Are you ready to stand out in your next interview? Understanding and preparing for Biomedical Device Legal and Regulatory Affairs interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Biomedical Device Legal and Regulatory Affairs Interview
Q 1. Explain the differences between 510(k) clearance and PMA approval.
In the United States, both 510(k) clearance and Premarket Approval (PMA) are pathways for medical device manufacturers to gain FDA approval before marketing their products. However, they differ significantly in their rigor and the types of devices they apply to.
A 510(k) clearance is a less stringent process used to demonstrate that a new device is substantially equivalent to a legally marketed predicate device. This means the new device has the same intended use and similar technological characteristics as the predicate. Think of it like showing the FDA that your new car is essentially the same as a previous model, just with minor improvements. This process involves submitting a detailed premarket notification to the FDA, including data demonstrating substantial equivalence. It’s faster and cheaper than PMA.
PMA approval, on the other hand, is required for devices that are significantly different from any legally marketed predicate. This pathway is much more rigorous, requiring extensive preclinical and clinical data to demonstrate the device’s safety and effectiveness. It’s akin to obtaining approval for a completely new type of vehicle – a flying car, for instance, would require a far more in-depth assessment of its design and functionality. The FDA conducts a thorough review, potentially including inspections of the manufacturing facility.
In essence, 510(k) is for incremental improvements, while PMA is for groundbreaking innovations.
Q 2. Describe the process of obtaining CE marking for a medical device.
Obtaining the CE mark for a medical device signifies conformity with the essential requirements of the European Union’s Medical Device Regulation (MDR) or In Vitro Diagnostic Regulation (IVDR), depending on the device type. The process isn’t a single event but a multifaceted journey involving several key steps.
- Technical Documentation Compilation: This forms the cornerstone of your application. It includes detailed information on the device’s design, manufacturing, performance, and risk management. This is where you thoroughly demonstrate compliance with all applicable regulations.
- Notified Body Selection and Involvement: You’ll need to engage a Notified Body – a third-party organization designated by an EU Member State to assess your device’s conformity. They’ll review your technical documentation and might conduct audits of your manufacturing facility.
- Conformity Assessment Procedure: The chosen procedure depends on the device’s risk class (Class I, IIa, IIb, or III). Higher-risk devices necessitate more stringent procedures, including more extensive testing and audits.
- Manufacturing Process Compliance: Your quality management system must comply with ISO 13485. Maintaining this compliance is crucial throughout the process and post-market surveillance.
- Declaration of Conformity: Once the Notified Body completes its assessment and confirms conformity, you issue a Declaration of Conformity. This legally binds you to the claims made in your technical documentation.
- CE Marking Application: Finally, the CE mark can be affixed to the device and its packaging. This signifies that your device complies with the essential requirements and can be legally marketed within the EU.
Failure to meet any of these requirements can lead to delays, rejection, or legal repercussions.
Q 3. What are the key requirements of ISO 13485?
ISO 13485:2016 is the internationally recognized standard for quality management systems (QMS) applied to medical devices. It provides a framework for manufacturers to ensure that their devices are consistently safe and effective. Key requirements include:
- Risk Management: Implementing a robust risk management process to identify, analyze, and mitigate potential hazards throughout the device’s lifecycle.
- Quality Policy and Objectives: Establishing a documented quality policy and setting specific objectives to achieve consistent quality.
- Resource Management: Ensuring adequate resources (personnel, infrastructure, equipment) are available to support the QMS.
- Product Realization: Defining and controlling processes related to design, development, procurement, production, and service provision.
- Measurement, Analysis, and Improvement: Continuously monitoring and measuring the effectiveness of the QMS, analyzing data, and implementing corrective and preventive actions (CAPA).
- Internal Audits: Conducting regular internal audits to assess compliance with the QMS and identify areas for improvement.
- Management Review: Periodically reviewing the QMS performance and making necessary adjustments to ensure its effectiveness.
- Corrective and Preventive Actions (CAPA): Establishing a system for identifying, investigating, and implementing corrective and preventive actions to address nonconformities.
Compliance with ISO 13485 is not optional for most medical device manufacturers aiming to sell their products globally. It underpins the reliability and safety of medical devices.
Q 4. How do you ensure compliance with HIPAA regulations for medical devices?
HIPAA (Health Insurance Portability and Accountability Act) regulations primarily focus on protecting the privacy and security of Protected Health Information (PHI). While HIPAA doesn’t directly regulate medical devices, compliance is crucial if the device handles or transmits PHI. This frequently occurs with devices integrated into Electronic Health Records (EHR) systems or those used for remote patient monitoring.
Ensuring HIPAA compliance involves several key steps:
- Data Minimization: Only collect the minimum necessary PHI required for the device’s intended function.
- Data Security: Implement strong security measures to protect PHI from unauthorized access, use, disclosure, disruption, modification, or destruction. This includes encryption, access controls, and regular security assessments.
- Privacy Rule Compliance: Adhere to HIPAA’s Privacy Rule, which governs the use and disclosure of PHI. This includes obtaining patient consent and providing appropriate notices of privacy practices.
- Breach Notification: Establish procedures for promptly notifying affected individuals and the appropriate authorities in case of a data breach.
- Business Associate Agreements: If using third-party vendors to handle PHI on behalf of the medical device manufacturer, ensure they are bound by Business Associate Agreements (BAAs) that comply with HIPAA.
Failure to comply with HIPAA can result in significant financial penalties and reputational damage. Proactive measures are crucial to avoid such consequences.
Q 5. Explain the role of a Unique Device Identifier (UDI).
A Unique Device Identifier (UDI) is a globally unique identification system for medical devices. It’s a combination of a device identifier and a production identifier that provides a way to accurately track and trace medical devices throughout their lifecycle. Think of it as a medical device’s digital fingerprint.
The device identifier is a unique code associated with the specific type of device, while the production identifier is a unique code for each specific instance of that device (e.g., the serial number). This system improves post-market surveillance, allows for accurate recall management, and helps identify counterfeit devices.
UDIs are crucial for regulatory compliance in many jurisdictions, including the United States and the European Union. They are essential for enhanced transparency and patient safety within the medical device ecosystem.
Q 6. What is a CAPA process, and how is it implemented?
A Corrective and Preventive Action (CAPA) process is a systematic approach to identify, investigate, and resolve quality issues and prevent their recurrence. It’s a critical component of any robust quality management system (QMS) and is fundamental to complying with standards like ISO 13485.
The implementation generally follows these steps:
- Identification of Nonconformities: Identifying instances where the product or process fails to meet specified requirements.
- Investigation: Conducting a thorough investigation to determine the root cause of the nonconformity. This often involves analyzing data, interviewing personnel, and reviewing documentation.
- Corrective Action: Implementing actions to correct the immediate nonconformity and restore compliance.
- Preventive Action: Implementing actions to prevent the recurrence of similar nonconformities. This is often the most proactive and crucial step in the CAPA process.
- Verification: Verifying that the corrective and preventive actions have been effective in addressing the root cause and preventing recurrence.
- Documentation: Thoroughly documenting all stages of the CAPA process.
A well-defined CAPA process helps manufacturers proactively address quality issues, reducing the risk of future problems and enhancing patient safety. It also ensures the company’s continued compliance with regulatory requirements.
Q 7. Describe your experience with post-market surveillance.
Post-market surveillance (PMS) involves monitoring the performance and safety of a medical device after it has been released to the market. It’s a crucial activity for continuously ensuring patient safety and product quality. My experience in PMS encompasses several key aspects:
- Developing PMS Plans: I’ve been involved in designing and implementing comprehensive PMS plans, including defining the scope, methodology, and key performance indicators (KPIs).
- Data Collection and Analysis: This includes gathering data from various sources, such as complaint reports, adverse events, field service reports, and post-market clinical follow-up studies. Analyzing this data helps identify potential safety issues and performance problems.
- Risk Management: Using the collected data to assess and manage risks associated with the device. This involves identifying potential hazards, evaluating their likelihood and severity, and implementing mitigating actions.
- Regulatory Reporting: Preparing and submitting regular reports to regulatory authorities, such as the FDA or the European Medicines Agency (EMA), regarding PMS findings and any identified safety issues.
- Communication and Collaboration: Working with cross-functional teams, including clinical affairs, quality assurance, and regulatory affairs, to share PMS data and implement corrective actions.
- Responding to Adverse Events and Complaints: Investigating and addressing adverse events and complaints related to the device, including initiating recalls when necessary.
Effective PMS is essential for maintaining patient safety and product quality. It’s an ongoing process that requires continuous vigilance and a commitment to data-driven decision-making. I’ve found that proactive PMS leads to better product performance and significantly reduces the potential for serious safety events.
Q 8. How do you handle a recall situation?
Handling a medical device recall is a complex, multi-faceted process requiring immediate action and meticulous execution. It’s not just about retrieving the devices; it’s about protecting patient safety and upholding regulatory compliance. My approach involves a structured, phased response, prioritizing communication and transparency at every step.
- Phase 1: Immediate Response: This involves immediately forming a recall team, confirming the problem, and assessing the scope and severity of the issue. We’d notify relevant regulatory authorities (like the FDA) within the legally mandated timeframe and initiate a thorough investigation to determine the root cause of the problem.
- Phase 2: Recall Strategy: Based on the risk assessment, we decide on the type of recall (Class I, II, or III, depending on the severity of the potential harm). A comprehensive communication plan is developed to inform healthcare providers, distributors, and patients. This includes creating clear and concise recall notices and ensuring effective distribution methods.
- Phase 3: Recall Execution: This phase involves the actual retrieval of the affected devices. We establish a system to track recalled devices and confirm their return. This often necessitates collaboration with distributors, hospitals, and other stakeholders.
- Phase 4: Post-Recall Activities: Following the recall, we undertake a thorough review of our quality systems, manufacturing processes, and design specifications to identify and correct the root cause of the failure. This might include implementing corrective and preventive actions (CAPAs) and potentially updating design controls. We also conduct post-market surveillance to monitor the effectiveness of the corrective actions.
For example, in a previous role, we handled a Class II recall involving a faulty sensor in a cardiac monitoring device. Our prompt response, effective communication, and thorough investigation minimized patient harm and ensured regulatory compliance. The experience highlighted the importance of proactive risk management and robust quality systems.
Q 9. Explain the importance of design controls in medical device development.
Design controls are the cornerstone of safe and effective medical device development. They provide a systematic approach to ensure that a device is designed to meet its intended use and specifications, while minimizing risks. Think of it as a blueprint for creating a safe and effective product. They are crucial for demonstrating compliance with regulations like 21 CFR 820.30.
- Planning: Defining the device’s intended use, user needs, and performance requirements.
- Input: Gathering all necessary information like specifications, design concepts, and test plans.
- Output: Defining the design outputs, such as detailed drawings, specifications, and protocols.
- Review: Regularly reviewing the design to ensure it meets requirements and addresses identified risks.
- Verification & Validation: Ensuring the design performs as intended through testing and validation processes. This includes verification activities to ensure the product aligns with design requirements and validation activities to ensure it delivers intended performance and safety in its target use environment.
- Transfer: Successfully transferring the approved design to manufacturing.
A strong design control system prevents costly rework down the line and ultimately protects patients from potentially harmful devices. For instance, neglecting design controls could lead to a device malfunctioning, resulting in patient injury and a costly recall.
Q 10. What are the key elements of a risk management plan?
A robust risk management plan is essential throughout the entire lifecycle of a medical device, from initial design to post-market surveillance. It’s a systematic process to identify, analyze, and control potential hazards associated with the device. This ensures patient safety and regulatory compliance, largely based on ISO 14971.
- Hazard Identification: Identifying all potential hazards associated with the device, including intended and unintended uses. This involves brainstorming sessions, failure mode and effects analysis (FMEA), and hazard analysis.
- Risk Analysis: Determining the likelihood and severity of each identified hazard. This uses qualitative or quantitative methods to estimate the risk level.
- Risk Evaluation: Assessing the acceptability of each risk level. This comparison is against predefined acceptance criteria.
- Risk Control: Implementing risk control measures to reduce or eliminate the identified risks. This can include design changes, warnings, instructions for use modifications, and other mitigative actions.
- Risk Monitoring: Continuously monitoring the effectiveness of the implemented risk controls through post-market surveillance and periodic reviews.
A well-executed risk management plan acts like a safety net, minimizing the potential for harm. It helps prevent accidents and reduces the potential for liability.
Q 11. What is your experience with auditing medical device quality systems?
I have extensive experience in auditing medical device quality systems, encompassing both internal audits and third-party audits following ISO 13485 and FDA QSR requirements. My audits have covered various aspects of the quality management system, including design controls, manufacturing processes, CAPA procedures, and complaint handling.
During an audit, I employ a risk-based approach, focusing on areas with the highest potential for non-compliance. I use checklists, interviews, document reviews, and observation of processes to gather evidence. My audit reports provide a comprehensive summary of findings, including both strengths and weaknesses, along with recommendations for improvement. I am proficient in identifying and reporting deviations from regulatory requirements and industry best practices. I’ve worked with companies of varying sizes and complexities, across multiple device classifications.
For instance, I recently led an audit of a company manufacturing implantable cardiac devices. The audit identified a gap in their CAPA process, which we helped them remediate. The experience highlighted the importance of continuous improvement and the vital role of audits in ensuring quality and compliance.
Q 12. Describe your understanding of the FDA’s Quality System Regulation (QSR).
The FDA’s Quality System Regulation (QSR), 21 CFR Part 820, establishes the minimum requirements for a quality system for medical device manufacturers. It’s designed to ensure that devices are safe and effective. Understanding the QSR is paramount for any medical device professional.
Key elements of the QSR include:
- Design Controls: Ensuring the device is designed to meet its intended use and specifications.
- Production and Process Controls: Controlling manufacturing processes to ensure consistent product quality.
- Corrective and Preventive Actions (CAPA): Addressing nonconformances and preventing recurrence.
- Nonconforming Material: Managing and handling materials that do not meet specifications.
- Quality Audits: Regularly auditing the quality system to ensure its effectiveness.
- Records and Documentation: Maintaining accurate and complete records of all activities.
Non-compliance with the QSR can result in significant penalties, including warning letters, recalls, and even facility closures. Therefore, a thorough understanding and rigorous implementation of the QSR are critical for any medical device company.
Q 13. How do you interpret and apply relevant medical device regulations?
Interpreting and applying medical device regulations requires a multifaceted approach. I begin by thoroughly understanding the specific requirements applicable to the device, its classification, and intended use. This involves a deep understanding of regulations from governing bodies like the FDA (US), EMA (Europe), and other international bodies.
My process involves:
- Regulatory Research: Identifying all relevant regulations and guidance documents.
- Risk Assessment: Evaluating the potential impact of non-compliance.
- Gap Analysis: Comparing current practices with regulatory requirements to identify any gaps.
- Implementation: Implementing changes and controls to address any identified gaps.
- Documentation: Maintaining comprehensive documentation to demonstrate compliance.
I stay current with regulatory changes through continuous professional development, participation in industry events, and monitoring regulatory updates. This ensures my interpretations remain accurate and my application is effective.
Q 14. What experience do you have with submissions to regulatory agencies (e.g., FDA, EMA)?
I have significant experience in preparing and submitting documentation to regulatory agencies, including the FDA and EMA. This includes preparing 510(k) premarket submissions, PMA applications, technical files, and other required documentation. My expertise encompasses the entire submission process, from initial planning and document preparation to responding to agency inquiries and obtaining approvals.
My experience includes:
- 510(k) Submissions: Preparing and submitting premarket notifications for Class II devices.
- PMA Submissions: Preparing and submitting premarket approvals for Class III devices.
- Technical File Preparation: Compiling comprehensive technical files for European regulatory submission.
- Responding to Agency Inquiries: Effectively responding to information requests from regulatory agencies.
- Regulatory Strategy Development: Collaborating with cross-functional teams to develop regulatory strategies.
I understand the importance of clear, concise, and well-supported submissions, and I prioritize accuracy and completeness to ensure timely approvals. I am also well-versed in the various regulatory pathways available and can advise on the optimal strategy for specific devices and situations.
Q 15. Describe a time you had to resolve a regulatory compliance issue.
During my time at MedTech Solutions, we faced a compliance issue concerning a newly released implantable cardiac device. Our post-market surveillance data revealed a slightly higher-than-expected incidence of a specific type of malfunction. Initially, we were concerned about the potential regulatory implications, specifically the need for a recall under 21 CFR Part 806.
My approach involved several steps. First, we immediately assembled a cross-functional team including engineering, quality, regulatory affairs, and clinical specialists. We meticulously reviewed the available data to determine the root cause of the malfunction, calculating the precise failure rate. We also conducted a thorough risk assessment to determine the severity of the malfunction and its potential impact on patient safety. This involved applying established risk management tools such as Fault Tree Analysis (FTA) and Failure Modes and Effects Analysis (FMEA).
Our investigation revealed a minor design flaw that could be addressed through a software update. Instead of a full-scale recall, which would have been costly and disruptive, we collaborated with the FDA to develop a corrective action plan, focusing on a field modification using the software update. We documented everything meticulously and submitted a 510(k) supplement. The FDA approved our plan, and we successfully implemented the software update to all affected devices. The issue was resolved with minimal patient impact and at a much lower cost than a recall would have incurred. This experience highlighted the importance of proactive post-market surveillance, thorough root cause analysis, and collaborative communication with regulatory bodies.
Career Expert Tips:
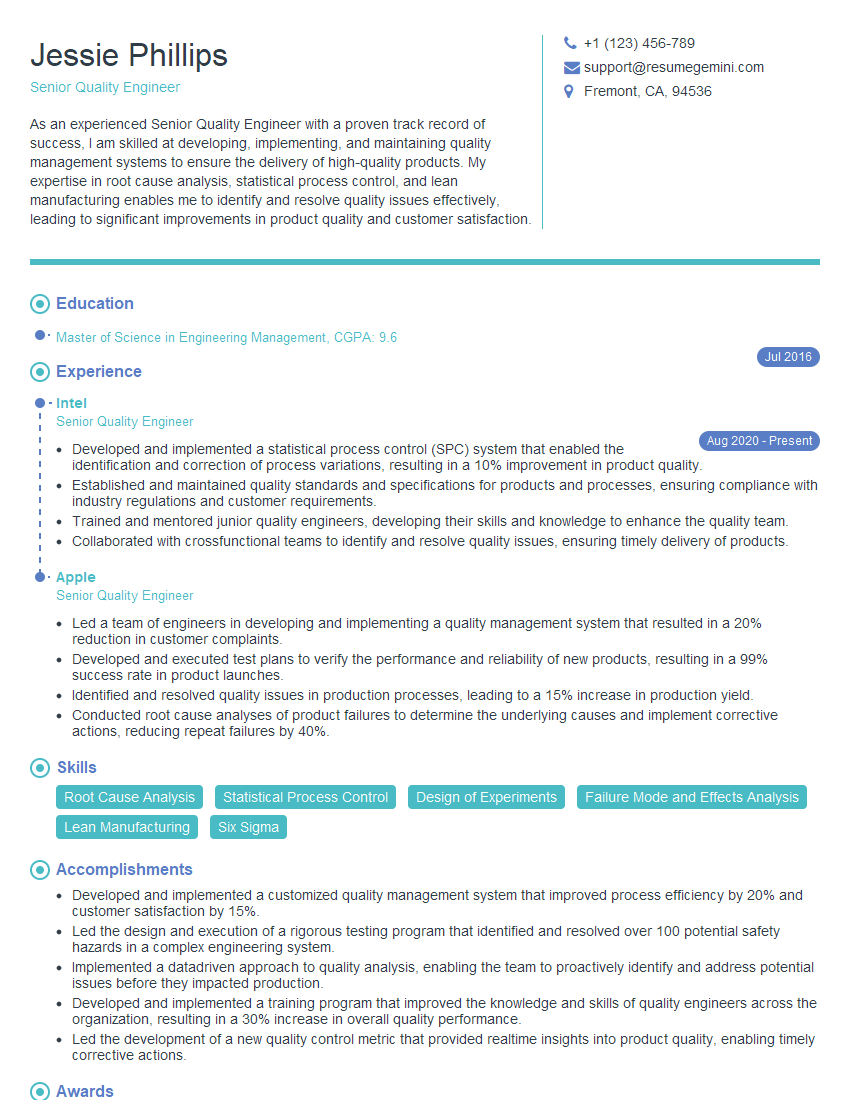
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How familiar are you with the Medical Device Single Audit Program (MDSAP)?
I’m very familiar with the Medical Device Single Audit Program (MDSAP). It’s a collaborative approach to medical device regulatory oversight, harmonizing audits conducted by participating regulatory authorities. The program aims to streamline the audit process for manufacturers by accepting a single audit that satisfies regulatory requirements in multiple countries simultaneously. This is a significant benefit, reducing duplication of effort and costs for companies operating in multiple MDSAP jurisdictions.
My understanding encompasses the requirements for participation, the audit process itself, including the various standards covered (like ISO 13485), and the management of non-conformances and corrective actions. I’ve worked directly with MDSAP auditors, preparing for and participating in audits. I’m proficient in navigating the MDSAP documentation requirements and the process for obtaining and maintaining MDSAP certification. I understand the implications of failing an MDSAP audit, including potential suspension or withdrawal of certification.
Q 17. What are your strategies for staying current with changes in medical device regulations?
Staying current with the ever-changing landscape of medical device regulations requires a multi-pronged approach. First, I subscribe to relevant newsletters and journals published by organizations such as the FDA, the EMA, and industry associations like AdvaMed. I also actively monitor the websites of these agencies for updates, guidance documents, and announcements of new regulations or enforcement actions.
Second, I attend industry conferences, webinars, and workshops to hear directly from regulators and experts on emerging trends and regulatory challenges. These events offer excellent networking opportunities to learn from colleagues’ experiences. Third, I leverage professional networks and online communities to participate in discussions and exchange information with other regulatory professionals. This allows for rapid dissemination of important updates and interpretation of new regulations.
Finally, I maintain a system for tracking and organizing regulatory updates, using tools like dedicated regulatory software or even a well-maintained spreadsheet, to ensure that I’m constantly aware of changes and can quickly access relevant information as needed.
Q 18. Explain your experience with adverse event reporting.
My experience with adverse event reporting is extensive. I’ve been involved in developing and implementing adverse event reporting systems for various medical devices, ensuring compliance with regulations like 21 CFR Part 803 (FDA) and the equivalent regulations in other jurisdictions. This involves defining reporting procedures, handling reported events, performing root cause analyses, and preparing the necessary reports for regulatory agencies.
I’m familiar with the various types of adverse events, ranging from minor malfunctions to serious injuries or deaths. The process includes prompt investigation, documentation (including medical records review when appropriate), and timely reporting to regulatory agencies. We always prioritize patient safety and transparency in our handling of adverse events, ensuring appropriate follow-up actions and corrective measures are taken.
For example, at my previous role we had a case involving a malfunction with our surgical stapler. We followed our established reporting procedures, immediately notified the FDA, conducted a thorough investigation, implemented corrective actions, and closely monitored post-market surveillance for similar incidents. This process reinforced the importance of a robust and well-documented adverse event reporting system.
Q 19. How do you ensure data integrity in regulatory submissions?
Data integrity is paramount in regulatory submissions. Compromised data can lead to regulatory delays, product recalls, and even legal action. My approach emphasizes ALCOA+ principles: Attributable, Legible, Contemporaneous, Original, Accurate, and complete with the addition of Enduring and Available. We utilize electronic systems with robust audit trails to ensure traceability of all data throughout its lifecycle.
Specific strategies include implementing rigorous data validation procedures, conducting regular data audits, and using electronic signatures to maintain data authenticity. We develop and adhere to strict standard operating procedures (SOPs) for data handling, data entry, and data review, including documented change control processes.
We utilize quality management systems (QMS) such as ISO 13485 to ensure data integrity is maintained throughout the product lifecycle. This involves not only the regulatory submission but also design and manufacturing processes.
Q 20. Describe your knowledge of Good Manufacturing Practices (GMP).
Good Manufacturing Practices (GMP) are a set of guidelines that ensure the consistent production of high-quality medical devices that meet pre-defined specifications and quality attributes. My understanding of GMP encompasses the entire manufacturing process, from raw materials to finished product. This includes facility design and maintenance, equipment qualification and calibration, personnel training, process validation, and quality control testing.
I have direct experience in implementing and maintaining GMP-compliant manufacturing processes, ensuring adherence to relevant regulations, including 21 CFR Part 820 (FDA) and ISO 13485. This involves developing and maintaining SOPs, conducting internal audits, managing deviations and corrective actions, and collaborating with manufacturing and quality teams to ensure continuous improvement. A strong understanding of GMP principles is fundamental to ensuring the safety and effectiveness of medical devices. It involves a culture of quality built into every aspect of the process.
Q 21. Explain your understanding of design verification and validation.
Design verification and validation are critical steps in the medical device development process. Design verification confirms that the device meets its pre-defined design specifications. This involves testing and analysis to ensure the device functions as intended. Design validation demonstrates that the finished device consistently performs its intended function in the intended clinical setting, thereby meeting user needs and addressing risks.
My experience includes designing and implementing verification and validation plans, selecting appropriate testing methods, conducting tests, analyzing results, and documenting findings. I’m proficient in using statistical methods to analyze data and demonstrate device performance. We use a risk-based approach, prioritizing verification and validation activities based on the potential risks associated with device failure. This involves applying risk management tools like FMEA and hazard analysis to identify potential problems and design robust testing protocols.
For example, we might use benchtop testing to verify specific design parameters, and clinical trials to validate the performance of an implantable device in actual patients. Properly designed verification and validation programs are essential to ensure the safety and effectiveness of medical devices.
Q 22. How do you navigate conflicting regulatory requirements in different regions?
Navigating conflicting regulatory requirements across different regions is a core challenge in biomedical device development. It requires a strategic approach combining thorough research, careful planning, and robust communication.
My approach begins with a comprehensive understanding of the target markets. I meticulously examine the specific regulations of each region, focusing on key differences in requirements for things like clinical trials, premarket approval pathways (like 510(k) in the US or CE marking in Europe), labeling, and post-market surveillance. This involves deep dives into official documentation from agencies like the FDA (US), EMA (Europe), PMDA (Japan), and others, as appropriate.
For example, if a device needs approval in both the US and Europe, the clinical data requirements might differ slightly. The US might necessitate a larger clinical trial for a higher-risk device, while Europe might focus on specific performance criteria. This requires careful planning to design clinical studies that satisfy both regulatory bodies, sometimes through a harmonized approach or using bridging studies.
Further, I employ a risk-based approach. We prioritize the most stringent requirements as a baseline, understanding this often ensures compliance in regions with less demanding regulations. We document this thoroughly, allowing for a clear audit trail and justification for the regulatory strategy. This includes detailed documentation of the regulatory requirements and the rationale for choosing specific compliance pathways.
Q 23. What is your experience with regulatory strategy development?
Developing a successful regulatory strategy is paramount to a product’s market entry. My experience involves creating comprehensive strategies that integrate product development, clinical trials, and regulatory submission. It’s a holistic process, not merely a series of regulatory filings.
I start by defining the product’s intended use and target market(s). Then, I conduct a thorough regulatory landscape assessment, identifying all relevant regulations and standards applicable to the device. This often involves extensive research and collaboration with regulatory experts in specific geographical areas. Once we have a complete picture of the regulatory pathways, I develop a detailed plan outlining the required steps, timelines, and resource allocation. This plan, often in the form of a Gantt chart, provides clear visibility to all stakeholders.
For instance, in one project, I developed a strategy for a novel cardiovascular implant targeting both the US and EU markets. The strategy included a detailed plan for conducting pivotal clinical trials fulfilling the requirements of both the FDA and EMA, designing the regulatory submission documents according to each agency’s guidelines, and determining how best to manage ongoing regulatory compliance and reporting.
The strategy was reviewed and iteratively refined based on feedback from internal teams and external regulatory consultants, ensuring its feasibility and alignment with business goals. It also incorporated contingency plans for addressing potential regulatory hurdles.
Q 24. Describe your experience with managing regulatory budgets and timelines.
Managing regulatory budgets and timelines effectively requires a highly organized and proactive approach. It’s about prioritizing, forecasting, and consistently monitoring progress.
I start by creating a detailed budget based on the regulatory strategy. This includes costs associated with clinical trials, testing, regulatory submissions, consultant fees, and any potential penalties or delays. I then use project management tools (like MS Project or Jira) to create a detailed timeline, breaking down the entire regulatory process into smaller, manageable tasks with assigned responsibilities and deadlines. Regular monitoring is vital. I regularly track the project’s progress against the budget and timeline using key performance indicators (KPIs). Early identification of potential issues allows for timely intervention and mitigation, preventing costly delays or budget overruns.
In a recent project, I identified a potential cost overrun by carefully analyzing the emerging data and anticipated costs of non-clinical testing. By proactively adjusting the budget and timeline, we avoided significant delays and maintained compliance. Transparency is key. I ensure that all stakeholders – from engineers to finance – have clear visibility into the budget and timeline. Regular reports, presentations, and updates help manage expectations and prevent misunderstandings.
Q 25. How do you effectively communicate complex regulatory information to both technical and non-technical audiences?
Communicating complex regulatory information effectively to both technical and non-technical audiences demands a nuanced approach. It’s about tailoring the message to the specific audience while maintaining accuracy and clarity.
For technical audiences (e.g., engineers, scientists), I use precise language and focus on the detailed regulatory requirements, emphasizing technical specifications and compliance strategies. I might present complex data using charts and graphs.
For non-technical audiences (e.g., management, investors), I simplify the information, using clear and concise language, analogies, and visual aids. I focus on the key takeaways and the impact on the business, emphasizing the potential risks and opportunities. I avoid jargon and technical terms as much as possible, opting for clear, straightforward explanations.
Regardless of the audience, I always ensure that the information is accurate, complete, and easily accessible. This might involve creating concise summaries, presentations, or written reports tailored to the specific audience’s needs and understanding.
Q 26. What are your strengths and weaknesses in handling regulatory pressure?
My greatest strength in handling regulatory pressure is my ability to remain calm, organized, and proactive under stress. I thrive on challenges and view regulatory hurdles as opportunities to demonstrate my expertise and problem-solving skills. My methodical approach and attention to detail ensure that I don’t miss crucial deadlines or details, even under pressure.
However, a weakness, one I am actively working to improve, is delegating tasks efficiently under pressure. Sometimes, I feel the need to oversee every detail personally, which can be detrimental in high-pressure situations. I’m currently working on building my team’s skills and trust, empowering them to handle more responsibilities, freeing up my time to focus on strategic decision-making.
Q 27. Describe your approach to proactively identifying and mitigating regulatory risks.
Proactive risk mitigation is crucial in regulatory affairs. My approach is based on continuous monitoring, early identification of potential issues, and the development of mitigation strategies.
I start by performing regular risk assessments, identifying potential regulatory issues early in the product development process. This includes evaluating the device’s design, intended use, and manufacturing processes to identify potential compliance gaps. I employ techniques like Failure Mode and Effects Analysis (FMEA) and Hazard Analysis and Risk Control (HARC) to proactively address potential hazards and risks.
For example, during the development of a new implantable device, I proactively identified a potential conflict with a specific FDA guidance document. This allowed us to modify the design and testing protocols early on, avoiding major delays later in the process. Furthermore, I regularly monitor changes in regulations, guidance documents, and enforcement actions, keeping abreast of any updates that might affect our products. Maintaining a thorough understanding of the regulatory landscape and actively seeking opportunities to collaborate with regulatory bodies helps minimize risks.
Finally, strong documentation is critical. Maintaining detailed records of all regulatory activities, including risk assessments, mitigation strategies, and communications with regulatory agencies, ensures compliance and provides a strong defense against potential issues. This proactive, risk-based approach minimizes disruptions and ensures a smoother path to market entry.
Key Topics to Learn for Biomedical Device Legal and Regulatory Affairs Interview
- Regulations and Compliance: Understanding FDA regulations (21 CFR Part 820, etc.), EU MDR/IVDR, and other international standards. This includes navigating the complexities of premarket submissions (510(k), PMA) and post-market surveillance.
- Quality Systems: Practical application of ISO 13485, understanding quality management systems (QMS), and experience with CAPA (Corrective and Preventive Action) investigations and documentation. Be prepared to discuss your experience with internal audits and regulatory inspections.
- Risk Management: Demonstrate your understanding of risk management principles, including hazard analysis (FMEA), risk control strategies, and the application of these methodologies throughout the product lifecycle.
- Product Labeling and Advertising: Knowledge of regulations related to device labeling, advertising claims, and promotional materials. Be prepared to discuss strategies for ensuring compliance with these regulations.
- Medical Device Reporting (MDR): Understanding the process of reporting adverse events, handling recalls, and maintaining accurate and compliant MDR records. Consider discussing practical problem-solving approaches to managing MDR situations.
- Intellectual Property (IP): Basic understanding of patent law, trademarks, and trade secrets as they apply to medical devices. This includes navigating IP issues in collaborations and licensing agreements.
- Contract Law: Familiarity with contracts relevant to medical device development, manufacturing, and distribution. This includes understanding confidentiality agreements and supply chain agreements.
Next Steps
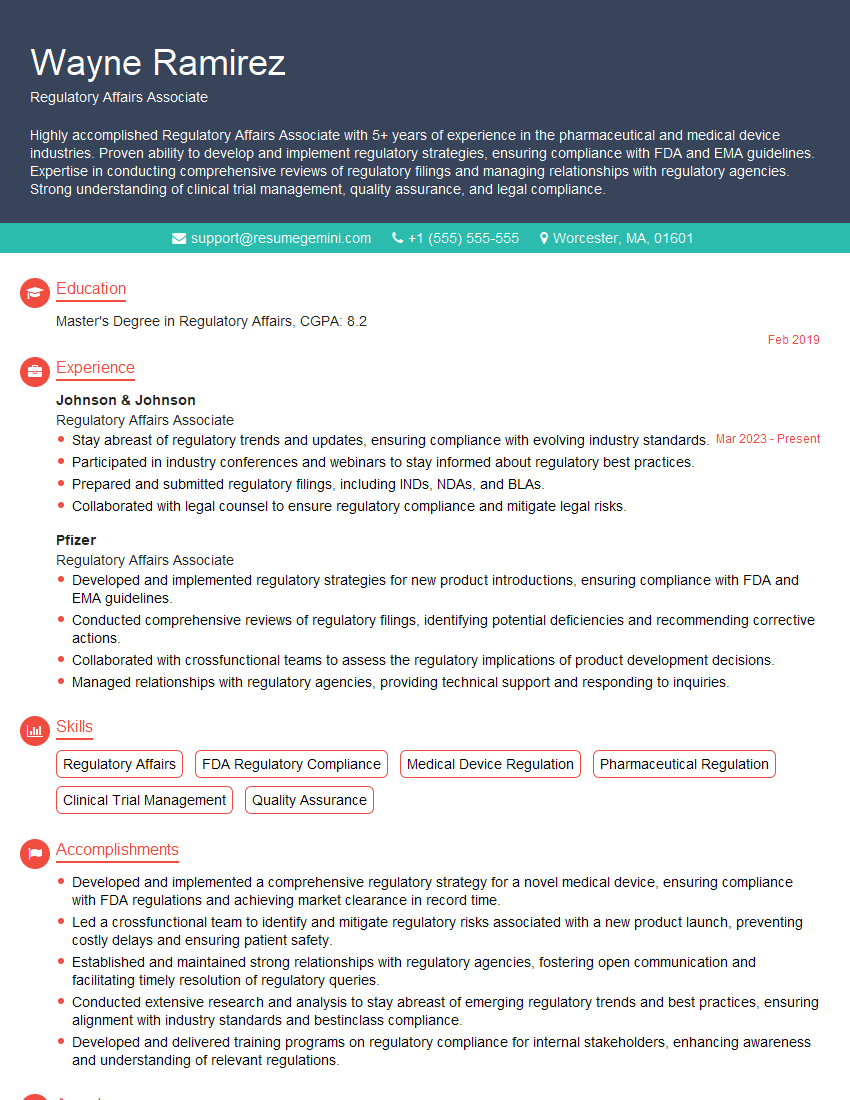
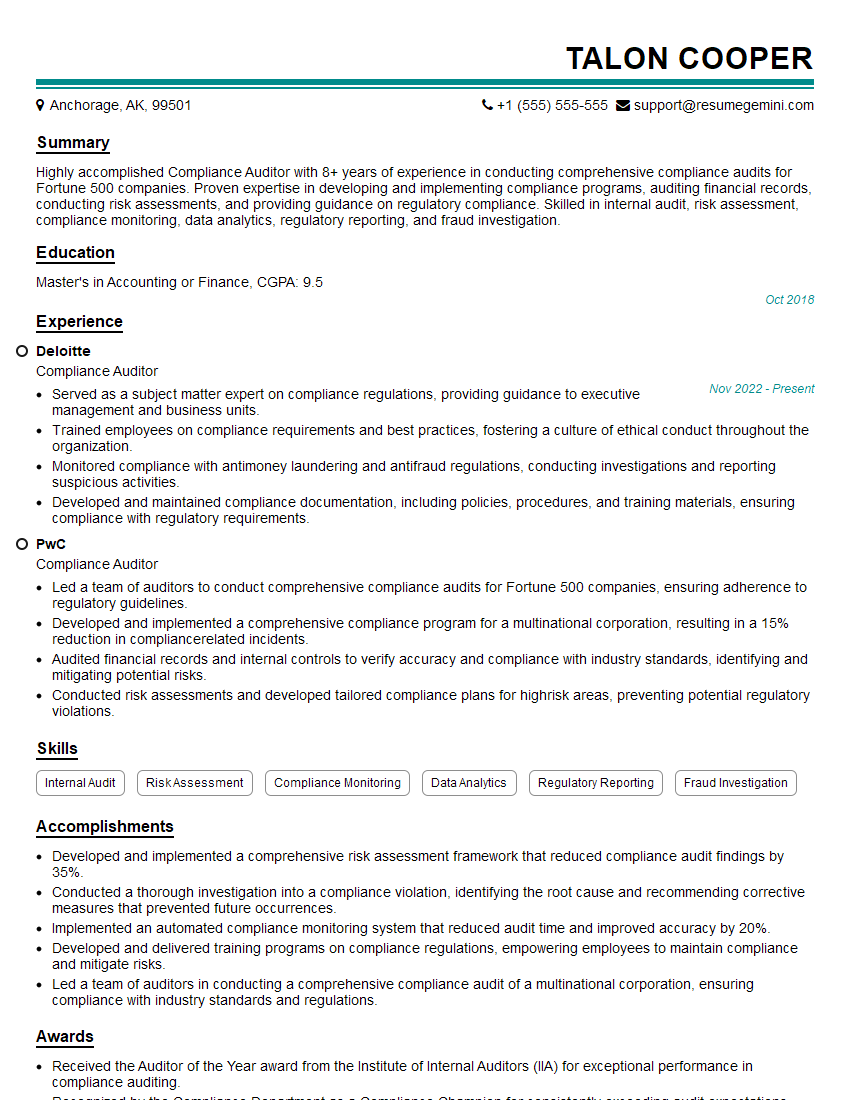
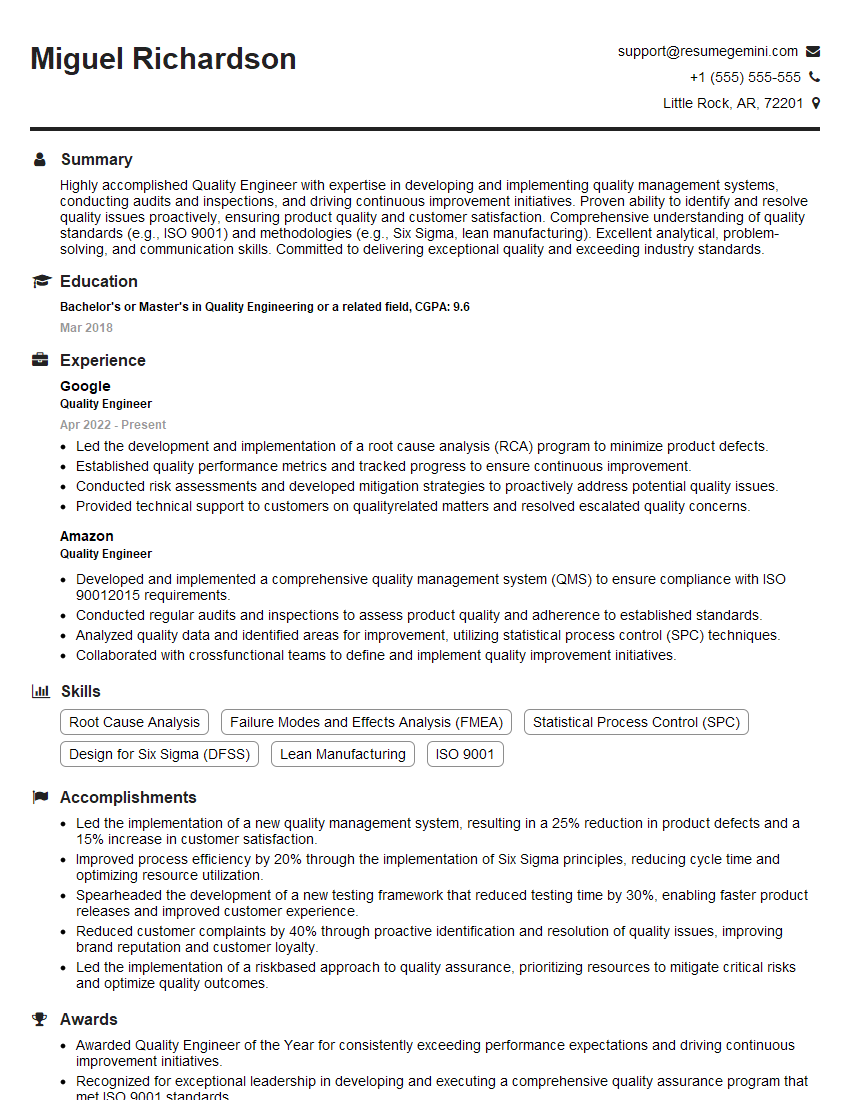
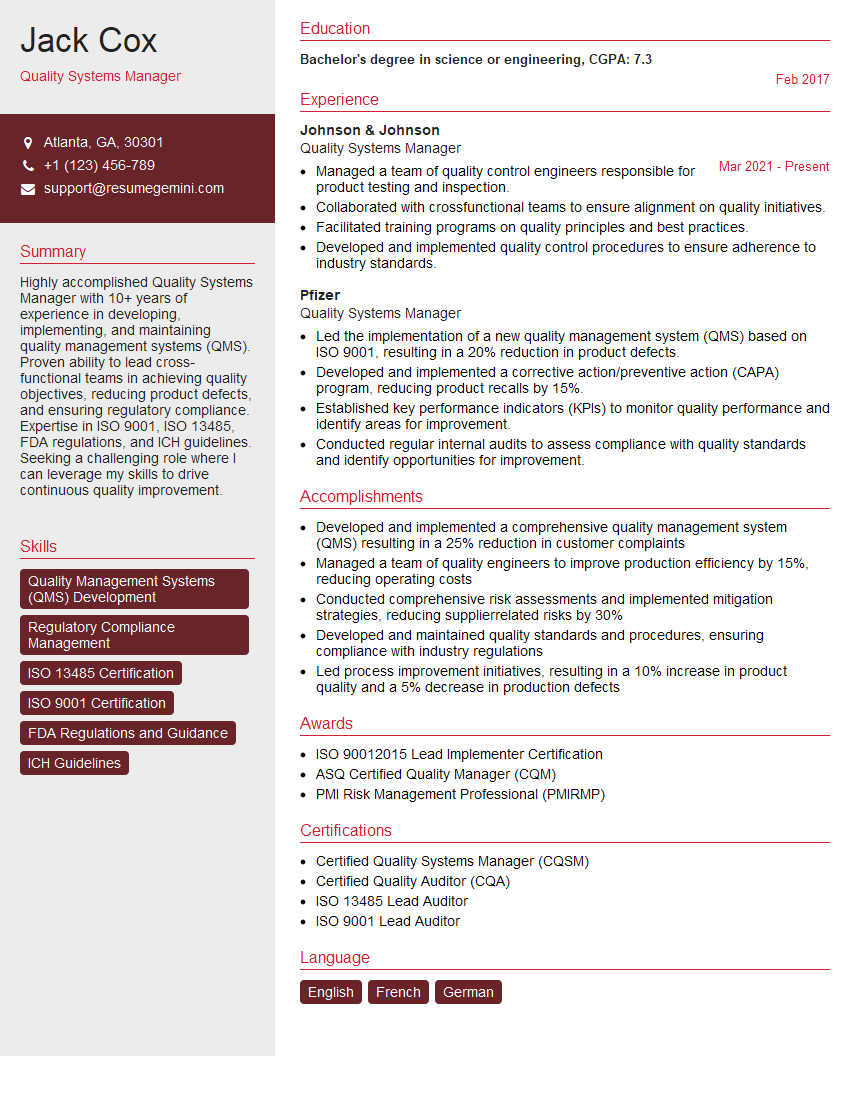
Mastering Biomedical Device Legal and Regulatory Affairs is crucial for a successful and rewarding career in this dynamic field. A strong understanding of these principles opens doors to leadership positions and ensures you can contribute meaningfully to patient safety and product quality. To maximize your job prospects, creating an ATS-friendly resume is essential. This ensures your qualifications are effectively highlighted to potential employers. We recommend using ResumeGemini, a trusted resource, to build a professional and impactful resume. ResumeGemini provides examples of resumes tailored specifically to Biomedical Device Legal and Regulatory Affairs, giving you a head start in showcasing your skills and experience.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good