The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Bloodborne Pathogen Training interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Bloodborne Pathogen Training Interview
Q 1. What are the key components of OSHA’s Bloodborne Pathogens Standard?
OSHA’s Bloodborne Pathogens Standard is a comprehensive set of regulations designed to minimize the risk of exposure to bloodborne pathogens in the workplace. Its key components aim to protect healthcare workers and others potentially exposed to infectious materials. These key components include:
- Exposure Control Plan: Every workplace with potential exposure must have a written plan detailing how risks will be minimized. This includes identifying tasks and procedures involving exposure, selecting appropriate engineering and work practice controls, providing personal protective equipment (PPE), and establishing a post-exposure follow-up protocol.
- Engineering Controls: These are physical modifications to the work environment to reduce exposure. Examples include using safer medical devices (needleless systems), self-sheathing needles, and sharps disposal containers.
- Work Practice Controls: These are methods that change the way tasks are performed to minimize exposure. Examples include hand hygiene, proper handling of contaminated materials, and avoiding recapping needles.
- Personal Protective Equipment (PPE): OSHA mandates the provision of appropriate PPE, such as gloves, gowns, masks, and eye protection, whenever there’s a risk of exposure. The type of PPE will depend on the specific task.
- Housekeeping: The standard requires regular cleaning and decontamination of work areas to prevent the spread of bloodborne pathogens. Spills must be cleaned up immediately and appropriately.
- Training: Employers must provide comprehensive training to all employees with potential exposure, covering topics like risk recognition, PPE use, handling of contaminated materials, and post-exposure procedures.
- Hepatitis B Vaccination: Employers must offer the Hepatitis B vaccine free of charge to all employees at risk of exposure.
- Post-Exposure Evaluation and Follow-up: A detailed procedure must be in place to manage incidents like needlestick injuries, including immediate first aid, medical evaluation, and counseling.
Imagine a hospital lab: Their exposure control plan would detail how they handle blood samples, how sharps are disposed of, and what PPE technicians wear when processing samples. Failure to follow this standard can result in significant penalties for employers.
Q 2. Describe the different types of bloodborne pathogens.
Several bloodborne pathogens pose significant risks in occupational settings. The most notable are:
- Hepatitis B Virus (HBV): A virus that attacks the liver, causing both acute and chronic infections. It’s transmitted through contact with infected blood or other bodily fluids.
- Hepatitis C Virus (HCV): Another liver-damaging virus, HCV is primarily transmitted through blood-to-blood contact. Chronic infection is common, and it can lead to cirrhosis and liver cancer.
- Human Immunodeficiency Virus (HIV): The virus that causes Acquired Immunodeficiency Syndrome (AIDS), HIV weakens the immune system, making individuals vulnerable to opportunistic infections. Transmission occurs primarily through sexual contact, sharing needles, and exposure to infected blood.
It’s crucial to remember that these are not the only bloodborne pathogens, and others, though less common, can also pose a risk. Proper safety precautions should always be employed when handling any bodily fluids.
Q 3. Explain the difference between sterilization and disinfection.
Sterilization and disinfection are both crucial for controlling the spread of infection, but they differ significantly in their effectiveness:
- Sterilization: This process eliminates ALL forms of microbial life, including bacteria, viruses, fungi, and spores. It renders an object completely free of infectious agents. Methods include autoclaving (using high-pressure steam), dry heat sterilization, and gas sterilization (e.g., ethylene oxide).
- Disinfection: This process reduces the number of microorganisms on a surface or object to a safe level. It does not necessarily kill all microbes, particularly resistant spores. Disinfectants can be chemical (e.g., bleach solutions, alcohol) or physical (e.g., ultraviolet light).
Think of it this way: Sterilization is like completely wiping a whiteboard clean, while disinfection is like erasing most of what’s on the board but leaving some faint markings. Surgical instruments require sterilization, while cleaning a contaminated countertop might only require disinfection.
Q 4. What are the proper procedures for handling needles and sharps?
Proper handling of needles and sharps is paramount to prevent needlestick injuries. Key procedures include:
- Never recap needles: This is a major source of injuries. If recapping is unavoidable (rare), use a one-handed scoop technique.
- Dispose of sharps immediately and properly: Use puncture-resistant, clearly labeled sharps containers. Never overload containers, and replace them when they are nearly full.
- Handle sharps carefully and avoid dropping them: Always maintain control when using and passing sharp instruments.
- Use appropriate engineering controls: Whenever possible, use needleless systems or self-sheathing needles to reduce the risk.
- Immediately clean any contaminated surfaces: If a sharp is dropped or a spill occurs, the area must be cleaned and disinfected promptly.
Imagine a nurse administering an injection: She should never recap the needle after use, but rather immediately place it in the designated sharps container. This simple step significantly reduces the risk of injury.
Q 5. How should a needlestick injury be handled?
A needlestick injury is a serious incident requiring immediate action:
- Immediately wash the area with soap and water: This helps remove any blood or bodily fluids.
- Report the injury to your supervisor immediately: This is crucial for initiating the post-exposure prophylaxis (PEP) process.
- Seek medical attention: A healthcare professional will assess the risk of infection and determine the need for PEP.
- Follow your workplace’s post-exposure plan: This plan outlines the necessary steps for testing and treatment.
- Complete incident reports and documentation: This is essential for tracking and preventing future injuries.
Imagine a phlebotomist accidentally pricking themselves with a used needle: They must immediately wash the area, report the incident, and seek medical attention as outlined by the facility’s post-exposure plan.
Q 6. What PPE is required when handling potentially infectious materials?
The required PPE varies based on the task and the potential for exposure, but generally includes:
- Gloves: Always wear appropriate gloves when handling potentially infectious materials. The type of glove (e.g., nitrile, latex) depends on the specific risk.
- Gowns or aprons: Protective outerwear should be worn to prevent contamination of clothing.
- Masks or respirators: These are needed to protect against airborne particles or splashes of bodily fluids.
- Eye protection: Safety glasses or face shields protect the eyes from splashes or sprays.
A dental hygienist cleaning a patient’s teeth would likely use gloves, a mask, and eye protection to prevent exposure to blood or saliva.
Q 7. What is the purpose of a Post-Exposure Prophylaxis (PEP) plan?
A Post-Exposure Prophylaxis (PEP) plan is a crucial component of OSHA’s Bloodborne Pathogens Standard. It’s a detailed procedure for managing exposures to bloodborne pathogens, such as needlestick injuries or mucous membrane contact with infectious materials. Its purpose is to:
- Minimize the risk of infection: PEP aims to prevent the development of infection after exposure by providing appropriate medical interventions.
- Provide timely medical care: The plan outlines the steps for seeking medical evaluation and treatment quickly, maximizing the effectiveness of interventions.
- Protect employee health and safety: PEP ensures that exposed workers receive the necessary medical care and support.
- Comply with OSHA regulations: Having a documented PEP plan is a legal requirement for workplaces with potential exposure.
The plan would typically outline the steps to take after exposure, including immediate first aid, testing (for HBV, HCV, and HIV), and medication protocols. This ensures that appropriate medical attention is provided in a timely manner.
Q 8. Describe the proper methods for cleaning up a blood spill.
Cleaning up a blood spill requires a meticulous approach to prevent exposure to bloodborne pathogens. Think of it like this: you wouldn’t clean a kitchen spill with your bare hands; similarly, you shouldn’t handle blood without proper protection. The first step is always safety.
- Don Personal Protective Equipment (PPE): This includes gloves (nitrile or latex are preferred), a gown or lab coat, eye protection (goggles or a face shield), and possibly a mask, depending on the amount of blood and the potential for aerosolization.
- Absorb the spill: Use absorbent materials like paper towels or specialized spill kits designed for blood cleanup. Avoid spreading the spill by working from the outside in.
- Clean the area: After absorbing the blood, clean the affected area with a 10% bleach solution (1 part bleach to 9 parts water) or an EPA-registered disinfectant appropriate for bloodborne pathogens. Let the disinfectant sit for at least 10 minutes before wiping it up.
- Dispose of waste properly: All contaminated materials – absorbent materials, gloves, gowns, etc. – should be placed in appropriate biohazard containers for disposal according to your institution’s policies.
- Document the incident: Report the spill to your supervisor and document the date, time, location, and the steps taken for cleanup. This is crucial for tracking and preventing future incidents.
Remember, prompt and proper cleanup is vital in mitigating the risk of exposure. Never hesitate to seek assistance if you’re unsure about any part of the process.
Q 9. What are the signs and symptoms of Hepatitis B and HIV infection?
Hepatitis B and HIV infections present differently, although both are serious bloodborne illnesses. Hepatitis B (HBV), a viral infection affecting the liver, often shows initial symptoms similar to the flu: fatigue, abdominal pain, nausea, jaundice (yellowing of the skin and eyes), dark urine, and clay-colored stools. Some individuals may experience no symptoms at all, yet still be infectious. HIV (Human Immunodeficiency Virus), which can lead to AIDS, has a more variable presentation. Acute infection can manifest with flu-like symptoms, but many people remain asymptomatic for years. As the virus progresses to AIDS, symptoms may include weight loss, fever or night sweats, fatigue, swollen lymph glands, diarrhea, skin rashes, or opportunistic infections (infections that wouldn’t usually affect a person with a healthy immune system).
It’s crucial to remember that the absence of symptoms doesn’t mean the absence of infection. If you suspect exposure to bloodborne pathogens, it’s essential to seek immediate medical attention. Post-exposure prophylaxis (PEP) can significantly reduce the risk of infection.
Q 10. Explain the importance of employee training regarding bloodborne pathogens.
Employee training on bloodborne pathogens is paramount for creating a safe and healthy work environment. It’s not just about compliance; it’s about protecting the health and well-being of your employees and preventing costly legal issues. Comprehensive training equips employees with the knowledge and skills to:
- Recognize and avoid hazards: Identifying situations and materials that pose a risk of exposure.
- Use PPE correctly: Understanding the types of PPE available, how to don and doff them properly, and the limitations of each type.
- Follow proper cleanup procedures: Knowing how to safely and effectively clean up blood and other potentially infectious materials.
- Understand exposure control plans: Knowing the institution’s specific policies and procedures for managing bloodborne pathogen exposures.
- Recognize signs and symptoms of infection: Knowing what to look for in themselves and their colleagues, and how to react responsibly.
- Understand reporting procedures:Knowing who to contact and how to report an exposure event.
This training significantly reduces the risk of exposure, promotes a culture of safety, and reduces the liability of an organization.
Q 11. How often should Bloodborne Pathogen training be renewed?
The frequency of Bloodborne Pathogen training renewal is dictated by OSHA (Occupational Safety and Health Administration) guidelines and often by individual organizational policies. While OSHA doesn’t explicitly state a rigid timeframe, it’s generally recommended to renew training annually. This ensures that employees remain updated on best practices, changes in procedures, and advancements in prevention and response techniques. More frequent training might be required if there are significant changes in procedures, new equipment, or a documented exposure event within the workplace. Regular refreshers ensure that the information remains top of mind and that employees continue to practice safe work habits.
Q 12. What are the elements of a comprehensive Exposure Control Plan?
A comprehensive Exposure Control Plan (ECP) is a detailed document outlining the methods and procedures to minimize or eliminate employee exposure to bloodborne pathogens. Think of it as a roadmap to a safer workplace. It should include:
- Exposure determination: Identifying job tasks or activities that may involve contact with blood or other potentially infectious materials.
- Engineering controls: Implementing strategies that physically remove or isolate the hazard, such as sharps containers and self-sheathing needles.
- Work practice controls: Implementing specific work practices to minimize or eliminate exposure, such as handwashing protocols and proper disposal methods.
- PPE: Specifying the appropriate PPE for various tasks, including gloves, gowns, masks, and eye protection.
- Housekeeping: Outlining procedures for routine cleaning and disinfection of work surfaces.
- Post-exposure evaluation and follow-up: A detailed plan for managing any exposure event, including providing medical evaluation and follow-up to exposed employees.
- Hepatitis B vaccination: Offering the Hepatitis B vaccine to all employees at risk of exposure.
- Training: Describing the training program for all employees with potential exposure, including the frequency and content.
- Record keeping: Specifying how exposure incidents, training records, and other relevant information will be maintained.
A well-structured ECP minimizes risk and demonstrates a commitment to employee safety.
Q 13. Describe the role of engineering controls in preventing exposure.
Engineering controls represent the most effective way to prevent exposure to bloodborne pathogens. These are physical modifications to the workplace environment that eliminate or minimize the risk of exposure *before* it even occurs. Examples include:
- Sharps disposal containers: Puncture-resistant containers for disposing of needles, scalpels, and other sharp instruments, preventing accidental needlesticks.
- Self-sheathing needles: Needles that automatically retract into a protective sheath after use, reducing the risk of accidental needlesticks.
- Safety-engineered devices: Equipment designed to prevent accidental contact with blood or other body fluids, such as needleless systems for intravenous injections.
- Biohazard bags and containers: Specially designed containers for storing and transporting contaminated waste materials.
- Improved ventilation: Proper ventilation systems in labs or other areas where bloodborne pathogens might be aerosolized.
Engineering controls prioritize prevention, making them the most desirable method for controlling exposure.
Q 14. What are work practice controls and provide examples.
Work practice controls are procedural changes that reduce or eliminate the risk of exposure. They complement engineering controls by focusing on how tasks are performed. Examples include:
- Hand hygiene: Regular and thorough handwashing with soap and water or use of an alcohol-based hand rub is crucial before and after any procedure involving potential exposure.
- Proper handling of sharps: Never recapping needles, using one-handed scoop technique for sharps disposal, and ensuring proper disposal in designated containers.
- Safe disposal of contaminated materials: Using appropriate biohazard bags and containers for disposal of all contaminated materials.
- Body substance isolation (BSI) precautions: Treating all bodily fluids as potentially infectious.
- Avoiding direct contact with blood or body fluids: Using appropriate barriers, such as gloves and gowns, to prevent contact with bodily fluids.
- Use of aseptic techniques: Following sterile procedures to avoid contamination during medical procedures.
These work practices, when consistently followed, significantly reduce the risk of exposure to bloodborne pathogens.
Q 15. What are the different types of Hepatitis viruses?
Hepatitis refers to an inflammation of the liver, primarily caused by viral infections. Several Hepatitis viruses exist, each with its own transmission characteristics and severity. The most significant in the context of bloodborne pathogens are Hepatitis B (HBV), Hepatitis C (HCV), and Hepatitis D (HDV).
- Hepatitis B Virus (HBV): A serious liver infection transmitted through contact with infected blood, semen, or other bodily fluids. It can lead to chronic liver disease, cirrhosis, and liver cancer. Vaccination is highly effective in preventing HBV infection.
- Hepatitis C Virus (HCV): Primarily spread through contact with infected blood, often via intravenous drug use or contaminated needles. Many HCV infections become chronic, resulting in long-term liver damage. While there’s no vaccine, effective treatments exist to cure HCV.
- Hepatitis D Virus (HDV): A defective virus that requires the presence of HBV to replicate and cause infection. HDV infection occurs only in individuals already infected with HBV. It leads to a more severe form of hepatitis than HBV alone.
- Hepatitis A and E: While not strictly bloodborne, Hepatitis A and E are important to mention because they are transmitted through the fecal-oral route and can cause serious liver inflammation. Proper hygiene practices are crucial for prevention.
Understanding the differences between these viruses is crucial for implementing appropriate prevention and control measures in healthcare and other settings where exposure risk is present.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the transmission routes of bloodborne pathogens.
Bloodborne pathogens are transmitted through direct contact with infected blood or other potentially infectious bodily fluids. The major routes of transmission include:
- Direct Contact with Blood: This involves direct exposure to infected blood through needlestick injuries, cuts, or splashes to mucous membranes (eyes, nose, mouth).
- Sexual Contact: Transmission can occur through unprotected sexual intercourse with an infected individual.
- Percutaneous Exposure: This refers to exposure through the skin, such as needlestick injuries or cuts from contaminated sharps.
- Permucosal Exposure: This is exposure through mucous membranes like the eyes, nose, or mouth, usually from splashes or sprays of contaminated blood or body fluids.
- Mother-to-Child Transmission (Vertical Transmission): Certain bloodborne pathogens, like HBV and HCV, can be passed from an infected mother to her child during pregnancy, delivery, or breastfeeding.
Think of it like this: bloodborne pathogens are tiny invaders that can only enter your body through breaks in the skin or direct contact with mucous membranes. Understanding these routes is key to effective prevention.
Q 17. What is the role of personal protective equipment (PPE)?
Personal Protective Equipment (PPE) serves as a barrier between healthcare workers and potentially infectious materials. It’s a critical component of infection control and significantly reduces the risk of exposure to bloodborne pathogens. PPE includes:
- Gloves: Prevent direct contact with blood and other body fluids.
- Gowns: Protect skin and clothing from contamination.
- Masks or Respirators: Reduce the risk of inhaling infectious aerosols.
- Eye Protection: Shields eyes from splashes of blood or body fluids.
- Shoe Covers: Protect footwear from contamination.
Proper use of PPE is essential. Think of it like wearing a suit of armor against microscopic invaders. Each piece of PPE serves a specific purpose in minimizing your risk of exposure.
Q 18. What are the limitations of PPE?
While PPE is highly effective, it’s crucial to understand its limitations. PPE is not foolproof. Some limitations include:
- Improper Use: Incorrect application, removal, or handling can compromise its protective function. Imagine wearing a helmet backwards – it wouldn’t offer the same protection.
- Equipment Failure: Tears, punctures, or degradation of PPE can lead to breaches in protection.
- Limited Protection: PPE does not offer 100% protection. Small exposures can still occur even with proper use. It’s always better to assume all bodily fluids are potentially infectious.
- Comfort and Heat Stress: Wearing PPE for extended periods can be uncomfortable and lead to heat stress, especially in warm environments.
It’s a misconception that PPE is a complete guarantee. It’s an essential element, but it’s just one part of a comprehensive infection control strategy.
Q 19. Describe the process for evaluating and selecting PPE.
Selecting appropriate PPE involves a risk assessment. Consider the specific task and the potential for exposure to bloodborne pathogens.
- Risk Assessment: Identify tasks with potential exposure to blood or other infectious materials. Consider the type of procedure, the volume of blood, and the likelihood of splashing.
- PPE Selection: Choose the appropriate PPE based on the risk assessment. For example, gloves are always necessary, but gowns may be needed for procedures with a higher risk of splashes.
- Fit and Comfort: Ensure the selected PPE fits properly and is comfortable to wear for extended periods. Ill-fitting PPE can compromise protection.
- Training: Provide proper training on the correct use, donning, and doffing (removal) procedures for each type of PPE.
- Regular Evaluation: Regularly assess the effectiveness of the chosen PPE and make adjustments if needed. Are there new procedures that require different PPE? Has there been a change in risk assessment?
A well-defined process is critical to protect workers and ensure compliance with safety regulations.
Q 20. How are contaminated sharps disposed of properly?
Contaminated sharps pose a significant risk of needlestick injuries and should be handled and disposed of with extreme care. The proper procedure includes:
- Never Recap Needles: Recapping needles increases the risk of accidental needle sticks. Use a safety-engineered device or dispose of the needle directly into a sharps container.
- Use Sharps Containers: Dispose of all contaminated sharps in a puncture-resistant, closable sharps container. These containers are specifically designed to prevent accidental needlesticks during handling and disposal.
- Proper Sharps Container Placement: Sharps containers should be readily accessible at the point of use and appropriately labeled.
- Do Not Overfill: Never overfill the sharps container. Once it reaches the fill line, it should be sealed and replaced.
- Proper Disposal of Sharps Containers: Follow the facility’s protocol for the proper disposal of filled sharps containers. This often involves a specialized waste disposal service.
The goal is to minimize risk and prevent injuries. Sharps disposal should never be taken lightly.
Q 21. What are the requirements for labeling hazardous materials?
Hazardous materials, including those containing bloodborne pathogens, must be clearly labeled according to OSHA and other relevant regulations. Labels should include:
- Name of the Hazardous Material: Clearly state the specific hazard, such as "Biohazardous Waste" or "Infectious Substances".
- Hazard Warning Symbol: Use the universally recognized biohazard symbol – a symbol featuring a orange-red triangle containing a black three-legged figure.
- Precautions: Include any necessary safety precautions for handling the material.
- Date of Preparation or Collection: This helps maintain accurate tracking of the material.
Proper labeling is essential for preventing accidental exposure and ensuring safe handling by all personnel. Consistent labeling is vital for workplace safety and compliance.
Q 22. Describe the importance of proper hand hygiene.
Proper hand hygiene is the cornerstone of preventing the spread of bloodborne pathogens. It’s a simple yet incredibly effective method to drastically reduce the risk of infection. Think of your hands as potential vectors—they can carry pathogens from one surface to another, including your eyes, nose, and mouth. Effective hand hygiene involves more than just a quick rinse.
The process should include:
- Washing with soap and water: This is the gold standard, particularly when dealing with visible soil or contamination. Rub hands vigorously for at least 20 seconds, covering all surfaces, including under nails. Rinse thoroughly and dry with a clean towel or air dry.
- Using alcohol-based hand rub: When soap and water aren’t readily available, an alcohol-based hand rub (at least 60% alcohol) is an effective alternative. Apply a sufficient amount to cover all hand surfaces and rub until dry.
Consistent and thorough hand hygiene prevents the transmission of pathogens like Hepatitis B, Hepatitis C, and HIV, safeguarding both healthcare workers and patients.
Q 23. What is the difference between universal precautions and standard precautions?
While both Universal Precautions and Standard Precautions aim to prevent the transmission of infectious agents, there’s a key difference. Universal Precautions, an older term, assumed that all blood and body fluids were potentially infectious. This approach, while effective, could be overly cautious in some situations.
Standard Precautions, the current and preferred approach, broadens the scope to include all patients, regardless of their known infection status. It emphasizes the use of barrier precautions (gloves, gowns, masks, eye protection) whenever contact with blood, body fluids, non-intact skin, and mucous membranes is anticipated. This accounts for a wider range of pathogens, not just bloodborne ones. Standard Precautions are a more comprehensive and inclusive strategy for infection control.
In essence, Standard Precautions evolved from Universal Precautions to provide a more comprehensive and nuanced approach to infection control, adapting to the understanding of various transmission routes.
Q 24. What are the reporting requirements for bloodborne pathogen exposure incidents?
Reporting requirements for bloodborne pathogen exposure incidents vary depending on the location and the specific regulations in place (OSHA guidelines in the US, for example). However, generally, any exposure incident must be reported promptly. This usually involves:
- Immediate First Aid: Wash the exposed area thoroughly. Report the incident to your supervisor immediately.
- Documentation: A detailed report of the incident must be completed, including the circumstances of the exposure, the source individual (if known), and the type of exposure (e.g., needlestick, splash to eyes).
- Post-Exposure Prophylaxis (PEP): Depending on the exposure and the source individual’s status, PEP (medical treatment to prevent infection) may be necessary and should be initiated as soon as possible.
- Medical Evaluation: A thorough medical evaluation will assess the risk of infection and determine the need for testing and follow-up care.
- Regulatory Reporting: The incident is typically reported to the appropriate regulatory authorities (OSHA, etc.), often within a specific timeframe.
Failure to report an exposure incident can have serious consequences for both the exposed individual and the facility.
Q 25. What are the ethical considerations related to bloodborne pathogen exposure?
Ethical considerations in bloodborne pathogen exposure center around the well-being and rights of both the exposed individual and the source individual (if identifiable). Key ethical principles include:
- Confidentiality: Maintaining the confidentiality of both individuals is crucial. Only essential personnel need to know about the incident.
- Informed Consent: The exposed individual must be fully informed about the risks, testing options, and available treatment (PEP). They must provide informed consent before any procedures are undertaken.
- Non-discrimination: The exposed individual should not face any discrimination or stigma as a result of the exposure.
- Duty of Care: Employers have a duty of care to provide a safe working environment and ensure appropriate training and procedures are in place to minimize the risk of exposure.
- Transparency and Honesty: Open communication between the exposed individual, employer, and healthcare providers is vital for effective management of the situation.
Addressing these ethical considerations builds trust and ensures the best possible outcome for all involved.
Q 26. How do you ensure compliance with relevant regulations?
Ensuring compliance with relevant regulations, such as OSHA’s Bloodborne Pathogens Standard, requires a multi-faceted approach:
- Comprehensive Training Program: Implementing a thorough training program that covers all aspects of bloodborne pathogen exposure prevention, including proper hand hygiene, use of personal protective equipment (PPE), and emergency response procedures.
- Regular Updates: Keeping training materials current with the latest regulations and best practices.
- Exposure Control Plan: Developing and implementing a detailed Exposure Control Plan that outlines procedures for handling potentially infectious materials, managing exposure incidents, and providing access to PEP.
- Record Keeping: Maintaining accurate records of training, exposure incidents, and PEP administration.
- Regular Inspections and Audits: Conducting regular workplace inspections and audits to ensure compliance with the Exposure Control Plan and all relevant regulations.
- Employee Involvement: Encouraging employee participation in the development and implementation of safety procedures to foster a culture of safety.
Proactive compliance minimizes risks, protects employees, and avoids potential penalties.
Q 27. What is your experience with developing and delivering bloodborne pathogen training?
I have extensive experience in developing and delivering Bloodborne Pathogen training programs for various healthcare settings, including hospitals, clinics, and long-term care facilities. My training programs are tailored to the specific needs of the audience and incorporate interactive elements such as case studies, demonstrations, and practical exercises to enhance learning and retention.
I utilize a variety of teaching methods, including lectures, group discussions, and hands-on simulations, to ensure that trainees understand the importance of proper infection control techniques and are equipped to handle potential exposure incidents. I emphasize practical application and provide ample opportunity for questions and clarification. My programs incorporate the latest guidelines and regulations, ensuring that trainees are up-to-date on best practices.
Feedback from previous training sessions consistently highlights the clarity, engagement, and practical value of my approach.
Q 28. Describe a situation where you had to address a bloodborne pathogen exposure incident.
In one instance, a nurse experienced a needlestick injury during a patient procedure. Following established protocol, the incident was immediately reported to the supervisor. The nurse received first aid, which included thorough washing of the affected area. We initiated the process of identifying the patient’s bloodborne pathogen status (with their consent, of course) and promptly contacted the occupational health department to arrange for post-exposure prophylaxis (PEP). The incident was meticulously documented, including details of the exposure, the steps taken, and the medical follow-up. A thorough review of the procedure and the involved equipment was conducted to identify and rectify any potential contributing factors to the incident, preventing similar occurrences in the future.
This experience reinforced the importance of having clear protocols, proper training, and a supportive environment for reporting and managing such incidents.
Key Topics to Learn for Bloodborne Pathogen Training Interview
- Understanding Bloodborne Pathogens: Defining bloodborne pathogens, transmission routes (e.g., needlestick injuries, mucous membrane contact), and examples of key pathogens (HIV, Hepatitis B and C).
- Exposure Control Plan (ECP): Understanding the components of an ECP, including engineering controls (e.g., sharps containers, self-sheathing needles), work practice controls (e.g., hand hygiene, proper disposal of contaminated materials), and personal protective equipment (PPE) selection and use (e.g., gloves, gowns, masks).
- Exposure Incidents: Procedures to follow after an exposure incident, including immediate first aid, reporting procedures, and post-exposure prophylaxis (PEP).
- Housekeeping and Decontamination: Proper cleaning and disinfection techniques for spills and contaminated surfaces, understanding different disinfectants and their effectiveness.
- Regulatory Compliance: Familiarity with OSHA’s Bloodborne Pathogens Standard and relevant regulations, including record-keeping requirements.
- Applying Knowledge in Scenarios: Practicing problem-solving by working through hypothetical scenarios involving exposure incidents or contaminated materials. Think critically about the appropriate response in each situation.
- Infection Prevention and Control: Beyond the specifics of bloodborne pathogens, understanding broader infection control principles, such as standard precautions, will demonstrate a comprehensive understanding of workplace safety.
Next Steps
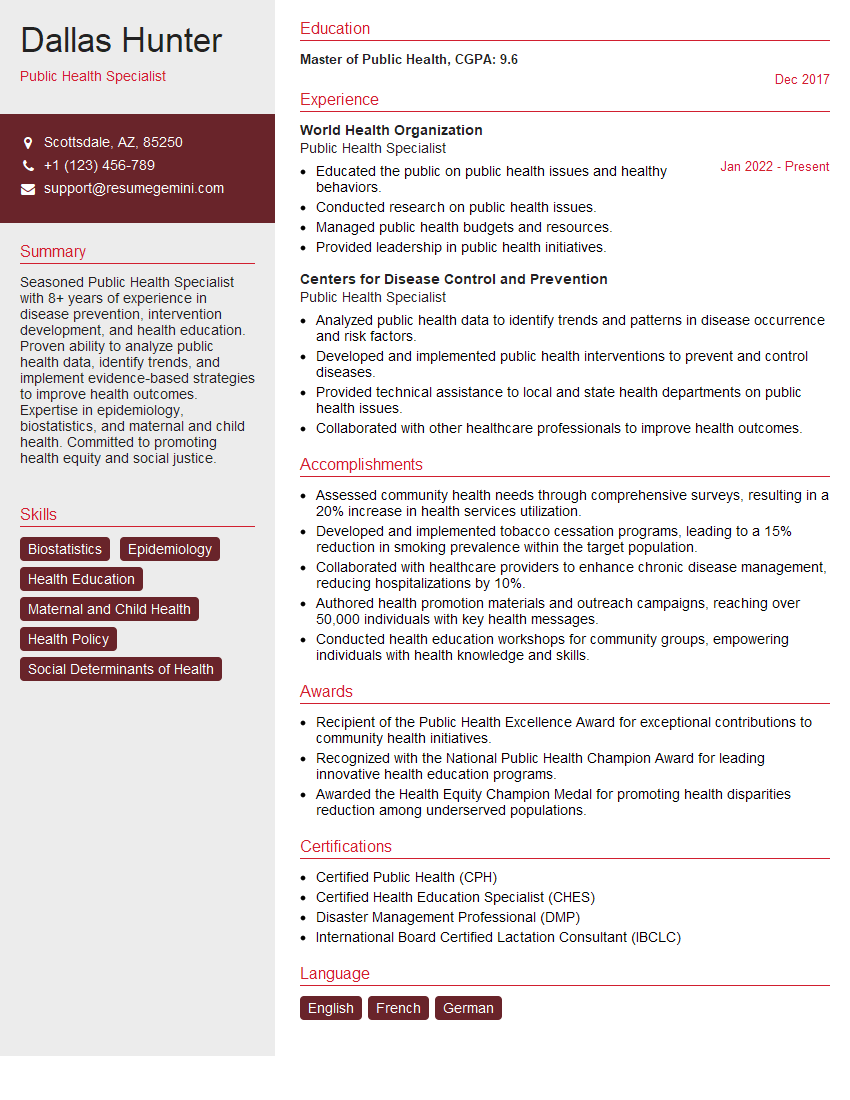
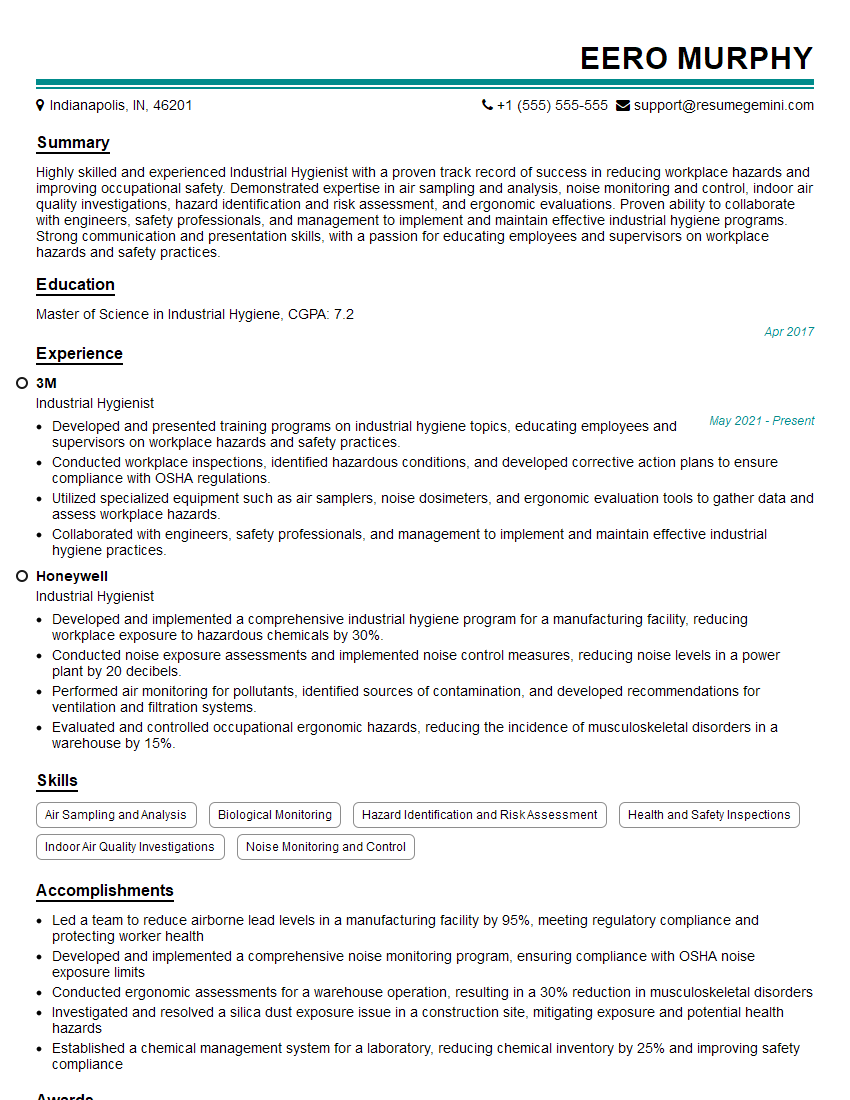
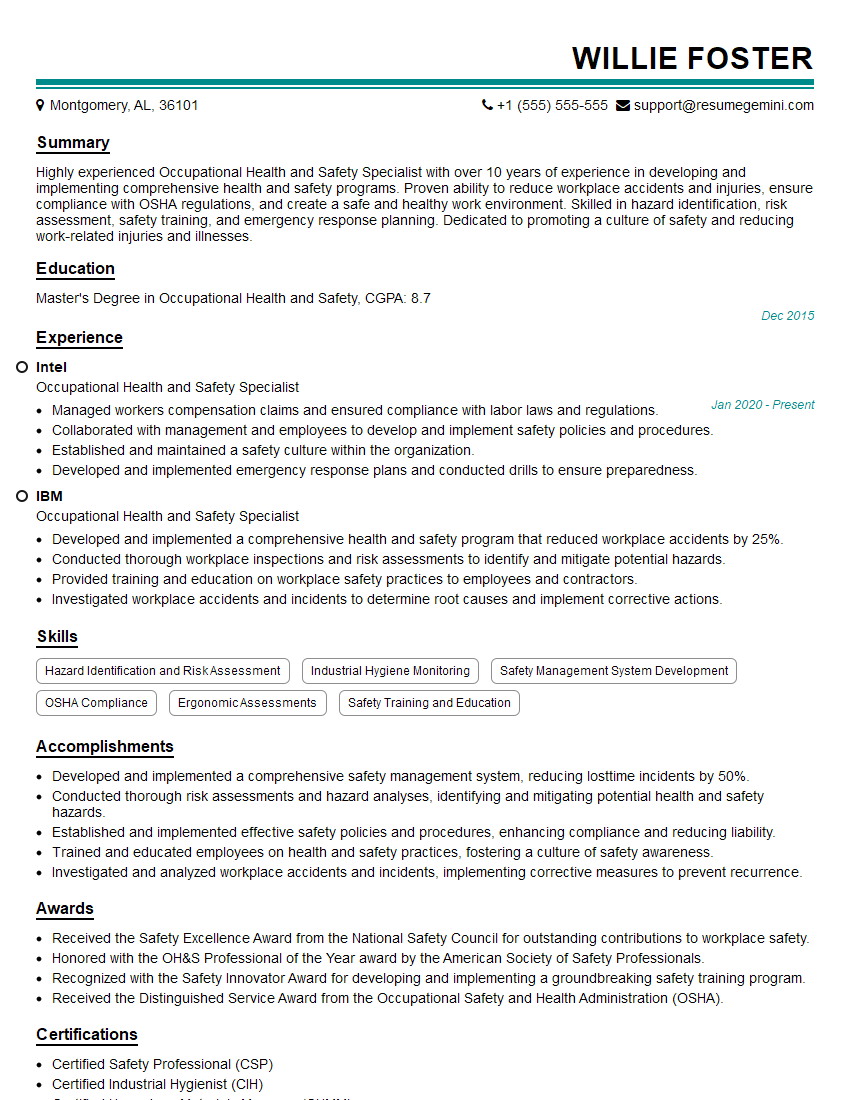
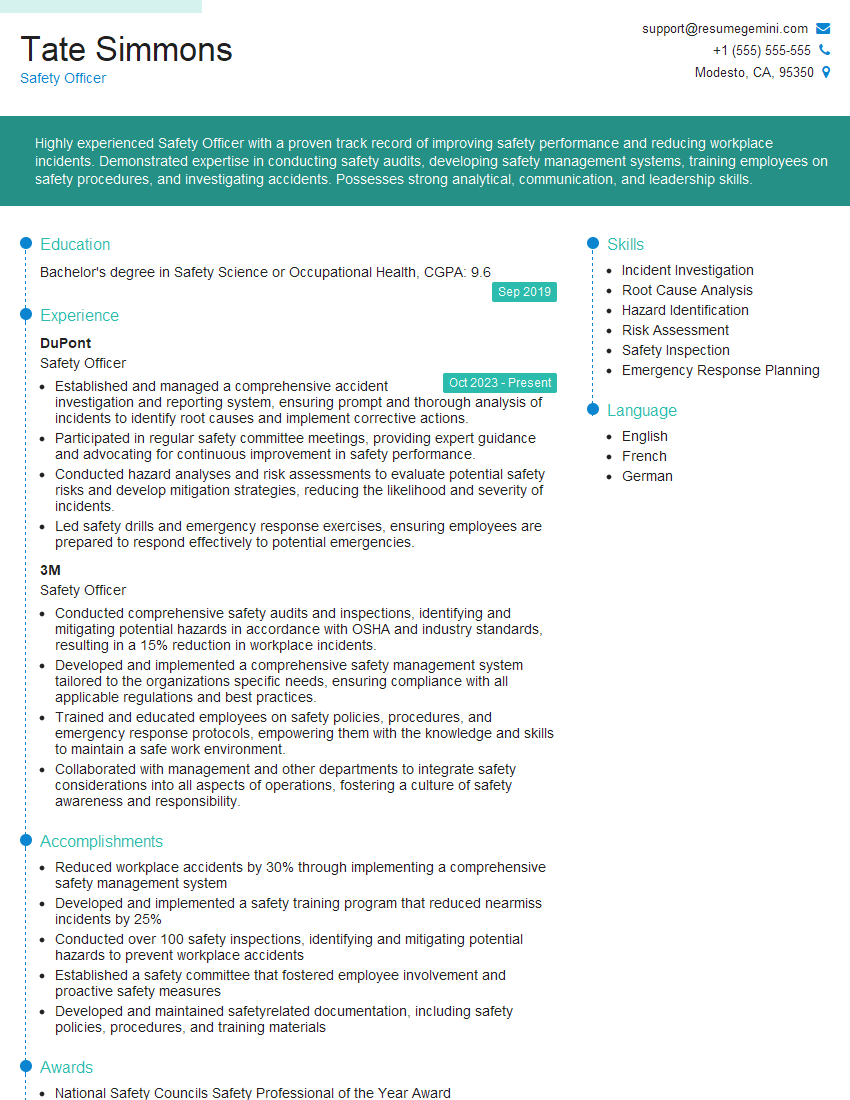
Mastering Bloodborne Pathogen Training significantly enhances your qualifications for various healthcare and safety-related roles, demonstrating your commitment to workplace safety and patient well-being. This knowledge is highly valued by employers and can open doors to exciting career opportunities. To maximize your chances of landing your dream job, crafting a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your skills and experience are highlighted effectively. Examples of resumes tailored to Bloodborne Pathogen Training are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good