Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Medical Device Manufacturing Automation interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Medical Device Manufacturing Automation Interview
Q 1. Explain your experience with PLC programming in a medical device manufacturing environment.
PLC programming is the cornerstone of automation in medical device manufacturing. I have extensive experience using various PLC platforms, primarily Allen-Bradley and Siemens, to control automated assembly lines, robotic arms, and individual machine processes. My expertise encompasses developing and debugging ladder logic programs, implementing motion control routines, and integrating PLC systems with HMI (Human Machine Interface) software for real-time monitoring and control. For example, I once developed a PLC program to control a high-speed automated assembly line for disposable syringes, ensuring precise dispensing and assembly of components while maintaining strict quality control parameters. This involved intricate timing sequences and error-handling routines to guarantee sterility and product integrity. Another project involved integrating a vision system with the PLC to perform quality checks on the finished products, flagging any defects for immediate rejection.
My proficiency extends to implementing safety protocols within the PLC code to mitigate potential hazards in accordance with FDA regulations. This includes emergency stop mechanisms, light curtains for operator safety, and interlocks to prevent unsafe machine states. I’m also experienced in utilizing advanced PLC functionalities such as PID control for precise temperature regulation in processes like welding or bonding.
Q 2. Describe your familiarity with various robotic systems used in medical device assembly.
My experience spans a broad range of robotic systems commonly used in medical device assembly. This includes articulated robots (like those from FANUC, ABB, and KUKA) for tasks such as picking and placing components, SCARA robots for their speed and precision in repetitive assembly operations, and delta robots for high-speed applications. I’ve also worked with collaborative robots (cobots) like Universal Robots, which allow for safe human-robot interaction in manufacturing settings. I understand the nuances of integrating different robot types into a larger automated system, including programming their control systems (often using Robot Operating System or proprietary languages) and coordinating their movements with other automated equipment. For instance, I was involved in a project where we used a KUKA robot to precisely insert delicate micro-components onto a medical implant, requiring extremely fine motor control and vision-guided assembly. In another project, I integrated collaborative robots to assist human operators with tasks like packaging and labeling medical devices, increasing productivity while maintaining quality and safety standards.
Q 3. How do you ensure the validation and verification of automated processes in medical device manufacturing?
Validation and verification are paramount in medical device manufacturing, ensuring the automated processes consistently meet predefined quality standards and regulatory requirements. Verification confirms that the system is built according to the specifications, while validation confirms it performs its intended function correctly and consistently. This often involves a multi-stage process. First, a Design Qualification (DQ) phase establishes that the system design meets its intended use and complies with regulatory standards (e.g., ISO 13485, FDA 21 CFR Part 820). Then, Installation Qualification (IQ) verifies that the system is installed correctly and complies with documented requirements. Next is Operational Qualification (OQ), testing the system’s performance under varying conditions to demonstrate it functions as intended. Finally, Performance Qualification (PQ) provides evidence of consistent performance over time by testing it under real-world production conditions. This process rigorously documents all testing procedures, results, and deviations, leaving an auditable trail for regulatory compliance. Throughout these stages, risk assessments are integral to identify and mitigate potential risks, ensuring patient safety.
Q 4. What are the key considerations for integrating automation into a cleanroom environment?
Integrating automation into a cleanroom demands careful consideration of several factors critical for maintaining a sterile environment. This includes selecting equipment with appropriate cleanroom classifications (ISO Class 5 or better typically), employing materials resistant to cleaning and sterilization procedures (stainless steel, epoxy-coated surfaces), and ensuring all automated systems are designed to minimize particle generation and shedding. It’s also crucial to use appropriate sealing and filtration systems in the automated equipment to prevent contamination. Regular cleanroom validation is also essential to ensure the automation hasn’t compromised the sterility of the environment. For example, the choice of lubricants for moving parts must be considered to ensure they are compatible with the cleanroom environment and don’t release particles. Furthermore, any robotic or automated system should be designed for easy cleaning and disinfection. This might involve incorporating features like sealed housings, easily accessible components, and the use of materials that can withstand cleaning agents.
Q 5. Explain your experience with different types of sensors used in automated medical device production.
A wide array of sensors are crucial in automated medical device production for precise control, monitoring, and quality assurance. These include:
- Vision Systems: Used for inspecting components, verifying assembly, and identifying defects. These systems utilize cameras and image processing software to ensure dimensional accuracy and product quality.
- Proximity Sensors: Detect the presence or absence of objects, often used for safety interlocks and preventing collisions in automated systems.
- Force/Torque Sensors: Measure the force applied during assembly operations, ensuring components are inserted correctly without damage.
- Laser Sensors: Used for precise distance measurement and alignment, particularly important in high-precision assembly tasks.
- Temperature Sensors: Monitor process parameters such as temperature during welding, bonding, or sterilization.
The selection of specific sensor types depends on the application. For instance, in the assembly of a micro-catheter, vision systems with high resolution would be crucial for verifying the proper assembly of intricate components, while force/torque sensors would ensure delicate parts aren’t damaged during insertion.
Q 6. How do you troubleshoot issues in automated medical device production lines?
Troubleshooting automated medical device production lines requires a systematic approach. It begins with understanding the nature of the issue: Is it a mechanical problem, a software glitch, or a sensor malfunction? I typically start by reviewing the system’s logs and HMI data to identify error codes and potential causes. This might involve checking for sensor failures, reviewing PLC program execution sequences, or examining the status of robotic arm movements. I’ll use diagnostic tools specific to the PLC and robotic systems to pinpoint the problem’s origin. This often involves testing individual components – for example, verifying sensor outputs, checking for air pressure leaks in pneumatic systems, or evaluating the integrity of electrical connections. Once the faulty component or software section is identified, I implement the appropriate corrective action, whether it’s replacing a faulty sensor, adjusting PLC program parameters, or fixing a software bug. After rectifying the issue, I thoroughly test the system to confirm the problem is resolved and doesn’t lead to further issues. Thorough documentation of troubleshooting steps is vital for maintaining a history of system performance and streamlining future maintenance and problem resolution.
Q 7. Describe your experience with designing and implementing automated assembly processes.
Designing and implementing automated assembly processes involves a multi-step approach starting with a thorough understanding of the product’s design and manufacturing requirements. This includes analyzing the assembly steps, identifying critical process parameters, and defining the desired level of automation. I then select appropriate automation technologies, which could involve designing custom fixtures, integrating robotic systems, implementing vision systems for quality control, and integrating PLCs for overall system control. The design phase incorporates principles of lean manufacturing to minimize waste and maximize efficiency. This involves optimizing the layout of the assembly line, minimizing material handling, and implementing strategies like just-in-time delivery of components. Careful consideration is given to safety aspects, including emergency stop systems, light curtains, and other protective measures in compliance with industry standards. Throughout the project, simulations and virtual models are used to test the design before actual implementation, minimizing risks and ensuring a smooth transition to full-scale production. For example, in a recent project, I designed an automated assembly line for implantable drug delivery systems. This included custom-designed fixtures for holding delicate components, robotic arms for precise insertion and assembly, and a vision system for verifying the proper placement of components. The implementation involved a phased approach, starting with testing individual components, followed by testing the integrated system before full-scale production.
Q 8. Explain your understanding of different automation architectures (e.g., centralized vs. decentralized).
Automation architectures in medical device manufacturing can be broadly classified into centralized and decentralized systems. Think of it like this: a centralized system is like a single, powerful brain controlling the entire factory floor, while a decentralized system is more like a network of independent, collaborating robots, each responsible for a specific task.
Centralized Architecture: In this model, a central control system manages all aspects of the manufacturing process. This usually involves a Programmable Logic Controller (PLC) or a supervisory control and data acquisition (SCADA) system that orchestrates the actions of all machines and processes. This offers greater control and centralized monitoring, but a single point of failure could bring the whole production line to a halt. Imagine a large, complex heart controlling the entire body; if it fails, everything suffers.
Decentralized Architecture: Here, individual machines or cells have their own controllers, communicating with each other over a network. This is much more fault-tolerant; if one component fails, the rest can continue operating. It’s more flexible, allowing for easier expansion and modification. Think of it as a team of specialists, each contributing to the overall goal independently but cooperating effectively through communication.
Hybrid Architectures: It’s common to find hybrid systems blending aspects of both approaches. For example, a large assembly line might employ a decentralized architecture for individual workstations, coordinated by a central system managing overall production flow and material handling. The best approach depends on factors like production scale, complexity, and required flexibility.
Q 9. How do you ensure the safety of automated systems in medical device manufacturing?
Ensuring safety in automated medical device manufacturing is paramount, as any failure could have dire consequences. This requires a multi-layered approach, combining hardware, software, and procedural safeguards. Think of it as building a fortress, with multiple defensive layers protecting the most valuable assets.
- Redundancy and Fail-safes: Critical systems must have backups. If a robot arm malfunctions, a secondary system should take over, or the process should automatically halt. We use dual-channel sensors, emergency stops, and fail-safe relays to achieve this.
- Safety Instrumented Systems (SIS): These systems are designed to detect and respond to hazardous situations. They are independently verified and validated to ensure their reliability. Examples include emergency shut-down circuits and pressure relief valves.
- Risk Assessments and HAZOP Studies: We perform rigorous risk assessments to identify potential hazards and vulnerabilities within the automated system. HAZOP (Hazard and Operability) studies help analyze every step to identify and mitigate potential problems before they occur.
- Validation and Verification: Automated systems undergo rigorous validation and verification procedures to ensure they meet stringent safety and performance standards. This includes simulations, testing with representative materials, and performance qualification.
- Operator Training and Procedures: Operators receive thorough training on safe operation, emergency procedures, and system limitations. Clear safety protocols are crucial to minimize human error.
- Regular Maintenance and Inspections: Proactive maintenance and inspections are critical for preventing malfunctions and maintaining safety. This involves regular inspections, lubrication, and calibration of equipment.
Compliance with relevant safety standards (e.g., ISO 13485, FDA regulations) is fundamental. Ultimately, safety in automation is not just a checkbox; it’s a continuous process of vigilance, improvement, and meticulous attention to detail.
Q 10. Describe your experience with statistical process control (SPC) in an automated manufacturing setting.
Statistical Process Control (SPC) is crucial in ensuring consistent product quality in automated manufacturing. Think of it as a quality detective, constantly monitoring the production process and alerting us to any deviations from expected behavior. It allows for proactive intervention rather than reacting to problems after they’ve occurred.
In automated settings, SPC is integrated with the machine controls. Data, like measurements from sensors, are automatically collected and analyzed in real-time. Control charts (e.g., X-bar and R charts, CUSUM charts) are generated to visualize the process variation. We set control limits based on historical data and process capability analysis, establishing acceptable ranges. When data points fall outside these limits or show other patterns suggesting a shift in the process mean or increase in variability, this triggers an alert, prompting an investigation to identify and correct root causes. This could involve adjustments to machine parameters, maintenance, or material changes.
For instance, in an automated injection molding process for medical implants, we use SPC to monitor critical dimensions of the implants. If the diameter starts drifting outside the acceptable range, the system would alert us. This would prompt a review of the mold temperature, injection pressure, or material properties. We utilize software packages such as Minitab or JMP for data analysis and to generate reports for quality assurance documentation.
Q 11. What are your experiences with different types of vision systems used in automated inspection?
Vision systems are fundamental in automated inspection, providing ‘eyes’ for the automated line. They enable automated inspection and verification of product quality, ensuring that defects are detected before they reach the customer. The type of vision system chosen depends heavily on the specific application and the required level of detail and speed.
- 2D Vision Systems: These are the most common and relatively inexpensive, suitable for inspecting flat surfaces or objects that can be easily oriented. They work by capturing a 2D image of the object and analyzing it using image processing algorithms to identify features and defects. Examples include inspecting labels for correct alignment or detecting scratches on a surface.
- 3D Vision Systems: These systems capture three-dimensional information about the object, offering more comprehensive inspection capabilities. They’re necessary for complex shapes or situations requiring precise dimensional measurements. Techniques like structured light, laser triangulation, or time-of-flight are used. This can be used to detect imperfections in complex medical implants.
- Multispectral Imaging: Going beyond visible light, multispectral imaging uses multiple wavelengths (e.g., near-infrared, ultraviolet) to capture information not visible to the naked eye, useful for detecting subtle defects or material variations that might be imperceptible to standard 2D or 3D vision systems.
In my experience, we’ve used a combination of these vision systems. For example, 2D systems are used for simple label verification, while 3D vision is essential for inspecting the geometry of complex surgical instruments. The choice of lighting, cameras, and image processing algorithms is crucial to achieving reliable inspection results.
Q 12. How do you manage change control within an automated medical device manufacturing process?
Change control in automated medical device manufacturing is critical to maintain quality, compliance, and regulatory approvals. It’s a systematic process ensuring that changes to the automated system are thoroughly evaluated, approved, and implemented without jeopardizing product quality or safety. Think of it as a well-defined roadmap for any modifications or improvements.
We typically follow a formal change control process involving:
- Change Request: Any proposed change is documented in a formal change request, specifying the rationale, impact, and proposed implementation.
- Impact Assessment: The potential effects of the change on the automated system, product quality, safety, and regulatory compliance are carefully evaluated.
- Risk Assessment: We assess the risks associated with the proposed change and develop mitigation strategies.
- Approval Process: The change request is reviewed and approved by relevant stakeholders, including engineering, quality, and regulatory affairs.
- Implementation: The change is implemented following documented procedures, often including validation and verification steps to ensure the change does not negatively impact product quality.
- Verification and Validation: Post-implementation testing and validation ensure that the change was successfully implemented and has the desired effect without introducing any unintended consequences.
- Documentation: All aspects of the change control process, including the change request, impact assessment, approval, and verification, are meticulously documented.
Software-based change control systems are often employed to manage and track change requests, ensuring traceability and regulatory compliance. In the event of an unexpected event disrupting production, a robust change control process allows us to implement a workaround while maintaining a documented audit trail.
Q 13. Explain your experience with Human-Machine Interface (HMI) design and implementation.
Human-Machine Interface (HMI) design is crucial for effective interaction between operators and automated systems. A well-designed HMI makes the system intuitive, efficient, and safe to operate. Think of it as the friendly face of a powerful machine, facilitating seamless communication.
My experience involves designing and implementing HMIs for various medical device manufacturing systems using industrial PCs and touch screen interfaces. Effective HMI design principles include:
- Intuitive Navigation: Clear and logical menu structures, intuitive icons, and consistent design elements. The operator should be able to easily find the information they need.
- Real-time Data Visualization: Clear graphical displays of key process parameters, production status, and alarms. Effective data visualization allows the operator to quickly understand the state of the system.
- Alarm Management: A well-defined alarm system that alerts the operator to critical events, without generating excessive false alarms. The severity of alerts is clearly indicated.
- User Access Control: Appropriate security measures to prevent unauthorized access and changes to system parameters.
- Error Handling: Clear and informative error messages guiding operators through troubleshooting and corrective actions.
- Ergonomics: The HMI should be designed for optimal viewing distance, screen size, and layout to minimize operator fatigue and errors.
Software platforms such as Ignition or WinCC are commonly used for HMI development. We leverage SCADA systems that allow for centralized monitoring and control of the entire manufacturing process via these interfaces, enabling better overview, troubleshooting, and data acquisition.
Q 14. Describe your familiarity with different types of industrial communication protocols (e.g., Ethernet/IP, Profibus).
Industrial communication protocols are the ‘nervous system’ of automated manufacturing, enabling different machines and systems to communicate and share data. The choice of protocol depends on factors like speed, reliability, distance, and network topology.
- Ethernet/IP: A widely used industrial Ethernet protocol, offering high speed and flexibility, suitable for large, complex networks. It’s commonly used in modern automation systems for real-time communication between PLCs, robots, and other devices.
- Profibus: A fieldbus protocol commonly used in European industrial automation, offering reliable communication over longer distances. It is used for both process automation and discrete manufacturing.
- Profinet: Another Ethernet-based industrial protocol, often used in conjunction with Siemens PLCs. It provides high-speed deterministic communication, which is crucial for applications requiring precise synchronization.
- Modbus: A simpler, widely adopted protocol, particularly suitable for less complex applications requiring less bandwidth.
My experience includes working with a variety of these protocols. In one project, we utilized Ethernet/IP for connecting high-speed robots and vision systems, while Modbus was used for communication with simpler devices like temperature sensors. The integration of these protocols requires careful planning and configuration to ensure seamless data exchange and avoid conflicts. Choosing the right protocol is vital for overall system efficiency and reliability.
Q 15. How do you ensure compliance with regulatory requirements (e.g., FDA, ISO 13485) in automated medical device manufacturing?
Ensuring compliance in automated medical device manufacturing is paramount. It requires a multifaceted approach encompassing design, manufacturing, and quality control. We begin by meticulously documenting every aspect of the automated system, from design specifications to validation protocols, ensuring traceability throughout the entire lifecycle. This documentation serves as a cornerstone for audits and regulatory inspections. Compliance with FDA 21 CFR Part 11 and ISO 13485 is achieved through a rigorous Quality Management System (QMS) that integrates risk management methodologies, such as Failure Mode and Effects Analysis (FMEA) and Hazard Analysis and Risk Control (HARAC), into every stage of the automation process. This allows us to proactively identify and mitigate potential risks to product quality and patient safety.
For example, we implement robust software validation processes to ensure that automated control systems consistently deliver expected results. We also use automated data acquisition and analysis systems to track critical process parameters, providing real-time monitoring and alerting capabilities for deviations from established parameters. Regular audits are conducted to assess the effectiveness of the QMS and ensure ongoing compliance. Failure to comply can result in significant repercussions, including regulatory actions, product recalls, and reputational damage, hence the meticulous approach to documentation and process validation is critical.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your experience with different types of automated material handling systems.
My experience spans a variety of automated material handling systems, each tailored to specific needs within medical device manufacturing. I’ve worked extensively with robotic arms for precision assembly and part placement, ensuring accuracy and repeatability in critical procedures. These robots are programmed using sophisticated software and integrated with vision systems for quality control. I’ve also implemented automated guided vehicles (AGVs) for transporting materials between different production areas, optimizing material flow and reducing lead times. Furthermore, I have experience with conveyor systems, both traditional and those incorporating advanced features such as programmable logic controllers (PLCs) to manage complex routing and sorting operations. Each system is chosen based on a thorough analysis of the specific application’s throughput requirements, precision needs, and overall cost-effectiveness.
For instance, in one project, we integrated a robotic arm with a vision system to accurately pick and place micro-components in a complex assembly process. This not only significantly increased production speed but also reduced human error, a critical consideration in medical device manufacturing.
Q 17. How do you optimize automated processes for efficiency and productivity?
Optimizing automated processes for efficiency and productivity involves a combination of techniques. Firstly, we perform a thorough process mapping exercise, identifying bottlenecks and inefficiencies in the existing workflow. This often involves using Lean Manufacturing principles, such as Value Stream Mapping, to pinpoint areas for improvement. Once bottlenecks are identified, we can explore solutions such as implementing advanced automation technologies, improving material flow, or streamlining work instructions. Data analysis plays a crucial role. We utilize manufacturing execution systems (MES) and other data collection tools to track key performance indicators (KPIs) like Overall Equipment Effectiveness (OEE), cycle time, and defect rates. This data-driven approach enables continuous improvement, allowing us to make informed decisions based on real-time performance.
For example, in one project, by analyzing OEE data, we identified that a particular automated assembly station was experiencing frequent stoppages due to part jams. Through a combination of process adjustments and the implementation of a more robust part feeding mechanism, we increased OEE by 15%, resulting in a significant boost in productivity.
Q 18. What are your experiences with preventative maintenance of automated equipment?
Preventative maintenance is crucial for maintaining the uptime and reliability of automated equipment. We implement a comprehensive preventative maintenance (PM) program that includes regular inspections, lubrication, cleaning, and calibration of all automated systems. This program is based on manufacturers’ recommendations and incorporates data collected through the equipment’s own diagnostics and historical performance. The PM schedule is carefully designed to minimize downtime while ensuring that potential issues are identified and addressed before they lead to failures. A computerized maintenance management system (CMMS) is utilized to track PM activities, manage spare parts inventory, and generate reports to monitor the effectiveness of the program. This structured approach extends the lifespan of equipment, reduces unexpected downtime, and ensures consistent product quality.
For example, we developed a predictive maintenance program using sensor data from robotic arms to identify potential issues before they became critical. This allowed us to schedule maintenance proactively, preventing costly unplanned downtime and ensuring continuous production.
Q 19. Describe your experience with the implementation of MES (Manufacturing Execution System) in medical device manufacturing.
My experience with MES implementation in medical device manufacturing involves the selection, configuration, and deployment of the system to track and manage production processes in real-time. This often involves integrating the MES with existing manufacturing equipment, enterprise resource planning (ERP) systems, and quality management systems. The MES provides real-time visibility into production metrics, enabling better decision-making and process optimization. Data collected by the MES is crucial for compliance reporting and analysis, ensuring that all regulatory requirements are met. Furthermore, a well-implemented MES facilitates traceability, a critical element in medical device manufacturing, allowing for easy identification of materials, processes, and personnel involved in the production of each device.
For instance, we implemented an MES system that provided real-time traceability of individual medical implants throughout the entire manufacturing process. This significantly simplified the investigation of potential quality issues and improved the overall efficiency of our quality control procedures.
Q 20. How do you handle unexpected downtime in automated production lines?
Unexpected downtime in automated production lines is addressed through a structured approach that prioritizes safety and minimizes disruption. First, we immediately secure the area to prevent further incidents and ensure the safety of personnel. Secondly, we initiate our established emergency response protocol, which includes notifying key personnel and activating the maintenance team. A detailed analysis of the problem is then performed using the data available from the system and through on-site investigation. Once the root cause is identified, the appropriate corrective action is taken to restore the system to operational status. Following the resolution of the immediate problem, we conduct a thorough root cause analysis to prevent future occurrences. This may involve improvements to the system’s design, operator training, or preventative maintenance procedures.
For example, during a recent power outage, our backup power system seamlessly transitioned, minimizing downtime and preventing loss of in-process materials. Post-outage, we analyzed the event and implemented measures to improve the resilience of the power system.
Q 21. Describe your experience with root cause analysis of automated system failures.
Root cause analysis (RCA) of automated system failures is a crucial element of maintaining reliable operations. We utilize a structured methodology, such as the ‘5 Whys’ technique or Fishbone diagrams, to systematically investigate the failure and identify its underlying causes. This involves gathering data from various sources, including machine logs, operator feedback, and maintenance records. A multi-disciplinary team, including engineers, technicians, and operators, collaborates to identify all contributing factors, leading to a comprehensive understanding of the root cause. Once the root cause is identified, effective corrective actions are implemented to prevent recurrence. These actions may range from simple adjustments to the system’s parameters to more extensive modifications of the hardware or software. Post-RCA, we review and update our preventative maintenance procedures and operator training programs to minimize the risk of similar failures in the future.
In a recent instance of a robotic arm malfunction, the RCA revealed that a combination of software bugs and inadequate lubrication led to the failure. Corrective actions involved software updates, improved lubrication schedules, and enhanced operator training on early detection of lubrication issues.
Q 22. What is your experience with lean manufacturing principles applied to automation?
Lean manufacturing principles, focused on eliminating waste and maximizing efficiency, are absolutely crucial in medical device automation. My experience involves applying these principles across various stages, from design and implementation to ongoing optimization. This includes using tools like Value Stream Mapping to identify bottlenecks and areas for improvement in automated processes. For instance, in one project involving automated assembly of a surgical instrument, we used Value Stream Mapping to pinpoint a slow-moving process step involving manual component loading. By redesigning the automated feeder system to utilize a more efficient vibratory bowl feeder, we reduced cycle time by 15%, resulting in increased throughput and cost savings. We also leverage Kanban systems for managing inventory and work-in-progress, ensuring a smoother flow and preventing overproduction of components – a common waste in automation. The application of 5S methodology (Sort, Set in Order, Shine, Standardize, Sustain) is equally important for maintaining a clean, organized and efficient workspace for optimal automated equipment performance and preventing defects.
Another key element is the use of Poka-Yoke (error-proofing) techniques within the automated systems themselves. For example, implementing sensors to detect missing or incorrectly placed components ensures automated processes halt before a faulty product is produced, minimizing scrap and rework.
Q 23. Explain your understanding of different types of automated testing equipment.
Automated testing equipment in medical device manufacturing is vital for ensuring product quality and compliance. There’s a wide variety, categorized by the type of testing they perform.
- Functional Testing: This verifies the device’s operational capabilities as per its specifications. Examples include automated systems that test the functionality of implantable cardiac defibrillators by simulating heart rhythms and evaluating the device’s response.
- Performance Testing: This measures critical parameters like speed, accuracy, and power consumption, often using automated data acquisition systems. An example would be an automated system that tests the precision of a robotic surgical instrument using high-speed cameras and measurement sensors.
- Environmental Testing: These systems simulate extreme conditions (temperature, humidity, pressure) to assess the device’s durability and reliability. Automated climate chambers are frequently used, for instance, to test the lifespan of disposable syringes under various temperature extremes.
- Dimensional Testing: This involves using automated coordinate measuring machines (CMMs) or vision systems to precisely measure the physical dimensions of components and assemblies to ensure they meet tight tolerances. Automated CMM inspection is critical for ensuring precise dimensions of orthopedic implants.
The choice of automated testing equipment depends heavily on the specific device, its functionality, and regulatory requirements.
Q 24. How do you ensure data integrity within automated medical device manufacturing systems?
Data integrity is paramount in medical device manufacturing, particularly when dealing with automated systems. Ensuring this requires a multi-faceted approach.
- Validation and Verification: Rigorous validation and verification protocols must be followed to confirm that automated systems function correctly and produce accurate, reliable data. This includes Software Validation (IQ/OQ/PQ) and ensuring systems operate under validated parameters.
- Audit Trails: Complete and auditable trails of all data generated, modified, or accessed by automated systems are essential. This allows for traceability and reconstruction of events, useful for investigations or compliance audits. This often involves utilizing secure databases with robust version control and access management.
- Access Control: Strict access control measures must be in place to limit access to data and systems to authorized personnel only, preventing unauthorized modifications or deletions. This involves using role-based access control (RBAC) and robust authentication systems.
- Data Backup and Recovery: Regular data backups and robust disaster recovery plans are crucial to protect against data loss. This protects against accidental or malicious data deletion, ensuring system reliability and business continuity.
- Data Security: Secure data storage and transmission techniques (encryption, firewalls) are essential to protect sensitive data from unauthorized access or cyber threats. This is particularly vital in relation to patient data if any is recorded during automated manufacturing.
By implementing these measures, we can ensure the accuracy, reliability, and security of data generated within automated medical device manufacturing systems, complying with regulatory requirements and maintaining patient safety.
Q 25. Describe your experience with the design and implementation of automated packaging systems.
My experience encompasses the entire lifecycle of automated packaging systems, from initial concept and design to implementation, validation, and ongoing maintenance. This includes selecting appropriate equipment for the specific medical device, such as automated cartoning machines, tray sealers, or blister packaging systems.
For example, in one project, we implemented a fully automated system for packaging sterile surgical instruments. This involved integrating a robotic arm to place the instruments into sterilized trays, a tray sealer for hermetic sealing, and a labeling system for unique identification. Critical considerations included ensuring the system maintained sterility throughout the packaging process. This required selecting appropriate materials, implementing cleanroom protocols, and incorporating real-time monitoring of critical parameters such as temperature and humidity. Design for Manufacturing (DFM) principles were applied throughout to simplify the packaging process, minimize material waste, and enhance the efficiency of the automated system. Validation procedures, including performance qualification (PQ) testing, verified that the system consistently met pre-defined specifications and maintained the required sterility levels.
Q 26. What is your experience with different types of robotic end-effectors?
Robotic end-effectors are the crucial interface between a robot and the object it manipulates. My experience encompasses a wide range of these, chosen based on the specific application and the characteristics of the medical device being handled.
- Grippers: These are perhaps the most common type, used to grasp and manipulate objects. Variations include two-finger, three-finger, and multi-finger grippers, as well as vacuum grippers (especially useful for delicate items). The choice depends on the shape and size of the medical device and the required grip force.
- Magnetic End-Effectors: Suitable for handling ferromagnetic materials, these are useful where a firm, non-damaging grip is needed for metallic components.
- Vacuum Cups: Ideal for handling smooth, flat surfaces, these are frequently used for picking and placing items like packaging materials or even medical trays.
- Specialized Tools: For more complex tasks, we might use customized end-effectors, such as tools for inserting small components or applying adhesives. A custom tool might be needed for screwing on a tiny cap onto a vial of medication.
Selecting the appropriate end-effector is critical for ensuring efficient and safe handling of medical devices without causing damage. This often requires extensive simulations and testing during the design phase.
Q 27. How do you balance the cost of automation with its potential benefits?
Balancing the cost of automation against its potential benefits is a key consideration in medical device manufacturing. It’s not just about the upfront investment; it’s a comprehensive cost-benefit analysis that considers the entire lifecycle.
Cost Factors: These include the initial investment in equipment, software, and integration, ongoing maintenance costs, training for personnel, and potential downtime during implementation.
Benefit Factors: Include increased throughput and productivity, improved product quality and consistency, reduced labor costs, minimized waste and scrap, enhanced traceability and data management, and better compliance with regulatory requirements.
Approaches to Balancing Costs and Benefits:
- Phased Implementation: Instead of a complete overhaul, implementing automation in phases allows for gradual investment and a controlled evaluation of return on investment (ROI).
- Return on Investment (ROI) Analysis: A detailed ROI analysis, projecting cost savings and increased revenues over a given period, is crucial for justifying the investment.
- Simulation and Modeling: Using simulation software to model different automation scenarios helps assess the potential benefits before committing to significant investments.
- Lifecycle Cost Analysis: Consider all costs over the equipment’s lifespan, including maintenance, repairs, and potential upgrades, to provide a holistic view of the cost of ownership.
Ultimately, the decision depends on a careful evaluation of the specific needs of the manufacturing process, considering the long-term implications and seeking to optimize both efficiency and cost-effectiveness.
Key Topics to Learn for Your Medical Device Manufacturing Automation Interview
- Cleanroom Environments and GMP Compliance: Understand the critical role of cleanroom design, classification, and adherence to Good Manufacturing Practices (GMP) in medical device manufacturing. Consider the impact of automation on maintaining these standards.
- Automation Technologies in Medical Device Manufacturing: Familiarize yourself with various automation technologies like robotics (SCARA, six-axis), vision systems, automated guided vehicles (AGVs), and programmable logic controllers (PLCs). Be prepared to discuss their applications and limitations in a medical device context.
- Process Validation and Qualification: Understand the importance of validating automated processes to ensure product quality and regulatory compliance. This includes IQ, OQ, and PQ phases. Be prepared to discuss your experience with documentation and record-keeping.
- Integration of Automation Systems: Explore the challenges and best practices involved in integrating various automation components into a cohesive manufacturing system. Consider data acquisition, control systems, and communication protocols (e.g., Ethernet/IP, PROFINET).
- Troubleshooting and Maintenance of Automation Equipment: Discuss your experience with preventative maintenance, troubleshooting malfunctions, and the importance of minimizing downtime in a regulated environment. Highlight your problem-solving skills and ability to work under pressure.
- Safety and Risk Assessment in Automated Systems: Understand the crucial role of safety considerations in designing and implementing automated systems in medical device manufacturing. This includes risk assessments, safety protocols, and machine guarding.
- Data Analytics and Process Optimization: Explore how data collected from automated systems can be used for process monitoring, quality control, and continuous improvement. Discuss your familiarity with relevant software and statistical methods.
Next Steps: Elevate Your Career in Medical Device Manufacturing Automation
Mastering Medical Device Manufacturing Automation opens doors to exciting and rewarding career opportunities. This field is constantly evolving, and professionals with expertise in automation are highly sought after. To maximize your job prospects, focus on creating a compelling and ATS-friendly resume that showcases your skills and experience effectively.
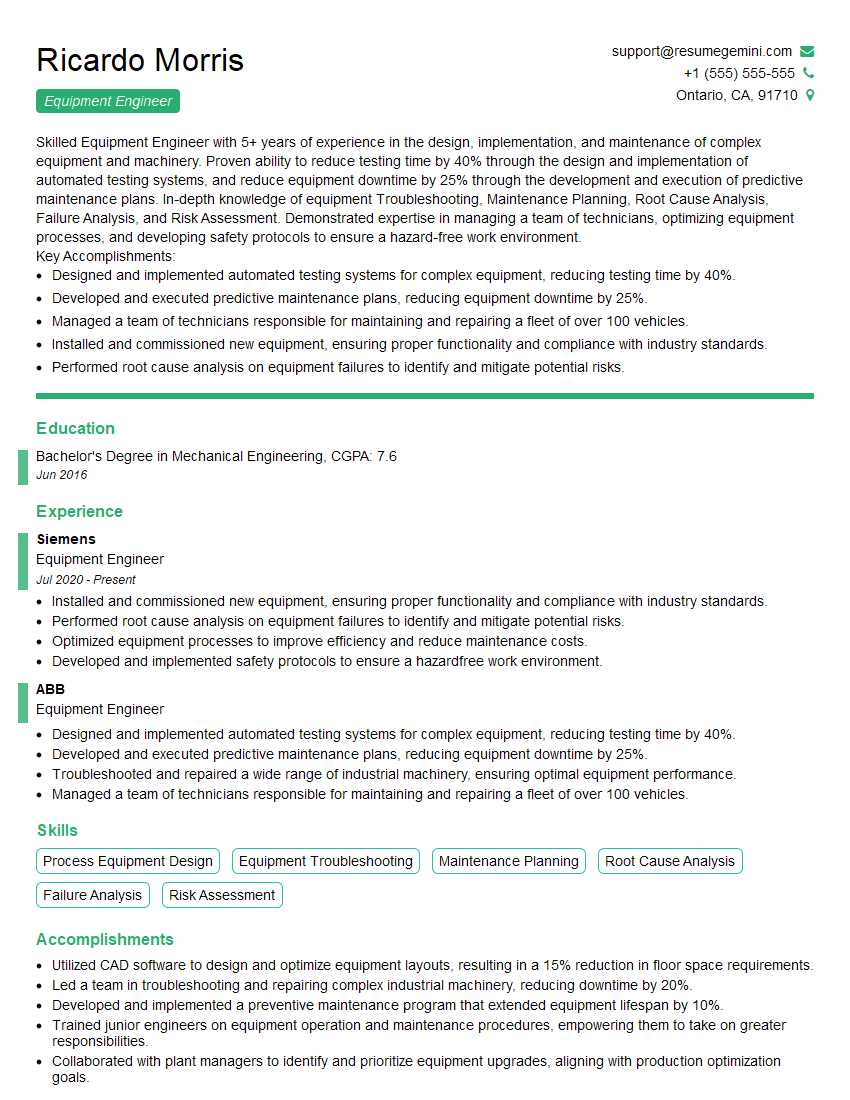
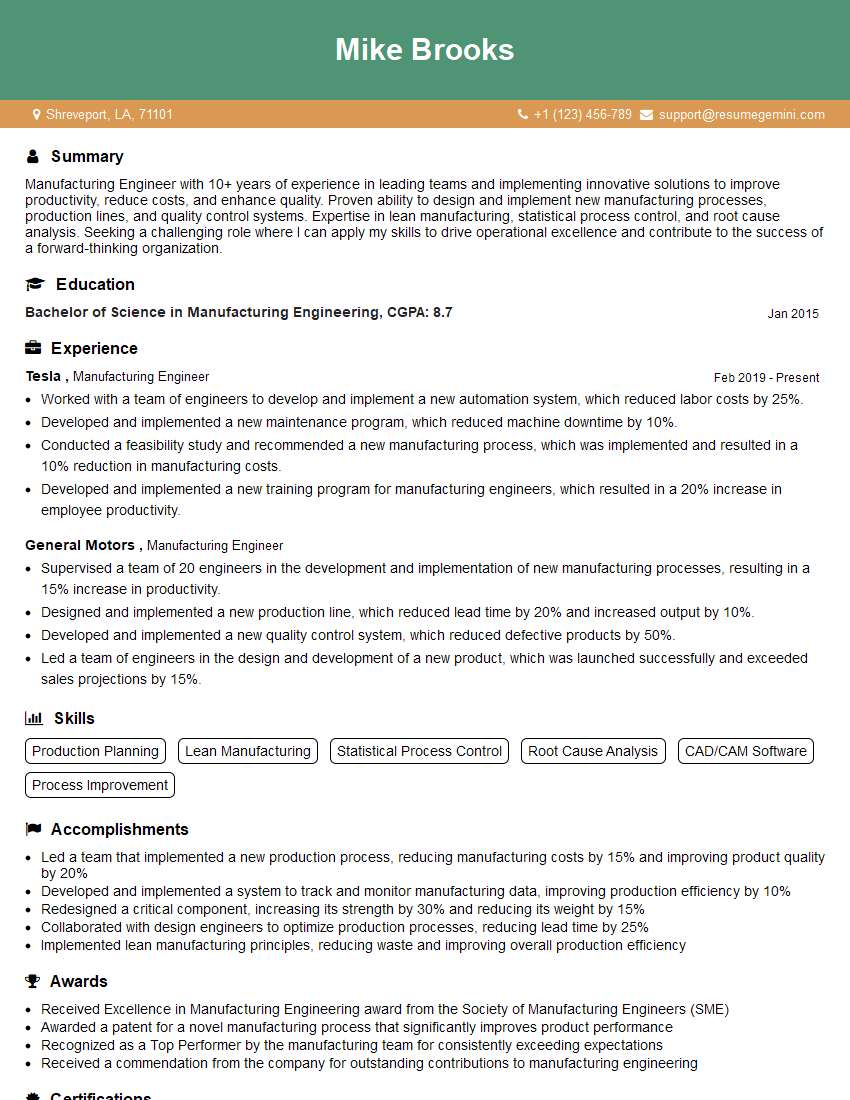
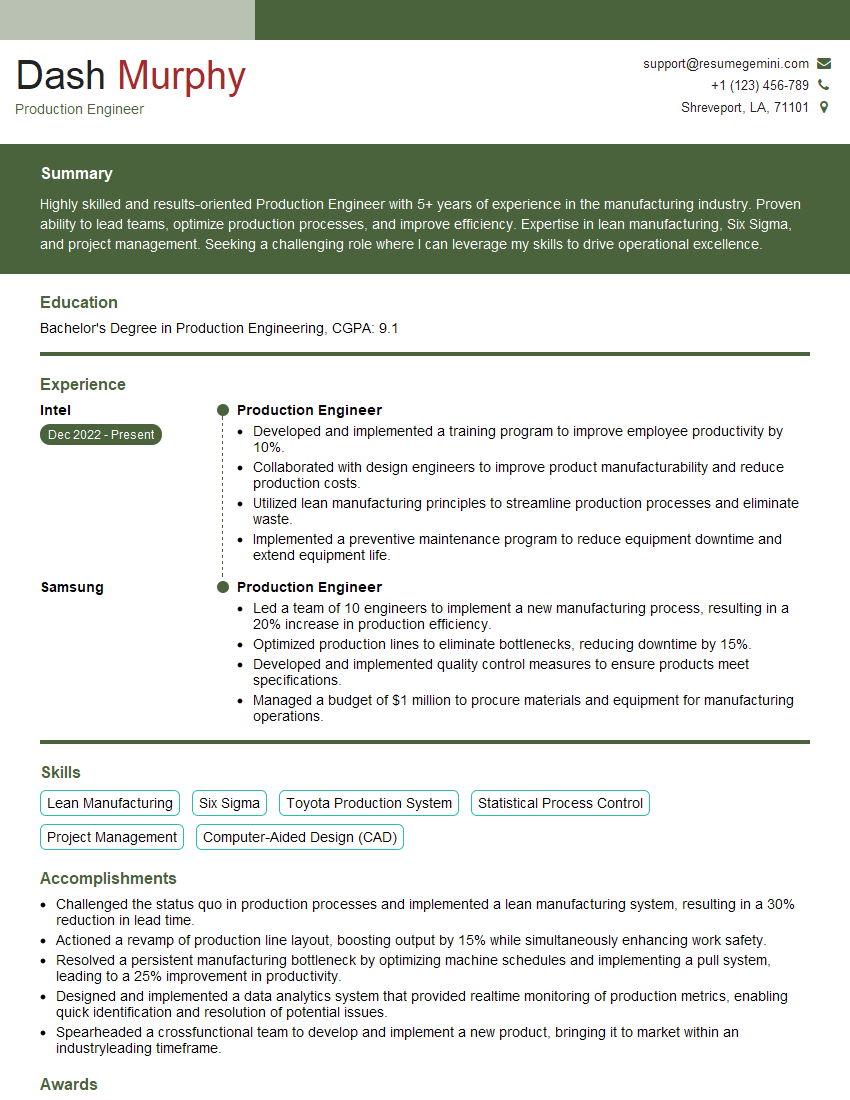
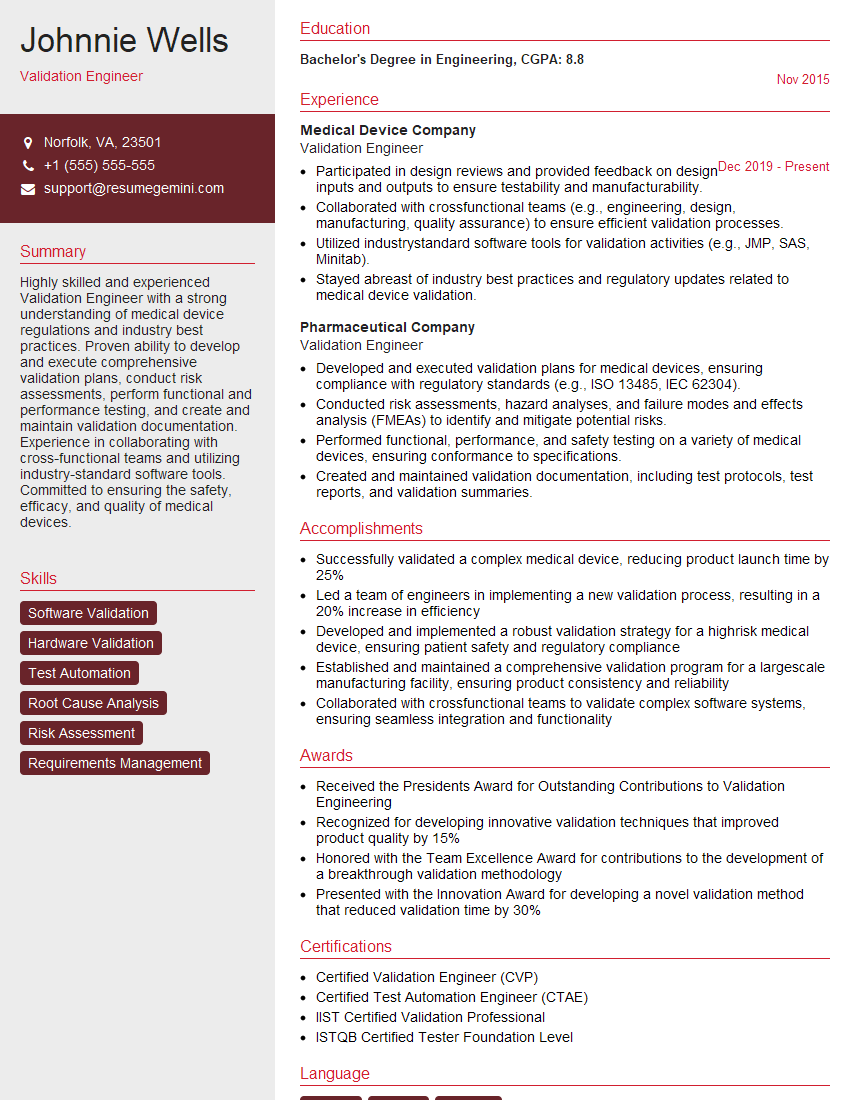
ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Leverage their tools and resources to craft a document that highlights your qualifications and experience in the best possible light. Examples of resumes tailored to Medical Device Manufacturing Automation are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good