Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Biomedical Device Clinical Trials Management interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Biomedical Device Clinical Trials Management Interview
Q 1. Explain the phases of a biomedical device clinical trial.
Biomedical device clinical trials typically follow a phased approach, mirroring the drug development process but with specific considerations for device safety and efficacy. These phases aren’t always strictly sequential; some devices may skip phases or combine them.
- Phase 1: This initial phase focuses on safety. A small group of healthy volunteers are given the device to evaluate its safety profile, tolerability, and identify potential side effects. For example, a new type of cardiac implant might be tested in a small group to assess its biocompatibility and the body’s response to the material.
- Phase 2: This phase assesses the device’s effectiveness (efficacy) and further evaluates safety in a larger group of patients with the target condition. Data collected helps refine the device design, dosage (if applicable), and treatment protocols. Imagine a new insulin pump – Phase 2 would involve a larger number of diabetic patients to assess how well it manages blood glucose levels.
- Phase 3: This large-scale trial confirms the device’s efficacy, compares it to existing treatments, and monitors its long-term safety and effectiveness. It helps establish the device’s benefit-risk profile. This might involve a multi-center trial with hundreds or thousands of patients using the new insulin pump compared to a standard pump.
- Phase 4: Post-market surveillance. This phase occurs after the device receives regulatory approval. It involves ongoing monitoring of the device’s safety and effectiveness in a broader population. Data collected in Phase 4 informs ongoing refinements and potential updates to the device’s design or use.
Q 2. Describe the difference between a prospective and retrospective study.
The key difference lies in the timing of data collection.
- Prospective studies collect data after the study begins. Participants are enrolled, and data is gathered as events unfold. This allows for more controlled data collection and minimizes bias related to pre-existing conditions, offering a clearer causal relationship.
- Retrospective studies use existing data. Researchers analyze data that was collected previously, often from medical records. This is faster and cheaper but is limited by the quality and completeness of the existing data. For instance, analyzing medical records to see the long-term outcomes of patients who received a particular type of knee implant would be a retrospective study.
Imagine a study investigating a new wound dressing. A prospective study would recruit patients, apply the dressing, and monitor wound healing progress. A retrospective study would look at existing patient charts, identifying those who received similar wound dressings in the past, and then analyze their healing outcomes.
Q 3. What are the key regulatory requirements for biomedical device clinical trials (e.g., FDA, ISO)?
Regulatory requirements for biomedical device clinical trials are stringent and vary depending on the device’s risk classification. Key agencies include the FDA (in the US) and organizations that align with ISO standards internationally.
- FDA (US): The FDA requires Investigational Device Exemptions (IDEs) for most investigational devices before clinical trials can begin. These IDEs outline the trial’s protocol, ensuring it meets safety and ethical standards. They also govern the reporting of adverse events and overall trial conduct. Compliance is crucial to avoid delays or rejection of the device’s market approval.
- ISO (International): ISO standards, such as ISO 14155 (clinical investigation of medical devices), provide a framework for good clinical practice (GCP). Adherence to GCP is essential for the integrity and reliability of the data generated in a clinical trial. This ensures consistency and quality across different countries and regulatory bodies.
Compliance with these regulations is paramount to ensure patient safety and the reliability of the trial results.
Q 4. How do you ensure patient safety in a clinical trial?
Patient safety is the top priority in any clinical trial. This involves a multi-faceted approach:
- Rigorous Protocol Design: The clinical study protocol must meticulously outline procedures to minimize risks. This includes careful selection of participants, appropriate monitoring, and clear escalation pathways for adverse events.
- Independent Ethics Committee (IEC) Review: An independent review board assesses the study design, ensuring it protects participant rights and well-being before the trial starts and throughout.
- Informed Consent: Participants must provide informed consent, fully understanding the risks and benefits of participation.
- Data Monitoring Committee (DMC): A DMC may oversee the trial, regularly reviewing safety data to detect any emerging concerns and recommend adjustments to the trial or its termination if necessary.
- Adverse Event Reporting: A robust system for reporting and investigating adverse events and serious adverse events is essential. This ensures timely interventions and identification of any serious safety signals.
Imagine a trial for a new heart valve. Thorough screening of participants would be essential to minimize risks. Regular monitoring of patients post-procedure and stringent reporting requirements for any complications would be crucial.
Q 5. What are the essential components of a clinical study protocol?
A clinical study protocol is the bible of the trial, outlining every aspect of its conduct. Key components include:
- Background & Objectives: A clear statement of the rationale, study aims, and hypotheses.
- Study Design: Description of the study type (e.g., randomized controlled trial, observational study), participant selection criteria, and data collection methods.
- Statistical Considerations: Details on sample size calculation, statistical analysis plans, and primary and secondary endpoints.
- Patient Population: Precise inclusion and exclusion criteria for participants to ensure the study population is well-defined.
- Procedures: Detailed step-by-step instructions for all aspects of the trial, including device implantation, data collection, and follow-up procedures.
- Data Management: Plan for data collection, storage, and management to ensure data integrity and confidentiality.
- Safety Monitoring Plan: A detailed plan for identifying, reporting, and managing adverse events.
A well-written protocol leaves no room for ambiguity, ensuring everyone involved understands their roles and responsibilities.
Q 6. Explain the process of informed consent.
Informed consent is a fundamental ethical principle in clinical research. It ensures that participants voluntarily agree to participate in a study after being fully informed about all aspects of the trial.
The process usually involves:
- Pre-Consent Discussion: A detailed explanation of the study’s purpose, procedures, potential risks and benefits, and participant rights. The investigator answers all questions to ensure the participant understands.
- Consent Form: A written document summarizing all information discussed, to which the participant signs, indicating their voluntary agreement.
- Ongoing Communication: Maintaining open communication throughout the trial, allowing participants to withdraw at any time without penalty.
It’s crucial that the informed consent process is conducted ethically and respectfully, ensuring participants aren’t coerced or pressured into participation. For example, in a trial for a new prosthetic limb, the participant must understand the surgical procedure, potential complications, and rehabilitation process.
Q 7. How do you manage adverse events (AEs) and serious adverse events (SAEs)?
Managing adverse events (AEs) and serious adverse events (SAEs) is critical for patient safety and trial integrity.
- Reporting: All AEs and SAEs must be reported promptly to the investigator, IEC, and relevant regulatory agencies according to the study protocol. SAEs are events resulting in death, life-threatening situations, or hospitalization.
- Causality Assessment: Each AE and SAE needs evaluation to determine if it’s possibly, probably, or definitely related to the investigational device. This assessment involves careful consideration of the timing of the event in relation to device use and the patient’s medical history.
- Investigation: A thorough investigation into the cause of the event is necessary to identify potential contributing factors and prevent recurrence. This might involve reviewing medical records, conducting interviews, and analyzing device data.
- Action Plan: Based on the investigation, an appropriate action plan is developed. This might involve modifications to the study protocol, changes in device design, or even trial termination if safety concerns outweigh the benefits.
For instance, if a patient in a trial for a new drug-eluting stent experiences a major bleeding event, this would be reported immediately as a SAE. A thorough investigation would follow, assessing the potential link to the stent and potentially leading to adjustments in the stent’s design or trial protocol.
Q 8. Describe your experience with data management and analysis in clinical trials.
My experience in clinical trial data management and analysis spans over ten years, encompassing various phases from study design to final report generation. I’m proficient in designing data collection instruments, implementing data quality checks, and performing statistical analysis. This includes everything from developing case report forms (CRFs) to ensure data integrity and consistency, to utilizing statistical software packages like SAS and R to conduct descriptive and inferential analyses, creating tables, listings, and figures for regulatory submissions. For example, in a recent study evaluating a novel cardiovascular device, I was instrumental in developing a comprehensive data management plan that included robust data validation rules, resulting in a significant reduction in data queries during the regulatory review process. I’ve also managed large datasets, often exceeding 10,000 patient records, utilizing database management systems such as Oracle and SQL Server. This experience has provided me with a keen understanding of data cleaning, validation, and analysis techniques specifically tailored to the demands of regulatory agencies.
Q 9. How do you handle deviations from the protocol?
Handling protocol deviations is critical to maintaining data integrity and the credibility of the clinical trial. My approach involves a multi-step process. First, any deviation is immediately documented, including the date, time, description of the deviation, and the reason for its occurrence. This documentation follows a standardized format to ensure consistency. Next, I assess the severity of the deviation; some might be minor and easily mitigated, while others might necessitate amendments to the protocol. A deviation report is then created, which outlines the deviation, its impact on the study, and the corrective actions taken. This report is reviewed by the study team, including the principal investigator, and appropriate measures are implemented to prevent similar deviations in the future. For example, if a patient misses a scheduled visit, I’d document this as a protocol deviation and then assess if this deviation will impact the integrity of the data. If the missing data point is crucial, we might consider strategies for recovery, such as contacting the patient to reschedule the visit. All of this is carefully documented and submitted to the IRB/IEC for review, as required. In the case of serious deviations, the IRB/IEC and regulatory agencies are notified immediately.
Q 10. Explain the importance of GCP (Good Clinical Practice) in biomedical device trials.
Good Clinical Practice (GCP) is the cornerstone of ethical and scientific conduct in biomedical device clinical trials. It provides a standardized framework for designing, conducting, recording, and reporting clinical trials. GCP ensures that the rights, safety, and well-being of trial participants are protected, and that data generated are credible and reliable. Compliance with GCP guidelines is crucial for obtaining regulatory approvals and market authorization for new devices. Key aspects include obtaining informed consent from participants, maintaining accurate and complete records, implementing robust data quality control measures, and adhering to ethical principles throughout the study. Failure to comply with GCP can lead to significant consequences, including study termination, regulatory sanctions, and damage to the reputation of the sponsor and investigators. For instance, inadequate documentation of informed consent could result in regulatory scrutiny and even legal action.
Q 11. What is your experience with electronic data capture (EDC) systems?
I have extensive experience with various electronic data capture (EDC) systems, including Medidata Rave, Oracle Clinical, and Veeva Vault. My expertise covers not only data entry and management but also system configuration, user training, and data validation. I’m adept at using EDC systems to build and maintain customized CRFs, to generate reports, and to manage queries, ensuring data accuracy and timely completion of the trial. In a recent trial using Medidata Rave, I played a key role in configuring the system to integrate seamlessly with other systems, optimizing data flow and reducing manual data entry. Moreover, I am skilled in using EDC systems to conduct various data quality checks – such as range checks, consistency checks, and plausibility checks – to identify and resolve data inconsistencies early in the process.
Q 12. How do you ensure the quality and integrity of clinical trial data?
Ensuring the quality and integrity of clinical trial data is paramount. My approach is multifaceted and incorporates several key strategies. Firstly, a well-defined data management plan, that is developed during the study design phase and is crucial. This plan outlines data collection procedures, data validation rules, and data quality control measures. Secondly, robust data validation checks are implemented throughout the data entry process using the EDC system’s built-in validation rules and additional manual checks. Thirdly, regular data monitoring and auditing are performed to identify and resolve any inconsistencies or errors. This includes review of the data by clinical monitors, statistical programmers and data managers. Fourthly, data query resolution is a critical step, ensuring that all inconsistencies are addressed appropriately and documented thoroughly. Finally, maintaining detailed audit trails allows for complete traceability of data changes. A combination of these strategies ensures data reliability and minimizes bias.
Q 13. Describe your experience with regulatory submissions.
My experience in regulatory submissions encompasses the preparation and submission of regulatory documents to agencies like the FDA (in the US) and the EMA (in Europe). This includes compiling and organizing clinical trial data according to regulatory requirements, preparing integrated summary of safety and efficacy data (ISS), writing sections of regulatory documents such as the Investigational Device Exemption (IDE) application or the Premarket Approval (PMA) application, and interacting with regulatory agencies to address queries. I’ve successfully supported submissions for various types of devices, including Class II and Class III medical devices. I understand the importance of adhering to regulatory guidelines such as ICH guidelines and FDA regulations. In one instance, I was instrumental in preparing the clinical data package for a PMA submission, which resulted in the successful approval of a novel surgical device. This involved meticulous organization of data, close collaboration with statisticians and clinicians, and careful preparation of the regulatory documents to meet the rigorous standards set by the FDA.
Q 14. What are the key metrics you track in a clinical trial?
The key metrics tracked in a clinical trial depend on the specific objectives of the study, but generally include recruitment rate, retention rate, data completeness, the number and resolution of data queries, the incidence of adverse events, key efficacy endpoints and safety endpoints, and timeliness of milestones. Recruitment rate shows how well the trial is attracting participants. Retention rate measures the proportion of participants who complete the study. Data completeness highlights the proportion of required data points collected. The number of queries reflects the quality of data collected, and timely resolution is essential. Adverse events are monitored to assess the safety profile of the device, and efficacy endpoints show whether the device achieves the intended clinical outcome. Tracking these metrics allows us to monitor the progress of the trial, identify potential problems early on, and ultimately ensure the quality and integrity of the study results. Regular review of these metrics allows for proactive intervention and course correction if needed.
Q 15. How do you manage risk in a clinical trial?
Risk management in clinical trials is a proactive and systematic process designed to identify, analyze, and mitigate potential threats to the trial’s success. It’s crucial for ensuring patient safety, data integrity, and regulatory compliance. Think of it like building a house – you wouldn’t start without blueprints and a plan to address potential issues like bad weather or material shortages.
- Identification: We use risk registers, brainstorming sessions, and review of trial protocols to pinpoint potential risks. These might include protocol deviations, adverse events, recruitment challenges, data management issues, or regulatory changes.
- Analysis: Once identified, we assess the likelihood and impact of each risk. A simple matrix can help categorize risks as low, medium, or high based on probability and severity.
- Mitigation: For each risk, we develop strategies to reduce its likelihood or impact. This might involve implementing stricter monitoring procedures, developing contingency plans, or seeking additional expertise.
- Monitoring: Ongoing monitoring is essential. We track key metrics, conduct regular audits, and review safety reports to identify emerging risks and ensure mitigation strategies are effective.
For example, if a recruitment target isn’t being met, we might analyze why (e.g., poor site selection, inadequate advertising) and adjust our recruitment strategy accordingly. This could involve adding new sites, refining our inclusion/exclusion criteria, or implementing a more effective marketing plan.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with budget management in clinical trials?
Budget management in clinical trials is a critical aspect, requiring meticulous planning and ongoing monitoring to stay on track. It involves forecasting costs, tracking expenditures, and managing variances effectively. It’s like managing a household budget, but with much higher stakes and more complex variables.
- Budget Creation: This involves a detailed breakdown of all anticipated costs – personnel, facilities, supplies, CRO services, regulatory filings, etc. We often use specialized budgeting software.
- Cost Tracking: We meticulously track all expenses against the budget. This involves regular reporting and reconciliation of invoices. Any deviations need to be investigated and addressed immediately.
- Variance Analysis: Regularly analyzing variances helps us identify trends and potential overruns. This might involve adjusting the budget or re-evaluating the trial design to mitigate cost increases.
- Forecasting: Accurately forecasting future costs is vital. This involves considering potential unforeseen expenses and building contingency reserves.
In a recent trial, we encountered unexpected increases in laboratory testing costs. By analyzing the data, we identified a vendor issue that was causing the overruns. We switched to a more cost-effective vendor, which helped mitigate the cost increase and stay within budget.
Q 17. How do you collaborate with cross-functional teams?
Collaboration is the cornerstone of successful clinical trials. Cross-functional teams typically include medical monitors, data managers, statisticians, project managers, regulatory affairs specialists, and clinical research associates. Effective collaboration requires clear communication, shared goals, and a respectful work environment. Think of it as an orchestra – each musician plays their part, but it’s the conductor’s role to coordinate them for a harmonious performance.
- Regular Meetings: We utilize regular team meetings (weekly or bi-weekly) to discuss progress, address challenges, and make decisions collaboratively.
- Clear Communication: Utilizing shared platforms and tools enhances transparency and facilitates timely communication among team members. We leverage project management software that allows for real-time updates.
- Conflict Resolution: Conflicts are inevitable. We have established protocols for resolving disagreements effectively and fairly.
- Shared Goals: Everyone needs to understand the overall trial objectives and their individual contributions towards them. This fosters a sense of shared purpose and accountability.
For instance, in one study, a conflict arose between the data management team and the biostatisticians regarding data cleaning procedures. By facilitating open communication, clarifying expectations, and defining clear protocols, we were able to resolve the conflict and ensure data integrity.
Q 18. Describe a challenge you faced in a clinical trial and how you overcame it.
In one clinical trial, we encountered significant challenges with patient recruitment. Our initial projections were significantly overestimated. We had to quickly adjust our strategy to overcome this hurdle. It was like navigating a ship through a storm – we needed to adapt quickly to avoid capsizing.
- Problem Diagnosis: We meticulously analyzed our recruitment strategy: marketing materials, site selection, and inclusion/exclusion criteria.
- Solution Implementation: We discovered several issues: our marketing was not reaching the target population effectively, several of our sites were underperforming, and our inclusion/exclusion criteria were too restrictive. We updated our marketing to use more targeted social media campaigns and local outreach initiatives, and we optimized our inclusion/exclusion criteria to expand our potential patient pool.
- Results: By implementing these changes, we saw a significant improvement in our recruitment numbers, eventually meeting our target enrollment. The key was our proactive approach to problem-solving and our willingness to adapt our strategy.
Q 19. How do you manage timelines and deadlines in a fast-paced clinical trial environment?
Managing timelines and deadlines in a fast-paced clinical trial environment necessitates meticulous planning, proactive communication, and efficient task management. It’s like running a marathon – you need a well-defined plan, stamina, and the ability to adjust your pace as needed.
- Project Planning: Creating a detailed project plan with clearly defined milestones and deadlines is paramount. We use Gantt charts and project management software to visualize timelines and dependencies between tasks.
- Risk Assessment: Identifying potential delays early on helps us implement contingency plans to mitigate these risks. This includes having backup plans for potential recruitment delays, vendor issues, and regulatory hold-ups.
- Progress Monitoring: Regularly monitoring progress against the timeline is crucial. This often involves weekly or bi-weekly status meetings to discuss progress and identify potential roadblocks.
- Communication: Clear and proactive communication is vital to keep all stakeholders informed of any delays or changes to the schedule.
In one instance, we faced a potential delay due to a regulatory hold-up. By proactively communicating with regulatory agencies and providing the required documentation quickly, we successfully minimized the delay.
Q 20. What is your experience with vendor management?
Vendor management in clinical trials is essential, as we rely heavily on external vendors for various services (e.g., CROs, labs, pharmacies). Effective vendor management ensures quality, timely delivery, and compliance. It’s like managing a supply chain – each vendor is a critical link, and any breakdown can impact the entire process.
- Vendor Selection: We carefully select vendors based on their experience, reputation, and capacity to meet our needs. This often involves a rigorous selection process, including reviewing proposals, conducting site visits, and reference checks.
- Contract Negotiation: We meticulously negotiate contracts to ensure clarity on responsibilities, timelines, deliverables, and payment terms. It’s crucial to have clear service level agreements (SLAs).
- Performance Monitoring: We regularly monitor vendor performance against the agreed-upon SLAs and contract terms. We usually have regular check-in meetings and utilize key performance indicators (KPIs).
- Issue Resolution: Any issues or discrepancies are addressed promptly and effectively through communication and collaboration with the vendor. We have escalation procedures in place.
In a previous trial, we experienced delays with a central laboratory vendor. By actively engaging with the vendor, proactively monitoring their progress, and implementing corrective actions, we were able to address the delays and ensure the trial stayed on track.
Q 21. Explain your understanding of statistical analysis in clinical trials.
Statistical analysis is the backbone of clinical trials, providing the evidence needed to demonstrate the safety and efficacy of a biomedical device. It allows us to answer the research question: Does the device work as intended? It’s like using a microscope to examine a sample – we use statistical methods to identify trends and draw meaningful conclusions from the data.
- Study Design: Appropriate statistical methods must be pre-specified in the study protocol before the trial starts. This involves determining the sample size needed to detect a clinically meaningful difference, defining primary and secondary endpoints, and selecting the appropriate statistical tests.
- Data Management: Rigorous data management procedures are necessary to ensure the accuracy and integrity of the data analyzed. This includes processes for data cleaning, validation, and handling of missing data.
- Statistical Analysis Plan: A detailed statistical analysis plan (SAP) is developed, outlining the methods to be used for analyzing the data, including the specific statistical tests and the handling of multiple comparisons.
- Interpretation: The results of the statistical analysis are interpreted within the context of the study design and the clinical question being addressed. It’s not just about p-values; we need to consider clinical relevance and potential confounding factors.
For example, in a trial evaluating a new cardiovascular device, we would use statistical methods such as t-tests or ANOVA to compare the outcomes (e.g., mortality, morbidity) in the treatment and control groups. We would also assess the statistical significance of the results and draw conclusions regarding the device’s effectiveness.
Q 22. What is your experience with different study designs (e.g., randomized controlled trials, observational studies)?
My experience encompasses a wide range of study designs crucial in biomedical device clinical trials. I’ve extensively worked with randomized controlled trials (RCTs), the gold standard for evaluating intervention efficacy. RCTs involve randomly assigning participants to either an experimental group receiving the new device or a control group receiving a standard treatment or placebo. This randomization minimizes bias and allows for robust comparison of outcomes. For example, I was involved in an RCT comparing a novel implantable cardiac defibrillator to the existing market leader, focusing on parameters like survival rates and complication occurrences.
Beyond RCTs, I’m proficient in various observational studies, such as cohort studies and case-control studies. These are particularly useful when RCTs are unethical, impractical, or too expensive. A cohort study I participated in followed patients implanted with a new type of hip prosthesis to assess long-term performance and failure rates. Observational studies are powerful for detecting long-term effects and safety signals but can be more prone to biases that must be carefully addressed during design and analysis.
Further, my experience includes designing and executing single-arm studies, appropriate when evaluating devices with established comparators or when the control group is not available for comparison. These are more efficient in terms of resources, but lack the direct comparison of an RCT.
Q 23. How do you ensure compliance with HIPAA regulations?
Ensuring HIPAA compliance is paramount in biomedical device clinical trials. HIPAA (Health Insurance Portability and Accountability Act) mandates the protection of patient health information. My approach incorporates several key strategies:
- Strict adherence to data security protocols: This includes employing robust encryption methods for both data at rest and data in transit, using secure servers and access controls, and adhering to data minimization principles (collecting only necessary data).
- Comprehensive training programs for all personnel: This training covers HIPAA regulations, data handling procedures, and incident response protocols. Regular refresher courses are implemented to ensure continued compliance.
- Secure data storage and disposal: Data are stored on encrypted servers and hard drives. Upon study completion, data are securely destroyed following established protocols to prevent unauthorized access.
- Implementation of robust data governance processes: This involves creating documented workflows and procedures for data management, access control, and audit trails.
- Regular audits and risk assessments: We conduct periodic internal audits and external assessments to identify potential vulnerabilities and ensure continuing compliance.
In practice, this means every step, from informed consent to data analysis, is meticulously documented and reviewed to guarantee patient privacy. We utilize tools like data masking and de-identification to protect sensitive information. We also maintain a detailed record of access control, showing who viewed and manipulated data and when. Failing to meet HIPAA compliance could result in severe penalties including significant financial fines and legal ramifications.
Q 24. Describe your experience with different types of biomedical devices.
My experience spans a broad spectrum of biomedical devices, encompassing various therapeutic areas and device types. This includes:
- Cardiovascular Devices: Implantable cardioverter-defibrillators (ICDs), pacemakers, coronary stents, and heart valves. I’ve worked on trials evaluating both their efficacy and safety.
- Orthopedic Implants: Hip and knee prostheses, spinal implants. These trials often focus on long-term outcomes, such as implant survival and patient functional capacity.
- Neurological Devices: Deep brain stimulators for Parkinson’s disease. Trials for these devices meticulously assess changes in clinical symptoms and quality of life.
- Ophthalmic Devices: Intraocular lenses, glaucoma drainage devices. These trials focus on visual acuity and intraocular pressure.
- Wound Care Devices: Advanced wound dressings and pressure relieving systems. Trials evaluating these devices often assess wound healing rates and patient comfort levels.
This diverse background allows me to approach new device types with a holistic understanding of the regulatory, clinical, and statistical considerations involved. Each device presents unique challenges and demands tailored study designs and outcome measures.
Q 25. What is your understanding of the process of device approval?
The process of device approval is complex, involving preclinical and clinical testing, followed by regulatory review and approval. The path is dictated by device classification (Class I, II, or III, with Class III being the highest risk). It begins with preclinical testing, using animal models to evaluate safety and efficacy. Results are crucial in shaping the clinical trial design.
Next comes clinical testing, involving phases that typically include:
Phase I: Focuses on safety and tolerability in a small group of healthy volunteers (or a small group of patients in certain cases).
Phase II: Assesses efficacy and further evaluates safety in a larger group of patients.
Phase III: Large-scale, multi-center trials to confirm efficacy and safety in a diverse patient population. This phase often requires statistical rigor to demonstrate clear benefit over existing treatments.
After successful completion of clinical trials, a detailed submission (e.g., a Premarket Approval (PMA) application for Class III devices, a 510(k) submission for Class II devices) is made to the relevant regulatory agency (such as the FDA in the US or the EMA in Europe). This application includes all data from preclinical and clinical studies, along with detailed information on the device’s design, manufacturing, and intended use. The regulatory agency reviews the submission, may request additional information, and ultimately decides whether to approve the device for marketing.
Q 26. Explain the differences between preclinical and clinical studies.
Preclinical studies are conducted before clinical trials and primarily focus on evaluating the safety and potential efficacy of a biomedical device in non-human subjects (usually animals). These studies help identify potential risks, refine the device design, and establish a foundation for clinical trials. Data from preclinical studies informs the design of clinical trials, including the selection of appropriate doses, treatment schedules, and endpoints.
Clinical studies, in contrast, involve human subjects and are designed to evaluate the safety and efficacy of the device in a clinical setting. They are conducted in phases (I, II, and III as mentioned above) with increasing numbers of participants and focusing on the effects of the device on human patients. The data collected informs the determination of whether the device is safe and effective enough for marketing.
An analogy: think of preclinical studies as the ‘testing phase’ in a software development process – checking for bugs and ensuring basic functionality before moving on to beta testing with a limited group of users. Clinical studies are then like the beta testing and final launch stages. They test the functionality of the product in its final version using real-world use cases and providing a comprehensive feedback loop.
Q 27. How do you handle conflicts of interest in a clinical trial?
Handling conflicts of interest is crucial for maintaining the integrity of clinical trials. A conflict of interest arises when a person or organization has competing interests that could compromise their objectivity or decision-making in the trial. My approach involves:
- Proactive identification and disclosure: All investigators, staff, and sponsors must disclose any potential conflicts of interest at the beginning of the trial and throughout its duration. This includes financial interests (such as stock ownership or consulting fees), personal relationships, or other competing commitments.
- Independent review boards: An independent ethics committee and/or data safety monitoring board reviews any potential conflicts, ensuring that they are appropriately managed or mitigated.
- Mitigation strategies: If conflicts of interest are identified, mitigation strategies may include blinding procedures (where investigators are unaware of the treatment allocation), independent data analysis, or the exclusion of the conflicted individual from certain trial activities.
- Transparency and documentation: All conflicts of interest, along with the mitigation strategies employed, are thoroughly documented and reported. This transparency assures the validity of the trial results.
Failing to address conflicts of interest can lead to biased results and compromise the integrity of the clinical trial and could even lead to legal issues. It’s imperative to have clear procedures and policies in place to address potential conflicts early in the study to maintain trial integrity.
Q 28. What is your experience with clinical trial reporting?
Clinical trial reporting is a critical component of the drug and device development process. It involves summarizing the results of the trial in a clear, concise, and comprehensive manner. I have extensive experience in generating various reports, including:
- Clinical Study Reports (CSRs): These are comprehensive documents that provide a detailed account of the study design, methodology, results, and conclusions. CSRs follow regulatory guidelines (e.g., ICH E3) and are essential for regulatory submissions.
- Investigator Brochures: These provide a summary of the clinical data to be used for the further development of the study.
- Safety Reports: These documents detail any adverse events that occurred during the study, ensuring that any safety issues are promptly identified and addressed. They often include a risk-benefit analysis.
- Publication-ready manuscripts: These reports synthesize the trial findings for publication in peer-reviewed journals, ensuring the dissemination of knowledge to the scientific community.
My reporting experience encompasses utilizing appropriate statistical methods to analyze data, presenting results clearly in tables and figures, adhering to Good Clinical Practice (GCP) guidelines and regulatory standards, and ensuring that the reports are compliant with relevant laws and regulations.
Key Topics to Learn for Biomedical Device Clinical Trials Management Interview
- Regulatory Landscape: Understand FDA regulations (21 CFR Part 812, Part 820), EU MDR/IVDR, and other relevant international guidelines. Be prepared to discuss the implications of these regulations on trial design and execution.
- Clinical Trial Design & Methodology: Familiarize yourself with various trial designs (e.g., randomized controlled trials, observational studies), statistical considerations, patient recruitment strategies, and data management plans. Consider how these elements interact in a real-world setting.
- Risk Management & Mitigation: Understand the importance of proactive risk identification and mitigation throughout the clinical trial lifecycle. Be ready to discuss examples of potential risks and strategies for addressing them.
- Data Management & Analysis: Grasp the principles of data integrity, database design, data cleaning, and statistical analysis techniques relevant to biomedical device trials. Practice interpreting and presenting data effectively.
- Project Management & Budgeting: Demonstrate understanding of clinical trial timelines, budget management, resource allocation, and effective communication within a cross-functional team. Be able to discuss challenges and problem-solving approaches.
- Ethical Considerations: Understand the ethical principles guiding clinical research, including informed consent, patient safety, data privacy, and the responsibilities of clinical trial personnel.
- Device-Specific Knowledge: Depending on the specific device and therapeutic area, demonstrate knowledge of the device’s function, intended use, and potential risks. This showcases your understanding of the practical application of clinical trials in this specific context.
Next Steps
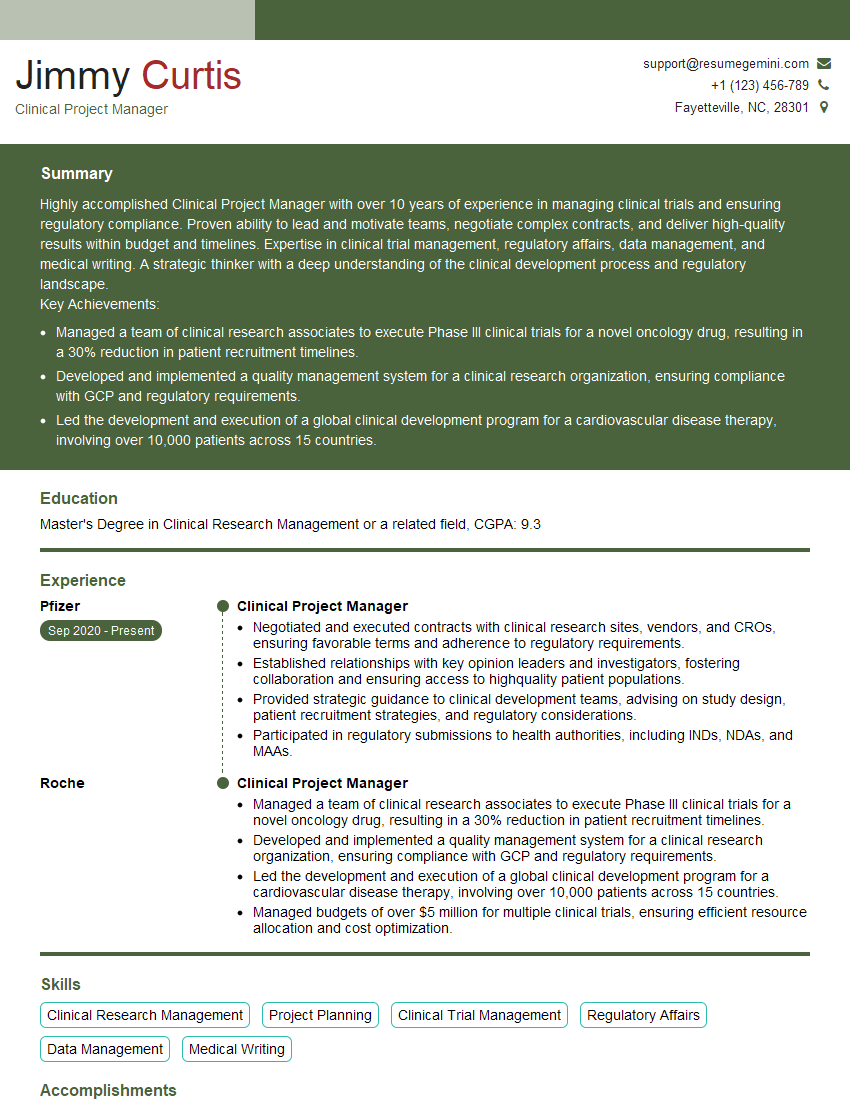
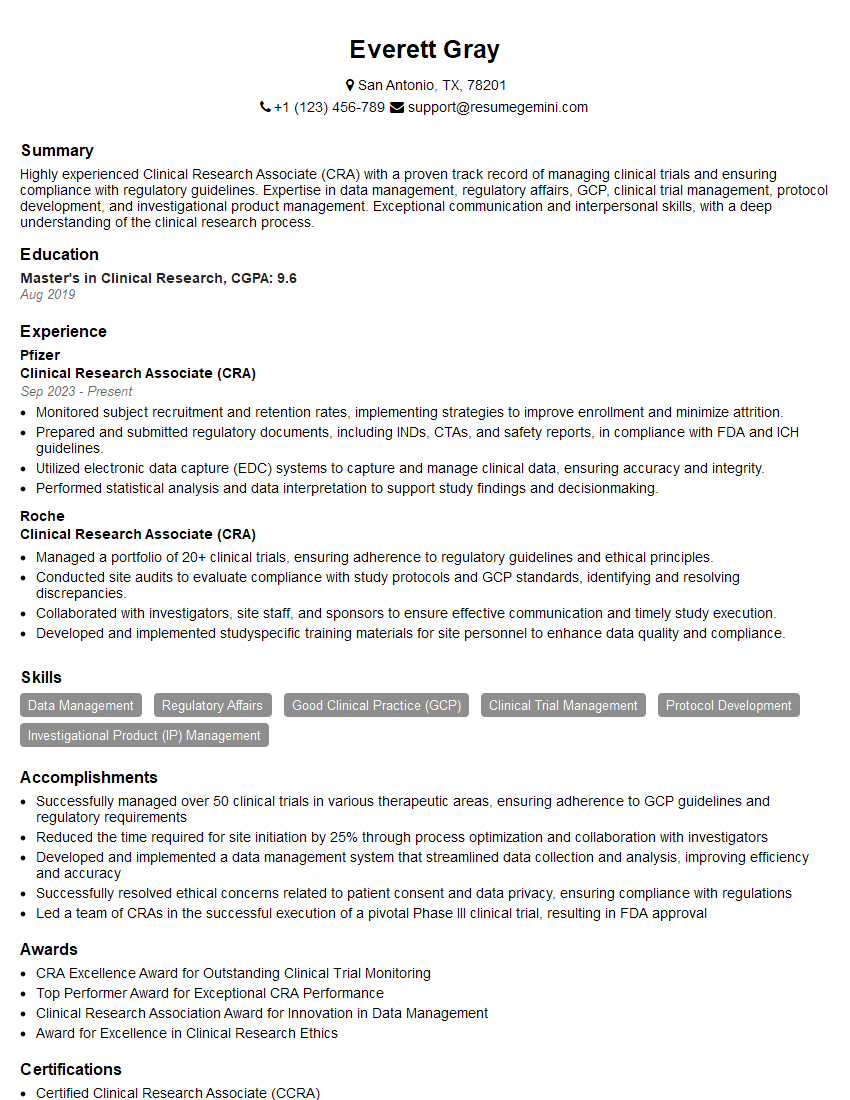
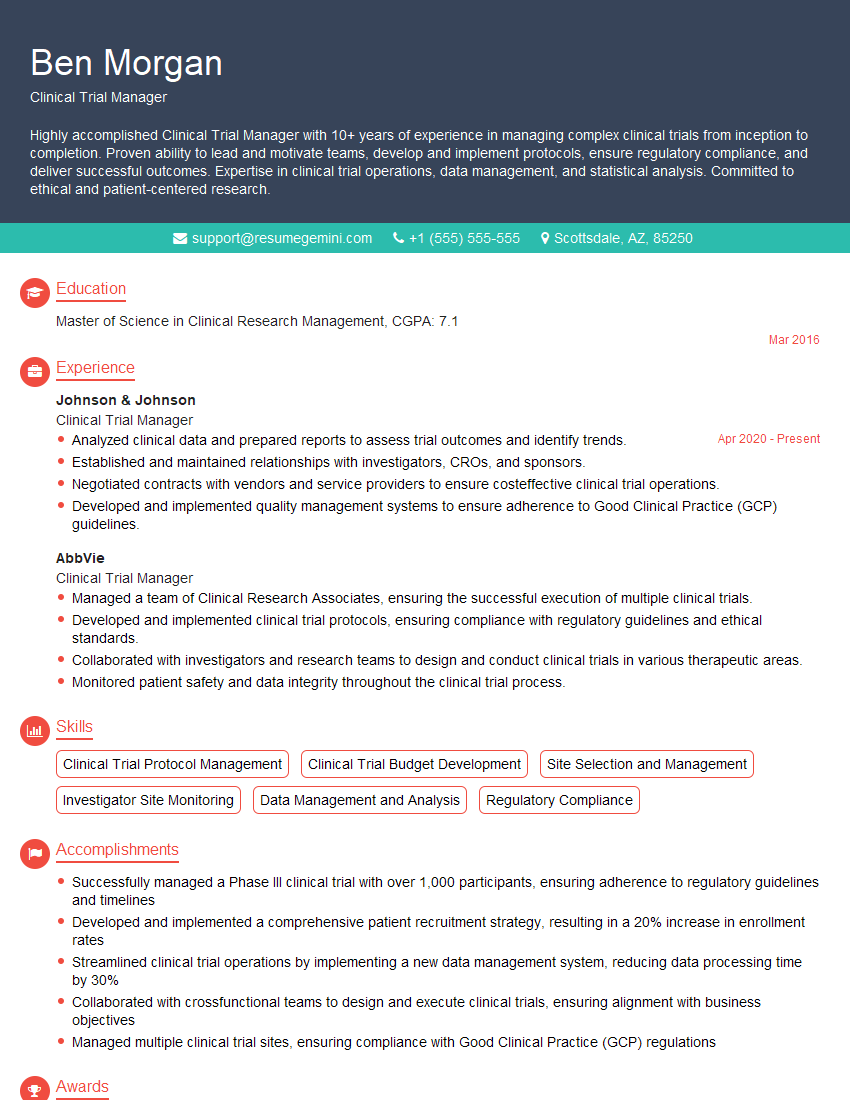
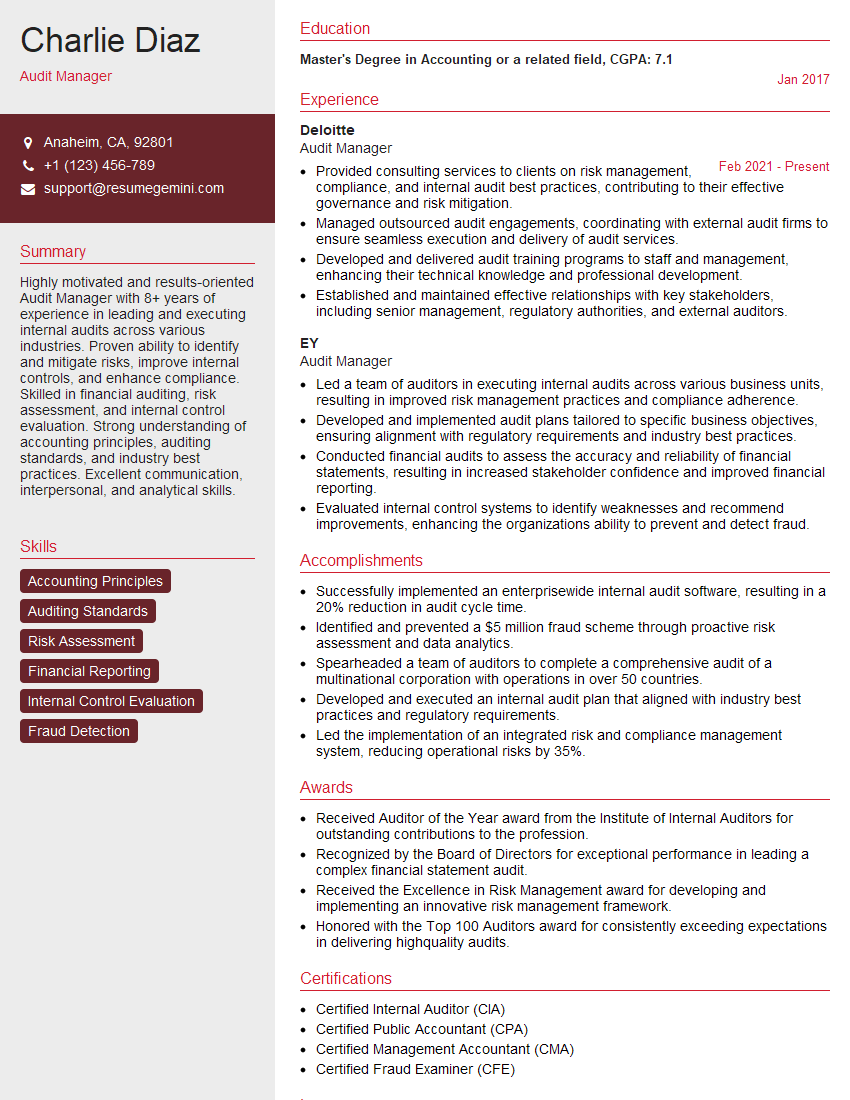
Mastering Biomedical Device Clinical Trials Management is crucial for advancing your career in the exciting and impactful field of medical technology. A strong understanding of these principles opens doors to leadership roles and greater responsibility within the industry. To maximize your job prospects, focus on creating an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. Take advantage of their tools and resources to craft a compelling document, and remember to check out their examples of resumes tailored to Biomedical Device Clinical Trials Management to gain further inspiration. This is your opportunity to present yourself as the ideal candidate!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good