Preparation is the key to success in any interview. In this post, we’ll explore crucial Bloodborne Pathogen Exposure Prevention interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Bloodborne Pathogen Exposure Prevention Interview
Q 1. What are the key components of an effective Bloodborne Pathogen Exposure Control Plan?
An effective Bloodborne Pathogen Exposure Control Plan is the cornerstone of a safe workplace. It’s not just a document; it’s a living strategy that outlines how to prevent, minimize, and respond to exposure to infectious agents like Hepatitis B, Hepatitis C, and HIV found in blood and other potentially infectious materials (OPIM).
- Exposure Determination: This crucial first step involves identifying all tasks and situations where employees might come into contact with blood or OPIM. Think phlebotomists, surgeons, nurses, janitorial staff in healthcare settings, even emergency responders. The plan needs to specifically address these.
- Standard Precautions: This is the bedrock of the plan. It emphasizes treating all blood and OPIM as infectious and using appropriate personal protective equipment (PPE) like gloves, gowns, masks, and eye protection all the time, not just when you suspect infection. Think of it as ‘better safe than sorry’ taken to its most rigorous level.
- Engineering and Work Practice Controls: These are proactive measures designed to eliminate or minimize exposure risks. Examples include using needleless systems, safer medical devices, sharps containers, and well-designed workspaces. This minimizes the need to rely solely on PPE.
- Housekeeping: Regular and thorough cleaning and decontamination procedures are essential for preventing the spread of bloodborne pathogens. This includes proper spill cleanup protocols, as detailed below.
- Hepatitis B Vaccination: Employers are required to offer the Hepatitis B vaccine free of charge to all employees with occupational exposure. This is a highly effective preventative measure.
- Post-Exposure Evaluation and Follow-up: A well-defined process must be in place to manage any exposure incidents. This includes immediate first aid, thorough documentation, medical evaluation, and potentially post-exposure prophylaxis (PEP).
- Training: Comprehensive, regularly updated training is vital. Employees must understand the plan, their roles, and how to use PPE and equipment safely. Regular refresher courses keep knowledge current.
A robust plan integrates all these components to create a layered defense against bloodborne pathogens, ensuring a safer working environment for everyone.
Q 2. Describe the OSHA Bloodborne Pathogens Standard.
The OSHA Bloodborne Pathogens Standard (29 CFR 1910.1030) is a comprehensive set of regulations designed to protect healthcare and other at-risk workers from exposure to bloodborne pathogens. It mandates employers to implement a comprehensive Exposure Control Plan, as described above, tailored to the specific risks in their workplace. The standard covers a wide range of aspects, including:
- Exposure Determination: Identifying tasks and procedures involving potential exposure.
- Exposure Control Plan: Developing and implementing a written plan with all elements discussed previously.
- Personal Protective Equipment (PPE): Providing and requiring appropriate PPE.
- Housekeeping: Establishing proper cleaning and disinfection protocols.
- Hepatitis B Vaccination: Offering free Hepatitis B vaccinations to at-risk employees.
- Post-Exposure Evaluation and Follow-up: Providing procedures for evaluating and managing exposure incidents.
- Communication of Hazards: Informing employees of the risks and preventative measures.
- Recordkeeping: Maintaining accurate records of employee exposures, vaccinations, and training.
Failure to comply with the OSHA Bloodborne Pathogens Standard can lead to significant penalties and legal repercussions. It’s crucial for employers to understand and adhere to all aspects of the regulation to protect their employees.
Q 3. List the common bloodborne pathogens.
Several bloodborne pathogens pose significant risks in occupational settings. The most common include:
- Hepatitis B Virus (HBV): A virus that attacks the liver, causing inflammation and potentially serious long-term health problems.
- Hepatitis C Virus (HCV): Another liver-damaging virus, often leading to chronic hepatitis and cirrhosis.
- Human Immunodeficiency Virus (HIV): The virus that causes Acquired Immunodeficiency Syndrome (AIDS), weakening the immune system and making individuals susceptible to opportunistic infections.
While less common in occupational settings, other bloodborne pathogens such as Human T-lymphotropic viruses (HTLV) can also be a concern.
Q 4. Explain the difference between sterilization and disinfection.
Sterilization and disinfection are both crucial for infection control, but they differ significantly in their effectiveness and applications:
- Sterilization: This process eliminates all forms of microbial life, including bacteria, viruses, fungi, and spores. It renders an object completely free of living organisms. Methods include autoclaving (steam sterilization), dry heat sterilization, and ethylene oxide gas sterilization. Sterilization is typically used for medical instruments and equipment that will penetrate the skin or come into contact with sterile tissues.
- Disinfection: This process reduces the number of microorganisms on a surface but doesn’t necessarily eliminate all of them, especially resistant spores. Disinfectants are chemical agents that kill or inhibit the growth of microorganisms. Examples include bleach solutions, alcohol-based solutions, and quaternary ammonium compounds. Disinfection is used for surfaces and equipment that don’t require sterility.
Think of it this way: sterilization is like completely wiping a chalkboard clean, while disinfection is like erasing most of what’s written but leaving a few faint marks.
Q 5. What are the appropriate methods for handling and disposing of contaminated sharps?
Handling and disposing of contaminated sharps requires meticulous care to prevent accidental needlesticks and other injuries. The key is to never recap needles, and use appropriate containers.
- Never Recap Needles: This single action is responsible for a significant portion of needlestick injuries. Dispose of needles immediately and safely after use without recapping.
- Use Designated Sharps Containers: These puncture-resistant containers are specifically designed for safe disposal of sharps. They should be readily available at all points of use and clearly labeled. Never overfill them.
- Proper Disposal Procedures: Follow your workplace’s established procedure for disposing of full sharps containers. This often involves sealing the container, labeling it appropriately, and placing it in a designated area for waste removal. This area and process should be detailed in your facility’s Exposure Control Plan.
- Engineering Controls: Use safety-engineered devices, such as needleless systems, whenever possible. These minimize the risk of sharps injury at the source.
Remember, even a small puncture wound can lead to a serious infection. Always treat sharps with the utmost respect and follow established protocols carefully.
Q 6. Describe the proper procedures for cleaning up a blood spill.
Cleaning up a blood spill demands immediate and cautious action to prevent exposure and contamination:
- Personal Protective Equipment (PPE): Don appropriate PPE immediately, including gloves, gown, eye protection, and mask. This is non-negotiable.
- Absorb the Spill: Use absorbent materials like paper towels or spill kits to soak up the blood. Avoid splashing or aerosolizing the blood.
- Disinfect the Area: Once the spill is absorbed, disinfect the area thoroughly with a suitable disinfectant, such as a 10% bleach solution (1 part bleach to 9 parts water), following the manufacturer’s instructions. Let it sit for at least 10 minutes before wiping.
- Proper Disposal: Dispose of all contaminated materials, including absorbent materials and PPE, in designated biohazard containers.
- Document the Incident: Record the details of the spill, including the time, location, and steps taken for cleanup. This is crucial for tracking and preventing future incidents.
Remember, a swift and proper response minimizes the risk of infection for everyone involved. Training is essential to ensure everyone knows the proper procedures. Treat every blood spill as a potential exposure event.
Q 7. What are the post-exposure prophylaxis (PEP) procedures for bloodborne pathogen exposure?
Post-exposure prophylaxis (PEP) is a critical intervention following a potential bloodborne pathogen exposure. It aims to prevent infection after exposure has occurred. It’s not a guaranteed prevention, but it significantly reduces the risk.
- Immediate Action: Wash the exposed area thoroughly with soap and water. Report the incident to your supervisor immediately.
- Medical Evaluation: Seek medical attention promptly. A healthcare provider will assess the risk based on the nature of the exposure, the source individual’s infection status (if known), and other factors.
- PEP Treatment: PEP may include medications such as antiretroviral drugs for HIV exposure, hepatitis B immune globulin and the hepatitis B vaccine for HBV exposure, and antiviral medications for HCV exposure. The specific regimen depends on the exposure and the individual’s health status. PEP must be started as soon as possible after exposure to be most effective.
- Testing and Monitoring: Following PEP, ongoing testing and monitoring may be recommended to check for infection. This ensures early detection and treatment if infection occurs.
- Counseling: Emotional support and counseling may be helpful to deal with the stress of the exposure incident.
Time is of the essence with PEP. The sooner treatment begins, the better the chance of preventing infection. Understanding the procedure and the importance of immediate action can be lifesaving.
Q 8. What is the importance of proper hand hygiene in preventing bloodborne pathogen transmission?
Proper hand hygiene is the cornerstone of preventing bloodborne pathogen transmission. It’s a simple yet incredibly effective method for dramatically reducing the risk of infection. Think of your hands as potential vectors – they can easily transfer pathogens from contaminated surfaces to your mucous membranes (eyes, nose, mouth) or even create tiny cuts on your skin, providing entry points for viruses like Hepatitis B or HIV.
Effective handwashing involves using soap and water for at least 20 seconds, scrubbing all surfaces thoroughly, including between fingers and under nails. Alcohol-based hand rubs are also effective when soap and water aren’t readily available, but they’re less effective against certain types of soil.
In a hospital setting, for example, a nurse who doesn’t wash their hands after handling a patient’s blood could inadvertently transfer the bloodborne pathogens to another patient, leading to a serious infection. This simple act of handwashing acts as a crucial barrier against the spread of disease.
Q 9. Explain the use of personal protective equipment (PPE) in preventing bloodborne pathogen exposure.
Personal Protective Equipment (PPE) provides a physical barrier between healthcare workers and potentially infectious materials. It’s a critical layer of defense in preventing exposure to bloodborne pathogens. Imagine PPE as a suit of armor, protecting you from the ‘enemies’ – infectious agents.
The effectiveness of PPE relies on proper selection, use, and disposal. Using the wrong PPE, or using it incorrectly, significantly compromises its protective capabilities. Proper training on PPE use is crucial for effectiveness.
Q 10. What are the different types of PPE and when should each be used?
Several types of PPE exist, each designed for specific situations:
- Gloves: Essential for any procedure involving contact with blood or body fluids. Different glove types exist (nitrile, latex, vinyl) each with varying levels of protection and allergy considerations. Always choose the appropriate glove for the task.
- Gowns: Provide protection for the body during procedures likely to generate splashes or sprays of blood or body fluids. They should be worn when performing tasks like wound cleaning or assisting in procedures that could produce significant splatter.
- Masks/Respirators: Protect the wearer from airborne pathogens. A simple surgical mask protects against splashes, while an N95 respirator provides more substantial protection from smaller particles, as in an aerosol-generating procedure.
- Eye Protection: Goggles or face shields protect the eyes from splashes of bodily fluids. This is particularly crucial during procedures with a high risk of splash hazards.
- Protective footwear: Appropriate footwear, such as closed-toe shoes, can provide additional protection from punctures or spills, ensuring better protection in case of accidents.
The selection of PPE depends entirely on the risk assessment of a specific task. A simple blood draw requires gloves, while a major surgical procedure might require a gown, gloves, mask, eye protection, and protective footwear.
Q 11. How would you assess the risk of bloodborne pathogen exposure in a healthcare setting?
Assessing the risk of bloodborne pathogen exposure involves a systematic approach. It’s not a guess; it’s a careful evaluation of the environment and procedures.
First, I would identify all tasks and procedures that have the potential to involve contact with blood or other potentially infectious materials. Then, I would assess the frequency and intensity of that contact. A phlebotomist, for instance, has a higher risk than a receptionist. Next, I would evaluate the infectiousness of the pathogens involved. HIV and Hepatitis B have different transmission risks. Finally, I consider the susceptibility of the healthcare workers involved. Are there any workers with compromised immune systems?
This systematic approach allows for a targeted approach to risk mitigation, focusing resources on the highest-risk areas. A thorough risk assessment is vital for creating an effective infection control plan.
Q 12. Describe your experience with training healthcare workers on bloodborne pathogen safety.
I have extensive experience in training healthcare workers on bloodborne pathogen safety. My approach emphasizes hands-on learning and scenario-based training. I find that simply lecturing is ineffective; participants need to actively practice safe techniques.
My training sessions cover proper hand hygiene techniques, the appropriate use and disposal of PPE, the recognition of potential exposure situations, post-exposure protocols (including immediate steps and reporting), and the importance of adherence to standard precautions. I also incorporate interactive exercises, such as simulated exposure scenarios, to help workers develop quick reflexes and proper responses. For example, we might simulate a needlestick injury to practice appropriate immediate response.
Post-training, I provide ongoing support and answer questions. It’s crucial to maintain continuous reinforcement and address any concerns workers might have.
Q 13. What are some common engineering controls used to prevent bloodborne pathogen exposure?
Engineering controls are physical changes to the work environment designed to minimize exposure to bloodborne pathogens. They are typically built-in features or modifications rather than relying on individual behavior. Think of them as ‘built-in safety features’.
- Needleless systems: These devices eliminate the need for needles, significantly reducing the risk of needlestick injuries.
- Safety-engineered sharps containers: These containers are designed to prevent accidental needlesticks during disposal.
- Self-sheathing needles: These needles retract into a protective sheath after use, reducing the risk of accidental sticks.
- Biohazard sharps disposal containers: These puncture-resistant containers prevent accidental needlesticks and exposure to sharps during waste disposal.
- Improved ventilation systems: In laboratories, proper ventilation systems can remove airborne pathogens and infectious aerosols.
Q 14. What are work practice controls and provide examples?
Work practice controls are procedures that modify how tasks are performed to minimize exposure risks. These controls rely on worker behavior and adherence to protocols. They work in conjunction with engineering controls.
- Never recapping needles: This significantly reduces needlestick injuries.
- Proper disposal of sharps: Immediately placing used needles and other sharps into designated containers.
- Hand hygiene after every patient contact: This removes pathogens and reduces cross-contamination.
- Use of appropriate PPE consistently: Always wear gloves and other PPE when necessary, ensuring proper donning and doffing techniques.
- Careful handling of specimens: Taking precautions to prevent spills and splashes.
- Following proper decontamination procedures: Cleaning and disinfecting all contaminated surfaces promptly and thoroughly.
Work practice controls require diligent training and consistent enforcement. They’re not just about following rules; it’s about making safety a deeply ingrained habit for every healthcare worker.
Q 15. What is the role of an employee in reporting a potential bloodborne pathogen exposure?
Reporting a potential bloodborne pathogen exposure is crucial for preventing further spread and ensuring appropriate medical care. An employee’s role begins the moment they suspect exposure. This could be anything from a needlestick injury to contact with potentially infectious bodily fluids. The employee should immediately:
- Report the incident to their supervisor.
- Follow the facility’s established exposure control plan.
- Seek first aid, including proper wound cleansing and potentially post-exposure prophylaxis (PEP).
- Undergo medical evaluation and testing as recommended by the Occupational Safety and Health Administration (OSHA) guidelines.
For example, if a nurse experiences a needlestick injury, they should immediately report it to their supervisor, wash the affected area thoroughly, and begin the process of documentation and medical evaluation. Failing to report an exposure can lead to serious health consequences for the employee and potentially others.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the importance of medical surveillance in bloodborne pathogen prevention.
Medical surveillance is vital in bloodborne pathogen prevention because it allows for early detection and treatment of infections. Regular monitoring of employees potentially exposed to bloodborne pathogens helps protect their health and prevents the spread of disease. This surveillance often includes:
- Baseline testing for Hepatitis B surface antigen (HBsAg), Hepatitis C antibodies (anti-HCV), and HIV antibodies.
- Periodic testing, depending on the risk level and nature of exposure.
- Monitoring for symptoms consistent with these infections.
- Providing access to vaccinations, such as the Hepatitis B vaccine.
Imagine a healthcare worker who experiences multiple low-risk exposures over time. Regular testing can catch an infection early, allowing for more effective treatment and potentially preventing the transmission to others. This proactive approach drastically minimizes long-term health risks.
Q 17. How would you investigate a needlestick injury incident?
Investigating a needlestick injury requires a methodical approach to ensure thoroughness and compliance with regulations. The process involves the following steps:
- Immediate First Aid: Wash the area with soap and water, and if appropriate, use an antiseptic solution.
- Report the Incident: Immediately report the incident to the supervisor and follow the facility’s established procedures.
- Source Identification (if possible): Attempt to identify the source patient, if safe and feasible. This aids in determining the need for PEP.
- Documentation: Meticulous documentation is crucial. This includes details of the incident, including date, time, location, type of device involved, description of the exposure, and the identity of individuals involved.
- Testing: The source patient’s blood (if possible and with patient consent) and the exposed employee’s blood should be tested for relevant bloodborne pathogens.
- Post-Exposure Prophylaxis (PEP): Based on the assessment of risk and testing results, PEP may be recommended, which can involve medications to prevent infection.
- Follow-up: Regular follow-up appointments with healthcare professionals are essential to monitor the employee’s health and address any concerns.
Every step is crucial; incomplete documentation or delayed reporting can seriously hinder the efficacy of prevention strategies. The investigation should aim to identify gaps in safety protocols and implement corrective actions to prevent similar occurrences.
Q 18. Describe the proper procedures for handling and labeling of biological samples.
Proper handling and labeling of biological samples are paramount to prevent contamination and ensure accurate identification. Here’s how it’s done:
- Use appropriate personal protective equipment (PPE): This includes gloves, lab coats, and eye protection.
- Handle specimens carefully: Avoid splashing or aerosolization of the samples.
- Label containers clearly and completely: Labels must include the patient’s name, date and time of collection, sample type, and unique identifier. Use biohazard labels when appropriate.
- Use leak-proof containers: Transport samples in securely sealed containers to prevent spills.
- Proper disposal: Dispose of all used materials and contaminated PPE according to the facility’s protocols and regulations.
- Maintain cold chain: If samples need to be kept cold, ensure that the proper temperature is maintained throughout transportation and storage.
For example, a blood sample should be labeled with the patient’s name, medical record number, the date and time of collection, the type of sample (‘whole blood’, ‘serum’, etc.), and a unique identifier. Any spills should be reported and cleaned promptly with appropriate disinfectants.
Q 19. What is your experience with bloodborne pathogen training programs?
My experience with bloodborne pathogen training programs is extensive. I’ve been involved in developing, delivering, and evaluating numerous training programs across various healthcare settings. I have a deep understanding of OSHA guidelines and best practices for effective training. My focus has been on creating interactive and engaging training that utilizes case studies, practical demonstrations, and hands-on exercises to ensure comprehension and retention. I’ve also designed training materials for diverse audiences, including healthcare professionals, laboratory technicians, and housekeeping staff, tailoring the content to their specific roles and responsibilities. Evaluating the effectiveness of training programs using post-training assessments and observation has been crucial in continuously improving the training experience and ensuring compliance.
Q 20. Explain the differences between Hepatitis B, Hepatitis C, and HIV.
Hepatitis B, Hepatitis C, and HIV are all bloodborne pathogens, but they have distinct characteristics:
- Hepatitis B (HBV): A virus that attacks the liver, causing inflammation and potentially serious liver damage. There’s a vaccine to prevent HBV infection. Chronic infection can lead to cirrhosis and liver cancer.
- Hepatitis C (HCV): Another liver-damaging virus. There is no vaccine for HCV, but there are effective antiviral treatments that cure a high percentage of infections. Chronic HCV can also lead to cirrhosis and liver cancer.
- HIV (Human Immunodeficiency Virus): Attacks the immune system, leading to acquired immunodeficiency syndrome (AIDS). There is no cure for HIV, but antiretroviral therapy (ART) can suppress viral replication and significantly extend life expectancy. Untreated HIV can weaken the immune system, making individuals susceptible to opportunistic infections.
The key differences lie in their preventability (HBV has a vaccine), treatability (HCV has highly effective treatments, HIV has effective management therapies), and the specific organs they target (all three, while able to spread via blood, primarily target the liver (HBV and HCV) or the immune system (HIV)).
Q 21. How do you ensure compliance with relevant regulations and guidelines?
Ensuring compliance with relevant regulations and guidelines, primarily OSHA’s Bloodborne Pathogens Standard, requires a multi-pronged approach. This includes:
- Developing and implementing a comprehensive exposure control plan: This plan outlines procedures for preventing, identifying, and responding to bloodborne pathogen exposure incidents.
- Providing comprehensive employee training: Regular training ensures employees understand risks, safe practices, and emergency procedures.
- Providing necessary PPE: Making sure employees have access to and are trained on the proper use of appropriate PPE is vital.
- Monitoring and evaluating the effectiveness of the control plan: Regularly review the plan and procedures, making adjustments as needed based on workplace incidents and best practices.
- Maintaining accurate records: This includes documentation of employee training, exposure incidents, and medical evaluations.
- Staying updated on changes in regulations and guidelines: OSHA’s guidelines are periodically updated, and it’s crucial to remain abreast of these changes.
Regular audits and internal reviews help maintain compliance and proactively address any potential deficiencies in safety protocols. Proactive compliance ensures a safer work environment and protects both employees and patients.
Q 22. Describe your experience with incident reporting and record-keeping related to bloodborne pathogens.
Incident reporting and record-keeping for bloodborne pathogens are critical for preventing future exposures and ensuring compliance with OSHA regulations. My experience encompasses meticulous documentation of every incident, no matter how seemingly minor. This includes completing detailed incident reports, which outline the circumstances of the exposure, the individuals involved, the type of exposure (e.g., needlestick, splash), and the immediate actions taken. These reports follow a standardized format, ensuring consistency and completeness.
Furthermore, I’m experienced in maintaining accurate records of employee training, including completion dates, and the provision of post-exposure prophylaxis (PEP) if necessary. This meticulous record-keeping facilitates trend analysis, helping identify potential weaknesses in our safety protocols and allowing for targeted improvements. For example, a cluster of needlestick injuries in a particular department might indicate a need for improved sharps safety training or equipment upgrades in that area.
Maintaining confidentiality is paramount throughout this process. All records are kept securely, in accordance with HIPAA regulations. Regular audits ensure the accuracy and completeness of all documentation.
Q 23. How do you educate staff on the proper use and disposal of PPE?
Educating staff on proper PPE use and disposal is paramount to preventing bloodborne pathogen exposure. My approach involves a multi-pronged strategy, combining didactic learning with hands-on practice. I begin with initial training, covering the different types of PPE (gloves, gowns, masks, eye protection), their appropriate selection based on the task, and the correct donning and doffing procedures. This training is reinforced through regular refresher courses and competency assessments. I use various methods including:
- Interactive presentations: Utilizing visual aids and real-life scenarios to illustrate best practices.
- Hands-on workshops: Allowing staff to practice donning and doffing PPE under supervision.
- Case studies: Analyzing real-world incidents to highlight the consequences of incorrect PPE use.
- Posters and signage: Providing visual reminders throughout the facility.
Emphasis is placed on the importance of proper disposal of contaminated PPE into designated biohazard containers to prevent accidental exposure. We utilize color-coded containers and clearly labeled disposal points to facilitate correct disposal. Regular audits ensure proper compliance.
Q 24. What strategies would you use to improve bloodborne pathogen safety within a healthcare facility?
Improving bloodborne pathogen safety in a healthcare facility requires a comprehensive approach focusing on engineering controls, work practice controls, and administrative controls.
- Engineering controls: This involves modifying the work environment to minimize exposure risk. Examples include using safety-engineered sharps disposal containers, implementing needleless systems, and providing appropriate ventilation systems.
- Work practice controls: These are changes in work procedures to reduce the likelihood of exposure. Examples include hand hygiene protocols, the correct handling and disposal of sharps, and using appropriate techniques for recapping needles (never by hand).
- Administrative controls: These include policies, procedures, and training programs. A robust bloodborne pathogen exposure control plan, regular staff training, incident reporting and investigation protocols, and access to appropriate PPE are vital.
Furthermore, regular safety audits, employee feedback mechanisms, and a proactive approach to identifying and mitigating potential hazards are crucial for sustained improvement. For example, regularly reviewing incident reports can pinpoint recurring issues, which can then be addressed through targeted interventions.
Q 25. Describe a time you had to troubleshoot a safety issue related to bloodborne pathogens.
During a routine safety audit, I discovered that several nursing stations lacked sufficient sharps containers. This posed a significant risk as improperly discarded needles could lead to accidental punctures. My immediate action was to report this deficiency to the facility manager and request an immediate provision of additional sharps containers.
Simultaneously, I initiated an investigation into why the containers had been depleted prematurely. Through discussions with the nursing staff, we identified two key issues: inadequate staff training on proper sharps disposal techniques and a lack of readily accessible containers in high-use areas. We then implemented a focused retraining program emphasizing proper sharps disposal practices and strategically repositioned sharps containers to ensure better access throughout the nursing stations. The retraining incorporated hands-on practice and visual aids, dramatically improving the staff’s understanding. Post-intervention monitoring showed a significant reduction in improperly discarded sharps.
Q 26. How would you identify and address potential hazards related to bloodborne pathogens in a specific work environment?
Identifying and addressing potential hazards in a specific work environment necessitates a thorough risk assessment. This involves a systematic evaluation of all tasks and procedures that could potentially result in bloodborne pathogen exposure. This involves a multi-step approach:
- Walkthrough Survey: A physical inspection of the workplace, noting potential hazards such as spills, broken glassware, or improperly stored sharps.
- Task Analysis: Identifying high-risk tasks, such as phlebotomy, wound care, or cleaning contaminated surfaces.
- Employee Input: Gathering feedback from staff on perceived hazards and safety concerns.
- Hazard Evaluation: Determining the likelihood and severity of potential exposures for each identified hazard.
- Control Implementation: Developing and implementing control measures (engineering, work practice, administrative) to mitigate identified risks. This might involve providing additional PPE, revising work procedures, or modifying the physical work environment.
- Monitoring and Evaluation: Regularly assessing the effectiveness of control measures and making adjustments as needed.
For instance, in a dental clinic, a risk assessment might identify high-risk tasks like scaling and root planing. Control measures could include implementing high-volume evacuation systems to reduce aerosol production, using appropriate PPE, and ensuring the proper disposal of contaminated instruments.
Q 27. Explain the concept of Universal Precautions
Universal Precautions are a cornerstone of infection control, representing a philosophy of treating all human blood and certain body fluids as potentially infectious for bloodborne pathogens. This approach eliminates the need to identify specific high-risk individuals or situations, simplifying the safety measures. It emphasizes treating every patient and every specimen as potentially infectious, regardless of their known status.
Instead of focusing on specific risk factors, Universal Precautions mandate the consistent use of barrier protection, such as gloves, gowns, and eye protection, whenever there’s a potential for contact with blood or other potentially infectious materials. It also emphasizes proper hand hygiene before and after patient contact and the safe handling and disposal of contaminated materials. This approach greatly reduces the risk of transmission of bloodborne pathogens like HIV, HBV, and HCV.
Think of it like this: It’s better to be over-prepared than under-prepared when it comes to protecting yourself and your colleagues from infectious diseases. Universal Precautions are a proactive, comprehensive approach that ensures consistent safety practices for all healthcare workers.
Key Topics to Learn for Bloodborne Pathogen Exposure Prevention Interview
- Understanding Bloodborne Pathogens: Define bloodborne pathogens, including HIV, Hepatitis B and C, and other relevant viruses. Discuss their transmission routes and the severity of potential infections.
- Standard Precautions: Explain the principles of Standard Precautions and their application in various healthcare settings. Detail proper hand hygiene techniques, personal protective equipment (PPE) selection and use (gloves, gowns, masks, eye protection), and safe handling of sharps.
- Exposure Control Plan (ECP): Discuss the components of a comprehensive ECP, including exposure determination, methods of control (engineering controls, work practice controls, PPE), postexposure prophylaxis (PEP) procedures, and employee training requirements.
- Engineering and Work Practice Controls: Explain the difference between engineering and work practice controls and provide examples of each in a healthcare setting. Discuss their effectiveness in reducing exposure risk.
- Post-Exposure Management: Detail the steps to take following a potential exposure incident, including immediate first aid, reporting procedures, and the importance of seeking medical evaluation and follow-up.
- OSHA Regulations and Compliance: Summarize key OSHA requirements related to bloodborne pathogens and their impact on workplace safety and employee rights. Discuss record-keeping and compliance procedures.
- Decontamination and Waste Disposal: Explain proper procedures for cleaning and disinfecting contaminated surfaces and equipment. Discuss appropriate methods for disposing of regulated medical waste, including sharps containers and biohazard bags.
- Effective Communication and Teamwork: Discuss the importance of clear communication and teamwork in maintaining a safe working environment and minimizing the risk of bloodborne pathogen exposure.
- Scenario-Based Problem Solving: Prepare to analyze hypothetical situations involving potential bloodborne pathogen exposures and apply your knowledge of prevention methods to propose effective solutions.
Next Steps
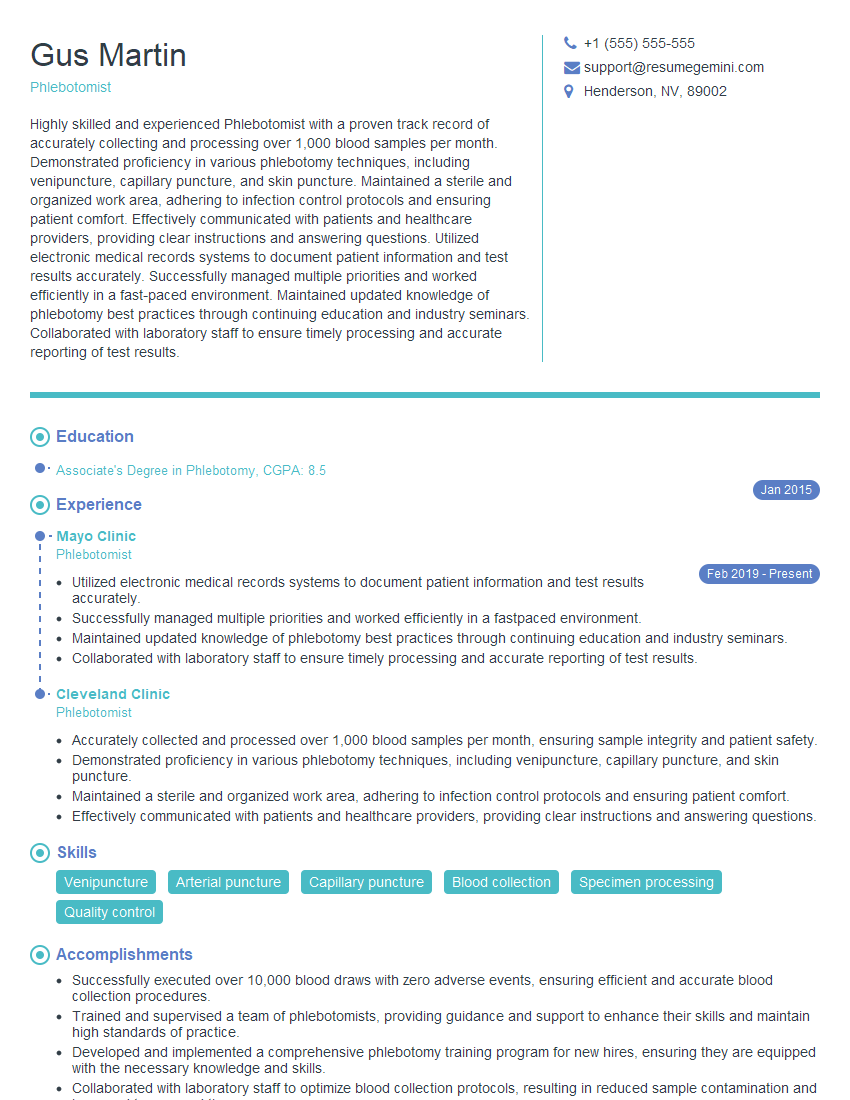
Mastering Bloodborne Pathogen Exposure Prevention demonstrates a crucial commitment to safety and professionalism, significantly enhancing your career prospects in healthcare and related fields. A strong, ATS-friendly resume is essential to showcasing your expertise to potential employers. To create a compelling resume that highlights your skills and experience in this critical area, we highly recommend using ResumeGemini. ResumeGemini provides a user-friendly platform and offers examples of resumes tailored to Bloodborne Pathogen Exposure Prevention to help you build a professional and effective document that grabs the attention of recruiters.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good