Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Medical Device Manufacturing Processes interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Medical Device Manufacturing Processes Interview
Q 1. Explain your experience with Good Manufacturing Practices (GMP).
Good Manufacturing Practices (GMP) are a set of guidelines that ensure the consistent design, production, and quality of pharmaceutical products, medical devices, and other healthcare products. My experience spans over 10 years, encompassing various roles from manufacturing engineer to quality assurance manager. I’ve worked extensively with GMP regulations, ensuring compliance across all aspects of production, from raw material handling to final product release. This involved implementing and maintaining robust quality systems, conducting internal audits, and proactively identifying and mitigating potential risks to product quality and patient safety. For example, in my previous role, we implemented a new system for tracking and managing deviations from GMP, significantly reducing the occurrence of non-conformances and improving our overall quality record.
- Raw Material Management: Ensuring proper storage, handling, and identification of all raw materials to prevent contamination and degradation.
- Production Processes: Maintaining cleanroom environments, validating equipment, and adhering to strict operating procedures to ensure product consistency and sterility.
- Quality Control: Implementing rigorous testing procedures at various stages of production to detect and rectify any defects.
- Documentation and Record Keeping: Maintaining complete and accurate records of all manufacturing processes, tests, and quality control checks.
Q 2. Describe your experience with ISO 13485.
ISO 13485 is an internationally recognized quality management system (QMS) standard for medical devices. My experience includes leading and participating in ISO 13485 certifications, which involved developing and implementing QMS procedures across various departments. This encompassed everything from documenting processes to conducting internal audits and managing corrective and preventive actions (CAPAs). I have a strong understanding of risk management principles as applied to medical device manufacturing, including Hazard Analysis and Risk Control (HARC) methodologies, ensuring patient safety is always prioritized. In one instance, we successfully transitioned our entire manufacturing facility to ISO 13485:2016, managing the complex requirements and ensuring seamless operational continuity. This involved extensive training for staff, updating documentation, and implementing new procedures to meet the latest standard’s requirements.
Q 3. What are your experiences with Design Control processes?
Design Control is a crucial part of medical device development, ensuring that the device meets its intended use and is safe and effective. My experience involves participating in every phase of the Design Control process, from initial requirements definition and design input to verification and validation testing. I’m proficient in using design control tools like FMEAs (Failure Mode and Effects Analysis), risk assessments, and design reviews. For example, I was involved in the development of a new implantable cardiac device, where my responsibilities included leading design reviews, conducting risk assessments, and ensuring compliance with all relevant regulations. We utilized a risk-based approach, focusing our efforts on high-risk components and functionalities, which helped us to streamline the development process and deliver a high-quality product.
Q 4. How do you ensure traceability in a medical device manufacturing environment?
Traceability in medical device manufacturing is essential for tracking components and products throughout their entire lifecycle. This allows for efficient recall management in case of defects, and demonstrates compliance with regulatory requirements. My experience involves implementing and maintaining traceability systems using unique identification numbers (UIDs) assigned to raw materials, components, and finished products. We use barcode scanning and automated data entry systems to track the movement and processing of materials at each stage of production, ensuring a complete audit trail. For instance, we leveraged a robust ERP system to integrate with our manufacturing execution system (MES), creating a seamless chain of traceability from raw material receipt to the final product shipping. This not only improved our efficiency but also enhanced our ability to respond to regulatory audits and potential recalls effectively.
Q 5. Describe your experience with process validation and verification.
Process validation and verification are critical steps in ensuring that manufacturing processes consistently produce high-quality products that meet their intended specifications. My experience includes designing, conducting, and documenting process validation studies. I’m adept at creating validation protocols, executing testing, and analyzing results to verify the effectiveness of production processes. Verification is a confirmation that the process is meeting its requirements and that the product is meeting design specifications. Validation confirms the process is capable of consistently producing a product that meets predefined acceptance criteria. A recent project involved validating a new sterilization process for a surgical instrument. We designed a comprehensive validation protocol, conducted multiple sterilization cycles, and analyzed the data to demonstrate that the process consistently achieved the desired sterility assurance level (SAL).
Q 6. Explain different sterilization methods used in medical device manufacturing.
Several sterilization methods are employed in medical device manufacturing, each suited for different types of devices and materials. These include:
- Ethylene Oxide (EtO) Sterilization: Used for heat-sensitive devices and materials. It’s effective but requires careful control and monitoring due to its toxicity.
- Steam Sterilization (Autoclaving): A widely used method for heat-stable devices and materials. It’s efficient and cost-effective but may not be suitable for all materials.
- Gamma Irradiation: Utilizes ionizing radiation to sterilize devices and is effective for a wide range of materials. It leaves no residue, but some materials can be affected by radiation.
- Electron Beam Sterilization: Similar to gamma irradiation, but using electron beams for sterilization.
- Dry Heat Sterilization: Suitable for certain heat-stable materials and is less damaging than steam sterilization but requires longer exposure times.
The choice of sterilization method depends on several factors including the type of device, material compatibility, and regulatory requirements. Understanding these factors is crucial for selecting the most appropriate and effective sterilization technique.
Q 7. What is your experience with root cause analysis in a manufacturing setting?
Root cause analysis (RCA) is a systematic approach to identifying the underlying causes of problems or defects in a manufacturing process. My experience includes leading RCA investigations using various methodologies such as the 5 Whys, Fishbone diagrams, and Fault Tree Analysis. I’ve trained teams in RCA techniques and facilitated investigations, ensuring that the root cause is identified, not just the symptoms. For example, we investigated a recurring issue with a particular component failing during assembly. By applying the 5 Whys technique and analyzing process data, we discovered that the problem stemmed from inconsistent material handling during the early stages of manufacturing, leading to damage and ultimately failure. This allowed us to implement corrective actions, focused on improving material handling procedures, resulting in a significant reduction in component failures and improved overall product quality.
Q 8. How do you handle deviations and non-conformances?
Handling deviations and non-conformances in medical device manufacturing is paramount for patient safety and regulatory compliance. It involves a structured approach to identify, investigate, and rectify any instance where a product or process deviates from established specifications or requirements.
My approach begins with immediate containment. This means stopping further production of the affected items to prevent widespread issues. We then conduct a thorough investigation, gathering data, interviewing personnel, and analyzing root causes. This is often done using tools like fishbone diagrams or 5 Whys analysis to get to the heart of the problem, not just the symptoms. For example, if a batch of catheters fails a sterility test, we wouldn’t just discard the batch; we’d investigate the sterilization cycle, equipment maintenance records, and even environmental factors to pinpoint the root cause.
Once the root cause is identified, we implement corrective actions to address the immediate issue. This might include reworking the affected product, implementing improved cleaning procedures, or replacing faulty equipment. We then develop preventive actions to prevent similar issues from occurring in the future. This could include implementing new training programs, updating work instructions, or installing new monitoring systems. All of this is meticulously documented and reviewed by management to ensure effectiveness and compliance.
Q 9. What is your experience with CAPA (Corrective and Preventive Action)?
Corrective and Preventive Action (CAPA) is the backbone of a robust quality management system in medical device manufacturing. My experience involves implementing and managing CAPA processes across various aspects of production. I’m proficient in using CAPA software to track investigations, document findings, and ensure timely resolution.
I’ve been involved in several CAPA investigations, ranging from minor issues like a labeling error to more significant events requiring extensive root cause analysis and regulatory reporting. For instance, one project involved a deviation in the welding process of a critical component. Through a detailed investigation, we discovered that inadequate operator training was the root cause. Our CAPA plan included enhanced training modules, updated work instructions with clear visual aids, and the implementation of a competency assessment program to ensure ongoing competence. We tracked the effectiveness of these actions, documenting the improvements and preventing future occurrences.
A key aspect of effective CAPA management is effective communication. Keeping all relevant stakeholders – from engineering and manufacturing to quality assurance and regulatory affairs – informed throughout the process is crucial for timely and effective resolution.
Q 10. Describe your understanding of statistical process control (SPC).
Statistical Process Control (SPC) is a powerful tool for monitoring and controlling manufacturing processes to ensure consistent product quality. It involves using statistical methods to analyze process data, identifying trends, and taking corrective actions to prevent defects.
I’m experienced in using various SPC tools, including control charts (like X-bar and R charts, p-charts, and c-charts), process capability analysis (Cp, Cpk), and process improvement techniques like Design of Experiments (DOE). For example, we used control charts to monitor the weight of a specific implantable device during the manufacturing process. By plotting the weight data on a control chart, we could readily identify any shifts or trends in the process, allowing us to take prompt corrective action before significant deviations occurred. This prevented costly scrap and rework while maintaining tight tolerances needed for proper device function.
SPC isn’t just about identifying problems; it’s also about understanding and improving the process. By analyzing data from control charts, we can gain valuable insights into process variability and identify opportunities for process optimization. Using techniques like DOE, for example, we could systematically alter process parameters to optimize efficiency and reduce variation while improving the overall quality of the end product.
Q 11. Explain your experience with different types of manufacturing processes (e.g., injection molding, machining).
My experience encompasses a broad range of medical device manufacturing processes, including injection molding, machining, and assembly. I understand the nuances of each process and its impact on product quality.
Injection molding is crucial for producing many plastic components. My experience includes optimizing molding parameters (temperature, pressure, injection speed) to achieve desired part geometry and material properties while minimizing defects. I’ve worked extensively on validating injection molding processes to ensure they consistently produce parts meeting specifications. For example, I worked on a project to improve the surface finish of a plastic housing for a medical instrument. By optimizing injection molding parameters and implementing strict quality control checks, we reduced surface defects significantly, improving the aesthetic appeal and reducing the risk of particulate contamination.
Machining, often used for metal components, requires precision and skill. I’m familiar with various machining techniques (e.g., milling, turning, drilling) and quality control measures to ensure dimensional accuracy and surface finish. Assembly processes, often the final step, involve various techniques from manual assembly to automated assembly lines. My experience includes optimizing assembly processes to ensure efficient production while minimizing errors. The focus always remains on the rigorous adherence to standards and quality control to produce safe and effective medical devices.
Q 12. How do you ensure the quality of raw materials and components?
Ensuring the quality of raw materials and components is a critical aspect of medical device manufacturing. This involves a multi-layered approach, beginning with supplier selection and qualification.
We rigorously qualify our suppliers, evaluating their quality management systems, manufacturing processes, and capabilities. This often involves on-site audits to verify their compliance with relevant standards (e.g., ISO 9001, ISO 13485). Incoming materials are then subjected to rigorous inspection and testing to verify that they meet the specified requirements. This includes visual inspection, dimensional checks, material testing (e.g., tensile strength, biocompatibility), and often, specialized testing relevant to the specific component. Failure to meet specifications results in rejection and immediate action with the supplier to rectify the issue. Documentation of all incoming material inspections is meticulously maintained.
We utilize a robust Material Review Board (MRB) process to handle non-conforming materials, which involves assessing the impact of the non-conformance on the final product and determining the appropriate course of action, whether it’s rework, rejection, or concession.
Q 13. Describe your experience with equipment qualification and validation.
Equipment qualification and validation are essential for ensuring the reliability and consistency of manufacturing processes. Equipment qualification involves demonstrating that the equipment is fit for its intended purpose, while validation confirms that the equipment consistently produces the desired results.
My experience includes performing IQ (Installation Qualification), OQ (Operational Qualification), and PQ (Performance Qualification) for various equipment types commonly used in medical device manufacturing, including autoclaves, cleanroom equipment, and specialized manufacturing machinery. IQ focuses on verifying the correct installation of the equipment, OQ confirms that the equipment operates according to its specifications, and PQ verifies that the equipment consistently produces the intended results under normal operating conditions. We meticulously document all stages of the qualification and validation process, including protocols, test results, and deviations. This documentation is essential for regulatory compliance and ensures traceability of equipment performance.
For example, validating an autoclave involved monitoring its temperature and pressure profiles across multiple cycles using calibrated sensors. This ensured the autoclave consistently achieved the necessary sterilization parameters, guaranteeing sterility of the processed medical devices.
Q 14. What is your experience with cleanroom protocols and aseptic techniques?
Cleanroom protocols and aseptic techniques are crucial in medical device manufacturing, especially for devices that come into direct contact with the patient’s body. Cleanrooms provide a controlled environment with low levels of particulate matter and microorganisms to minimize contamination risks.
My experience includes working in various cleanroom classifications (e.g., ISO Class 7, ISO Class 8) and adhering to strict protocols for gowning, environmental monitoring, and equipment cleaning and sterilization. Aseptic techniques, essential for preventing microbial contamination, are employed throughout the manufacturing process. This includes using proper techniques for handling sterile materials, maintaining a sterile field, and employing methods like laminar flow hoods and isolators to protect the product from contamination.
I am proficient in using environmental monitoring equipment (e.g., particle counters, microbial air samplers) to monitor the cleanroom environment, ensuring it consistently meets the required cleanliness standards. Any deviations from established protocols are thoroughly investigated and documented. Regular training and competency assessments are conducted for personnel working in cleanrooms to ensure they are proficient in aseptic techniques and cleanroom protocols.
Q 15. Explain your experience with production planning and scheduling.
Production planning and scheduling in medical device manufacturing is a complex process that requires meticulous attention to detail. It involves forecasting demand, allocating resources, and sequencing production to meet deadlines while adhering to strict quality and regulatory standards. My experience spans several years, working with both MRP (Material Requirements Planning) and ERP (Enterprise Resource Planning) systems to optimize production flows.
For example, in my previous role, we implemented a new scheduling algorithm that reduced lead times by 15% by prioritizing critical components and leveraging Kanban principles for managing work-in-progress. We also utilized simulation software to model different scheduling scenarios and identify potential bottlenecks before they occurred. This proactive approach significantly reduced production delays and improved on-time delivery.
- Demand Forecasting: Utilizing historical data, market trends, and sales forecasts to predict future demand for various medical devices.
- Capacity Planning: Assessing the available resources – equipment, personnel, and materials – to determine production capacity and identify potential constraints.
- Master Production Schedule (MPS): Developing a detailed schedule outlining the production sequence for different products, considering dependencies and constraints.
- Material Requirements Planning (MRP): Calculating the necessary raw materials and components needed for production, taking into account lead times and inventory levels.
- Shop Floor Control: Monitoring actual production progress against the schedule and making adjustments as needed to address any deviations.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage inventory and supply chain challenges in medical device manufacturing?
Managing inventory and supply chain challenges in medical device manufacturing is crucial for maintaining production continuity and meeting patient needs. The high regulatory scrutiny and the often specialized nature of components necessitate a robust and proactive approach. My strategy involves a multi-pronged approach focusing on vendor management, inventory optimization, and risk mitigation.
For instance, I’ve successfully implemented a Vendor Managed Inventory (VMI) system for key components, allowing our suppliers to manage their inventory levels based on our forecasted demand. This minimized our storage costs and reduced the risk of stockouts. We also implemented a sophisticated inventory tracking system using RFID technology to improve accuracy and traceability of components throughout the supply chain. This allowed for real-time visibility into inventory levels and helped identify and address potential supply chain disruptions promptly.
- Supplier Relationship Management: Building strong relationships with key suppliers to ensure reliable supply of high-quality materials.
- Inventory Optimization: Utilizing inventory management techniques like Just-in-Time (JIT) to minimize inventory holding costs while ensuring sufficient stock to meet demand.
- Risk Management: Identifying and mitigating potential risks in the supply chain, such as natural disasters, geopolitical instability, and supplier disruptions.
- Supply Chain Diversification: Exploring alternative suppliers to reduce dependence on a single source and mitigate supply chain risks.
Q 17. Describe your experience with lean manufacturing principles.
Lean manufacturing principles are fundamental to efficiency and quality in medical device manufacturing. My experience includes implementing several lean tools and methodologies to eliminate waste, improve flow, and enhance overall productivity. These principles focus on optimizing value streams and reducing non-value-added activities.
In a previous project, we applied the 5S methodology (Sort, Set in Order, Shine, Standardize, Sustain) to our assembly line, resulting in a 20% reduction in production time. We also implemented Kaizen events – focused improvement workshops – to identify and eliminate bottlenecks in the production process. These continuous improvement initiatives have led to significant gains in efficiency and quality.
- Value Stream Mapping: Visually mapping the entire production process to identify areas of waste and inefficiency.
- 5S Methodology: Organizing the workplace to improve efficiency and reduce errors.
- Kaizen Events: Short, focused workshops to identify and eliminate bottlenecks.
- Kanban System: Managing work-in-progress to reduce lead times and improve flow.
- Poka-Yoke (Mistake-Proofing): Designing processes to prevent errors from occurring.
Q 18. How do you improve efficiency and reduce costs in a medical device manufacturing setting?
Improving efficiency and reducing costs in medical device manufacturing requires a holistic approach focusing on process optimization, waste reduction, and technology adoption. My approach typically involves a combination of lean manufacturing principles, automation, and data-driven decision-making.
For example, we implemented a new automated inspection system that reduced inspection time by 50% and improved the accuracy of defect detection. This not only saved labor costs but also improved product quality and reduced scrap. We also implemented a preventative maintenance program for our equipment, minimizing downtime and extending the lifespan of our assets. This proactive approach reduced maintenance costs and improved overall equipment effectiveness (OEE).
- Process Optimization: Analyzing and streamlining production processes to eliminate waste and improve efficiency.
- Automation: Implementing automated systems to reduce labor costs and improve consistency.
- Waste Reduction: Identifying and eliminating sources of waste, such as excess inventory, defects, and waiting time.
- Data Analytics: Using data to identify trends, predict issues, and make informed decisions.
- Preventative Maintenance: Implementing a schedule of preventative maintenance on equipment to avoid costly breakdowns.
Q 19. What experience do you have with automation and robotics in medical device manufacturing?
Automation and robotics play an increasingly critical role in modern medical device manufacturing. My experience includes working with various automated systems, from robotic assembly lines to automated inspection equipment. These technologies enhance precision, consistency, and efficiency while reducing human error and improving throughput.
In one project, we integrated a robotic arm into our assembly line, automating a repetitive and labor-intensive task. This resulted in a significant reduction in assembly time and improved product quality. We also implemented an automated vision system for inspection, increasing the speed and accuracy of defect detection.
- Robotic Assembly: Utilizing robots to perform repetitive assembly tasks, improving speed, precision, and consistency.
- Automated Inspection Systems: Employing vision systems and other automated methods for quality control, enhancing accuracy and efficiency.
- Automated Material Handling: Using automated guided vehicles (AGVs) and other systems to move materials efficiently throughout the facility.
- Integration of MES Systems: Connecting automation systems to Manufacturing Execution Systems (MES) for real-time data collection and monitoring.
Q 20. Explain your knowledge of different types of medical device packaging and labeling.
Medical device packaging and labeling are critical for ensuring product sterility, safety, and traceability. My knowledge encompasses a wide range of packaging types, from blister packs and pouches to trays and cartons, each with its specific applications and regulatory requirements. Labeling must adhere to strict guidelines, including information on product identification, usage instructions, and warnings.
For example, I’ve been involved in selecting appropriate packaging materials for implantable devices, ensuring sterility and protection from environmental factors. We’ve also implemented a barcode tracking system for all packaging, allowing us to track devices throughout the supply chain and ensure accurate inventory management. This ensures compliance with regulations like Unique Device Identification (UDI).
- Sterile Packaging: Understanding various sterilization methods and selecting appropriate packaging materials to maintain sterility.
- Protective Packaging: Choosing packaging materials that protect the device from damage during shipping and handling.
- Labeling Requirements: Adhering to all relevant regulatory labeling requirements, including UDI, warnings, and instructions for use.
- Packaging Materials Selection: Choosing appropriate materials based on device type, sterilization method, and environmental conditions.
- Packaging Validation: Verifying that the selected packaging meets all performance requirements.
Q 21. Describe your experience with regulatory submissions and approvals (e.g., FDA 510(k)).
Regulatory submissions and approvals, such as FDA 510(k) submissions, are a critical aspect of medical device manufacturing. My experience includes preparing and submitting regulatory documentation, working closely with regulatory bodies to ensure compliance, and managing the entire approval process. This involves meticulous record-keeping, demonstrating compliance with quality system regulations (e.g., ISO 13485), and managing post-market surveillance.
For instance, I was part of a team that successfully navigated the 510(k) submission process for a new implantable device, working closely with regulatory consultants and internal teams to ensure all requirements were met. This involved compiling extensive documentation, including design history files, test results, and risk assessments. We meticulously managed the review process, addressing any queries from the regulatory body promptly and professionally. Following approval, we established a robust post-market surveillance program to monitor device performance and address any issues that may arise.
- 510(k) Submissions: Preparing and submitting 510(k) applications to the FDA, demonstrating substantial equivalence to a predicate device.
- Premarket Approval (PMA): Understanding the PMA process for high-risk devices and assisting with the preparation of PMA submissions.
- ISO 13485 Compliance: Ensuring that the quality management system meets the requirements of ISO 13485.
- Regulatory Affairs Strategy: Developing a comprehensive regulatory strategy to ensure compliance with all relevant regulations.
- Post-Market Surveillance: Implementing and managing a robust post-market surveillance program to monitor device performance and address any safety concerns.
Q 22. How do you manage risk in medical device manufacturing?
Risk management in medical device manufacturing is paramount, as even minor failures can have severe consequences. We employ a multifaceted approach based on ISO 14971, which dictates a systematic process for identifying, analyzing, evaluating, and controlling risks. This includes proactively identifying potential hazards throughout the entire product lifecycle, from design and development to manufacturing and post-market surveillance.
- Hazard Analysis: We use Failure Mode and Effects Analysis (FMEA) to systematically identify potential failures, their effects, and the severity of those effects. For example, a faulty sensor in a pacemaker could lead to incorrect pacing, a critical hazard. We assign risk priority numbers (RPNs) based on severity, probability, and detectability.
- Risk Control: Once hazards are identified, we implement control measures to mitigate the risks. These might include design modifications, process improvements (e.g., tighter tolerances, additional quality checks), or operator training. For instance, if the FMEA reveals a high risk of contamination during assembly, we might introduce a cleanroom with stricter environmental controls.
- Risk Acceptance/Mitigation: Not all risks can be eliminated entirely. We establish acceptable risk levels and document the rationale for accepting residual risks. We continuously monitor and review our risk controls to ensure their effectiveness.
- Post-Market Surveillance: We actively monitor our devices after they’ve been released to the market to identify and address any emerging risks. This includes collecting data on adverse events and implementing corrective and preventive actions (CAPA).
This structured approach allows us to prioritize resources, focus on the most critical risks, and maintain a consistently high level of product safety and quality.
Q 23. Describe your experience with change control procedures.
Change control is essential for maintaining compliance and preventing unintended consequences. I’ve been involved in numerous change control processes throughout my career, adhering to strict procedures that ensure any modifications to designs, processes, or materials are thoroughly reviewed and approved before implementation. This typically involves a formal change request, impact assessment, risk assessment, and a multi-disciplinary review before approval.
For example, consider a change to a supplier’s material. We’d initiate a change request, thoroughly evaluate the new material’s properties to ensure it meets all requirements (e.g., biocompatibility, sterilization compatibility), and conduct validation testing to confirm the change doesn’t negatively impact product performance or reliability. A comprehensive documentation trail is maintained throughout this process to meet audit requirements and demonstrate regulatory compliance. Failure to properly manage change control could lead to deviations in quality, regulatory violations, and even patient harm.
Q 24. What is your experience with auditing and inspections?
I have extensive experience with internal and external audits and inspections, having participated in numerous audits conducted by regulatory bodies (e.g., FDA, notified bodies) and internal quality audits. I’m familiar with various auditing standards (e.g., ISO 13485, 21 CFR Part 820). My role involves preparing for audits, providing documentation, and answering auditor questions. A crucial aspect is maintaining comprehensive and auditable records.
For instance, during an FDA inspection, we need to readily provide documentation like design history files, manufacturing records, and quality system procedures. I’ve actively contributed to corrective actions following audits, focusing on both immediate corrective actions and longer-term preventative measures to prevent recurring issues. Successful audits demonstrate our commitment to quality and regulatory compliance.
Q 25. How familiar are you with different types of manufacturing documentation (e.g., batch records, work instructions)?
I’m very familiar with various types of manufacturing documentation, understanding their critical roles in traceability, compliance, and product quality. These documents form the backbone of our quality system.
- Batch Records: These are detailed records documenting all steps in the manufacturing process for a specific batch of product, providing complete traceability. They include information such as materials used, equipment settings, personnel involved, test results, and deviations.
Example: A batch record for a drug-eluting stent would specify the exact lot numbers of the stent material, the drug coating, the packaging materials, and all testing performed. - Work Instructions: These documents provide step-by-step instructions for performing specific tasks, ensuring consistency and preventing errors. They are crucial for standardizing operations.
Example: A work instruction for assembling a syringe would detail each step, including the specific tools and equipment needed, the sequence of operations, and quality checks at each stage. - Master Manufacturing Records: These are control documents that define the overall manufacturing process. Work instructions are derived from these master records.
- Deviations and CAPAs: Documentation of deviations from established processes and corrective and preventative actions (CAPAs) is crucial for continuous improvement and demonstrating regulatory compliance.
The accuracy and completeness of these documents are critical for demonstrating compliance during audits and investigations.
Q 26. Describe your experience with problem-solving methodologies (e.g., 5 Whys, Fishbone diagrams).
Problem-solving is a critical skill in manufacturing. I’m proficient in various methodologies, including the 5 Whys and Fishbone diagrams (Ishikawa diagrams).
- 5 Whys: This iterative technique helps uncover the root cause of a problem by repeatedly asking “why” until the fundamental issue is identified. It’s simple but effective for relatively straightforward problems.
- Fishbone Diagram: This visual tool helps brainstorm potential causes categorized by different factors (e.g., materials, methods, manpower, machinery, environment, measurement). It’s helpful for complex problems with multiple potential causes.
For instance, imagine a recurring issue with device malfunction. Using the 5 Whys, we might discover: 1. Why are devices malfunctioning? Because of faulty sensors. 2. Why are sensors faulty? Because of poor soldering. 3. Why is the soldering poor? Because of insufficient training. 4. Why is training insufficient? Because training materials were outdated. 5. Why were training materials outdated? Because of a lack of process for regular review. This would reveal the root cause and allow for targeted improvements to training and materials review processes.
In more complex scenarios, a Fishbone diagram would provide a more structured approach for analyzing multiple potential contributing factors.
Q 27. How do you ensure compliance with regulatory requirements?
Ensuring regulatory compliance is a cornerstone of medical device manufacturing. Compliance is achieved through a robust quality management system (QMS) that adheres to relevant regulations and standards (e.g., ISO 13485, 21 CFR Part 820, MDR/IVDR (where applicable)). This includes establishing processes for design control, risk management, manufacturing processes, quality control, and post-market surveillance.
We employ several strategies to ensure compliance: regular internal audits, training on regulatory requirements, continuous improvement initiatives, thorough documentation, and effective communication with regulatory bodies. We actively monitor regulatory updates and adapt our processes as needed to stay compliant. Non-compliance can lead to significant consequences, including regulatory actions, product recalls, and reputational damage. Therefore, proactive and diligent compliance efforts are crucial.
Q 28. Explain your experience with training and development of manufacturing personnel.
Training and development of manufacturing personnel are vital for maintaining product quality and ensuring consistent compliance. I have extensive experience in developing and delivering training programs tailored to the specific needs of our manufacturing teams. This includes both initial training and ongoing continuing education. Effective training programs cover:
- Standard Operating Procedures (SOPs): Training on specific procedures followed in the manufacturing process.
- Quality Systems: Training on our quality management system, including documentation and compliance requirements.
- Good Manufacturing Practices (GMP): Training on proper manufacturing techniques to ensure product quality and safety.
- Equipment Operation: Training on the safe and proper operation of all manufacturing equipment.
- Regulatory Requirements: Training on relevant regulatory requirements and standards.
We utilize various training methods, such as classroom instruction, hands-on training, and online modules, to cater to different learning styles. Regular competency assessments are conducted to ensure personnel maintain the required skills and knowledge. A well-trained workforce is essential for reducing errors, improving product quality, and ensuring compliance.
Key Topics to Learn for Medical Device Manufacturing Processes Interview
- Good Manufacturing Practices (GMP): Understand the principles and regulations governing medical device manufacturing, including FDA guidelines and ISO 13485.
- Design Control: Explore the process of designing medical devices to meet regulatory requirements and user needs, focusing on risk management and verification/validation.
- Material Selection and Characterization: Learn about the properties of biocompatible materials used in medical devices and their impact on manufacturing processes.
- Sterilization Methods: Familiarize yourself with various sterilization techniques (e.g., ethylene oxide, gamma irradiation, steam sterilization) and their effects on device integrity.
- Manufacturing Processes: Gain a strong understanding of common manufacturing processes such as injection molding, machining, extrusion, and assembly, including their strengths and limitations for medical devices.
- Quality Control and Assurance: Master the principles of quality control and assurance, including inspection methods, statistical process control (SPC), and corrective and preventative actions (CAPA).
- Cleanroom Technology and Contamination Control: Understand the importance of maintaining a controlled environment to prevent contamination during manufacturing.
- Process Validation and Verification: Learn how to demonstrate that manufacturing processes consistently produce devices meeting pre-defined specifications.
- Troubleshooting and Problem-Solving: Develop your ability to identify, analyze, and resolve manufacturing process issues effectively.
- Documentation and Traceability: Understand the critical role of comprehensive documentation in maintaining regulatory compliance and product traceability.
Next Steps
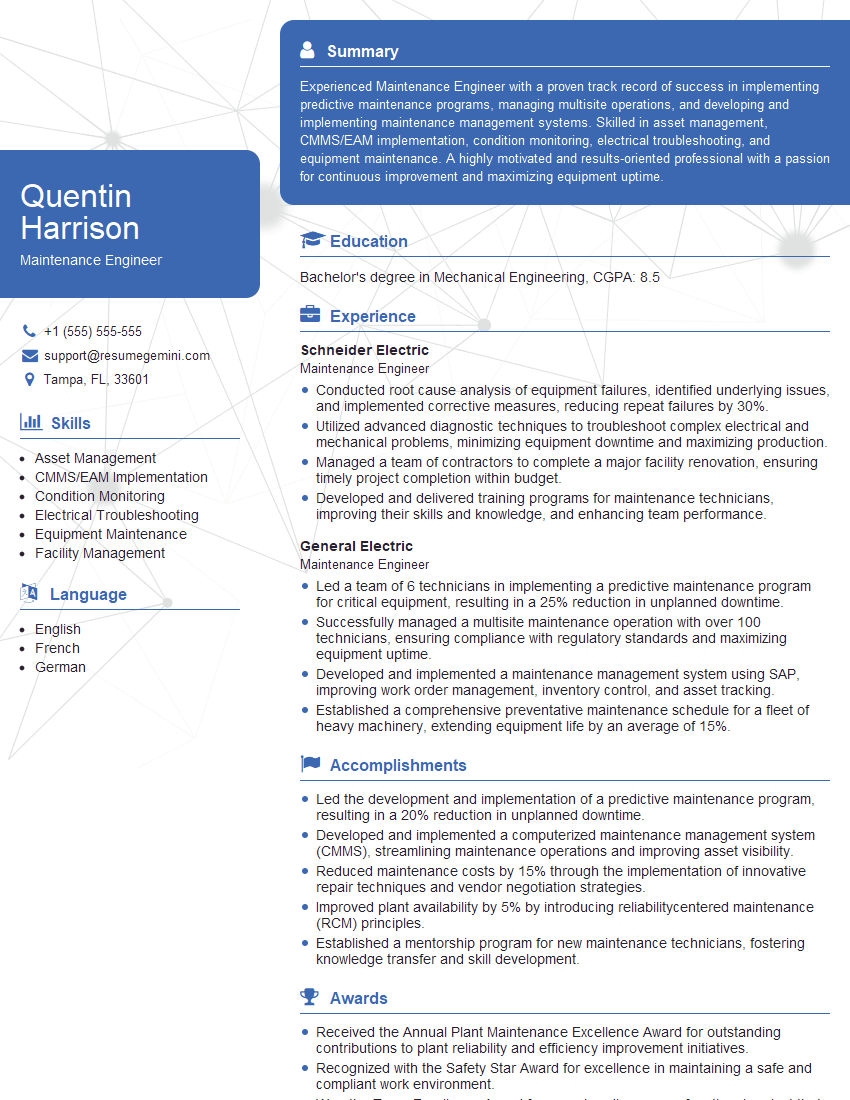
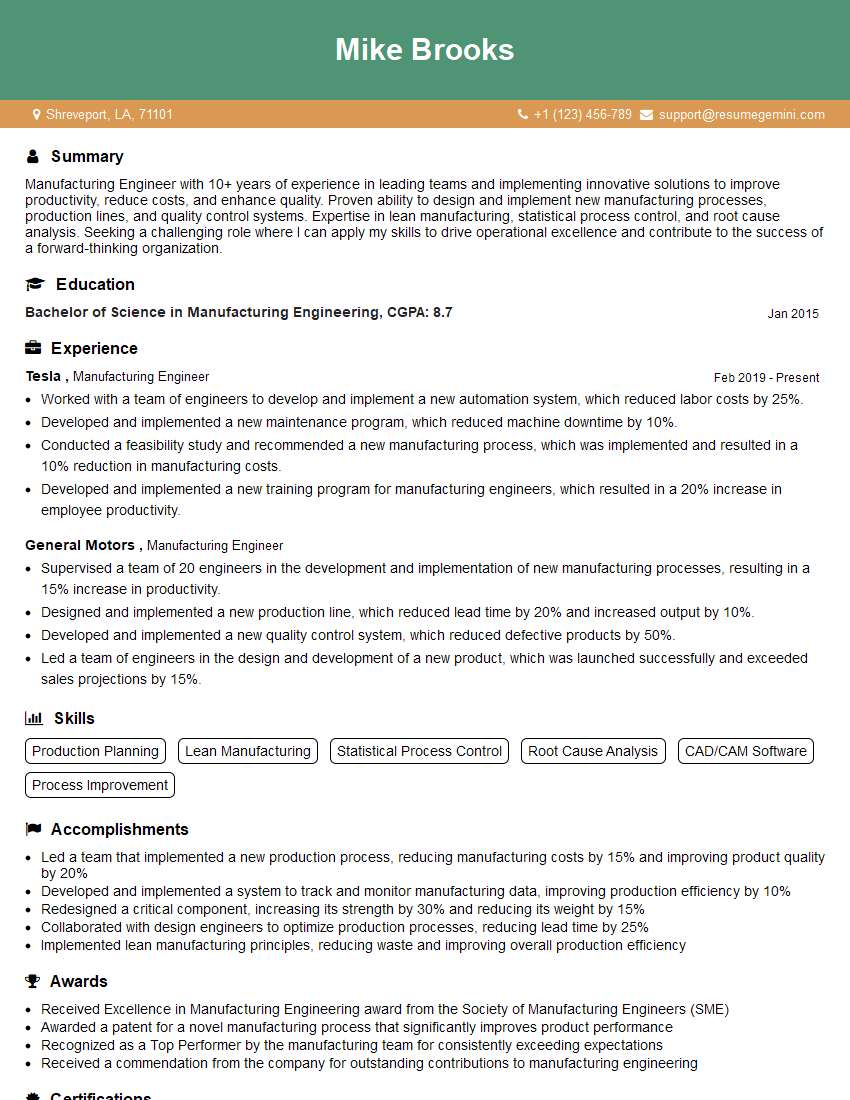
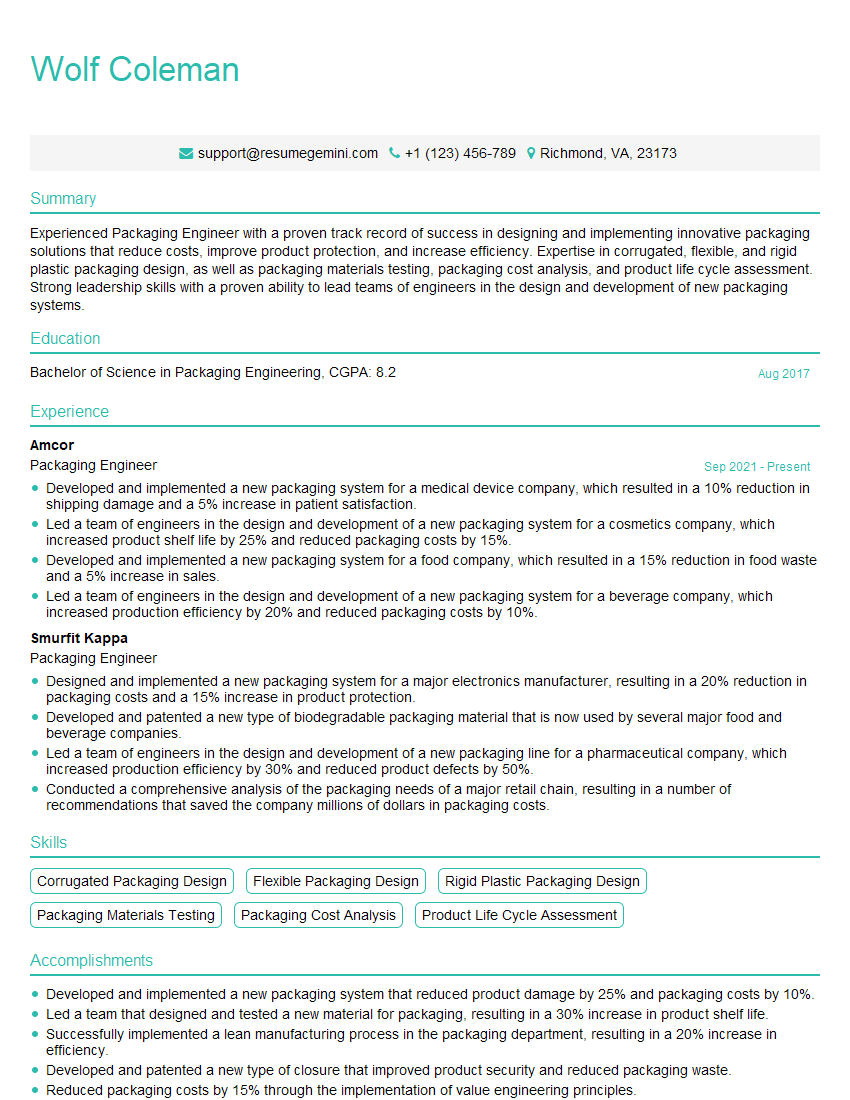
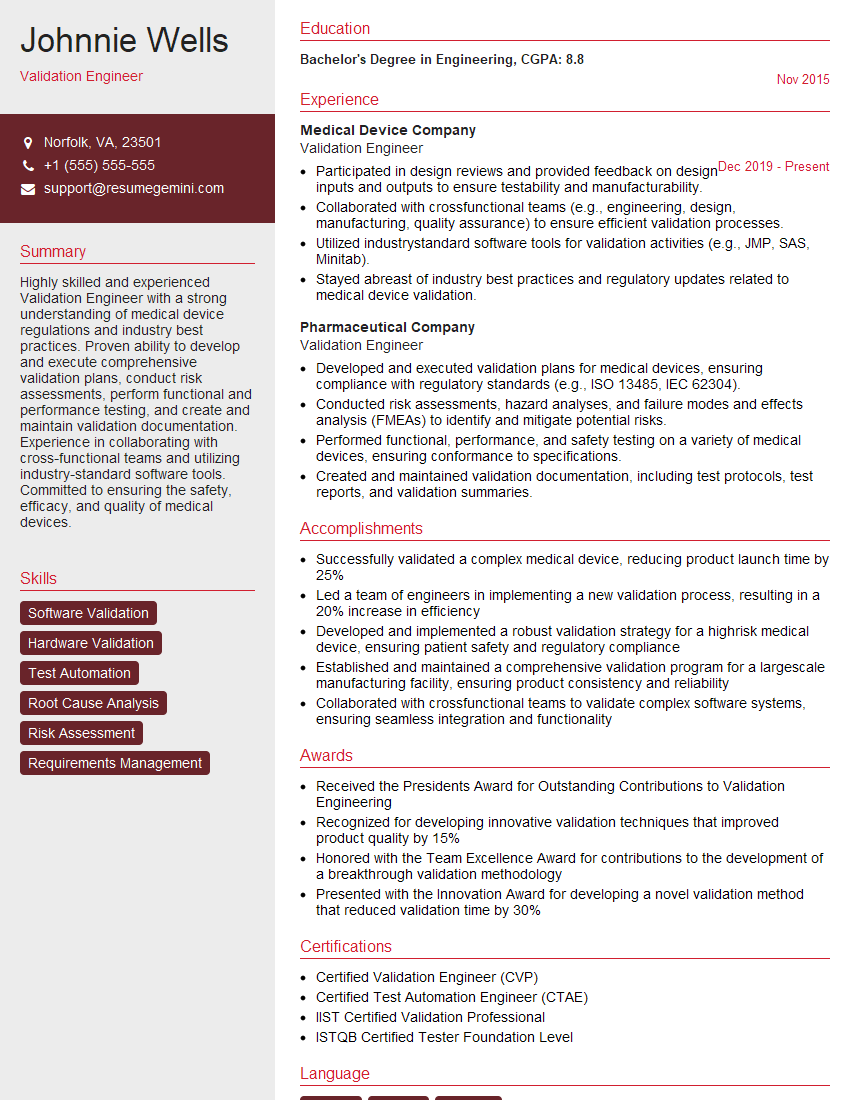
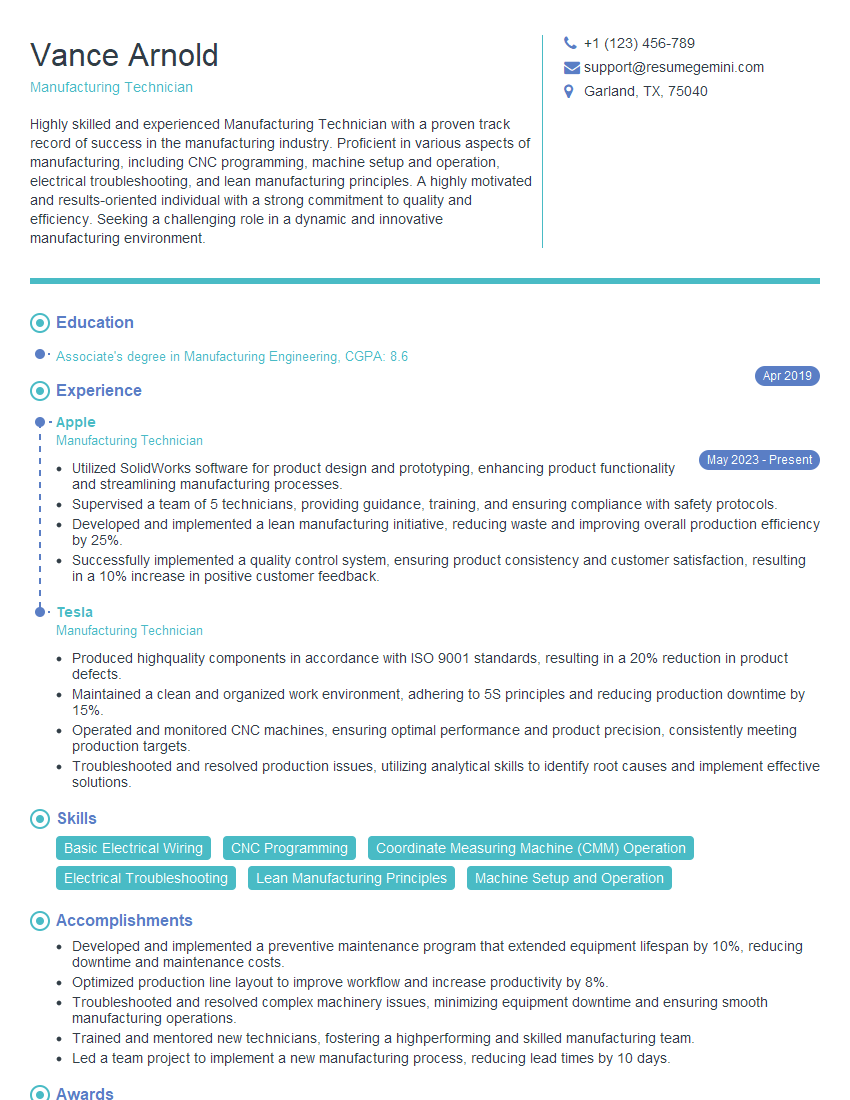
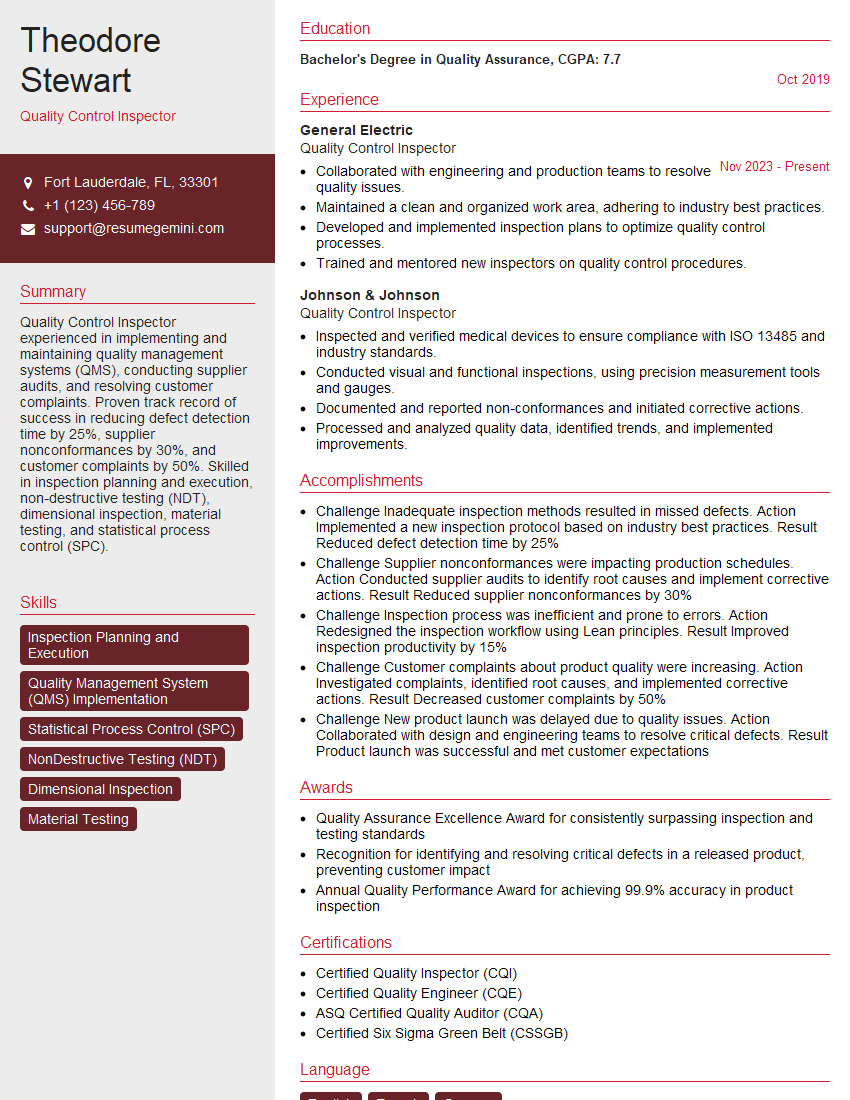
Mastering Medical Device Manufacturing Processes is crucial for career advancement in this highly regulated and demanding field. A strong understanding of these processes significantly enhances your marketability and opens doors to more challenging and rewarding roles. To maximize your job prospects, creating a compelling and ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume that highlights your skills and experience effectively. Examples of resumes tailored to Medical Device Manufacturing Processes are available to guide you through the process. Invest time in crafting a strong resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good