Preparation is the key to success in any interview. In this post, we’ll explore crucial Intervention Techniques interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Intervention Techniques Interview
Q 1. Describe your experience implementing different intervention strategies.
Throughout my career, I’ve implemented a wide range of intervention strategies, tailoring my approach to the specific needs of each individual and situation. This includes utilizing Cognitive Behavioral Therapy (CBT) techniques to help individuals identify and modify negative thought patterns and behaviors, particularly effective in addressing anxiety and depression. I’ve also employed motivational interviewing, a client-centered approach that guides individuals towards recognizing their own intrinsic motivation for change. In crisis situations, I’ve relied heavily on de-escalation techniques, focusing on active listening, empathy, and establishing safety. Furthermore, I have experience with family systems therapy, focusing on improving communication and interaction dynamics within families, to address issues such as conflict or substance abuse.
For instance, I worked with a young adult struggling with substance abuse. Initially, I used motivational interviewing to explore their reasons for wanting change, addressing their ambivalence. Then, we incorporated CBT techniques to manage cravings and develop coping mechanisms for stressful situations that triggered substance use. The results were very positive, as the individual successfully completed their rehab program and maintained sobriety.
In another case, I worked with a family experiencing intense conflict. Using family systems therapy, I guided them in identifying dysfunctional communication patterns and developed strategies for improving healthy interaction. The result was a significant decrease in conflict and improved family cohesion.
Q 2. Explain the difference between crisis intervention and preventative intervention.
Crisis intervention and preventative intervention are distinct but related approaches. Crisis intervention focuses on immediate stabilization and support during a period of acute distress. It’s about managing the immediate situation, providing short-term relief, and connecting individuals with necessary resources. Think of it as putting out a fire – addressing the immediate danger. Preventative intervention, on the other hand, aims to prevent problems from developing in the first place. This involves proactive strategies designed to enhance coping skills, resilience, and protective factors before a crisis occurs. It’s akin to installing a fire alarm – mitigating future risks.
For example, crisis intervention might involve de-escalating a suicidal individual, providing immediate emotional support, and connecting them to emergency mental health services. Preventative intervention, in contrast, might involve providing stress management workshops to high-risk populations or implementing early childhood education programs to foster resilience.
Q 3. How do you assess the urgency and risk level in a crisis situation?
Assessing urgency and risk in a crisis situation requires a comprehensive approach. I utilize a multi-faceted assessment, considering several key factors: The individual’s immediate behaviors (e.g., self-harm threats, aggression), their emotional state (e.g., intense anxiety, panic), their history (e.g., previous suicide attempts, substance abuse), their social support system (e.g., lack of support network), and the environment (e.g., access to weapons, unsafe living conditions).
This assessment typically involves careful observation, direct questioning, and potentially consulting with collateral sources when appropriate (e.g., family members, previous therapists). I use standardized risk assessment tools whenever necessary and always prioritize the safety of the individual and those around them. A higher score on a risk assessment or more concerning indicators significantly increase urgency and the need for immediate intervention.
For instance, if someone is actively expressing suicidal ideation with a detailed plan and access to lethal means, the urgency level is extremely high. Conversely, someone expressing general feelings of hopelessness but without a plan or means, would have lower urgency, although intervention is still necessary.
Q 4. What ethical considerations guide your intervention choices?
Ethical considerations are paramount in intervention work. My practice is guided by several key principles: Confidentiality, ensuring the privacy of individuals unless legally mandated to disclose information; Beneficence, acting in the best interests of the individual; Non-maleficence, avoiding harm; Autonomy, respecting the individual’s right to self-determination; and Justice, ensuring fair and equitable treatment.
This also includes being mindful of cultural sensitivity and avoiding biases in my assessment and intervention planning. I always strive to maintain professional boundaries and adhere to relevant professional codes of ethics, ensuring my actions are transparent and accountable. For example, if a client shares information that suggests potential harm to others, I must carefully weigh the ethical obligation of confidentiality against the duty to protect those at risk. This frequently necessitates consultation with supervisors or legal counsel.
Q 5. Describe your approach to building rapport with individuals in crisis.
Building rapport with individuals in crisis is crucial for effective intervention. It involves creating a safe and trusting environment where individuals feel heard, understood, and validated. This starts with demonstrating empathy, active listening, and using non-judgmental language. I make sure to verbally and nonverbally communicate genuine care and concern. I employ techniques such as mirroring body language, reflecting emotions, and validating their experiences. I avoid interrupting and demonstrate active listening through verbal cues and summarizing their points.
It’s about meeting people where they are, acknowledging their emotions without minimizing or dismissing them. Building rapport often starts with simply acknowledging their distress and validating their feelings. For example, “I can see that you are really upset right now, and that must be very difficult.” This can help to de-escalate the situation and create an opening for further communication.
Q 6. How do you handle resistance or non-compliance during an intervention?
Resistance or non-compliance is common in intervention situations and should be understood as a sign that the individual might need a different approach. It’s crucial to avoid confrontation and instead explore the reasons behind the resistance. This might involve asking open-ended questions, reflecting their feelings, and exploring their concerns. The goal is not to force compliance, but rather to build trust and collaboration.
Strategies for addressing resistance might include collaboratively developing a plan, offering choices, and acknowledging the individual’s autonomy. It might also involve modifying the intervention strategy, exploring different approaches, or involving other supports. It’s important to remember that forcing compliance can be counterproductive and potentially harmful.
For example, if a client refuses to engage in a specific therapy technique, I might explore their reasons for refusal, perhaps uncovering underlying anxieties or mistrust. Then, I would work collaboratively to find a more acceptable alternative.
Q 7. What are some common barriers to effective intervention, and how do you overcome them?
Several barriers can hinder effective intervention. Lack of resources, including limited access to mental health services, financial constraints, or lack of support networks, can significantly impact the effectiveness of intervention. Cultural barriers, such as language differences or cultural misunderstandings, can create obstacles in communication and trust. Resistance from the individual or their family, as previously discussed, can also hinder progress. Additionally, ethical dilemmas, such as confidentiality concerns, can complicate decision-making.
To overcome these barriers, I prioritize collaboration, advocacy, and resourcefulness. I work closely with individuals and their families to address their concerns, advocate for access to necessary resources, and creatively find solutions to challenges. I ensure cultural sensitivity and competence in my interactions and actively seek consultation with colleagues or supervisors when facing ethical dilemmas or complex situations.
For instance, if a client lacks access to affordable mental health services, I would assist them in navigating resources such as community mental health clinics, sliding-scale therapists, or public assistance programs.
Q 8. Explain the importance of cultural competency in intervention strategies.
Cultural competency is paramount in intervention strategies because it ensures that interventions are relevant, respectful, and effective for individuals from diverse backgrounds. Ignoring cultural differences can lead to misunderstandings, mistrust, and ultimately, intervention failure. It’s about understanding and appreciating the unique values, beliefs, practices, and worldviews of individuals and communities, adapting approaches accordingly.
For example, consider a family therapy session with a family of Hispanic descent. A culturally competent therapist would be aware of the strong emphasis on family cohesion and respect for elders within many Hispanic cultures. They would tailor their approach to include the entire family in the discussion, giving due respect to the elder’s input, rather than focusing solely on the identified patient, as might be typical in a more individualistic therapeutic approach.
- Awareness: Recognizing one’s own biases and assumptions.
- Knowledge: Understanding the diverse cultural groups you serve.
- Skills: Using culturally appropriate communication and intervention techniques.
- Engagement: Building rapport and trust with clients from diverse backgrounds.
Q 9. Describe your experience working with diverse populations requiring intervention.
Throughout my career, I’ve worked with a wide range of populations, including individuals experiencing substance abuse, mental health challenges, trauma, and various other difficulties. This has encompassed working with diverse ethnic, racial, socioeconomic, religious, and LGBTQ+ communities. For instance, I worked with a refugee population experiencing significant post-traumatic stress disorder (PTSD) following displacement from their home country. Understanding their cultural context – their experiences with violence, loss, and their unique coping mechanisms – was vital to developing effective intervention strategies. We adapted traditional trauma-informed care to incorporate culturally relevant elements, such as group therapy sessions facilitated by a bilingual interpreter who was part of their community.
Another example involved working with young people from marginalized communities who were at risk of gang involvement. Understanding their lived experiences, including systemic inequalities and social pressures, was critical. Intervention focused on building resilience, empowering them through mentorship programs, and fostering positive connections with supportive adults within their community. Successful interventions required building trust, establishing safe spaces, and addressing the root causes of their risk behaviors, rather than simply addressing the symptoms.
Q 10. How do you document interventions and progress notes?
Documentation is crucial for accountability, continuity of care, and legal protection. I use a clear and concise format that includes the date, time, and type of intervention provided. This includes a detailed description of the client’s presentation, the goals of the intervention, the methods used, and the client’s response. I also document any relevant collateral information, such as communication with other professionals or family members.
Progress notes specifically track the client’s progress towards their treatment goals. I use measurable outcomes to track improvement. For example, if a client’s goal is to reduce anxiety, I might document changes in their self-reported anxiety levels using validated scales, their attendance at therapy sessions, and observable behaviors indicative of reduced anxiety during our sessions.
All documentation adheres to strict confidentiality guidelines, following HIPAA regulations and agency-specific policies. The language used is professional, objective, and avoids subjective opinions or judgments.
Q 11. What methods do you use to assess the effectiveness of your interventions?
Assessing intervention effectiveness is an ongoing process, not a single event. I utilize various methods, including:
- Client self-report measures: Standardized questionnaires and scales assess changes in symptoms, behaviors, and overall well-being.
- Behavioral observations: I directly observe changes in the client’s behavior and interactions.
- Objective data: I collect data such as attendance rates, medication adherence, and completion of assignments.
- Feedback from others: When appropriate, I involve family members or other professionals in the evaluation process to gather a holistic view of progress.
Regular progress reviews with the client allow for open discussion of the effectiveness of the interventions. We collaboratively adjust the intervention plan as needed to ensure it remains appropriate and beneficial. If an intervention is not effective, we explore alternative approaches.
Q 12. How do you collaborate with other professionals to provide comprehensive intervention?
Effective interventions often require a multidisciplinary approach. I regularly collaborate with psychiatrists, psychologists, social workers, case managers, and other professionals to provide holistic and comprehensive care. This involves:
- Regular meetings: Case conferences and team meetings provide a forum for sharing information and coordinating care.
- Written communication: Progress notes and reports ensure all relevant professionals have access to the client’s information.
- Direct communication: Phone calls or emails allow for immediate clarification or coordination of services.
For example, in a case of substance abuse, I would collaborate with a psychiatrist for medication management, a case manager for housing and employment support, and a family therapist for family dynamics.
Q 13. How do you maintain confidentiality and ethical boundaries in your work?
Maintaining confidentiality and ethical boundaries is fundamental to my practice. I strictly adhere to HIPAA regulations and agency policies. This involves:
- Protecting client information: Securely storing and transmitting client records, only disclosing information with the client’s consent or as required by law.
- Avoiding dual relationships: Maintaining professional boundaries and avoiding personal relationships with clients.
- Managing potential conflicts of interest: Disclosing any potential conflicts and taking appropriate steps to mitigate them.
- Seeking supervision: Regularly consulting with supervisors for guidance on complex ethical dilemmas.
If a situation arises where I am unsure about ethical considerations, I consult with my supervisor or ethical resources to ensure compliance with professional standards.
Q 14. Describe your experience with specific intervention models (e.g., motivational interviewing, CBT).
I have extensive experience with various intervention models. Motivational Interviewing (MI) is a client-centered approach that helps individuals resolve ambivalence toward change by exploring their own reasons for and against change. I use MI frequently with clients who are resistant to change or unsure about their readiness for intervention. For example, with a client struggling with substance abuse, I might use MI to explore their values and goals, helping them identify their own reasons for wanting to make changes.
Cognitive Behavioral Therapy (CBT) helps clients identify and modify negative thought patterns and maladaptive behaviors. I often use CBT to address anxiety, depression, and trauma. For example, in treating anxiety, CBT might involve identifying anxious thoughts, challenging their validity, and developing coping strategies.
My approach is eclectic, integrating aspects of different models depending on the client’s needs and the presenting problem. The choice of intervention is always tailored to the individual’s unique circumstances and preferences.
Q 15. How do you tailor your intervention approach to the specific needs of individuals?
Tailoring interventions requires a deep understanding of the individual’s unique circumstances. It’s not a one-size-fits-all approach. I begin with a thorough assessment, considering factors like the person’s age, cultural background, developmental stage, presenting problem, strengths, and support system. This might involve using validated assessment tools, conducting interviews, and reviewing relevant records. For example, an intervention for a teenager struggling with substance abuse will differ significantly from one for an elderly adult experiencing depression. With the teenager, I might focus on peer influence, social media usage, and school performance, while with the older adult, I’d prioritize their physical health, social isolation, and potential grief or loss. The intervention strategy then becomes a personalized plan focusing on achievable goals, building on existing strengths, and addressing specific needs. This might involve selecting specific therapeutic modalities, such as Cognitive Behavioral Therapy (CBT) for anxiety or Dialectical Behavior Therapy (DBT) for emotional regulation, tailored to their individual learning style and preferences.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of trauma-informed care and its relevance to interventions.
Trauma-informed care is crucial in intervention. It recognizes that many individuals have experienced traumatic events that significantly impact their behavior, emotions, and relationships. It emphasizes understanding the impact of trauma and avoiding re-traumatization. Instead of focusing solely on deficits, a trauma-informed approach centers on strengths, resilience, and empowerment. This means creating a safe and supportive environment, fostering trust, respecting autonomy, emphasizing collaboration, and avoiding potentially triggering language or actions. For instance, if working with a client who has experienced domestic violence, I would be mindful of not using language that could be triggering, such as ‘attack’ or ‘victim’. Instead, I might use terms like ‘experience’ or ‘difficult situation.’ I would prioritize building rapport, and allow the client to set the pace of the session. This approach builds a stronger therapeutic alliance and improves the effectiveness of the intervention.
Q 17. Describe your experience with de-escalation techniques in high-stress situations.
De-escalation is a critical skill in high-stress situations. My approach centers on maintaining calm and establishing rapport. I start by actively listening and validating the individual’s feelings, even if I don’t agree with their behavior. I use verbal and nonverbal communication to convey empathy and understanding. For example, maintaining eye contact at an appropriate level, using a calm and reassuring tone of voice, and mirroring their body language (without mimicking aggression) can help. Physical de-escalation techniques are used only as a last resort and should be employed safely and ethically, ideally with proper training and in accordance with established protocols. I might utilize techniques like creating physical space, offering choices, and redirecting attention towards a calming activity. In one instance, I de-escalated a situation with a client experiencing a psychotic episode by calmly speaking to him in a quiet room, offering him a drink of water and allowing him some time to compose himself before engaging in a therapeutic dialogue.
Q 18. How do you ensure safety for both the client and yourself during an intervention?
Ensuring safety is paramount. This involves risk assessment at the outset of any intervention, considering both the client’s potential for harm to themselves or others and my own safety. Environmental factors, such as having a clear escape route or ensuring the setting is well-lit and free from potential weapons, are considered. For example, having a colleague present during a particularly high-risk session is a standard precaution. I’m also very familiar with de-escalation techniques and crisis management protocols. Clear boundaries are set from the beginning of the intervention process, clearly defining acceptable and unacceptable behaviors. If a situation escalates beyond my abilities, I will immediately seek support from colleagues or emergency services. Regular supervision and continuing education on safety protocols are essential to maintain competence and minimize risks.
Q 19. What are the key components of a successful intervention plan?
A successful intervention plan comprises several key components. First, a thorough assessment of the client’s needs and strengths is crucial. Then, clearly defined, measurable, achievable, relevant, and time-bound (SMART) goals are established in collaboration with the client. The plan outlines specific interventions, such as therapy modalities, medication management (if applicable), and support services. A timeline is established, and methods for monitoring progress are determined. Regular reviews of the plan ensure it remains relevant and effective. Furthermore, a clear process for addressing any setbacks or crises is included, emphasizing flexibility and adaptability to changing circumstances. For example, an intervention plan for substance abuse might include regular therapy sessions, participation in a support group, random drug testing, and contingency management strategies.
Q 20. How do you involve family and support systems in the intervention process?
Involving family and support systems is often crucial for successful interventions. I strive to create a collaborative relationship with the family, acknowledging their important role in the client’s life. This involves explaining the intervention plan in a clear and accessible manner, and actively soliciting their feedback and involvement. This can include family therapy sessions, education about the client’s condition, and the development of strategies for supporting the client at home. However, ethical considerations, such as client confidentiality, must always be respected, and the client’s consent should be obtained before sharing information with family members. Respecting boundaries and empowering the client to lead the way in this collaboration are central to this aspect of the intervention process. In some cases, involving a family member in the intervention itself can significantly contribute to success.
Q 21. What is your approach to managing your own stress and burnout while working in intervention?
Working in interventions can be emotionally demanding, and self-care is essential to prevent burnout. I prioritize maintaining a healthy work-life balance, setting boundaries, and engaging in regular self-reflection. I make use of techniques like mindfulness and stress-reduction practices to manage stress and improve emotional regulation. Regular supervision sessions with a qualified professional provide a supportive forum for processing complex cases and seeking guidance on challenging situations. Connecting with colleagues and engaging in peer support also helps foster a sense of community and shared understanding. This professional community provides emotional support and acts as a preventative measure against professional isolation. It’s a continuous process of self-awareness, seeking help when needed, and prioritizing my own well-being to ensure I can effectively support those I work with.
Q 22. Describe a challenging intervention case and how you successfully resolved it.
One of the most challenging intervention cases I handled involved a young adult struggling with severe substance abuse and co-occurring depression. He had multiple failed attempts at rehab, a strained relationship with his family, and a history of self-harm. The initial challenge was establishing trust. He was deeply cynical and resistant to any form of help.
My approach involved a collaborative, person-centered strategy. Instead of imposing solutions, I focused on actively listening to his experiences and validating his feelings. We worked together to identify his strengths, values, and goals, even seemingly small ones. I utilized motivational interviewing techniques to explore his ambivalence toward change, guiding him to discover his own reasons for wanting to get better, rather than lecturing him on the consequences of his actions. We developed a tailored intervention plan, focusing on building coping mechanisms for stress and depression alongside addressing his substance abuse. This included connecting him with a therapist specializing in trauma and substance abuse, and incorporating mindfulness practices. Regular check-ins, flexible goal setting, and consistent positive reinforcement were vital. Eventually, he found his own motivation for change, and with continued support and consistent effort, he made significant progress, staying sober for over a year and successfully navigating his depressive symptoms. The case highlighted the crucial role of building rapport, utilizing motivational interviewing, and employing a holistic approach that addresses both the substance abuse and underlying mental health issues.
Q 23. Explain your understanding of the different stages of change in the intervention process.
The stages of change, often referred to as the Transtheoretical Model, are crucial in understanding and guiding the intervention process. They illustrate the progression an individual goes through as they modify a behavior or address a problem. These stages are:
- Precontemplation: The individual isn’t considering change. They might be unaware of the problem or unwilling to acknowledge it.
- Contemplation: The individual is aware of the problem and is starting to think about changing but hasn’t yet made a commitment.
- Preparation: The individual is planning to take action and making small changes to prepare for a bigger shift.
- Action: The individual is actively working towards changing their behavior.
- Maintenance: The individual has maintained the change for a significant period and is working to prevent relapse.
- Relapse: The individual experiences a setback and returns to their previous behavior. This isn’t considered a failure but rather a part of the process.
Understanding these stages allows an interventionist to tailor their approach to the individual’s current position. For example, with someone in the precontemplation stage, the focus is on raising awareness and building motivation, whereas someone in the action stage needs support and strategies to maintain their progress.
Q 24. How do you measure the long-term outcomes of your interventions?
Measuring long-term outcomes of interventions requires a multifaceted approach. It’s not enough to simply track immediate changes. We need to assess sustained behavioral modifications and improved overall well-being.
I employ several methods:
- Follow-up assessments: Regular check-ins using standardized questionnaires and interviews to track progress on key indicators (e.g., substance use, mental health symptoms, social functioning).
- Data collection from multiple sources: Collaborating with other professionals (e.g., therapists, physicians) to gain a comprehensive picture. This might include review of medical records or reports from family members (with appropriate consent).
- Qualitative data: Gathering narratives and feedback through interviews, to understand the individual’s lived experience and perceive changes in their perspective and self-efficacy.
- Objective measures: Utilizing quantifiable data, such as lab results (for substance use) or reduced hospital readmissions.
The frequency of follow-up assessments depends on the individual’s needs and the nature of the intervention. A long-term perspective, often encompassing years, is essential for truly understanding the impact and effectiveness of the intervention.
Q 25. What are your strengths and weaknesses regarding intervention techniques?
My strengths lie in my ability to build rapport quickly, adapt my approach to diverse individuals, and employ evidence-based strategies, tailoring them to each person’s unique circumstances. I am skilled in motivational interviewing and person-centered therapy. I actively listen, and I strive to create a safe and trusting environment where individuals feel comfortable sharing their vulnerabilities.
Areas for improvement include further development of my skills in working with individuals from certain cultural backgrounds and increasing my proficiency in utilizing specific technology platforms for data analysis. I’m actively working on this through continuing education and seeking mentorship from experienced colleagues.
Q 26. What are some continuing education activities you have undertaken related to intervention?
To maintain my expertise, I’ve completed several continuing education activities. This includes a specialized workshop on trauma-informed care, an advanced training in motivational interviewing, and a certification program in substance abuse treatment. I regularly attend conferences and workshops to stay abreast of cutting-edge research and best practices in the field. Furthermore, I’ve participated in ongoing supervision and peer consultation sessions to enhance my clinical skills and address challenging case presentations.
Q 27. How do you stay updated on the latest research and best practices in intervention?
Staying updated on the latest research and best practices is vital. I achieve this through several avenues:
- Subscription to professional journals: I regularly read publications such as the Journal of Consulting and Clinical Psychology and the Journal of Substance Abuse Treatment.
- Membership in professional organizations: My membership in relevant professional groups provides access to publications, conferences, and continuing education opportunities.
- Participation in online communities and forums: Engagement with online communities and discussion forums allows for an exchange of knowledge and experiences with other professionals.
- Attending conferences and workshops: Conferences and workshops provide the chance to network with others in the field and gain practical insights from experts.
I also actively search for relevant research studies through databases like PubMed and PsycINFO.
Q 28. Describe your experience with specific software or technology used for intervention documentation or support.
I have extensive experience using electronic health record (EHR) systems for intervention documentation and client management. I am proficient in using [Name of specific EHR system], which allows for secure documentation, progress tracking, and communication with other professionals involved in the client’s care. The system’s features include progress note templates, customized reporting tools for tracking outcomes, and secure messaging functionality for client communication and collaboration with the treatment team. I also utilize [Name of specific telehealth platform, if applicable] for remote sessions and data sharing when appropriate. The ability to use these technologies seamlessly and efficiently ensures client confidentiality and enhances the overall efficiency of the intervention process.
Key Topics to Learn for Intervention Techniques Interview
- Crisis Intervention Models: Understanding various models (e.g., Directive vs. Non-Directive) and their appropriate application in diverse situations.
- Assessment and Planning: Developing comprehensive assessments of individuals in crisis, formulating effective intervention plans, and setting realistic goals.
- Communication Skills: Mastering active listening, empathy, and building rapport to establish trust and facilitate open communication during interventions.
- Ethical Considerations: Navigating ethical dilemmas, ensuring client confidentiality, and understanding legal boundaries within the scope of intervention practice.
- Case Management and Collaboration: Coordinating care with multidisciplinary teams, navigating referral processes, and ensuring continuity of care.
- Trauma-Informed Approaches: Implementing trauma-sensitive strategies and recognizing the impact of trauma on individuals’ responses to intervention.
- Specific Intervention Techniques: Understanding and applying various techniques such as motivational interviewing, cognitive behavioral therapy (CBT) principles, and de-escalation strategies.
- Documentation and Reporting: Maintaining accurate and comprehensive records of interventions, adhering to agency guidelines, and preparing effective reports.
- Self-Care and Resilience: Recognizing the importance of self-care practices to mitigate vicarious trauma and maintain professional well-being.
- Cultural Sensitivity and Competency: Understanding and adapting intervention strategies to meet the diverse cultural and linguistic needs of clients.
Next Steps
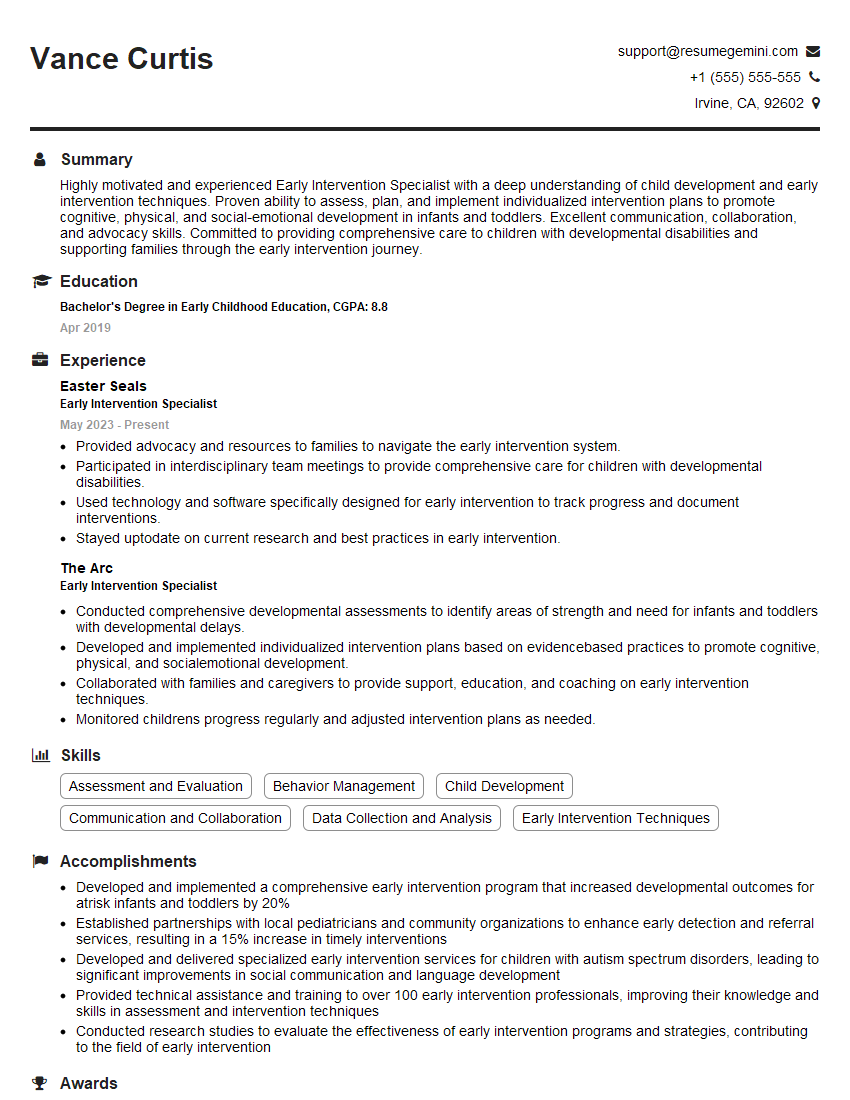
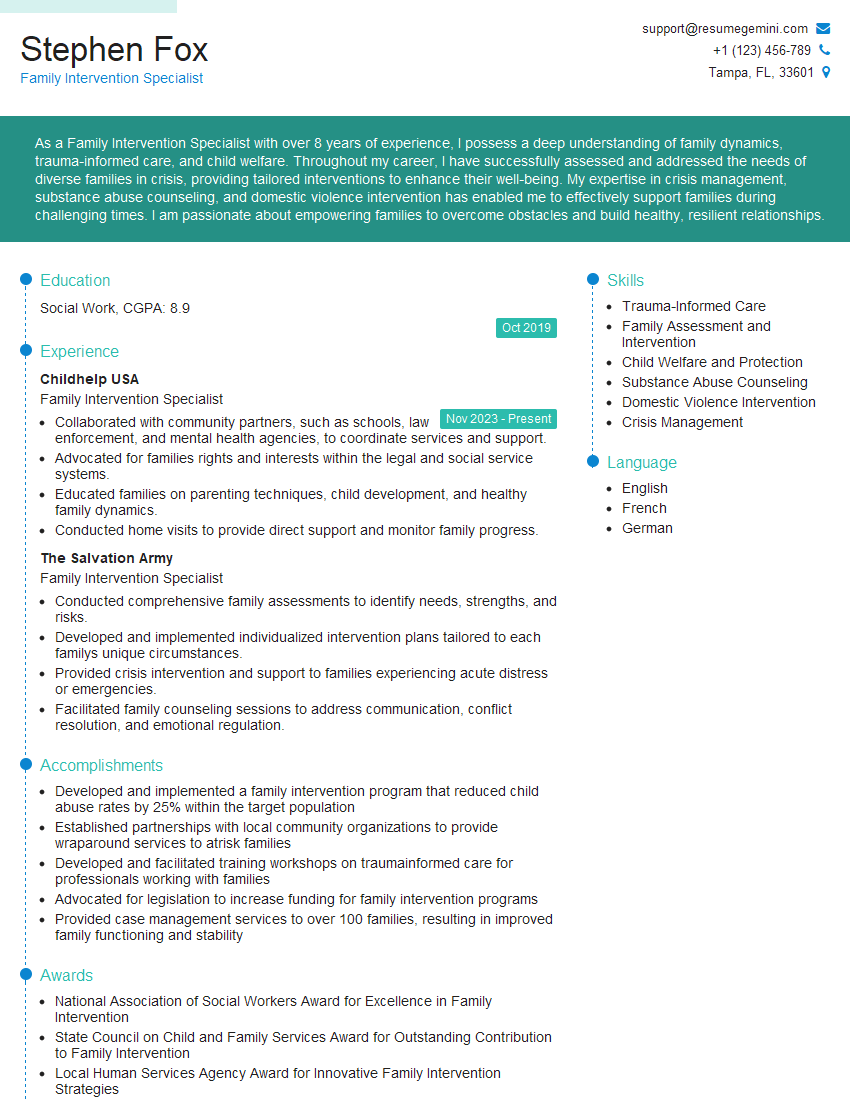
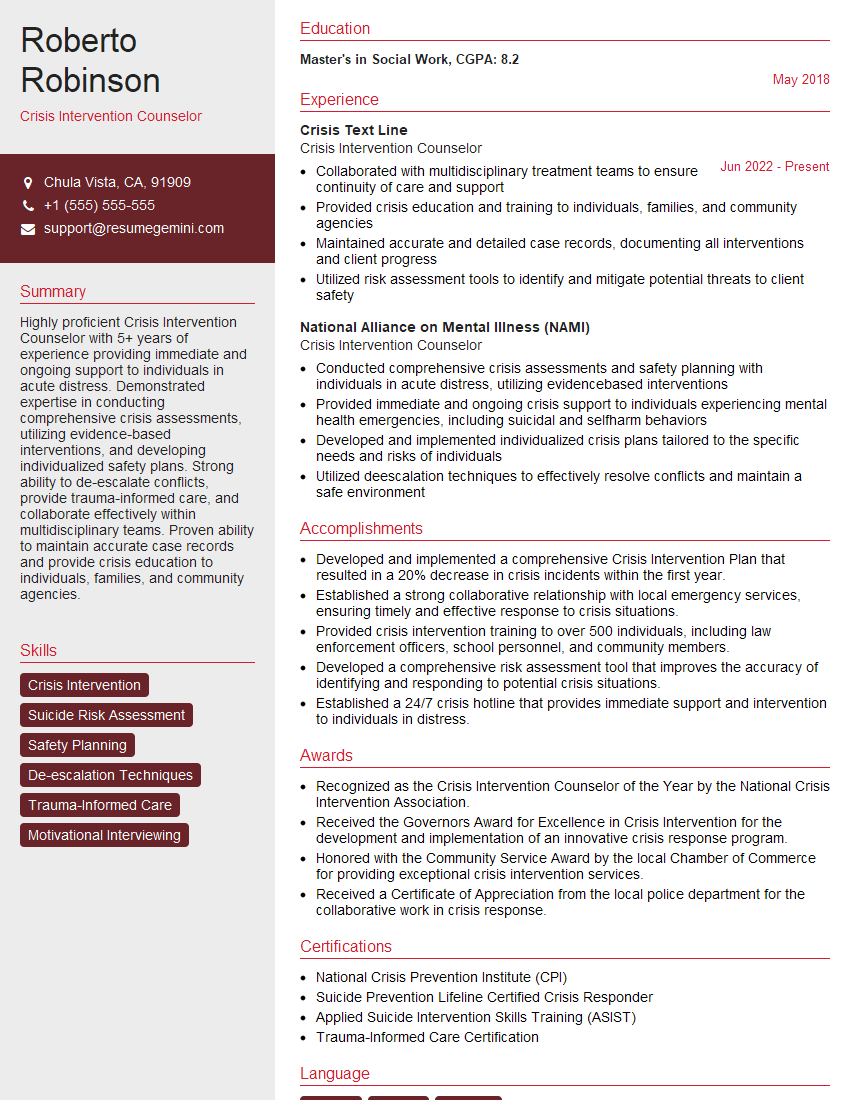
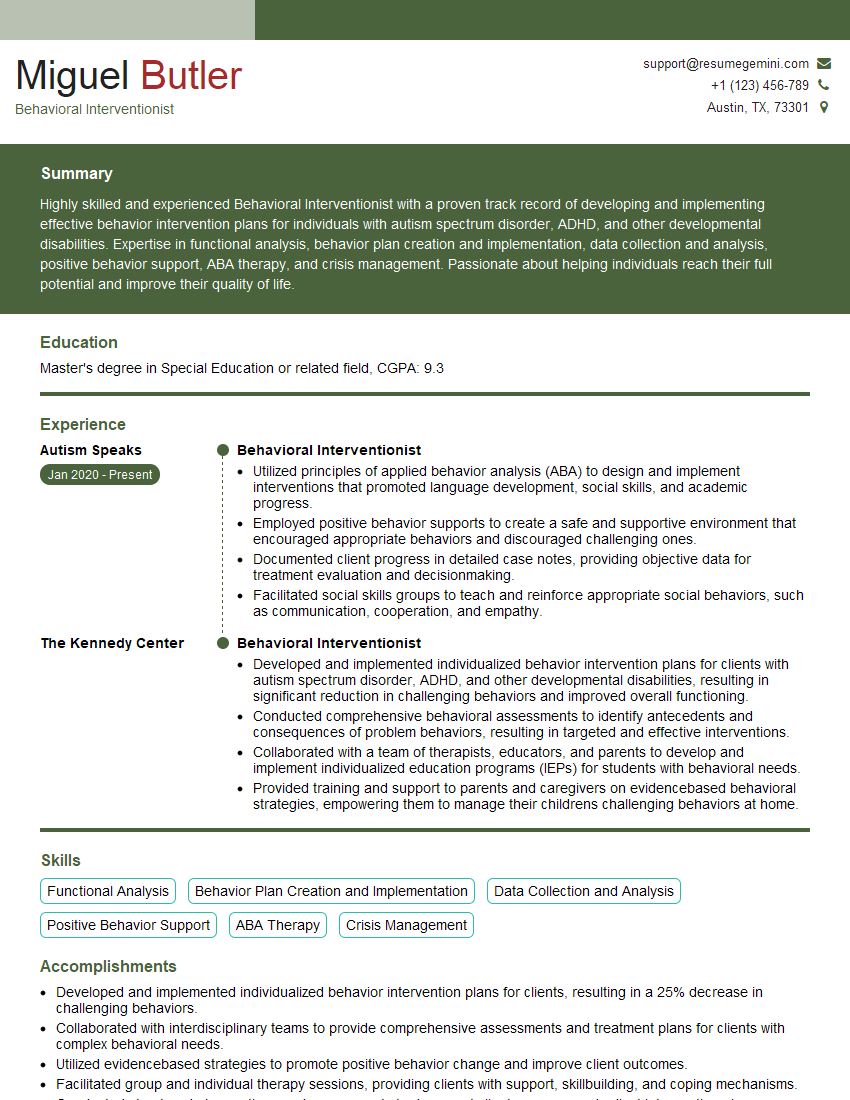
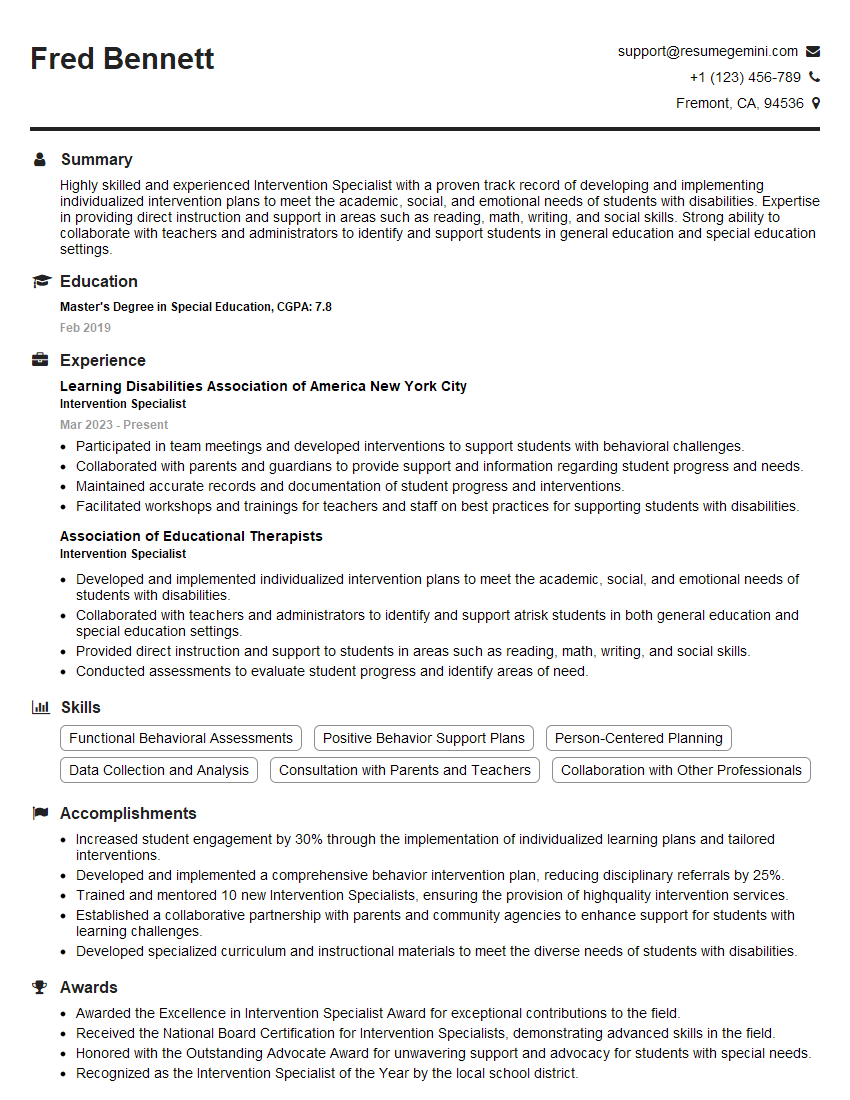
Mastering Intervention Techniques is crucial for career advancement in fields requiring crisis management and client support. A strong understanding of these techniques demonstrates competence and commitment, opening doors to exciting opportunities and leadership roles. To enhance your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to Intervention Techniques to guide you through the process. Invest in your future; craft a resume that showcases your expertise and lands you your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good