Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Biomedical Device Validation and Verification interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Biomedical Device Validation and Verification Interview
Q 1. Explain the difference between verification and validation in the context of medical devices.
In the world of medical devices, verification and validation are distinct but equally crucial processes aimed at ensuring patient safety and product effectiveness. Think of it like baking a cake: verification confirms you followed the recipe correctly (did you use the right ingredients and steps?), while validation confirms the cake meets your expectations (is it tasty, the right texture, and the desired size?).
Verification focuses on ensuring the design and development process adheres to predefined specifications and requirements. It’s all about building the product right. This involves activities like design reviews, inspections, and tests to confirm that the device meets its design inputs. For example, verifying that a specific material meets its strength requirements as per the design specification.
Validation, on the other hand, confirms that the finished device performs its intended function effectively and safely. It focuses on building the right product. This is achieved through testing the device under real-world or simulated conditions to demonstrate its intended use and safety. An example would be conducting clinical trials to confirm the effectiveness and safety of a new pacemaker.
Q 2. Describe the key stages of a device validation process.
The device validation process typically involves several key stages:
- Defining Validation Requirements: Clearly outlining the intended use of the device and establishing specific performance criteria that must be met.
- Validation Planning: Developing a comprehensive plan detailing the validation strategy, methods, test procedures, acceptance criteria, and responsibilities.
- Protocol Development: Creating detailed protocols that outline how the validation tests will be conducted, including sample sizes, test procedures, and data analysis methods.
- Test Execution: Carrying out the validation tests according to the established protocols, meticulously documenting all procedures, results, and observations.
- Data Analysis: Analyzing the collected data to determine whether the device meets the predefined acceptance criteria. Statistical methods are often employed.
- Report Writing: Preparing a comprehensive validation report that summarizes the findings, conclusions, and any deviations from the plan. This report is a critical regulatory document.
- Validation Approval: Obtaining formal approval of the validation report by designated personnel with the necessary expertise and authority.
Q 3. What are the different types of validation studies used for biomedical devices?
Various validation studies are employed depending on the device’s characteristics and intended use. These include:
- Performance Validation: Demonstrating that the device consistently performs its intended function under specified conditions. This could involve testing accuracy, precision, sensitivity, and other relevant performance parameters.
- Biocompatibility Validation: Evaluating the device’s interaction with biological systems, ensuring it doesn’t cause adverse reactions. This often involves in vitro and in vivo tests.
- Sterility Validation: Confirming that the sterilization process effectively eliminates or reduces microbial contamination to an acceptable level. Methods include biological indicators and sterility testing.
- Software Validation (for software-containing devices): Verifying that software functions as intended, including functionality, security, and usability. This usually involves a combination of unit, integration, and system testing.
- Clinical Validation: This involves testing the device in a real-world clinical setting to evaluate its efficacy and safety in human patients (often required for high-risk devices).
Q 4. How do you determine the appropriate validation method for a specific device?
Selecting the right validation method is crucial and depends on several factors:
- Device Classification: Higher-risk devices require more rigorous validation. Class III devices need extensive clinical trials, while Class I may require less stringent testing.
- Intended Use: The specific function and application of the device dictate the necessary validation tests. A simple thermometer will have different validation needs compared to a complex surgical robot.
- Device Design and Complexity: The complexity of the device’s design and functionality influences the validation strategy. A device with sophisticated software will need more extensive software validation.
- Regulatory Requirements: Applicable regulations (e.g., ISO 13485, 21 CFR Part 820) specify the necessary validation activities. These requirements vary based on the device classification and geographical region.
A risk-based approach is essential. Identify potential hazards, evaluate the risks associated with those hazards, and select validation methods that adequately address those risks.
Q 5. What are the regulatory requirements for validating a medical device (e.g., ISO 13485, 21 CFR Part 820)?
Regulatory requirements for medical device validation are stringent and vary based on the device’s classification and the regulatory body (e.g., FDA in the US, EMA in Europe). Key regulations include:
- ISO 13485:2016: This international standard specifies the requirements for a quality management system (QMS) for the design, development, production, installation, and servicing of medical devices. It strongly emphasizes risk management and validation throughout the product lifecycle.
- 21 CFR Part 820: This US FDA regulation sets forth the quality system regulation (QSR) for medical device manufacturers. It mandates design controls, including verification and validation activities, to ensure product quality and safety.
- EU Medical Device Regulation (MDR): This regulation specifies stringent requirements for design, development, and validation, particularly focusing on post-market surveillance and clinical evidence.
These regulations emphasize the need for comprehensive documentation, traceability, and a robust quality management system to support the validation process.
Q 6. Explain the concept of design verification and its importance.
Design verification confirms that the device design meets the specified requirements before the device is manufactured. It’s a crucial step in the design control process, ensuring that the engineering specifications translate into a functional device. Think of it as a ‘proof of concept’ for the design. It verifies that the design meets all the requirements defined in the design input document. This avoids costly and time-consuming issues in the later stages of development.
Its importance lies in:
- Early Problem Detection: Identifying and resolving design flaws early in the process, saving time and resources.
- Reduced Risk: Minimizing the risks associated with manufacturing and releasing a flawed device.
- Regulatory Compliance: Meeting regulatory requirements for design control and documentation.
- Improved Product Quality: Ensuring the device meets performance and safety standards.
Methods for design verification include reviews, analyses, simulations, prototypes, and inspections.
Q 7. How do you create a validation plan?
Creating a robust validation plan is essential for a successful validation process. It should be a living document that evolves as the project progresses. A well-structured validation plan should include:
- Introduction: Defining the purpose and scope of the validation plan.
- Device Description: Providing detailed information about the medical device, including its intended use and intended users.
- Validation Objectives: Specifying the key performance characteristics to be validated and the acceptance criteria.
- Validation Methodology: Describing the testing methods, including test protocols and procedures.
- Test Equipment and Materials: Listing all the equipment and materials required for the validation testing.
- Test Schedule: Establishing a timeline for the execution of the validation tests.
- Data Analysis Plan: Outlining the methods for analyzing the collected data and determining if the acceptance criteria are met.
- Reporting Requirements: Defining the format and content of the validation report.
- Responsibilities: Assigning roles and responsibilities to the individuals involved in the validation process.
- Risk Assessment: Identifying potential risks and defining mitigation strategies.
The plan should be reviewed and approved by appropriate personnel before the commencement of the validation activities.
Q 8. Describe the process of risk assessment in device validation.
Risk assessment in device validation is a systematic process to identify, analyze, and control potential hazards associated with a medical device throughout its lifecycle. It’s crucial for ensuring patient safety and regulatory compliance. We use methodologies like Failure Mode and Effects Analysis (FMEA) or Hazard Analysis and Critical Control Points (HACCP) to identify potential failures and their severity, occurrence, and detectability. This helps prioritize risks and determine the necessary mitigation strategies.
For example, consider a new insulin pump. A risk assessment might identify the potential for inaccurate insulin delivery as a high-risk event. This would trigger a thorough investigation into the pump’s software, hardware, and user interface, resulting in rigorous testing and potentially design modifications to mitigate this risk.
- Identify Hazards: Brainstorming sessions, reviewing similar devices, and analyzing potential malfunctions.
- Analyze Risks: Assessing the severity, probability, and detectability of each hazard using risk matrices.
- Control Risks: Implementing design changes, process improvements, or testing procedures to reduce or eliminate risks.
- Risk Acceptance: Some residual risks might be acceptable if they are adequately mitigated and justified.
Q 9. What are the key performance indicators (KPIs) you monitor during validation?
Key Performance Indicators (KPIs) in device validation vary depending on the device and its intended use, but generally include:
- Accuracy: How closely the device’s measurements or outputs match the true values (e.g., for a blood pressure monitor).
- Precision: The consistency and repeatability of the device’s measurements (e.g., repeated measurements should be close to each other).
- Sensitivity and Specificity (for diagnostic devices): The ability to correctly identify positive and negative results.
- Usability: How easily the device can be used by its intended users (often assessed through user testing).
- Reliability: The device’s ability to function consistently over its intended lifespan. This often involves measuring Mean Time Between Failures (MTBF).
- Safety: The absence of hazards and risks to the user or patient.
- Performance under various conditions: How the device performs under different environmental conditions (temperature, humidity), power supply variations, or usage patterns.
We continuously monitor these KPIs throughout the validation process, using statistical methods to evaluate if the device meets predefined acceptance criteria. Any significant deviation triggers a thorough investigation.
Q 10. Explain the significance of statistical analysis in validation studies.
Statistical analysis is essential for validation studies because it provides an objective way to assess the device’s performance and demonstrate compliance with regulatory requirements. It allows us to move beyond anecdotal evidence and make data-driven decisions.
For example, instead of simply stating that a thermometer is accurate, we use statistical methods like ANOVA (analysis of variance) or t-tests to compare its readings against a gold standard. We calculate confidence intervals to determine the range within which the true value likely falls. This allows us to determine if the device meets pre-defined acceptance criteria with a certain level of confidence (e.g., 95%).
Furthermore, statistical process control (SPC) charts help us monitor the device’s performance during manufacturing and use, allowing for early detection of potential problems and preventing outliers from reaching the patient.
Q 11. How do you handle deviations or failures during validation testing?
Deviations or failures during validation testing are carefully documented and investigated. We follow a well-defined deviation management process. This typically involves:
- Immediate action: Stopping the test, securing the device, and ensuring patient safety (if applicable).
- Investigation: Determining the root cause of the failure through thorough analysis, including review of test procedures, equipment calibration, and device design.
- Corrective and Preventive Actions (CAPA): Implementing changes to prevent recurrence of the failure. This might involve design modifications, process improvements, or enhanced training.
- Documentation: Meticulously documenting the deviation, investigation, CAPA, and verification of its effectiveness.
- Impact assessment: Determining whether the deviation affects the validity of the overall validation study. In some cases, retesting or additional testing might be required.
For example, if a critical parameter falls outside the acceptance criteria during a durability test, we would investigate potential causes, such as a material defect or a flaw in the assembly process. This would trigger a CAPA process, potentially involving modifications to the manufacturing process or material selection.
Q 12. How do you document and report validation results?
Validation results are documented in a comprehensive validation report, which is a crucial part of the regulatory submission. The report should include:
- Introduction: Description of the device and the purpose of the study.
- Methods: Detailed description of the test methods, including equipment used, test procedures, and statistical analysis techniques.
- Results: Presentation of the data, including tables, graphs, and statistical summaries.
- Conclusion: Summary of the findings and assessment of whether the device meets its intended performance specifications.
- Appendices: Supporting documents, such as raw data, calibration certificates, and test protocols.
The report should be clear, concise, and well-organized, allowing regulatory agencies to easily understand the study’s objectives, methodology, and results. We use electronic data management systems to maintain the integrity and traceability of the validation data.
Q 13. What is a Design History File (DHF) and its role in validation?
A Design History File (DHF) is a comprehensive collection of documents that traces the design and development of a medical device. It’s a critical element in demonstrating compliance with regulatory requirements and plays a vital role in validation. The DHF documents every aspect of the device’s development, from initial concept to final design, ensuring traceability and supporting the validation process.
The DHF contains documents such as design specifications, risk assessments, test protocols and results, design reviews, and manufacturing process documents. Validation activities, including the results of verification and validation testing, are directly linked to the DHF, demonstrating that the device meets its design intent and intended use. A complete and well-maintained DHF is essential for successful regulatory submissions and post-market surveillance.
Q 14. What is a Device Master Record (DMR) and its relevance to validation?
A Device Master Record (DMR) contains all the information necessary to manufacture a medical device consistently and according to specifications. It’s a critical document used during manufacturing and quality control and is closely linked to validation. While the DHF focuses on the design, the DMR outlines the manufacturing processes and specifications that ensure the device manufactured meets the validated design.
The DMR includes details such as specifications for raw materials, manufacturing processes, quality control tests, packaging, and labeling. Validation activities demonstrate that the manufacturing processes defined in the DMR consistently produce devices that meet the validated design specifications and performance requirements. A well-defined and controlled DMR ensures that the manufacturing process produces devices that are consistent with the validated design, contributing to product quality and safety.
Q 15. Explain the concept of equivalence testing in validation.
Equivalence testing in validation isn’t about proving a device is exactly the same as a previous version or a competitor’s product, but rather demonstrating it’s similar enough to be considered interchangeable for its intended use. Instead of focusing on exact numerical matches, it focuses on whether the differences between two products (e.g., a new design and an existing one) are clinically insignificant. This is crucial for demonstrating that changes to a device don’t negatively impact its performance and safety.
For example, imagine a new blood pressure cuff design. Instead of rigorously proving its measurements are identical to the old cuff’s, we might conduct equivalence testing. We might establish an acceptable difference of ±2 mmHg. If statistical analysis shows that 95% of measurements from the new cuff fall within ±2 mmHg of the old cuff’s measurements under identical conditions, equivalence is established, and regulatory approval is more likely. This approach is often more practical and efficient than striving for perfect equivalence.
The statistical methods used in equivalence testing are more complex than traditional hypothesis testing and usually involve calculating confidence intervals to demonstrate that the difference between the products falls within predefined acceptance limits. Careful selection of appropriate statistical tests and acceptance criteria is paramount for successful equivalence testing.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is a validation master plan?
A Validation Master Plan (VMP) is a high-level document that outlines the overall strategy and approach for validating all aspects of a medical device’s lifecycle. Think of it as the roadmap for the entire validation process. It ensures a consistent, compliant, and efficient approach across all validation activities. A comprehensive VMP should clearly define the scope of validation, including specific devices, processes, and software components. It also details the methodologies, resources, timelines, responsibilities, and documentation requirements for each validation activity.
A well-structured VMP generally includes:
- Scope and Objectives: Clearly defines which devices, processes, and software are to be validated.
- Validation Methodology: Specifies the validation techniques to be employed (e.g., IQ, OQ, PQ; design verification and validation).
- Responsibilities: Assigns roles and responsibilities to team members involved in validation.
- Timeline and Resources: Establishes a realistic project timeline and identifies required resources.
- Documentation Requirements: Describes the required documentation and reporting procedures.
- Risk Management: Addresses potential risks and mitigation strategies.
- Approval Process: Outlines the approval procedures for all validation documents.
The VMP is a living document – it needs to be updated to reflect any changes in the device, process, or regulatory requirements throughout the product’s lifecycle.
Q 17. How do you manage changes to a validated device or process?
Managing changes to a validated device or process requires a rigorous and documented change control process. This is crucial for maintaining the validated state and ensuring continued compliance with regulatory requirements. Changes, no matter how seemingly insignificant, must be assessed for their potential impact on the device’s performance and safety.
A typical change control process includes:
- Change Request Submission: A formal request documenting the proposed change, its rationale, and potential impact.
- Risk Assessment: Evaluation of the potential risks associated with the change. This may involve Failure Mode and Effects Analysis (FMEA).
- Impact Assessment: Determining the impact of the change on the validated state of the device or process.
- Approval: Review and approval of the change request by relevant stakeholders.
- Implementation: Implementing the change following a pre-defined protocol.
- Verification and Validation: Verifying that the change was implemented correctly and validating that the device or process continues to meet its specifications and intended use.
- Documentation: Maintaining thorough documentation throughout the entire process, including change requests, risk assessments, approvals, and validation results.
Depending on the nature and impact of the change, a full revalidation may not always be necessary. A partial revalidation, focusing on affected aspects of the device or process, might suffice. This helps to optimize resources while still maintaining regulatory compliance.
Q 18. Describe your experience with different validation techniques (e.g., IQ, OQ, PQ).
My experience encompasses the complete suite of validation techniques, namely Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ), frequently used in the medical device industry. These are crucial for demonstrating that equipment and processes perform consistently as intended.
- IQ: This involves verifying that the equipment was installed correctly and meets the manufacturer’s specifications. For instance, verifying that a sterilizer is correctly connected to the power supply, utilities, and monitoring systems and that its documentation, such as manuals, are available.
- OQ: This focuses on verifying that the equipment performs consistently according to its operational parameters. For example, for a sterilizer, this would involve verifying that it reaches the target temperature and pressure, holds these parameters for the required duration, and maintains appropriate documentation. I’ve used OQ protocols to assess numerous types of equipment, from automated assembly machines to specialized testing equipment.
- PQ: This phase demonstrates that the equipment performs as intended throughout its complete operational life cycle and consistently produces the expected results under normal operating conditions. For the sterilizer, this might entail running multiple sterilization cycles using various test materials to ensure consistent sterility levels. We would record and analyze the outcome to confirm device effectiveness.
Beyond IQ, OQ, and PQ, I’ve also been involved in software validation using techniques such as unit, integration, and system testing. This also includes experience with design verification and validation, which uses a more holistic approach, encompassing risk analysis, design reviews, and testing across the full product lifecycle.
Q 19. Explain your understanding of Design of Experiments (DOE) in validation.
Design of Experiments (DOE) is a powerful statistical method used to efficiently investigate the effects of multiple factors on a response variable. It’s incredibly valuable in validation because it helps optimize processes and designs while minimizing the number of experiments needed. Instead of varying factors one at a time, DOE allows you to study the interaction between factors simultaneously.
In a medical device context, DOE might be used to optimize a manufacturing process. Let’s say we’re making a drug-eluting stent. We might use DOE to determine the optimal combination of factors like coating thickness, polymer type, and drug concentration to achieve the desired drug release profile. We’d design the experiment using techniques like factorial designs or response surface methodologies to identify optimal parameter combinations, reducing the resources required for development and characterization.
The results from a DOE provide statistical evidence regarding the significance of the different factors and their interactions, enabling data-driven decision-making during validation. Proper interpretation of DOE results is crucial for drawing valid conclusions and making informed decisions.
Q 20. How do you ensure the traceability of validation activities?
Traceability in validation ensures that all activities, results, and decisions can be linked back to their source and rationale. This is critical for auditing purposes and demonstrates compliance. A robust traceability system is essential.
Strategies I utilize include:
- Unique Identification Numbers: Assigning unique IDs to all documents, test results, and equipment.
- Version Control: Maintaining strict version control of all documents to prevent confusion and ensure that the correct versions are used.
- Cross-Referencing: Including clear cross-references between related documents and records.
- Electronic Document Management Systems (EDMS): Using EDMS to manage and track documents electronically, which provides an audit trail and enhances traceability.
- Documented Procedures: Maintaining clear, concise, and meticulously documented procedures for all validation activities.
By meticulously documenting every step and linking all relevant information, we build a robust audit trail. This not only ensures regulatory compliance but also simplifies troubleshooting and future modifications.
Q 21. How do you address challenges in validating software components of a medical device?
Validating software components in medical devices presents unique challenges due to the complexity and iterative nature of software development. The goal is to ensure the software functions as intended, is reliable, and does not compromise the safety and effectiveness of the device.
Addressing these challenges requires a multi-pronged approach:
- Software Development Life Cycle (SDLC) Compliance: Adhering to a well-defined SDLC, such as the Waterfall or Agile methodology, helps manage the validation process. This ensures that validation activities are integrated throughout the development process.
- Risk Management: Conducting a thorough risk assessment to identify potential software-related hazards and develop mitigation strategies.
- Software Verification and Validation (V&V): Employing rigorous V&V techniques, including unit testing, integration testing, system testing, and performance testing, to demonstrate that the software meets its requirements and performs as intended. Static code analysis tools can also be used to identify potential defects early in the process.
- Software Requirements Specification (SRS): A comprehensive SRS provides a clear and unambiguous description of software requirements and facilitates testing.
- Automated Testing: Automating test cases whenever possible to increase efficiency and improve consistency.
- Traceability Matrix: Creating a traceability matrix that links software requirements to test cases, ensuring that all requirements are tested. This is crucial for demonstrating compliance.
The complexities of software necessitate robust documentation and traceability. The increased level of rigor is necessary to ensure patient safety and regulatory compliance.
Q 22. Explain your approach to resolving validation discrepancies.
Resolving validation discrepancies requires a systematic approach combining technical expertise with meticulous documentation. My first step is to thoroughly analyze the discrepancy, identifying the root cause. This often involves reviewing the test data, the validation protocol, and the device’s design specifications. I then classify the discrepancy based on its severity – is it a minor deviation within acceptable limits, or a major failure requiring immediate attention?
For minor discrepancies, a thorough investigation may suffice, documenting the findings and potentially adjusting acceptance criteria if justified. For major discrepancies, a more comprehensive investigation is needed. This could involve repeating the test, modifying the test setup, or even redesigning aspects of the device. The process is always documented, with clear justification for each decision made.
For example, if a pressure sensor consistently reads 1% below the expected value, we’d first verify the calibration of the sensor and the accuracy of the testing equipment. We’d then check the manufacturing tolerances of the sensor and consider if this deviation falls within the pre-defined acceptance criteria. If not, and it affects the device’s intended use, we’d investigate the discrepancy and either adjust the acceptance criteria or rectify the issue via design changes or improved manufacturing processes. The entire process is rigorously documented, ensuring traceability and accountability.
Q 23. Describe your experience working with regulatory bodies on validation matters.
My experience with regulatory bodies, primarily the FDA (Food and Drug Administration) and other international equivalents, centers on clear communication and meticulous documentation. I’ve worked extensively on submissions for 510(k) clearances and premarket approvals (PMAs), ensuring that our validation documentation meets their stringent requirements. This includes preparing comprehensive reports that clearly demonstrate the safety and effectiveness of our devices.
I’ve also participated in audits conducted by regulatory bodies, demonstrating a deep understanding of validation principles and procedures. For example, during one audit, the FDA questioned our approach to software validation. We proactively provided detailed documentation outlining our software development lifecycle (SDLC) and verification activities. This resulted in a successful audit with no findings. A key aspect of my work involves staying up-to-date on evolving regulatory guidelines and incorporating them into our validation processes. Proactive compliance minimizes surprises and strengthens our position throughout the approval process.
Q 24. How do you ensure the robustness of your validation protocol?
Robustness in a validation protocol is crucial. I ensure this by incorporating several key elements: a comprehensive risk assessment, rigorous design of experiments (DoE), and the use of statistical methods.
The risk assessment identifies potential sources of variability and establishes control measures to mitigate them. For example, we might account for temperature fluctuations by performing tests under different temperature conditions. DoE helps to optimize the testing process and ensure that we are collecting sufficient data to draw meaningful conclusions. We frequently use techniques like factorial design to efficiently explore a range of factors.
Statistical methods, such as analysis of variance (ANOVA), provide an objective assessment of the data, allowing us to determine the significance of observed differences. Moreover, I always ensure the protocol considers edge cases and scenarios that may challenge the device’s performance, thus ensuring real-world applicability and robustness. For instance, we might test a drug delivery device at the extremes of its operational parameters (maximum flow rate, minimum pressure, etc.) to ascertain its capabilities and limits.
Q 25. What is your experience with different types of testing equipment used in device validation?
My experience spans a wide range of testing equipment commonly used in device validation. This includes but is not limited to: pressure sensors and transducers, temperature chambers, material testing machines (e.g., tensile testers, compression testers), spectrophotometers, and various electronic measurement devices (multimeters, oscilloscopes).
I’m also experienced in using specialized equipment depending on the specific device under validation. For instance, while validating a neurostimulator, we used sophisticated electrophysiological recording systems. The critical aspect is not just familiarity with these instruments but also a thorough understanding of their calibration procedures, limitations, and potential sources of error. Regular calibration and maintenance are vital to ensure the accuracy and reliability of the data obtained. All data acquisition equipment is properly qualified and the results of these qualifications are documented and readily available.
Q 26. How do you ensure the integrity of data collected during validation?
Maintaining data integrity is paramount. My approach incorporates several strategies, starting with a well-defined data management plan. This plan outlines procedures for data acquisition, storage, handling, and archiving. We use electronic data acquisition systems wherever possible to minimize manual transcription errors.
Data is always appropriately secured and backed up regularly. We employ a system of electronic signatures and audit trails to track all changes and access to data. Furthermore, appropriate checks are in place to ensure data consistency and identify potential outliers. These might include range checks or plausibility checks, and any deviations are investigated and documented. Calibration data for testing instruments is always linked to the validation data. The validation protocol itself mandates data handling protocols to ensure all data is reliable, accurate and untampered.
Q 27. How do you maintain a compliant and auditable validation system?
Maintaining a compliant and auditable validation system relies on a combination of proactive planning, meticulous documentation, and ongoing monitoring. We utilize a validated electronic document management system (EDMS) for storing all validation-related documents. This provides easy access to information and facilitates version control.
Our procedures are based on recognized industry standards and regulatory guidelines, and we adhere to a structured quality management system (QMS). We conduct periodic internal audits to identify potential weaknesses and ensure compliance. The results of these audits are documented, corrective actions are implemented, and follow-up is performed. Moreover, training programs are regularly conducted to ensure personnel are well-versed in relevant validation procedures and regulatory requirements. By consistently adhering to these principles, we can maintain a robust and auditable validation system, facilitating successful regulatory inspections and fostering trust in our device’s safety and effectiveness.
Key Topics to Learn for Biomedical Device Validation and Verification Interview
- Design Verification: Understanding the process of verifying that the design meets the specified requirements. This includes reviewing design specifications, risk assessments, and test plans.
- Design Validation: Demonstrating that the final design performs its intended function effectively and safely in its intended use environment. This involves developing and executing validation protocols and analyzing results.
- Risk Management: Applying risk management principles (e.g., ISO 14971) throughout the device lifecycle, identifying hazards, analyzing risks, and implementing controls to mitigate those risks.
- Regulatory Compliance: Familiarity with relevant regulations (e.g., FDA 21 CFR Part 820, ISO 13485) and their impact on validation and verification activities. This includes understanding documentation requirements and audit preparedness.
- Testing Methodologies: Knowledge of various testing methods used in validation and verification, including statistical analysis, equivalence testing, and performance testing. Practical experience with test execution and data analysis is highly valued.
- Verification and Validation Planning: Developing comprehensive plans and protocols that align with project timelines and regulatory requirements. This includes defining acceptance criteria and outlining the necessary resources.
- Documentation and Reporting: Understanding the importance of meticulous documentation, including test protocols, reports, and traceability matrices. The ability to clearly and concisely communicate technical information is crucial.
- Problem-Solving and Troubleshooting: Experience in identifying and resolving discrepancies, deviations, and failures during the validation and verification process. Demonstrating a systematic approach to troubleshooting is essential.
Next Steps
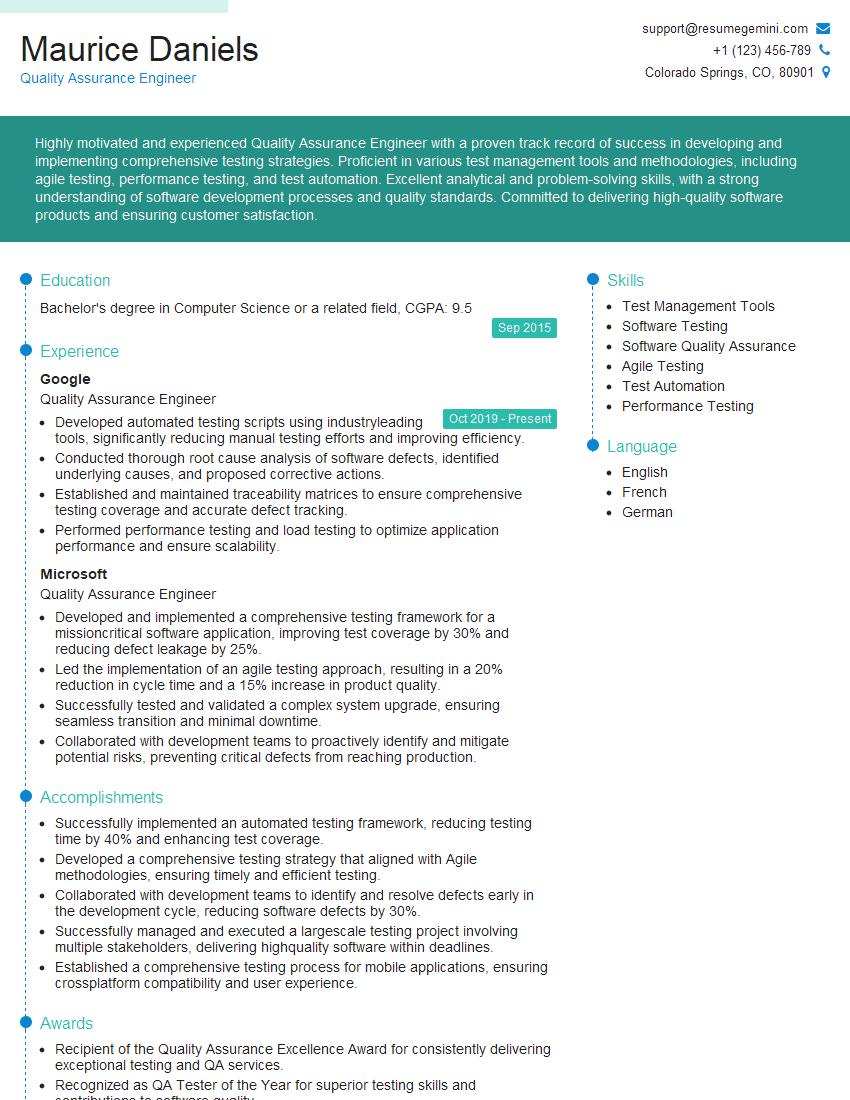
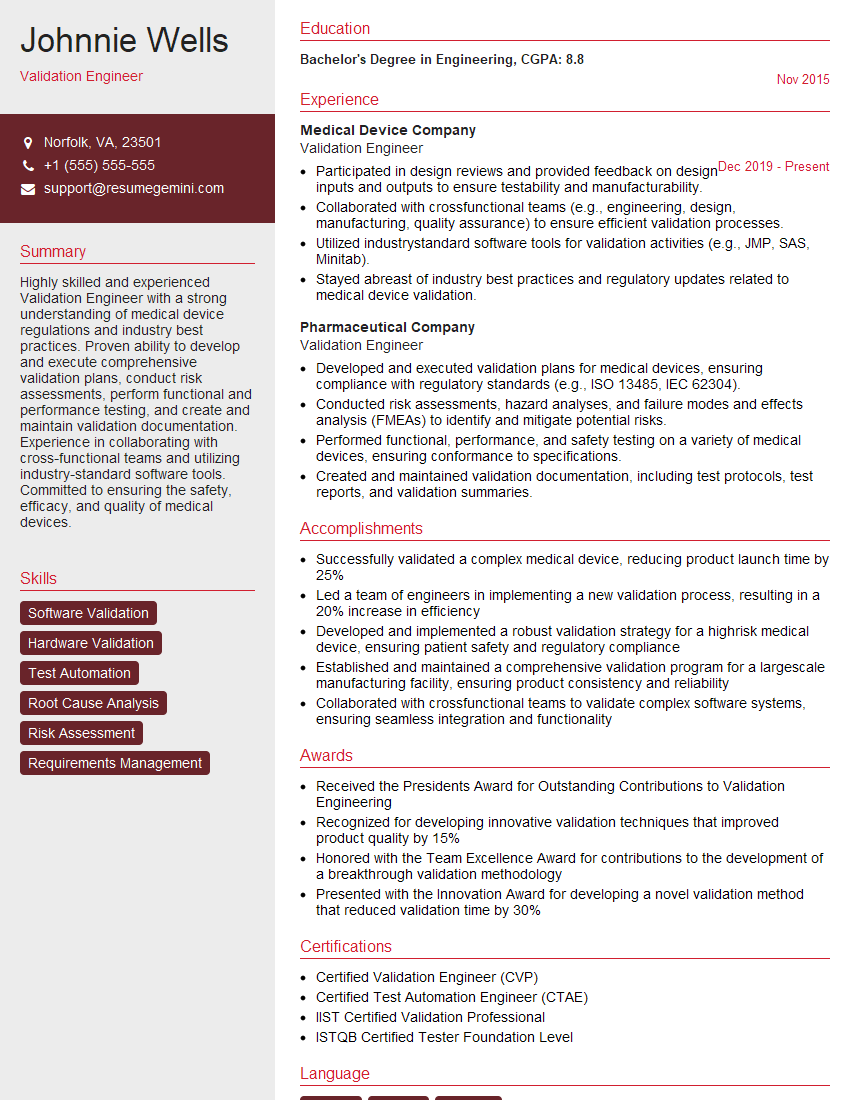
Mastering Biomedical Device Validation and Verification is crucial for career advancement in this highly regulated industry. A strong understanding of these principles significantly enhances your marketability and opens doors to exciting opportunities. To maximize your chances of securing your dream role, crafting an ATS-friendly resume is paramount. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. We provide examples of resumes tailored to Biomedical Device Validation and Verification professionals to help you get started. Invest the time to create a compelling resume that showcases your expertise – it’s a critical first step in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).