Are you ready to stand out in your next interview? Understanding and preparing for Fertility Recommendations interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Fertility Recommendations Interview
Q 1. Explain the difference between primary and secondary infertility.
Infertility is defined as the inability to conceive after one year of regular, unprotected intercourse. Primary infertility refers to couples who have never conceived, while secondary infertility describes couples who have conceived at least once in the past but are now unable to conceive again. Think of it like this: primary infertility is like never starting a car, while secondary infertility is like a car that once ran but now won’t start. The underlying causes can be similar or quite different in both cases, necessitating a thorough evaluation.
Q 2. Describe the various diagnostic tests used in infertility evaluations.
Infertility evaluations involve a comprehensive approach for both partners. Tests for women often include:
- Ovulation testing: Tracking menstrual cycles, basal body temperature, and using ovulation predictor kits to confirm ovulation.
- Hysterosalpingography (HSG): An X-ray procedure to assess the fallopian tubes for blockages.
- Sonohysterography (SHG): A saline ultrasound to visualize the uterine cavity for abnormalities.
- Laparoscopy: A minimally invasive surgical procedure to directly visualize the pelvic organs.
- Hormone testing: Blood tests to measure levels of hormones such as FSH, LH, estradiol, and prolactin.
Tests for men typically involve:
- Semen analysis: Evaluating sperm count, motility, and morphology (shape).
- Hormone testing: Assessing levels of testosterone and other hormones.
- Genetic testing: In some cases, identifying potential genetic causes of infertility.
These tests help pinpoint the underlying cause of infertility, paving the way for appropriate treatment.
Q 3. What are the common causes of male infertility?
Male infertility stems from various factors affecting sperm production or function. Common causes include:
- Varicocele: Enlarged veins in the scrotum, impairing sperm production.
- Infections: Infections like mumps or sexually transmitted infections can damage the reproductive system.
- Hormonal imbalances: Low testosterone levels or other hormonal problems can affect sperm production.
- Genetic factors: Certain genetic conditions can lead to impaired sperm development or function.
- Obstructions: Blockages in the reproductive tract can prevent sperm from reaching the ejaculate.
- Lifestyle factors: Smoking, excessive alcohol consumption, and obesity can negatively impact sperm quality.
A detailed semen analysis is crucial for identifying the specific cause and guiding treatment strategies. For example, a low sperm count might indicate a need for hormone therapy, while an obstruction might require surgical intervention.
Q 4. What are the common causes of female infertility?
Female infertility is multifaceted and can originate from various sources. Common causes include:
- Ovulatory dysfunction: Irregular or absent ovulation due to hormonal imbalances or other conditions like PCOS (Polycystic Ovary Syndrome).
- Fallopian tube problems: Blockages or damage to the fallopian tubes, preventing egg and sperm from meeting.
- Uterine factors: Conditions like uterine fibroids or polyps that interfere with implantation.
- Endometriosis: The presence of uterine tissue outside the uterus, causing inflammation and pain.
- Cervical factors: Cervical mucus abnormalities that hinder sperm transport.
- Age: Diminished egg quality and quantity as women age.
Diagnosing the underlying cause requires a thorough evaluation, incorporating tests like ovulation tracking, HSG, and potentially laparoscopy, enabling tailored treatment approaches.
Q 5. Outline the steps involved in an IVF cycle.
In-vitro fertilization (IVF) is a complex procedure involving several steps. It begins with:
- Ovarian stimulation: Medications are used to stimulate the ovaries to produce multiple eggs.
- Egg retrieval: Eggs are retrieved from the ovaries using a needle guided by ultrasound.
- Sperm preparation: Sperm are collected and processed to select the healthiest ones.
- Fertilization: Eggs and sperm are combined in a laboratory dish to allow fertilization.
- Embryo culture: Fertilized eggs (embryos) are cultured in a laboratory for several days.
- Embryo transfer: One or more embryos are transferred to the uterus using a catheter.
- Pregnancy test: A pregnancy test is performed several weeks after the embryo transfer.
Each step is carefully monitored, and the process requires a dedicated team of medical professionals. The success rate of IVF varies depending on several factors, including the age of the woman and the underlying cause of infertility.
Q 6. Explain the process of intrauterine insemination (IUI).
Intrauterine insemination (IUI) is a less invasive fertility treatment than IVF. In IUI, processed sperm is directly placed into the uterus near the time of ovulation. This procedure bypasses the cervix, increasing the chances of sperm reaching the egg. IUI is often used for couples with mild male factor infertility or unexplained infertility where ovulation is confirmed. The process usually involves monitoring ovulation with ultrasound and blood tests, then scheduling the IUI procedure around the time of ovulation. The procedure itself is relatively quick and minimally invasive, typically causing minimal discomfort.
Q 7. Describe different types of assisted reproductive technologies (ART).
Assisted reproductive technologies (ART) encompass a range of procedures designed to help individuals or couples achieve pregnancy. Besides IVF and IUI, other ART options include:
- Gamete intrafallopian transfer (GIFT): Eggs and sperm are placed directly into the fallopian tubes.
- Zygote intrafallopian transfer (ZIFT): Fertilized eggs (zygotes) are placed into the fallopian tubes.
- Intracytoplasmic sperm injection (ICSI): A single sperm is directly injected into an egg to achieve fertilization.
- Preimplantation genetic testing (PGT): Genetic screening of embryos to identify chromosomal abnormalities before implantation.
The choice of ART depends on various factors, including the cause of infertility, the couple’s preferences, and the success rates of each procedure. A fertility specialist will guide couples towards the most appropriate option.
Q 8. What are the risks and benefits of IVF?
In-vitro fertilization (IVF) is a powerful assisted reproductive technology, but like any medical procedure, it carries both risks and benefits. The benefits are primarily the chance to conceive a child for couples struggling with infertility. This includes those with blocked fallopian tubes, endometriosis, unexplained infertility, male factor infertility, or those using donor eggs or sperm.
- Benefits: Increased chance of pregnancy for couples facing infertility, ability to use donor gametes, preimplantation genetic testing (PGT) options to screen embryos for genetic abnormalities.
However, IVF also involves several risks:
- Risks: Ovarian hyperstimulation syndrome (OHSS), which can cause severe abdominal pain and fluid buildup; multiple pregnancies, increasing risks for both mother and fetuses; ectopic pregnancy (pregnancy outside the uterus); miscarriage; risks associated with anesthesia and medication; emotional stress and financial burden.
The decision to pursue IVF is highly personal and should be made after careful consideration of the potential benefits and risks, alongside a thorough discussion with a fertility specialist.
Q 9. How do you counsel patients about the emotional challenges of infertility?
Counseling patients about the emotional challenges of infertility is a crucial part of my role. Infertility can be a deeply isolating and emotionally draining experience, often accompanied by feelings of grief, loss, anger, frustration, and depression. I approach these conversations with empathy and understanding, creating a safe space for open and honest communication.
My approach involves active listening, validating their feelings, and providing emotional support. I educate them about the various stages of the fertility journey and the potential emotional ups and downs they might experience. I encourage couples to communicate openly with each other and to seek support from family, friends, or support groups. I also discuss strategies for coping with stress, such as mindfulness, relaxation techniques, and seeking professional counseling when needed. Sometimes, simply acknowledging their pain and validating their experience can make a significant difference.
For example, I often share stories of other couples who’ve gone through similar experiences, highlighting their resilience and ultimately successful outcomes. This helps normalize their feelings and reduces feelings of isolation.
Q 10. Explain the role of genetic testing in fertility treatments.
Genetic testing plays an increasingly important role in fertility treatments. It helps identify genetic abnormalities that may affect embryo viability or increase the risk of certain conditions in the child. This is especially relevant for couples with a history of genetic disorders or recurrent miscarriages.
Preimplantation genetic testing (PGT) is a common type of genetic testing performed on embryos created through IVF. There are several types of PGT, including PGT-A (aneuploidy screening), PGT-M (monogenic disease testing), and PGT-SR (structural rearrangement testing). PGT-A screens for chromosomal abnormalities in embryos before implantation, increasing the chances of a successful pregnancy and reducing the risk of miscarriage. PGT-M tests for specific genetic disorders known to be present in the family, while PGT-SR screens for structural chromosomal abnormalities like translocations or inversions.
Carrier screening is another important genetic test performed on prospective parents before undergoing IVF. It identifies if parents carry recessive genes for certain genetic disorders. If both parents carry the same recessive gene, there’s a risk of passing the condition to their child. Genetic testing allows for informed decision-making and can significantly impact treatment plans.
Q 11. Discuss the ethical considerations surrounding fertility treatments.
Ethical considerations in fertility treatments are complex and multifaceted. Key ethical considerations include:
- Access to treatment: Ensuring equitable access to fertility treatments, regardless of socioeconomic status or other factors. The high cost of IVF can be a barrier for many couples.
- Multiple births: The ethical implications of multiple pregnancies resulting from IVF, given the increased risks to both mother and babies. Strategies to avoid multiple pregnancies, such as single embryo transfer (SET), are being emphasized.
- Embryo disposition: Decisions about what to do with unused embryos, including freezing, donation to research, or disposal. These are deeply personal decisions with significant ethical implications.
- Preimplantation genetic diagnosis (PGD): The ethical considerations surrounding PGD, particularly the potential for selective abortion based on genetic traits. There are ongoing debates about its appropriate application.
- Third-party reproduction: The ethical issues surrounding gamete donation and surrogacy, including the rights and responsibilities of all involved parties. Legal and ethical frameworks are continually evolving to address this.
Fertility specialists must navigate these ethical considerations with sensitivity, transparency, and respect for patient autonomy. Open communication with patients is essential to ensure that they are fully informed about the potential ethical implications of different treatment options.
Q 12. How do you manage patient expectations regarding success rates?
Managing patient expectations is critical in fertility treatment. It’s crucial to be upfront about the realities of success rates, which vary significantly depending on factors such as age, diagnosis, and the specific treatment employed. While I’m optimistic and supportive, I avoid giving false hope.
I explain success rates using clear, understandable language, avoiding technical jargon. For example, instead of saying “the live birth rate is 45%,” I might say, “For couples of your age and with your diagnosis, about 45 out of every 100 women undergoing this treatment will have a live birth. However, this is just a statistic; it doesn’t guarantee your outcome. Many factors play a role.” I emphasize the importance of managing expectations and focusing on the overall well-being of the couple.
I discuss alternative options if the first cycle of IVF is unsuccessful. This might involve modifying treatment, exploring other treatments, or considering lifestyle changes. Open and honest communication helps build trust and prepares couples for any eventualities.
Q 13. Describe your experience with ovulation induction.
Ovulation induction is a common fertility treatment used to stimulate the ovaries to produce multiple eggs. This is particularly helpful for women who don’t ovulate regularly or have infrequent ovulation. My experience involves using a variety of medications, such as clomiphene citrate or letrozole, to stimulate ovulation. The choice of medication depends on factors such as the patient’s age, medical history, and overall health. Close monitoring is vital to ensure the ovaries respond appropriately and to avoid the risks of OHSS.
The process typically involves regular monitoring of follicular growth using ultrasound and blood tests to measure hormone levels. Once the follicles reach the appropriate size, I would prescribe a trigger shot (usually hCG) to induce final maturation and ovulation. Timing of intercourse or intrauterine insemination (IUI) is critical for optimal fertilization. Throughout the process, I provide clear explanations and address any concerns patients may have.
For example, I might explain the potential side effects of medications like bloating, mood swings, and hot flashes, and provide strategies for managing them. Regular communication and monitoring allow for individualized treatment plans and the best chances of success.
Q 14. How do you approach cases of unexplained infertility?
Unexplained infertility presents a unique challenge as it lacks a clear identifiable cause. My approach to these cases is comprehensive and involves a thorough investigation to rule out any underlying, subtle issues. This includes a detailed evaluation of both partners, including hormone testing, semen analysis, and imaging studies such as hysterosalpingography (HSG) to assess the fallopian tubes. I also assess lifestyle factors like stress levels, weight, and diet as these can indirectly affect fertility.
Once all readily identifiable causes are excluded, we often begin with simpler treatments like ovulation induction or IUI. If these are unsuccessful, IVF might be considered as a next step. It’s important to remember that even in unexplained infertility, the chance of conceiving is still present, and treatments can still be successful. Regular monitoring and patient support are essential in guiding the couple through the process. Sometimes a wait-and-see approach is recommended, allowing time for the couple to manage stress, make lifestyle adjustments, and address other potentially underlying factors. This holistic approach helps address not just the medical aspects but also the psychological impacts of this challenging diagnosis.
Q 15. What is your experience with gamete intrafallopian transfer (GIFT)?
Gamete Intrafallopian Transfer (GIFT) is a fertility treatment where the egg and sperm are placed directly into the fallopian tube. This allows fertilization to occur naturally within the body, mimicking the natural conception process. My experience with GIFT involves a thorough patient evaluation to assess fallopian tube patency and ovarian reserve. This includes ultrasound scans, hormone level testing, and a detailed discussion of the risks and benefits. The procedure itself is performed laparoscopically under general anesthesia. Post-procedure, patients receive close monitoring, including pregnancy tests and follow-up appointments to assess the success of the procedure. I’ve found that meticulous attention to detail during egg retrieval and placement significantly impacts success rates. For example, one patient with unexplained infertility achieved a successful pregnancy following a single GIFT cycle after years of unsuccessful attempts with other methods.
GIFT is a less commonly used procedure now compared to IVF due to the advancements in IVF techniques and higher success rates reported with IVF. However, for selected patients who meet specific criteria, such as those with patent fallopian tubes and a desire for a more natural approach, GIFT can be a viable option.
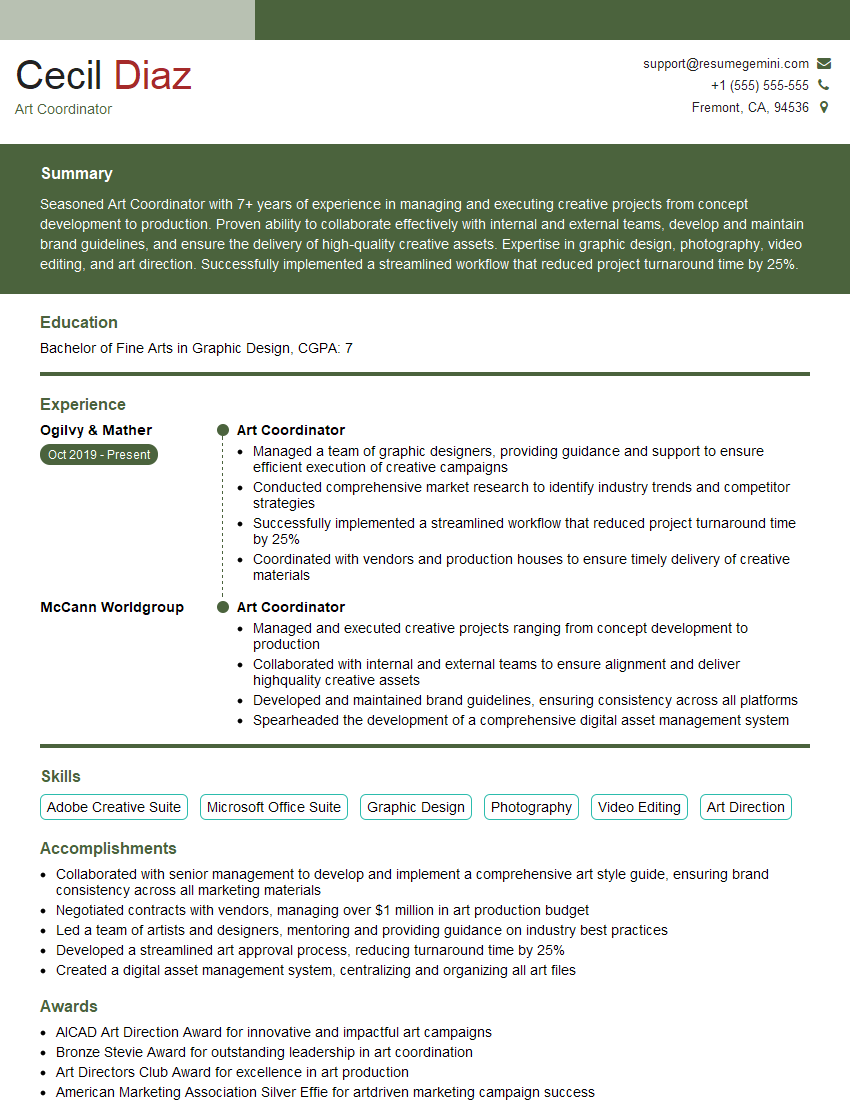
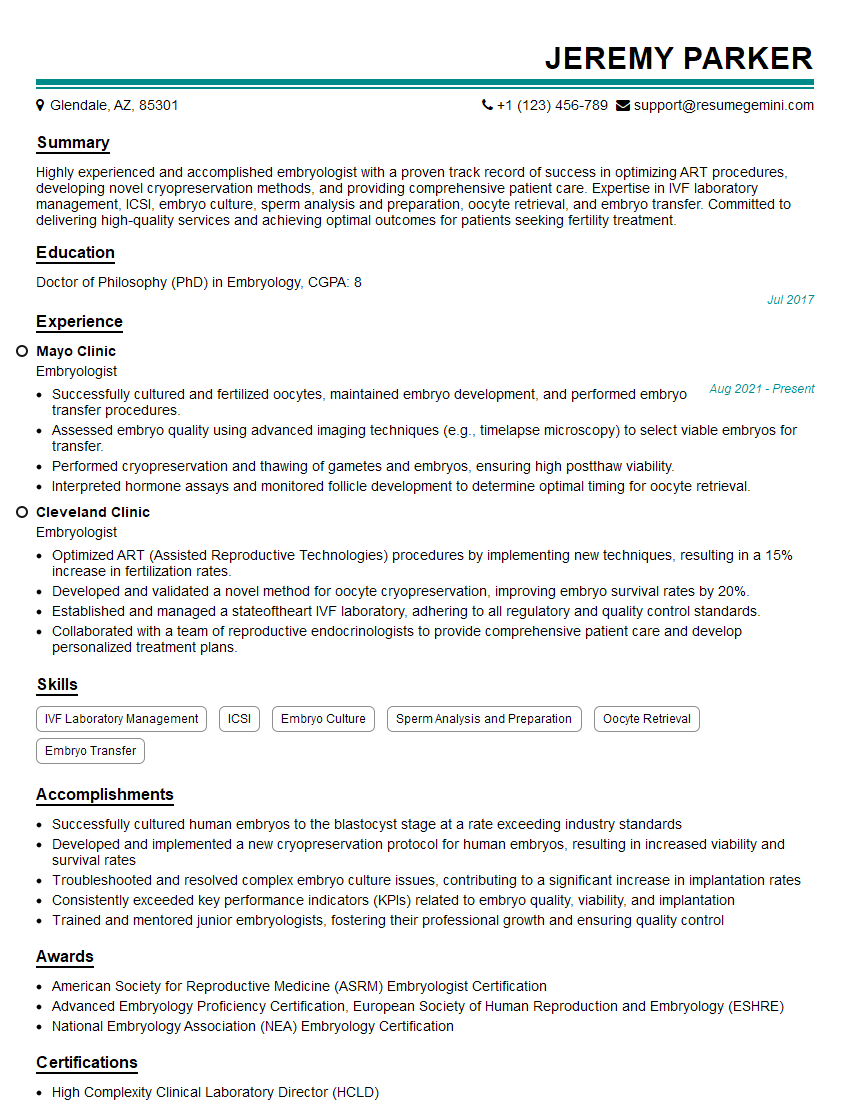
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with zygote intrafallopian transfer (ZIFT)?
Zygote Intrafallopian Transfer (ZIFT) is another assisted reproductive technology (ART) where fertilization occurs in the laboratory, similar to IVF. However, instead of transferring the embryos directly into the uterus, the resulting zygote (fertilized egg) is transferred into the fallopian tube. My experience with ZIFT has shown that it’s a valuable technique for patients who have issues with fertilization, but whose fallopian tubes are healthy and functioning. The procedure involves ovarian stimulation, egg retrieval, in-vitro fertilization (IVF), and then laparoscopic transfer of the zygote into the fallopian tube. Post-procedure care is similar to GIFT, involving close monitoring and follow-up. I’ve had success with ZIFT in cases where IVF alone has failed due to issues with early embryo development.
Like GIFT, ZIFT is less frequently performed compared to embryo transfer directly into the uterus, but it offers a valuable option for specific patient populations, providing a bridge between IVF and natural conception.
Q 17. How do you manage complications associated with fertility treatments?
Managing complications associated with fertility treatments requires a multifaceted approach. Potential complications can range from ovarian hyperstimulation syndrome (OHSS) following ovarian stimulation, to infections related to procedures, and psychological distress. My strategy focuses on prevention, early detection, and prompt intervention.
- Ovarian Hyperstimulation Syndrome (OHSS): Careful monitoring of ovarian response during stimulation cycles is key, potentially modifying the medication protocol to avoid excessive stimulation. Severe cases require hospitalization and supportive care.
- Infections: Strict adherence to sterile techniques during procedures is paramount. Prompt treatment with antibiotics is initiated if infection is suspected.
- Psychological Distress: Fertility treatment can be emotionally challenging. Providing psychological support through counseling and emotional support groups is crucial. I encourage open communication and work closely with patients to address their anxieties.
A collaborative approach with other specialists, such as anesthesiologists and reproductive endocrinologists is essential in managing complex complications.
Q 18. Describe your experience with preimplantation genetic testing (PGT).
Preimplantation Genetic Testing (PGT) is a valuable tool used to screen embryos for genetic abnormalities before implantation. My experience involves offering various types of PGT, including PGT-A (aneuploidy testing), PGT-M (monogenic disease testing), and PGT-SR (structural rearrangement testing). PGT significantly improves the chances of a successful pregnancy and reduces the risk of miscarriage and birth defects. The process involves performing IVF, followed by a biopsy of the embryo at the blastocyst stage. Genetic analysis is then conducted on the biopsied cells. Only genetically healthy embryos are then selected for transfer.
For example, I recently assisted a couple with a family history of cystic fibrosis. Through PGT-M, we successfully screened their embryos and transferred a healthy embryo resulting in a healthy pregnancy and the birth of a baby free from the disease. Ethical considerations are paramount, ensuring informed consent is obtained and addressing patient anxieties related to genetic testing.
Q 19. How do you address patient concerns about multiple pregnancies?
Multiple pregnancies carry significant risks, including premature birth, low birth weight, and potential complications for both the mother and babies. Addressing patient concerns begins with a frank discussion of the risks associated with multiple gestation. Options for reducing the risk, such as selective reduction (reducing the number of embryos) are carefully explained. It’s important to underscore that the decision regarding the number of embryos to transfer rests with the patient, based on their understanding of the risks and benefits. I always encourage patients to carefully weigh the risks and make informed choices. I often use visual aids like charts and diagrams to help patients understand the statistics and probabilities of multiple pregnancies. Building trust and ensuring the patient feels heard and supported is crucial throughout this process.
Q 20. Explain your approach to managing patients with endometriosis.
Endometriosis, characterized by the growth of endometrial-like tissue outside the uterus, can significantly impact fertility. My management approach is individualized based on the patient’s symptoms, stage of endometriosis, and desire for pregnancy. Options include medical management with hormonal therapies (like GnRH agonists or antagonists) to suppress endometriosis growth, and surgical management to remove endometrial implants and improve pelvic anatomy.
In some cases, a combination of medical and surgical therapies is necessary. For patients attempting pregnancy, timing treatments to coincide with optimal fertility windows is critical. Assisted reproductive technologies (ART), such as IVF, may be recommended depending on the severity of endometriosis and the patient’s response to other treatments. Regular follow-up assessments and monitoring are crucial for long-term management and monitoring of fertility outcomes.
Q 21. Describe your experience with polycystic ovary syndrome (PCOS) management in relation to fertility.
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting ovulation and fertility. My experience with PCOS management emphasizes a multi-pronged approach. First, lifestyle modifications, including weight management (if needed), regular exercise, and dietary changes, are prioritized. These lifestyle changes can significantly improve ovulation and increase chances of conception. Second, medication may be prescribed to induce ovulation, such as clomiphene citrate or letrozole. Third, assisted reproductive technologies (ART), like IVF, may be considered if lifestyle changes and medication are unsuccessful.
Regular monitoring of hormone levels, menstrual cycles, and ultrasound scans is essential to track progress and adjust treatment as needed. I emphasize the importance of patient education and empower patients to actively participate in their treatment plan. Understanding the impact of PCOS on their overall health and fertility is crucial for successful management and improved outcomes.
Q 22. How do you counsel patients about the risks of ovarian hyperstimulation syndrome (OHSS)?
Ovarian Hyperstimulation Syndrome (OHSS) is a serious complication that can occur after fertility treatments involving hormone injections, most commonly in-vitro fertilization (IVF). It happens when the ovaries become significantly enlarged and produce excessive fluid. Counseling patients about OHSS involves a multi-step process focused on informed consent and risk mitigation.
- Risk Factor Assessment: I begin by assessing the patient’s individual risk factors, such as age, body mass index (BMI), previous history of OHSS, and type of fertility medication being used. Higher risk patients receive more detailed counseling.
- Symptom Explanation: I explain the potential symptoms of OHSS, ranging from mild discomfort like bloating and abdominal pain to severe complications requiring hospitalization, such as shortness of breath, severe abdominal distension, and blood clots. I use clear, non-medical jargon to ensure understanding.
- Prevention Strategies: We discuss preventative measures, including meticulous monitoring of ovarian response through regular ultrasound scans and blood tests to adjust medication dosages as needed. This allows us to minimize overstimulation.
- Management Plan: A clear management plan is crucial. Patients are taught how to recognize warning signs and immediately contact the clinic if they experience any concerning symptoms. They are also given instructions on fluid intake and rest to support their recovery.
- Emotional Support: Acknowledging the anxiety associated with OHSS is vital. I provide emotional support and answer questions openly and honestly, ensuring the patient feels empowered to make informed decisions.
For example, I might explain the risk of OHSS in a way like this: ‘Imagine your ovaries as balloons. The medication helps them grow, but sometimes they grow too much and that can cause problems. We use careful monitoring to prevent this from happening.’ This analogy helps patients understand the concept without being overwhelmed by medical jargon.
Q 23. What is your experience with sperm donation and egg donation?
I have extensive experience with both sperm and egg donation, encompassing all aspects from initial patient consultations to post-donation counseling and support. In sperm donation cases, I focus on donor screening to ensure eligibility, including genetic testing and thorough medical history review to minimize the risk of passing on genetic diseases. Strict adherence to regulatory guidelines is paramount.
With egg donation, the process is considerably more involved. I counsel prospective recipients on the implications of using donated eggs, the success rates, and ethical considerations. I also work closely with egg donors, ensuring they understand the commitment involved, including physical and emotional aspects, while respecting their autonomy and reproductive rights. This includes extensive counseling and support throughout the donation process.
One particularly memorable case involved a couple who, after years of unsuccessful attempts, chose egg donation. We worked together to navigate the selection process, providing detailed information about donor profiles and guiding them through the emotional journey. Their success, resulting in a healthy baby, remains a highlight of my career. This underscores the profound impact that these services have on individuals and families.
Q 24. How do you stay current with advancements in fertility treatments?
Staying current in fertility treatments requires a multi-faceted approach.
- Professional Organizations: Active membership in organizations like the American Society for Reproductive Medicine (ASRM) provides access to the latest research, guidelines, and continuing medical education (CME) opportunities. I regularly attend conferences and workshops to expand my knowledge base.
- Peer-Reviewed Journals: I closely follow reputable peer-reviewed journals such as Human Reproduction and Fertility and Sterility, critically evaluating new studies and advancements.
- Online Resources and Databases: Databases like PubMed provide access to a vast collection of research papers, keeping me updated on the latest clinical trials and technological advancements.
- Collaboration with Colleagues: Regular discussions and collaboration with colleagues from different specialties, including endocrinologists, geneticists, and embryologists, broaden my perspectives and facilitate knowledge sharing.
For instance, recent advancements in preimplantation genetic testing (PGT) have significantly improved the chances of avoiding genetic disorders in embryos. Staying abreast of these developments allows me to offer patients the most advanced and appropriate treatments.
Q 25. Describe your experience working in a multidisciplinary team.
My experience working in a multidisciplinary team has been invaluable. In fertility treatment, a successful outcome often depends on the coordinated efforts of various specialists.
- Effective Communication: Clear and concise communication is key. I regularly participate in team meetings, sharing patient information and collaborating on treatment plans with embryologists, reproductive endocrinologists, nurses, and genetic counselors. We use established communication protocols to avoid misunderstandings and ensure patient safety.
- Shared Decision-Making: Multidisciplinary teams encourage shared decision-making, ensuring that the best possible treatment strategy is selected based on collective expertise. This collaborative approach fosters a more holistic and personalized approach to patient care.
- Enhanced Patient Outcomes: The combined expertise and coordinated efforts of a multidisciplinary team significantly contribute to improved patient outcomes and satisfaction. The interdisciplinary approach reduces errors and enhances the overall efficiency of the process.
For example, in a case involving a patient with recurrent implantation failure, our team, including a geneticist and an embryologist, collaborated extensively to investigate potential underlying genetic factors and optimize the embryo transfer procedure, ultimately resulting in a successful pregnancy.
Q 26. How do you handle difficult conversations with patients?
Difficult conversations with patients are an inevitable part of this profession. My approach centers on empathy, active listening, and clear communication.
- Empathetic Approach: I start by acknowledging the patient’s emotions and validating their feelings. Creating a safe and supportive environment is crucial, allowing patients to express their concerns and anxieties freely.
- Active Listening: I actively listen to the patient’s concerns, asking clarifying questions to ensure I understand their perspective fully. I avoid interrupting and show genuine interest in their situation.
- Clear and Honest Communication: I deliver information honestly and clearly, using plain language to avoid medical jargon. I tailor my communication style to the individual patient’s needs and emotional state.
- Providing Options and Support: When delivering difficult news, I strive to present options and explore alternative solutions collaboratively. I also ensure access to appropriate support services, such as counseling or support groups.
For instance, when delivering the news of a failed IVF cycle, I would begin by saying something like, ‘I understand this is disappointing news, and I’m truly sorry. Let’s discuss what we learned from this cycle and explore the different options we can consider moving forward.’ This demonstrates empathy and initiates an open conversation.
Q 27. How do you maintain patient confidentiality?
Maintaining patient confidentiality is paramount. I adhere strictly to HIPAA regulations and all relevant privacy laws.
- HIPAA Compliance: All patient information is handled with the utmost care, strictly adhering to HIPAA guidelines regarding protected health information (PHI). Access to patient records is limited to authorized personnel only.
- Secure Data Management: Electronic medical records are stored securely using encrypted systems, protecting sensitive patient data from unauthorized access.
- Confidential Communication: All communication, whether written or verbal, is conducted in a confidential manner. Patient discussions are held in private spaces, ensuring patient privacy.
- Informed Consent: I always obtain informed consent from patients before sharing their information with other healthcare providers or researchers.
Any breaches of confidentiality are dealt with immediately and reported following established protocols. My commitment to patient privacy is unwavering and forms the cornerstone of my professional practice.
Q 28. What are your salary expectations?
My salary expectations are commensurate with my experience, qualifications, and the market rate for fertility specialists with my level of expertise in a similar setting. I am open to discussing a competitive compensation package that reflects my contributions to the organization and my commitment to providing high-quality patient care.
Key Topics to Learn for Fertility Recommendations Interview
- Reproductive Physiology: Understanding the menstrual cycle, ovulation, fertilization, and implantation. This includes knowledge of hormonal influences and potential disruptions.
- Infertility Diagnosis and Treatment Options: Familiarize yourself with common diagnostic tests (e.g., semen analysis, hormone testing, hysterosalpingography) and various treatment approaches (e.g., ovulation induction, intrauterine insemination, in-vitro fertilization).
- Patient Counseling and Communication: Mastering the art of explaining complex medical information to patients in a clear and empathetic manner. Practice active listening and addressing patient concerns effectively.
- Ethical Considerations in Fertility Treatments: Understand the ethical dilemmas surrounding assisted reproductive technologies (ART), including issues of consent, embryo selection, and genetic testing.
- Data Analysis and Interpretation: Develop skills in analyzing patient data to identify trends, make informed recommendations, and track treatment outcomes. This might involve working with fertility charts or electronic medical records.
- Legal and Regulatory Frameworks: Be aware of relevant laws and regulations pertaining to fertility treatments and patient privacy.
- Risk Assessment and Management: Understand potential risks associated with fertility treatments and develop strategies for mitigating those risks.
- Evidence-Based Practice: Know how to critically evaluate scientific literature and apply evidence-based guidelines to clinical decision-making.
Next Steps
Mastering Fertility Recommendations is crucial for career advancement in the reproductive health field, opening doors to exciting opportunities and higher earning potential. A strong resume is your first impression – make it count! An ATS-friendly resume is essential for getting your application noticed by recruiters and hiring managers. ResumeGemini is a trusted resource to help you build a professional and effective resume that showcases your skills and experience in the best light. Examples of resumes tailored to Fertility Recommendations are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good