Cracking a skill-specific interview, like one for Experience in Bioelectronics and Biomedical Devices, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Experience in Bioelectronics and Biomedical Devices Interview
Q 1. Explain the difference between biocompatible and biodegradable materials.
Biocompatibility and biodegradability are distinct but related properties of materials used in biomedical devices. Biocompatibility refers to a material’s ability to perform with an appropriate host response in a specific application. This means the material doesn’t cause harmful reactions like inflammation, toxicity, or rejection by the body. Biodegradability, on the other hand, describes a material’s ability to be broken down into harmless byproducts by biological processes within the body. A material can be biocompatible but not biodegradable (like titanium used in implants), or it can be both (like certain polymers used in sutures or drug delivery systems). For example, a heart valve implant needs to be biocompatible to prevent clotting and inflammation, but it doesn’t necessarily need to be biodegradable since it’s intended for long-term use. Conversely, a biodegradable scaffold used for tissue engineering needs both properties: to support cell growth and then safely disappear as the tissue regenerates.
Q 2. Describe your experience with different types of biosensors.
My experience encompasses a wide range of biosensor technologies. I’ve worked extensively with electrochemical biosensors, which utilize changes in electrical current or potential to detect analytes like glucose in blood glucose meters. I’ve also worked with optical biosensors, where changes in light absorption or fluorescence are measured, often using techniques like surface plasmon resonance for detecting protein-protein interactions. Furthermore, I have experience with piezoelectric biosensors, employing the piezoelectric effect to transduce biological events into electrical signals. For instance, I was involved in a project developing a piezoelectric sensor for detecting bacterial growth based on their metabolic activity. Each type presents unique challenges and advantages; for example, electrochemical sensors are often inexpensive and easy to miniaturize, while optical sensors can provide high sensitivity and specificity. The choice of biosensor depends heavily on the application, analyte, and desired performance characteristics.
Q 3. What are the challenges in designing implantable biomedical devices?
Designing implantable biomedical devices presents a unique set of challenges. The foremost is biocompatibility – ensuring the device doesn’t trigger an adverse immune response or cause tissue damage. Then there’s the issue of long-term stability and reliability; the device must function reliably for years, often in a harsh physiological environment. Miniaturization is also crucial, particularly for minimally invasive procedures. Power sources are another significant hurdle; powering implantable devices for extended periods without requiring frequent replacements is a major design consideration. Finally, signal transmission and data acquisition need to be solved; accurately and reliably collecting data from the implant and transmitting it to an external device requires careful engineering. For example, designing a long-term implantable drug delivery system requires careful consideration of material degradation rates and drug release kinetics to avoid unexpected side effects or premature device failure.
Q 4. How do you ensure the sterility of a biomedical device during manufacturing?
Ensuring sterility in biomedical device manufacturing is paramount to patient safety. We employ a multi-step process, starting with meticulous cleanroom design and stringent environmental control. All manufacturing processes occur within ISO Class 7 or better cleanrooms, minimizing particulate and microbial contamination. Components are thoroughly cleaned and sterilized before assembly using methods such as ethylene oxide gas sterilization or gamma irradiation. These methods effectively eliminate or reduce microbial loads to acceptable levels. After assembly, the devices are packaged in sterile containers using aseptic techniques, preventing recontamination. Sterility is then rigorously validated using bioburden testing and sterility assurance level (SAL) calculations to confirm the effectiveness of our sterilization processes and ensure devices meet regulatory requirements. This is not a one-size-fits-all approach; the chosen sterilization method is dependent on the device materials and design.
Q 5. Explain your understanding of signal processing in bioelectronic devices.
Signal processing in bioelectronic devices is crucial for extracting meaningful information from the often noisy biological signals. It involves several stages. First, raw signals are amplified and filtered to remove noise and unwanted artifacts. This often requires specialized techniques like adaptive filtering or wavelet denoising. Next, signal features are extracted using methods such as Fourier transforms to analyze frequency components or time-domain analysis to identify patterns. These extracted features are then processed using machine learning algorithms to classify different physiological states or events. Finally, the processed data is used to control the device or provide feedback to the user. For instance, in a neural prosthesis, raw neural signals are processed to control prosthetic limb movements. Effective signal processing is critical to improve the accuracy, reliability, and performance of bioelectronic devices.
Q 6. What are the regulatory pathways for medical device approval (e.g., FDA)?
The regulatory pathways for medical device approval, such as those by the FDA (Food and Drug Administration) in the US, are complex and vary depending on the device’s risk classification. Devices are categorized into classes (I, II, and III) based on their potential risks. Class I devices, posing the lowest risk, require minimal regulatory oversight. Class II devices undergo more rigorous premarket review, involving submission of data demonstrating safety and effectiveness. Class III devices, representing the highest risk (e.g., implantable pacemakers), require premarket approval (PMA), including extensive clinical trials to demonstrate safety and effectiveness. The regulatory process includes submission of documentation, such as design specifications, manufacturing processes, test data, and clinical trial results. The FDA assesses these materials to ensure compliance with regulatory requirements. Navigating these regulations requires specialized expertise and often involves substantial time and resources.
Q 7. Describe your experience with different types of microfabrication techniques.
My experience in microfabrication techniques is extensive. I’m proficient in photolithography, a cornerstone technique for creating micro-scale patterns on substrates. This involves using UV light to expose photoresist material, allowing precise etching of patterns for creating microfluidic channels, electrodes, or other features. I’ve also worked extensively with thin-film deposition techniques, such as sputtering and evaporation, to deposit materials like metals or insulators onto substrates. These are essential for fabricating electrodes or insulating layers within bioelectronic devices. I’m experienced with etching techniques such as wet etching and dry etching (e.g., plasma etching) to define the three-dimensional structures of microdevices. Additionally, I have experience with soft lithography, which uses elastomeric molds to create microstructures, particularly useful for creating microfluidic devices. The choice of microfabrication techniques depends on the specific device requirements and the materials involved; for instance, creating complex 3D microstructures might require techniques like deep reactive-ion etching.
Q 8. How would you troubleshoot a malfunctioning bioelectronic device?
Troubleshooting a malfunctioning bioelectronic device requires a systematic approach. It’s like detective work, carefully examining clues to pinpoint the problem. First, I’d carefully review the device’s operational history, checking for any recent changes or unusual events that might have preceded the malfunction. Then, I’d move to a visual inspection, looking for any obvious physical damage, loose connections, or corrosion.
Next, I’d systematically test each component of the device, starting with the simplest and most accessible. This might involve checking power supply, signal integrity, sensor functionality, and data transmission pathways. I’d use specialized diagnostic tools and software to assist in this process, such as oscilloscopes to measure signal quality or impedance analyzers to assess the electrical characteristics of the device and its interface with the body.
If the problem persists, I’d consult the device’s technical specifications and troubleshooting guides. If the fault cannot be identified using these methods, more sophisticated techniques might be employed such as simulations to replicate and understand device behavior under fault conditions. For example, if a neural implant is malfunctioning, I might use biocompatible simulations to test different hypotheses on the cause of failure. Ultimately, documenting every step of the troubleshooting process is crucial for future analysis and preventing similar failures.
Q 9. Explain the principles of electrophysiology relevant to biomedical devices.
Electrophysiology is the study of the electrical properties of biological cells and tissues. In the context of biomedical devices, it’s fundamental because many devices interact with the body’s electrical signals. For example, a pacemaker relies on sensing the heart’s electrical activity (ECG) to regulate its rhythm. Understanding the principles of electrophysiology is vital for designing devices that safely and effectively interact with the body’s complex electrical environment.
Key principles include:
- Membrane Potentials: The difference in electrical potential across a cell membrane, crucial for nerve and muscle function.
- Action Potentials: Brief, rapid changes in membrane potential that transmit signals along nerves and muscles.
- Synaptic Transmission: Communication between nerve cells via chemical or electrical signals.
- Biopotential Signals: Electrical signals generated by the body, such as ECG, EEG, and EMG.
Knowledge of these principles allows engineers to design electrodes that effectively couple with biological tissues, choose appropriate signal processing techniques, and prevent unintended stimulation or interference with the body’s natural electrical activity. For instance, understanding the frequency range of various biopotentials informs the design of filters in biomedical amplifiers to minimize noise and artifact interference.
Q 10. What are the key considerations for designing a user-friendly biomedical device?
Designing a user-friendly biomedical device is paramount for patient compliance and effective therapy. It’s not just about functionality; it’s about ease of use, comfort, and safety. Key considerations include:
- Intuitive Interface: The device should be easy to operate, with clear instructions and minimal complexity. This might involve the use of simple graphical interfaces or voice commands.
- Ergonomics: The device should be comfortable to wear or use, considering factors like size, weight, and placement on the body. Consideration should be given to specific patient populations, such as children or the elderly.
- Feedback Mechanisms: The device should provide clear feedback to the user about its status and operation. This might involve visual displays, auditory cues, or haptic feedback. Consider the impact of visual or auditory impairments on feedback mechanisms.
- Safety Features: The device should incorporate safety features to prevent accidental harm or malfunction. This includes safeguards against overcurrent, overheating, and unintended stimulation.
- Accessibility: The design should accommodate diverse needs, such as accessibility for users with visual or auditory impairments.
For example, a wearable insulin pump should be easy to fill, have a clear display showing insulin levels and delivery rate, and include alarms for low insulin levels or malfunctions. Thorough user testing and feedback are crucial throughout the design process to ensure usability.
Q 11. Describe your experience with data analysis and interpretation from bioelectronic experiments.
My experience with data analysis in bioelectronic experiments involves a multi-step process. It begins with data acquisition, using specialized software to record biopotential signals and other relevant physiological data. This raw data often contains noise and artifacts, requiring careful signal processing techniques, such as filtering and artifact rejection, to enhance its quality. This might involve using techniques like wavelet denoising or independent component analysis.
After preprocessing, I employ various analytical methods, depending on the research question. For example, time-domain analysis might focus on features like amplitude and duration of signals, whereas frequency-domain analysis (using Fourier transforms) might reveal dominant frequencies and their changes over time. I also use statistical methods to analyze the significance of observed effects and to control for confounding factors. For example, we might utilize advanced statistical models like mixed-effects models or generalized linear models to account for inter-subject variability.
I’m proficient in using statistical software packages like MATLAB, Python (with libraries such as SciPy and scikit-learn), and R for data analysis and visualization. I’ve used these tools to identify correlations between bioelectronic signals and physiological changes, test hypotheses about device efficacy, and develop predictive models. One example is our recent work on characterizing the relationship between neural activity patterns and motor control using machine learning algorithms, allowing us to create better brain-computer interface control schemes.
Q 12. Explain your understanding of different types of biopotential signals (EEG, ECG, EMG).
Biopotential signals are electrical signals generated by the body’s biological processes. Understanding their characteristics is crucial for developing effective bioelectronic devices. Here are three common types:
- Electroencephalogram (EEG): Measures electrical activity in the brain using electrodes placed on the scalp. EEG signals are characterized by their low amplitude (microvolts) and wide frequency range (from less than 1 Hz to over 100 Hz). Different frequency bands are associated with different states of consciousness and brain activity (e.g., delta waves during sleep, beta waves during wakefulness).
- Electrocardiogram (ECG): Measures electrical activity in the heart using electrodes placed on the chest. ECG signals have a more defined waveform, representing the electrical depolarization and repolarization of the heart chambers. Analysis of ECG provides vital information about heart rate, rhythm, and conduction pathways.
- Electromyogram (EMG): Measures electrical activity in muscles using electrodes placed on the skin surface or inserted into the muscle. EMG signals reflect the activity of motor units, providing information about muscle contraction, fatigue, and neurological disorders.
Each type of signal has unique characteristics in terms of amplitude, frequency, and waveform, requiring specialized signal processing techniques for optimal analysis. For example, noise cancellation is crucial for accurately detecting subtle changes in EEG signals.
Q 13. How do you ensure the long-term stability and reliability of a bioelectronic device?
Ensuring the long-term stability and reliability of a bioelectronic device is crucial for its safety and efficacy. It requires a multi-faceted approach that considers various aspects of the design, materials, and manufacturing process. Imagine building a house that needs to withstand decades of weather and use – it requires careful planning and quality materials.
Here’s how we approach it:
- Biocompatibility: Choosing biocompatible materials that will not cause adverse reactions or degradation over time is vital. Thorough testing in relevant biological environments is required.
- Robust Design: Designing the device to withstand mechanical stress, vibrations, and other environmental factors ensures its durability. This might involve using protective coatings, hermetic sealing, or shock absorbers.
- Quality Control: Strict quality control measures during manufacturing are critical to minimize defects and ensure consistent performance. This involves rigorous testing at multiple stages of the manufacturing process.
- Power Management: Efficient power management is crucial to prolong battery life and prevent device failure. This could involve using low-power components and optimization of power consumption.
- Regular Maintenance and Calibration: Designing devices that allow for easy maintenance and calibration enhances long-term performance and safety.
For instance, implantable devices undergo rigorous biocompatibility testing to ensure that materials don’t degrade over time and cause immune reactions. Similarly, external devices are designed with durable casings and connectors to resist wear and tear from daily use.
Q 14. What are the ethical considerations of using bioelectronic devices?
The use of bioelectronic devices raises several important ethical considerations. It’s not simply about the technology; it’s about its responsible and ethical application.
- Informed Consent: Patients must be fully informed about the risks and benefits of using a bioelectronic device before giving their consent. This information must be easily understood and free from coercion.
- Data Privacy: Bioelectronic devices often collect sensitive physiological data, raising concerns about privacy and security. Robust data protection measures are essential to prevent unauthorized access or misuse of this information.
- Equity and Access: Ensuring equitable access to bioelectronic devices, regardless of socioeconomic status or geographical location, is crucial. Addressing affordability and distribution challenges is important.
- Safety and Efficacy: Rigorous testing and evaluation are necessary to ensure the safety and efficacy of bioelectronic devices. This includes careful monitoring for unintended side effects.
- Long-Term Effects: The long-term effects of using bioelectronic devices are often unknown, requiring ongoing monitoring and research. This involves careful assessment of both the benefits and potential risks associated with long-term use.
For example, brain-computer interfaces raise profound questions about personal identity and autonomy, requiring careful consideration of the potential impact on users’ cognitive functions and decision-making capabilities. Ethical guidelines and regulations must be established and adhered to ensure responsible innovation in this field.
Q 15. Describe your experience with different types of biomaterials (e.g., polymers, metals, ceramics).
My experience with biomaterials spans a wide range, encompassing polymers, metals, and ceramics. Each material class offers unique properties crucial for different biomedical applications.
- Polymers: I’ve worked extensively with polymers like polydimethylsiloxane (PDMS), poly(lactic-co-glycolic acid) (PLGA), and various hydrogels. PDMS is excellent for its flexibility and biocompatibility, often used in microfluidic devices and flexible electronics. PLGA, a biodegradable polymer, is ideal for drug delivery systems and temporary implants as it degrades over time, eliminating the need for a second surgery. Hydrogels, with their high water content, mimic the body’s natural environment and are useful in tissue engineering scaffolds and contact lenses.
- Metals: Metals like titanium, stainless steel, and platinum are frequently used due to their strength and biocompatibility. Titanium, for example, is widely used in orthopedic implants due to its high strength-to-weight ratio and excellent corrosion resistance. Stainless steel, though less biocompatible than titanium, is commonly employed in less demanding applications due to its cost-effectiveness. Platinum, with its excellent electrical conductivity, is used in electrodes for neural stimulation and recording.
- Ceramics: Bioceramics like hydroxyapatite and alumina are utilized for their bone-bonding capabilities. Hydroxyapatite, a major component of natural bone, promotes osseointegration (the direct bonding of bone to the implant surface), making it perfect for bone replacement and dental implants. Alumina’s high strength and wear resistance are valuable in hip and knee replacements.
Selecting the appropriate biomaterial involves careful consideration of factors like mechanical strength, biocompatibility, degradation rate, and the specific application requirements. For instance, in a flexible neural probe, a soft, biocompatible polymer like PDMS is favored over a rigid ceramic.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you design for biofouling mitigation in implantable devices?
Biofouling, the unwanted accumulation of biological material on a device’s surface, is a significant challenge for implantable devices. It can lead to device malfunction, inflammation, and infection. Mitigation strategies focus on creating surfaces that resist protein adsorption and cell adhesion.
- Surface modification: Techniques like creating hydrophilic surfaces (water-loving), employing zwitterionic polymers, or grafting polyethylene glycol (PEG) onto the surface can prevent protein adsorption. These modifications make the surface less attractive to proteins and cells.
- Antimicrobial coatings: Incorporating antimicrobial agents like silver nanoparticles or antibiotics into the device material can inhibit bacterial growth and prevent biofilm formation. However, careful consideration is required to minimize potential toxicity.
- Material selection: Selecting inherently bioinert materials can minimize biofouling. For example, materials like highly-ordered pyrolytic graphite (HOPG) have demonstrated excellent antifouling properties.
- Surface texturing: Carefully designed surface textures can hinder cell adhesion and biofilm formation. This approach has shown promising results in various studies.
A multi-pronged approach, combining several of these methods, is often the most effective. For example, a device could use a bioinert base material, modified with a PEG coating and incorporated antimicrobial nanoparticles to provide robust protection against biofouling. Each design must be tested rigorously in vitro and in vivo to assess its effectiveness.
Q 17. What are the different types of wireless power transfer techniques used in implantable devices?
Wireless power transfer (WPT) is crucial for implantable devices, eliminating the need for external wires that can cause infection and limit movement. Several techniques exist:
- Inductive coupling: This is the most common method. A primary coil outside the body generates a magnetic field that induces current in a secondary coil implanted within the device. The efficiency depends heavily on the distance between the coils and their alignment.
- Capacitive coupling: This method uses an electric field to transfer power. Two capacitor plates are used, one external and one internal. It can be more efficient over short distances but less robust to misalignment.
- Radio frequency (RF) energy harvesting: External RF energy is collected by a receiver antenna inside the implanted device and converted into usable power. This method offers potentially longer range but requires more sophisticated circuitry.
- Ultrasound: Ultrasound energy can be transmitted through tissue and converted to electricity using piezoelectric materials. This approach is still under development but offers potential for deeper implants.
The optimal technique depends on factors like power requirements, implant depth, desired range, and overall system complexity. For example, inductive coupling is often sufficient for near-body implants like pacemakers, while RF energy harvesting might be necessary for deeper implants requiring more power.
Q 18. Describe your experience with circuit design for biomedical applications.
My experience in circuit design for biomedical applications focuses on low-power, high-reliability circuits that are biocompatible and safe. I’ve worked extensively with:
- Analog circuit design: This is crucial for signal conditioning and processing from biological sensors. Designing amplifiers with low noise and high input impedance is critical for accurately capturing weak biosignals. I use techniques such as operational amplifier (op-amp) circuits and instrumentation amplifiers to achieve this. Example:
An instrumentation amplifier with a gain of 1000 to amplify a microvolt-level biopotential. - Digital circuit design: Used for data processing, control systems, and communication. I have experience designing microcontrollers, digital signal processing (DSP) units, and communication interfaces to interface with external devices. For instance, I’ve implemented algorithms for real-time signal analysis on an embedded microcontroller. Example:
A microcontroller program that processes an electrocardiogram (ECG) signal and triggers an alert based on predefined thresholds. - Mixed-signal circuit design: Combining analog and digital components is common. This allows for efficient signal processing and data acquisition. For example, I’ve designed a system that combines an analog front-end for signal amplification with a digital back-end for data analysis and wireless transmission.
All designs are rigorously tested and simulated using tools like SPICE to ensure functionality, power consumption, and safety within the context of the biological environment. Emphasis is always placed on minimizing power consumption to extend battery life for implantable devices.
Q 19. How do you perform risk analysis and mitigation for biomedical devices?
Risk analysis and mitigation are paramount in biomedical device development. I use a systematic approach following established standards like ISO 14971.
- Hazard identification: This involves identifying potential hazards associated with the device throughout its lifecycle, from design and manufacturing to use and disposal. This may involve brainstorming sessions, Failure Mode and Effects Analysis (FMEA), and reviewing existing literature.
- Risk analysis: This step assesses the likelihood and severity of each identified hazard. Risk is typically expressed as a combination of probability and severity. This may be a qualitative or quantitative approach.
- Risk evaluation: This evaluates the acceptability of the identified risks. If risks are deemed unacceptable, mitigation strategies are developed.
- Risk control: This involves implementing measures to reduce or eliminate risks. Examples include redesigning a component to improve reliability, implementing stricter quality control measures, or adding warning labels.
- Risk monitoring: Continuous monitoring and review of risks are critical throughout the device’s lifecycle. This ensures that potential risks are addressed proactively.
For example, in designing an implantable neurostimulator, potential hazards could include battery failure, lead fracture, or device malfunction. A risk analysis would assess the probability and severity of each hazard, and mitigation measures, such as redundant power sources and rigorous quality control during manufacturing, would be implemented. This process is documented thoroughly, forming an integral part of the device’s regulatory submission.
Q 20. Explain your understanding of different types of packaging for biomedical devices.
Packaging for biomedical devices is critical for sterility, protection, and long-term stability. The choice of packaging depends on the device type, intended use, and storage conditions.
- Sterile packaging: Methods like ethylene oxide sterilization or gamma irradiation require specialized packaging to maintain sterility after processing. Tyvek pouches and blister packs are frequently used.
- Hermetic sealing: For implants requiring long-term stability, hermetic sealing is necessary to protect the device from moisture and oxygen. This may involve using glass or metal containers with welded seams.
- Protective packaging: Packaging should protect the device from physical damage during shipping and handling. This might include foam inserts, corrugated cardboard boxes, and specialized shipping containers.
- Biocompatible packaging materials: Materials used in packaging should not leach harmful substances into the device or the body. Testing for biocompatibility is required.
The complexity of the packaging increases with the device’s sensitivity. For example, a simple disposable diagnostic sensor might be packaged in a blister pack, while a complex implantable device would require multiple layers of packaging to ensure sterility, protect from damage, and provide a barrier against environmental factors.
Q 21. What are the key challenges in miniaturizing bioelectronic devices?
Miniaturizing bioelectronic devices presents many significant challenges:
- Power consumption: Smaller devices often have limited space for batteries, necessitating ultra-low-power circuits and energy-efficient components. This is a major design constraint.
- Signal-to-noise ratio (SNR): Miniaturization can increase noise levels, reducing the SNR of sensitive biosignals. Careful circuit design and noise reduction techniques are crucial.
- Heat dissipation: Smaller devices have a limited surface area for heat dissipation, requiring advanced thermal management strategies to prevent overheating.
- Component density and integration: Integrating many components into a small space requires sophisticated packaging techniques and potentially advanced manufacturing processes like 3D printing or microfabrication.
- Biocompatibility: As device dimensions decrease, the surface area increases relative to volume, increasing the importance of biocompatible materials and surface treatments to reduce adverse reactions.
Addressing these challenges requires an interdisciplinary approach, combining expertise in materials science, microfabrication, circuit design, and biocompatibility testing. Advanced packaging techniques and innovative circuit architectures are needed to create truly miniaturized, high-performance bioelectronic devices.
Q 22. Explain your experience with different types of sterilization techniques.
Sterilization is crucial for biomedical devices to eliminate harmful microorganisms and ensure patient safety. My experience encompasses several techniques, each with its pros and cons.
- Autoclaving (steam sterilization): This is a widely used method involving high-pressure saturated steam. It’s effective against a broad range of microorganisms but unsuitable for heat-sensitive materials. For example, I’ve used autoclaving extensively for sterilizing stainless steel surgical instruments.
- Ethylene Oxide (EtO) sterilization: This gas sterilization is effective for heat-sensitive materials like plastics and polymers commonly found in implantable devices. However, EtO is a known carcinogen, requiring careful handling and specialized equipment. I’ve incorporated EtO sterilization in projects involving complex polymeric microfluidic devices.
- Gamma irradiation: This method uses ionizing radiation to sterilize medical devices. It’s highly effective and penetrates packaging, making it suitable for pre-packaged items. However, it can alter the properties of certain materials. I’ve used gamma irradiation for sterilizing disposable sensors and catheters.
- Dry heat sterilization: This method uses high temperatures in the absence of moisture and is suitable for glassware and certain metal instruments. It’s less effective than autoclaving and requires longer exposure times.
- Plasma sterilization: This emerging technology utilizes low-temperature plasma to sterilize devices. It’s effective, environmentally friendly, and suitable for heat-sensitive materials. Currently exploring its application for sterilizing miniature biosensors.
The choice of sterilization method depends on the device material, its design, and the intended application. A thorough risk assessment is crucial to selecting the most appropriate and effective technique.
Q 23. How do you select appropriate materials for a specific biomedical application?
Material selection for biomedical applications is critical, demanding careful consideration of biocompatibility, mechanical properties, and manufacturing feasibility. The process involves a multi-step approach:
- Defining requirements: First, we clearly define the device function, intended use (e.g., implantable, external), and required performance characteristics (e.g., strength, flexibility, electrical conductivity).
- Biocompatibility assessment: This involves evaluating the material’s interaction with biological tissues and fluids. ISO 10993 provides a comprehensive standard for biocompatibility testing. Factors like cytotoxicity, genotoxicity, and inflammation potential are assessed. I’ve used various biocompatibility testing methods, including cell culture assays and in vivo studies.
- Mechanical properties: Materials must possess adequate strength, elasticity, and fatigue resistance depending on the intended application. For example, a flexible stent requires different material properties than a rigid bone plate. I frequently use FEA to predict and optimize mechanical behavior.
- Manufacturing considerations: The chosen material should be readily manufacturable using cost-effective techniques. This might involve injection molding, machining, 3D printing, or other methods.
- Regulatory compliance: The selected material must comply with relevant regulatory standards and guidelines to ensure patient safety.
For example, in designing a neurostimulator, I chose a biocompatible polymer for the encapsulation to ensure long-term stability and prevent adverse reactions, while using platinum for the electrodes due to its excellent biocompatibility and electrical conductivity.
Q 24. What are the key considerations for designing a biocompatible drug delivery system?
Designing a biocompatible drug delivery system requires careful consideration of several key factors to ensure efficacy and safety:
- Drug properties: The physicochemical properties of the drug, including its solubility, stability, and degradation rate, influence the choice of delivery system. For example, a hydrophobic drug requires a different delivery strategy than a hydrophilic drug.
- Target site: The location of the target tissue or organ dictates the route of administration (e.g., intravenous, oral, topical, implantable) and the system’s design. For localized delivery, implantable systems are preferred.
- Release kinetics: The desired drug release profile (e.g., sustained release, pulsatile release, controlled release) is critical. This is often achieved through the material’s properties, device geometry, or the incorporation of smart stimuli-responsive materials.
- Biocompatibility: All materials used in the system must be biocompatible to avoid adverse reactions. This involves selecting materials that are non-toxic, non-immunogenic, and do not elicit inflammation.
- Degradability: The system’s degradation rate is crucial, particularly for implantable devices. Biodegradable polymers offer advantages in reducing the need for a second surgery to remove the device.
- Manufacturing feasibility: The chosen design must be feasible to manufacture using efficient and cost-effective techniques.
For instance, designing a system for controlled release of an anti-cancer drug to a specific tumor site might involve incorporating the drug into biodegradable microspheres and implanting them near the tumor. This allows for localized drug delivery, minimizing systemic side effects.
Q 25. Explain your understanding of the principles of tissue engineering.
Tissue engineering aims to regenerate or repair damaged tissues using a combination of cells, biomaterials, and growth factors. The principles involve:
- Scaffold design: A biocompatible scaffold provides structural support for cell attachment, growth, and differentiation. The scaffold’s architecture, porosity, and degradation rate are crucial for optimal tissue regeneration. Different materials like collagen, hydrogels, and ceramics are used depending on the application.
- Cell seeding and culture: The chosen cells (e.g., stem cells, fibroblasts) are seeded onto the scaffold and cultured under appropriate conditions to promote cell proliferation and differentiation into the desired tissue type.
- Growth factors and signaling molecules: These molecules promote cell growth, differentiation, and tissue formation. They can be incorporated into the scaffold or delivered separately.
- Bioreactor technology: Bioreactors provide a controlled environment for cell culture, mimicking the in vivo environment and facilitating tissue development.
- Implantation and integration: Once the tissue construct is formed, it is implanted into the patient, where it integrates with the surrounding tissue.
For example, in bone tissue engineering, a porous scaffold made of bioactive ceramics is seeded with bone marrow-derived stem cells and cultured in a bioreactor. The resulting bone tissue construct can then be implanted to repair bone defects.
Q 26. Describe your experience with Finite Element Analysis (FEA) in biomedical device design.
Finite Element Analysis (FEA) is an indispensable tool in biomedical device design, enabling the prediction and optimization of device performance under various loading conditions. My experience with FEA involves:
- Stress and strain analysis: FEA helps determine stress and strain distribution within the device under physiological loads, ensuring that the device can withstand the stresses experienced during its use. For example, simulating the stress on a hip implant during walking.
- Fatigue analysis: Predicting fatigue life and potential failure points is crucial for implantable devices. FEA allows us to assess the device’s durability over its lifespan.
- Fluid-structure interaction (FSI): In applications involving fluid flow, such as blood flow in cardiovascular devices, FSI analysis is used to assess the device’s performance and its interaction with blood.
- Bioheat transfer analysis: This is essential in analyzing the temperature distribution within and around implantable devices, especially in situations where heat generation is significant, ensuring safe operation.
- Optimization studies: FEA allows us to optimize the device geometry and material properties to enhance performance and minimize stress concentrations.
I typically use commercial FEA software such as ANSYS or Abaqus. For instance, in designing a catheter, I used FEA to optimize its flexibility and prevent kinking while ensuring sufficient strength to withstand insertion forces. This helped improve patient comfort and reduce the risk of device failure.
Q 27. How do you design experiments to validate the performance of a bioelectronic device?
Validating the performance of a bioelectronic device requires a rigorous experimental design incorporating in vitro and in vivo studies:
- In vitro testing: This involves evaluating device performance in a controlled laboratory setting using cell cultures or tissue models. This allows us to assess biocompatibility, electrical stimulation efficacy, and sensor performance. For example, we would test the biocompatibility of the device materials on cell lines representative of the target tissue.
- In vivo testing: Once in vitro testing is successful, in vivo studies in animal models are conducted to evaluate device functionality and safety in a living organism. This involves implanting the device in animals and monitoring its performance over time. Ethical considerations and appropriate animal models are crucial.
- Electrophysiological recordings: These recordings are used to measure the electrical signals produced or modulated by the device. In a neurostimulator, for example, this may involve recording nerve activity before, during, and after stimulation.
- Histological analysis: Post-implantation histological analysis is used to evaluate the tissue response to the device, looking for signs of inflammation or fibrosis.
- Statistical analysis: All data is rigorously analyzed using appropriate statistical methods to determine the significance of the results. This includes sample size calculations to ensure statistical power.
The specific experimental design depends on the device’s function and intended application. For example, designing experiments to assess a neural implant’s ability to restore motor function may involve behavioral tests in addition to electrophysiological recordings. A well-defined experimental protocol is crucial to generate reliable and reproducible data that support the device’s efficacy and safety.
Key Topics to Learn for Your Bioelectronics and Biomedical Devices Interview
Landing your dream role in bioelectronics and biomedical devices requires a strong understanding of the field’s core principles and their practical applications. This section outlines key areas to focus on during your preparation.
- Biomaterial Selection and Characterization: Understand the properties of different biomaterials (metals, polymers, ceramics) and their suitability for specific biomedical applications. Consider factors like biocompatibility, degradation rates, and mechanical properties.
- Biosensors and Bioelectronics: Explore the principles of various biosensors (optical, electrochemical, piezoelectric) and their application in diagnostics, therapeutics, and monitoring systems. Be prepared to discuss signal transduction mechanisms and data analysis techniques.
- Medical Imaging and Instrumentation: Familiarize yourself with common medical imaging modalities (MRI, CT, ultrasound) and their underlying principles. Consider the design and function of associated instrumentation and data processing techniques.
- Biomedical Signal Processing: Understand the techniques used to process and analyze biological signals (EEG, ECG, EMG) for diagnosis and treatment. This includes filtering, noise reduction, and feature extraction.
- Drug Delivery Systems: Explore different approaches to targeted drug delivery, including implantable devices, micro- and nanoparticles, and controlled-release systems. Discuss the challenges and advantages of each method.
- Regulatory Affairs and Compliance: Gain a basic understanding of the regulatory landscape for biomedical devices, including FDA regulations and quality control processes. This demonstrates a commitment to safety and ethical considerations.
- Problem-solving and Design Thinking: Prepare to discuss your approach to solving complex engineering problems within the biomedical field. Highlight your experience with design methodologies and iterative development processes.
Next Steps: Maximize Your Job Prospects
Mastering these key areas will significantly enhance your interview performance and demonstrate your readiness for a challenging and rewarding career in bioelectronics and biomedical devices. This expertise is highly sought after, leading to excellent career growth opportunities and impactful contributions to healthcare.
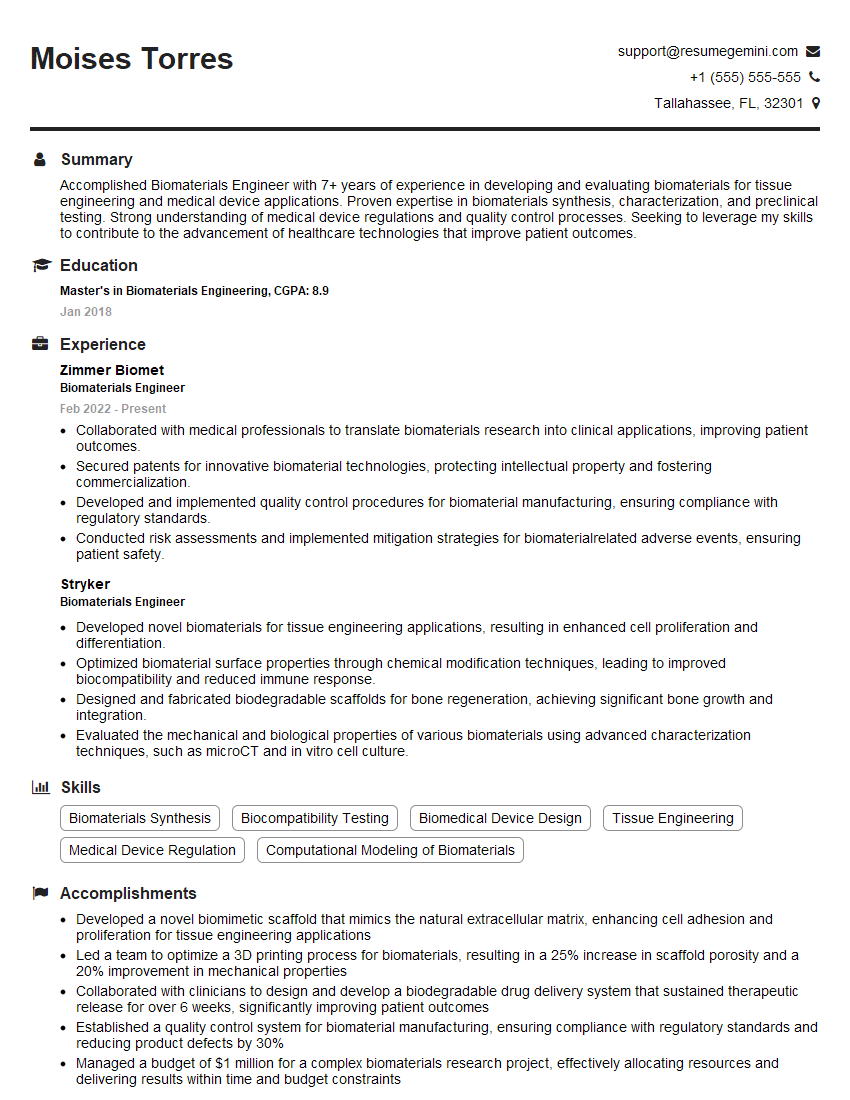
To further strengthen your application, creating a compelling and ATS-friendly resume is crucial. A well-structured resume highlights your skills and experience effectively, increasing your chances of getting noticed by recruiters. We recommend using ResumeGemini, a trusted resource for building professional and impactful resumes. ResumeGemini provides examples of resumes tailored to the bioelectronics and biomedical devices field, guiding you to showcase your qualifications effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good