Preparation is the key to success in any interview. In this post, we’ll explore crucial First Aid and Emergency Response Training interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in First Aid and Emergency Response Training Interview
Q 1. Describe the steps involved in performing CPR on an adult.
Performing CPR (Cardiopulmonary Resuscitation) on an adult is a life-saving technique used when someone is unresponsive and not breathing normally. It involves chest compressions and rescue breaths to circulate blood and oxygen. Remember to always call emergency services first (or have someone else do it) before starting CPR.
- Check for Responsiveness: Gently shake the person and shout, “Are you okay?”
- Call for Help: Immediately call emergency medical services (EMS) or have someone else do so.
- Check for Breathing: Look, listen, and feel for normal breathing for no more than 10 seconds.
- Start Chest Compressions: Position yourself over the person’s chest, placing the heel of one hand on the center of their chest (between the nipples). Place your other hand on top, interlacing your fingers. Keep your arms straight and push hard and fast, at a rate of 100-120 compressions per minute, compressing the chest about 2 inches deep.
- Give Rescue Breaths: After 30 compressions, give two rescue breaths. Pinch the person’s nose closed, seal your mouth over theirs, and give two slow breaths, each lasting about one second, making the chest rise.
- Continue CPR: Repeat the cycle of 30 compressions and two breaths until EMS arrives or the person shows signs of life (breathing normally, moving).
Example: Imagine you find a colleague collapsed at work. You check for responsiveness, call 911, check breathing, and then begin CPR, following the 30:2 compression-to-breath ratio. You continue until paramedics take over.
Q 2. Explain the difference between stable and unstable side recovery positions.
Both the stable and unstable side recovery positions are used to help an unconscious, breathing person maintain an open airway and prevent choking on vomit or other secretions. The key difference lies in the patient’s stability and potential for spinal injury.
- Stable Side Recovery Position: Used when there’s no suspected spinal injury. The person is carefully rolled onto their side, allowing fluids to drain from the mouth. One arm is placed above the head, the other across the chest, and the top knee is bent to stabilize the position.
- Unstable Side Recovery Position (also known as the log roll): Used when a spinal injury is suspected. This involves carefully rolling the person as a single unit, supported by several people to maintain spinal alignment throughout the process. A rigid collar might be applied before rolling, if available. The goal is to prevent further injury to the spine.
Example: An elderly person faints and is breathing. You can use the stable side recovery position. However, if someone is involved in a car accident and has a possible spinal injury, the unstable recovery position or log roll is necessary to minimize the risk of further harm.
Q 3. How do you assess a patient’s airway, breathing, and circulation (ABCs)?
Assessing a patient’s ABCs (Airway, Breathing, Circulation) is the first step in any emergency situation. It helps you quickly determine the severity of the situation and prioritize treatment.
- Airway: Check if the airway is open and clear. Look for any obstructions (vomit, blood, foreign objects). Open the airway if needed using the head-tilt-chin-lift maneuver (unless a spinal injury is suspected, in which case use the jaw-thrust maneuver).
- Breathing: Look for chest rise and fall, listen for breath sounds, and feel for breath on your cheek near their mouth and nose. Assess the rate, depth, and quality of breathing.
- Circulation: Check for a pulse (carotid pulse is usually checked in an emergency). Check skin color (pale, cyanotic, or flushed) and capillary refill time (press on a fingernail to see how quickly color returns).
Example: Imagine a person is involved in a car accident. You would check for any airway obstructions, assess their breathing by looking for chest rise and fall and listening for breath sounds, and feel for a carotid pulse to evaluate circulation. This quick assessment guides further treatment.
Q 4. What are the signs and symptoms of a stroke?
Stroke, also called a cerebrovascular accident (CVA), occurs when blood supply to the brain is interrupted. Recognizing the signs and symptoms is crucial for timely intervention, as prompt treatment can significantly improve outcomes.
Use the FAST acronym to remember the key signs:
- Face: Ask the person to smile. Does one side of the face droop?
- Arms: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- Time: If you observe any of these signs, call emergency services immediately. Time is critical.
Other symptoms can include sudden numbness or weakness (especially on one side of the body), confusion, trouble seeing, dizziness, severe headache with no known cause.
Example: If someone suddenly has trouble speaking, their face droops on one side, or they experience sudden weakness in one arm, suspect a stroke and call emergency services immediately. Every minute counts.
Q 5. How would you treat a severe bleeding wound?
Treating severe bleeding requires immediate action to control the blood loss. Direct pressure is the primary method.
- Direct Pressure: Apply firm, direct pressure to the wound using a clean cloth. Do not remove the cloth even if it becomes soaked with blood; add more cloths on top. Elevate the injured limb above the heart, if possible, to slow the bleeding.
- Tourniquet (as a last resort): If direct pressure fails to control the bleeding and the injury is life-threatening, a tourniquet may be necessary. Apply it only as a last resort and follow the instructions carefully. Note the time of application, as this is crucial information for medical professionals.
- Call Emergency Services: Always call emergency medical services to get the injured person to a hospital for definitive care.
Example: Imagine a person severely cuts their leg with a chainsaw. You would immediately apply direct pressure to the wound, elevate the leg, and continue applying pressure until paramedics arrive. If the bleeding doesn’t stop despite direct pressure, a tourniquet might become necessary (if trained in its use), but only as a last resort.
Q 6. Describe the procedure for using an AED (Automated External Defibrillator).
An AED (Automated External Defibrillator) is a portable device used to deliver an electric shock to the heart to restore a normal heartbeat in cases of sudden cardiac arrest.
- Turn on the AED: Follow the voice prompts provided by the device.
- Attach the Pads: Expose the patient’s chest and attach the AED pads to the bare skin as indicated by the device. One pad is typically placed on the right upper chest, and the other on the lower left side of the chest.
- Analyze the Heart Rhythm: The AED will analyze the heart rhythm and indicate whether a shock is advised.
- Deliver Shock (if advised): If the AED instructs you to deliver a shock, ensure that no one is touching the patient. Push the shock button when prompted by the device.
- Resume CPR: Immediately begin CPR (chest compressions and rescue breaths) after the shock is delivered, following the usual 30:2 compression-to-breath ratio, continuing until EMS arrives or the person shows signs of life.
Example: Someone collapses suddenly and is unresponsive and not breathing. You turn on the AED, attach the pads, allow the device to analyze the rhythm, deliver a shock if advised, and immediately resume CPR until paramedics arrive.
Important Note: Always ensure the patient is on a dry surface to prevent interference with the device and follow manufacturer instructions carefully. Proper training is essential before using an AED.
Q 7. How do you manage a suspected spinal injury?
Suspected spinal injuries require careful management to prevent further damage to the spinal cord. The primary goal is to stabilize the spine and minimize movement.
- Call Emergency Services: Immediately call emergency services.
- Minimize Movement: Do not move the person unless absolutely necessary to prevent further spinal cord damage.
- Manual Stabilization: If you must move the person, use proper techniques like the log roll (with assistance if needed), maintaining spinal alignment at all times.
- Neck and Spinal Immobilization (if trained and available): Apply a cervical collar and a spinal board to help stabilize the spine. This should be done by trained personnel.
- Monitor Breathing and Circulation: Continuously monitor the person’s breathing and circulation while awaiting medical assistance.
Example: You witness a person fall from a height. Because of the mechanism of injury, you suspect a spinal injury. You immediately call emergency services, avoid moving the person unnecessarily, and wait for trained professionals to arrive and immobilize the spine before carefully moving them.
Important Note: Spinal immobilization should be performed by trained personnel. Improper immobilization can potentially worsen the injury.
Q 8. What are the different types of burns and how are they treated?
Burns are classified into three degrees based on the depth of tissue damage: first-degree (superficial), second-degree (partial-thickness), and third-degree (full-thickness). First-degree burns affect only the outer layer of skin, causing redness and mild pain. Second-degree burns involve the deeper skin layers, resulting in blisters, significant pain, and swelling. Third-degree burns destroy all layers of the skin, appearing white, charred, or leathery, often with minimal pain due to nerve damage.
Treatment focuses on cooling the burn, preventing infection, and relieving pain. For first-degree burns, cool running water for 10-20 minutes is usually sufficient. For second-degree burns, after cooling, cover the burn loosely with a clean, sterile dressing to protect it. Third-degree burns require immediate medical attention; do not attempt to remove clothing stuck to the burn. Always monitor for signs of infection like increased pain, swelling, pus, or red streaks. Remember, the size and location of a burn also impacts severity, and larger burns or those on the face, hands, feet, or joints need urgent medical help.
Q 9. Explain the proper way to splint a fractured limb.
Splinting a fractured limb aims to immobilize the injury, preventing further damage and reducing pain. Before splinting, assess the injury, checking for circulation (feeling, warmth, and color distal to the fracture) and controlling any bleeding. Gentle handling is crucial. The splint should immobilize the joint above and below the fracture.
Steps:
- Padding: Place soft padding (e.g., cloth, rolled-up towels) around the injured area to prevent pressure sores.
- Splint Application: Use a rigid material (e.g., a board, folded cardboard) to support the limb. Secure the splint using bandages or other available materials, ensuring it is snug but not too tight, to avoid compromising circulation.
- Immobilization: The splint should extend beyond the joints above and below the fracture to prevent movement.
- Check Circulation: After splinting, recheck the circulation (feeling, warmth, color) in the affected limb. If there are any signs of compromised circulation, readjust the splint or remove it carefully and seek immediate medical attention.
Remember, this is temporary stabilization; professional medical care is essential for proper diagnosis and treatment of fractures.
Q 10. How do you handle a choking victim who is conscious and unconscious?
Conscious Choking Victim: Encourage the victim to cough forcefully to try to dislodge the obstruction. If ineffective, perform abdominal thrusts (Heimlich maneuver). Stand behind the victim, wrap your arms around their waist, make a fist and place it just above their navel, grasp your fist with your other hand, and give quick, upward thrusts into their abdomen. Repeat until the obstruction is cleared or the victim loses consciousness.
Unconscious Choking Victim: Carefully lower the victim to the ground. Begin CPR immediately, starting with chest compressions. Look inside the mouth; if you see the obstruction, attempt to remove it with your finger sweep. Continue CPR until medical help arrives or the obstruction is cleared. It is critical to identify the level of responsiveness (Conscious or Unconscious) accurately and tailor your response accordingly.
Q 11. What are the signs and symptoms of anaphylaxis?
Anaphylaxis is a severe, life-threatening allergic reaction. Signs and symptoms can vary but often include:
- Difficulty breathing or wheezing
- Swelling of the tongue, lips, or face
- Hives or rash
- Dizziness or lightheadedness
- Rapid pulse
- Nausea or vomiting
- Loss of consciousness
Anaphylaxis progresses rapidly, so immediate medical attention is crucial. The signs can manifest in a combination or individually. It is important to note the speed of onset and severity of symptoms as this dictates the urgency of treatment and the need for epinephrine.
Q 12. Describe the treatment for someone experiencing an asthma attack.
Asthma attacks involve a narrowing of the airways in the lungs, making it difficult to breathe. Treatment typically involves helping the person use their prescribed inhaler (usually a bronchodilator, like albuterol). Encourage them to sit upright, support their breathing and ensure they are comfortable. If they have a spacer, encourage its use. If their inhaler isn’t helping or the person appears to be worsening rapidly, seek immediate medical attention. Monitor breathing rate, oxygen saturation if possible, and level of consciousness. Knowing the patient’s medical history and preferred method of medication administration is vital. Stay calm and reassure the patient, managing their anxiety can assist with reducing the severity of the attack.
Q 13. What are the steps involved in treating a diabetic emergency?
Diabetic emergencies can result from either high blood sugar (hyperglycemia) or low blood sugar (hypoglycemia). Hypoglycemia is more common and often presents with symptoms like confusion, shakiness, sweating, and rapid heartbeat. Hyperglycemia can present with increased thirst, frequent urination, and blurred vision.
Treatment: For hypoglycemia, if the person is conscious and able to swallow, give them a fast-acting carbohydrate like sugar, juice, or glucose tablets. For hyperglycemia, the person needs medical attention; do not attempt to treat this at home. In both cases, monitor the person’s condition carefully and seek medical assistance if symptoms don’t improve or worsen. Knowing whether the individual has Type 1 or Type 2 diabetes and the potential for other complications influences the approach to managing their emergency.
Q 14. How do you manage a seizure?
Seizures involve abnormal electrical activity in the brain, causing temporary disruptions in brain function. Management focuses on protecting the person from injury and ensuring their safety.
- Protect from Injury: Move any nearby objects that could cause harm. Turn the person gently onto their side to help them breathe easily and prevent choking. Do not restrain them or attempt to put anything in their mouth.
- Monitor Time and Symptoms: Note the duration of the seizure and observe any symptoms such as stiffening, jerking, loss of consciousness, or changes in breathing.
- Post-Seizure Care: Once the seizure has stopped, turn the person onto their side and monitor their breathing and level of consciousness. They may be confused or disoriented. Call for medical help if this is their first seizure, or if the seizure is prolonged or severe.
It is important to avoid panicking and provide a calm and reassuring environment. Knowing the individual’s medical history, such as a history of epilepsy and medication, helps in managing the situation effectively.
Q 15. Explain the importance of scene safety in an emergency.
Scene safety is paramount in any emergency response. Before even approaching a victim, ensuring your own safety and the safety of others is crucial. This prevents further injuries or even fatalities. It involves assessing the immediate environment for hazards like traffic, downed power lines, unstable structures, or aggressive individuals.
- Hazard Identification: Actively scan the scene for potential dangers. For instance, if responding to a car accident, check for leaking fluids, broken glass, and oncoming traffic before approaching.
- Personal Protective Equipment (PPE): Using appropriate PPE, such as gloves, eye protection, and a mask, protects against exposure to bodily fluids or hazardous materials. This is especially critical in situations involving blood or other potentially infectious substances.
- Securing the Area: If possible and safe to do so, try to secure the area to prevent further injuries. This might involve directing traffic or asking bystanders to move back from the immediate vicinity.
- Calling for Backup: Don’t hesitate to call for backup if the situation is beyond your capabilities or if the scene is too unsafe to manage alone. The safety of responders is never compromised.
Example: Imagine responding to a house fire. Before entering, I’d assess for structural instability, potential explosions, and smoke inhalation risks. I would wait for firefighters to secure the scene before approaching the victims.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your approach to communicating with patients and bystanders?
Effective communication is vital during emergencies. My approach involves clear, concise, and empathetic communication with both patients and bystanders. With patients, I prioritize calm reassurance, explaining my actions clearly and obtaining their consent where appropriate. Bystanders often need direction and reassurance as well. Maintaining a calm demeanor and using simple language helps reduce panic and facilitates a smoother response.
- Active Listening: I carefully listen to the patient and bystanders to understand their concerns and obtain vital information. This includes asking open-ended questions rather than leading questions.
- Clear Instructions: I give concise, simple instructions, avoiding medical jargon. For instance, instead of saying ‘I need you to maintain a supine position,’ I’d say ‘Please lie flat on your back.’
- Empathy and Reassurance: I acknowledge their fear and distress, offering comfort and reassurance as much as possible.
- Managing Bystanders: I delegate tasks appropriately to bystanders, keeping them informed about the progress and ensuring their safety.
Example: While assisting a patient with a suspected broken leg, I would calmly introduce myself, explain what I’m doing, and reassure them that help is on the way. I’d also direct bystanders to call emergency services or retrieve a blanket.
Q 17. Describe your experience with documenting emergency responses.
Accurate documentation is crucial for legal and medical reasons. My experience involves detailed recording of the incident, including time, location, nature of the injury, actions taken, and patient responses. This is essential for continuity of care, as well as potential legal protection.
- Objective Observations: I focus on objective observations, avoiding subjective interpretations. For example, instead of writing ‘The patient was in severe pain,’ I’d write ‘The patient exhibited signs of acute pain, including moaning and guarding the injured area.’
- Chronological Order: I maintain a chronological record of events, noting the time each action was taken. This enhances the clarity and accuracy of the report.
- Patient Information: I gather and record pertinent patient information where possible, including name, age, medical history (if available), and allergies.
- Treatment Administered: I document all treatments given, including dosages and times.
- Incident Report Forms: I’m proficient in using standard incident report forms, ensuring all relevant fields are completed accurately and completely.
Example: After responding to a bicycle accident, I would meticulously document the time of the call, location, the patient’s injuries (abrasions, lacerations, etc.), my assessment findings, the treatment I administered (e.g., cleaning and bandaging wounds), and the patient’s response to treatment. This detailed record would be vital in ensuring continuity of care at the hospital.
Q 18. How do you handle stress and trauma in emergency situations?
Emergency situations can be intensely stressful and traumatic. My approach involves employing several coping mechanisms to manage stress and trauma both during and after an incident.
- Self-Care: Prioritizing sleep, healthy eating, and regular exercise helps build resilience against stress. I also take time to debrief with colleagues after particularly challenging incidents.
- Mindfulness and Breathing Techniques: Deep, controlled breathing exercises help regulate my physiological response to stress and promote calmness.
- Teamwork and Support: Working as part of a team provides emotional support and allows for sharing responsibilities.
- Debriefing and Support Services: Participating in critical incident stress debriefings (CISDs) helps process emotions and trauma after particularly difficult events. I’m aware of the availability of support services for mental health and utilize them as needed.
Example: After a particularly gruesome accident, I’d take time to sit quietly and practice deep breathing before debriefing with my colleagues. Accessing a support group if needed is a crucial part of maintaining well-being in this high-stress profession.
Q 19. Explain your understanding of Good Samaritan Laws.
Good Samaritan Laws are designed to protect individuals who provide emergency medical assistance to others in good faith without expecting compensation. They offer legal protection from liability for negligence, provided that the assistance is rendered reasonably and without gross negligence or recklessness. However, these laws vary by jurisdiction, and it’s crucial to understand the specific regulations of your location.
- Duty to Act: Good Samaritan laws typically do not impose a legal duty to act; you are not obligated to provide assistance. However, if you choose to help, the law offers protection.
- Standard of Care: The protection afforded under these laws usually applies only to actions taken within the scope of the individual’s training and knowledge. Providing assistance that is beyond one’s capabilities can void the protection.
- Gross Negligence: Acts of gross negligence or recklessness are not covered under Good Samaritan laws. This means that providing help in a manner that is clearly irresponsible or careless can still lead to legal consequences.
Example: If I stop to assist someone who has collapsed, and I provide aid consistent with my first aid training, Good Samaritan Laws would generally protect me from liability for any unintended consequences, provided I acted reasonably and in good faith. However, if I were to administer medication without proper training or knowledge, I could be held liable, regardless of the Good Samaritan Law.
Q 20. What are your skills in using various first aid equipment?
I am proficient in using a wide range of first aid equipment, including:
- Automated External Defibrillator (AED): I’m trained in the proper use and operation of an AED, including recognizing shockable rhythms and performing defibrillation.
- Bandages and Dressings: I’m skilled in applying various types of bandages and dressings, including sterile dressings for wounds, pressure bandages for bleeding control, and slings and splints for fractures.
- Splints and Immobilization Devices: I can effectively use various splints and immobilization devices to stabilize injuries of the extremities.
- Oxygen Administration: I’m trained in administering oxygen using nasal cannulas or masks, as needed.
- Basic airway adjuncts: I am proficient in the use of airway adjuncts, such as oropharyngeal airways, as needed.
- Other equipment: I am familiar with the use of other first aid equipment, including but not limited to tourniquets, suction devices, and personal protective equipment.
Example: I’ve used an AED successfully to revive a patient experiencing cardiac arrest, and I’m proficient in applying splints to immobilize broken bones, control bleeding using direct pressure and tourniquets, and using other first aid equipment.
Q 21. How do you prioritize multiple casualties in a mass casualty incident?
In a mass casualty incident (MCI), prioritizing multiple casualties involves using triage systems to quickly assess and categorize victims based on the severity of their injuries and the likelihood of survival. The most commonly used system is START (Simple Triage and Rapid Treatment).
- START Triage: This system categorizes victims into four groups: Immediate (red), Delayed (yellow), Minimal (green), and Expectant (black). It is based on respiration, perfusion, and mental status.
- Rapid Assessment: In an MCI, speed is crucial. A rapid assessment focusing on the most life-threatening injuries is vital.
- Resource Allocation: Triage informs resource allocation, ensuring the most critically injured receive immediate attention and treatment. Resources are often limited in an MCI, so prioritization is essential.
- Teamwork and Coordination: Effective triage in an MCI requires teamwork and clear communication among responders.
Example: Using the START system, I would rapidly assess each victim, checking for breathing, perfusion (pulse), and mental status. A victim who is not breathing would be immediately tagged as ‘expectant’ (black) if not resuscitated. Victims with severe bleeding or compromised airway would be prioritized and tagged ‘immediate’ (red), while those with less severe injuries would be designated ‘delayed’ (yellow) or ‘minimal’ (green). The ‘immediate’ (red) cases would receive care first, followed by the ‘delayed’ (yellow) and ‘minimal’ (green).
Q 22. Describe your knowledge of different types of wounds and their management.
Wound management is a critical aspect of first aid, and understanding the different types is paramount. Wounds are broadly classified by their depth and cause.
- Abrasions (Scrapes): These are superficial wounds involving the outer layers of skin. Management involves cleaning the wound gently with mild soap and water, applying an antibiotic ointment, and covering with a sterile dressing.
- Lacerations (Cuts): These are deeper wounds caused by sharp objects. Assessment involves checking for depth, bleeding, and foreign bodies. Management may involve direct pressure to control bleeding, cleaning with sterile saline, and potentially sutures or stitches by a medical professional. Deep lacerations require immediate medical attention.
- Puncture Wounds: These are deep, narrow wounds caused by pointed objects like needles or nails. They are particularly dangerous because they can easily become infected. Management focuses on cleaning the surrounding area, applying an antibiotic ointment, and monitoring for signs of infection. A tetanus shot may be necessary depending on vaccination history.
- Avulsions: These wounds involve the tearing away of skin and/or tissue. They require immediate medical attention as they can lead to significant blood loss and may need surgical repair. Management involves controlling bleeding, covering the wound with a sterile dressing, and transporting the individual to a medical facility.
- Burns: Burns are classified by depth (superficial, partial-thickness, full-thickness) and extent (percentage of body surface area). Management focuses on cooling the burn (unless a chemical burn), covering with a sterile dressing, and seeking medical attention, especially for second and third-degree burns.
Proper wound assessment, which includes checking for signs of infection (redness, swelling, pain, pus), is crucial. Always remember to prioritize controlling bleeding and preventing further contamination before any cleaning or dressing application.
Q 23. How do you assess and treat heat stroke and hypothermia?
Heat stroke and hypothermia are serious conditions requiring prompt intervention.
Heat Stroke: This occurs when the body’s temperature regulation system fails, resulting in dangerously high body temperatures. Assessment includes checking for high body temperature (above 104°F or 40°C), altered mental status (confusion, disorientation, unconsciousness), rapid pulse, and hot, dry skin. Treatment involves immediately cooling the person down by removing excess clothing, applying cool compresses or a cool bath, and fanning. Seek immediate medical attention.
Hypothermia: This occurs when the body loses heat faster than it can produce it, leading to dangerously low body temperatures. Assessment involves checking for low body temperature (below 95°F or 35°C), shivering (initially), slow pulse, shallow breathing, confusion, and drowsiness. In advanced stages, shivering stops. Treatment involves gently warming the person, removing wet clothing, providing warm blankets, and giving warm fluids (if conscious). Avoid rough handling and sudden warming, as this can be dangerous. Seek immediate medical attention.
Both heat stroke and hypothermia are life-threatening emergencies. Early recognition and swift action are crucial for improving outcomes.
Q 24. What are the key differences between first aid and emergency medical treatment?
While both first aid and emergency medical treatment aim to alleviate suffering and save lives, there are key differences.
- First Aid: Is the immediate care given to a person who has suffered an injury or sudden illness before professional medical help arrives. It focuses on stabilizing the victim, preventing further injury, and providing basic life support. It’s typically performed by untrained or minimally trained individuals using readily available resources.
- Emergency Medical Treatment: Is the advanced care provided by trained paramedics and EMTs using specialized equipment and medication. It focuses on advanced life support, stabilization for transport, and providing definitive care before reaching a hospital. Emergency medical treatment involves more sophisticated procedures and equipment.
Think of it like this: first aid buys time until professional help arrives. It’s the bridge between the injury and definitive medical care.
Q 25. Describe your experience with working in a team during emergencies.
Teamwork is essential in emergency response. I’ve had extensive experience working collaboratively in diverse team settings during simulated and real-life emergencies. My experience includes:
- Effective communication: I can clearly and concisely communicate assessment findings, treatment plans, and priorities to team members.
- Role clarity: I understand and can effectively perform my role within a team, while also supporting other team members.
- Leadership and delegation: I can assess situations quickly and assign tasks appropriately, based on the strengths of individual team members.
- Stress management: I can maintain composure and focus under pressure, providing guidance and support to others in high-stress situations.
For example, during a simulated mass casualty incident, I effectively coordinated the triage and initial treatment of multiple victims, delegating tasks to volunteers and ensuring effective communication with emergency medical services.
Q 26. How do you stay updated on changes in first aid and emergency response protocols?
Staying updated is crucial in this field, due to constant evolution of best practices. I employ several strategies:
- Professional organizations: I am an active member of [mention relevant organizations, e.g., American Heart Association, American Red Cross], regularly attending conferences and webinars.
- Continuing education: I actively participate in continuing education courses and workshops to stay abreast of the latest advancements in first aid and emergency response protocols.
- Peer review and journals: I regularly read peer-reviewed journals and publications to stay informed about new research and guidelines.
- Online resources: I utilize reputable online resources to access updated guidelines and information from trusted sources.
Continuous learning ensures I maintain high-quality care standards and proficiency in delivering first aid and emergency response.
Q 27. What are your personal strengths and weaknesses related to this position?
Strengths: I possess strong problem-solving skills, remain calm under pressure, have excellent communication skills, am a quick learner, and dedicated to continuing education. My experience in diverse emergency scenarios has made me highly adaptable and resourceful.
Weaknesses: I sometimes find it challenging to delegate tasks when working with individuals less experienced than myself – but I am actively working on improving my delegation and trust-building skills.
Q 28. What are your salary expectations for this role?
My salary expectations are in the range of $[mention salary range] per year, depending on the overall compensation package and benefits offered. I am open to discussing this further.
Key Topics to Learn for First Aid and Emergency Response Training Interview
- Primary Assessment: Understanding the initial steps in assessing a casualty’s condition, including airway, breathing, and circulation (ABCs). Practical application: Describing your approach to a victim found unconscious.
- CPR and Automated External Defibrillator (AED) Use: Mastering the techniques of chest compressions, rescue breaths, and AED operation. Practical application: Explaining the steps involved in performing CPR on an adult and child, including recognizing appropriate scenarios for AED use.
- Bleeding Control: Techniques for controlling various types of bleeding, including direct pressure, elevation, and tourniquet application. Practical application: Differentiating between types of bleeding and selecting appropriate control methods.
- Shock Management: Recognizing the signs and symptoms of shock and implementing appropriate management strategies. Practical application: Explaining how to position a casualty in shock and the importance of maintaining body temperature.
- Fracture and Sprain Management: Proper techniques for splinting and immobilizing injuries. Practical application: Discussing the principles of proper splinting and choosing appropriate splinting materials for different types of fractures.
- Emergency Response Procedures: Understanding scene safety, calling emergency services, and patient handover protocols. Practical application: Describing your actions in a multi-casualty incident and outlining effective communication strategies with emergency responders.
- Legal and Ethical Considerations: Understanding the legal implications of providing first aid and the importance of obtaining consent. Practical application: Discussing the boundaries of your scope of practice and the importance of documentation.
- Specific First Aid for common emergencies: Burns, poisoning, allergic reactions, heat stroke/hypothermia. Practical application: Detailing your approach to managing these specific scenarios based on best practices.
Next Steps
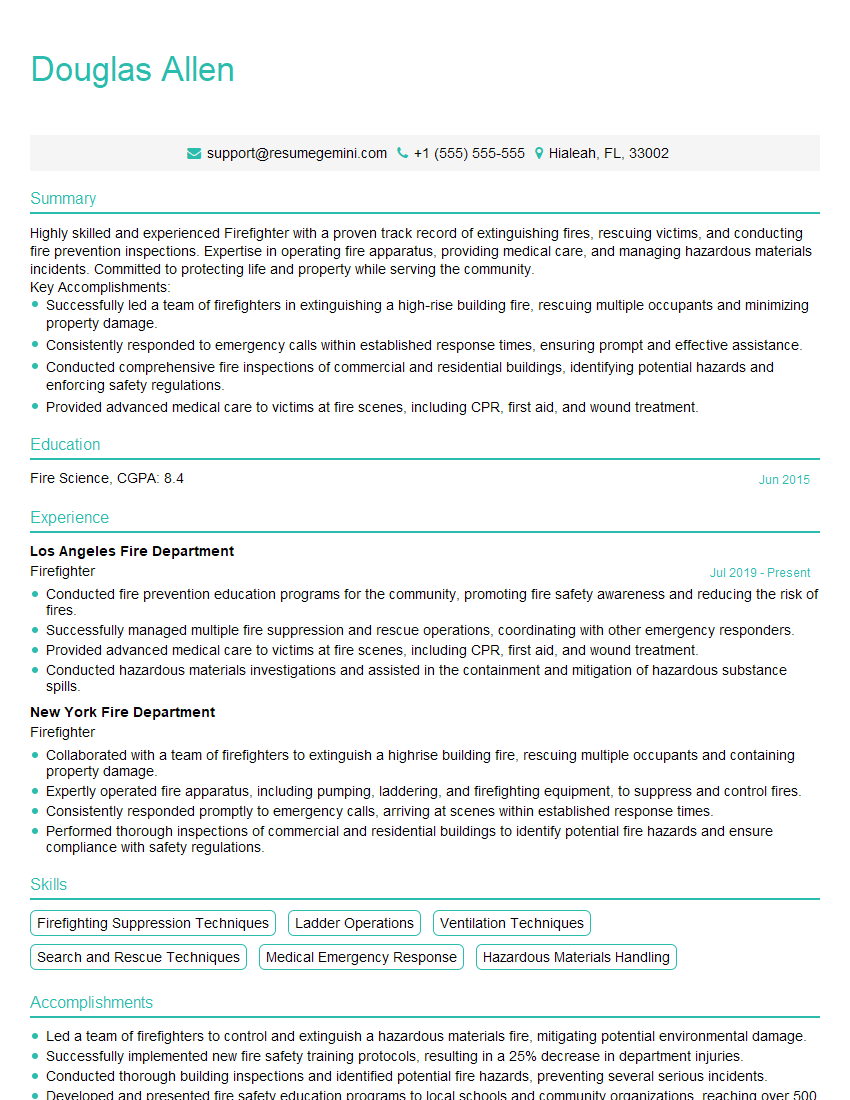
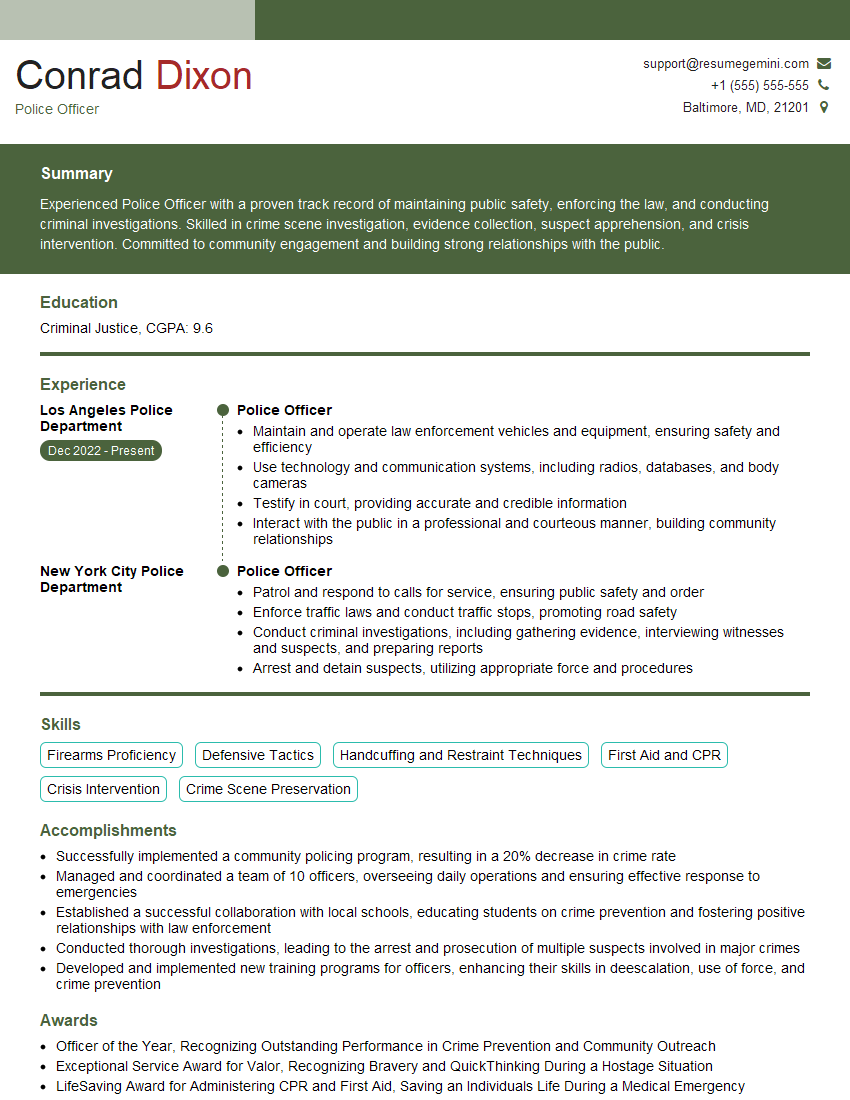
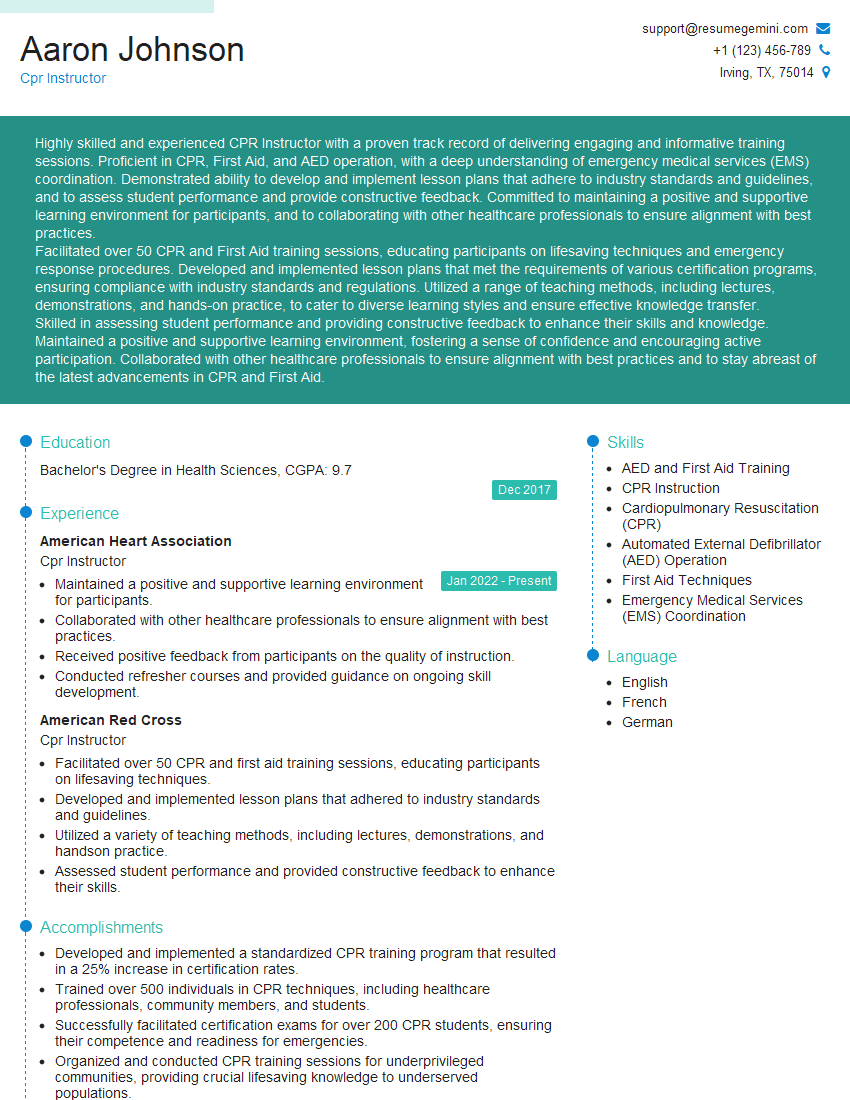
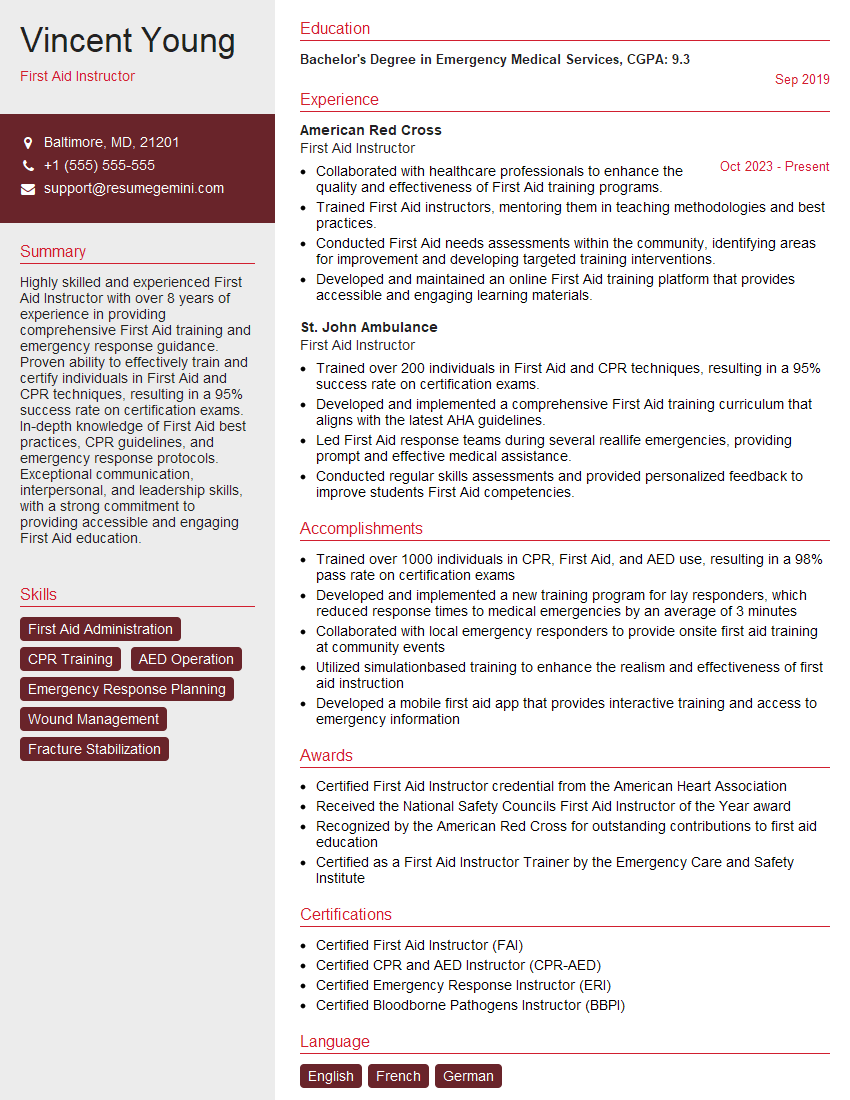
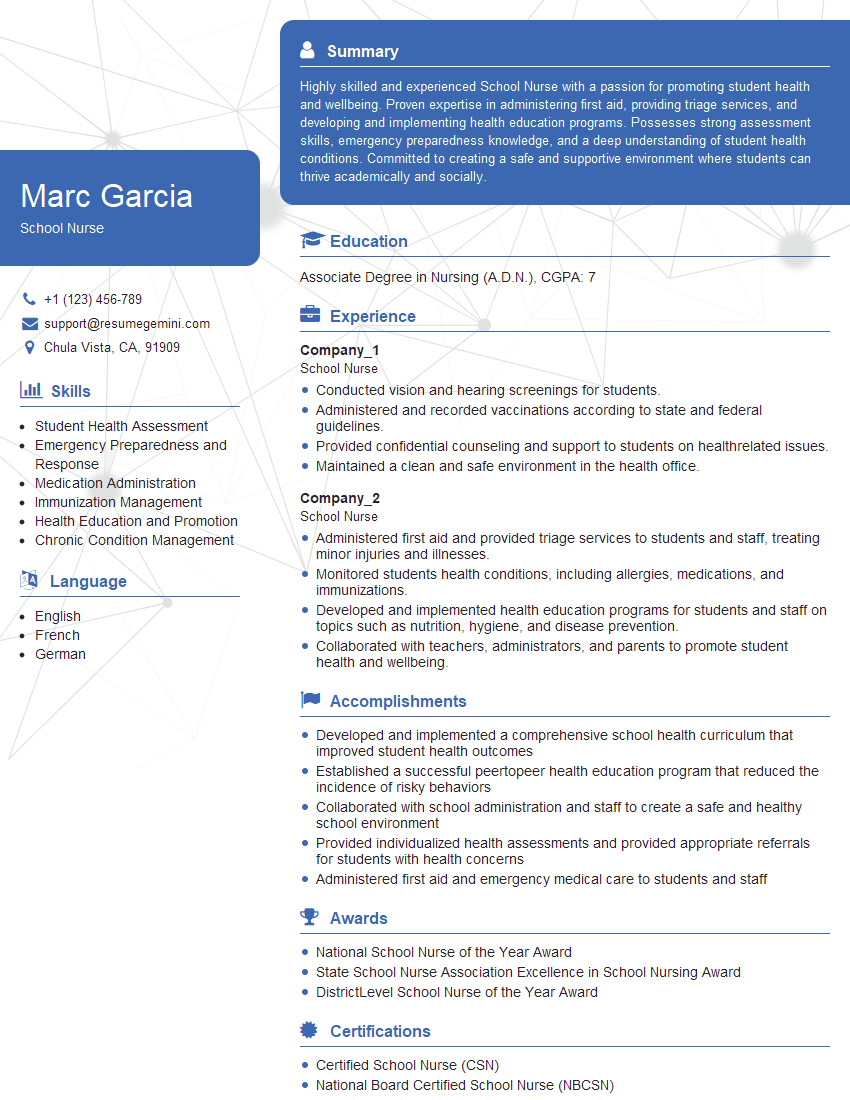
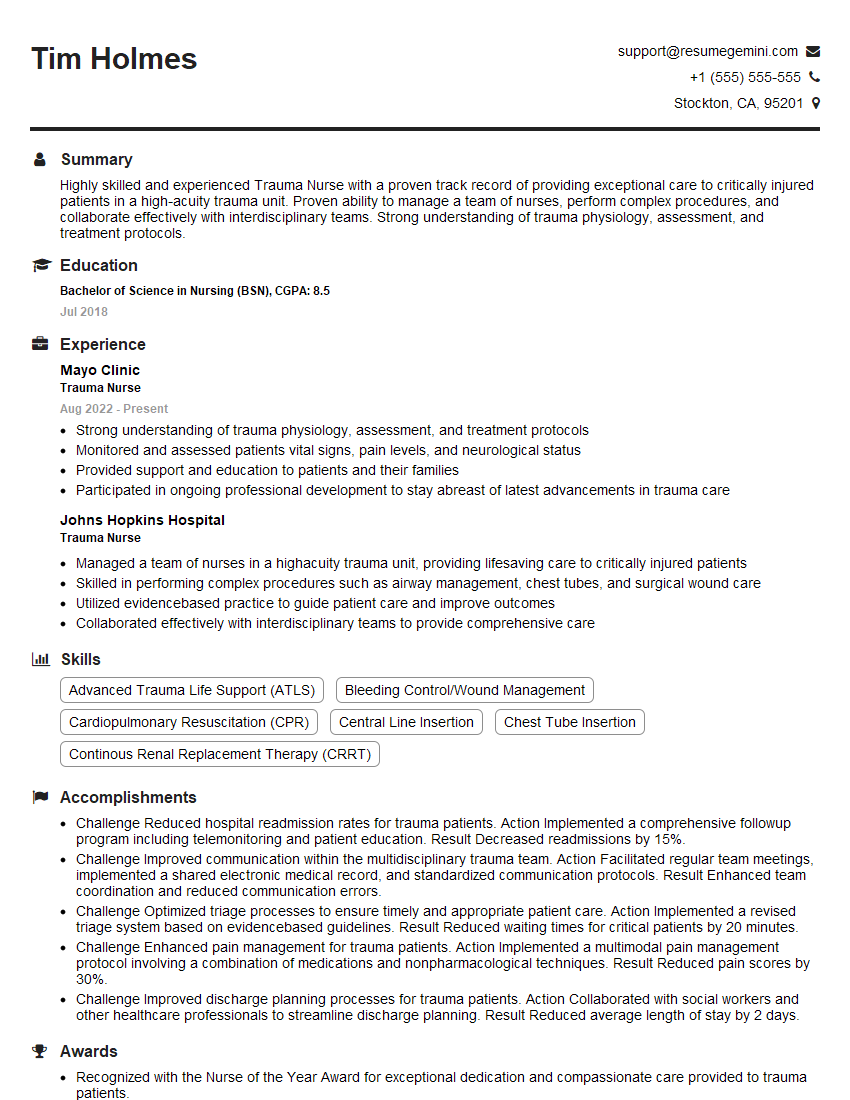
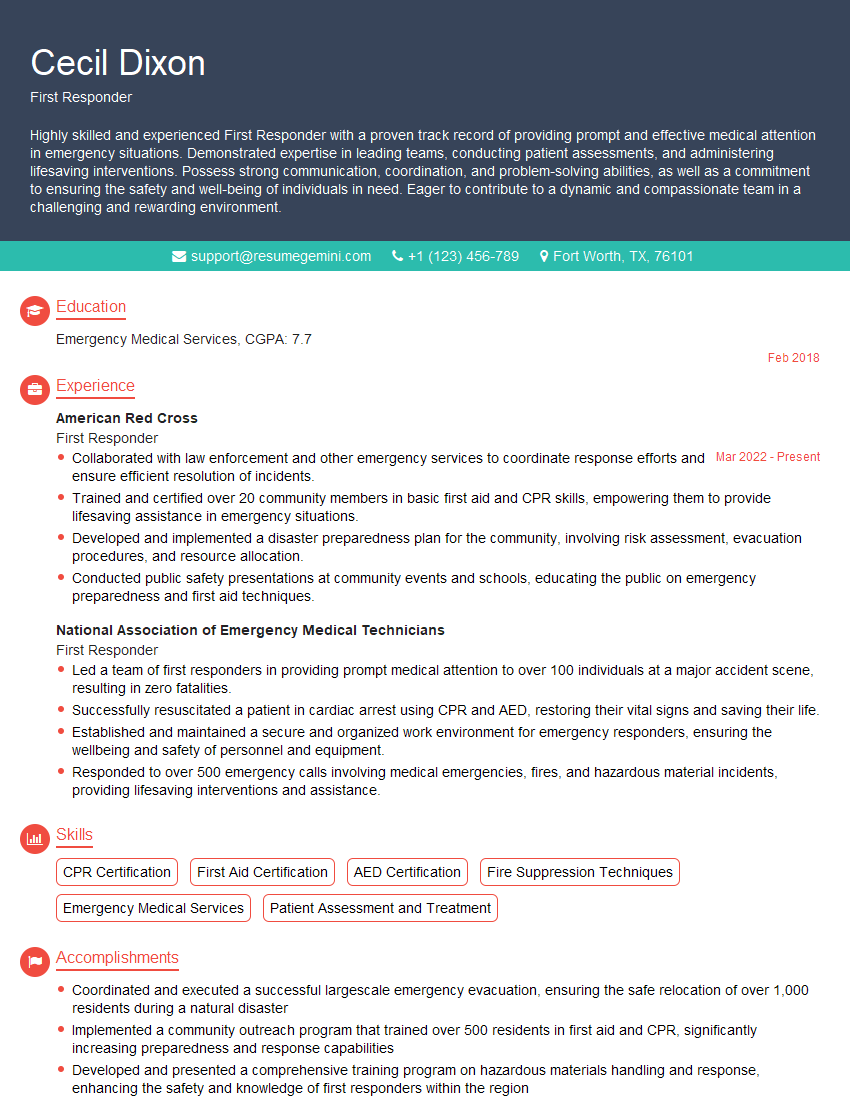
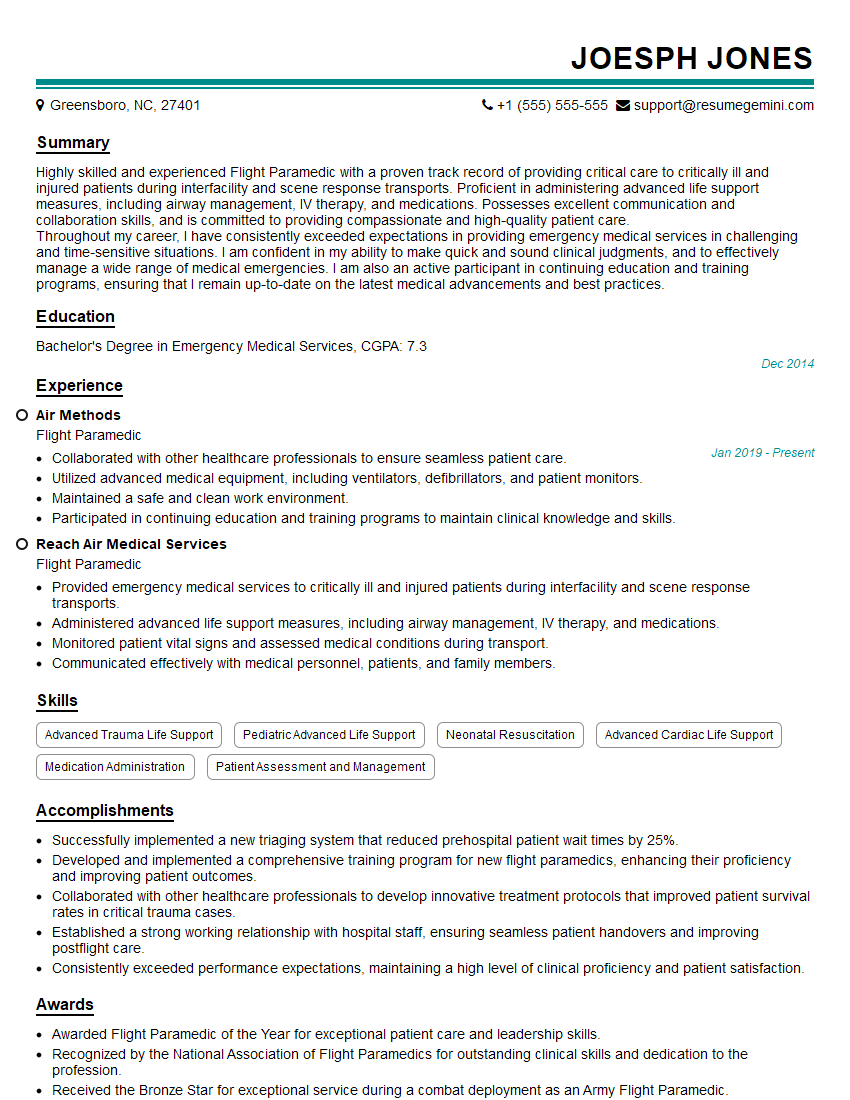
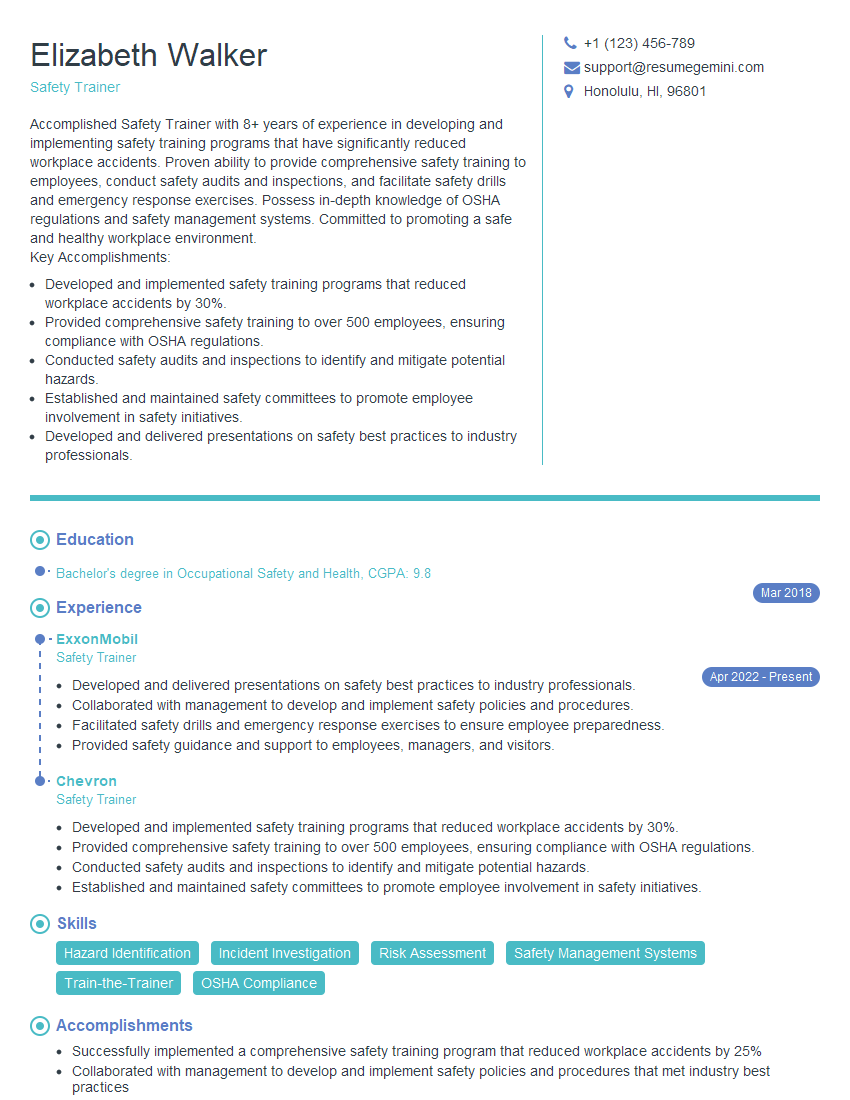
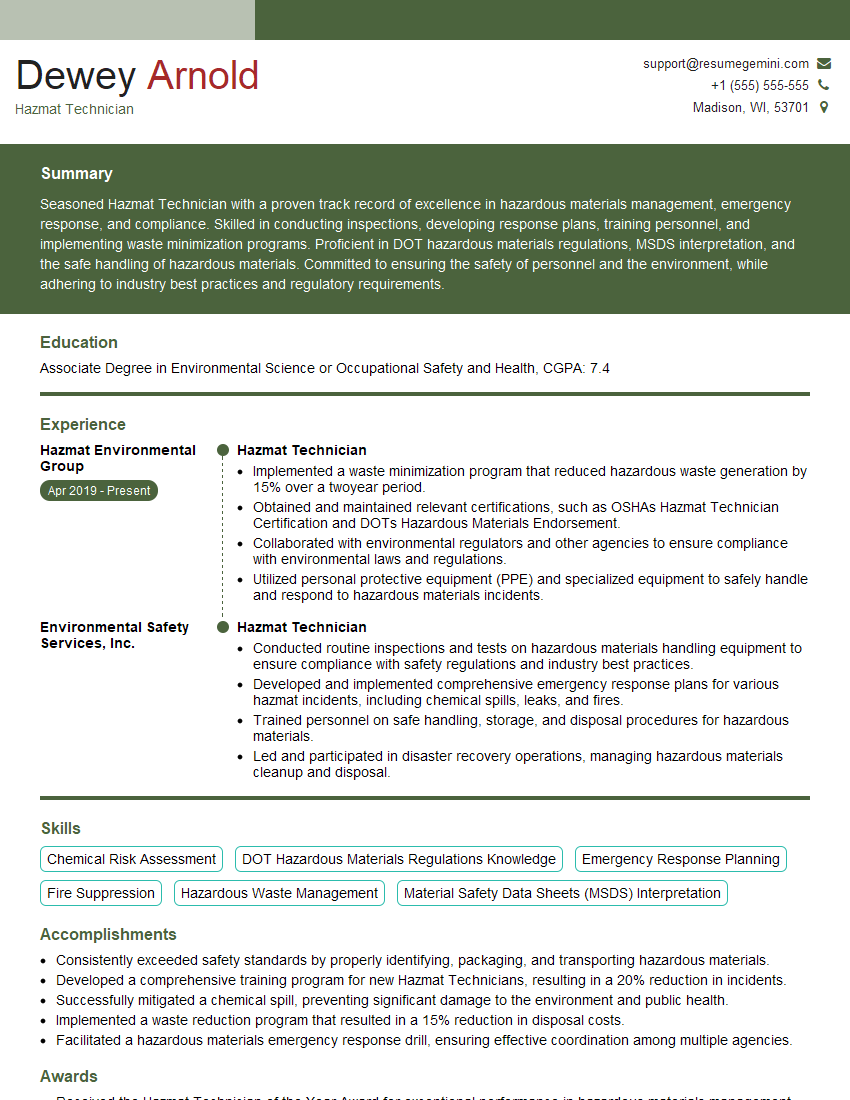
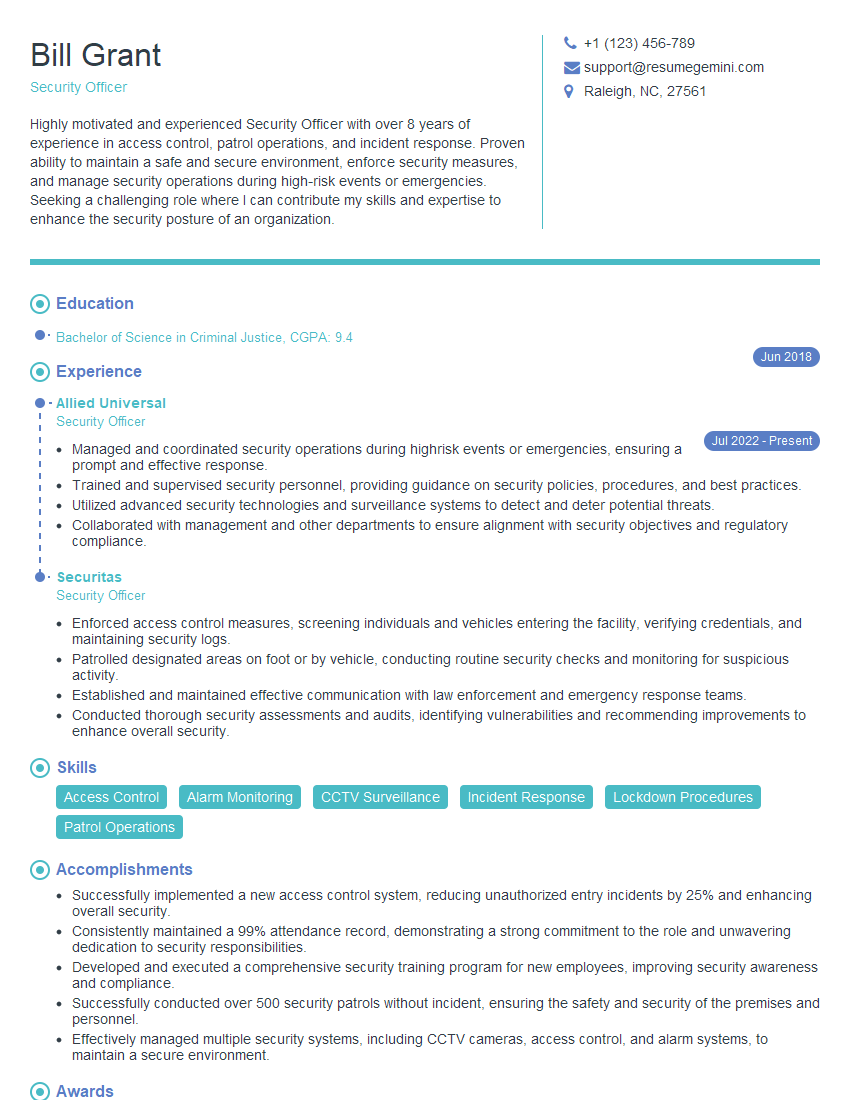
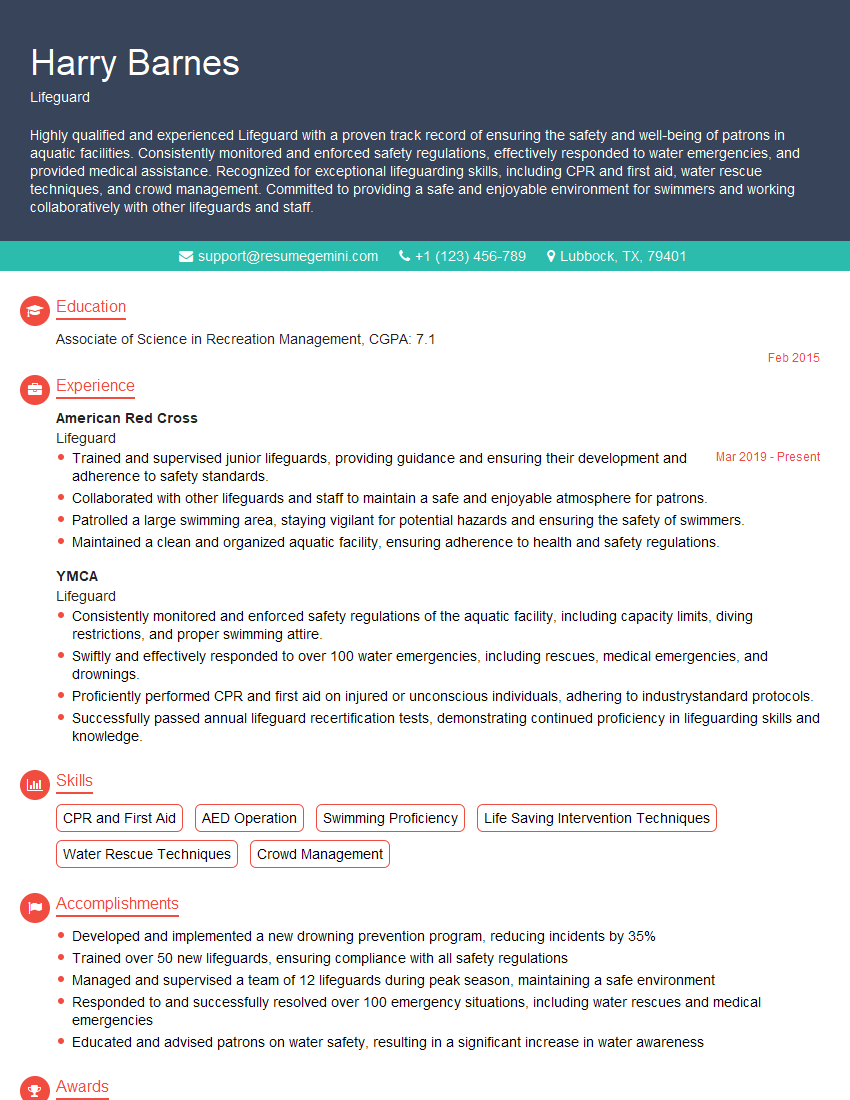
Mastering First Aid and Emergency Response Training significantly enhances your career prospects in healthcare, safety, and related fields. It demonstrates a commitment to helping others and possessing valuable, in-demand skills. To maximize your chances of securing your dream role, create a compelling and ATS-friendly resume that showcases your abilities effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored specifically to First Aid and Emergency Response Training positions to help you get started. This will significantly improve your chances of getting noticed by potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
we currently offer a complimentary backlink and URL indexing test for search engine optimization professionals.
You can get complimentary indexing credits to test how link discovery works in practice.
No credit card is required and there is no recurring fee.
You can find details here:
https://wikipedia-backlinks.com/indexing/
Regards
NICE RESPONSE TO Q & A
hi
The aim of this message is regarding an unclaimed deposit of a deceased nationale that bears the same name as you. You are not relate to him as there are millions of people answering the names across around the world. But i will use my position to influence the release of the deposit to you for our mutual benefit.
Respond for full details and how to claim the deposit. This is 100% risk free. Send hello to my email id: [email protected]
Luka Chachibaialuka
Hey interviewgemini.com, just wanted to follow up on my last email.
We just launched Call the Monster, an parenting app that lets you summon friendly ‘monsters’ kids actually listen to.
We’re also running a giveaway for everyone who downloads the app. Since it’s brand new, there aren’t many users yet, which means you’ve got a much better chance of winning some great prizes.
You can check it out here: https://bit.ly/callamonsterapp
Or follow us on Instagram: https://www.instagram.com/callamonsterapp
Thanks,
Ryan
CEO – Call the Monster App
Hey interviewgemini.com, I saw your website and love your approach.
I just want this to look like spam email, but want to share something important to you. We just launched Call the Monster, a parenting app that lets you summon friendly ‘monsters’ kids actually listen to.
Parents are loving it for calming chaos before bedtime. Thought you might want to try it: https://bit.ly/callamonsterapp or just follow our fun monster lore on Instagram: https://www.instagram.com/callamonsterapp
Thanks,
Ryan
CEO – Call A Monster APP
To the interviewgemini.com Owner.
Dear interviewgemini.com Webmaster!
Hi interviewgemini.com Webmaster!
Dear interviewgemini.com Webmaster!
excellent
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good