewarming: For moderate to severe hypothermia, active measures might include warmed intravenous fluids, warmed humidified oxygen, and in some cases, extracorporeal rewarming techniques (like a heart-lung bypass machine) in a specialized setting.
Imagine a car accident victim on a cold night. Besides their injuries, the exposure to cold significantly compromises their physiological response to the trauma. The initial focus would be on preventing further heat loss with blankets and moving them inside an ambulance, before more active measures are considered.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your understanding of the Glasgow Coma Scale (GCS).
The Glasgow Coma Scale (GCS) is a neurological assessment tool used to objectively quantify a patient’s level of consciousness. It assesses three key areas: eye opening, verbal response, and motor response, each scored numerically. The scores are added to obtain a total GCS score ranging from 3 (deep coma) to 15 (fully alert). Lower scores indicate more severe neurological impairment.
- Eye Opening: Spontaneous (4), to speech (3), to pain (2), none (1).
- Verbal Response: Oriented (5), confused (4), inappropriate words (3), incomprehensible sounds (2), none (1).
- Motor Response: Obeys commands (6), localizes pain (5), withdraws from pain (4), flexion (decorticate) (3), extension (decerebrate) (2), none (1).
For example, a patient who opens their eyes to pain (2), speaks incomprehensible words (2), and flexes their limbs to pain (3) would have a GCS score of 7. This score indicates a severe impairment of consciousness, requiring immediate advanced neurological care.
Q 17. Explain the role of pain management in trauma care.
Pain management is paramount in trauma care. Uncontrolled pain can lead to increased stress response, hypertension, tachycardia, decreased oxygen saturation, and impaired respiratory function – all worsening the patient’s condition and hindering recovery. The goal is to provide analgesia (pain relief) as soon as possible, balancing the benefits against potential risks of the medication itself, including respiratory depression.
Effective pain management utilizes a multimodal approach, combining different analgesic methods: opioid analgesics for severe pain, non-opioid analgesics like NSAIDs (non-steroidal anti-inflammatory drugs) to reduce inflammation and pain, and regional anesthesia techniques like nerve blocks or epidurals for localized pain control. Regular pain reassessment is crucial. The use of a pain scale allows us to track the effectiveness of interventions and adjust treatment as needed.
Think about a patient with multiple fractures. The combination of opioid analgesics for the severe pain of the fractures coupled with NSAIDs to address swelling and inflammation, provides a more comprehensive and effective approach.
Q 18. How do you prioritize patients in a mass casualty incident?
Prioritizing patients in a mass casualty incident (MCI) is crucial to maximizing survival and resource allocation. The widely adopted system is START (Simple Triage and Rapid Treatment). It categorizes patients into four color-coded groups based on their immediate needs:
- Immediate (Red): Patients with life-threatening injuries requiring immediate attention, such as respiratory compromise, uncontrolled hemorrhage, or altered mental status.
- Delayed (Yellow): Patients with serious injuries that can be treated after the immediate cases, for instance, a stable fracture or moderate burns.
- Minor (Green): Patients with minor injuries who can wait for treatment, like small lacerations or minor abrasions.
- Expectant (Black): Patients with unsurvivable injuries who receive minimal care or palliative measures.
The process involves assessing respiration, perfusion (pulse and capillary refill), and mental status. This quick assessment helps to efficiently allocate resources to those most likely to benefit from immediate interventions.
Q 19. Describe your experience with different types of airway management.
Airway management is a cornerstone of trauma care. Securing a patent (open) airway is the first priority. Methods range from simple maneuvers to advanced techniques depending on the patient’s condition.
- Basic Airway Maneuvers: Head tilt-chin lift or jaw thrust (for suspected cervical spine injury) to open the airway are often the first steps. Suctioning of the oral and nasal cavities may be necessary.
- Adjunctive Airway Devices: Oropharyngeal and nasopharyngeal airways are used to maintain airway patency in unconscious patients without the need for intubation.
- Endotracheal Intubation: This involves inserting a tube into the trachea to allow for mechanical ventilation, primarily used for patients with significant respiratory compromise or impaired consciousness requiring ventilator support.
- Surgical Airways: Cricothyrotomy or tracheostomy are last-resort techniques used when endotracheal intubation is impossible.
I’ve personally utilized all methods, from simple head-tilt-chin lift in a conscious patient with mild airway obstruction to performing endotracheal intubation in a patient with severe head trauma and respiratory depression, highlighting the importance of adaptable skills in trauma management.
Q 20. What are the indications for blood transfusion in trauma?
Blood transfusion in trauma is indicated when significant blood loss has caused hypovolemic shock (low blood volume), threatening the patient’s survival. The decision to transfuse isn’t taken lightly. It’s guided by clinical assessment, including vital signs, ongoing bleeding, and laboratory results like hemoglobin and hematocrit levels. The goal is to restore adequate tissue perfusion and oxygen delivery.
Factors such as the patient’s age, comorbidities, and the presence of ongoing bleeding significantly influence the decision-making process. Massive transfusion protocols are often employed in cases of severe trauma with substantial blood loss, aiming to deliver balanced blood products (red blood cells, plasma, platelets) in a timely manner.
For instance, a patient with a penetrating chest injury, exhibiting signs of shock, would necessitate immediate blood transfusion along with efforts to control bleeding. Careful monitoring post-transfusion is vital to assess for adverse effects and ensure adequate oxygen-carrying capacity is maintained.
Q 21. Explain the importance of continuous monitoring in trauma patients.
Continuous monitoring in trauma patients is essential for early detection of complications and prompt intervention, greatly improving patient outcomes. This includes meticulous observation of vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation, temperature), along with neurological assessment (GCS, pupillary response) and ongoing monitoring of urine output and fluid balance.
Continuous cardiac monitoring detects arrhythmias and other cardiac complications that can arise from blood loss, hypothermia, or electrolyte imbalances. Pulse oximetry provides a real-time measure of oxygen saturation, revealing hypoxemia (low blood oxygen) that might not be immediately apparent. Intracranial pressure (ICP) monitoring may be necessary in patients with severe head injuries to guide appropriate therapy.
Imagine a patient with a severe pelvic fracture. Continuous monitoring allows us to detect early signs of internal bleeding reflected in a dropping blood pressure or increasing heart rate, enabling prompt intervention to prevent further deterioration and improve the chances of survival.
Q 22. How do you document your actions during a trauma event?
Accurate and meticulous documentation is paramount in trauma care. It’s not just about recording events; it’s about creating a comprehensive, legally defensible record that allows for effective treatment, communication, and potential future legal proceedings. My documentation process follows a structured approach, ensuring clarity and completeness.
- Timely Recording: I document findings immediately, or as soon as it’s feasible, ensuring accuracy while the events are fresh in my memory. I use military time (24-hour clock) for precision.
- Objective Observations: I focus on objective data – vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation), injuries observed, interventions performed, and patient responses. Subjective information, such as the patient’s reported pain level, is noted clearly as such. For example, instead of ‘The patient was in severe pain,’ I would write, ‘The patient reported pain at a 10/10 on the numeric pain scale.’
- Concise and Clear Language: I use clear, concise language, avoiding jargon unless absolutely necessary and defining any specialized terms used. Abbreviations are used sparingly and in accordance with institutional standards.
- Sequential Order: I maintain a chronological order of events, making it easy to follow the timeline of care. Each entry is dated and time-stamped.
- Signature and Credentials: All entries are signed and include my credentials (name and professional designation).
- Use of Standardized Forms: I use pre-printed forms whenever possible to ensure consistency and comprehensive data collection, such as trauma flow sheets. These often include sections for mechanism of injury, initial assessment, interventions, and ongoing monitoring.
For example, if I were to document a patient’s response to intravenous fluid administration, I would note: ’14:30 – 1000ml lactated Ringer’s solution administered IV. Patient’s blood pressure increased from 80/50 to 90/60 mmHg. Heart rate remained unchanged at 120 bpm.’
Q 23. Describe your experience with trauma patient transfer.
Trauma patient transfer requires a coordinated effort to ensure patient safety and the continuity of care. My experience encompasses various transfer scenarios, from inter-facility transfers to transferring patients to specialized units within the same hospital. The process always prioritizes maintaining hemodynamic stability and minimizing the risk of further injury.
- Pre-Transfer Assessment: Before any transfer, I perform a thorough assessment, ensuring that the patient’s condition is stable enough for transport. This includes reviewing vital signs, assessing the severity of injuries, and confirming appropriate pain management and respiratory support. For example, if a patient has an unstable cervical spine, appropriate immobilization must be in place before transfer.
- Communication: Clear and concise communication with the receiving facility is crucial. This includes providing a detailed handover report, including the patient’s history, current condition, treatment provided, and ongoing needs. This handover typically utilizes a standardized form and process like SBAR (Situation, Background, Assessment, Recommendation).
- Appropriate Equipment and Personnel: The transfer team must be adequately staffed and equipped for the patient’s specific needs. This may involve specialized transport vehicles, such as ambulances equipped with advanced life support (ALS) equipment, or even air ambulances for critical patients requiring rapid transport.
- Monitoring During Transport: Continuous monitoring of the patient’s vital signs and overall condition is essential throughout the transport. Any changes in condition require immediate attention and adjustments to the care plan.
- Post-Transfer Handover: Upon arrival at the receiving facility, a detailed handover of the patient and their care plan is crucial. This ensures continuity of treatment and avoids potential gaps in care.
For instance, I was once involved in the transfer of a patient with severe multiple trauma from a rural hospital to a level-1 trauma center. The pre-transfer assessment was crucial; we stabilized the patient’s airway and breathing and ensured proper pain management before transport via helicopter. We then maintained continuous monitoring during transport and gave a detailed verbal report to the trauma team upon arrival.
Q 24. What is your understanding of consent and ethical considerations in trauma care?
Consent and ethical considerations are fundamental to trauma care. Treating a patient without proper consent, except in emergencies, is both ethically wrong and legally problematic. My understanding encompasses these key aspects:
- Informed Consent: In situations where the patient is conscious and competent, I explain their condition, the proposed treatment options, risks, and benefits in a way they can understand, before obtaining their informed consent. If language barriers exist, I utilize appropriate interpreters.
- Implied Consent: In emergencies, when a patient is unconscious or unable to provide consent, the principle of implied consent applies. We proceed with life-saving interventions under the assumption that a reasonable person would consent to such treatment in that situation. This is always documented thoroughly.
- Next of Kin: If possible, I seek consent from the next of kin for non-emergency procedures, but this does not override the patient’s own autonomy if they are capable of making decisions. For example, if a patient is conscious but requires surgery and family members disagree with the treatment plan, we will discuss options to get the patient to consent themselves if they are capable.
- Confidentiality: Maintaining patient confidentiality is paramount. I only share information with authorized personnel on a need-to-know basis. I adhere strictly to HIPAA regulations (or equivalent) governing patient privacy.
- Ethical Dilemmas: In cases of resource limitations, ethical considerations like triage are crucial, prioritizing patients with the greatest chance of survival. This isn’t about choosing who lives or dies, but making the most effective use of limited resources. I always strive for fairness and transparency in these situations.
For example, I once had to deal with a situation where a patient’s family refused a blood transfusion due to religious beliefs, despite the life-threatening situation. I spent time explaining the risks and benefits, and worked with the family to find common ground to preserve the patient’s life to the fullest extent possible while still honoring their cultural beliefs.
Q 25. How do you handle difficult or emotionally charged situations in trauma care?
Trauma care often involves emotionally charged situations, both for the patient and the care team. Developing coping mechanisms and strategies is crucial for maintaining professionalism and providing effective care.
- Emotional Detachment: While empathy is important, maintaining a degree of emotional detachment can prevent burnout. This doesn’t mean I lack empathy, but rather that I focus on the objective tasks at hand while remaining sensitive to the patient’s emotional state.
- Active Listening and Empathy: I actively listen to the patient and their family, acknowledging their emotions and offering support as appropriate, even if it’s just a compassionate presence. However, there is a limit to what a trauma professional can be expected to do in the midst of a stressful event.
- Team Support: I rely heavily on my colleagues and supervisors for support, especially after emotionally demanding cases. Peer support is invaluable in these situations, along with any professional counselling services provided.
- Self-Care: Prioritizing self-care is non-negotiable. This includes adequate rest, healthy lifestyle choices, and seeking help when needed. De-briefing sessions with colleagues or mental health professionals can be significantly beneficial. Trauma affects the provider as much as the patient.
- Stress Management Techniques: I utilize stress management techniques, such as mindfulness and deep breathing exercises, to cope with stress in high-pressure environments.
A specific example might involve a case involving a child. While the initial focus would be on stabilizing the child medically, taking the time to speak comfortingly to the child and providing a sense of safety can make a significant difference. Post-incident, I would seek support from colleagues or participate in a debriefing session to discuss the emotional impact of the case.
Q 26. Describe your understanding of disaster preparedness and response in relation to trauma.
Disaster preparedness and response are critical aspects of trauma care. My understanding involves several key components:
- Mass Casualty Incident (MCI) Plans: I’m familiar with MCI plans, including triage protocols, resource allocation strategies, and communication procedures. These plans are designed to manage large-scale trauma events efficiently and effectively.
- Triage Systems: I’m proficient in various triage systems, such as START (Simple Triage and Rapid Treatment) and SALT (Start, Assess, Life, Transport), allowing me to quickly prioritize patients based on the severity of their injuries and likelihood of survival.
- Emergency Response Teams: I’ve participated in training exercises and drills simulating disaster scenarios, enhancing my preparedness for such events. I understand my role within a broader emergency response team and how to effectively collaborate with other professionals.
- Communication Systems: Effective communication is paramount during disasters. I’m familiar with the use of communication systems used during MCI’s including radios, cell phones, and designated communication channels.
- Post-Disaster Response: My understanding extends to the post-disaster phase, including the psychological and emotional support required for both survivors and emergency responders.
For example, I’ve participated in simulated mass casualty exercises that involved a mock train derailment. These exercises help solidify my understanding of triage protocols, resource allocation under stress, and coordinating effective team response. They also reinforce the importance of clear communication during chaos.
Q 27. Explain your experience with different types of trauma equipment and technologies.
My experience with trauma equipment and technologies is extensive and encompasses a wide range of tools and techniques used in assessing, treating, and managing trauma patients.
- Advanced Life Support (ALS) Equipment: I’m proficient in using advanced life support equipment, including cardiac monitors, defibrillators, ventilators, and intravenous pumps. I understand the proper application and maintenance of this equipment.
- Trauma Resuscitation Equipment: I have experience with trauma resuscitation equipment such as fluid warmers, blood warmers, and rapid infusion devices, crucial for maintaining hemodynamic stability in critically injured patients.
- Imaging Technologies: I understand the importance and interpretation of various imaging modalities, including X-rays, CT scans, and ultrasound, in the rapid assessment of traumatic injuries. For example, the use of FAST scans (Focused Assessment with Sonography for Trauma) is often crucial in diagnosing internal bleeding rapidly.
- Surgical Instruments and Techniques: My experience extends to the use of surgical instruments and techniques for wound management, hemorrhage control, and other trauma-related surgical interventions.
- Point-of-care testing (POCT): I am comfortable with using POCT devices such as blood glucose meters, coagulation analyzers and blood gas analyzers to obtain immediate results to guide treatment decisions.
For example, I’ve utilized ultrasound for rapid assessment of internal bleeding during the initial trauma resuscitation of a patient with a blunt abdominal injury. This enabled timely intervention and improved the patient’s outcome.
Key Topics to Learn for Basic Trauma Care Interview
- Primary Assessment: Understanding the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) and its practical application in prioritizing life-threatening injuries.
- Shock Management: Recognizing the signs and symptoms of various types of shock, and applying appropriate interventions like fluid resuscitation and positioning.
- Wound Management: Mastering techniques for controlling bleeding (direct pressure, tourniquets), cleaning wounds, and applying appropriate dressings. Understanding the difference in managing open vs. closed wounds.
- Fracture Management: Knowing how to assess and immobilize fractures using splints and slings, while prioritizing patient comfort and preventing further injury.
- Head Injury Management: Recognizing signs of head injury (GCS, pupil response), and understanding the importance of airway management and spinal immobilization.
- Burn Management: Understanding the different types of burns, and applying appropriate first aid measures, including cooling and wound care. Recognizing the need for advanced medical attention.
- Teamwork and Communication: Understanding the crucial role of effective communication and teamwork within a trauma care setting. This includes clear reporting and effective collaboration with colleagues.
- Legal and Ethical Considerations: Familiarizing yourself with relevant legal and ethical guidelines pertaining to patient consent, confidentiality, and documentation.
- Trauma Triage: Prioritizing patients based on the severity of their injuries using appropriate triage systems.
Next Steps
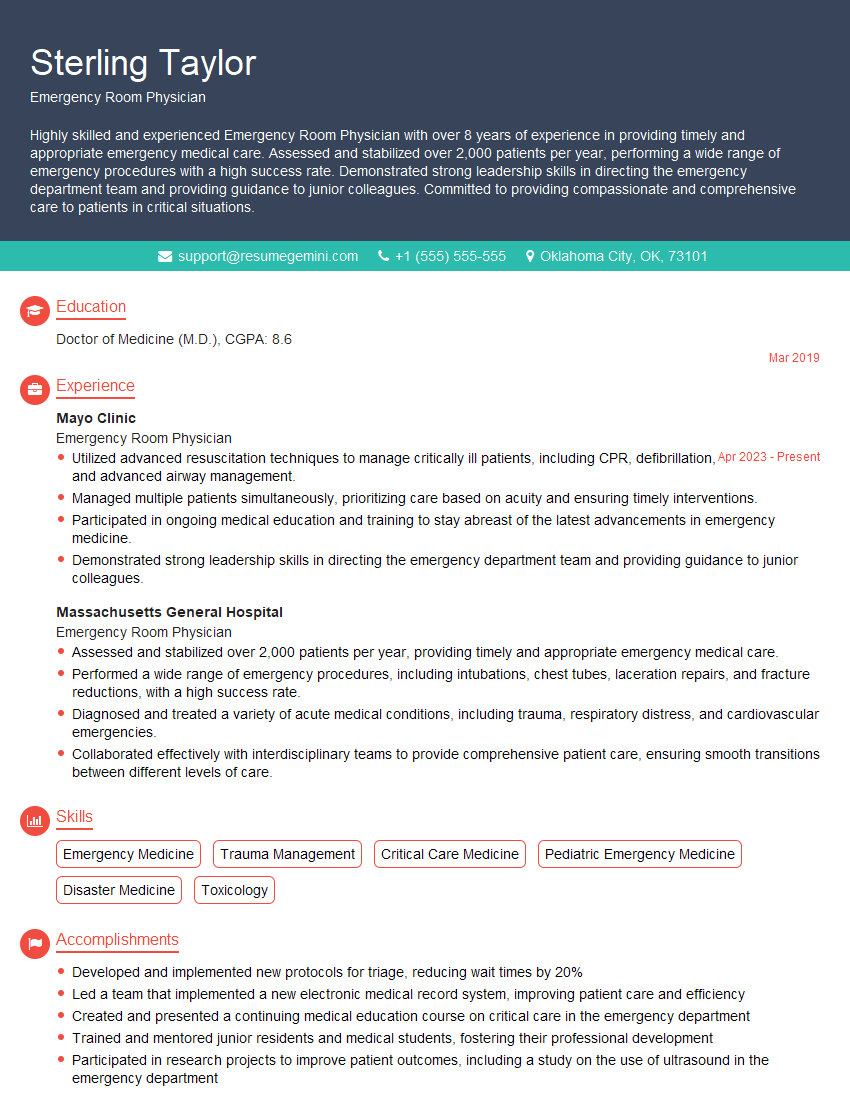
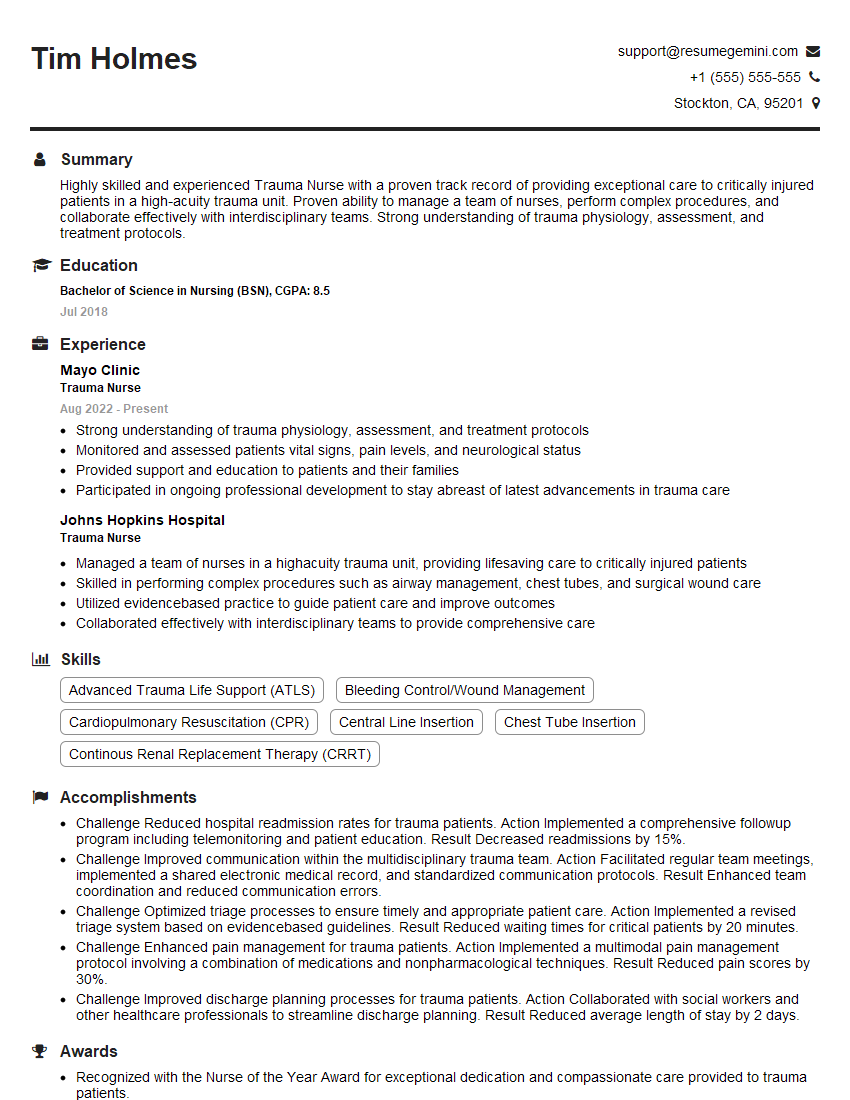
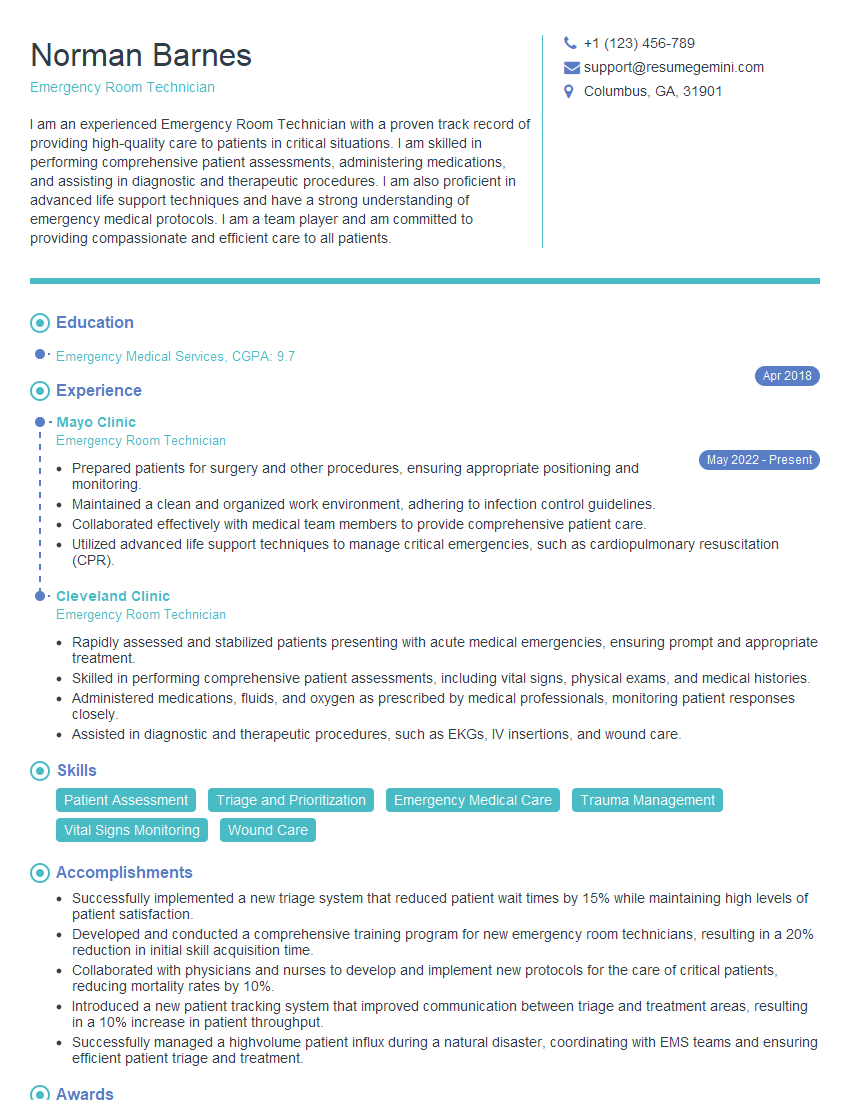
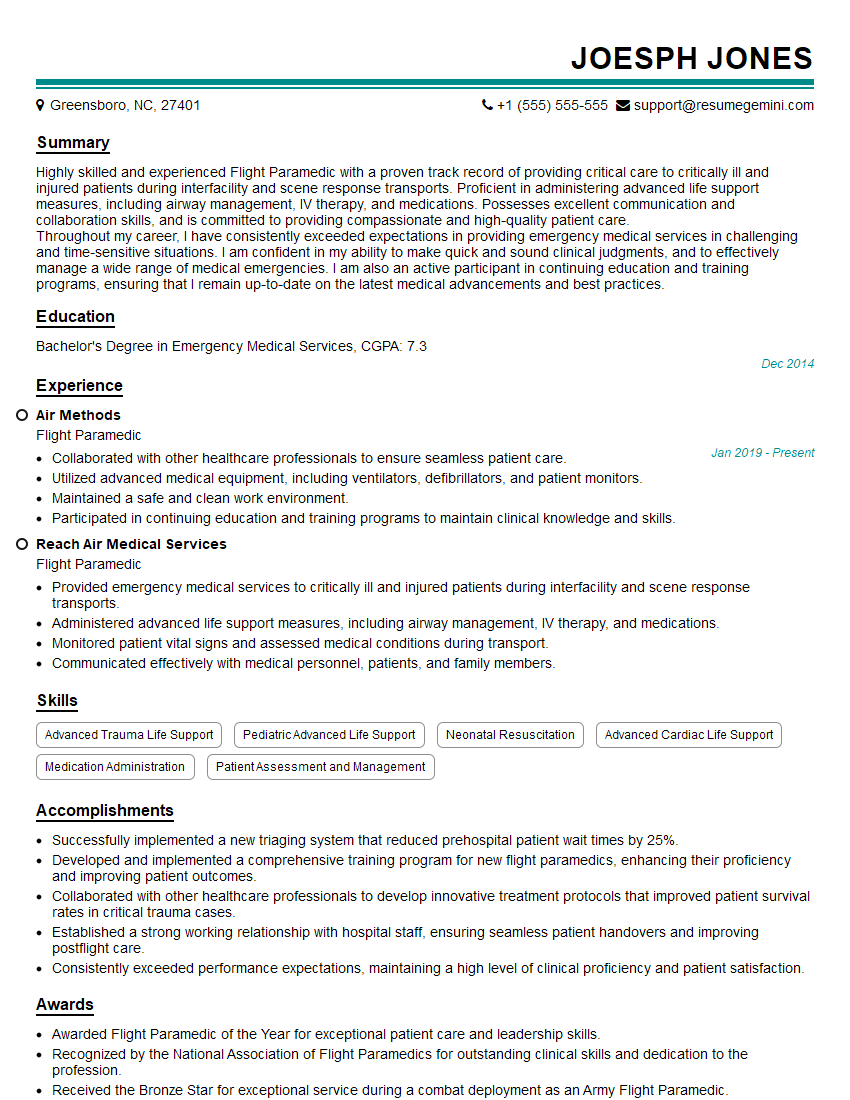
Mastering Basic Trauma Care significantly enhances your career prospects, opening doors to rewarding roles in emergency medicine, pre-hospital care, and other related fields. A strong resume is crucial for showcasing your skills and experience to potential employers. Crafting an ATS-friendly resume is key to ensuring your application gets noticed. We highly recommend using ResumeGemini to build a professional and impactful resume that highlights your qualifications effectively. ResumeGemini offers examples of resumes tailored to Basic Trauma Care to help guide you in creating a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good