Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Bioceramics and Medical Devices interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Bioceramics and Medical Devices Interview
Q 1. Explain the difference between bioactive and bioinert bioceramics.
The key difference between bioactive and bioinert bioceramics lies in their interaction with the body. Bioactive ceramics actively bond with living tissues, forming a strong interfacial bond. This bond promotes tissue integration and growth into the implant material, leading to improved long-term stability and functionality. Think of it like a seed germinating and growing roots into the surrounding soil. Bioinert ceramics, on the other hand, are biologically passive; they don’t chemically interact with the surrounding tissues. Instead, they remain isolated from the biological environment. They are essentially inert, acting as a structural scaffold. An example of this would be a ceramic ball in a ball-and-socket joint replacement.
A simple analogy: Imagine placing a smooth stone (bioinert) and a rough, porous rock (bioactive) into a garden. The smooth stone would sit independently, while the porous rock would allow roots to grow into its crevices and become part of the ecosystem.
Q 2. Describe the properties of Hydroxyapatite (HA) and its applications in medical devices.
Hydroxyapatite (HA), Ca10(PO4)6(OH)2, is a naturally occurring mineral component of bone and teeth. Its exceptional biocompatibility and osteoconductivity (ability to promote bone growth) make it a popular choice in biomedical applications. HA possesses several key properties that contribute to its success:
- Biocompatibility: It is well-tolerated by the body, eliciting minimal inflammatory response.
- Osteoconductivity: It provides a scaffold for bone cells to attach, grow, and mineralize, facilitating bone regeneration.
- High compressive strength: This allows it to withstand significant mechanical loads in weight-bearing applications.
- Porosity: Porous HA structures can improve bone ingrowth and vascularization.
In medical devices, HA finds diverse applications, including:
- Bone grafts and fillers: Used to fill bone defects and aid in fracture healing.
- Coatings on orthopedic implants: Enhancing osseointegration of metal implants such as hip and knee replacements.
- Dental implants: Improving the bonding between the implant and the surrounding jawbone.
- Maxillofacial reconstruction: Repairing bone defects in the craniofacial region.
Q 3. What are the main challenges in designing biocompatible medical devices?
Designing biocompatible medical devices presents a multitude of challenges. The primary aim is to ensure the device interacts harmlessly with the body while fulfilling its intended function. Key challenges include:
- Biocompatibility: Ensuring the device doesn’t trigger an adverse immune response, such as inflammation or rejection.
- Mechanical properties: The device must have the appropriate strength, flexibility, and durability to withstand the stresses imposed by the body’s movement and physiological conditions.
- Sterility: Preventing microbial contamination is crucial to avoid infections.
- Long-term stability: The device needs to maintain its structural integrity and functionality over its intended lifespan, often many years.
- Manufacturing and cost: Producing complex devices with precise dimensions and superior quality while remaining cost-effective.
- Regulatory hurdles: Navigating the complex regulatory pathways required for approval before the device can be used clinically.
A good example of a challenge is designing a vascular stent that is strong enough to keep an artery open but flexible enough to not damage the vessel wall. The material choice, surface finish and design all play critical roles.
Q 4. Discuss the different types of bioceramic materials and their respective applications.
Various bioceramic materials are used in medical devices, each possessing unique properties and applications:
- Hydroxyapatite (HA): As discussed previously, its excellent biocompatibility and osteoconductivity make it ideal for bone grafts, coatings, and dental implants.
- Tricalcium Phosphate (TCP): Another calcium phosphate ceramic, TCP is bioresorbable, meaning it gradually dissolves in the body after implantation, being replaced by newly formed bone tissue. It’s often used in bone grafts where gradual replacement is desirable.
- Bioglass (45S5): A silica-based glass-ceramic, it possesses excellent bioactivity, bonding strongly to bone. It is often used in coatings and as a bone filler.
- Zirconia (ZrO2): Known for its high strength and toughness, zirconia is used in dental implants and as a structural material in load-bearing applications. However, its bioactivity is lower than that of HA.
- Alumina (Al2O3): A very hard and wear-resistant ceramic, alumina is used in hip and knee joint replacements, primarily as bearing surfaces.
The choice of bioceramic material depends heavily on the specific application and the desired properties, including bioactivity, strength, resorption rate, and cost.
Q 5. Explain the process of sintering in bioceramic manufacturing.
Sintering is a crucial step in bioceramic manufacturing. It involves heating a powdered bioceramic material below its melting point to bond the particles together, forming a solid, dense structure. This process enhances the mechanical strength and density of the bioceramic component, while also influencing its porosity and overall performance.
The process typically involves these steps:
- Powder Preparation: The bioceramic powder needs to be uniformly sized and mixed to ensure homogeneous sintering.
- Forming: The powder is shaped into the desired form (e.g., pressing, injection molding).
- Sintering: The shaped component is placed in a high-temperature furnace under controlled atmospheric conditions. The temperature and time are crucial parameters, determined by the material’s characteristics.
- Cooling: The sintered component is slowly cooled to avoid thermal shock and cracking.
- Post-Sintering Treatment (Optional): Steps such as machining, polishing, or surface modification may be necessary to achieve the final desired product.
Controlling the sintering temperature and duration allows tailoring the final material properties, such as porosity, which can be crucial for bone ingrowth in applications like bone grafts.
Q 6. How do you assess the biocompatibility of a bioceramic material?
Assessing the biocompatibility of a bioceramic material is a rigorous process involving multiple in vitro (cell culture) and in vivo (animal studies) tests. The goal is to determine the material’s safety and its interaction with biological systems.
Common methods include:
- Cytotoxicity assays: Evaluating the material’s effect on cell viability and proliferation using cell cultures.
- Genotoxicity assays: Assessing the potential of the material to cause DNA damage.
- Inflammation testing: Measuring the inflammatory response in the surrounding tissues.
- In vivo implantation studies: Implanting the material in animal models to observe its long-term effects on tissues and organs.
- Mechanical testing: Evaluating strength, wear resistance and other key properties critical for device function.
The specific tests performed depend on the intended application of the bioceramic. For example, a bioceramic used in bone grafts would require rigorous testing of osteoconductivity and bioresorbability. The data obtained from these tests help determine the biocompatibility profile of the bioceramic and inform the design and selection of appropriate materials.
Q 7. What are the regulatory pathways for medical devices?
The regulatory pathways for medical devices vary across different countries and regions but generally involve several stages of review and approval. The process is designed to ensure the safety and effectiveness of the device before it reaches the market. In the United States, the Food and Drug Administration (FDA) is the primary regulatory body. The classification of the device (Class I, II, or III) based on risk level significantly impacts the regulatory requirements. Class III devices, those that support or sustain human life, face the most stringent requirements.
Key stages typically include:
- Premarket notification (510(k)): Demonstrates substantial equivalence to an already-approved device.
- Premarket approval (PMA): Requires extensive clinical data to demonstrate safety and effectiveness, typically for high-risk Class III devices.
- Investigational Device Exemption (IDE): Allows the testing of new devices in clinical trials before seeking full approval.
- Postmarket surveillance: Monitoring the device’s safety and performance after it’s on the market.
Similar regulatory bodies exist in Europe (e.g., the European Medicines Agency) and other parts of the world, each with specific requirements and procedures.
Q 8. Describe the different types of degradation mechanisms for bioceramics.
Bioceramics, like all materials, degrade over time, albeit at vastly different rates. The degradation mechanisms are complex and often intertwined, but we can broadly categorize them into:
- Dissolution: This is a chemical process where the ceramic material dissolves into the surrounding body fluids. Think of it like sugar dissolving in water. The rate depends on the ceramic’s solubility and the pH of the body fluid. For instance, highly soluble calcium phosphates can dissolve relatively quickly, while more inert ceramics like alumina are much more resistant.
- Hydrolysis: Water molecules react with the ceramic’s chemical bonds, breaking them down and leading to the release of ions. This is particularly relevant for ceramics containing siloxane bonds (Si-O-Si), like bioglasses. The rate of hydrolysis is affected by factors such as the surface area of the material and the presence of catalysts in the body.
- Corrosion: This occurs when the ceramic interacts with the body’s environment, leading to chemical attack and material loss. This is less common with many bioceramics compared to metallic implants, but can still happen, particularly if the ceramic is not completely biocompatible.
- Wear: Mechanical wear and tear can occur through friction or contact with other materials in the body, such as bone or other implants. This is especially relevant in load-bearing applications like hip or knee replacements. The wear debris can cause inflammation and other complications.
Understanding these mechanisms is crucial for designing bioceramics with predictable degradation profiles, ensuring the implant performs its intended function and integrates safely with the body.
Q 9. How do you design a medical device for specific anatomical locations?
Designing a medical device for a specific anatomical location is a multifaceted process requiring detailed knowledge of the anatomy, physiology, and biomechanics of that region. We need to consider several key factors:
- Geometry and Size: The implant must fit precisely within the target location without causing unnecessary stress or damage to surrounding tissues. This often requires intricate 3D modeling and prototyping.
- Biomechanics: The implant must withstand the stresses and strains encountered in that specific anatomical region. A knee replacement, for example, experiences far greater forces than a dental implant, so the material choice and design would be vastly different.
- Tissue Interactions: The device’s surface properties must promote integration with the surrounding tissue and prevent inflammation or adverse reactions. Surface modification techniques can be employed to enhance biocompatibility and osseointegration (bone bonding).
- Access and Surgical Considerations: The device’s design needs to accommodate surgical access and implantation techniques. Minimally invasive surgery often dictates smaller, more streamlined implant designs.
- Material Properties: The chosen biomaterial must exhibit appropriate mechanical properties, biocompatibility, and degradation characteristics within the specific environment. For example, a material used in a load-bearing joint replacement requires much higher strength and durability than one used in a bone-filling application.
Imagine designing a stent for a coronary artery versus a bone screw for the femur – the designs and materials would be completely different to account for the differing biomechanical and anatomical environments.
Q 10. What are the key considerations in selecting biocompatible materials for implants?
Selecting biocompatible materials for implants is paramount to ensuring patient safety and the success of the medical device. Key considerations include:
- Cytotoxicity: The material shouldn’t be toxic to cells. Extensive in vitro (cell culture) and in vivo (animal studies) testing is necessary to evaluate this.
- Genotoxicity: The material shouldn’t damage DNA. This is another crucial aspect of safety testing.
- Inflammation: The material should minimize the body’s inflammatory response. A material that triggers excessive inflammation can lead to implant failure and complications.
- Immunogenicity: The implant should not trigger an immune response, avoiding rejection by the patient’s body. Surface modifications can help reduce immunogenicity.
- Mechanical Properties: The material must possess the required mechanical strength, stiffness, and durability for its intended application. A hip implant requires vastly different mechanical properties than a scaffold for bone regeneration.
- Degradation: The degradation rate should be carefully considered. Some applications require bioresorbable materials that break down over time, while others require long-term stability.
- Sterilizability: The material should withstand sterilization processes without compromising its integrity or biocompatibility.
A thorough risk assessment and material characterization are essential steps in the selection process. Choosing the wrong material can have severe consequences for the patient.
Q 11. Explain the concept of bioresorbability and its relevance in bioceramics.
Bioresorbability refers to the ability of a material to be gradually absorbed and metabolized by the body. In the context of bioceramics, this means that the implant will eventually dissolve or be replaced by host tissue, eliminating the need for a second surgery to remove it. This is particularly advantageous in applications where a temporary scaffold is required, such as bone regeneration. Think of it like a temporary cast for a broken bone – once the bone heals, the cast is removed. Similarly, a bioresorbable scaffold provides structural support for bone growth, and once the bone is healed, the scaffold is gradually absorbed.
The relevance of bioresorbability in bioceramics is substantial. For example, bioresorbable calcium phosphate ceramics are used in bone grafts and tissue engineering applications, providing structural support while promoting bone regeneration. The controlled degradation of these materials allows for gradual replacement by newly formed bone tissue, minimizing the risk of adverse effects from a permanent implant.
Q 12. Describe the mechanical properties of common bioceramics used in medical implants.
Common bioceramics used in medical implants exhibit a wide range of mechanical properties, depending on their composition and processing. Here are some examples:
- Hydroxyapatite (HA): Relatively brittle, with a compressive strength similar to cortical bone, but low tensile strength. Widely used in bone grafts and coatings due to its excellent biocompatibility and osteoconductive properties.
- Tricalcium Phosphate (TCP): Slightly more brittle than HA, but with faster bioresorbability. Often used in bone fillers and scaffolds.
- Bioactive Glasses: Exhibit a range of mechanical properties depending on their composition, generally having lower strength than HA and TCP but offering enhanced bioactivity and bonding with bone.
- Alumina (Al2O3): Very high strength and hardness, making it suitable for load-bearing applications like hip and knee replacements, although its bioinertness means it doesn’t bond with bone as effectively as HA.
- Zirconia (ZrO2): Exceptional strength and fracture toughness, also suitable for load-bearing implants, but more expensive than alumina.
The choice of bioceramic is dictated by the specific requirements of the application, balancing mechanical properties with biocompatibility and degradation characteristics.
Q 13. What are some common failure modes of medical implants made of bioceramics?
Medical implants made of bioceramics can fail due to several common modes:
- Fracture: This can occur due to excessive stress or fatigue loading, particularly in load-bearing applications. Improper design or material selection can increase this risk. Imagine a hip replacement fracturing due to a fall.
- Debonding: In implants where bonding to bone is crucial (like bone cement in hip replacements), failure can occur if the bond weakens or breaks. This can lead to loosening of the implant and pain.
- Corrosion/Dissolution: While less common than in metallic implants, excessive corrosion or dissolution of the bioceramic can compromise its structural integrity and lead to failure.
- Wear: Friction between the implant and surrounding tissues can cause wear and the production of wear debris, which can trigger inflammation and accelerate degradation.
- Infection: Infection around the implant can lead to its degradation and failure. Strict sterile techniques and careful surgical practices are crucial to prevent this.
Understanding these failure modes and incorporating design features and material choices to mitigate their occurrence is vital in ensuring long-term implant success.
Q 14. How do you ensure the sterility of medical devices?
Ensuring the sterility of medical devices is critical to prevent infections. A multi-pronged approach is usually employed, involving:
- Sterilization Process Selection: Several methods exist, each with its pros and cons. Common methods include:
- Ethylene Oxide (EtO) Sterilization: Effective for a wide range of materials but requires careful handling due to its toxicity.
- Gamma Irradiation: A highly effective method for many materials but can alter the properties of some polymers or bioceramics.
- Steam Sterilization (Autoclaving): A reliable and cost-effective method for heat-resistant materials.
- Validation: Rigorous testing is required to verify the effectiveness of the chosen sterilization method in achieving sterility. This often involves biological indicators to ensure complete microbial kill.
- Aseptic Processing: Maintaining a sterile environment throughout the manufacturing process is crucial to prevent contamination of the device before sterilization.
- Packaging: Appropriate packaging is essential to maintain sterility after sterilization. The packaging must protect the device from environmental contamination.
- Sterility Assurance Level (SAL): The manufacturer must define a SAL, which represents the probability of a single viable microorganism surviving the sterilization process (typically 10-6 or lower).
Stringent quality control measures and adherence to regulatory guidelines are essential to ensure that medical devices are sterile and safe for use.
Q 15. Explain the concept of surface modification in bioceramics.
Surface modification in bioceramics is a crucial technique used to enhance the biocompatibility and functionality of these materials. Essentially, it involves altering the surface properties—chemical composition, topography, and wettability—without significantly changing the bulk properties. This is vital because the surface is the primary point of interaction between the bioceramic implant and the surrounding biological environment.
Several methods achieve surface modification, including:
- Plasma treatment: This introduces reactive species to the surface, altering its chemistry and creating functional groups for further modifications like protein attachment.
- Chemical etching: This roughens the surface, increasing surface area and promoting bone integration.
- Coatings: Applying bioactive coatings like hydroxyapatite (HA) or bioactive glasses enhances osteoconductivity (the ability to promote bone growth).
- Sol-gel deposition: This method allows precise control over the coating composition and thickness, enabling the creation of gradient coatings with tailored properties.
For example, modifying the surface of a titanium implant with a bioactive glass coating can significantly improve its osseointegration, leading to a more stable and durable implant. This principle is applied in orthopedic, dental, and maxillofacial applications, where good bone integration is critical for success.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the ethical considerations in designing and using medical devices?
Ethical considerations in medical device design and use are paramount. They span the entire lifecycle, from initial conception to post-market surveillance. Key areas include:
- Patient safety: This is the foremost consideration. Designs must prioritize minimizing risks and maximizing benefits, with rigorous testing and validation to ensure safety and efficacy.
- Informed consent: Patients must be fully informed about the device, its risks and benefits, and alternative treatments before consenting to its use. This requires clear and accessible communication.
- Equity and access: Devices should be designed and priced to ensure equitable access for all patients, regardless of socioeconomic status or geographic location. This addresses potential health disparities.
- Data privacy and security: Medical devices often collect patient data, raising concerns about privacy and security. Robust safeguards must be in place to protect patient information.
- Environmental impact: The environmental footprint of device manufacturing and disposal should be minimized through sustainable practices and responsible waste management.
- Transparency and accountability: Clear and transparent communication regarding device performance, risks, and adverse events is essential, along with accountability for any failures or shortcomings.
Ignoring these ethical considerations can lead to devastating consequences, including patient harm, loss of public trust, and legal repercussions.
Q 17. Describe your experience with ISO 13485 standards.
My experience with ISO 13485:2016 standards is extensive. Throughout my career, I’ve been directly involved in the design, development, and manufacturing of medical devices that meet these rigorous quality management system requirements. This includes:
- Implementing quality management systems: I’ve spearheaded the implementation and maintenance of ISO 13485-compliant QMS within several companies, ensuring that all processes, from design control to post-market surveillance, adhere to the standard.
- Conducting internal audits: I have participated in numerous internal audits to assess the effectiveness of the QMS and identify areas for improvement. This helps to proactively identify and mitigate potential risks.
- Supporting regulatory submissions: I’ve contributed to the preparation of regulatory submissions to various agencies, ensuring that our documentation meets the stringent requirements outlined in ISO 13485 and other relevant regulations.
- Training and mentoring: I have trained and mentored colleagues on ISO 13485 requirements, fostering a culture of quality and compliance within the organization.
Understanding and applying ISO 13485 isn’t just about ticking boxes; it’s about establishing a robust framework that ensures the safety and efficacy of medical devices and protects patients.
Q 18. Explain the role of bioceramics in tissue engineering.
Bioceramics play a critical role in tissue engineering by providing a scaffold or matrix for tissue regeneration. Their biocompatibility, osteoconductivity, and customizable properties make them ideal for guiding cell growth and tissue formation.
Examples include:
- Hydroxyapatite (HA): HA is a naturally occurring mineral component of bone, making it highly biocompatible and osteoconductive. It’s used in bone grafts and coatings for orthopedic implants.
- Bioactive glasses: These glasses react with body fluids to form a bioactive layer that promotes bone bonding. They’re used in bone regeneration applications and drug delivery systems.
- Tricalcium phosphate (TCP): TCP is another calcium phosphate ceramic that is bioresorbable, meaning it’s gradually replaced by new bone tissue. This makes it suitable for bone void fillers.
In tissue engineering, bioceramics are often combined with other biomaterials like polymers or growth factors to create sophisticated constructs that promote tissue regeneration. The porous structure of many bioceramics allows for cell infiltration and vascularization, essential for successful tissue integration.
Q 19. How do you characterize the microstructure of a bioceramic material?
Characterizing the microstructure of a bioceramic material is essential for understanding its properties and performance. This involves a range of techniques:
- Scanning Electron Microscopy (SEM): SEM provides high-resolution images of the surface morphology, revealing pore size distribution, grain size, and surface roughness. This information is crucial for assessing the material’s suitability for cell growth and interaction.
- Transmission Electron Microscopy (TEM): TEM allows for higher magnification imaging and provides detailed information about crystal structure and defects within the material, impacting its mechanical properties.
- X-ray Diffraction (XRD): XRD identifies the crystalline phases present in the bioceramic, revealing the material’s composition and influencing its bioactivity.
- Mercury intrusion porosimetry: This technique quantifies the pore size distribution and total porosity of the bioceramic, which is essential for its biocompatibility and mechanical properties.
- Image analysis software: Software is used to quantify microstructural features such as pore size, shape, and interconnectivity from SEM or TEM images.
By combining these techniques, a comprehensive understanding of the bioceramic’s microstructure can be obtained, linking its structure to its properties and ultimately, its performance in a biological environment.
Q 20. What are the advantages and disadvantages of using bioceramics compared to other biomaterials?
Bioceramics offer several advantages compared to other biomaterials, but also have some limitations.
Advantages:
- Biocompatibility: Many bioceramics are highly biocompatible, exhibiting minimal adverse reactions in the body.
- Osseointegration: Certain bioceramics, like HA, exhibit excellent osteoconductivity, promoting direct bone bonding to the implant.
- Strength and durability: Some bioceramics possess good mechanical strength and wear resistance, suitable for load-bearing applications.
- Tailorable properties: The properties of bioceramics can be adjusted by altering their composition, microstructure, and surface modification.
Disadvantages:
- Brittleness: Many bioceramics are brittle and susceptible to fracture under stress.
- Limited flexibility: Bioceramics generally lack flexibility compared to polymers or metals.
- Processing challenges: The processing of bioceramics can be complex and require specialized techniques.
- Cost: Some bioceramics can be relatively expensive compared to other biomaterials.
The choice of biomaterial depends on the specific application and the desired properties. For example, while the brittleness of some bioceramics might be a limitation for load-bearing applications, their bioactivity and osteoconductivity make them ideal for bone regeneration.
Q 21. Describe your experience with different manufacturing techniques for bioceramics (e.g., pressing, casting, 3D printing).
My experience encompasses a range of manufacturing techniques for bioceramics:
- Powder pressing: This is a common method for producing dense bioceramic components. It involves compacting a fine powder under high pressure, followed by sintering (high-temperature heat treatment) to achieve the desired density and strength. This is suitable for producing simple shapes with good dimensional accuracy.
- Slip casting: This technique utilizes a suspension of ceramic powder (slip) which is poured into a porous mold. Water is absorbed by the mold, leaving behind a solid ceramic layer. Slip casting is effective for creating complex shapes, but control over density can be challenging.
- Tape casting: This involves preparing a slurry of ceramic powder, binder, and solvent, which is cast into a thin tape using a doctor blade. These tapes can then be laminated and cut to create components with specific configurations. This is efficient for creating thin and intricate structures.
- 3D printing (Additive Manufacturing): This rapidly evolving technology offers unprecedented capabilities for creating complex and customized bioceramic scaffolds. Various 3D printing techniques, such as stereolithography (SLA) or inkjet printing, are used depending on the desired resolution and material properties. This allows for creating scaffolds with precisely controlled pore architectures to optimize cell growth and tissue integration.
The selection of the most appropriate manufacturing technique depends on the desired component shape, size, properties, and production volume. For instance, while powder pressing is suitable for mass production of simple implants, 3D printing allows for the fabrication of patient-specific implants with intricate designs.
Q 22. Explain the importance of in-vitro and in-vivo testing for biocompatibility.
Biocompatibility testing is crucial for ensuring the safety and efficacy of medical devices. In-vitro and in-vivo tests form a crucial two-pronged approach to evaluating this. In-vitro tests, meaning “in glass,” are conducted in a controlled laboratory setting, using cell cultures or tissue samples to assess the material’s effects on biological systems. This allows us to screen materials quickly and cost-effectively, evaluating parameters like cytotoxicity (cell death), genotoxicity (DNA damage), and inflammatory responses.
In-vivo tests, on the other hand, are conducted within a living organism, typically animal models. These studies provide a more holistic picture by mimicking the actual physiological environment in which the bioceramic device will operate. This allows us to evaluate long-term effects, tissue integration, and systemic responses that might not be apparent in in-vitro assays. For example, we might implant a bioceramic scaffold into a bone defect in a rat model to assess bone regeneration and the biomaterial’s overall biocompatibility in the living system.
A combination of both is essential. In-vitro data helps screen potential candidates and narrow the selection before committing to more resource-intensive in-vivo studies, reducing animal use while still ensuring rigorous safety evaluations.
Q 23. How do you address potential toxicity concerns associated with bioceramic materials?
Addressing toxicity concerns with bioceramics requires a multi-faceted approach that begins even before material synthesis. Careful selection of raw materials is critical; we need to thoroughly understand the potential impurities and their possible toxic effects. For example, heavy metal contamination can lead to significant problems. Rigorous characterization techniques like X-ray diffraction (XRD), scanning electron microscopy (SEM), and inductively coupled plasma mass spectrometry (ICP-MS) help us analyze the material composition and ensure purity.
Next, in-vitro cytotoxicity assays, such as the MTT assay or live/dead cell staining, are used to assess the material’s effect on cell viability and function. We then perform in-vivo studies to evaluate systemic toxicity, looking for signs of inflammation, organ damage, or other adverse effects. If toxicity is detected, we might explore surface modifications, such as coatings or different processing techniques, to improve biocompatibility. For example, a bioactive glass might be modified with a polymer coating to reduce its initial burst release of ions.
Furthermore, robust data analysis and risk assessment are essential. We need to understand the relationship between the material’s properties and its biological response, allowing us to make informed decisions about its safety and suitability for medical applications.
Q 24. Describe your experience with designing and conducting experiments related to bioceramics and medical devices.
My experience encompasses the entire lifecycle of bioceramic medical device development, from initial concept to final testing. I’ve been involved in designing and conducting experiments on a range of bioceramics, including hydroxyapatite, tricalcium phosphate, and bioactive glasses. My work includes synthesizing materials using techniques like sol-gel processing and powder metallurgy, followed by extensive characterization to evaluate their physical, chemical, and biological properties.
For instance, in one project, I designed and executed in-vitro experiments to assess the osteogenic differentiation potential of a novel bioactive glass scaffold. This involved culturing osteoblast cells on the scaffold and evaluating gene expression, alkaline phosphatase activity, and calcium deposition over several weeks. In another project, we conducted in-vivo studies in a rabbit model to assess bone regeneration following implantation of a porous hydroxyapatite implant. This included radiographic imaging, micro-CT analysis, and histological examination to assess bone ingrowth and integration.
My experimental design always adheres to rigorous scientific principles, ensuring reproducibility and data integrity. I’m proficient in statistical analysis and data interpretation, enabling me to draw meaningful conclusions from the experimental findings.
Q 25. What are your strategies for troubleshooting problems encountered during the development or manufacturing of medical devices?
Troubleshooting during medical device development requires a systematic and multidisciplinary approach. My strategy involves a structured problem-solving framework. First, I meticulously document all aspects of the process, creating a detailed record of materials, methods, and results. This allows for efficient tracking of issues and helps prevent recurrence.
Second, a thorough analysis of the problem is performed, considering potential sources including material defects, manufacturing flaws, or design limitations. Third, I employ a hypothesis-driven approach, formulating potential solutions and testing them systematically. For example, if an implant exhibits unexpected degradation, we might investigate the influence of pH, ionic strength, or mechanical stresses on its stability.
Collaboration is crucial. I often work closely with engineers, clinicians, and regulatory affairs professionals to address challenges, ensuring a holistic approach. Finally, thorough documentation of the troubleshooting process is necessary for continuous improvement and future project planning. Effective communication ensures that solutions are implemented effectively and efficiently.
Q 26. Describe your knowledge of different types of medical device coatings.
Medical device coatings play a critical role in enhancing biocompatibility, improving functionality, and extending the lifespan of implants. The choice of coating depends heavily on the specific application and desired properties. Several types exist, each with its advantages and disadvantages.
- Bioactive coatings: These coatings, such as hydroxyapatite or bioactive glasses, promote bone bonding and integration. They are frequently used on orthopedic implants to enhance osseointegration.
- Polymer coatings: Polymers like polyethylene glycol (PEG) or polylactic acid (PLA) can reduce protein adsorption and cell adhesion, minimizing inflammation and improving biocompatibility. They can also provide lubricity in joint replacements.
- Metallic coatings: Coatings like titanium nitride (TiN) or gold can enhance wear resistance, corrosion resistance, and reduce friction in joint replacements and other moving parts of implants.
- Drug-eluting coatings: These coatings incorporate therapeutic agents that are released gradually, improving healing and reducing inflammation. This is particularly valuable in cardiovascular stents or drug delivery systems.
The selection of the appropriate coating is a complex process, considering factors like the substrate material, the desired biological response, and the regulatory requirements for the specific device.
Q 27. What is your experience with finite element analysis (FEA) and its application to medical device design?
Finite Element Analysis (FEA) is an indispensable tool in medical device design. It’s a computational method that allows us to simulate the mechanical behavior of a device under various loading conditions, helping predict its performance and durability within the body. My experience includes using FEA software to model stress and strain distribution in various bioceramic implants, particularly in orthopedic and dental applications.
For example, I’ve used FEA to optimize the design of a hip implant, ensuring that the stress concentrations were minimized in critical areas to reduce the risk of fracture or loosening. This involved creating a detailed 3D model of the implant and the surrounding bone, defining material properties, and applying relevant boundary conditions, such as body weight and muscle forces. The simulation provided valuable insights into the implant’s performance under physiological loading, leading to design modifications that improved its longevity and safety.
FEA is also critical in predicting the long-term behavior of bioceramic materials, evaluating their degradation, and optimizing their design for improved biointegration.
Q 28. How do you stay updated with the latest advancements in bioceramics and medical devices?
Staying current in the rapidly evolving fields of bioceramics and medical devices requires a multifaceted approach. I regularly attend conferences and workshops, such as those organized by the Society for Biomaterials or the Biomedical Engineering Society, to network with peers and learn about cutting-edge research.
I actively follow peer-reviewed scientific journals like Biomaterials, Journal of Biomedical Materials Research, and Acta Biomaterialia. Furthermore, online resources such as PubMed and Google Scholar are invaluable for accessing the latest research publications. I also participate in online communities and forums to engage in discussions with experts in the field.
Finally, collaboration with researchers and industry professionals plays a crucial role. Engaging in collaborative research projects allows me to access new ideas, techniques, and perspectives, fostering continuous learning and professional development.
Key Topics to Learn for Bioceramics and Medical Devices Interviews
Preparing for a Bioceramics and Medical Devices interview requires a comprehensive understanding of both theoretical foundations and practical applications. This section outlines key areas to focus your studies.
- Biomaterial Selection and Characterization: Understanding the properties of various bioceramics (e.g., hydroxyapatite, alumina, zirconia) and their suitability for specific medical applications. This includes mechanical properties, biocompatibility, and degradation mechanisms.
- Biocompatibility and Tissue Response: Exploring the interaction between bioceramics and living tissue. Focus on concepts like osseointegration, inflammation, and foreign body reaction. Consider the role of surface modification techniques in enhancing biocompatibility.
- Medical Device Design and Manufacturing: Familiarize yourself with the design principles and manufacturing processes involved in creating medical devices incorporating bioceramics. This includes considerations for sterilization, biodegradability, and regulatory compliance.
- Applications in Orthopedics and Dentistry: Gain a solid understanding of the use of bioceramics in orthopedic implants (e.g., hip replacements, bone grafts) and dental applications (e.g., dental implants, bone fillers).
- Advanced Topics (depending on the role): Depending on the specific job description, you might want to delve into areas like 3D printing of bioceramics, drug delivery systems using bioceramics, or the latest research and advancements in the field.
- Problem-Solving and Case Studies: Practice analyzing case studies that involve challenges in bioceramic design, manufacturing, or clinical applications. Focus on developing your problem-solving skills and ability to articulate your thought process.
Next Steps
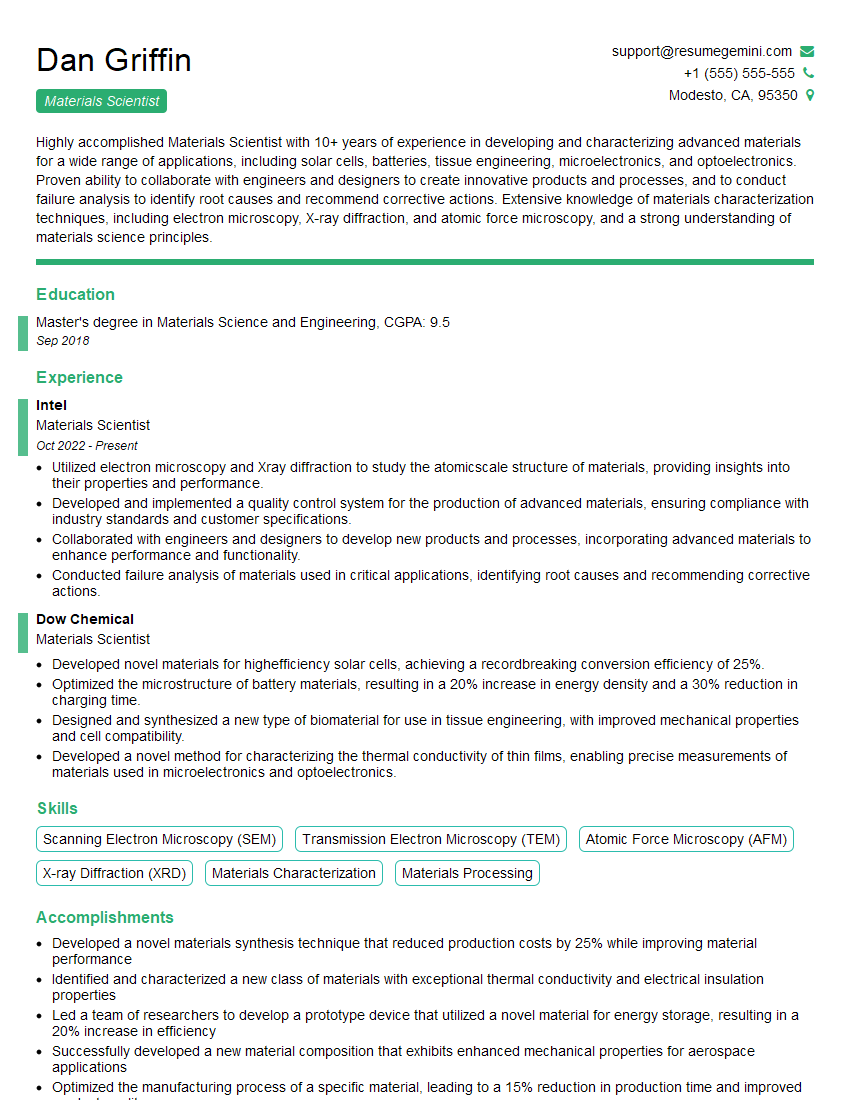
Mastering the concepts of Bioceramics and Medical Devices is crucial for a successful career in this rapidly evolving field. A strong understanding of these areas will significantly enhance your interview performance and open doors to exciting opportunities. To maximize your job prospects, it’s vital to create a compelling and ATS-friendly resume that effectively showcases your skills and experience.
We highly recommend using ResumeGemini to build a professional resume tailored to the Bioceramics and Medical Devices industry. ResumeGemini provides a user-friendly platform to create a resume that stands out and increases your chances of landing your dream job. Examples of resumes tailored to this specific field are available to help guide your resume creation process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good