Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Orthotics Fabrication interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Orthotics Fabrication Interview
Q 1. Describe your experience with different casting materials used in orthotics fabrication.
My experience encompasses a wide range of casting materials used in orthotics fabrication, each with its own advantages and disadvantages. The choice depends heavily on the patient’s needs, the type of orthotic being made, and the practitioner’s preference.
- Plaster of Paris: A classic, inexpensive material, it’s known for its strength and ability to capture fine details. However, it’s messy, has a longer setting time, and can be irritating to some patients. I use it primarily for initial models in less demanding cases.
- Foam Casting: These materials offer excellent patient comfort during the casting process because they are lightweight and conform easily. They are particularly beneficial for patients with sensitive skin or those who find traditional plaster uncomfortable. However, they may not capture the finest details as precisely as plaster. I often prefer this for patients with edema or those requiring multiple casts.
- Pliable Plastic Sheets (e.g., Thermoplastic): These are excellent for creating positive models for vacuum-formed orthotics, providing a smooth and consistent surface for the final product. This method is efficient and produces predictable results. They’re also great for creating custom modifications on pre-fabricated orthotics.
- Scanning Systems: Digital scanning systems are becoming increasingly common, eliminating the need for traditional casting entirely. This approach offers accurate, repeatable results with minimal patient discomfort and faster turnaround times. I frequently use these systems, particularly for complex cases requiring precise measurements and intricate designs.
I’ve found that a thorough understanding of each material’s properties is critical in selecting the best option for each patient. For example, a patient with significant edema might require a foam cast to avoid discomfort and pressure, while a patient requiring a very precise orthotic might benefit from a digital scan.
Q 2. Explain the process of creating a custom foot orthotic from initial patient assessment to final product.
Creating a custom foot orthotic is a meticulous process that begins with a comprehensive patient assessment and culminates in a precisely fitted device. The steps are as follows:
- Patient History and Examination: I start by gathering detailed medical history, understanding the patient’s condition (e.g., plantar fasciitis, bunions, arthritis), their activity level, and any previous treatments. A thorough physical examination of the feet and lower limbs helps identify structural deformities, gait abnormalities, and other relevant factors.
- Foot Tracing and Measurement: Accurate measurements are crucial. I obtain detailed foot outlines and measurements using a variety of tools, including plantographs and calipers. These measurements guide the design of the orthotic and ensure proper size and shape.
- Casting (or Scanning): Depending on the patient’s needs and my preferred method, I take a plaster, foam, or digital scan of the patient’s foot. The cast or scan provides a three-dimensional representation of the foot structure.
- Model Creation: From the cast or scan, a positive model of the foot is created using appropriate techniques. For traditional plaster casts, I would create a positive model using a molding material. For digital scans, I would use CAD software to create a virtual 3D model.
- Design and Modification: Using the model, I design the orthotic, considering the patient’s specific needs and biomechanical requirements. This may involve adding support, cushioning, or other modifications as needed. I would use CAD/CAM software to design the orthotic if using a digital workflow.
- Material Selection: Selecting the right materials is crucial and involves considering the patient’s condition, activity level, and desired level of support and cushioning. I consider factors like flexibility, durability, and weight.
- Fabrication: I fabricate the orthotic using various techniques, including milling (with CAD/CAM), vacuum forming, or manual shaping. Quality control is paramount at this stage.
- Fitting and Adjustment: The orthotic is carefully fitted to the patient’s foot, and adjustments are made to ensure optimal comfort and function. I’ll observe the patient’s gait and make any necessary modifications.
- Patient Education and Follow-up: I provide the patient with instructions on how to care for the orthotic and address any questions or concerns. Follow-up appointments are scheduled to monitor the orthotic’s effectiveness and make further adjustments if needed.
Q 3. What are the key considerations when selecting materials for a given orthotic design?
Material selection is a critical aspect of orthotic design, directly impacting the orthotic’s effectiveness, comfort, and durability. Several key considerations guide my choices:
- Patient Needs: The patient’s condition, activity level, weight, and any existing skin conditions significantly influence material selection. For example, a patient with diabetes might need a very low-shear material to prevent skin breakdown.
- Orthotic Design: Different designs (e.g., UCBL, accommodative, semi-rigid) have specific material requirements. A rigid orthotic will require a more durable material than a flexible one.
- Mechanical Properties: Materials need to have the right balance of flexibility, rigidity, and cushioning. I consider factors like density, tensile strength, and shear modulus. For example, a material with a high tensile strength is needed for a supportive orthotic, while a material with high shear modulus provides stability.
- Biocompatibility: The material must be compatible with the patient’s skin, minimizing the risk of allergic reactions or irritations. Materials must be non-toxic and hypoallergenic. I will often carefully consider the material options for patients with known allergies or sensitivities.
- Durability and Longevity: The material must be durable enough to withstand daily use without significant wear and tear. The lifespan of the orthotic and the level of wear a patient’s activities will impose factor into my selection.
- Cost: The cost of different materials can vary significantly. This is often balanced with the patient’s budget and the long-term benefits of investing in higher-quality, more durable materials.
For example, a patient with plantar fasciitis who is relatively sedentary might benefit from a semi-rigid orthotic made from ethylene vinyl acetate (EVA) for its cushioning and flexibility. A more active patient with severe foot deformities might require a more rigid orthotic made from polypropylene or carbon fiber.
Q 4. How do you ensure proper fit and function of an orthotic device?
Ensuring proper fit and function is paramount. I employ several strategies to achieve this:
- Precise Measurements and Casting: Accurate measurements are fundamental to a proper fit. I diligently check the fit of the cast before proceeding to the model-making stage. I meticulously review the digital scan to confirm there are no artifacts that would affect the final device.
- Careful Orthotic Design: The design itself must accommodate the patient’s foot shape and biomechanical needs. Pressure mapping systems may be used to identify pressure points before and after modification.
- Material Selection: Selecting the appropriate material is crucial for both comfort and support. I carefully consider the patient’s individual needs to avoid compromising proper fit.
- Multiple Fittings: I provide multiple fitting sessions to ensure a comfortable and functional fit. Adjustments are made based on patient feedback and my observations of gait and weight-bearing.
- Gait Analysis (When Needed): For complex cases, gait analysis might be used to assess how the patient moves while wearing the orthotic, providing valuable insights for adjustments and modifications.
- Patient Education: I educate the patient on how to properly wear and care for the orthotic, which is essential for optimal function and to prevent issues like pressure sores.
For example, I had a patient with a Charcot foot who required a custom-molded orthotic. Through multiple fittings and careful modifications based on pressure mapping, we were able to achieve an excellent fit that prevented pressure sores and improved ambulation.
Q 5. Explain your experience with different orthotic designs (e.g., UCBL, semi-rigid, accommodative).
My experience covers a broad range of orthotic designs, each tailored to different needs:
- UCBL (University of California Biomechanics Laboratory) Orthotics: These are highly customized, often rigid orthotics designed to control rearfoot motion and provide substantial support. I use them for patients with significant biomechanical abnormalities, such as pes cavus or pes planus. The design principles of the UCBL orthotic system allow me to address rearfoot valgus or varus, forefoot varus or valgus, and other common biomechanical issues. Proper assessment and understanding of the foot’s mechanics are crucial for selecting and modifying a UCBL orthotic.
- Semi-Rigid Orthotics: These offer a balance between support and flexibility, making them suitable for a wider range of conditions. They are often used for patients with mild to moderate biomechanical issues or those who require some cushioning. EVA foam is a common material for this style, allowing for variations in thickness and flexibility to meet individual needs.
- Accommodative Orthotics: These are typically soft, flexible orthotics designed primarily for comfort and pressure relief. They are often used for patients with foot ulcers, diabetes, or other conditions that require cushioning and protection. Various materials, including soft foams and gel padding, are used. A proper assessment of plantar pressure is crucial for design and modification of these types of orthotics.
The selection of orthotic design depends entirely on the patient’s needs, diagnosis, and activity level. It’s crucial to remember that the best orthotic is the one that effectively addresses the patient’s specific biomechanical problems and enhances their overall comfort and functionality.
Q 6. Describe your proficiency in using CAD/CAM software for orthotics design.
I am highly proficient in using CAD/CAM software for orthotics design. My experience includes using several leading programs in the field. These systems allow me to create precise, three-dimensional models of orthotics, enabling the creation of highly customized devices based on patient-specific measurements and scans.
The workflow typically involves:
- Digital Scanning/Image Acquisition: The process begins by acquiring digital representations of the patient’s feet, usually through 3D scanning systems, which generate a point cloud.
- Model Creation and Manipulation: Using CAD software, I refine the point cloud data, correcting for minor imperfections and creating a smooth, accurate surface representation of the patient’s foot.
- Orthotic Design: I then design the orthotic using the 3D model of the foot as a base. This allows for precise placement of support structures, cushioning, and other modifications to address the patient’s specific needs. The ability to visualize the design in 3D, and even virtually ‘fit’ the orthotic, is a major advantage.
- CAM (Computer-Aided Manufacturing): Once the design is finalized, I can use the CAM software to generate instructions for the milling machine. The CAM system translates the digital design into instructions that the milling machine uses to carve the orthotic from a block of material.
- Fabrication and Quality Control: The milling machine creates the orthotic, and I perform a final quality check to ensure the orthotic meets the design specifications and is free from any defects.
CAD/CAM technology significantly improves accuracy, efficiency, and consistency in orthotics fabrication, leading to better patient outcomes.
Q 7. How do you address common patient issues such as pressure sores or skin irritations related to orthotics?
Pressure sores and skin irritations are common issues related to orthotic use. Addressing them requires a multi-pronged approach:
- Proper Fitting: The most crucial step is ensuring a proper fit. Poorly fitting orthotics are the primary cause of these problems. Regular follow-up appointments help monitor fit and make timely adjustments.
- Material Selection: Selecting biocompatible materials with low-shear properties is essential. Materials that wick away moisture and allow for good breathability can reduce the risk of skin irritation. Materials with varying degrees of cushioning and rigidity are important for pressure redistribution.
- Padding and Modifications: Adding padding to pressure points identified through pressure mapping can significantly reduce the risk of sores. I might use materials like gel pads, foam, or other specialized padding. Custom modifications of the orthotic itself may be necessary to redistribute pressure and eliminate hotspots.
- Patient Education: Educating patients on proper hygiene, sock selection (moisture-wicking fabrics are recommended), and regular inspection of their feet is crucial. They should report any discomfort promptly.
- Skin Care: Recommending appropriate skin care products and strategies, like the use of moisturizing lotions and barrier creams, is important to maintain skin health. In cases of severe skin breakdown, I would work collaboratively with other healthcare professionals.
- Temporary Removal: If a pressure sore or irritation develops, the orthotic may need to be temporarily removed to allow the skin to heal. The orthotic may require further modification to prevent recurrence of the problem.
For example, I recently worked with a patient who developed a pressure sore under their orthotic. By using pressure mapping to pinpoint the exact location of the pressure, making adjustments to the design, and adding additional padding, we were able to resolve the issue and prevent recurrence.
Q 8. What are the common biomechanical principles you consider when designing an orthotic?
Designing effective orthotics hinges on understanding fundamental biomechanical principles. We consider factors influencing gait, posture, and joint function. This includes:
- Lever Arm Lengths: The length of bones and the muscles acting on them significantly impact forces and moments at joints. For example, a longer lever arm on a foot requires more substantial support to control motion.
- Joint Kinetics and Kinematics: Analyzing joint angles (kinematics) and the forces acting on them (kinetics) helps determine the necessary support and control. Excessive pronation, for example, requires medial arch support.
- Weight Bearing: The distribution of weight across the foot and lower limb during various activities informs the design. A high-impact activity like running necessitates different orthotic support than walking.
- Muscle Function: Orthotics can either assist or restrict muscle action depending on the condition. For instance, a weak tibialis posterior muscle might benefit from medial arch support to aid in preventing collapse.
- Ground Reaction Forces: Understanding how forces from the ground affect the body, especially during gait, is crucial. This directs design features like heel cushioning or metatarsal pads.
In essence, we aim to create an orthotic that works synergistically with the body’s natural biomechanics, promoting efficient movement and reducing stress on compromised structures.
Q 9. Explain your experience with modifying prefabricated orthotics.
Modifying prefabricated orthotics requires precision and a thorough understanding of material properties. I frequently adapt prefabricated devices to address specific patient needs that go beyond standard designs. This often involves:
- Heat Molding: Using a heat gun to carefully reshape the orthotic to conform better to the patient’s foot. This is crucial for achieving optimal alignment and pressure distribution. I have successfully used this technique numerous times to adjust the heel cup depth or to improve longitudinal arch support in patients with pes planus (flat feet).
- Grinding and Shaping: Precise trimming with appropriate tools to remove excess material and create more specific contours. This is essential when accommodating bony prominences or other anatomical variations. For example, I’ve frequently had to grind down the medial aspect of a prefabricated orthotic to accommodate a bunion.
- Adding Components: Incorporating supplementary elements like heel wedges, metatarsal pads, or longitudinal arch supports to enhance the orthotic’s functional capabilities. This customization can address specific biomechanical needs, such as accommodating a leg-length discrepancy or correcting excessive pronation.
- Material Additions: Carefully applying additional layers of suitable material to provide targeted support or cushioning in specific areas. This may include adding felt padding to reduce friction or using foam to improve pressure relief in areas of high stress.
Careful measurement and assessment of the patient’s foot are paramount before, during and after any modification. Safety is a priority, and I always ensure the modifications don’t compromise the structural integrity of the orthotic.
Q 10. How do you manage and troubleshoot manufacturing errors during orthotics fabrication?
Manufacturing errors are unfortunately inevitable. My approach involves a systematic troubleshooting process:
- Immediate Visual Inspection: The first step involves carefully examining the finished orthotic for any visible defects, such as cracks, inconsistencies in material thickness, or misalignment of components.
- Comparison to Prescription: I meticulously compare the final product with the initial prescription and casting to identify discrepancies. This often highlights issues with heat molding or material application.
- Patient Feedback: Following the initial fitting, I gather feedback from the patient regarding comfort, fit, and functional improvement. This often reveals subtle issues not detected during visual inspection.
- Corrective Action: Depending on the nature of the error, the corrective actions can range from minor adjustments (e.g., slight trimming) to remaking the orthotic entirely. Documenting the error and the corrective measures taken is crucial for quality control.
- Root Cause Analysis: For recurring errors, I conduct a thorough analysis to identify the underlying cause, whether it’s a problem with the equipment, materials, or my own technique. This proactive approach helps prevent future issues.
Through this structured approach, I ensure both quality and patient satisfaction. A well-documented process is fundamental to resolving manufacturing errors effectively and efficiently.
Q 11. Describe your experience with different types of thermoplastic materials and their applications.
My experience encompasses a range of thermoplastic materials, each with specific applications:
- Polyethylene (PE): A versatile and cost-effective material, ideal for simple orthotics and modifications. Its flexibility makes it suitable for accommodating mild deformities.
- Ethylene Vinyl Acetate (EVA): Offers superior cushioning and shock absorption, making it a preferred choice for high-impact activities or patients with significant plantar pressure issues. I often use this for sports orthotics and diabetic footwear.
- Polypropylene (PP): Known for its high strength and rigidity, polypropylene is suited for orthotics requiring significant structural support, such as those for patients with severe foot deformities or those requiring significant arch support.
- Thermoplastic Polyurethane (TPU): This offers excellent durability, flexibility, and shock absorption. Its superior strength and flexibility make it well-suited for orthotics that need to withstand repeated stress. I often use this for high-performance athletic orthotics.
The material selection critically depends on the patient’s needs, the level of support required, and the activity level. For example, a patient with a simple plantar fasciitis case might benefit from an EVA orthotic, while a patient with severe Charcot-Marie-Tooth disease would likely require a more rigid polypropylene device.
Q 12. How do you maintain quality control throughout the orthotics fabrication process?
Maintaining quality control is a continuous process that begins with the initial patient assessment and extends through to post-fabrication follow-up. My approach includes:
- Accurate Casting and Measurements: Precise measurements and casting techniques ensure the orthotic accurately reflects the patient’s foot structure and biomechanics. This involves utilizing proper casting materials and techniques to capture fine details.
- Material Selection and Storage: Appropriate materials are chosen based on patient-specific needs and stored under optimal conditions to maintain their structural integrity. Proper storage helps prevent material degradation and ensures consistent performance.
- Strict Adherence to Protocols: The fabrication process strictly follows established protocols, including heating times and pressures during molding, ensuring consistent results. Standardized procedures contribute to repeatability and reliability.
- Regular Equipment Calibration: Calibration checks are performed on all fabrication equipment to ensure accuracy and precision. Well-maintained equipment is key to producing consistently high-quality orthotics.
- Post-Fabrication Quality Checks: Each completed orthotic undergoes a rigorous quality control check to identify and correct any deviations from the initial prescription or any manufacturing errors.
By maintaining a commitment to standardized procedures and consistent quality checks, I ensure the delivery of high-quality orthotics that meet both clinical needs and patient expectations.
Q 13. What are the limitations of different orthotic materials and designs?
All orthotic materials and designs have limitations. Some key considerations include:
- Material Durability: Even the most durable materials can degrade over time with repeated use and exposure to environmental factors. This necessitates periodic orthotic replacement, especially for high-impact activities.
- Material Flexibility: While flexibility is advantageous in some cases, excessive flexibility can compromise support. Conversely, insufficient flexibility can limit comfort and movement.
- Design Limitations: Certain orthotic designs may not be suitable for all foot types or conditions. For example, a rigid orthotic may not be suitable for patients with significant edema or neuropathy.
- Patient Compliance: Orthotic effectiveness depends heavily on patient compliance. Poor adherence to wearing schedules or improper use can negatively impact outcomes.
- Skin Irritation: Certain materials may trigger skin irritation in some individuals, necessitating material changes or the incorporation of cushioning layers.
A thorough understanding of these limitations is crucial in selecting the appropriate material and design to optimize the balance between support, comfort, and patient compliance.
Q 14. How do you ensure the hygiene and sterilization of orthotics?
Maintaining the hygiene and sterilization of orthotics is crucial to prevent infection and ensure patient safety. My approach emphasizes:
- Patient Education: Educating patients about proper hygiene practices, including regular cleaning, is paramount. This includes advising them to wash the orthotics with soap and water and to allow them to air dry completely.
- Material Selection: Selecting materials that are easy to clean and resistant to microbial growth. Materials like polypropylene are preferable to porous materials which retain moisture.
- Appropriate Cleaning Solutions: Using mild soap and water for cleaning and avoiding harsh chemicals that could damage the orthotic material. For more thorough cleaning, appropriate disinfectants can be used following manufacturer’s instructions.
- Regular Inspection: Regularly inspecting orthotics for signs of wear and tear, discoloration, or odor. This allows for early identification and replacement if necessary.
- Patient-Specific Instructions: Providing individualized instructions on cleaning and hygiene tailored to the specific orthotic material and the patient’s individual needs and health conditions.
By emphasizing these strategies, we minimize the risk of infection and maintain the integrity of the orthotic, ensuring patient health and comfort.
Q 15. Describe your experience working with patients with various foot pathologies.
Throughout my career, I’ve worked with a diverse patient population presenting with a wide range of foot pathologies. This includes common conditions like plantar fasciitis, metatarsalgia, and hallux valgus (bunions), as well as more complex issues such as diabetic foot ulcers, Charcot-Marie-Tooth disease, and rheumatoid arthritis. Each patient presents unique challenges, requiring a customized approach to orthotic design and fabrication. For example, a patient with plantar fasciitis might need a device with a firm medial longitudinal arch support to alleviate heel pain, whereas a patient with a diabetic foot ulcer might require a highly accommodative orthotic to offload pressure from the affected area and prevent further complications. I’ve also worked with patients post-surgical procedures requiring specific modifications to their orthotics to facilitate healing and prevent recurrence. My experience spans different age groups, activity levels and body weights, allowing me to tailor my approach to individual patient needs.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of the role of orthotics in managing specific conditions (e.g., plantar fasciitis, diabetes).
Orthotics play a crucial role in managing various foot conditions by providing support, cushioning, and correcting biomechanical imbalances. In plantar fasciitis, for instance, orthotics help reduce strain on the plantar fascia by providing arch support and cushioning the heel. This reduces inflammation and pain. For patients with diabetes, custom orthotics are essential for preventing foot ulcers. They redistribute pressure away from high-risk areas like the metatarsal heads, reducing the risk of injury. Proper offloading is critical to prevent complications like infection and amputation. In cases of diabetic neuropathy, orthotics can provide cushioning and support to compensate for reduced sensation and protect the feet from injury. The design specifics vary depending on the severity and type of the condition. For example, a patient with severe diabetic neuropathy might need a total contact cast orthotic for maximal pressure redistribution, whereas a mild case might benefit from a more functional orthotic with arch support and cushioning. The goal is always to improve function, reduce pain, and prevent further complications.
Q 17. How do you communicate effectively with patients, physicians, and other healthcare professionals?
Effective communication is paramount in my profession. I believe in a patient-centered approach, taking the time to actively listen to the patient’s concerns, understand their lifestyle, and explain the treatment plan clearly and concisely, avoiding overwhelming medical jargon. I use visual aids like anatomical diagrams to illustrate points and ensure the patient understands the purpose and function of their orthotics. When communicating with physicians, I maintain a professional and collaborative relationship, providing detailed reports and progress updates. This often involves providing clinical photos and digital pressure mapping data. I always ensure that my communication with all stakeholders is detailed, accurate and reflects patient confidentiality. For example, I routinely update the referring physician on the patient’s progress using secure digital communication methods.
Q 18. Describe your experience with documentation and record-keeping related to orthotics fabrication.
Meticulous documentation is critical for legal compliance, patient care, and quality control. My record-keeping includes comprehensive patient history, including medical diagnoses, treatment goals, initial casting notes, material specifications for the orthotic, adjustment details, and follow-up visits. All patient information is stored securely and confidentially, adhering to HIPAA guidelines. I use electronic medical record (EMR) systems to maintain accurate and easily accessible records. In addition to electronic records, I also maintain a physical file of each patient, including impressions, photos, and copies of all relevant medical records. This ensures redundancy and accessibility in various situations.
Q 19. What is your experience with different types of orthotic adjustments?
My experience encompasses a broad range of orthotic adjustments, from minor modifications to major revisions. Minor adjustments may involve trimming excess material or making slight alterations to the heel or forefoot. Major adjustments might involve remolding portions of the orthotic, altering the arch support, or adding accommodative features to address pressure areas identified through clinical observation or pressure mapping. I am proficient in various techniques for modifying different orthotic materials, including thermoplastic materials, carbon fiber and other composite materials. The choice of adjustment method is determined by the patient’s specific needs and the nature of the problem. For instance, if a patient is experiencing pain under the metatarsal heads, I might adjust the metatarsal pad to redistribute pressure. If a patient is experiencing excessive pronation, I might increase the medial longitudinal arch support. Each adjustment is meticulously documented to track progress and ensure the orthotic effectively addresses the patient’s needs.
Q 20. Explain your understanding of relevant safety regulations and procedures in orthotics fabrication.
Safety is a top priority in orthotics fabrication. I am well-versed in OSHA regulations regarding workplace safety, including proper handling of materials, use of personal protective equipment (PPE) like respirators and safety glasses during material preparation, and safe disposal of biohazardous waste. I also follow strict sterilization procedures to prevent the spread of infection. I meticulously maintain and regularly calibrate all equipment to ensure accuracy and safety. Furthermore, I strictly adhere to infection control protocols when handling casts and orthotics to minimize the risk of cross-contamination. This involves proper hand hygiene, use of barrier protection, and appropriate disinfection techniques. Any potential hazards associated with the materials I use are thoroughly researched and appropriate safety measures are always in place.
Q 21. Describe your experience with the use of pressure mapping systems in orthotics.
Pressure mapping systems are invaluable tools in orthotics. They provide objective data on pressure distribution under the foot, allowing for precise identification of high-pressure areas and accurate orthotic design. I have extensive experience using various pressure mapping systems, both static and dynamic. This data helps in identifying areas of excessive pressure that contribute to pain or ulceration. I use this information to customize the orthotic design, focusing on pressure relief in problem areas. For example, if a pressure map reveals a high-pressure area under the metatarsal heads, I can modify the orthotic to incorporate a metatarsal pad or modify the shape to redistribute the pressure. This precise approach ensures more effective and personalized orthotic treatment, leading to improved patient outcomes. The data also helps in the objective assessment of the effectiveness of the orthotic after fabrication and adjustments.
Q 22. How do you handle unexpected challenges or changes in the fabrication process?
Handling unexpected challenges in orthotics fabrication requires a methodical approach. Think of it like building a house – sometimes the foundation isn’t perfectly level, or the materials arrive damaged. My strategy focuses on three key steps: assessment, adaptation, and documentation.
First, I carefully assess the situation. What exactly went wrong? Is it a material defect, a measurement error, or a change in patient needs? For example, if the heat-moldable plastic arrives cracked, I wouldn’t proceed; I’d immediately contact the supplier for a replacement and document the issue. If the patient experiences unexpected pain, I meticulously re-evaluate the fit and pressure points.
Second, I adapt my approach. This might involve adjusting the design, using alternative materials, or modifying my fabrication techniques. Perhaps I need to add extra padding to alleviate pressure, or use a different adhesive to better secure a component. I always prioritize patient comfort and functional outcome.
Finally, I thoroughly document the entire process – including the initial problem, my corrective actions, and the final result. This documentation is crucial for quality control and also helps me learn from my experiences. This detailed record ensures that I can avoid similar issues in the future and facilitates better communication with colleagues and the referring clinician.
Q 23. What is your experience with using different types of adhesives in orthotics?
My experience with adhesives in orthotics is extensive. Different adhesives are suited to different materials and applications. I’m proficient in using a range of adhesives, including cyanoacrylates (super glues), polyurethane adhesives, and acrylic adhesives. Each has its strengths and weaknesses.
Cyanoacrylates are excellent for quick bonding of small components, but their rigidity can be a drawback for certain applications where flexibility is required. Polyurethane adhesives offer superior strength and flexibility, making them ideal for bonding larger components or materials with varying properties. Acrylic adhesives offer a good balance of strength, flexibility, and ease of application. However, cure time can vary depending on the type of acrylic and environmental conditions.
Selecting the right adhesive is critical. For instance, when constructing a custom foot orthotic from carbon fiber and EVA foam, I would likely use a strong, flexible polyurethane adhesive to ensure durable and comfortable bonding. If I’m working with delicate components like straps or thin foams, I might use a cyanoacrylate carefully, in small quantities to avoid excess glue causing discomfort.
Q 24. Explain your proficiency in using hand tools and power tools commonly used in orthotics fabrication.
Proficiency with both hand and power tools is fundamental in orthotics fabrication. My skills encompass the safe and efficient use of a wide variety of tools, ranging from basic hand tools like shears, rasps, files, and rotary tools to more advanced power tools like band saws, routers, and heat guns.
Hand tools allow for precise adjustments and finishing work, critical for achieving a customized and comfortable fit. For instance, I use rasps and files to refine the shape and contours of an orthotic, ensuring a smooth and even surface. Rotary tools are invaluable for creating intricate details or removing small amounts of material with precision.
Power tools are essential for more efficient material removal and shaping, especially when working with larger or more rigid materials. A band saw is ideal for accurately cutting sheets of plastics or foams to the desired size and shape. A router is used to create channels or grooves in orthotic components. Heat guns are important for shaping and molding thermoplastic materials. Safety is paramount. I always adhere strictly to safety procedures, wear appropriate personal protective equipment (PPE), and maintain my tools in excellent working condition.
Q 25. How do you stay up-to-date with the latest advancements in orthotics and technology?
Staying current in the rapidly evolving field of orthotics requires a proactive and multi-faceted approach. I actively engage in several strategies to maintain my expertise.
- Professional Organizations: I am a member of [Name relevant professional organizations], participating in conferences, workshops, and webinars to learn about the latest research, materials, and techniques.
- Peer-Reviewed Journals and Publications: I regularly read peer-reviewed journals such as the Journal of Orthotic and Prosthetic Technology and other relevant publications to stay abreast of groundbreaking advancements.
- Continuing Education Courses: I actively pursue continuing education courses to improve my knowledge and skills in specialized areas like biomechanics, CAD/CAM technology, and new materials science.
- Industry Events and Trade Shows: Attending industry trade shows and events provides a great opportunity to network with other professionals and see firsthand the latest technologies and innovations in the field.
- Online Resources: I utilize reputable online resources, including reputable websites and professional forums, to access current information and engage in professional discussions.
This multifaceted approach ensures that I remain at the forefront of orthotics fabrication.
Q 26. Describe your problem-solving skills related to fitting and adjusting orthotics.
My problem-solving skills in fitting and adjusting orthotics are honed by years of experience and a commitment to patient-centric care. The process often involves a combination of observation, assessment, and iterative adjustments.
First, I carefully observe the patient’s gait and posture, identifying any abnormalities or areas of concern. Then, I assess the fit of the orthotic, checking for pressure points, heel slippage, and proper alignment. I might use pressure mapping systems or other diagnostic tools to gather objective data.
Based on my observations and assessments, I make targeted adjustments. These can range from minor modifications like adding padding or trimming excess material to more substantial changes involving reshaping or remaking parts of the orthotic. I continually assess patient feedback, making iterative changes until optimal comfort and function are achieved. A recent example involved a patient with a severe bunion. The initial orthotic caused excessive pressure, leading to discomfort. By meticulously adjusting the depth and shape of the medial portion using a combination of rasps and heat molding, I achieved a much better fit, relieving the pressure and improving the patient’s mobility. This iterative approach, coupled with close patient communication, is crucial for successful outcomes.
Q 27. What are your salary expectations?
My salary expectations are commensurate with my experience and skills, and align with the industry standards for a highly skilled Orthotics Fabricator with my level of expertise. I am open to discussing a competitive compensation package that reflects my value and contributions to your team.
Q 28. What are your long-term career goals in orthotics fabrication?
My long-term career goals involve continued growth and leadership within the field of orthotics fabrication. I aspire to become a highly proficient and respected expert, contributing to advancements in the field through innovation and mentorship. This includes possibly specializing in a particular area such as pediatric orthotics or advanced CAD/CAM technology. I also see myself mentoring younger professionals and contributing to the advancement of the field through participation in research projects or publication of findings.
Key Topics to Learn for Orthotics Fabrication Interview
- Casting Techniques: Understanding various casting methods (plaster, foam, digital scanning), their applications, and limitations. Consider the implications of choosing one method over another for specific patient needs.
- Material Selection: Knowledge of different orthotic materials (plastics, thermoplastics, foams, etc.), their properties (strength, flexibility, durability), and appropriate selection based on the patient’s diagnosis and activity level. Be prepared to discuss the pros and cons of each.
- Design Principles: Grasping the biomechanical principles behind orthotic design, including pressure distribution, alignment, and support. Be ready to discuss how design choices impact patient outcomes.
- Fabrication Processes: Detailed knowledge of the entire fabrication process, from initial casting to final finishing and adjustments. This includes trimming, heating, shaping, and polishing techniques.
- Quality Control and Assessment: Understanding procedures for ensuring the quality and fit of the finished orthotic, including quality checks and potential adjustments. Be prepared to discuss how you identify and address issues.
- Patient Communication and Collaboration: Highlighting the importance of clear communication with patients, clinicians, and other healthcare professionals to understand requirements and ensure patient satisfaction. Discuss effective collaboration techniques.
- Safety Protocols and Hygiene: Demonstrate awareness and adherence to safety regulations and hygienic practices within the orthotics fabrication lab. Be ready to discuss relevant safety procedures.
- Troubleshooting and Problem-Solving: Showcase your ability to identify and resolve common issues encountered during the fabrication process, demonstrating practical problem-solving skills.
- Technological Advancements: Familiarity with current trends and technologies in orthotics fabrication, such as CAD/CAM systems and 3D printing. Discuss how these technologies are impacting the field.
Next Steps
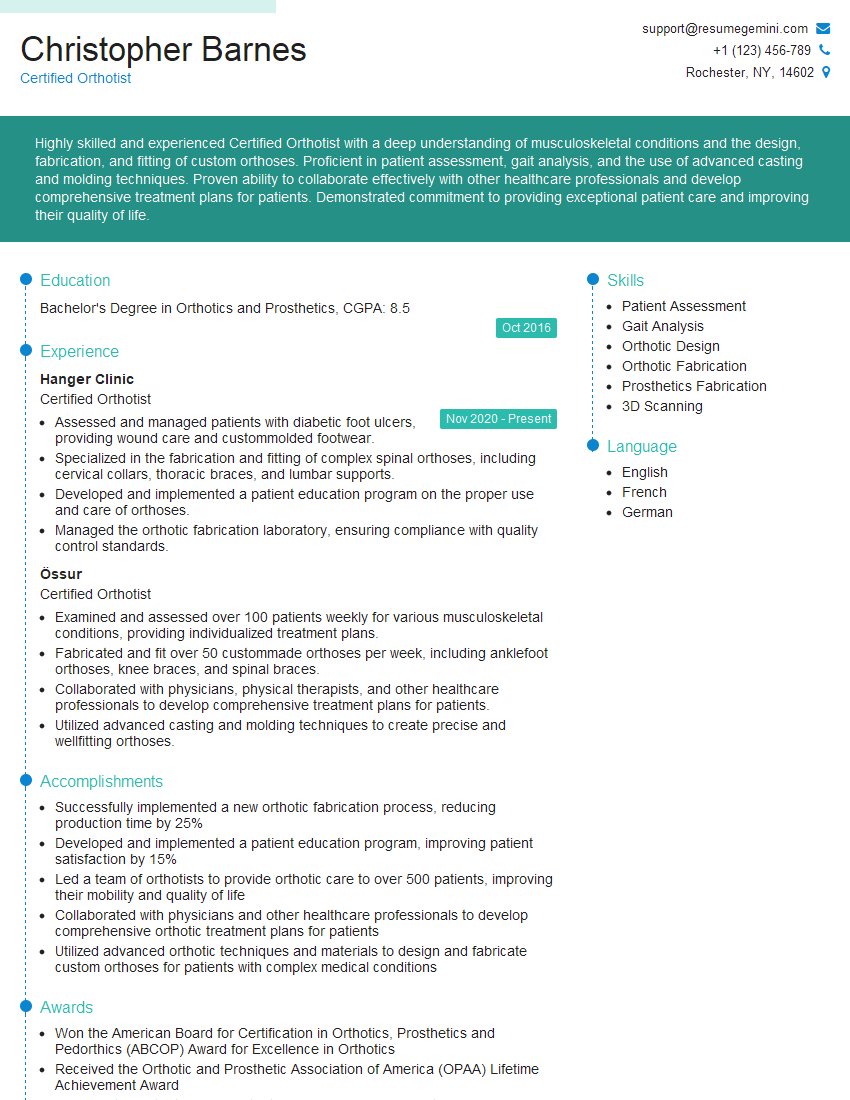
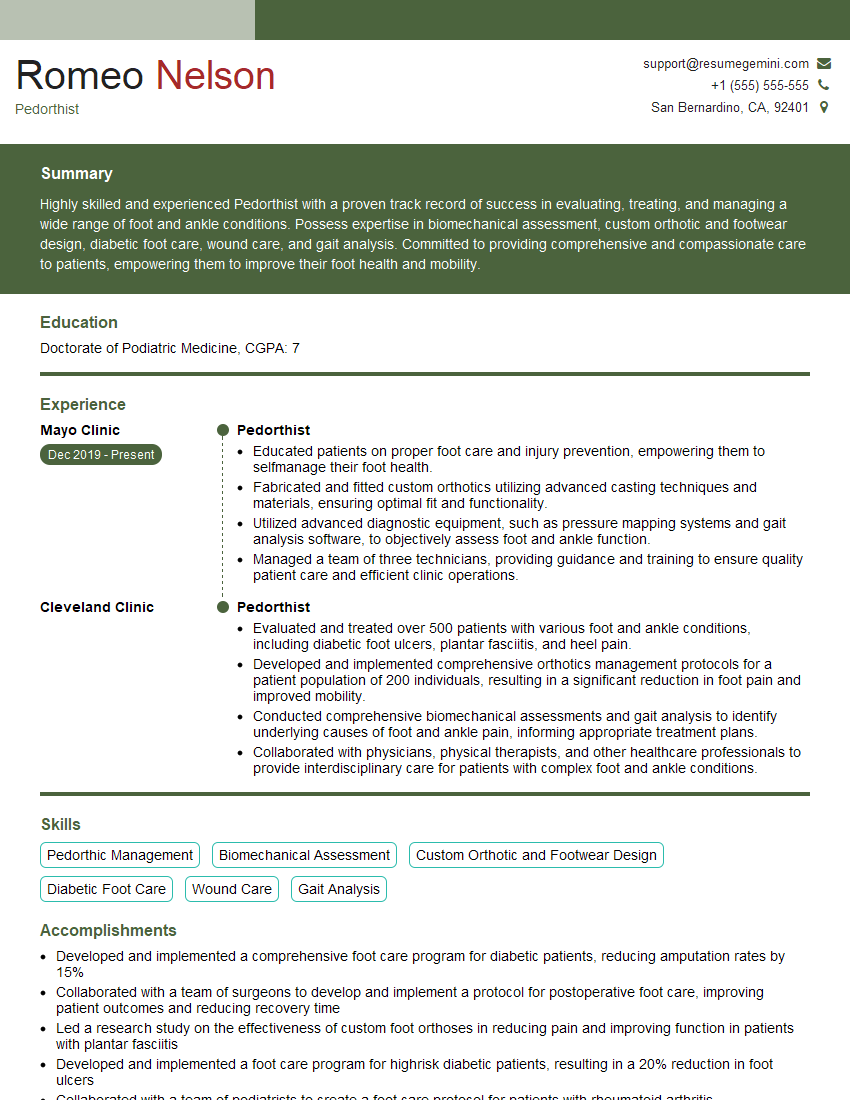
Mastering Orthotics Fabrication opens doors to a rewarding career with opportunities for specialization and advancement. A strong foundation in these key areas will significantly improve your interview performance and career prospects. To maximize your chances, focus on creating an ATS-friendly resume that effectively showcases your skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Examples of resumes tailored to Orthotics Fabrication are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good