The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Performing CPR and first aid interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Performing CPR and first aid Interview
Q 1. Describe the steps involved in performing adult CPR.
Adult CPR is a life-saving technique used when someone stops breathing or their heart stops beating. It combines chest compressions and rescue breaths to circulate blood and oxygen throughout the body. Remember, always call emergency services (911 or your local equivalent) immediately before starting CPR.
- Check for Responsiveness: Gently shake the person and shout, “Are you okay?” If there’s no response, proceed to the next step.
- Call for Help: Immediately call emergency services. If you are alone, perform 2 minutes of CPR before calling.
- Check for Breathing: Look, listen, and feel for normal breathing for no more than 10 seconds. Look for chest rise and fall, listen for breathing sounds, and feel for breath on your cheek. Absence of normal breathing indicates the need for CPR.
- Chest Compressions: Position your hands correctly. Place the heel of one hand in the center of the chest (between the nipples). Place the other hand on top, interlacing your fingers. Keep your arms straight and push hard and fast, compressing the chest at least 2 inches deep at a rate of 100-120 compressions per minute. Allow the chest to fully recoil after each compression.
- Rescue Breaths: After 30 chest compressions, give two rescue breaths. Pinch the nose closed, create a seal over the mouth, and give slow, gentle breaths, each lasting about 1 second, ensuring you see the chest rise.
- Continue CPR: Continue cycles of 30 compressions and 2 breaths until help arrives or the person shows signs of life (e.g., breathing, movement).
Imagine you’re at a park and see someone collapse. Calling 911 is the first priority, then you’d assess the person’s breathing. If they are not breathing normally, immediate CPR is essential.
Q 2. What are the differences between adult, child, and infant CPR?
The main differences in CPR for adults, children, and infants lie in hand placement, compression depth, and the ratio of compressions to breaths.
- Adults (8 years and older): Two hands are used for chest compressions, compressing at least 2 inches deep. The compression-to-breath ratio is 30:2.
- Children (1-8 years): Use one or two hands depending on the child’s size. Compress about 2 inches deep. The compression-to-breath ratio is 30:2.
- Infants (less than 1 year): Use two fingers for chest compressions, compressing about 1.5 inches deep. The compression-to-breath ratio is 30:2. For infants, breaths are given over the mouth and nose.
The key difference is adjusting technique based on the victim’s size and development to ensure effective compressions and breaths. A smaller victim requires less force and a smaller hand placement area.
Q 3. Explain the recovery position and when it should be used.
The recovery position is used to help an unconscious but breathing person maintain an open airway and prevent choking on vomit or other secretions. It’s crucial to only use it if the person is breathing normally and doesn’t have a spinal injury suspected.
- Extend the arm: Extend the person’s arm closest to you straight out to the side.
- Bend the knee: Bend the person’s opposite knee, bringing it up towards their chest.
- Roll the person: Roll the person towards you onto their side by pulling the straight arm and knee, gently supporting their head and neck.
- Tilt the head: Tilt the person’s head back slightly to keep the airway open.
- Check breathing: Continuously monitor breathing.
Imagine someone faints and is breathing. Placing them in the recovery position will help protect their airway until medical assistance arrives. Do not move a person if you suspect a spinal injury.
Q 4. How do you check for responsiveness in an unconscious person?
Checking for responsiveness is the first step in any emergency situation. It involves gently shaking the person and shouting, “Are you okay?” Observe their response – any movement, sound, or reaction indicates responsiveness.
If there is no response to your voice or gentle shake, the person is considered unresponsive. This is a critical sign that further action is required.
For instance, if you find someone collapsed, you’d start by gently shaking them and speaking loudly to see if they respond. No response signals a need for immediate action such as initiating CPR and calling emergency services.
Q 5. What are the signs and symptoms of a heart attack?
A heart attack occurs when blood flow to a part of the heart is blocked, causing damage to the heart muscle. Signs and symptoms can vary, but common ones include:
- Chest pain or discomfort: This is often described as pressure, squeezing, fullness, or pain in the center of the chest that lasts more than a few minutes or goes away and comes back.
- Shortness of breath: Difficulty breathing can accompany chest pain or occur independently.
- Pain spreading to other areas: Pain can radiate to the arm, shoulder, back, neck, or jaw.
- Other symptoms: These may include breaking out in a cold sweat, nausea, lightheadedness, or feeling unusually tired.
It’s important to remember that heart attack symptoms can be subtle and may vary between individuals. If you suspect someone is having a heart attack, call emergency medical services immediately.
Q 6. What are the signs and symptoms of a stroke?
A stroke happens when blood supply to part of the brain is interrupted or reduced, causing brain damage. Recognizing the signs of a stroke is crucial for timely intervention. Use the FAST acronym:
- Face: Ask the person to smile. Does one side of their face droop?
- Arms: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- Time: If you observe any of these signs, call emergency services immediately. Time is critical in stroke treatment.
Other symptoms can include sudden numbness or weakness on one side of the body, sudden confusion, trouble seeing in one or both eyes, trouble walking, dizziness, or severe headache with no known cause.
Q 7. How do you manage a choking adult?
Managing a choking adult involves a series of steps to dislodge the object obstructing their airway. Always call emergency services immediately, and if you are trained, proceed with the Heimlich maneuver.
- Encourage coughing: If the person can cough forcefully, encourage them to continue, as this may dislodge the object.
- Abdominal thrusts (Heimlich maneuver): Stand behind the choking person. Make a fist with one hand and place it just above their navel. Grasp your fist with your other hand and give quick, upward thrusts into their abdomen. Repeat until the object is dislodged or the person becomes unconscious.
- Chest thrusts (if you cannot perform abdominal thrusts): If you can’t get behind the person, such as if they are sitting or too large to properly perform abdominal thrusts, perform chest thrusts. Similar to abdominal thrusts, except thrusts are given in the middle of the chest.
- Unconscious person: If the person becomes unconscious, carefully lower them to the ground and begin CPR, checking the mouth for any visible obstruction before starting rescue breaths.
Remember, proper training is essential for administering the Heimlich maneuver. This procedure is crucial to potentially saving a life. If you’re ever unsure, immediately call for emergency medical help.
Q 8. How do you manage a choking infant?
Managing a choking infant is a life-threatening emergency requiring immediate action. The key is to act quickly and effectively. Remember, your actions could save a life.
- Check for responsiveness: Gently tap the infant’s feet and shout, ‘Are you okay?’
- If unresponsive and choking, call emergency services immediately (911 or your local equivalent). Simultaneously begin rescue breaths and chest compressions.
- Back blows: Support the infant’s head and neck, laying them face down along your forearm. Give five firm back blows between the infant’s shoulder blades with the heel of your hand.
- Chest thrusts: Turn the infant face up, supporting the head and neck. Using two or three fingers, give five chest thrusts in the center of the infant’s chest, just below the nipple line.
- Repeat: Alternate between back blows and chest thrusts until the obstruction is cleared or emergency medical services arrive.
- If the obstruction is cleared and the infant is breathing, monitor their condition closely. If not, continue CPR and wait for medical help.
Example: Imagine you’re at a park and witness a parent struggling with a choking infant. Knowing these steps allows you to confidently intervene and potentially save the child’s life before professional help arrives. The speed and efficiency of your actions are critical.
Q 9. What are the steps for managing severe bleeding?
Severe bleeding is a critical emergency demanding immediate attention. The goal is to control the bleeding and prevent shock.
- Call emergency services immediately (911 or your local equivalent).
- Direct pressure: Apply firm, direct pressure to the wound using a clean cloth. Elevate the injured limb above the heart if possible, promoting blood flow away from the wound.
- Do not remove any embedded objects. Instead, carefully bandage around them to help control bleeding.
- Tourniquet (as a last resort): If direct pressure fails to control the bleeding, a tourniquet may be necessary. Apply it at least two inches above the wound, but only if absolutely essential. Note the time of application and make it clear to emergency responders.
- Monitor vital signs: Keep checking the casualty’s pulse and breathing. Signs of shock (pale skin, rapid pulse, shallow breathing) require immediate attention.
- Keep the casualty warm and calm.
Example: Imagine a construction worker severely injured on the job with a profusely bleeding leg. Quick and effective application of direct pressure, elevation, and potentially a tourniquet can significantly improve their chances of survival before paramedics arrive. The knowledge of when and how to use a tourniquet is vital.
Q 10. How do you treat a burn?
Burn treatment depends entirely on the severity and type of burn. Always prioritize the casualty’s safety and ensure your own protection.
- Cool the burn: Run cool (not cold) water over the burn for 10-20 minutes. This helps to reduce pain and tissue damage. Do not use ice or ice water, as this can further damage tissues.
- Remove jewelry or clothing: If clothing is stuck to the burn, do not force it off; this can further damage tissue. Cut around the clothing instead.
- Cover the burn loosely: Use a clean, non-adhesive dressing to cover the burn. This helps protect it from infection.
- Do not apply butter, creams, or ointments. These can trap heat and increase the risk of infection.
- Monitor for signs of shock: Keep a close eye on the casualty for symptoms of shock, such as rapid pulse, shallow breathing, and pale skin.
- Seek medical attention: For serious burns (deep burns, burns covering large areas, or burns to the face, hands, feet, or genitals), immediately seek medical attention.
Example: A child accidentally touches a hot stove. Quickly running cool water over the burn, loosely covering it with a clean cloth, and seeking medical advice for a proper assessment would be the appropriate response. Understanding burn severity is paramount.
Q 11. How do you treat a fracture?
Treating a fracture requires careful handling to avoid further injury. The primary goals are to immobilize the injured limb and prevent further damage.
- Check for responsiveness and ABCs (Airway, Breathing, Circulation).
- Immobilize the fracture: Use a splint or sling to keep the injured limb still. Do not attempt to straighten a visibly deformed limb.
- Apply cold packs: Cold compresses can help reduce pain and swelling. Avoid direct contact with the skin.
- Elevate the injured limb: Raising the limb above the heart level can help reduce swelling.
- Monitor vital signs: Observe for any signs of shock, such as pale skin, rapid pulse, or shallow breathing.
- Seek medical attention immediately: Fractures require professional medical care for proper diagnosis and treatment.
Example: You witness someone fall and sustain a possible leg fracture. By carefully immobilizing the leg with available materials like a rolled-up jacket before the arrival of medical aid, you prevent further injury and minimize pain. Understanding the principles of splinting is very important.
Q 12. What are the key differences between stable and unstable side position?
Both the stable and unstable side positions are used to help maintain an open airway and prevent aspiration (inhalation of vomit or fluids) in unconscious individuals. The key difference lies in the level of stability provided.
- Stable Side Position: Used for individuals who are unconscious but breathing normally. The head is tilted to keep the airway open. This position helps to prevent aspiration.
- Unstable Side Position: Used for individuals who are unconscious and have a potential or existing airway obstruction, and where more aggressive airway management may be necessary, before being moved to a medical facility. More support may be required to maintain the position of the head and neck.
In essence, the stable side position is for relatively stable unconscious casualties, while the unstable side position is a more temporary measure for maintaining the airway in a less stable individual, before definitive airway management or transport. The choice depends entirely on the casualty’s condition.
Q 13. Explain the importance of maintaining a clear airway.
Maintaining a clear airway is absolutely paramount in first aid and emergency care. A blocked airway prevents oxygen from reaching the lungs, leading to brain damage and ultimately death. Even a partially obstructed airway can significantly reduce oxygen levels.
Think of the airway as a vital pipeline. If this pipeline is blocked, the body’s most crucial resource—oxygen—cannot reach its destination. Therefore, ensuring a clear airway is the first step in saving a life.
Techniques to ensure a clear airway include: head tilt-chin lift, jaw thrust, suctioning, and recovery position.
Q 14. How would you prioritize multiple casualties in an emergency situation?
Prioritizing multiple casualties in an emergency situation is crucial and requires a systematic approach. The widely used method is known as START triage (Simple Triage And Rapid Treatment).
- Assess Responsiveness: Quickly assess each casualty’s responsiveness. Those who are unresponsive are prioritized.
- Assess Breathing: Check if they are breathing spontaneously. Those who are not breathing are prioritized.
- Assess Circulation: Check for a palpable pulse. Those without a pulse receive the lowest priority (unless immediate intervention might restore a pulse, as per guidelines).
- Assess Ability to Follow Commands: Those who can follow simple commands are categorized as ‘walking wounded’ and can often wait for treatment.
- Prioritization: Casualties are tagged based on their condition: Immediate (red), Delayed (yellow), Minimal (green), Expectant (black).
Example: In a mass casualty incident like a car crash, START triage helps you rapidly assess and categorize many injured people, enabling you to focus resources on those with the most immediate life-threatening injuries first. This ensures the most efficient use of limited resources and maximizes survival rates. It’s all about maximizing the impact of limited available resources.
Q 15. What is the role of rescue breaths in CPR?
Rescue breaths in CPR are crucial because they provide oxygen to the victim’s lungs and help maintain oxygenation in the blood. Without adequate oxygen, brain damage and death can occur quickly. Think of it like this: chest compressions circulate blood, but rescue breaths supply the oxygen that blood needs to deliver to the body’s vital organs.
In adult CPR, two rescue breaths are given after every 30 chest compressions. The breaths should be slow, deliberate and each breath should take about one second to deliver. You should see the chest rise to indicate that air is entering the lungs. The ratio of compressions to breaths is designed to optimize both oxygen delivery and blood circulation.
It’s important to note that the technique slightly varies for infants and children, where the ratio may differ. Proper training on rescue breathing techniques is absolutely essential for effectively performing CPR.
Career Expert Tips:
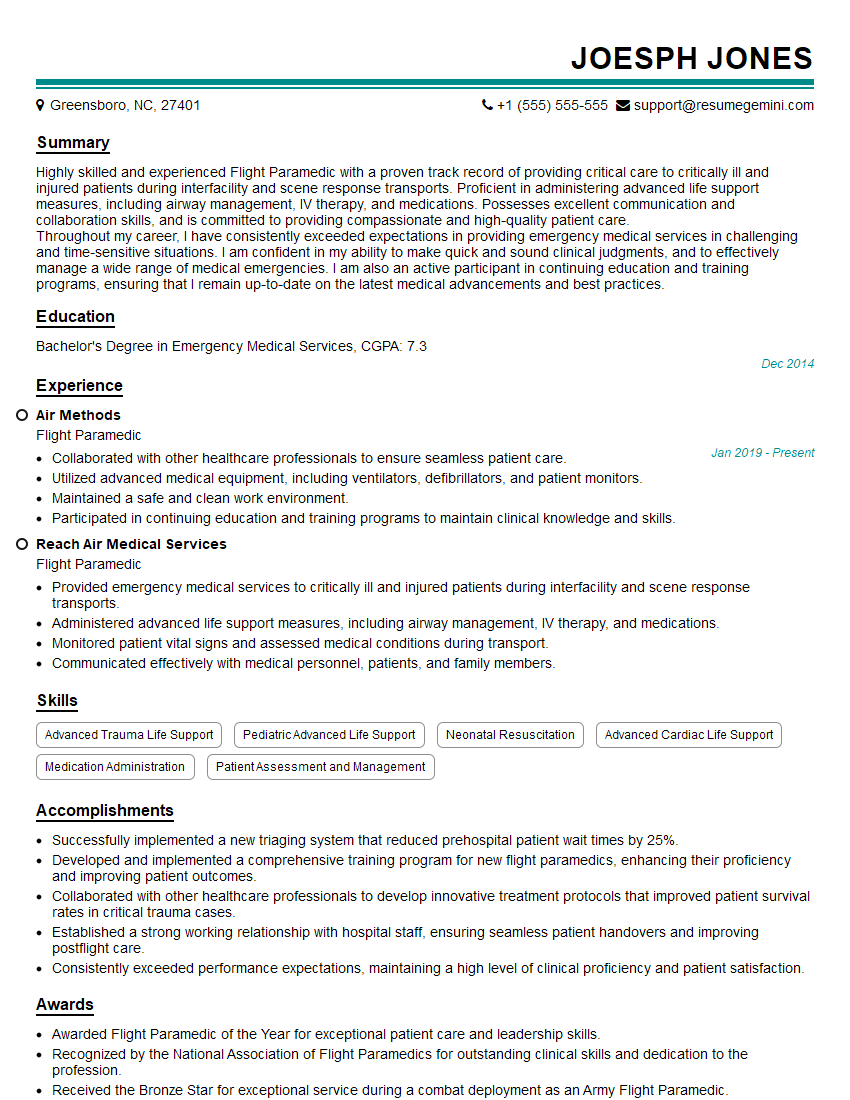
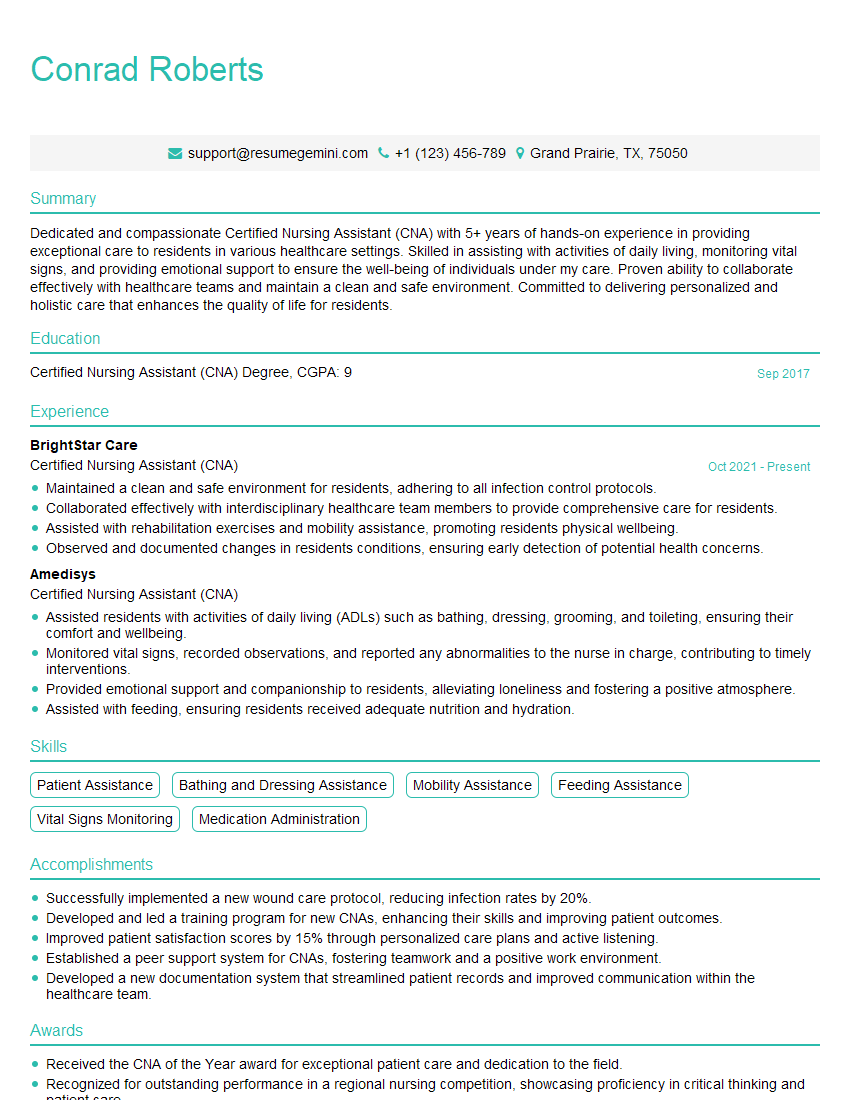
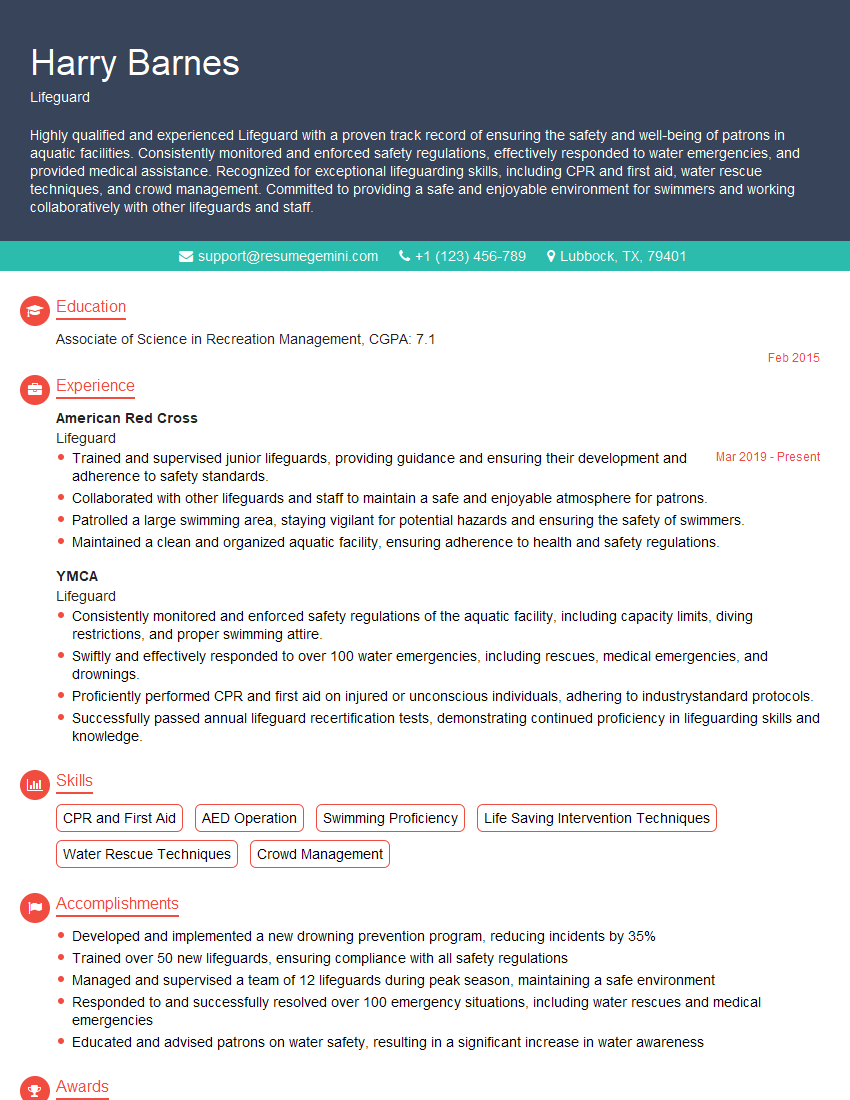
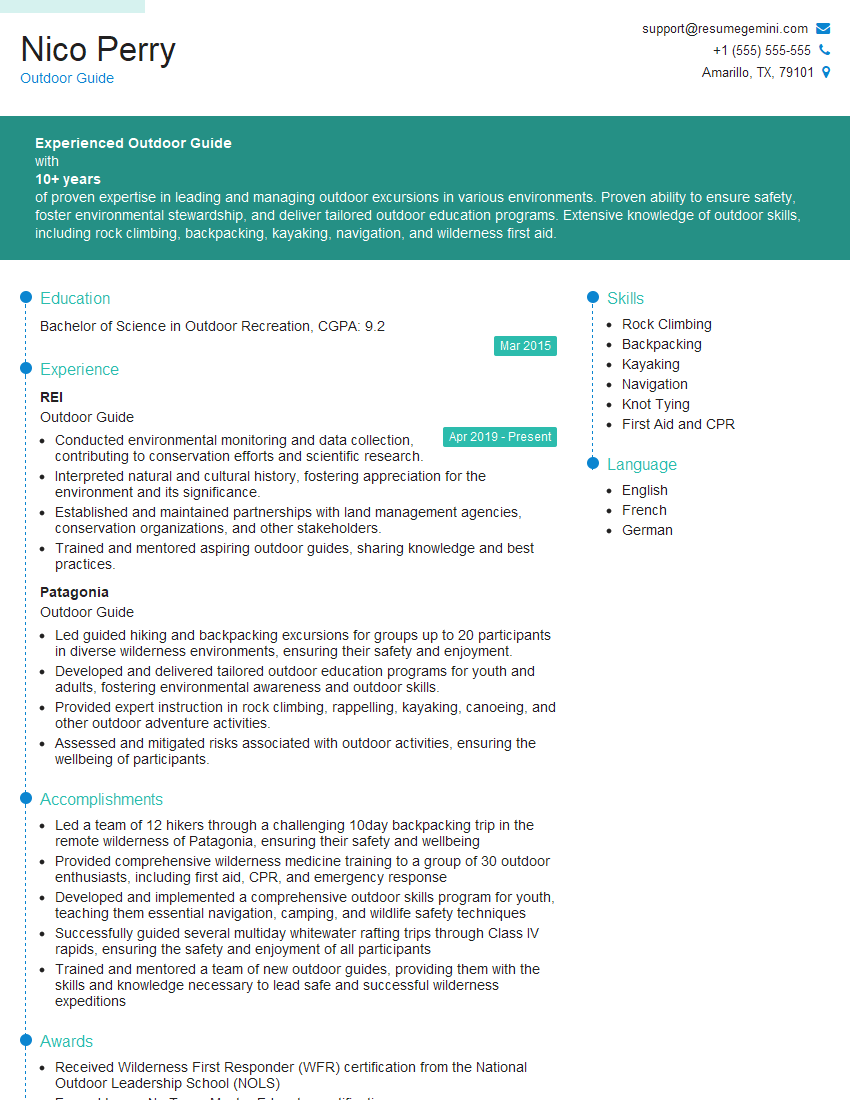
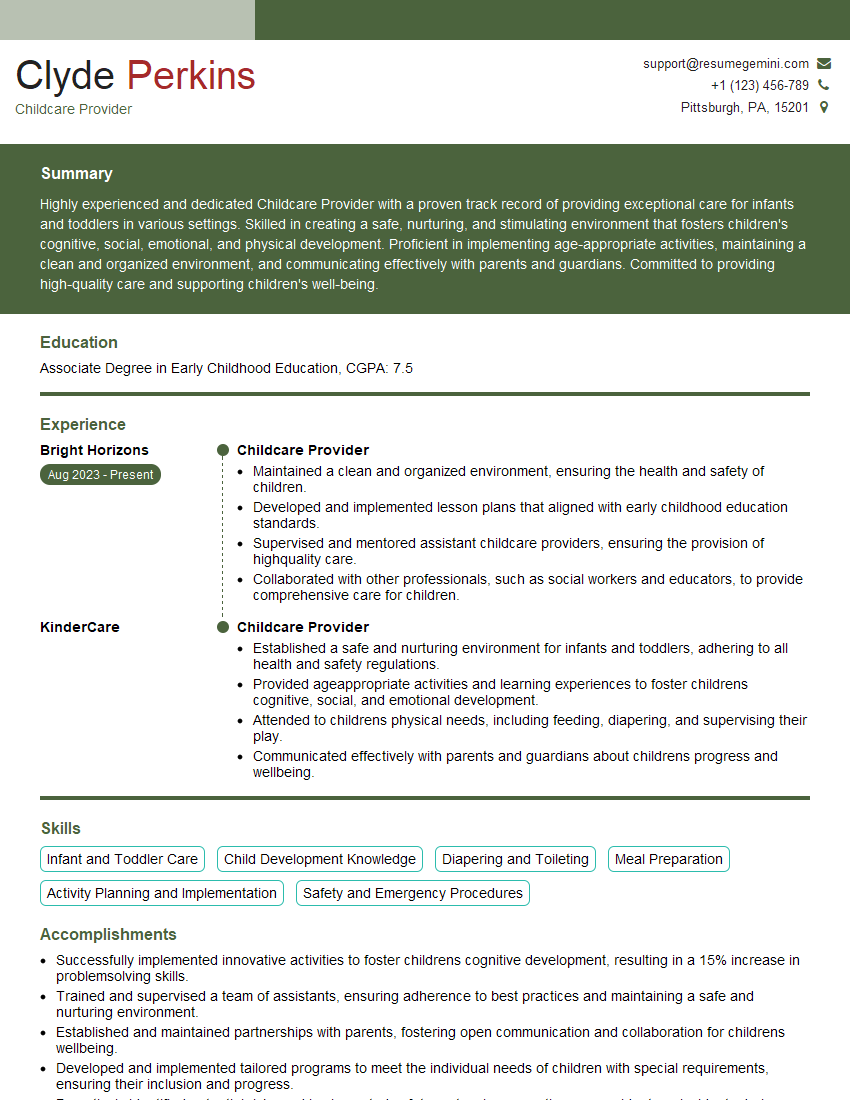
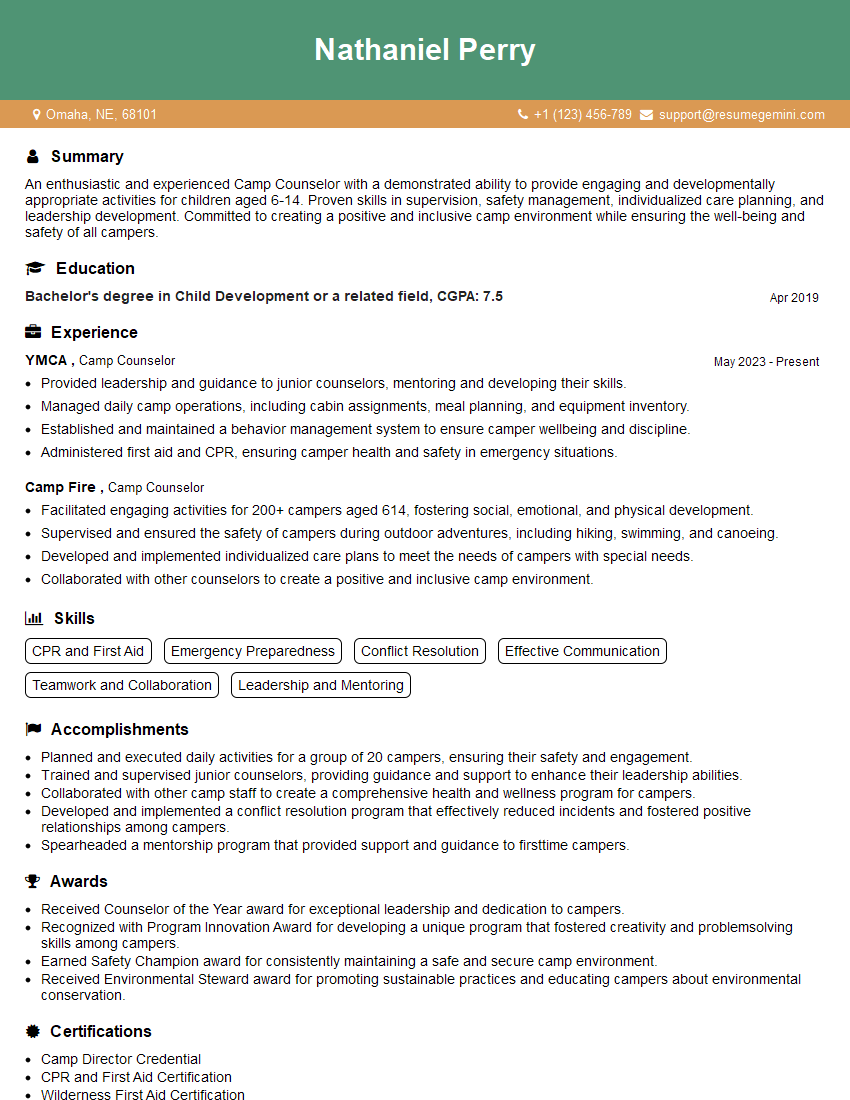
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the limitations of CPR?
CPR, while life-saving, has limitations. It’s not a perfect substitute for a normally functioning heart and lungs. Even with effective CPR, brain damage can occur due to lack of oxygen during the period of cardiac arrest.
- Irreversible damage: If cardiac arrest has lasted for an extended period, the damage to vital organs, particularly the brain, may be irreversible, even with successful resuscitation.
- Underlying conditions: CPR addresses the immediate life-threatening situation but doesn’t treat the underlying cause of cardiac arrest (e.g., a heart attack, drug overdose). Underlying conditions need to be addressed by medical professionals.
- Rib fractures: Vigorous chest compressions can sometimes cause rib fractures, but this is a risk that is accepted in view of the life-threatening situation.
- Effectiveness varies: The effectiveness of CPR depends on various factors, including the quality of the compressions, the time elapsed since cardiac arrest, and the presence of underlying medical conditions.
It is crucial to remember that CPR is a temporary measure; the goal is to buy time until professional medical help arrives.
Q 17. Describe different types of shock and their treatment.
Shock is a life-threatening condition where the body isn’t getting enough blood flow to its organs. There are several types, each with its own cause and treatment:
- Hypovolemic shock: This is caused by significant blood or fluid loss (e.g., from severe bleeding, dehydration, burns). Treatment involves stopping the bleeding, giving fluids intravenously (IV), and possibly blood transfusions.
- Cardiogenic shock: This happens when the heart can’t pump enough blood to meet the body’s needs (e.g., heart attack, heart failure). Treatment includes medication to support heart function, possibly surgery, and mechanical circulatory support.
- Distributive shock (e.g., septic shock, anaphylactic shock, neurogenic shock): This occurs when blood vessels widen excessively, leading to decreased blood pressure. Septic shock results from overwhelming infection, anaphylactic shock from a severe allergic reaction, and neurogenic shock from spinal cord injury. Treatment varies depending on the cause and might involve antibiotics (septic shock), epinephrine (anaphylaxis), and fluids.
- Obstructive shock: This occurs when blood flow is blocked (e.g., pulmonary embolism, cardiac tamponade). Treatment involves addressing the blockage, often requiring emergency surgery or procedures.
In all types of shock, it’s vital to call emergency medical services immediately. While waiting, focus on maintaining the person’s airway, breathing, and circulation (ABCs). Keep the person warm and lying flat with their legs slightly raised (unless a head or spinal injury is suspected).
Q 18. How would you assess a person for spinal injuries?
Assessing for spinal injuries requires a careful and systematic approach, prioritizing the victim’s safety. Avoid unnecessary movement. Here’s how to proceed:
- Check for responsiveness: Gently shake the person’s shoulder and ask, “Are you okay?” If they don’t respond, proceed to the next step.
- Activate emergency services: Call 911 or your local emergency number immediately.
- Stabilize the head and neck: This is crucial to prevent further spinal cord injury. Manually stabilize the head and neck in a neutral position, using your hands to support the head and neck in alignment with the body. Do not move the person unless it is absolutely necessary to protect them from immediate danger.
- Assess breathing and circulation: Check for breathing and a pulse. Begin CPR if necessary, taking care to support the head and neck throughout.
- Observe for signs of spinal injury: Look for obvious signs of trauma, such as deformities, swelling, bruising, or bleeding around the head, neck, or back. Also, assess for neurological symptoms like numbness, tingling, weakness, or paralysis in the extremities.
- Maintain spinal immobilization: Once emergency services arrive, assist them in immobilizing the victim’s spine on a spinal board or other appropriate device.
Remember, the primary focus is on stabilizing the head and neck and preventing any further movement that could worsen a potential spinal injury. This procedure requires proper training. Improper handling could result in further damage.
Q 19. What are some common causes of cardiac arrest?
Cardiac arrest, the sudden cessation of heart function, has several common causes:
- Coronary artery disease (CAD): Blockages in the coronary arteries reduce blood flow to the heart muscle, leading to a heart attack that can cause cardiac arrest.
- Heart rhythm disorders (arrhythmias): Abnormal heart rhythms, such as ventricular fibrillation or ventricular tachycardia, disrupt the heart’s electrical impulses, causing it to stop beating effectively.
- Congenital heart defects: People born with heart defects are at a higher risk of cardiac arrest.
- Drug overdose: Certain drugs can depress the heart’s function and lead to cardiac arrest.
- Trauma: Severe injuries, such as blunt force trauma to the chest, can disrupt the heart’s rhythm.
- Electrocution: Electric shock can disrupt the heart’s electrical activity.
- Severe infections: Sepsis (a severe infection) can trigger cardiac arrest.
This is not an exhaustive list, and often multiple factors contribute to cardiac arrest.
Q 20. What is the purpose of using an AED?
An automated external defibrillator (AED) is a portable electronic device that analyzes the heart’s rhythm and delivers an electric shock (defibrillation) if needed to restore a normal heartbeat. It’s designed for use by lay rescuers in emergency situations such as cardiac arrest. The purpose is to treat life-threatening arrhythmias like ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT), which are often the cause of sudden cardiac arrest. Defibrillation can successfully restart the heart in these situations, significantly improving the chances of survival.
Q 21. How do you operate an AED?
Operating an AED is straightforward, but proper training is essential. Here’s a step-by-step guide:
- Turn on the AED: Follow the device’s instructions to power it on. The device will provide clear voice prompts and visual instructions.
- Attach the pads: Carefully attach the adhesive pads to the victim’s bare chest as indicated on the pads and device. One pad goes on the upper right side of the chest and the other on the lower left side below the armpit.
- Analyze the heart rhythm: The AED will analyze the heart rhythm. Allow the device to complete this analysis. Do not touch the patient during this time.
- Deliver a shock (if advised): If the AED advises a shock, ensure that no one is touching the victim. Then, press the shock button.
- Begin CPR: Immediately after the shock, start CPR (chest compressions and rescue breaths) for two minutes. Then, check for a pulse, and allow the AED to analyze the heart rhythm again.
- Repeat steps 3-5: Continue the cycle of AED analysis, shocking (if advised), and CPR until the victim regains a pulse, or until emergency medical services take over.
Remember, always follow the device’s instructions. Each AED model may have slightly different operation procedures. It’s crucial to undergo proper AED training to ensure safe and effective use.
Q 22. Explain the importance of scene safety.
Scene safety is paramount before administering any first aid or CPR. It’s about protecting yourself and the victim from further harm. Think of it as a crucial first step, like checking the brakes before driving a car. Failing to ensure safety can lead to secondary incidents and impede effective rescue efforts.
- Assess the environment: Look for hazards like traffic, downed power lines, unstable structures, or aggressive animals. For example, if a car accident victim is in the middle of a busy highway, waiting for emergency services in a safe location is essential before approaching.
- Control the scene: If possible, secure the area to prevent others from entering and causing further risks. This could involve directing traffic or asking bystanders to create a safe perimeter.
- Personal Protective Equipment (PPE): Always consider using appropriate PPE such as gloves to avoid contact with bodily fluids. Gloves are a simple precaution but critical in preventing the transmission of diseases.
- Call for help: Once the scene is deemed safe (or as safe as possible), call emergency medical services. This allows professionals with specialized training and equipment to handle the situation.
Q 23. What are your personal limitations and when would you seek additional help?
Recognizing my limitations is crucial for responsible first aid. My training equips me to handle many situations, but I have boundaries. I’m not a medical professional, and my skills are limited to basic life support and first aid techniques. I would seek additional help in several scenarios:
- Unconscious victim: If a person is unconscious, I would prioritize calling for professional help immediately and would only initiate CPR if trained to do so and if there are no obvious signs of trauma.
- Serious injuries: Situations involving severe bleeding, penetrating injuries, broken bones, or suspected spinal injuries are beyond my scope. I would wait for paramedics and provide only basic comfort measures.
- Beyond my skillset: If the situation is beyond my training, such as advanced airway management or the administration of medication, I would immediately defer to trained professionals.
- Personal safety: If the scene becomes unsafe or if my own safety is compromised, I would prioritize my well-being and retreat while calling for help. This ensures I can assist others effectively in the future.
Q 24. Describe your experience handling stressful situations.
Handling stressful situations is a crucial part of this role. My training has equipped me with techniques to manage stress and prioritize tasks during emergencies. I’ve learned to focus on clear thinking and systematic action rather than panic.
For instance, during a mock emergency scenario involving a simulated cardiac arrest, the initial adrenaline rush was significant. However, my training kicked in. I systematically assessed the scene, checked for responsiveness, initiated CPR, and delegated tasks to simulated bystanders. Following this established protocol helped me navigate the pressure and focus on providing the best possible care. The experience reinforced the importance of proper training and calm, deliberate action.
Q 25. How do you stay updated on the latest CPR and first aid guidelines?
Staying current on CPR and first aid guidelines is essential. Medical knowledge is constantly evolving, and techniques are refined for better efficacy and safety. To stay up-to-date, I utilize several methods:
- Continuing education courses: I regularly participate in refresher courses and advanced training programs to maintain and enhance my skills. These courses cover updated guidelines and techniques, and also offer opportunities for hands-on practice.
- Professional organizations: I’m a member of relevant professional organizations that provide updates, publications, and guidelines. This ensures access to current research and best practices.
- Reputable online resources: I review materials from trusted sources such as the American Heart Association (AHA) and the American Red Cross. These organizations release updates and offer online learning modules.
Q 26. What are the legal implications of administering CPR and first aid?
The legal implications of administering CPR and first aid are significant, focusing on the concept of ‘Good Samaritan’ laws. These laws generally protect individuals from liability for providing aid in good faith, as long as their actions are within the scope of their training and not negligent. However, it’s important to understand the nuances.
- Good Samaritan Laws: These laws vary by location and may offer different levels of protection. It’s vital to understand the specific laws in your area.
- Duty to act: In some cases, a duty to act might exist (e.g., for certain professions or if a pre-existing relationship is present), which means there may be legal ramifications for failing to provide aid. However, the vast majority of first aid providers have no duty to act, unless they directly contribute to the harm.
- Negligence: Providing care that is significantly below the accepted standard of care can lead to legal action, regardless of Good Samaritan laws. Acting outside the bounds of your training or causing harm through recklessness can have consequences.
Therefore, staying within the limits of your training, acting reasonably, and obtaining consent (if possible) are critical factors in mitigating legal risks.
Q 27. Explain the importance of documentation after providing first aid.
Documentation after providing first aid is crucial for several reasons. It serves as a record of the event, aids in follow-up care, and can be essential for legal protection. The documentation should be clear, accurate, and objective.
- Patient information: If possible, record the patient’s name, age, and contact information.
- Incident details: Document the time, location, and nature of the incident. Describe the injuries or condition observed.
- Actions taken: Describe the first aid or CPR provided, including the techniques used and the patient’s response.
- Observations: Note any significant observations, such as changes in the patient’s condition.
- Time of EMS arrival: Record the time when emergency medical services arrived at the scene.
This detailed account creates a comprehensive record, minimizing the potential for misunderstandings and supporting claims regarding the care administered. It is best to keep this record safe and private.
Q 28. How would you handle a situation where a patient refuses treatment?
Respecting a patient’s autonomy is vital. If a patient refuses treatment, even if it seems detrimental, I must respect their decision. However, I would follow a structured approach:
- Explain the risks: Clearly and calmly explain the potential consequences of refusing treatment, emphasizing the urgency if appropriate.
- Document the refusal: Thoroughly document the refusal of treatment, including the time, date, and the patient’s statement. Get a witness signature if possible.
- Encourage reconsideration: Gently encourage the patient to reconsider their decision, but do not pressure them.
- Inform EMS: If emergency services are involved, notify them of the patient’s refusal.
- Ensure safety: Assess if there are safety concerns for the patient or others resulting from the refusal. It is necessary to alert emergency services if there is a risk to life.
Ultimately, the choice rests with the patient. My role is to provide information and support their informed decision, ensuring their safety is prioritized as much as possible.
Key Topics to Learn for Performing CPR and First Aid Interviews
- Adult CPR: Understanding the steps involved in chest compressions, rescue breaths, and recognizing cardiac arrest. Practical application: Demonstrating proficiency in CPR techniques using a manikin or through simulations.
- Child and Infant CPR: Differentiating techniques and adapting CPR procedures based on age and size. Practical application: Explaining modifications to hand placement and compression depth for children and infants.
- Choking Rescue: Knowing the Heimlich maneuver for adults, children, and infants. Practical application: Describing the proper technique and differentiating the approach for each age group.
- Bleeding Control: Techniques for stopping different types of bleeding, including direct pressure, elevation, and tourniquet application (when appropriate). Practical application: Explaining the decision-making process in choosing the most appropriate method for a given bleeding injury.
- Wound Care: Basic wound cleaning and dressing procedures. Practical application: Describing the steps for proper wound assessment and management, including prevention of infection.
- Shock Management: Recognizing and responding to shock. Practical application: Explaining the signs and symptoms of shock and outlining appropriate first aid measures.
- Legal and Ethical Considerations: Understanding Good Samaritan laws and the importance of obtaining consent (when possible). Practical application: Discussing scenarios that may present ethical dilemmas in a first aid situation.
- AED Operation: Safe and effective use of an automated external defibrillator (AED). Practical application: Describing the step-by-step process of using an AED, including safety precautions.
- Team Dynamics and Communication: Effectively communicating with patients, bystanders, and emergency medical services (EMS). Practical application: Describing effective communication strategies in stressful situations.
Next Steps
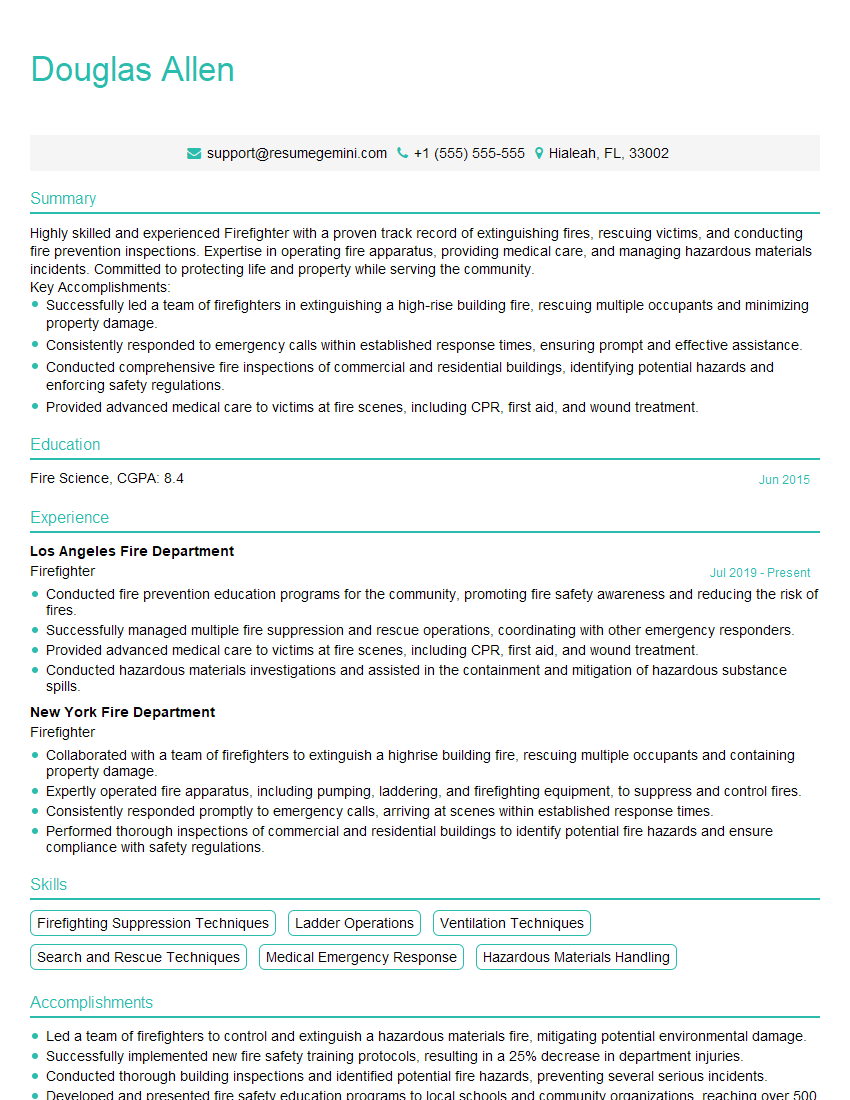
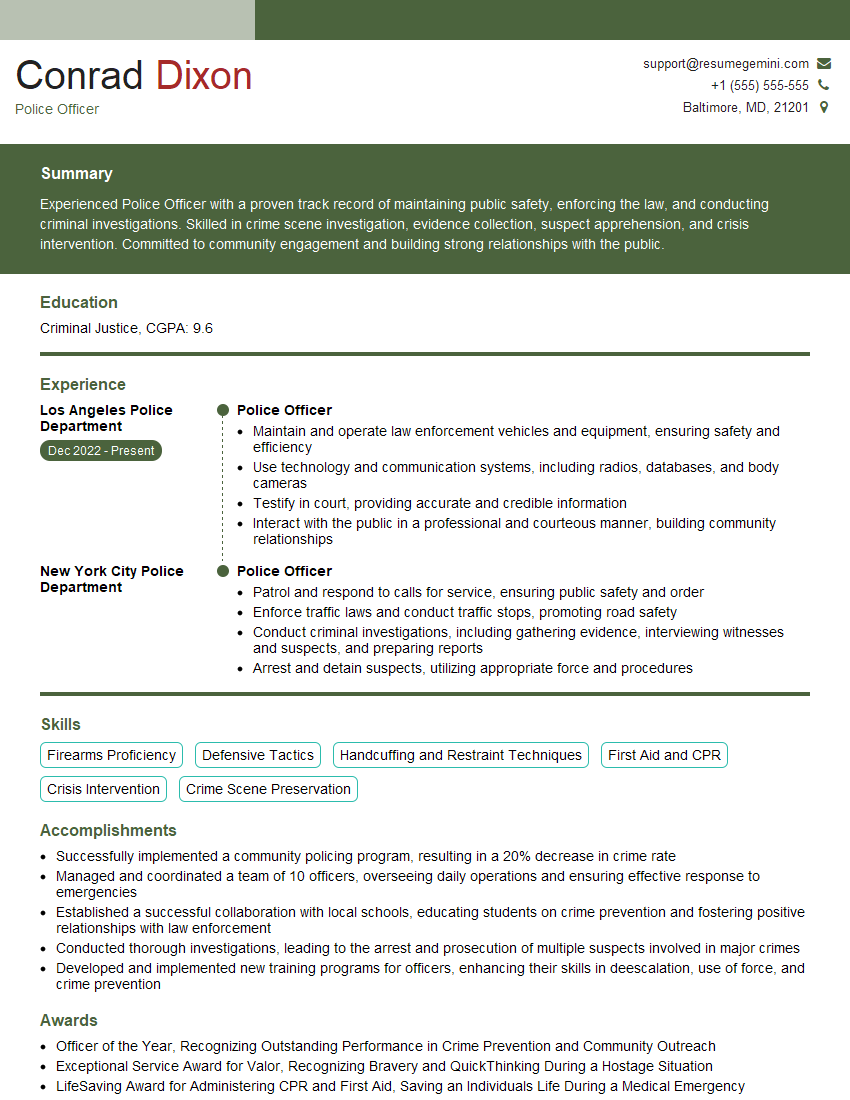
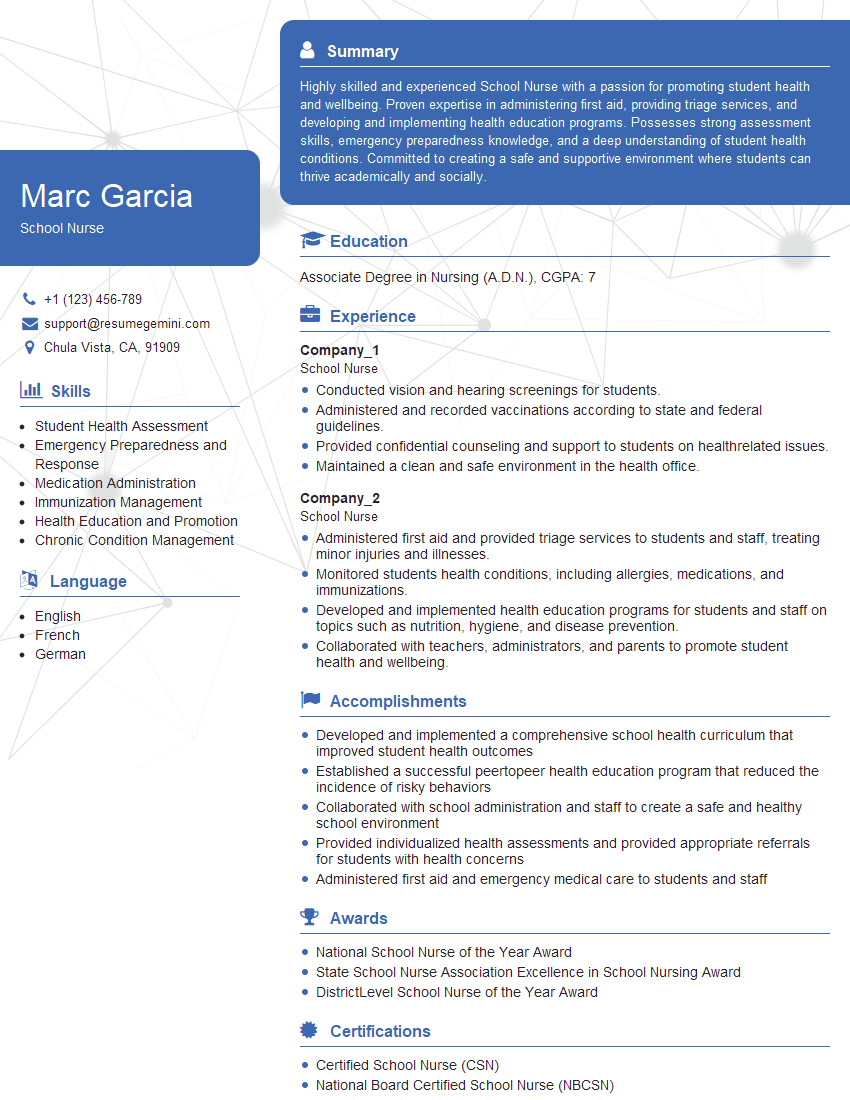
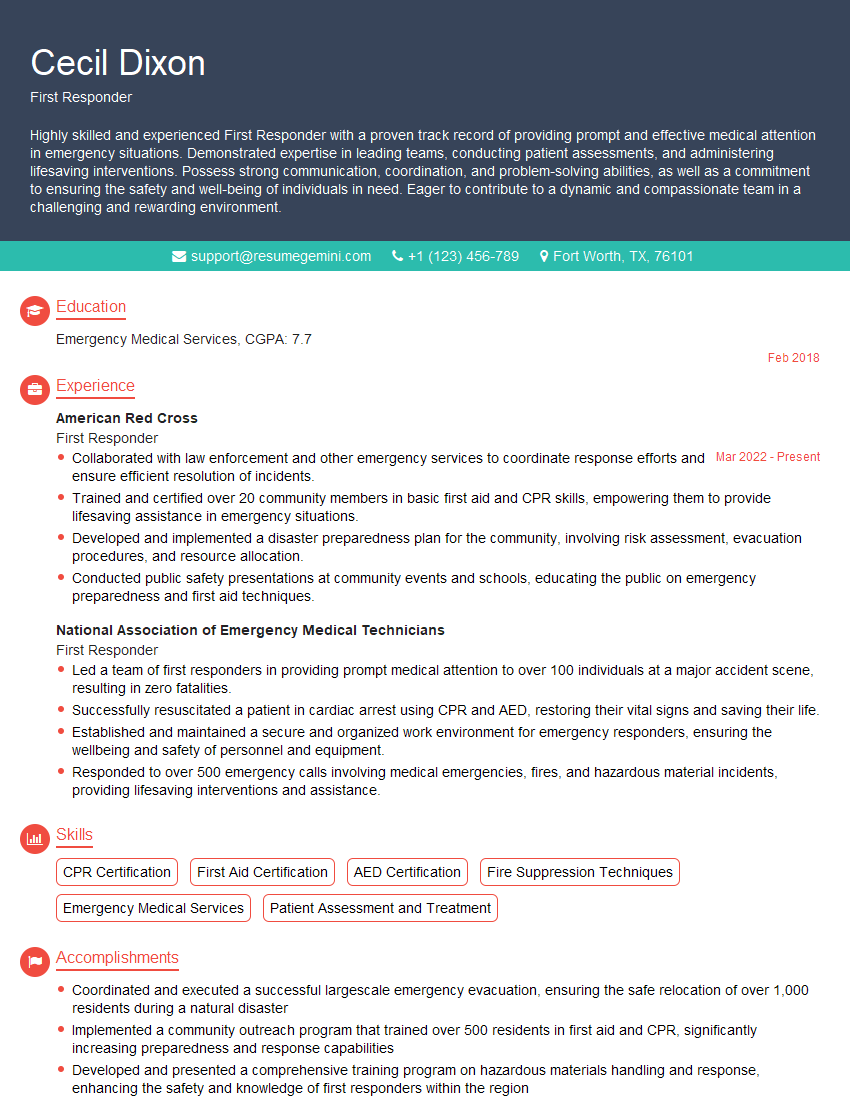
Mastering CPR and first aid significantly enhances your value as a candidate in various healthcare and safety-related roles. It demonstrates commitment to patient well-being and a readiness to act decisively in emergency situations. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. They provide examples of resumes tailored to Performing CPR and first aid certifications and experience, giving you a strong foundation for building your own. Take the next step toward your career goals today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good