Preparation is the key to success in any interview. In this post, we’ll explore crucial Patient Care and Assessment interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Patient Care and Assessment Interview
Q 1. Describe your process for conducting a comprehensive patient assessment.
A comprehensive patient assessment is a systematic process of collecting and analyzing data about a patient’s health status. It forms the foundation for developing a safe and effective care plan. My process involves several key steps:
- Gathering Subjective Data: This involves actively listening to the patient’s description of their symptoms, medical history, lifestyle, and concerns. I use open-ended questions to encourage detailed responses and build rapport. For example, instead of asking ‘Do you have pain?’, I might ask ‘Can you describe the pain you’re experiencing?’
- Collecting Objective Data: This step involves performing a physical examination, reviewing medical records, and obtaining relevant laboratory and diagnostic test results. I meticulously observe vital signs (temperature, pulse, respiration, blood pressure, oxygen saturation), assess skin turgor, listen to heart and lung sounds, and palpate the abdomen, adapting my approach based on the patient’s presenting complaint and overall health.
- Analyzing Data: After gathering both subjective and objective data, I analyze the information to identify patterns, inconsistencies, and potential risk factors. I compare the patient’s current condition with their baseline health status to determine the severity and urgency of their needs. For example, a sudden drop in blood pressure could indicate a serious complication requiring immediate intervention.
- Formulating a Nursing Diagnosis: Based on the data analysis, I formulate nursing diagnoses using a standardized framework (e.g., NANDA-I). These diagnoses identify the patient’s health problems and their related factors. This step guides the development of targeted interventions.
- Planning and Implementing Interventions: A care plan is developed outlining specific, measurable, achievable, relevant, and time-bound (SMART) goals. Interventions are implemented based on the care plan, including medication administration, wound care, patient education, and support.
- Evaluating Outcomes: The effectiveness of the interventions is continuously monitored and evaluated, and the care plan is modified as needed based on the patient’s response to treatment. This is a cyclical process; ongoing assessment informs adjustments to the care plan.
Q 2. How do you prioritize patient needs in a fast-paced environment?
Prioritizing patient needs in a fast-paced environment requires a structured approach. I use the ABCDE method (Airway, Breathing, Circulation, Disability, Exposure) to triage patients based on the urgency of their needs. This helps to quickly identify life-threatening situations and allocate resources efficiently. For example, a patient with respiratory distress takes precedence over a patient with a minor laceration. Beyond ABCDE, I utilize a combination of strategies:
- Prioritization Frameworks: I use Maslow’s Hierarchy of Needs and the urgency/importance matrix to categorize patient needs. This helps to focus on essential tasks first, ensuring that immediate threats to life and well-being are addressed before less urgent issues.
- Time Management Techniques: Efficient time management is crucial. Techniques like task delegation, setting priorities, clustering similar tasks, and using checklists help to streamline workflows and minimize delays.
- Clinical Judgement & Intuition: Experience plays a vital role. My clinical judgment, informed by years of practice, helps me anticipate potential problems and quickly adapt to changing circumstances. It guides my decisions on prioritizing multiple patients’ needs simultaneously.
- Effective Communication: Open and efficient communication with colleagues and the multidisciplinary team is critical. Clearly communicating patient needs and priorities allows for effective collaboration and timely interventions.
Q 3. Explain your experience with documenting patient care.
Accurate and comprehensive documentation of patient care is crucial for continuity of care, legal protection, and improved patient outcomes. My approach to documentation emphasizes accuracy, completeness, and timeliness. I use the SOAP note method (Subjective, Objective, Assessment, Plan), documenting all interactions and observations concisely and clearly. I include:
- Specific Details: Instead of general statements, I provide specific details about the patient’s condition and the care provided. For instance, instead of ‘Patient is in pain,’ I write ‘Patient reports sharp, stabbing pain in the right lower quadrant, rated 8/10 on the pain scale.’
- Objective Data: I focus on objective data obtained from physical examination, vital signs, and diagnostic tests. This avoids biases and ensures consistency.
- Timeliness: Documentation is completed immediately after patient interactions or as soon as possible, to minimize recall bias and ensure accurate records.
- Electronic Health Records (EHR): I am proficient with EHR systems, utilizing them efficiently to accurately document assessments, interventions, and patient responses. I ensure that all entries are legible, accurate, and comply with institutional policies and guidelines.
- Legal & Ethical Considerations: I am mindful of legal and ethical implications of documentation, ensuring patient confidentiality and adhering to HIPAA regulations.
My experience spans various healthcare settings, utilizing different charting systems. This has equipped me with strong adaptation skills to different charting formats and requirements.
Q 4. How do you identify and respond to changes in a patient’s condition?
Identifying and responding to changes in a patient’s condition requires vigilance and a proactive approach. Regular and frequent assessment is key. I monitor for subtle changes in vital signs, pain levels, mental status, and other relevant parameters. For example:
- Frequent Monitoring: For patients with unstable conditions, I implement frequent monitoring schedules, perhaps checking vital signs every 15 minutes or more, depending on the patient’s acuity. This allows early detection of deterioration.
- Comparison to Baseline: I consistently compare a patient’s current status to their baseline data. Any deviation from established norms warrants further investigation.
- Patient Communication: I encourage open communication with patients and families. Changes reported by the patient or family are considered valuable information, even seemingly minor ones.
- Collaboration: I promptly communicate observed changes to the medical team, ensuring prompt and appropriate intervention. Timely notification is crucial to preventing adverse events.
- Data Analysis: I analyze trends in data to identify deteriorating conditions. For example, a gradual increase in respiratory rate or a decline in oxygen saturation might indicate worsening respiratory status, prompting timely escalation of care.
Q 5. Describe a situation where you had to make a difficult clinical decision.
In my previous role, I cared for a patient experiencing severe post-operative pain despite receiving prescribed analgesics. The patient was exhibiting signs of distress and anxiety, but their pain score remained high. This presented a dilemma; increasing opioid dosages risked respiratory depression, while insufficient pain management caused further suffering. I carefully considered the risk-benefit ratio and:
- Comprehensive Assessment: I performed a thorough pain assessment, exploring potential contributing factors like nerve compression or inadequate medication delivery.
- Consultations: I consulted with the physician and pain management specialist, outlining the situation and discussing alternative pain management strategies.
- Non-Pharmacological Interventions: We implemented non-pharmacological pain relief measures like repositioning, ice packs, and relaxation techniques.
- Titration of Medication: The physician adjusted the analgesia regimen carefully, monitoring the patient’s response closely. We switched to a different analgesic, minimizing opioid dependence while effectively managing the pain.
- Close Monitoring: I monitored the patient’s respiratory rate, oxygen saturation, and level of consciousness meticulously. This allowed for prompt detection and management of potential side effects.
The situation highlighted the importance of comprehensive assessment, collaborative decision-making, and the need to consider both the patient’s physical and emotional well-being when making clinical decisions.
Q 6. How do you handle conflicting priorities in patient care?
Conflicting priorities in patient care are common. I address these by using a structured approach based on ethical principles and clinical judgment:
- Prioritization: Utilizing frameworks like Maslow’s Hierarchy of Needs and ABCDE principles guides the prioritization of tasks based on urgency and importance. Life-threatening issues always take precedence.
- Collaboration: I actively collaborate with the healthcare team, including physicians, nurses, and other specialists. Open communication and teamwork allow us to pool resources and expertise, finding the most effective solutions for multiple competing demands.
- Resource Allocation: I consider available resources (staffing, equipment, time) to make the most efficient use of them. This includes delegating tasks appropriately when possible.
- Advocacy: If a decision impacts a patient negatively due to resource limitations, I advocate for the patient’s needs by communicating the issue to appropriate decision-makers. This can involve escalating concerns or seeking additional support.
- Documentation: I meticulously document all decisions made, the rationale behind them, and the discussions held with the healthcare team. This transparent documentation ensures that everyone is on the same page and protects all stakeholders.
Q 7. How do you ensure patient safety during procedures?
Ensuring patient safety during procedures is paramount. My approach is multi-faceted and incorporates several strategies:
- Pre-procedure Checklist: I always use a standardized checklist to verify the patient’s identity, allergies, and consent. This reduces the risk of medication errors or procedural mishaps.
- Sterile Technique: Maintaining a sterile field during procedures is essential. I strictly follow guidelines for asepsis to prevent infection. This includes proper hand hygiene, using sterile gloves and instruments, and maintaining a clean environment.
- Equipment Checks: I meticulously check all equipment prior to use, ensuring it is functioning properly and is safe. This includes checking the functionality of infusion pumps, ventilators, and monitoring devices.
- Patient Monitoring: Close monitoring of the patient’s vital signs, oxygen saturation, and other parameters during procedures is critical. I remain vigilant for any signs of adverse events and intervene promptly.
- Post-Procedure Care: After the procedure, I monitor the patient for complications and provide appropriate post-procedure care to ensure a safe recovery. This includes assessing pain levels, administering medications as prescribed, and providing patient education.
- Incident Reporting: In the event of any incident or near-miss, I promptly report it through the appropriate channels. This facilitates investigation, learning, and the implementation of corrective measures.
Q 8. Explain your understanding of HIPAA regulations and patient confidentiality.
HIPAA, the Health Insurance Portability and Accountability Act, is the cornerstone of patient privacy in the United States. It mandates the protection of Protected Health Information (PHI), which includes anything that can identify a patient and relate to their past, present, or future physical or mental health or payment for healthcare. This encompasses medical records, diagnoses, treatment plans, insurance details, and even conversations about a patient’s health.
My understanding of HIPAA extends beyond simply knowing the law; it’s deeply ingrained in my practice. I meticulously follow procedures to ensure PHI is only accessed by authorized personnel. This includes secure storage of physical records, using encrypted electronic health records (EHRs), and adhering to strict protocols for sharing information, only disclosing it with the patient’s explicit consent or as legally mandated. For instance, I would never discuss a patient’s condition with a family member without their permission, even if that family member is present. I also ensure that all computer systems are password-protected and that I log out of EHRs when finished with patient charts. Violating HIPAA has serious legal and ethical consequences, and I take my responsibility to protect patient confidentiality very seriously.
Q 9. How do you communicate effectively with patients and their families?
Effective communication is paramount in patient care. It involves active listening, clear and concise language, and empathy. I always begin by introducing myself and explaining my role. I then make a conscious effort to understand the patient’s perspective, using open-ended questions to encourage them to share their concerns and experiences. For example, instead of asking, ‘Are you in pain?’, I might ask, ‘Can you describe the pain you are experiencing?’ This allows for a more detailed and nuanced understanding.
When communicating with families, I ensure all relevant parties understand the treatment plan. I use visual aids, such as diagrams or charts, when necessary. I tailor my language to the family’s understanding, avoiding medical jargon. I also make myself available to answer questions and address concerns, fostering a collaborative approach to care. A memorable instance involved a family struggling to comprehend their loved one’s prognosis. I spent extra time explaining the condition in simpler terms and answered their questions patiently, creating an atmosphere of trust and mutual understanding. This ensured they were fully informed and involved in decision-making.
Q 10. Describe your experience with medication administration.
My experience with medication administration is extensive and includes both oral and parenteral routes. I’m proficient in the ‘five rights’ of medication administration – right patient, right medication, right dose, right route, and right time – and also include verifying the right documentation. Before administering any medication, I carefully review the patient’s chart, allergies, and current medication list. I always double-check the medication label and calculate the dose meticulously. For instance, when administering insulin, I verify the dose with a colleague before injecting.
I am experienced in different administration techniques, such as intramuscular, subcutaneous, and intravenous injections, and I am familiar with different types of medications, including controlled substances. Any deviation from the standard procedure, even a minor one, is meticulously documented, highlighting the reason and any observed reactions. Patient education regarding their medications is crucial; I always explain the purpose, dosage, potential side effects, and the importance of adherence. If a patient expresses concerns or confusion, I patiently clarify their doubts before proceeding.
Q 11. How do you manage a patient with aggressive or challenging behavior?
Managing patients exhibiting aggressive or challenging behavior requires a calm, patient, and de-escalation-focused approach. First and foremost, ensuring the safety of myself and others is priority. I would assess the situation, determining the cause of the agitation – is it pain, fear, confusion, or medication side effects? This assessment guides my response.
I employ de-escalation techniques, such as maintaining a calm tone, using clear and simple language, creating a safe space, and offering reassurance. Physical restraint is used only as a last resort, and always according to established protocols. Collaboration with the healthcare team and, if needed, contacting security personnel is critical. Documentation of the incident, including the patient’s behavior, interventions taken, and the outcome, is crucial for future care and risk assessment. For example, if a patient is experiencing heightened anxiety, offering a calming presence, and perhaps a warm drink, can significantly de-escalate the situation. If the behavior is related to pain, administering appropriate analgesics as prescribed is vital.
Q 12. Explain your experience with wound care.
My wound care experience encompasses a wide range of wound types, from simple abrasions to complex pressure ulcers and surgical wounds. I am skilled in assessing wounds using standardized tools and documentation methods, such as the Braden scale for pressure ulcer risk. This assessment helps determine the appropriate treatment plan, which might include wound cleaning, debridement, dressing application, and pain management.
I am proficient in various dressing techniques, selecting the most appropriate type for each wound – for example, using hydrocolloids for moderate exudate, alginates for heavy exudate, and foams for absorption and protection. I meticulously monitor the wound’s progress and adjust the treatment plan as needed. Patient education about wound care, including hygiene practices and signs of infection, is a critical component of my approach. For example, a patient with a pressure ulcer needs regular repositioning, skin hygiene, and specific dressing changes, and I ensure that the patient and their caregiver understand these procedures thoroughly.
Q 13. Describe your process for educating patients and their families.
Patient and family education is a core aspect of holistic care. My approach starts with assessing their understanding of the condition and treatment plan. I use clear, concise language, avoiding medical jargon, and supplement verbal instruction with visual aids such as diagrams and brochures. I tailor my explanations to their individual learning styles and health literacy levels.
I encourage questions and actively seek feedback to ensure understanding. I also provide written materials reinforcing the information discussed. For instance, when educating a patient about diabetes management, I would explain the importance of diet and exercise, demonstrate proper blood glucose monitoring, and provide written instructions and contact information for support groups. Following up with patients to answer any additional questions or address concerns after they leave the clinical setting ensures that they’re well-equipped to manage their health effectively. Effective patient education empowers patients and families, leading to improved outcomes and increased adherence to treatment plans.
Q 14. How do you handle emergency situations involving patients?
Handling emergency situations demands swift, decisive action based on established protocols. My response starts with a rapid assessment of the patient’s condition, prioritizing the ABCs: airway, breathing, and circulation. I immediately call for help, utilizing the facility’s emergency response system.
Depending on the nature of the emergency, my actions may include administering first aid, CPR, or initiating advanced life support procedures as per my training and the situation demands. I continuously monitor the patient’s vital signs and document all actions taken. Clear and concise communication with the emergency medical team is crucial for effective collaboration and timely intervention. After the emergency, a comprehensive debriefing with the team is conducted to evaluate the response, identify areas for improvement, and prevent similar occurrences in the future. Effective emergency response requires a combination of knowledge, skills, and a calm, methodical approach under pressure.
Q 15. How do you utilize electronic health records (EHRs) in patient care?
Electronic Health Records (EHRs) are indispensable tools in modern patient care. I utilize them throughout the entire patient journey, from initial assessment to ongoing management and discharge planning.
- Patient Charting: I use EHRs to meticulously document all aspects of a patient’s visit, including vital signs, medical history, physical exam findings, diagnoses, treatment plans, medications, and progress notes. This ensures a complete and readily accessible record.
- Order Entry: EHRs allow me to efficiently order lab tests, imaging studies, consultations, and medications, reducing errors and streamlining the process. For example, I can directly order a blood glucose test through the system and have the results automatically integrated into the patient’s chart.
- Medication Management: EHRs provide alerts for potential drug interactions, allergies, and contraindications, improving patient safety. They also provide a comprehensive medication history, which is vital for managing polypharmacy.
- Communication and Collaboration: EHRs facilitate seamless communication among healthcare professionals. I can communicate with specialists, refer patients to other services, and share information securely and efficiently.
- Data Analysis and Reporting: EHRs provide access to valuable data that can be used for population health management, quality improvement initiatives, and research. I can track patient outcomes and identify trends to enhance care delivery.
For example, I recently used the EHR to track the effectiveness of a new diabetes management protocol within our clinic. The data revealed significant improvements in blood sugar control among our patients.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with pain management.
Pain management is a critical component of holistic patient care. My approach involves a comprehensive assessment, considering both the physical and psychological aspects of pain.
- Assessment: I begin by thoroughly evaluating the patient’s pain using standardized scales like the numeric rating scale (NRS) or the visual analog scale (VAS). This includes exploring the location, intensity, duration, quality, and aggravating/relieving factors of the pain. I also investigate the impact of pain on daily activities and overall quality of life.
- Non-pharmacological Interventions: I utilize various non-pharmacological methods, including heat/cold therapy, massage, physical therapy referrals, cognitive behavioral therapy (CBT), and relaxation techniques. These methods are often effective in reducing pain and improving function without the risks associated with medication.
- Pharmacological Interventions: When necessary, I work with the patient to develop a pharmacological plan, considering factors such as the patient’s medical history, potential drug interactions, and personal preferences. I carefully monitor for side effects and adjust the medication regimen as needed. I prioritize the use of the least potent medication with the least side effects while maintaining effective pain control.
- Multidisciplinary Approach: Severe or chronic pain often requires a multidisciplinary approach. I collaborate closely with pain specialists, physical therapists, psychologists, and other healthcare professionals to create a comprehensive care plan tailored to the patient’s individual needs.
For instance, I recently helped manage a patient with chronic back pain. Through a combination of physical therapy, medication management, and CBT, we achieved significant pain reduction, improving the patient’s quality of life and mobility.
Q 17. How do you adapt your approach to care based on a patient’s cultural background?
Cultural competence is essential for providing equitable and effective healthcare. I adapt my approach by considering the patient’s cultural beliefs, values, and practices, understanding that these factors significantly influence health behaviors and treatment preferences.
- Communication: I use clear and concise language, avoiding medical jargon. I actively listen to understand the patient’s perspective and ensure they feel heard and respected. I am mindful of nonverbal cues and communication styles that may differ across cultures. If needed, I will utilize a translator or interpreter.
- Health Beliefs and Practices: I inquire about the patient’s traditional healing practices and beliefs, respecting their autonomy. This includes asking about the use of herbal remedies or traditional medicine. I aim to integrate these practices into the care plan when appropriate and safe.
- Family Dynamics: I acknowledge the importance of family involvement in decision-making, particularly in cultures with strong family ties. I involve the family members in conversations as appropriate, always respecting the patient’s wishes.
- Dietary Preferences: I consider the patient’s dietary needs and restrictions based on their cultural background. Dietary preferences can significantly impact treatment adherence and overall health.
For example, I recently cared for a patient from a culture where direct eye contact is considered disrespectful. I adjusted my communication style accordingly to build rapport and trust.
Q 18. Explain your understanding of different types of vital signs and their significance.
Vital signs are fundamental indicators of a patient’s physiological state. Understanding their significance is crucial for early detection of problems and effective intervention.
- Temperature: Measures core body temperature, reflecting the balance between heat production and heat loss. Elevated temperature (fever) suggests infection or inflammation; low temperature (hypothermia) may indicate exposure to cold or underlying medical conditions.
- Heart Rate (Pulse): Represents the number of times the heart beats per minute. An elevated heart rate (tachycardia) can indicate stress, fever, dehydration, or heart conditions; a low heart rate (bradycardia) can indicate heart block or other cardiac issues.
- Respiratory Rate: Indicates the number of breaths per minute. Rapid breathing (tachypnea) may be caused by lung disease, pain, anxiety, or metabolic acidosis; slow breathing (bradypnea) can be a sign of neurological disorders or drug overdose.
- Blood Pressure: Measures the force of blood against artery walls. High blood pressure (hypertension) increases the risk of heart disease and stroke; low blood pressure (hypotension) can cause dizziness, fainting, or shock.
- Oxygen Saturation (SpO2): Measures the percentage of hemoglobin saturated with oxygen in the blood. Low oxygen saturation (hypoxemia) indicates inadequate oxygen delivery to the tissues and requires prompt intervention.
- Pain: While subjective, pain is a vital sign indicating potential physical or emotional distress requiring assessment and management. Using pain scales such as NRS and VAS allows for objective quantification.
Changes in any vital sign can indicate a deterioration in a patient’s condition and necessitate immediate attention. For instance, a sudden drop in blood pressure can signify internal bleeding, requiring prompt medical intervention.
Q 19. How do you identify and respond to potential medical errors?
Identifying and responding to potential medical errors is paramount in ensuring patient safety. My approach involves a multi-faceted strategy focused on prevention, detection, and correction.
- Preventive Measures: I diligently follow established protocols and guidelines. I utilize checklists and double-check medications and procedures to minimize errors. I also advocate for clear communication and collaboration among healthcare professionals.
- Error Detection: I remain vigilant in monitoring my own work and the work of my colleagues. I am actively involved in medication reconciliation, ensuring that all medications are correctly documented and administered. I use critical thinking skills to identify inconsistencies or discrepancies in patient data.
- Reporting and Corrective Actions: If I identify a potential or actual medical error, I immediately report it using the appropriate channels within the organization. I collaborate with other healthcare professionals to analyze the circumstances surrounding the error and implement corrective actions to prevent recurrence. I participate actively in root cause analysis to understand contributing factors.
- Near Miss Reporting: Reporting near misses (events that could have resulted in an error) is vital for identifying system weaknesses and preventing future errors. I actively participate in near miss reporting, contributing my observations and experiences.
For example, I once noticed a discrepancy in a medication order, preventing a potential adverse drug interaction. I reported this immediately and participated in a root cause analysis, which led to process improvements in our medication ordering system.
Q 20. Describe a time you had to advocate for a patient’s needs.
I once had to advocate for a patient who was scheduled for a procedure that she was unsure about. She was feeling pressured by her family to proceed with the procedure, despite her own reservations.
- Listening and Understanding: First, I spent time listening to her concerns and understanding her hesitations. She expressed anxiety and uncertainty about the potential risks and benefits of the procedure.
- Educating and Empowering: I provided clear and unbiased information about the procedure, addressing her specific questions and concerns. I explained the possible outcomes, both positive and negative, ensuring she felt empowered to make her own decision.
- Supporting Autonomy: I reiterated her right to refuse the procedure and explained that her autonomy was respected. I reassured her that delaying or declining the procedure would not affect her relationship with the healthcare team.
- Collaborating with the Team: I communicated the patient’s concerns to the surgical team and discussed alternatives that might address her concerns. We explored different options, including delaying the surgery for further consultation or exploring non-surgical options.
- Documenting Everything: I meticulously documented the conversation, the patient’s concerns, the discussion with the surgical team, and the final decision. This ensured a clear and accurate record of the events.
Ultimately, the patient decided to postpone the procedure, giving herself more time to consider her options. My role was to support her autonomy and ensure that her voice was heard.
Q 21. How do you maintain accurate patient records?
Maintaining accurate patient records is essential for providing high-quality care and avoiding legal issues. My approach to record keeping is meticulous and follows best practices.
- Real-Time Documentation: I strive to document patient information immediately after assessment or intervention. This ensures that the information is fresh and accurate.
- Accuracy and Completeness: I use precise and objective language when documenting findings. I ensure all relevant information is included, avoiding ambiguity or omissions.
- Consistency: I maintain consistency in terminology and format, adhering to institutional guidelines and standards.
- Error Correction: If an error is made, I correct it appropriately by adding an addendum rather than obliterating the original entry. This preserves the integrity and chronological order of the record.
- Confidentiality: I strictly adhere to confidentiality protocols and use appropriate security measures to protect patient information. I ensure that only authorized individuals have access to patient data.
For example, I always double-check medication names and dosages before documenting them to ensure accuracy. I also utilize the EHR’s built-in tools to flag and correct any potential errors.
Q 22. Explain your understanding of infection control protocols.
Infection control protocols are a set of procedures designed to prevent the spread of infectious agents in healthcare settings. They are crucial for protecting both patients and healthcare workers. These protocols encompass a wide range of practices, all aimed at minimizing the risk of infection transmission.
- Hand Hygiene: This is the cornerstone of infection control. It involves frequent and thorough handwashing with soap and water or the use of an alcohol-based hand rub. The correct technique, including covering all surfaces of the hands and fingers, is paramount.
- Personal Protective Equipment (PPE): PPE, such as gloves, gowns, masks, and eye protection, is used to create a barrier between the healthcare worker and potentially infectious materials. The selection of appropriate PPE depends on the specific risk involved, for example, using a N95 respirator when dealing with airborne pathogens.
- Environmental Cleaning and Disinfection: Regular cleaning and disinfection of surfaces, equipment, and the environment are essential to reduce the microbial load. Different disinfectants are used based on the type of surface and the suspected pathogens.
- Waste Management: Proper handling and disposal of medical waste, including sharps and contaminated materials, are critical to prevent accidental exposure and spread of infection. This involves following strict protocols for segregation, packaging, and disposal.
- Isolation Precautions: Isolation precautions, such as contact, droplet, and airborne precautions, are implemented for patients with known or suspected infectious diseases to limit the spread of infection to others. These precautions dictate specific measures like wearing gowns and gloves, using private rooms, and adhering to specific ventilation requirements.
For example, during a recent influenza outbreak, I meticulously implemented droplet precautions for a patient by wearing a surgical mask, practicing frequent hand hygiene, and ensuring proper disposal of contaminated materials. My commitment to these protocols ensured both patient and staff safety.
Q 23. Describe your experience with patient discharge planning.
Patient discharge planning is a collaborative process that begins upon admission and involves coordinating the patient’s transition from the hospital or healthcare facility to their home or another care setting. It aims to ensure a smooth, safe, and effective transfer, minimizing potential complications and maximizing the patient’s well-being.
- Assessment of Needs: This involves evaluating the patient’s physical, emotional, and psychosocial needs, including medication requirements, mobility limitations, and social support systems.
- Development of a Discharge Plan: A comprehensive plan is created, outlining the patient’s care needs, medication regimen, follow-up appointments, rehabilitation services, and any necessary equipment or home modifications.
- Coordination of Care: This involves coordinating with various healthcare professionals, family members, and community resources, such as home healthcare agencies and social workers. Effective communication is essential throughout this process.
- Patient and Family Education: Providing clear and concise instructions regarding medication administration, wound care, diet, and potential complications is crucial for successful discharge. We also address any concerns or questions the patient or family may have.
- Follow-up: After discharge, follow-up calls or visits are conducted to ensure the patient is doing well, to address any problems and to provide continued support.
In one instance, I worked with a patient recovering from a stroke. We collaborated with physical therapists, occupational therapists, and a home health nurse to develop a discharge plan that included home modifications, physical therapy sessions, and ongoing medication management. Regular follow-up calls ensured a successful transition and prevented readmission.
Q 24. How do you collaborate effectively with other members of the healthcare team?
Effective collaboration within a healthcare team is essential for providing high-quality patient care. My approach involves open communication, active listening, mutual respect, and shared decision-making. I believe in fostering a team environment where everyone’s expertise and perspective are valued.
- Open Communication: I regularly communicate with other members of the team, including physicians, nurses, therapists, and social workers, to share updates on patient progress, address concerns, and coordinate care.
- Active Listening: I actively listen to the input of others, valuing their insights and experience. This helps identify potential problems early and develop comprehensive solutions.
- Respectful Interactions: I treat all team members with respect, recognizing their contributions and expertise. This creates a positive and collaborative environment.
- Shared Decision-Making: I actively participate in shared decision-making processes, contributing my expertise while considering the input of others. This leads to better-informed and patient-centered decisions.
- Team Meetings and Huddles: I actively participate in team meetings and huddles to discuss patient cases, share information, and address challenges collaboratively.
For example, during a multidisciplinary team meeting regarding a patient with complex medical needs, I effectively communicated my assessment findings, listened to the input of the physician and physical therapist, and collaboratively developed a comprehensive treatment plan that considered the patient’s overall needs and goals.
Q 25. How do you handle stressful situations in a calm and professional manner?
Healthcare is inherently stressful. My ability to handle stressful situations calmly and professionally stems from a combination of experience, training, and a proactive approach.
- Prioritization: In stressful situations, I prioritize tasks based on urgency and importance. This helps me focus my efforts effectively and prevent feeling overwhelmed.
- Deep Breathing and Mindfulness: I utilize techniques like deep breathing and mindfulness to manage my stress levels. These practices help me remain calm and focused.
- Time Management: Effective time management helps me stay organized and prevents unnecessary stress. This involves prioritizing tasks and delegating when appropriate.
- Seeking Support: When needed, I seek support from colleagues or supervisors. This helps me manage particularly challenging situations and gain valuable insights.
- Self-Care: Prioritizing self-care, including adequate rest, exercise, and healthy eating habits, is essential for managing stress and maintaining well-being.
During a recent emergency situation involving a patient experiencing respiratory distress, I remained calm, prioritizing immediate life-saving interventions while simultaneously communicating effectively with the medical team. My calm demeanor helped maintain a safe and controlled environment.
Q 26. Explain your experience with obtaining informed consent from patients.
Obtaining informed consent is a critical aspect of ethical patient care. It involves ensuring the patient has a full understanding of the proposed medical procedure or treatment, including its benefits, risks, and alternatives, before providing voluntary agreement. This process requires clear communication, patience, and attention to the patient’s individual needs and comprehension levels.
- Clear Explanation: I explain the procedure or treatment in simple, understandable terms, avoiding medical jargon as much as possible. I make sure the patient understands the purpose, process, benefits, risks, and alternatives.
- Addressing Questions: I answer any questions the patient or their family may have thoroughly and patiently. I ensure they feel comfortable asking questions and expressing concerns.
- Assessment of Understanding: I assess the patient’s understanding by asking them to summarize the information in their own words. This confirms comprehension and helps identify any areas needing further clarification.
- Documentation: I meticulously document the informed consent process, including the date, time, and the information discussed. I obtain the patient’s signature on the consent form, ensuring they are fully aware of what they are consenting to.
- Respect for Autonomy: I always respect the patient’s autonomy and right to refuse treatment. I do not coerce or pressure them into making a decision.
For example, before a patient underwent a complex surgical procedure, I explained the procedure, potential risks (including bleeding, infection, and nerve damage), and the benefits in detail. I answered all their questions, ensured they understood the alternatives, and obtained their fully informed consent.
Q 27. Describe your knowledge of common medical terminology.
A strong understanding of common medical terminology is essential for effective communication and accurate documentation. My knowledge encompasses a wide range of terms related to anatomy, physiology, pathology, pharmacology, and diagnostics. I am familiar with abbreviations and acronyms commonly used in healthcare.
- Anatomy and Physiology: I have a comprehensive understanding of the structure and function of the human body, including organ systems, tissues, and cells.
- Pathology: I understand the nature and causes of diseases, including common medical conditions, their symptoms, and their progression.
- Pharmacology: I am familiar with the properties and effects of various medications, including their indications, contraindications, side effects, and interactions.
- Diagnostics: I understand various diagnostic tests and procedures, including laboratory tests, imaging techniques, and other diagnostic modalities.
- Abbreviations and Acronyms: I am proficient in understanding and using common medical abbreviations and acronyms, such as
BP(blood pressure),ECG(electrocardiogram), andCBC(complete blood count).
For instance, understanding terms like tachycardia (rapid heart rate), hypertension (high blood pressure), and hypoxia (low blood oxygen) allows me to quickly grasp the patient’s condition and contribute effectively to their care.
Q 28. How do you utilize critical thinking skills in patient care?
Critical thinking is crucial in patient care, as it allows for a systematic and objective approach to assessment, planning, and evaluation. I utilize a framework that incorporates several key steps.
- Data Collection: Thorough data collection from various sources, including the patient’s history, physical examination findings, and laboratory results, is the first step. This ensures a comprehensive understanding of the patient’s condition.
- Analysis and Interpretation: Next, I analyze and interpret the collected data, identifying patterns, inconsistencies, and potential problems. This often involves identifying relevant information while disregarding irrelevant details.
- Problem Identification: Based on the analysis, I identify the underlying problem or problems. This might involve distinguishing between symptoms and underlying causes.
- Hypothesis Formation: I formulate hypotheses regarding the possible causes and contributing factors to the identified problems.
- Plan Development: I develop a plan to address the identified problems based on evidence-based practices and patient-specific needs. This includes treatment strategies, monitoring parameters, and potential risk management.
- Evaluation and Adjustment: Finally, I continuously evaluate the effectiveness of the intervention and adjust the plan as necessary. This ensures that the care plan remains appropriate and effective.
For example, a patient presented with chest pain. Instead of jumping to conclusions, I systematically gathered data, performed a thorough physical examination, and ordered relevant tests. By analyzing the results, I identified the cause as angina, developed a treatment plan that included lifestyle modifications and medication, and then continuously monitored its effectiveness.
Key Topics to Learn for Patient Care and Assessment Interview
- Patient History Taking & Documentation: Mastering the art of effectively gathering comprehensive patient information, including medical history, social history, and presenting complaints. Understand different documentation methods and their importance for continuity of care.
- Physical Assessment Techniques: Develop proficiency in performing accurate and thorough physical assessments, including vital signs measurement, auscultation, palpation, and percussion. Be prepared to discuss the rationale behind each technique and its clinical significance.
- Recognizing and Responding to Changes in Patient Condition: Understand how to identify subtle changes in a patient’s status, interpret their significance, and escalate concerns appropriately. Discuss your approach to prioritizing patient needs and communicating effectively with the healthcare team.
- Clinical Reasoning & Problem Solving: Practice applying critical thinking skills to analyze patient data, formulate differential diagnoses, and develop appropriate care plans. Be ready to articulate your thought process in a clear and concise manner.
- Communication & Interpersonal Skills: Demonstrate your ability to communicate effectively with patients, families, and other healthcare professionals. Highlight your skills in active listening, empathy, and building rapport.
- Safety & Risk Management: Discuss your understanding of patient safety protocols and your approach to minimizing risks associated with patient care. Showcase your knowledge of fall prevention, medication safety, and infection control.
- Legal and Ethical Considerations: Be prepared to discuss relevant legal and ethical principles related to patient care, such as confidentiality, informed consent, and end-of-life care.
Next Steps
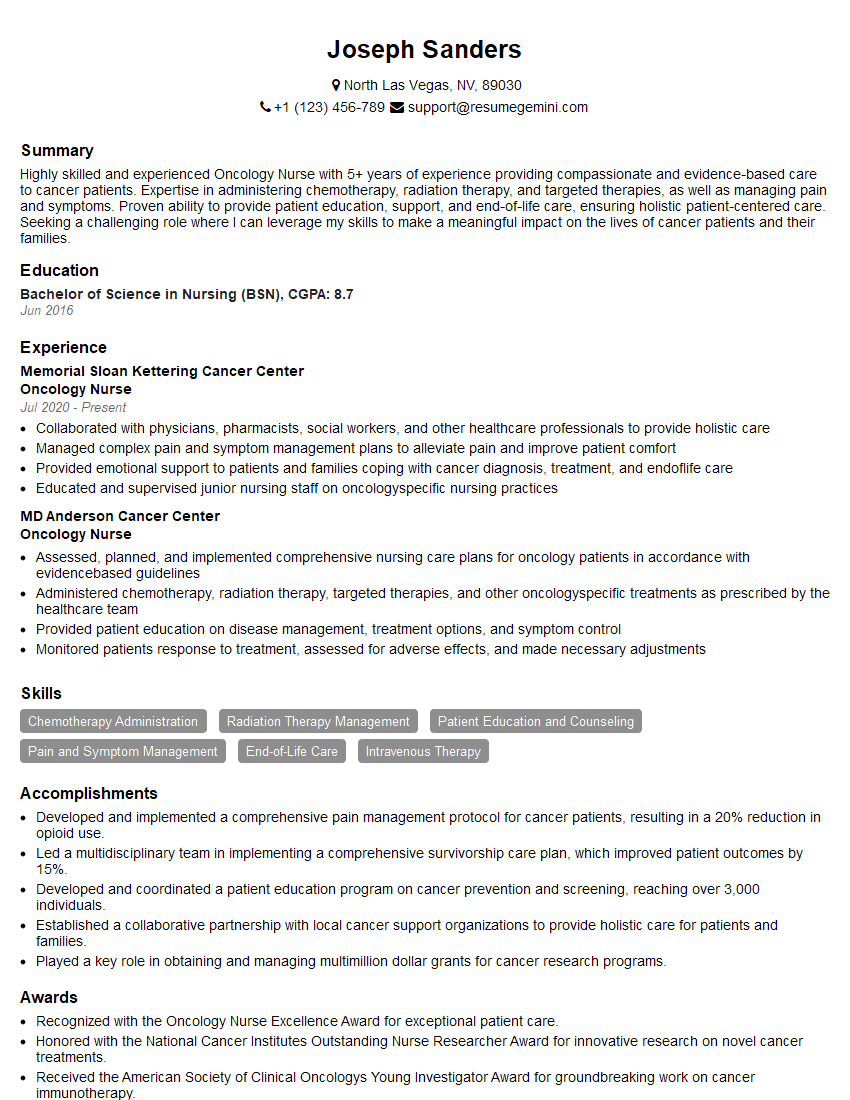
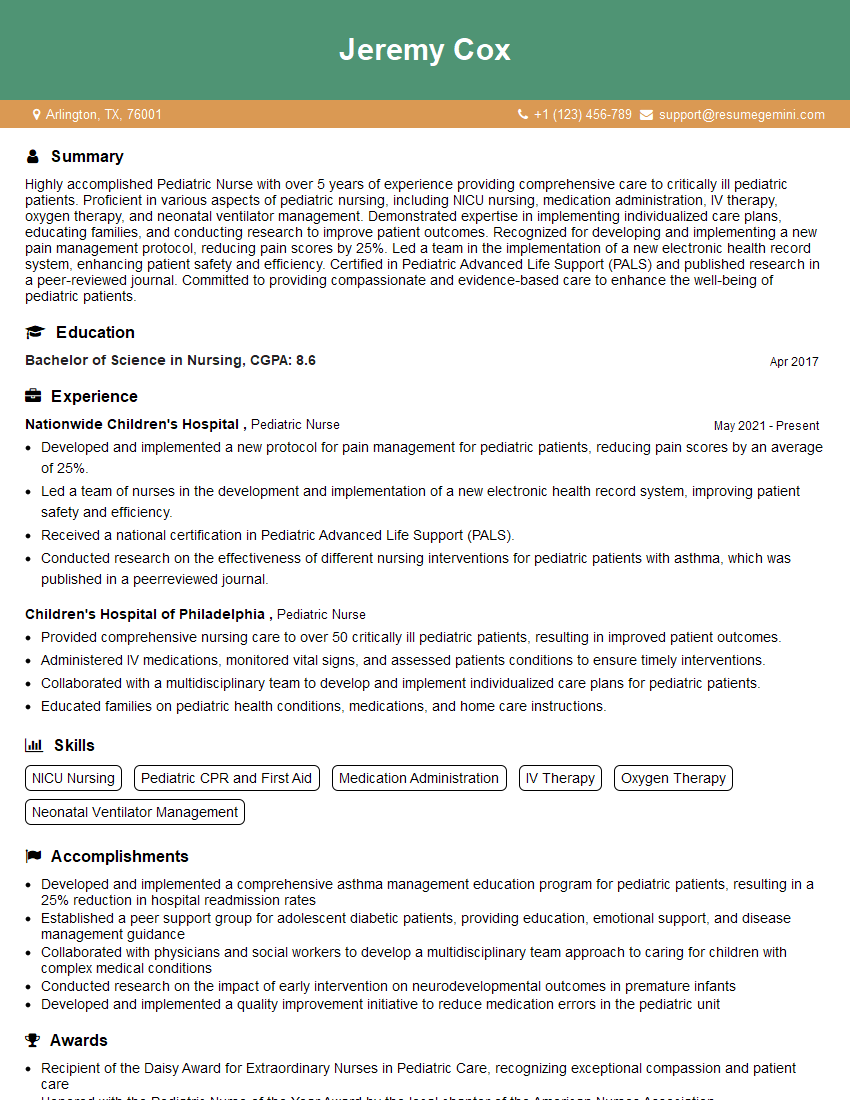
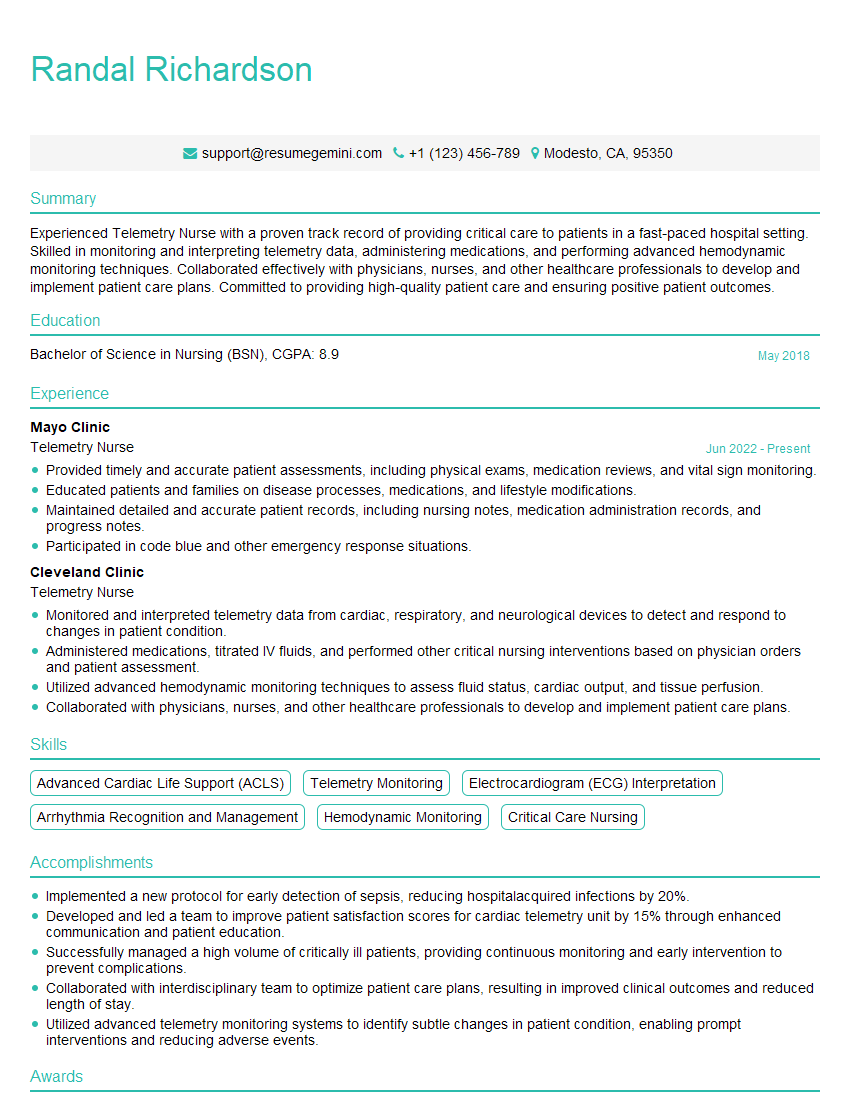
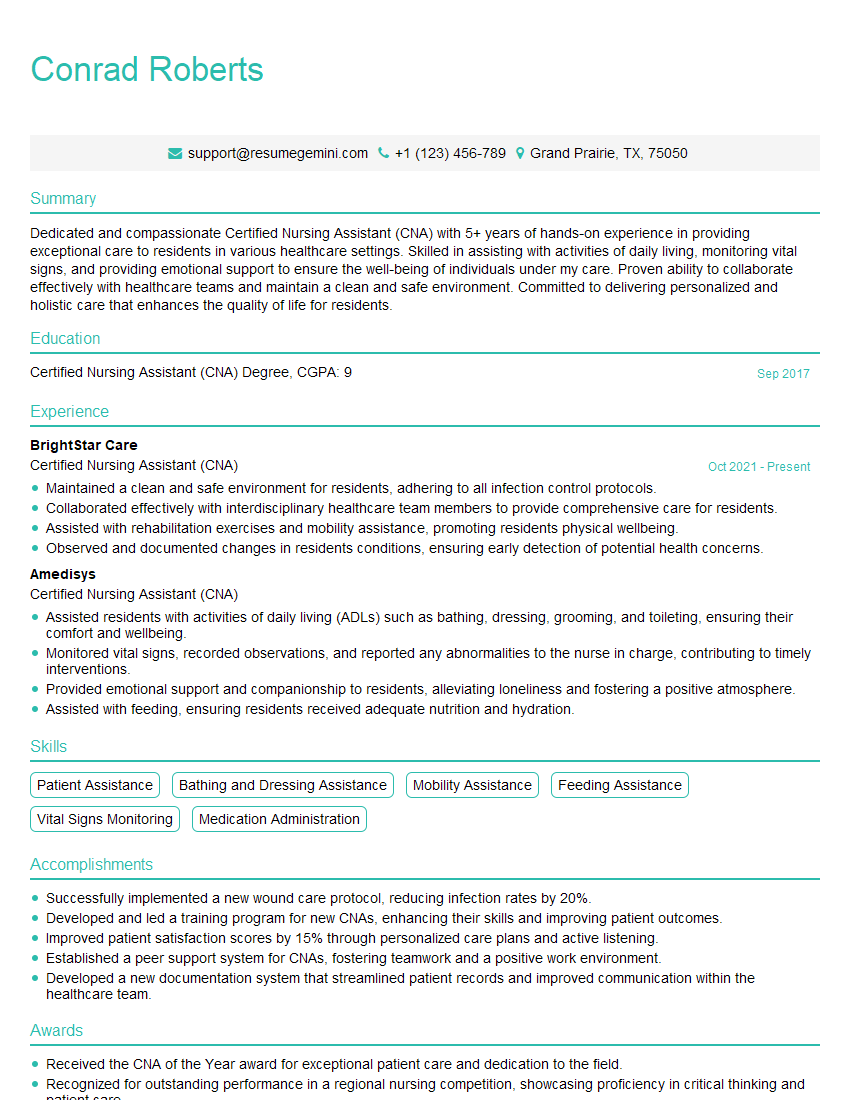
Mastering Patient Care and Assessment is crucial for career advancement in healthcare. A strong understanding of these concepts demonstrates competence and commitment, opening doors to more challenging and rewarding roles. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume that highlights your skills and experience effectively. Examples of resumes tailored to Patient Care and Assessment are available through ResumeGemini, showcasing how to present your qualifications in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi I am a troller at The aquatic interview center and I suddenly went so fast in Roblox and it was gone when I reset.
Hi,
Business owners spend hours every week worrying about their website—or avoiding it because it feels overwhelming.
We’d like to take that off your plate:
$69/month. Everything handled.
Our team will:
Design a custom website—or completely overhaul your current one
Take care of hosting as an option
Handle edits and improvements—up to 60 minutes of work included every month
No setup fees, no annual commitments. Just a site that makes a strong first impression.
Find out if it’s right for you:
https://websolutionsgenius.com/awardwinningwebsites
Hello,
we currently offer a complimentary backlink and URL indexing test for search engine optimization professionals.
You can get complimentary indexing credits to test how link discovery works in practice.
No credit card is required and there is no recurring fee.
You can find details here:
https://wikipedia-backlinks.com/indexing/
Regards
NICE RESPONSE TO Q & A
hi
The aim of this message is regarding an unclaimed deposit of a deceased nationale that bears the same name as you. You are not relate to him as there are millions of people answering the names across around the world. But i will use my position to influence the release of the deposit to you for our mutual benefit.
Respond for full details and how to claim the deposit. This is 100% risk free. Send hello to my email id: [email protected]
Luka Chachibaialuka
Hey interviewgemini.com, just wanted to follow up on my last email.
We just launched Call the Monster, an parenting app that lets you summon friendly ‘monsters’ kids actually listen to.
We’re also running a giveaway for everyone who downloads the app. Since it’s brand new, there aren’t many users yet, which means you’ve got a much better chance of winning some great prizes.
You can check it out here: https://bit.ly/callamonsterapp
Or follow us on Instagram: https://www.instagram.com/callamonsterapp
Thanks,
Ryan
CEO – Call the Monster App
Hey interviewgemini.com, I saw your website and love your approach.
I just want this to look like spam email, but want to share something important to you. We just launched Call the Monster, a parenting app that lets you summon friendly ‘monsters’ kids actually listen to.
Parents are loving it for calming chaos before bedtime. Thought you might want to try it: https://bit.ly/callamonsterapp or just follow our fun monster lore on Instagram: https://www.instagram.com/callamonsterapp
Thanks,
Ryan
CEO – Call A Monster APP
To the interviewgemini.com Owner.
Dear interviewgemini.com Webmaster!
Hi interviewgemini.com Webmaster!
Dear interviewgemini.com Webmaster!
excellent
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good