The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Biomaterials Characterization interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Biomaterials Characterization Interview
Q 1. Explain the principles of Atomic Force Microscopy (AFM) in biomaterials characterization.
Atomic Force Microscopy (AFM) is a powerful technique used to characterize the surface topography and mechanical properties of biomaterials at the nanoscale. It works by scanning a sharp tip, attached to a cantilever, across the sample’s surface. A laser beam reflects off the back of the cantilever, and minute deflections caused by interactions between the tip and the sample are detected by a photodiode. These deflections are then used to create a three-dimensional image of the surface.
There are several modes of AFM, including contact mode (where the tip maintains constant contact with the surface), tapping mode (where the cantilever oscillates and lightly taps the surface), and non-contact mode (where the tip oscillates above the surface). The choice of mode depends on the sample’s properties and the desired information. For example, tapping mode is often preferred for soft, biological samples to minimize damage.
In biomaterial characterization, AFM is used to visualize surface features like roughness, porosity, and protein adsorption. It can also be used to measure the mechanical properties of biomaterials, such as stiffness (Young’s modulus) and adhesion forces. Imagine trying to understand the texture of a tiny, delicate flower petal – AFM provides that same level of detail for biomaterials at the nanoscale.
Q 2. Describe the applications of X-ray diffraction (XRD) in analyzing biomaterial crystallinity.
X-ray diffraction (XRD) is a crucial technique for analyzing the crystallinity of biomaterials. It exploits the phenomenon of X-ray scattering from the crystal lattice of a material. When a beam of X-rays is directed at a crystalline material, the X-rays are diffracted at specific angles depending on the spacing between the atoms in the crystal lattice. This diffraction pattern is then recorded and analyzed to determine the crystal structure, crystallite size, and degree of crystallinity.
In biomaterials, XRD is used to identify the phases present in a material, quantify the degree of crystallinity (how much of the material is organized in a crystalline structure versus amorphous), and determine the orientation of crystallites. For instance, understanding the crystallinity of a polymer is essential for predicting its mechanical strength and degradation behavior. A highly crystalline polymer will generally be stronger and less susceptible to degradation compared to an amorphous one. XRD can be used to monitor changes in crystallinity during processing or aging of biomaterials.
For example, in the analysis of hydroxyapatite (HA) – a common bioceramic – XRD helps verify the successful synthesis of crystalline HA, which is crucial for its bioactivity and integration with bone tissue. The sharp diffraction peaks in the XRD pattern confirm the crystalline nature of the material.
Q 3. How does Scanning Electron Microscopy (SEM) differ from Transmission Electron Microscopy (TEM) in imaging biomaterials?
Both Scanning Electron Microscopy (SEM) and Transmission Electron Microscopy (TEM) are powerful techniques for imaging biomaterials, but they differ significantly in their imaging principles and the information they provide. SEM produces images of the sample’s surface by scanning it with a focused beam of electrons, while TEM creates images by transmitting electrons through a very thin sample.
SEM provides high-resolution images of the sample’s surface morphology, including texture, roughness, and topography. It’s ideal for visualizing surface features and analyzing the overall structure of a biomaterial. SEM is typically used on relatively thicker samples and requires less sample preparation compared to TEM.
TEM, on the other hand, provides higher magnification and resolution, allowing for the visualization of internal structures and crystal lattices. Because the electrons pass through the sample, TEM is best suited for very thin samples and offers information about the sample’s internal microstructure, crystal structure and composition. Sample preparation for TEM is significantly more complex and time-consuming than for SEM, often requiring ultra-thin sectioning.
Think of it like this: SEM is like taking a picture of the outside of a house, showing its shape and texture. TEM is like cutting the house in half and examining the internal structure of its walls and rooms. Each technique offers unique and valuable insights into the structure of biomaterials.
Q 4. What are the advantages and limitations of using Differential Scanning Calorimetry (DSC) for biomaterial analysis?
Differential Scanning Calorimetry (DSC) is a thermal analysis technique used to study the thermal transitions of biomaterials. It measures the difference in heat flow between a sample and a reference material as a function of temperature. This allows for the identification of glass transitions, melting points, crystallization events, and other thermal changes.
Advantages: DSC is relatively simple to use, provides quantitative data on thermal transitions, and requires small sample sizes. It’s useful for characterizing the thermal stability of biomaterials, identifying phase transitions, and studying the effects of processing parameters on the thermal behavior. For example, DSC can be used to determine the glass transition temperature (Tg) of a polymer, a critical parameter for determining its processing conditions and performance.
Limitations: DSC is not suitable for studying materials that undergo significant degradation or decomposition during the experiment. Also, the interpretation of DSC data can sometimes be complex and require careful consideration of the instrument’s baseline and sample preparation. The results can be affected by factors like heating rate and sample size, requiring standardization and careful control.
Q 5. Explain the principles of Thermogravimetric Analysis (TGA) and its relevance to biomaterial degradation.
Thermogravimetric Analysis (TGA) is a thermal analysis technique that measures the weight change of a sample as a function of temperature or time under a controlled atmosphere. This weight change is usually due to decomposition, oxidation, or other thermally induced reactions.
In biomaterial analysis, TGA is extremely useful for studying the degradation behavior of materials. By monitoring the weight loss of a biomaterial as it is heated, we can determine the temperature ranges at which degradation occurs, the kinetics of degradation, and the amount of residual mass remaining after degradation. This information is critical for assessing the long-term stability and biocompatibility of the material within the body.
For example, TGA can be used to study the degradation of biodegradable polymers used in drug delivery systems or tissue engineering scaffolds. The rate of weight loss can indicate how quickly the polymer will degrade in the body, which is crucial for designing devices with appropriate lifetimes. The residual mass after degradation can inform about any inorganic components remaining after the organic components degrade.
Q 6. How would you determine the mechanical properties (e.g., tensile strength, Young’s modulus) of a biomaterial?
The mechanical properties of a biomaterial, such as tensile strength and Young’s modulus, are typically determined using tensile testing. In this technique, a sample of the biomaterial is subjected to a controlled tensile load, and its elongation is measured. The stress-strain curve obtained from this test is then used to calculate the material’s mechanical properties.
Tensile strength represents the maximum stress a material can withstand before it breaks. Young’s modulus (or elastic modulus) is a measure of the material’s stiffness, representing its resistance to deformation under stress. Other properties such as yield strength (stress at which plastic deformation begins), and elongation at break (the extent of elongation before failure) can also be determined from the stress-strain curve.
The specific test method and sample preparation will depend on the type of biomaterial being tested. For example, polymers might be tested as films or fibers, while ceramics or metals might be tested as bars or cylinders. Precise sample preparation and controlled testing conditions are crucial to obtaining reliable and reproducible results, ensuring the accuracy and validity of mechanical testing data.
Q 7. Describe different techniques for evaluating the biocompatibility of a biomaterial.
Biocompatibility evaluation is crucial for ensuring the safety and efficacy of biomaterials. Several techniques are employed to assess this, ranging from in vitro (cell culture-based) to in vivo (animal model-based) studies.
In vitro methods typically involve exposing cells to extracts from the biomaterial or direct cell-material contact. Cell viability assays (MTT, WST-1) assess cell survival and proliferation, while assays like cytokine release analysis evaluate the inflammatory response triggered by the material. Cytotoxicity testing provides crucial information on the toxic effects of the material on cells.
In vivo methods involve implanting the biomaterial in an animal model and observing its effects on the surrounding tissues. This can involve histological analysis of tissue sections to assess inflammation, foreign body response, and tissue integration. Imaging techniques like micro-CT can monitor the material’s behavior and interaction with the surrounding tissue over time.
Other methods include protein adsorption studies to assess how proteins interact with the biomaterial surface, and blood compatibility studies that examine the interaction of the biomaterial with blood components to evaluate its potential for thrombogenicity (blood clot formation). The selection of appropriate methods depends on the intended application of the biomaterial and regulatory requirements.
Q 8. Explain the concept of surface roughness and its impact on cell-material interactions.
Surface roughness describes the texture of a material’s surface, encompassing the peaks and valleys at the microscopic level. It’s typically quantified using parameters like Ra (average roughness) and Rz (maximum peak-to-valley height). This seemingly minor detail significantly influences cell-material interactions because cells are incredibly sensitive to their immediate environment.
Think of it like this: a smooth surface (low Ra) provides a less-challenging environment for cell adhesion, spreading, and proliferation. Cells might adhere uniformly, spreading across the surface easily. Conversely, a rough surface (high Ra) presents numerous crevices and protrusions that can either hinder or enhance cell attachment depending on the cell type and the surface chemistry. Some cells may prefer to anchor themselves in these crevices, while others may find it difficult to adhere stably. This translates directly into the functionality of a biomaterial implant – for example, a rough titanium implant might promote stronger bone integration (osseointegration) due to enhanced cell anchorage compared to a smoother one. The surface roughness is also crucial for designing scaffolds for tissue engineering. A rough scaffold with an interconnected pore network allows for better cell infiltration and tissue growth.
The impact extends beyond simple attachment; surface roughness affects cell morphology, differentiation, and ultimately the overall biocompatibility and functionality of the implanted biomaterial. For instance, a rough surface might promote osteoblast (bone-forming cell) differentiation leading to better bone regeneration but could also trigger inflammation in some contexts.
Q 9. How do you assess the degradation rate of a biodegradable polymer?
Assessing the degradation rate of a biodegradable polymer involves tracking its mass loss and/or changes in its physical and chemical properties over time. Several techniques are used, each with its own strengths and limitations.
- Mass Loss Measurement: Samples are weighed at regular intervals during incubation in a biologically relevant medium (e.g., phosphate-buffered saline, or a simulated body fluid). The change in mass is an indicator of degradation. Simple, but can underestimate degradation if the products are soluble.
- Mechanical Testing: Tensile strength, compressive strength, and modulus are measured periodically. Degradation leads to a decrease in mechanical properties.
- Visual Inspection: Changes in the physical appearance, such as cracking, swelling, or erosion, can provide qualitative insights into the degradation process.
- Chemical Analysis: Techniques like FTIR (Fourier Transform Infrared Spectroscopy) or NMR (Nuclear Magnetic Resonance) spectroscopy can detect changes in the chemical structure of the polymer as it degrades, showing bond breaking and the formation of degradation products.
- Size Exclusion Chromatography (SEC): This technique analyzes the molecular weight distribution of the polymer during degradation. A decrease in the average molecular weight indicates chain scission during degradation.
Choosing the appropriate technique often depends on the specific polymer and its application. For instance, measuring changes in mechanical properties is particularly important when considering the polymer’s use in load-bearing implants. Combining multiple methods provides a comprehensive understanding of degradation kinetics and mechanisms.
Q 10. What are the key factors to consider when selecting a characterization technique for a specific biomaterial?
Selecting the right characterization technique is paramount in biomaterials science. It depends on several crucial factors:
- The property of interest: Do you need to assess surface roughness, mechanical properties, chemical composition, degradation rate, or biological interactions?
- The biomaterial’s nature: Is it a polymer, ceramic, metal, composite? Different techniques are suited for different material types. For example, electron microscopy is ideal for high-resolution imaging of nanostructured materials, while X-ray diffraction is excellent for determining the crystal structure of ceramics.
- The required sensitivity and resolution: The desired level of detail dictates the choice of technique. For instance, if you need atomic-level resolution, you might employ techniques like atomic force microscopy (AFM) or transmission electron microscopy (TEM).
- The sample’s size and shape: The technique should be compatible with the available sample size and geometry.
- Cost and accessibility: The budget and availability of equipment also influence the decision.
For example, if you are interested in the mechanical properties of a polymer scaffold for bone tissue engineering, tensile testing would be an appropriate choice. If you are interested in the cellular response, you might use cell viability assays and microscopy. Often a combination of techniques is needed to fully characterize a biomaterial.
Q 11. Explain the principles of contact angle measurements and their significance in biomaterials science.
Contact angle measurement is a simple yet powerful technique used to assess the wettability of a biomaterial’s surface. It’s based on the principle of observing the angle formed at the three-phase boundary where a liquid droplet (e.g., water) sits on a solid surface (the biomaterial) in air.
A high contact angle (above 90°) indicates low wettability or hydrophobicity (water repelling), while a low contact angle (below 90°) indicates high wettability or hydrophilicity (water-loving). The contact angle directly reflects the surface energy and interactions between the liquid and the solid surface.
In biomaterials science, wettability is critical because it greatly influences cell adhesion, protein adsorption, and overall biocompatibility. For example, a highly hydrophobic surface might inhibit cell adhesion, while a hydrophilic surface may promote cell attachment and spreading, as seen in many commercially available cell culture plates. Furthermore, the design of implants often considers wettability to achieve desired interactions with surrounding tissues. Thus, contact angle measurements can provide essential insight into the biomaterial’s interaction with the biological environment.
Q 12. How can you determine the porosity of a biomaterial scaffold?
Determining the porosity of a biomaterial scaffold is crucial as pore size and interconnectivity influence cell infiltration, nutrient transport, and overall tissue integration. Several methods are available:
- Image Analysis: Microscopic images (SEM, micro-CT) of the scaffold are analyzed using image processing software. This allows for the quantification of pore size distribution and porosity. This is a popular method but can be time-consuming and depend heavily on image quality and resolution.
- Mercury Intrusion Porosimetry (MIP): This technique involves forcing mercury into the pores of the scaffold under pressure. The volume of mercury intruded at different pressures provides information on pore size distribution and total porosity. However, this is destructive and may not be suitable for all materials.
- Archimedes’ Principle: This method involves measuring the weight of the dry scaffold, its weight in water, and its apparent weight when submerged. The difference between these measurements can be used to calculate the scaffold’s porosity. This is a simple method but assumes uniform density and shape and may not capture the full complexity of porous structures.
- Gas Pycnometry: This method uses a gas (typically helium) to determine the true volume of the solid matrix, which can then be used to calculate porosity.
The choice of method depends on the scaffold’s characteristics (e.g., pore size, material, fragility) and the required level of detail. Often, a combination of methods is used to obtain a more complete picture.
Q 13. Describe different methods for analyzing the chemical composition of biomaterials.
Analyzing the chemical composition of biomaterials is fundamental to understanding their properties and biocompatibility. A variety of techniques are employed:
- Fourier Transform Infrared Spectroscopy (FTIR): This technique identifies the functional groups present in the material by analyzing its absorption of infrared light. It’s a powerful tool for identifying polymers and other organic materials.
- X-ray Photoelectron Spectroscopy (XPS): This surface-sensitive technique provides information on the elemental composition and chemical states of atoms at the surface of the material. It’s particularly useful for analyzing surface modifications and coatings.
- Energy-Dispersive X-ray Spectroscopy (EDS): Combined with electron microscopy (SEM, TEM), EDS provides elemental mapping of the material’s composition at high spatial resolution. This is useful for determining the distribution of elements in composite materials.
- Nuclear Magnetic Resonance (NMR) Spectroscopy: This technique provides detailed information on the molecular structure and dynamics of organic materials. It’s especially useful for characterizing polymers and other organic biomaterials.
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS): This technique is used to determine the concentration of trace elements in biomaterials. It’s particularly important for detecting potential contaminants.
- Gas Chromatography-Mass Spectrometry (GC-MS): This technique separates and identifies volatile organic compounds and is often used to analyze degradation products or residual solvents in biomaterials.
The choice of technique depends on the specific biomaterial and the information sought. Often, a combination of techniques is needed to obtain a complete understanding of its chemical composition.
Q 14. Explain the importance of statistical analysis in biomaterials characterization.
Statistical analysis plays a vital role in biomaterials characterization. Biological systems exhibit inherent variability, and biomaterial responses are influenced by various factors, such as cell culture conditions and material processing techniques. Therefore, relying solely on single measurements can lead to misleading conclusions.
Statistical analysis allows us to:
- Quantify variability: It provides metrics such as standard deviation and variance, which describe the spread of data around the mean. This highlights the level of uncertainty in our measurements.
- Determine statistical significance: Techniques like t-tests and ANOVA are used to assess if differences between groups (e.g., different biomaterials or treatments) are statistically significant or just due to random variation.
- Identify outliers: Statistical methods can help detect and remove outliers, data points that deviate significantly from the rest of the dataset. Outliers can skew results and affect the interpretation of findings.
- Correlate different properties: Correlation analysis allows us to investigate the relationships between different properties of the biomaterial (e.g., surface roughness and cell adhesion). This is a cornerstone of gaining better insights to how various characteristics interplay.
- Build predictive models: Regression analysis can be used to build models that predict the behavior of the biomaterial based on its properties. This can help in optimizing biomaterial design and properties.
Proper statistical analysis ensures robust and reliable conclusions, leading to a better understanding of biomaterial behavior and its implications for biomedical applications.
Q 15. What are the challenges associated with characterizing biomaterials in vivo?
Characterizing biomaterials in vivo presents unique challenges compared to in vitro studies. The biggest hurdle is the complexity of the biological environment. Think of it like trying to understand a single instrument in a full orchestra – you’re not just dealing with the instrument itself, but also how it interacts with all the other instruments and the conductor (the body’s complex regulatory systems).
- Immune response: The body’s natural defense mechanisms can significantly alter the biomaterial’s properties and performance. For example, a biomaterial might trigger inflammation, fibrosis (scar tissue formation), or even rejection.
- Degradation and remodeling: Biomaterials degrade at different rates in vivo, affected by factors like pH, enzymatic activity, and mechanical forces. Predicting this degradation accurately is difficult.
- Ethical considerations: Animal models are often necessary for in vivo studies, raising ethical concerns regarding animal welfare and the need for rigorous experimental design to minimize harm.
- Technical difficulties: Imaging and sampling in vivo can be technically challenging, often requiring sophisticated techniques like micro-CT scanning or minimally invasive surgical procedures. Real-time monitoring is especially difficult.
- Variability: Biological systems are inherently variable; individual responses to biomaterials can differ greatly. This makes it crucial to have large sample sizes and robust statistical analysis.
For example, a seemingly biocompatible material in cell culture might elicit a strong inflammatory response in vivo. Therefore, in vivo characterization is essential, even after successful in vitro testing, to ensure safety and efficacy.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you interpret results from a cytotoxicity assay?
Cytotoxicity assays assess the toxic effects of a material on cells. The results aren’t simply ‘toxic’ or ‘non-toxic’ but rather provide a quantitative measure of cell viability and function. Imagine it as a report card for your biomaterial – it tells you how well it’s doing in terms of cell health.
Interpretation involves analyzing several parameters:
- Cell viability: This is usually expressed as a percentage of live cells compared to a control (untreated cells). A significant reduction in viability indicates cytotoxicity.
- Metabolic activity: Assays like MTT or resazurin measure the metabolic activity of cells, providing an indication of their functional state. Reduced metabolic activity reflects impaired cell function, even if the number of cells remains relatively high.
- Morphological changes: Microscopic examination can reveal changes in cell shape, size, and organization due to the biomaterial. Rounded, detached cells, for example, often signify cytotoxicity.
- Cell death mechanisms: Some assays differentiate between apoptosis (programmed cell death) and necrosis (uncontrolled cell death), offering more detailed insights into the cytotoxic mechanism.
A combination of these parameters allows a comprehensive interpretation. For example, a material may show high cell viability but reduced metabolic activity, suggesting that it impacts cell function rather than causing immediate cell death. Careful consideration of positive and negative controls is vital for accurate interpretation and the selection of appropriate statistical tests is crucial for ensuring the reliability of any conclusions.
Q 17. Describe the principles of Dynamic Mechanical Analysis (DMA).
Dynamic Mechanical Analysis (DMA) measures a material’s viscoelastic properties – its ability to deform elastically (like a rubber band) and viscously (like honey) – as a function of temperature, frequency, or time. Think of it as a stress test for your material, revealing how it responds to different forces and conditions.
DMA applies an oscillating force to a sample and measures its response. The key parameters measured are:
- Storage modulus (E’): Represents the elastic component of the material’s response. A high E’ indicates a stiffer material.
- Loss modulus (E”): Represents the viscous component. A high E” indicates higher energy dissipation (more ‘damping’).
- Tan δ (E”/E’): The ratio of loss modulus to storage modulus. It provides information on the damping characteristics of the material – a high tan δ signifies a more viscous material.
By varying temperature or frequency, DMA reveals how these properties change. For example, a biomaterial’s glass transition temperature (Tg), the temperature at which it transitions from a glassy to a rubbery state, can be determined using DMA. This is crucial for understanding its behavior in the body, as temperature changes can significantly affect its mechanical properties.
DMA is frequently used to characterize hydrogels, polymers, and other biomaterials, providing critical information for applications ranging from drug delivery systems to tissue engineering scaffolds.
Q 18. How would you assess the bioactivity of a biomaterial?
Assessing bioactivity involves determining how a biomaterial interacts with biological systems, triggering specific cellular responses. It’s more than just biocompatibility (absence of toxicity); it’s about promoting beneficial interactions.
Methods for assessing bioactivity include:
- Cell adhesion and proliferation assays: These measure the ability of cells to attach to and grow on the biomaterial’s surface. A high level of cell adhesion and proliferation indicates good bioactivity.
- Gene expression analysis: This examines changes in gene expression patterns in cells in contact with the biomaterial. Specific genes associated with cell differentiation, extracellular matrix production, or bone formation can be monitored to assess the biomaterial’s ability to direct cellular behavior.
- Protein adsorption studies: Analyzing the types and amounts of proteins that adsorb onto the material’s surface helps understand its initial interactions with biological fluids. Some proteins can promote cell attachment and others may inhibit it.
- In vivo studies: Implanting the biomaterial in a living organism allows assessment of its effects on tissue regeneration, bone formation, or other desired biological processes.
- Mineralization assays: For bone tissue engineering applications, assessing the biomaterial’s ability to induce calcium phosphate deposition is a key indicator of bioactivity.
For instance, a bioactive glass scaffold used in bone regeneration would be assessed by its ability to induce osteoblast (bone-forming cell) adhesion, proliferation, differentiation, and the formation of new bone tissue in vivo.
Q 19. Explain the differences between in vitro and in vivo biomaterial testing.
In vitro and in vivo biomaterial testing represent different stages of evaluation, each offering unique insights but with limitations.
In vitro testing involves evaluating the biomaterial’s properties in a controlled laboratory setting, typically using cells or tissues cultured in dishes or flasks. Think of it as a simplified, controlled environment like a greenhouse for your biomaterial. It’s relatively inexpensive, easy to control, and allows for high throughput screening. However, it lacks the complexity of the living organism, meaning results might not fully predict in vivo performance.
In vivo testing involves evaluating the material in a living organism (animal models are commonly used). This represents the ‘real-world’ scenario, providing a more accurate assessment of the material’s long-term performance and interaction with the body’s complex environment. However, it’s more expensive, time-consuming, ethically complex, and involves significant biological variability.
In essence, in vitro tests are useful for preliminary screening and identifying promising candidates, whereas in vivo tests are necessary to confirm their efficacy and safety before clinical translation. Ideally, a tiered approach involving both in vitro and in vivo testing is crucial for a comprehensive biomaterial evaluation.
Q 20. What are some common artifacts encountered in microscopy techniques and how can they be minimized?
Microscopy techniques, while powerful, are susceptible to artifacts – unwanted features that distort the image and misrepresent the sample. These can be caused by sample preparation, the microscopy technique itself, or image processing.
Common artifacts and their minimization strategies:
- Sample preparation artifacts:
- Drying artifacts: Shrinkage or distortion of the sample during drying can be minimized by using critical point drying or freeze-drying techniques.
- Sectioning artifacts: Damage to the sample during sectioning (e.g., compression, tearing) can be reduced by using sharper blades and optimizing sectioning parameters.
- Fixation artifacts: Improper fixation can alter the sample’s structure. Optimized fixation protocols are necessary.
- Microscopy-specific artifacts:
- Spherical aberration: Distortion due to differences in refractive index can be minimized by using immersion oil (optical microscopy) or appropriate sample preparation (electron microscopy).
- Chromatic aberration: Color fringing due to different wavelengths of light can be reduced by using apochromatic objectives.
- Beam damage (Electron Microscopy): High-energy electron beams can damage the sample. Lowering the beam intensity or using cryo-EM can minimize damage.
- Image processing artifacts:
- Noise: Random variations in pixel intensity can be reduced by using noise reduction filters, but excessive filtering can lead to loss of detail.
- Artifacts from image processing algorithms: Careful selection and application of image processing algorithms are crucial to avoid introducing artifacts.
Careful attention to sample preparation, meticulous experimental design, and proper control of imaging parameters are crucial for minimizing artifacts and obtaining accurate representations of the biomaterial’s structure.
Q 21. Describe your experience with image analysis software for biomaterials characterization.
I have extensive experience using image analysis software for quantifying various aspects of biomaterial characterization. My expertise spans several software packages including ImageJ/Fiji, CellProfiler, and Imaris. These tools have been instrumental in my research in quantifying parameters such as:
- Cell adhesion and spreading: Analyzing the area and perimeter of cells adhered to biomaterial surfaces.
- Porosity and pore size distribution: Quantifying the porosity and pore size of porous scaffolds using various thresholding and measurement techniques within ImageJ/Fiji.
- Fiber orientation and alignment: Analyzing the orientation and alignment of fibers in engineered tissues using ImageJ/Fiji’s plugin offerings and bespoke scripts.
- 3D reconstruction and quantification: Utilizing Imaris to create 3D reconstructions of samples from confocal or electron microscopy data and then calculating volumes and distances of different structures within the 3D model.
- Co-localization studies: Determining the spatial relationship between different molecules or structures within cells or tissues using software like CellProfiler.
I’m proficient in writing macros and scripts within these software packages to automate image analysis workflows, ensuring reproducibility and consistency. I am also familiar with the limitations of automated image analysis and always employ manual validation to ensure accuracy and correct for any bias. For example, in analyzing cell density, I always conduct manual checks to identify and remove artifacts and ensure correct counting of clustered cells. My strong programming skills enable me to adapt and modify existing plugins or develop new ones to address specific research needs.
Q 22. How would you troubleshoot a failed experiment in biomaterials characterization?
Troubleshooting a failed biomaterials characterization experiment involves a systematic approach. Think of it like detective work – you need to gather clues and eliminate possibilities. First, I’d meticulously review the experimental protocol, checking for any deviations from the established procedure. This includes verifying the accuracy of reagent preparation, instrument calibration, and sample handling. Common issues include incorrect sample preparation (e.g., insufficient drying, contamination), instrument malfunctions (e.g., faulty detectors, incorrect settings), or errors in data acquisition and processing.
Next, I’d analyze the raw data for any anomalies. Are there unexpected peaks in spectroscopic data? Are there inconsistencies in the measurements? This might point towards problems with the sample, the instrument, or the experimental design. If the problem persists, I would then systematically test each component of the experiment individually. For example, I might repeat the experiment using a different batch of reagents, a different instrument, or a different sample preparation method to isolate the source of the error. Finally, I’d document all troubleshooting steps and findings to prevent future occurrences. A well-maintained lab notebook is critical for this process.
For instance, if I’m performing cell viability assays and get unexpectedly low viability, I would first check for contamination (bacterial or fungal), then assess the cell seeding density and culture conditions (temperature, media), and then examine the handling of the biomaterial sample (sterility, potential cytotoxic effects of the sample itself). A control experiment with a known biocompatible material would also be crucial.
Q 23. Explain your experience with different types of spectroscopies (e.g., FTIR, Raman).
I have extensive experience with various spectroscopic techniques, particularly FTIR (Fourier Transform Infrared Spectroscopy) and Raman spectroscopy. These are invaluable tools for characterizing the chemical composition and structure of biomaterials. FTIR provides information on functional groups present in a material by analyzing the absorption of infrared light. This helps identify polymer types, the presence of crosslinks, and the extent of crystallinity. Think of it like a fingerprint for the molecules in your sample. Raman spectroscopy, on the other hand, relies on the inelastic scattering of light to provide complementary structural information, often revealing subtle differences that FTIR might miss. It’s particularly useful for studying water content and molecular interactions.
In my previous role, I used FTIR to characterize the degree of crosslinking in a collagen-based hydrogel for tissue engineering. By comparing the FTIR spectra of the hydrogel before and after crosslinking, we could quantify the changes in the amide bands, indicating successful crosslinking. In another project, I employed Raman microscopy to map the distribution of different drug molecules within a polymeric scaffold for drug delivery. This gave us spatial information about drug release and penetration into the scaffold.
Beyond FTIR and Raman, my experience also includes other spectroscopic methods like UV-Vis spectroscopy, which is useful for determining the concentration of molecules or detecting chromophores in biomaterials, and X-ray photoelectron spectroscopy (XPS), which is incredibly powerful for determining the surface elemental composition and chemical states, critical for understanding surface modifications and their impact on biocompatibility.
Q 24. How do you ensure the accuracy and reproducibility of your biomaterials characterization results?
Ensuring the accuracy and reproducibility of results in biomaterials characterization demands rigorous attention to detail at every stage. It’s a multifaceted approach that starts with proper experimental design and extends to data analysis and reporting.
- Standardization: Using standardized protocols and validated methods is crucial. This includes following established guidelines and using certified reference materials whenever possible.
- Calibration and Validation: Regular calibration of instruments is essential. Validation experiments using known samples help assess the accuracy and precision of our measurements. Internal validation with multiple runs to assess inter-operator and intra-operator variability and external validation using previously published data or a reference laboratory is beneficial.
- Controls: Incorporating appropriate controls, such as positive and negative controls, helps rule out artifacts and ensure that the observed effects are due to the biomaterial and not external factors.
- Sample Preparation: Consistent and meticulous sample preparation is vital. Using standardized protocols to handle, process, and store samples minimizes variability.
- Data Analysis: Statistical analysis is crucial for evaluating the significance of results and assessing reproducibility. This might involve ANOVA, t-tests, or regression analysis.
- Documentation: Maintaining detailed records of all experimental steps, data, and analysis is essential for reproducibility and transparency.
For example, to minimize variability in cell adhesion assays, I would use standardized cell culture protocols, ensure consistent cell seeding density, and always maintain the same incubation conditions. Each experiment would be conducted in triplicate, with statistical analysis performed to confirm the significance of any observed differences.
Q 25. Describe your experience with data analysis and presentation.
Data analysis and presentation are integral parts of my work. I’m proficient in various statistical software packages (e.g., GraphPad Prism, SPSS, R), which I use to perform statistical analyses, generate graphs, and create comprehensive reports. I can effectively present complex data in a clear and concise manner using a variety of tools, including scientific figures, tables, and presentations.
My approach to data analysis begins with a thorough understanding of the data’s context and the research question. I choose appropriate statistical methods and critically assess the results, taking into account potential sources of error or bias. I firmly believe in transparent data presentation; I avoid misleading graphical representations and ensure that all results are clearly labeled and explained. My presentations are designed to effectively communicate my findings to both technical and non-technical audiences.
For example, in a recent project, I used R to analyze the results of a mechanical testing experiment and created a publication-ready figure showing the stress-strain curves for different biomaterials. I also used Prism to perform statistical tests to compare the mechanical properties of these materials and clearly presented this analysis in a concise table in my final report. This demonstrated not only the data but also the statistical significance of our findings.
Q 26. What are the regulatory requirements for biomaterial characterization in medical devices?
Regulatory requirements for biomaterial characterization in medical devices are stringent and vary depending on the specific application and regulatory body (e.g., FDA in the US, EMA in Europe). However, several overarching principles apply. Manufacturers must demonstrate the biocompatibility and safety of their devices through comprehensive testing. This typically involves characterizing the material’s physical, chemical, and biological properties. Key aspects include:
- Chemical Characterization: Identifying all components, impurities, and extractables/leachables. This may require techniques like FTIR, GC-MS, and HPLC.
- Physical Characterization: Determining mechanical properties (e.g., tensile strength, elasticity), degradation rate, and morphology (e.g., surface roughness, pore size).
- Biological Characterization: Assessing cytotoxicity, genotoxicity, sensitization, and other relevant biological endpoints using in vitro and in vivo studies. This often involves cell culture assays and animal studies.
- Sterility: Demonstrating sterility through appropriate sterilization methods and testing.
The specific tests required are outlined in ISO standards and regulatory guidelines. For example, ISO 10993 provides guidance on biocompatibility testing, while specific guidelines exist for different device classifications. Failure to meet these requirements can lead to delays or rejection of medical device approvals.
Q 27. Explain your understanding of biomaterial-tissue interactions.
Biomaterial-tissue interactions are complex and crucial for determining a biomaterial’s success or failure in a living system. These interactions encompass a wide range of processes, starting from initial protein adsorption at the biomaterial surface. The surface chemistry and topography play significant roles in determining which proteins adsorb and how they orient themselves. This adsorbed protein layer acts as an intermediary between the biomaterial and the cells.
Cells then interact with this protein layer via specific receptors on their surface. This interaction dictates cell adhesion, spreading, proliferation, and differentiation. The biological response can range from integration and tissue regeneration (ideal for implants) to inflammation, fibrosis, or even rejection (undesirable outcomes). Factors influencing these interactions include the material’s surface properties (wettability, charge, roughness), degradation products, and the host’s immune response.
For example, a biomaterial with a hydrophilic surface may promote protein adsorption that favors cell adhesion and tissue integration, while a hydrophobic surface might elicit an adverse immune response. Similarly, the release of degradation products from a biomaterial can either aid in tissue regeneration or trigger inflammation. Understanding these interactions is key to designing biomaterials that are safe, effective, and biocompatible.
Q 28. How would you design an experiment to investigate the effect of surface modification on cell adhesion?
To investigate the effect of surface modification on cell adhesion, I would design a controlled experiment using a well-defined biomaterial and a relevant cell type. The experiment would involve several key steps:
- Material Selection and Modification: Choose a suitable biomaterial (e.g., titanium, a polymer) and apply different surface modifications (e.g., plasma treatment, coating with a bioactive molecule). It’s important to have a control group with the unmodified material.
- Cell Culture: Select an appropriate cell type relevant to the intended application (e.g., osteoblasts for bone implants, fibroblasts for skin grafts). Ensure that the cells are healthy and consistently cultured before the experiment.
- Cell Seeding and Incubation: Seed the cells onto the modified and unmodified biomaterials. Maintain consistent culture conditions (temperature, humidity, CO2 concentration) during the incubation period.
- Adhesion Assays: Quantify cell adhesion using appropriate assays such as cell counting (using a hemocytometer or automated cell counter after washing away unattached cells), live/dead staining to differentiate between attached live and dead cells, or more sophisticated techniques like immunofluorescence to detect focal adhesion markers.
- Statistical Analysis: Perform appropriate statistical analysis (e.g., t-tests, ANOVA) to determine if there are significant differences in cell adhesion between the modified and unmodified materials. The experiment should be conducted in at least triplicate to ensure reproducibility.
The data obtained from these assays would provide valuable insights into how different surface modifications affect cell adhesion. For example, if the surface modification increases cell adhesion, this could suggest a positive impact on tissue integration. Conversely, decreased adhesion could suggest the modification might hinder the material’s performance.
Key Topics to Learn for Biomaterials Characterization Interview
- Surface Characterization Techniques: Understanding methods like XPS, SEM, AFM, and contact angle goniometry; their principles, applications in biomaterials analysis (e.g., surface roughness, wettability, chemical composition), and limitations.
- Mechanical Properties: Tensile testing, compression testing, nanoindentation; relating mechanical properties to biomaterial design and performance (e.g., implant stability, tissue integration); interpreting stress-strain curves and understanding relevant parameters.
- Biocompatibility and Cytotoxicity Assays: In vitro and in vivo testing methods; understanding cell viability, proliferation, and differentiation assays; interpreting data related to biocompatibility and toxicity; discussing the importance of appropriate controls.
- Degradation and Bioresorbability: Mechanisms of biomaterial degradation (e.g., hydrolysis, enzymatic degradation); in vitro and in vivo degradation studies; impact of degradation products on the surrounding environment; selecting appropriate biomaterials based on desired degradation profiles.
- Imaging Techniques: Confocal microscopy, optical coherence tomography (OCT), micro-CT; their use in visualizing biomaterials in vivo and in vitro; analyzing 3D structures and cellular interactions with biomaterials.
- Data Analysis and Interpretation: Statistical analysis of experimental data; error analysis and uncertainty quantification; effectively presenting and interpreting results in a scientific context.
- Specific Biomaterial Classes: Deep understanding of the characterization techniques relevant to your specific area of interest (e.g., polymers, ceramics, metals, composites).
Next Steps
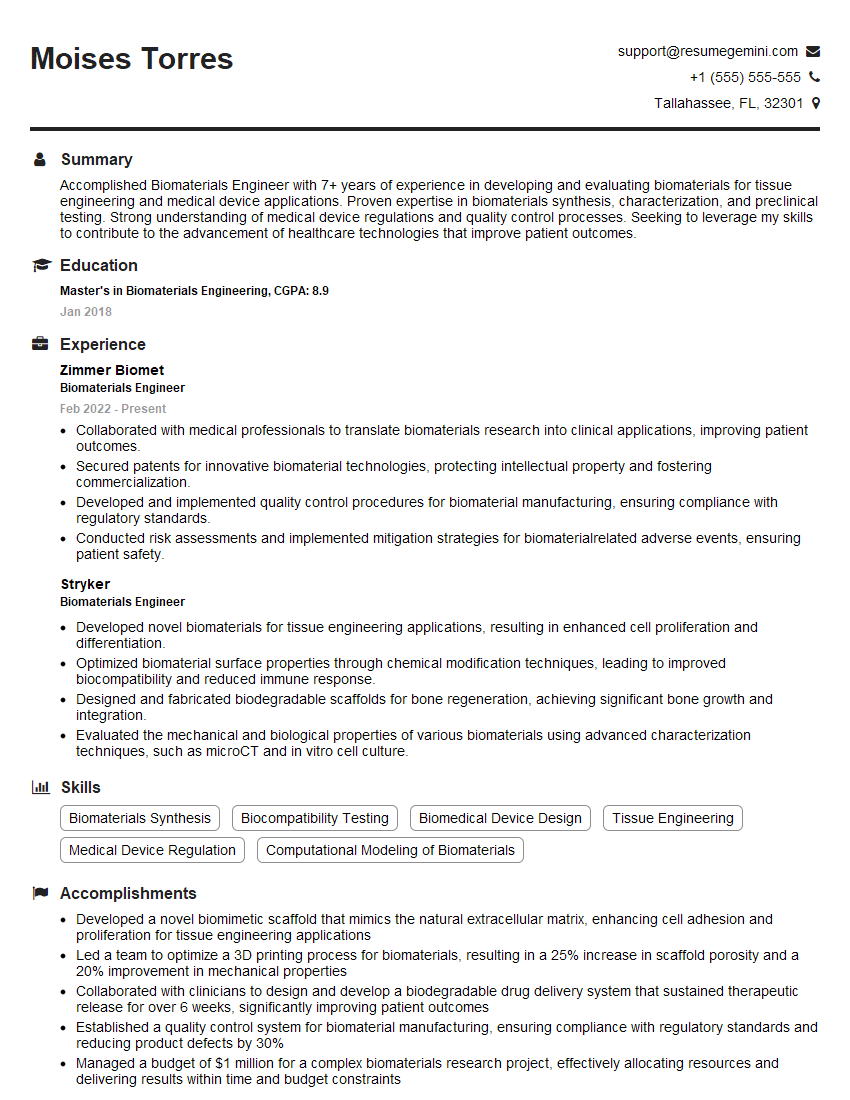
Mastering Biomaterials Characterization is crucial for career advancement in this rapidly evolving field. A strong understanding of these techniques allows you to contribute meaningfully to research, development, and regulatory affairs within the biomedical industry. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to your unique qualifications. Examples of resumes tailored to Biomaterials Characterization are available, demonstrating how to showcase your expertise and secure that dream interview.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good