Cracking a skill-specific interview, like one for Medical Care on Board, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Medical Care on Board Interview
Q 1. Describe your experience managing medical emergencies at sea.
Managing medical emergencies at sea requires rapid assessment, decisive action, and resourcefulness. My experience spans several years working on various vessels, from cruise ships to cargo carriers. I’ve handled a range of emergencies, including cardiac arrests, severe trauma from accidents, acute appendicitis, and severe allergic reactions. Each situation demanded a different approach, but the core principles remained consistent: prioritization of immediate life threats using the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure), stabilization of the patient using available resources, and prompt communication with onshore medical professionals via satellite communication or HF radio. For example, during a severe storm, a crew member suffered a head injury. I immediately secured the airway, controlled bleeding, and immobilized the injury before contacting a medical evacuation team. The successful outcome was a result of prompt action and effective communication.
One key aspect is recognizing the limitations of the onboard medical facilities and acting swiftly to get the patient to definitive care. Timely communication with shore-based medical professionals is critical, including detailed patient history and current clinical findings.
Q 2. What is your familiarity with the International Maritime Organisation (IMO) Medical First Aid Guidelines?
I am thoroughly familiar with the International Maritime Organisation (IMO) Medical First Aid Guidelines. These guidelines provide a comprehensive framework for medical care onboard ships, covering everything from prevention and basic first aid to emergency response and the management of common illnesses and injuries. My training includes extensive study of these guidelines, emphasizing their practical application in diverse maritime settings. I regularly review and update my knowledge to stay abreast of any changes or revisions to the IMO guidelines. I particularly appreciate the detailed protocols for the treatment of specific medical conditions, which significantly aid in decision-making during critical situations.
These guidelines serve as a fundamental cornerstone of my practice. My adherence to them ensures a consistent and standardized approach to medical care, regardless of the specific ship or situation. They are not simply a checklist, but a philosophy of prioritizing safety and efficacy in a challenging environment.
Q 3. Explain your approach to diagnosing and treating common illnesses and injuries in a remote environment.
Diagnosing and treating illnesses and injuries in a remote environment requires a systematic approach. It starts with a thorough history-taking, focusing on the onset, duration, and nature of symptoms. A detailed physical examination follows, guided by the patient’s complaint. While advanced diagnostic tools are limited, I utilize focused history-taking and physical examination techniques to arrive at a presumptive diagnosis. For example, a patient presenting with sudden onset of chest pain, shortness of breath, and diaphoresis would raise suspicion for acute coronary syndrome. Further examination would focus on evaluating the cardiovascular system, and potentially administering life-saving treatments such as oxygen and nitroglycerin while awaiting medical evacuation.
- History: Detailed information about the patient’s symptoms and medical background.
- Physical Examination: Comprehensive assessment to detect abnormalities.
- Differential Diagnosis: Considering various possibilities before settling on a diagnosis.
- Treatment: Applying appropriate medical interventions based on the diagnosis and available resources.
- Monitoring: Close observation of the patient’s response to treatment and any changes in condition.
Treatment is always tailored to the resources available onboard. Simple analgesics, anti-emetics, and antibiotics for common infections are usually available. However, managing complex cases requires careful decision-making, prioritization of immediate life-saving interventions, and timely communication with onshore medical experts.
Q 4. How do you handle limited medical resources and equipment onboard?
Resourcefulness is paramount in managing limited medical resources. Effective inventory management is essential, ensuring that medications are properly stored, rotated according to expiry dates, and used judiciously. I regularly perform stock checks and reorder supplies to maintain adequate reserves. Prioritization of medical needs is key; critical supplies are given precedence, and less urgent needs are addressed as resources allow. Creative problem-solving is often needed – for instance, adapting existing equipment for different purposes or using readily available materials for improvising medical aids.
For instance, I once had to manage a laceration with limited supplies. By meticulously cleaning the wound and utilizing appropriate sterile dressings, and carefully monitoring for infection, I was able to manage the injury effectively until medical evacuation could be arranged.
Q 5. What is your experience with telemedicine and its application in maritime settings?
Telemedicine plays a crucial role in enhancing the quality of medical care in maritime settings. My experience involves utilizing satellite communication systems to consult with onshore medical specialists regarding complex cases. This allows for real-time expert advice, guiding diagnoses and treatments beyond my onboard capabilities. For example, during an incident involving a severe allergic reaction, a telemedicine consultation allowed me to obtain immediate guidance on the appropriate dose and administration of epinephrine, ultimately saving the patient’s life.
Telemedicine relies heavily on secure communication channels and clear transmission of patient information, including images and vital signs. Accurate and detailed descriptions of symptoms and clinical findings are essential to ensure effective remote consultations. Successful telemedicine necessitates a well-equipped vessel with reliable communication systems.
Q 6. Describe your protocol for documenting medical events and patient information onboard.
Maintaining meticulous documentation is vital for both legal and medical reasons. My protocol involves creating a detailed medical record for each patient, including a comprehensive history, physical examination findings, diagnostic tests performed, treatment administered, and patient response. All entries are dated and signed. This documentation serves as a legal record of the medical care provided, and also ensures continuity of care should the patient be transferred to another medical facility. I use standardized forms adapted from international best practices to maintain consistency.
This documentation is essential for tracking treatment effectiveness, identifying trends, and improving future medical care onboard. It aids in making informed decisions during subsequent medical emergencies. In the event of a litigation, such thorough and accurate records are indispensable.
Q 7. How do you maintain medical supplies and equipment onboard to ensure readiness?
Maintaining medical supplies and equipment requires a proactive approach. Regular inventory checks, including expiration date monitoring, ensure the availability of necessary medications and equipment. Equipment is regularly inspected for functionality and calibrated as needed. Emergency supplies are kept separate and readily accessible. A comprehensive maintenance schedule is followed, with detailed records kept for each item. This includes both preventative maintenance and reactive repairs or replacements.
In addition to regular checks, I conduct training sessions for the crew on basic first aid and the use of onboard medical equipment. This ensures that in case of an emergency, there are individuals who can provide immediate assistance until I arrive on the scene.
Q 8. Explain your approach to infection control and prevention in a confined space.
Infection control in a confined space like a ship requires a multi-pronged approach emphasizing strict adherence to hygiene protocols and proactive measures. Think of it like building a fortress against invaders – we’re protecting against the spread of illness.
- Hand Hygiene: Frequent handwashing with soap and water or alcohol-based sanitizer is paramount. We implement rigorous hand hygiene protocols after every patient interaction, before and after donning gloves, and after any contact with potentially contaminated surfaces.
- Personal Protective Equipment (PPE): Appropriate PPE, including gloves, gowns, masks, and eye protection, is crucial when dealing with potentially infectious patients or bodily fluids. We follow strict guidelines on PPE usage and disposal.
- Environmental Cleaning and Disinfection: Regular and thorough cleaning and disinfection of high-touch surfaces – door handles, railings, medical equipment – using hospital-grade disinfectants is essential. We establish a clear schedule and ensure meticulous cleaning of the medical bay and patient areas.
- Waste Management: Proper segregation and disposal of medical waste, including sharps and contaminated materials, is critical to prevent cross-contamination. We utilize color-coded bins and follow strict protocols for waste removal.
- Isolation Procedures: We have designated isolation facilities and protocols for managing patients with suspected or confirmed infectious diseases to prevent spread within the ship. This includes strict visitor restrictions and specialized cleaning procedures.
- Vaccination and Prophylaxis: We encourage crew and passengers to get the recommended vaccinations and provide prophylactic medications where necessary (e.g., antimalarials in relevant regions).
For example, during a recent outbreak of norovirus on a cruise ship, our rapid implementation of enhanced cleaning protocols, hand hygiene reinforcement, and isolation procedures significantly limited the spread of the infection.
Q 9. How do you manage patients with chronic illnesses during long voyages?
Managing patients with chronic illnesses during long voyages requires meticulous planning and proactive care. It’s similar to managing a complex orchestra – each instrument (patient) needs careful attention to maintain harmony (health).
- Comprehensive Medical History: A detailed medical history of each patient is crucial, including current medications, allergies, and any recent or past health concerns. This allows us to anticipate potential problems.
- Medication Management: We ensure patients have sufficient medication for the entire voyage, with contingency plans for refills or emergencies. Accurate tracking and administration are paramount.
- Regular Monitoring: Regular check-ups and monitoring of vital signs are necessary to detect any deterioration in the patient’s condition early on. We adapt the frequency of monitoring based on the severity of the illness.
- Patient Education: We educate patients about their condition, medication, and potential complications, empowering them to actively participate in their care. This fosters compliance and helps identify problems early.
- Telemedicine: In complex cases, we utilize telemedicine to consult specialists ashore for remote diagnosis and treatment advice. This allows us to access expert opinions even in remote locations.
For instance, I once managed a diabetic patient on a three-month voyage. Through careful monitoring of blood glucose levels, meticulous medication management, and regular communication with the patient, we successfully prevented any major complications throughout the journey.
Q 10. Describe your experience with mental health care in a maritime environment.
Mental health care in a maritime environment is particularly challenging, requiring sensitivity, understanding, and specialized skills. The isolation and confinement can exacerbate pre-existing conditions or trigger new ones. Imagine a pressure cooker – the confined space can amplify stress and tension.
- Early Identification: We actively look for signs of mental distress, such as changes in behavior, sleep disturbances, or expressions of anxiety or depression. Proactive identification is key.
- Confidentiality and Support: Creating a safe and confidential environment for individuals to discuss their concerns is essential. We offer empathy and provide supportive listening.
- Therapeutic Interventions: Depending on the severity, interventions can range from supportive counseling and stress management techniques to medication management (if medically necessary and in consultation with onshore specialists).
- Collaboration: We work closely with onshore mental health professionals via telemedicine when necessary to provide specialist care.
- Promoting Mental Well-being: We organize recreational activities, provide access to mental health resources, and promote stress-reduction techniques like mindfulness and relaxation exercises to improve overall crew well-being.
For example, I have successfully helped crew members experiencing anxiety related to sea sickness or isolation through a combination of counseling, relaxation techniques and medication, ensuring they could continue their duties safely and effectively.
Q 11. How do you ensure the confidentiality and privacy of patient information onboard?
Maintaining confidentiality and privacy of patient information onboard is paramount and ethically crucial. It’s like guarding a precious treasure – the patient’s trust must be earned and protected.
- HIPAA Compliance (or equivalent): We adhere to strict data privacy regulations, similar to HIPAA in the US, to protect patient information. This includes secure storage of medical records, restricted access to patient data, and appropriate disposal of medical records.
- Secure Data Management: Electronic health records are stored on secure servers with access controls to prevent unauthorized access. Paper records are kept in locked cabinets.
- Limited Access: Access to patient information is restricted to authorized medical personnel only. We do not share information unnecessarily.
- Patient Consent: We always obtain informed consent from patients before sharing their information with anyone, even with other crew members, except in emergency situations where consent is implied by the circumstances.
- Data Breach Protocols: We have protocols in place for managing potential data breaches and reporting them to relevant authorities.
We make sure every aspect of patient information handling adheres to the highest standards of confidentiality. For example, we use encrypted communication channels when discussing patient information with onshore specialists via telemedicine.
Q 12. How do you handle situations requiring medical evacuation?
Medical evacuations are critical situations requiring swift and decisive action. It’s a race against time – coordinating a complex operation to get a patient to appropriate care.
- Assessment and Stabilization: The first step is a thorough assessment of the patient’s condition to determine the urgency of evacuation and necessary stabilization measures. We prioritize life-saving interventions.
- Contacting Medical Assistance: We contact onshore medical facilities and air or maritime evacuation services to coordinate the transfer, considering weather conditions and distance to the nearest appropriate medical facility.
- Documentation: Thorough documentation of the patient’s condition, treatment administered, and the evacuation process is essential for continuity of care.
- Handoff: We ensure a smooth handover of the patient to the receiving medical team, including a complete medical history and ongoing treatment plan. Clear communication is vital.
- Emergency Preparedness: Regular drills and training are crucial to ensure a smooth and effective evacuation process. We also maintain a detailed emergency plan with contact information for relevant authorities.
For example, during a recent incident involving a crew member suffering a severe heart attack, we swiftly coordinated a medevac helicopter transfer, stabilizing the patient in transit, leading to a successful outcome.
Q 13. What is your experience with water-related injuries and illnesses?
Water-related injuries and illnesses are common in a maritime environment and require specialized knowledge and prompt action. Think of it as being a marine life first responder.
- Drowning: Immediate CPR and advanced life support techniques are crucial in cases of drowning. We are trained in these procedures.
- Marine Stings and Bites: Management of jellyfish stings, sea urchin punctures, or shark bites requires specific treatments, including pain management, wound care, and antivenom if necessary.
- Dehydration and Heat Exhaustion: Prolonged exposure to sun and water can lead to dehydration and heat exhaustion. We emphasize preventative measures such as hydration and appropriate clothing and address these conditions promptly.
- Seasickness: Managing seasickness through medication and supportive care is important for patient comfort and preventing dehydration.
- Infections from Contaminated Water: We are aware of the risks of infections from contaminated water, so we always emphasize safe water practices and treat infections promptly.
I once had to manage a case of severe jellyfish stings; my knowledge of appropriate first aid, antivenom administration, and wound care helped prevent serious complications.
Q 14. How do you adapt your medical care to diverse cultural backgrounds of patients onboard?
Adapting medical care to diverse cultural backgrounds requires cultural sensitivity and understanding. It’s about recognizing that healthcare is deeply personal and culturally shaped.
- Cultural Awareness Training: We receive training to enhance cultural awareness and sensitivity, helping us to understand diverse beliefs and practices regarding health and illness.
- Communication: Effective communication is essential, and we utilize translators or communication aids when necessary. Non-verbal cues are also carefully observed.
- Dietary Considerations: We consider dietary restrictions and preferences based on patients’ cultural backgrounds to ensure adequate nutrition.
- Religious and Spiritual Beliefs: We respect patients’ religious and spiritual beliefs and accommodate their practices whenever possible, for example, providing prayer space or respecting dietary restrictions.
- Family Involvement: We actively involve family members in decision-making, respecting their cultural roles and values.
For example, while treating a patient from a culture where family involvement in healthcare decisions is central, I involved the family members in every step of the decision-making process which fostered trust and improved the outcome.
Q 15. Explain your understanding of the legal and ethical considerations of medical practice at sea.
Medical practice at sea operates within a unique legal and ethical framework. It’s governed by a blend of international maritime law, the flag state’s laws (the country where the vessel is registered), and the principles of medical ethics. Legally, the ship’s master holds ultimate authority, but their decisions must align with established medical practice and ethical standards. Ethical considerations are paramount, particularly around informed consent, patient confidentiality (challenging in a shared environment), and resource allocation in crisis situations. For example, a doctor might face a difficult decision regarding triage in a mass casualty incident, needing to prioritize care based on likelihood of survival and available resources, a scenario governed by both legal precedence and ethical principles like utilitarianism and beneficence.
Furthermore, the limitations of onboard medical facilities and the remoteness of the location necessitate a greater reliance on telemedicine and pre-emptive risk mitigation strategies. The legal responsibilities of the onboard medical professional extend to documenting all medical interventions meticulously, as these records may become crucial in potential legal proceedings. International conventions, like the STCW (Standards of Training, Certification and Watchkeeping for Seafarers) convention, play a significant role in defining the legal and professional expectations for medical care at sea.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your familiarity with maritime regulations concerning medical care.
My familiarity with maritime regulations concerning medical care is extensive. I’m thoroughly versed in the International Maritime Organization (IMO) guidelines, specifically the Medical First Aid Guide for Ships, which outlines minimum medical requirements for various vessel types. This includes understanding the mandatory medical equipment lists, crew health assessment procedures, and the reporting requirements for illnesses and injuries. I’m also aware of the regulations concerning the carriage of medical supplies and the documentation needed for their use. The flag state’s specific regulations often dictate additional compliance necessities, and I ensure all practice adheres to those standards. For instance, I am adept at interpreting and applying the requirements for maintaining accurate medical records, adhering to the privacy regulations for patients’ health information, and reporting significant medical events as mandated by relevant authorities.
Q 17. How do you manage challenging situations involving limited communication or language barriers?
Communication barriers are a significant challenge in medical care at sea. I have extensive experience in managing these situations. My approach involves using visual aids (pictures, diagrams), employing translation apps and seeking assistance from multilingual crew members whenever possible. I prioritize non-verbal communication, focusing on observing patient behavior and using gestures to understand their needs. I also rely heavily on universal medical symbols and standardized medical terminology. For instance, I utilize the widely accepted visual communication system for assessing pain levels. If necessary, I attempt to contact onshore medical professionals who might have language skills relevant to the situation for a remote consultation, leveraging technology to bridge the communication gap.
In cases of severe language barriers, I would prioritize actions that address the most immediate and life-threatening needs, focusing on stabilization until more effective communication can be established. The importance of clear, concise, and culturally sensitive communication is critical throughout, emphasizing building trust with patients to encourage their cooperation and minimize misunderstandings.
Q 18. What is your experience with administering medications and performing medical procedures in a resource-constrained setting?
My experience in administering medications and performing procedures in resource-constrained settings is considerable. Onboard, I regularly manage medications with limited storage and monitoring capabilities, ensuring proper dosages and adhering to strict protocols for handling and disposal. I’ve conducted procedures with basic equipment, often relying on improvisation and creativity. For example, I’ve adapted standard medical techniques to use available resources for wound care and minor surgical interventions. The challenge lies in prioritizing interventions based on the urgency of the condition and the available resources. This involves making critical judgments about what treatment is essential and what can wait until reaching port. Documentation is key to maintaining transparency and accountability in these situations.
Q 19. How do you ensure the safety and well-being of both patients and crew in emergency situations?
Ensuring the safety and well-being of patients and crew in emergencies is paramount. This involves a multi-faceted approach: First, having a comprehensive emergency plan is essential, including clear protocols for communication, evacuation, and triage. This plan is regularly reviewed and practiced with crew members. Second, maintaining a well-stocked medical kit and having proficiency with all available equipment are critical. Third, establishing clear communication channels with shore-based medical assistance is vital, enabling remote guidance and coordinated emergency medical services (EMS) if needed. Fourth, effective teamwork is essential. I train the crew in basic first aid, enabling them to provide immediate assistance while awaiting professional medical attention. Finally, proactive risk management, identifying and mitigating potential hazards before they lead to emergencies, is crucial to preventing accidents and health issues altogether.
Q 20. Describe a time you had to make a difficult medical decision onboard; what was the outcome?
During a transatlantic voyage, a crew member suffered a severe allergic reaction to an unknown substance. The reaction was progressing rapidly, and we had limited resources. I had to make a quick decision to administer epinephrine (adrenaline), even without a clear identification of the allergen. The decision was based on the severity of the symptoms, which indicated a life-threatening anaphylactic shock. Documenting every step of the intervention was critical. Fortunately, the epinephrine was effective, stabilizing the patient’s condition. Post-incident, a thorough investigation was conducted to determine the allergen, and the crew’s training on recognizing and responding to allergic reactions was enhanced. This experience highlighted the importance of swift decision-making, resourcefulness, and comprehensive documentation in resource-limited environments.
Q 21. Explain your experience with training crew members in basic first aid and emergency procedures.
Training crew members in basic first aid and emergency procedures is an ongoing responsibility. I regularly conduct training sessions, covering topics such as CPR, basic wound care, recognizing and responding to various medical emergencies (e.g., strokes, heart attacks, seizures), and using the available onboard medical equipment. Practical drills and simulations are incorporated to test their preparedness and build their confidence in handling emergency situations. The training also emphasizes the importance of early recognition of symptoms, effective communication with the onboard medical professional, and maintaining accurate records of any incidents. This ongoing education helps empower the crew to contribute meaningfully to emergency responses and ensures a higher level of preparedness throughout the voyage, thereby enhancing both patient and crew safety.
Q 22. How do you utilize preventative measures to reduce the risk of illness and injury amongst crew?
Preventative measures are crucial in maritime medical care, aiming to proactively minimize health risks for the crew. This involves a multi-pronged approach encompassing education, environmental control, and access to healthcare.
- Health Education: We conduct regular training sessions covering topics like hygiene (handwashing, sanitation), safe working practices (lifting techniques, avoiding slips, trips, and falls), and recognizing early signs of illnesses. For example, we’d teach crew members about the importance of staying hydrated in hot climates to prevent heatstroke.
- Environmental Control: This focuses on maintaining a clean and safe working environment. Regular inspections are conducted to identify and address potential hazards like rodent infestations, inadequate ventilation, and unsafe storage of chemicals. Implementing proper waste disposal methods is also critical.
- Access to Healthcare: This involves ensuring easy access to medical advice and care, promoting regular health checks, and providing readily available first-aid kits and supplies. We also emphasize early reporting of illness or injury to allow for prompt intervention.
A successful preventative program results in fewer illnesses and injuries, boosting crew morale, productivity, and overall vessel efficiency. It also minimizes the need for costly evacuations and medical repatriation.
Q 23. What is your experience with pre-employment health assessments for seafarers?
Pre-employment health assessments are a cornerstone of ensuring a healthy and productive crew. My experience involves conducting thorough examinations, including physical assessments, medical history reviews, and relevant laboratory tests. I’m proficient in interpreting the results to identify any potential health concerns that could impact a seafarer’s ability to perform their duties safely.
For example, I would look for conditions like cardiovascular disease, respiratory problems, or visual impairments that might pose risks at sea. The process goes beyond simply checking boxes; it includes discussions with the seafarers about their lifestyle, work history, and any pre-existing medical conditions. This allows for informed decision-making about seaworthiness and the creation of a tailored plan for ongoing health management. I also ensure that all findings are documented thoroughly and confidentially, adhering to relevant regulations and privacy laws.
Q 24. How familiar are you with the STCW Convention concerning medical care?
I am very familiar with the STCW Convention’s stipulations regarding medical care on board vessels. I understand the requirements for the medical chest contents, the qualifications and training standards for ship’s medical officers and personnel providing first aid, and the procedures for medical emergencies at sea. The convention’s emphasis on a risk-based approach to medical care is something I actively incorporate into my practice.
Specifically, I know the importance of maintaining accurate medical records, conducting regular health checks, and implementing appropriate preventive measures. The convention’s guidelines concerning the reporting and documentation of medical events, particularly serious injuries or illnesses, are paramount in ensuring transparency and the ability to learn from past incidents to improve future practices. Understanding the limitations of onboard medical capabilities and the need for timely communication with shore-based medical support is also critical.
Q 25. Describe your experience with working independently and making quick, accurate decisions under pressure.
Working independently and making critical decisions under pressure is a daily reality in maritime medical care. I’ve had numerous situations requiring immediate action, often with limited resources and time.
For instance, I once had to manage a severe appendicitis case aboard a vessel hundreds of miles from shore. I had to assess the patient, initiate treatment to stabilize their condition, coordinate with a shore-based medical team for guidance, and ultimately, make a decision on the most appropriate course of action (medical evacuation versus continued onboard care). The situation demanded quick thinking, calm judgment, and effective communication. This experience enhanced my ability to stay composed, analyze the situation systematically, and make informed decisions even under immense stress.
Q 26. How would you handle a conflict between a patient’s wishes and medical best practice?
Conflicts between patient wishes and medical best practice are delicate situations requiring careful navigation. My approach involves a patient-centered, empathetic, yet ethically sound framework.
- Open Communication: I would start by engaging in a respectful and open conversation with the patient, actively listening to their concerns, understanding their beliefs, and clarifying their wishes.
- Exploration of Options: I would thoroughly explain the medical best practice, outlining the potential benefits, risks, and alternatives. I’d emphasize the rationale behind the recommended treatment.
- Shared Decision-Making: Where possible, we’d aim for shared decision-making. This involves offering the patient all the available information, assisting them in understanding the potential outcomes, and helping them make a choice that aligns with their values and preferences, while also explaining the potential implications of their decision.
- Documentation: Regardless of the decision, detailed documentation of the conversation, the patient’s preferences, the medical advice provided, and any agreed-upon course of action is crucial. This protects both the patient and the medical provider.
If the patient’s wishes are unsafe or contravene fundamental ethical guidelines, I would seek advice from shore-based medical experts and potentially involve the ship’s master and company representatives to facilitate a responsible decision-making process. The well-being and safety of the patient remain the highest priority, even when their desires differ from established medical practices.
Q 27. What software or medical records management systems are you proficient in?
I am proficient in several medical records management systems, including Meditech, Epic, and Allscripts. My experience extends to using these systems in a variety of settings, ensuring accurate and timely documentation of patient data, including demographics, medical history, diagnoses, treatments, and progress notes. I understand the importance of maintaining patient confidentiality and adhering to data privacy regulations. I am also familiar with electronic health record (EHR) systems commonly used in telemedicine, enabling efficient communication and information sharing with shore-based medical teams.
Q 28. How do you stay up-to-date with the latest medical advancements and guidelines relevant to maritime medical practice?
Staying current with medical advancements is vital in maritime medicine. I utilize several strategies to keep my knowledge up-to-date.
- Professional Journals and Publications: I regularly read peer-reviewed journals like the Journal of Travel Medicine and the Maritime Medicine to stay informed on the latest research, guidelines, and best practices in maritime health.
- Online Resources and Continuing Medical Education (CME): I actively participate in online courses and webinars offered by organizations like the International Maritime Health Association (IMHA) to earn CME credits and enhance my skills.
- Conferences and Workshops: Attending relevant conferences and workshops allows for networking with other professionals and learning about the latest innovations and challenges in the field. This also provides opportunities for case study discussions and valuable peer learning.
- Professional Networks: Maintaining connections with other maritime medical professionals through online forums and professional organizations helps to disseminate information and facilitates discussion of important issues.
This multi-faceted approach ensures I’m equipped with the most up-to-date knowledge to provide effective and high-quality medical care aboard vessels.
Key Topics to Learn for Medical Care on Board Interview
- Emergency Medical Care: Understanding triage protocols, managing trauma, and providing basic life support (BLS) in a maritime environment. Consider practical applications like responding to different types of injuries at sea and the limitations of onboard resources.
- Pharmacology and Medication Management: Knowledge of common medications used onboard, their dosages, side effects, and interactions. Explore practical scenarios such as managing a patient with a pre-existing condition or dispensing medication in emergency situations.
- Disease Prevention and Hygiene: Understanding sanitation procedures, infection control, and the prevention of common illnesses in a confined space. Consider how to educate crew members about hygiene practices and the importance of disease prevention.
- Medical Record Keeping and Documentation: Properly maintaining patient records, following legal and regulatory guidelines for medical documentation onboard vessels. Consider the specific requirements for reporting injuries and illnesses.
- Communication and Teamwork: Effective communication with patients, crew members, and onshore medical professionals. Explore scenarios involving coordinating medical evacuations and collaborating with other healthcare providers remotely.
- Medical Equipment and Supplies: Familiarity with common medical equipment used onboard, including their operation, maintenance, and limitations. Consider troubleshooting scenarios and understanding the importance of regular equipment checks.
- Legal and Ethical Considerations: Understanding medical confidentiality, informed consent, and the legal responsibilities of onboard medical personnel. Consider ethical dilemmas that may arise in a maritime setting.
Next Steps
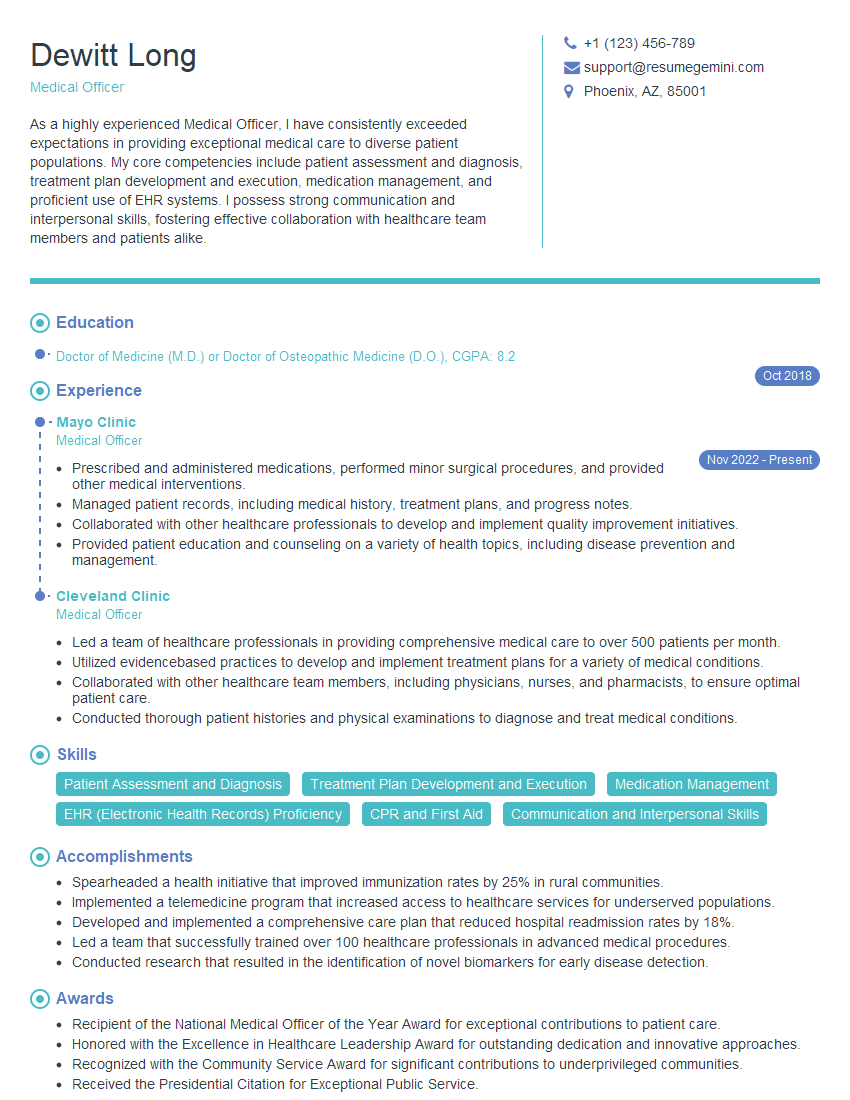
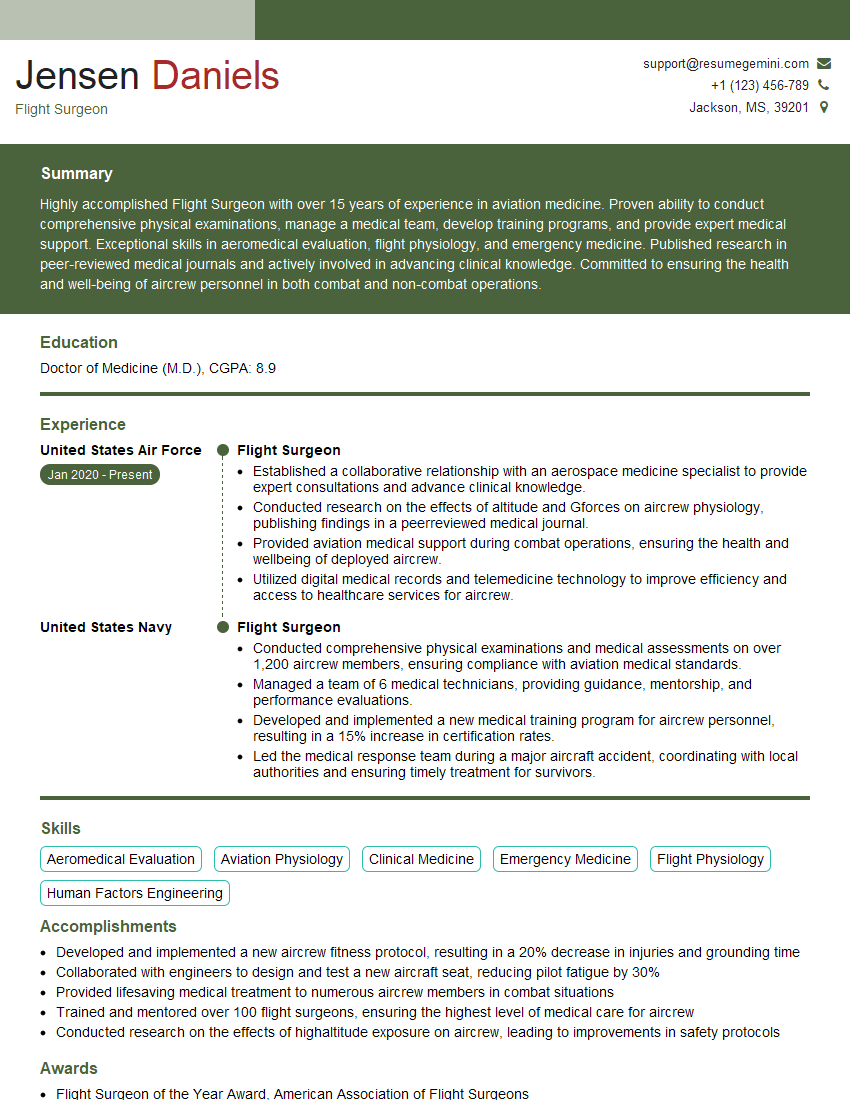
Mastering Medical Care on Board significantly enhances your career prospects in the maritime industry, opening doors to rewarding positions with increased responsibility and compensation. To make the most of your job search, focus on crafting an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource that can help you build a professional resume that stands out. ResumeGemini provides examples of resumes tailored to Medical Care on Board roles, making the process easier and more efficient. Invest time in creating a strong resume; it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good