Preparation is the key to success in any interview. In this post, we’ll explore crucial Pharmaceutical Quality Assurance (PQA) interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Pharmaceutical Quality Assurance (PQA) Interview
Q 1. Describe your experience with Good Manufacturing Practices (GMP).
Good Manufacturing Practices (GMP) are a set of guidelines that ensure the consistent quality of manufactured products. Think of them as the recipe for producing safe and effective pharmaceutical products. My experience spans over [Number] years, encompassing various roles within the pharmaceutical industry. I’ve been involved in implementing and maintaining GMP compliance across different manufacturing sites, working with diverse product types ranging from tablets and capsules to sterile injectables. This involved reviewing and updating standard operating procedures (SOPs), conducting audits, and actively participating in process improvements to ensure consistent adherence to GMP principles. For instance, in my previous role, I was instrumental in implementing a new cleaning validation program that significantly reduced the risk of cross-contamination, ensuring product quality and patient safety. Another example involved training staff on the proper documentation and handling procedures, contributing to increased GMP compliance across the board.
Q 2. Explain the difference between Quality Control and Quality Assurance.
While both Quality Control (QC) and Quality Assurance (QA) aim for product quality, they approach it differently. QC is like a quality ‘inspector’; they test the finished product to ensure it meets predefined specifications. They are the ones performing tests to verify the product’s purity, potency, and other critical attributes. QA, on the other hand, is more proactive. It’s like the ‘quality architect’; it oversees the entire manufacturing process to prevent problems *before* they occur. QA focuses on systems, procedures, and training to ensure the manufacturing process itself is robust and reliable. Think of it this way: QC checks the final product; QA makes sure the process that creates the product is sound. A simple analogy is building a house. QC checks if the walls are straight and the roof doesn’t leak. QA ensures that the blueprints are accurate, the construction workers are properly trained and follow safety regulations.
Q 3. How do you ensure compliance with regulatory requirements (e.g., FDA, EMA)?
Ensuring compliance with regulatory requirements, such as those from the FDA and EMA, is paramount. This involves a multi-faceted approach. First, we must thoroughly understand the relevant regulations and guidelines for each product and its intended market. This includes staying up-to-date on any changes or updates. Second, we implement robust systems and procedures to demonstrate compliance. This covers everything from documentation and record-keeping to equipment calibration and validation. Regular internal audits are conducted to identify areas needing improvement and potential compliance gaps. We also proactively engage with regulatory agencies through submissions, responding to queries, and participating in inspections. I have direct experience in navigating FDA and EMA inspections, successfully addressing their findings and demonstrating our commitment to compliance. We use a system of documented procedures, training and audits, supplemented by software that tracks regulatory updates and compliance status. This provides a clear and auditable trail of compliance efforts.
Q 4. Describe your experience with deviation investigations.
Deviation investigations are crucial for identifying the root cause of any unexpected event that deviates from established procedures or specifications. My experience includes leading and participating in numerous deviation investigations across various manufacturing processes. The process typically involves a structured approach: First, we thoroughly document the deviation, gathering all relevant data. Second, we conduct a thorough investigation, following established protocols and employing tools like fault tree analysis or ‘5 Whys’ to identify the root cause. Third, we develop a comprehensive report summarizing the findings, root cause analysis, and proposed corrective actions. For example, in one investigation involving a batch failure, we used the 5 Whys method to trace the issue to a faulty piece of equipment and then developed a comprehensive CAPA plan to prevent it from happening again. The entire investigation and corrective actions are thoroughly documented and reviewed to ensure effectiveness.
Q 5. What is your experience with CAPA (Corrective and Preventive Actions)?
Corrective and Preventive Actions (CAPA) are critical for preventing recurrence of deviations or other quality issues. My experience shows a proficiency in developing, implementing, and verifying the effectiveness of CAPAs. This involves ensuring that the root cause is properly identified and addressed and that corrective actions are implemented and verified for effectiveness. For instance, in response to a recurring issue with tablet weight variation, we implemented a CAPA plan that involved recalibrating the equipment, retraining the operators, and improving the process parameters. We also established a system of monitoring and review to track the effectiveness of the implemented corrective actions and evaluate the need for preventive actions. A key element of a successful CAPA system is continuous monitoring to ensure the effectiveness of corrective and preventive actions. We use a CAPA tracking system that allows us to monitor the status of each CAPA and measure effectiveness.
Q 6. Explain your understanding of change control processes.
Change control is a systematic approach to managing any proposed modifications to manufacturing processes, equipment, or materials. It’s vital for ensuring that changes are implemented safely and without compromising product quality or compliance. My experience encompasses developing and managing change control processes which involves a step-by-step approach; first, a change request is submitted and reviewed to assess the potential impact on product quality and compliance. Then, a risk assessment is conducted, determining the need for additional testing or validation. Following approval, the changes are implemented, and a post-implementation review is performed to verify the effectiveness and identify any unintended consequences. For example, we successfully implemented a change to our manufacturing process by carefully following our change control process which included a thorough risk assessment, cross-functional team review, and post-implementation validation, ultimately improving efficiency and product quality without jeopardizing patient safety.
Q 7. How do you handle quality complaints?
Handling quality complaints efficiently and effectively is paramount for maintaining product reputation and patient safety. My experience includes managing quality complaints, from initial receipt to final resolution. The process usually begins with acknowledging the complaint, documenting all details, and conducting a thorough investigation into the nature of the complaint and whether it involves a potential quality defect. This is followed by a root cause analysis to determine the underlying causes of the complaint. Corrective actions are implemented to prevent similar incidents from recurring. Depending on the severity, the complaint may involve regulatory reporting. For example, in a case of a reported allergic reaction to our product, we followed a rigorous investigation, notifying regulatory authorities and initiating a recall if needed. Transparency and prompt communication with the affected individuals and relevant authorities were always prioritized.
Q 8. Describe your experience with document control systems.
Document control systems are the backbone of any regulated industry, ensuring version control, accuracy, and accessibility of crucial documents. My experience encompasses working with various systems, from simple shared drives with version numbering to sophisticated Electronic Document Management Systems (EDMS). I’ve been involved in the implementation, maintenance, and improvement of these systems. For example, in a previous role, we transitioned from a paper-based system to an EDMS. This involved not only the technical migration of documents but also the significant task of training staff on the new system, developing standard operating procedures (SOPs) for its use, and implementing robust change control processes to ensure document integrity.
- Version Control: Ensuring only the most current version of a document is accessible and identifying previous versions for audit trails.
- Change Control: Implementing a process for reviewing, approving, and distributing changes to documents, ensuring that all stakeholders are aware of updates.
- Access Control: Defining who can view, edit, or approve specific documents based on roles and responsibilities. This involves creating user groups with different permission levels.
- Document Retention: Establishing policies for storing and archiving documents, adhering to regulatory requirements (e.g., ALCOA+).
In practice, this involves regularly reviewing and updating the document control system, performing audits, and actively participating in continuous improvement initiatives.
Q 9. How do you ensure data integrity in a pharmaceutical setting?
Data integrity in pharmaceuticals is paramount. It means ensuring that data is complete, consistent, accurate, reliable, and trustworthy throughout its lifecycle. This is crucial for regulatory compliance and patient safety. My approach involves a multi-faceted strategy:
- ALCOA+ Principles: Adhering to the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate + Complete, Consistent, Enduring, Available) is fundamental. This forms the foundation of all data handling practices.
- SOPs and Training: Implementing and regularly updating Standard Operating Procedures (SOPs) that clearly define how data should be collected, recorded, reviewed, and archived. Thorough training of personnel is essential to ensure consistent adherence to these procedures.
- Validation of Systems: All systems used for data generation and management (e.g., LIMS, Chromatography Data Systems) must be validated to ensure they perform as intended and produce reliable results. This includes IQ, OQ, and PQ.
- Audit Trails: Maintaining comprehensive audit trails for all data modifications and access. This allows tracking changes and identifying potential discrepancies.
- Data Backup and Recovery: Implementing robust data backup and recovery procedures to protect against data loss.
- Deviation Management: Establishing a systematic approach to investigating and documenting any deviations from established procedures.
For instance, imagine a situation where a chromatograph produces an unexpected result. A thorough investigation, including review of the audit trail, would be conducted to determine the root cause. If a data integrity issue is identified, a corrective action and preventive action (CAPA) plan would be implemented to prevent recurrence.
Q 10. What is your experience with audits (internal and external)?
I have extensive experience with both internal and external audits. Internal audits are crucial for proactively identifying areas for improvement within our quality system. External audits, conducted by regulatory agencies or clients, assess compliance with regulatory requirements and good manufacturing practices (GMP).
- Internal Audits: I’ve led and participated in numerous internal audits, developing audit plans, conducting audits, and preparing audit reports. These reports help identify gaps in our systems and provide recommendations for improvement.
- External Audits: I’ve been involved in numerous external audits, providing documentation, answering questions from auditors, and working to address any findings. Successful navigation of these audits requires thorough preparation and a deep understanding of regulatory requirements.
- CAPA Implementation: Following both internal and external audits, I actively participate in implementing Corrective and Preventive Actions (CAPAs) to address any identified deficiencies.
A recent example involved an external audit where a minor discrepancy was found in our documentation. By proactively addressing the issue and providing clear evidence of our corrective actions, we successfully demonstrated our commitment to GMP and achieved a positive audit outcome. The experience highlighted the importance of meticulous record keeping and continuous improvement.
Q 11. Explain your understanding of validation processes (e.g., equipment, cleaning).
Validation is a critical aspect of pharmaceutical quality assurance, demonstrating that equipment and processes consistently perform as intended. This involves a series of tests and documentation to prove the reliability and suitability of systems.
- Equipment Validation: This process verifies that equipment is properly installed, operates within specified parameters, and consistently produces accurate and reliable results. It typically involves Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ).
- Cleaning Validation: This ensures that cleaning procedures effectively remove residues from equipment, preventing cross-contamination. This often involves testing for residue limits using appropriate analytical methods.
For example, validating a high-performance liquid chromatograph (HPLC) would involve verifying that the instrument meets manufacturer specifications (IQ), demonstrating that it operates correctly under various conditions (OQ), and proving that it consistently produces accurate and precise results within defined limits (PQ). Cleaning validation of a reactor might involve assessing the effectiveness of a cleaning procedure in removing residual drug product, employing techniques like swab tests and rinse samples.
Q 12. Describe your experience with statistical process control (SPC).
Statistical Process Control (SPC) is a powerful tool for monitoring and controlling manufacturing processes. It uses statistical methods to identify trends, variations, and potential problems before they significantly impact product quality. My experience with SPC includes designing control charts, analyzing data, and interpreting results to identify opportunities for process improvement.
- Control Charts: I’m proficient in designing and interpreting various control charts, including X-bar and R charts, and individuals and moving range charts, to monitor key process parameters (KPIs).
- Data Analysis: I use statistical software to analyze process data and identify trends, patterns, and sources of variation.
- Process Improvement: I apply SPC principles to identify areas for improvement and implement changes to reduce process variability and improve product quality.
For example, in a tablet manufacturing process, we used SPC to monitor tablet weight and hardness. By analyzing control charts, we identified a trend of increasing variability in tablet weight. This led to an investigation that uncovered a problem with the tablet press feeder, which was subsequently corrected. This prevented the production of out-of-specification tablets and ensured consistent product quality.
Q 13. How do you manage supplier quality?
Managing supplier quality is critical for ensuring the quality of our own products. My approach involves a multi-faceted strategy focused on supplier selection, qualification, and ongoing monitoring.
- Supplier Selection: Selecting reliable suppliers who meet our quality standards involves careful evaluation of their capabilities, track record, and quality systems.
- Supplier Qualification: We conduct thorough audits of our suppliers to assess their compliance with GMP and our quality requirements. This often involves reviewing their quality systems, manufacturing processes, and documentation.
- Ongoing Monitoring: We continuously monitor the quality of materials and services received from our suppliers through regular inspections, testing, and performance reviews. This involves evaluating metrics such as on-time delivery, quality of materials, and responsiveness to issues.
- Supplier Performance Metrics: Tracking key performance indicators (KPIs) enables us to identify trends and address any supplier performance issues proactively.
For instance, if a supplier consistently fails to meet our specifications for a critical raw material, we would implement corrective actions, such as working with the supplier to identify and address the root cause of the problem, or considering alternative suppliers.
Q 14. Explain your understanding of risk assessment methodologies.
Risk assessment methodologies are essential for identifying, analyzing, and mitigating potential risks that could impact product quality, patient safety, or regulatory compliance. My experience involves applying various risk assessment tools and techniques, such as Failure Mode and Effects Analysis (FMEA) and Hazard Analysis and Critical Control Points (HACCP).
- FMEA: This systematic approach identifies potential failure modes, their effects, and their severity, occurrence, and detectability. This allows us to prioritize risks and implement appropriate controls.
- HACCP: This focuses on identifying critical control points (CCPs) in processes that could lead to hazards. This methodology is commonly used in the food and pharmaceutical industries to manage food safety risks, adapting well to various manufacturing processes.
- Risk Matrix: This involves assigning risk scores based on the likelihood and impact of potential events, allowing for prioritization of mitigation efforts.
For example, during the development of a new drug product, we use FMEA to identify potential risks associated with the manufacturing process. This includes risks related to equipment failures, raw material variability, and human error. By prioritizing these risks based on their severity, occurrence, and detectability, we can implement appropriate controls to mitigate their impact.
Q 15. What is your experience with root cause analysis techniques?
Root cause analysis (RCA) is crucial in PQA for identifying the underlying reasons behind deviations or failures, preventing recurrence. I’m proficient in several techniques, including the 5 Whys, Fishbone diagrams (Ishikawa diagrams), Fault Tree Analysis (FTA), and Failure Mode and Effects Analysis (FMEA).
For instance, if a batch of tablets fails dissolution testing, I wouldn’t just address the immediate issue (low dissolution). Instead, using the 5 Whys, I’d systematically investigate: Why was the dissolution low? (Insufficient granulation). Why was the granulation insufficient? (Incorrect binder concentration). Why was the binder concentration incorrect? (Weighing error). Why was there a weighing error? (Malfunctioning balance). This reveals the root cause: a malfunctioning balance. Similarly, FTA would visually map potential causes leading to that failure, helping to prevent future similar occurrences.
My experience spans various applications, from investigating manufacturing equipment malfunctions to analyzing deviations in analytical testing and supply chain issues. Each technique’s effectiveness depends on the complexity of the problem; often, a combination is most effective.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with laboratory testing and analysis.
My laboratory experience encompasses a wide range of analytical techniques vital in pharmaceutical quality control, including HPLC (High-Performance Liquid Chromatography), GC (Gas Chromatography), UV-Vis spectroscopy, titrations, and dissolution testing. I’m familiar with both routine testing and more complex analyses like impurity profiling and stability studies. I have a strong understanding of method validation and qualification, ensuring that our testing methods are accurate, precise, and reliable.
For example, I’ve extensively worked on HPLC method validation for various active pharmaceutical ingredients (APIs) and excipients. This involved evaluating parameters such as linearity, accuracy, precision, specificity, and robustness to guarantee reliable quantitative analysis. I also have experience in troubleshooting analytical instruments and maintaining equipment calibration records.
Q 17. How do you ensure the accuracy and reliability of test results?
Ensuring accurate and reliable test results is paramount in PQA. It relies on a multi-pronged approach:
- Method Validation: Rigorous validation of analytical methods ensures accuracy and precision. This involves confirming the method’s suitability for its intended purpose.
- Calibration and Maintenance: Regular calibration and preventative maintenance of analytical instruments are essential to maintain accuracy and prevent errors. We follow strict calibration schedules and maintain comprehensive records.
- Quality Control Samples: Using quality control samples, including blanks, standards, and replicates, allows for ongoing monitoring of instrument performance and method accuracy. Out-of-specification results trigger investigations.
- Standard Operating Procedures (SOPs): Clear and well-defined SOPs ensure that all testing procedures are performed consistently and correctly, minimizing human error.
- Data Integrity: Maintaining data integrity is crucial. This means ensuring data is accurate, complete, consistent, and reliable. This includes proper data recording, handling, and review processes.
- Audits and Inspections: Internal and external audits help identify areas for improvement and ensure compliance with regulatory requirements.
Think of it like baking a cake – you need precise measurements, calibrated tools (oven thermometer), and a proven recipe (SOP) to ensure the final product meets expectations. Any deviation triggers an investigation (RCA).
Q 18. Explain your understanding of quality metrics and KPIs.
Quality metrics and Key Performance Indicators (KPIs) are vital for monitoring and improving quality performance. In PQA, we use various metrics to track aspects like product quality, manufacturing efficiency, and compliance. Some examples include:
- Defect rate: The percentage of non-conforming products.
- On-time delivery rate: The percentage of products delivered on schedule.
- Process capability: Measures the ability of a process to consistently produce products within specifications.
- Out-of-specification (OOS) rate: The frequency of test results outside established limits.
- Number of deviations and CAPAs (Corrective and Preventive Actions): Tracks the frequency and effectiveness of corrective actions for quality issues.
These metrics are regularly reviewed and analyzed to identify trends, pinpoint areas for improvement, and demonstrate compliance. For example, a high OOS rate may indicate a problem with an analytical method, equipment, or manufacturing process requiring immediate investigation.
Q 19. How do you handle non-conformances?
Handling non-conformances is a critical aspect of PQA. My approach involves a structured process:
- Immediate containment: Isolate the non-conforming material to prevent further distribution or use.
- Investigation: Conduct a thorough investigation to determine the root cause of the non-conformance using RCA techniques.
- Corrective action: Implement corrective actions to prevent recurrence of the issue. This may include equipment repairs, process changes, or employee retraining.
- Preventive action: Develop preventive actions to prevent similar problems in the future. This often involves process improvements or system enhancements.
- Documentation: Maintain detailed documentation of the entire process, including the investigation, corrective actions, preventive actions, and verification of effectiveness.
- Disposition: Determine the appropriate disposition of the non-conforming material (e.g., rework, rejection, quarantine).
Imagine a batch of tablets that fails weight uniformity testing. We’d immediately quarantine the batch, investigate (using RCA) to pinpoint the root cause (e.g., malfunctioning tablet press), implement corrective actions (repair or replace the press), prevent recurrence (implement a preventive maintenance schedule), and document everything. The batch’s ultimate fate would then be determined based on the severity of the non-conformances.
Q 20. Describe your experience with quality management systems (QMS).
Quality Management Systems (QMS) are the backbone of pharmaceutical quality assurance. My experience includes working with QMS compliant with Good Manufacturing Practices (GMP) guidelines, such as ISO 9001 and other industry-specific standards. I understand the importance of establishing, implementing, and maintaining a comprehensive QMS that covers all aspects of product development, manufacturing, and quality control.
This includes developing and revising SOPs, conducting internal audits, managing change control processes, handling deviations and CAPAs, and ensuring compliance with regulatory requirements. I’m familiar with electronic QMS (eQMS) software, which streamlines various processes and documentation management. A well-defined QMS is like a blueprint, ensuring everything runs smoothly and efficiently, ultimately producing high-quality products consistently and safely.
Q 21. Explain your understanding of the different types of pharmaceutical documentation.
Pharmaceutical documentation is extensive and critical for traceability and regulatory compliance. I’m familiar with various types, including:
- Batch Records: Detailed records of all manufacturing steps for each batch of product.
- Standard Operating Procedures (SOPs): Written instructions for performing routine tasks.
- Analytical Method Validation Reports: Documents demonstrating the validity of analytical methods.
- Deviation Reports: Documents describing any deviation from standard procedures.
- Change Controls: Documents describing changes made to products, processes, or equipment.
- Corrective and Preventive Action (CAPA) Reports: Documents describing the investigation, root cause analysis, corrective, and preventive actions taken to address quality issues.
- Stability Reports: Documents describing the stability of a drug product over time.
- Master Batch Records: Template for the manufacturing of the product.
Each document serves a specific purpose in ensuring product quality, safety, and regulatory compliance. Maintaining accurate, complete, and readily accessible documentation is crucial for audits and investigations.
Q 22. What is your experience with LIMS (Laboratory Information Management System)?
My experience with LIMS (Laboratory Information Management System) is extensive. I’ve worked with several different LIMS platforms throughout my career, including [mention specific LIMS e.g., Thermo Fisher’s SampleManager, LabWare LIMS], and I’m proficient in their core functionalities. This includes sample management, instrument integration, data analysis, and reporting. I understand the critical role LIMS plays in ensuring data integrity and traceability within a regulated environment. For instance, in my previous role at [Previous Company Name], I was instrumental in implementing a new LIMS system, leading the training program for 30+ lab personnel and ensuring seamless data migration from the legacy system. This involved meticulous data validation and verification to ensure the accuracy and reliability of all transferred data. Beyond data entry and retrieval, I’m experienced in configuring workflows, customizing reports, and troubleshooting system issues. My expertise extends to using LIMS data for trend analysis and identifying potential process deviations, which is invaluable for proactive quality control.
Q 23. How do you ensure the security and confidentiality of pharmaceutical data?
Ensuring the security and confidentiality of pharmaceutical data is paramount. We adhere to strict guidelines, including those stipulated by 21 CFR Part 11 and other relevant regulations. This involves a multi-layered approach. Firstly, access control is crucial. We implement role-based access, meaning users only have access to the data necessary for their roles. Secondly, data encryption both in transit and at rest is fundamental. We utilize robust encryption protocols to protect data from unauthorized access. Thirdly, we maintain detailed audit trails of all data modifications, ensuring complete traceability. Any changes made to the data are logged, including the user, timestamp, and the nature of the change. Regular security audits and penetration testing are conducted to identify and mitigate vulnerabilities. We also have strict policies regarding data backup and disaster recovery to ensure data availability and business continuity. Finally, employee training on data security best practices is an ongoing process. Think of it like a fortress – multiple layers of protection working together to safeguard our valuable data.
Q 24. Explain your understanding of the lifecycle of a pharmaceutical product.
The lifecycle of a pharmaceutical product is a complex journey encompassing several key stages. It begins with Research & Development, where the drug is conceived, developed, and tested in pre-clinical studies. Next comes Pre-clinical testing, followed by Clinical Trials (Phase I, II, III) to evaluate safety and efficacy in humans. Once approved by regulatory bodies like the FDA, the product enters the Manufacturing stage, adhering strictly to Good Manufacturing Practices (GMP). This involves selecting appropriate raw materials, manufacturing the drug substance and drug product, and conducting thorough quality control testing. The Post-Market Surveillance phase is crucial, where we continually monitor the product’s safety and effectiveness, addressing any adverse events or quality issues promptly. Finally, the product may eventually enter the Product Life Cycle Management phase, which may involve reformulation, line extensions, or eventually, discontinuation. Each stage has specific regulatory requirements and quality control checkpoints to ensure patient safety and product quality.
Q 25. Describe your experience with process improvement initiatives.
I have a proven track record in process improvement initiatives. In my previous role, we identified a significant bottleneck in our stability testing process, leading to delays in product release. Using Lean Six Sigma methodologies, we mapped the current state, identified waste, and implemented a new workflow. This included optimizing sample handling, streamlining data entry, and automating certain tasks using LIMS capabilities. The result was a 25% reduction in turnaround time for stability testing without compromising data integrity. Another example involves improving our non-conformance reporting process. We implemented a new electronic system which automated several steps, reduced manual errors and provided better data analysis to identify root causes and prevent recurrence. I am proficient in various process improvement tools, such as Value Stream Mapping, 5 Whys analysis, and Kaizen events, and I am always eager to apply them to enhance efficiency and quality.
Q 26. What is your experience with training and development in a QA/QC environment?
Training and development in a QA/QC environment are vital. I’ve been involved in designing, implementing, and delivering training programs on various topics, including GMP, SOPs (Standard Operating Procedures), data integrity, and regulatory compliance. I use a blended learning approach, combining classroom sessions with hands-on training and e-learning modules, ensuring comprehensive knowledge transfer. At [Previous Company], I developed a comprehensive training program for new QA/QC personnel, resulting in improved compliance and reduced error rates. The training modules were regularly updated to reflect regulatory changes and new technologies, and included interactive exercises and case studies to enhance engagement and knowledge retention. I believe in continuous professional development, not just for myself but also for the team, thereby fostering a culture of learning and improvement.
Q 27. How do you stay up-to-date with current regulatory changes?
Staying abreast of current regulatory changes is crucial in PQA. I regularly monitor publications from regulatory agencies like the FDA, EMA (European Medicines Agency), and WHO (World Health Organization). I subscribe to industry-specific newsletters and journals, attend conferences and webinars, and actively participate in professional organizations like [mention relevant professional organization]. I also leverage online resources and databases to access the latest regulatory updates and guidance documents. Keeping up-to-date with these changes allows me to anticipate potential impacts on our processes and ensures our compliance with the latest regulations. This proactive approach is vital for maintaining the quality and safety of our pharmaceutical products.
Q 28. Describe a situation where you had to resolve a significant quality issue.
In one instance, we discovered a significant discrepancy in the results of a critical assay during the batch release testing of a new product. The initial results were outside the acceptance criteria. Following our established deviation procedures, we initiated a thorough investigation. We first verified the testing equipment calibration, reviewed the raw data, and re-analyzed the samples using alternative methods. We interviewed the personnel involved, checked for any procedural deviations, and examined the raw materials. After meticulous investigation, we traced the issue to a malfunctioning piece of equipment that hadn’t been properly calibrated. Once the equipment was fixed, the subsequent testing results fell within the acceptance criteria, confirming the root cause. We implemented corrective actions, including recalibrating all similar equipment and reinforcing training on proper equipment maintenance and calibration procedures. The incident underscored the importance of rigorous data review, thorough investigation, and adherence to established deviation management protocols. A robust root cause analysis was documented, and preventive actions implemented to avoid recurrence.
Key Topics to Learn for Pharmaceutical Quality Assurance (PQA) Interview
- Good Manufacturing Practices (GMP): Understand the core principles and regulations governing pharmaceutical manufacturing, including FDA guidelines and ICH Q7.
- Quality Control (QC) Testing: Become familiar with various analytical techniques used in QC, their applications, and interpretation of results. Consider practical examples like HPLC, titrations, and microbiological assays.
- Quality System Management: Learn about implementing and maintaining quality systems, including documentation control, change control, CAPA (Corrective and Preventive Actions), and deviation management. Practice applying these principles to hypothetical scenarios.
- Regulatory Compliance: Understand the role of PQA in ensuring compliance with relevant regulations (e.g., FDA 21 CFR Part 11, GMP guidelines). Explore case studies of non-compliance and their consequences.
- Audits and Inspections: Prepare for potential questions on internal and external audits, including their purpose, preparation, and execution. Consider how to respond effectively to auditor findings.
- Risk Management: Demonstrate understanding of risk assessment methodologies (e.g., FMEA) and their application in pharmaceutical quality. Prepare examples of risk mitigation strategies.
- Quality by Design (QbD): Familiarize yourself with the principles of QbD and how it impacts pharmaceutical development and manufacturing.
- Data Integrity: Understand the importance of data integrity in PQA and the measures taken to ensure data reliability and traceability.
- Supply Chain Management and Quality: Explore the role of PQA in ensuring the quality of materials and products throughout the supply chain.
Next Steps
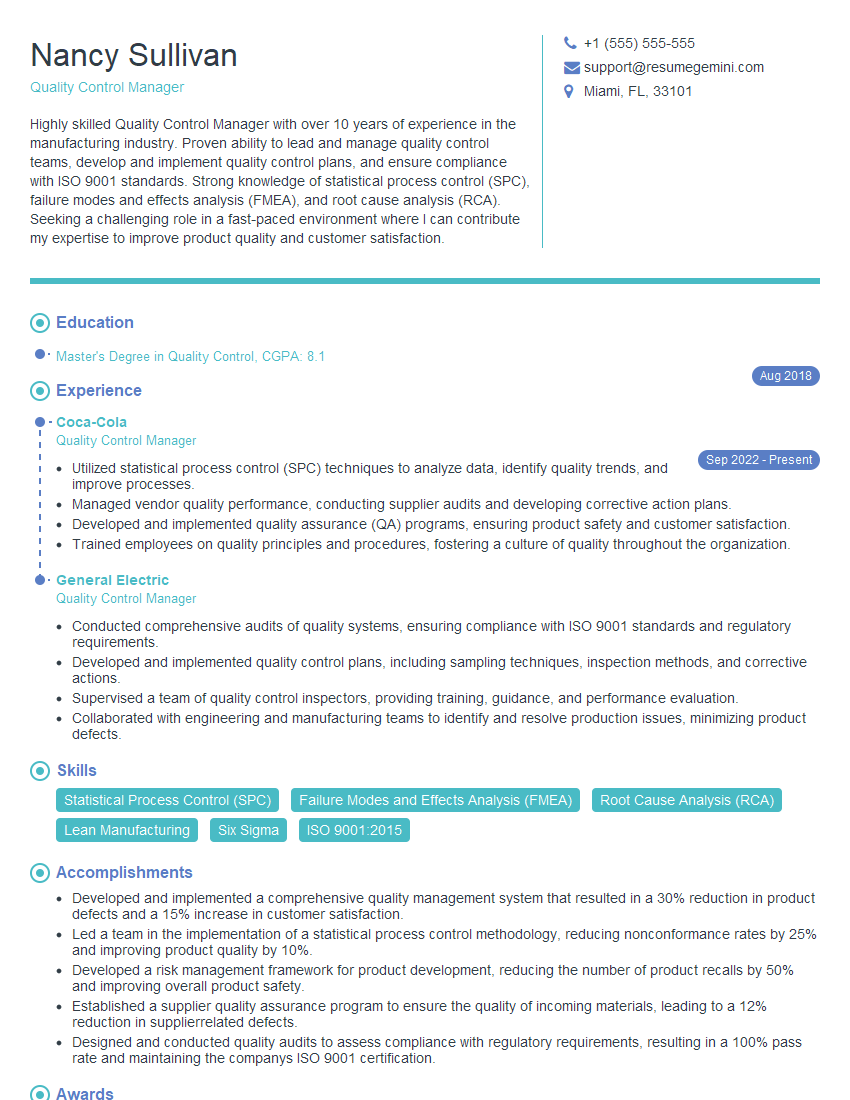
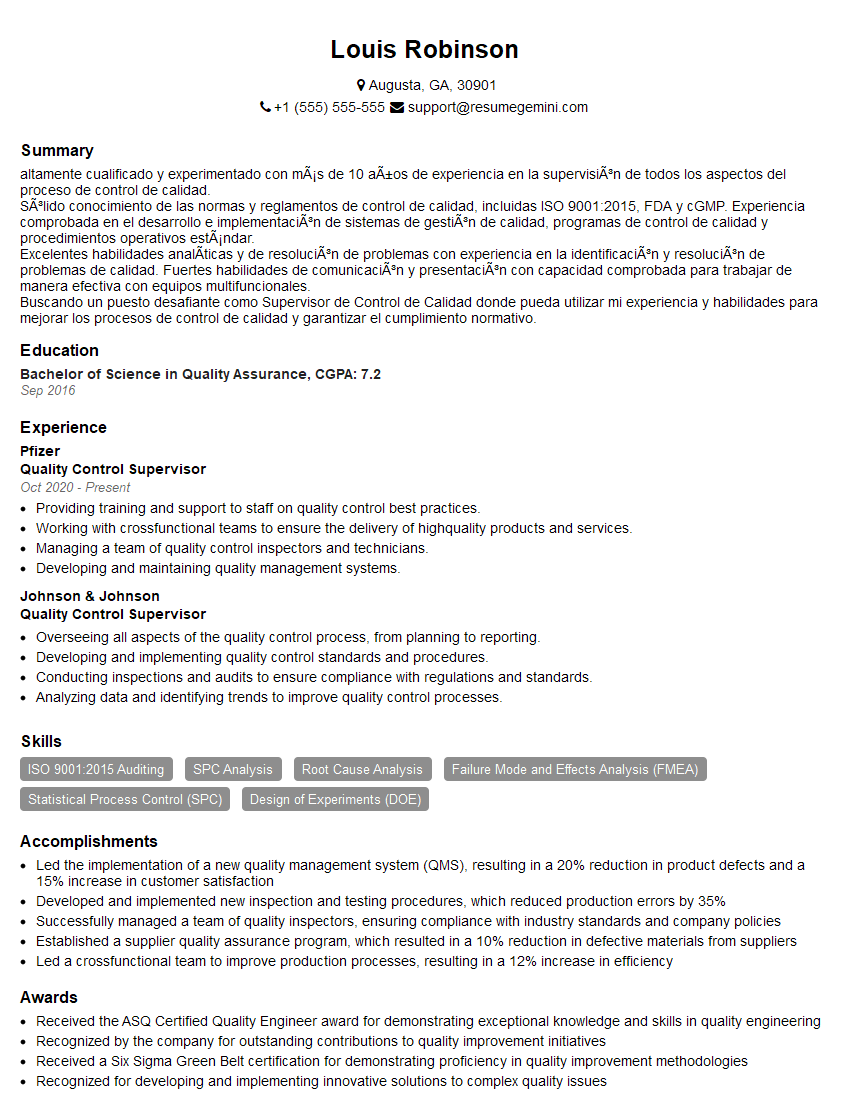
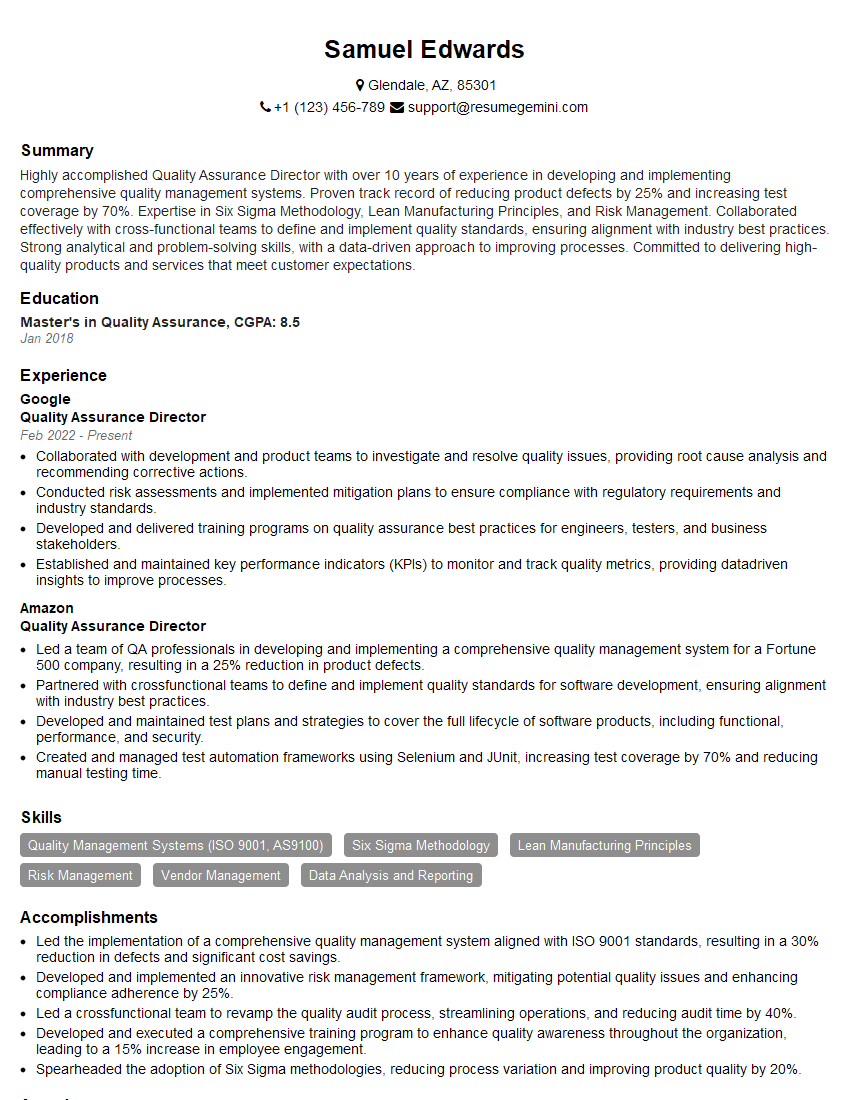
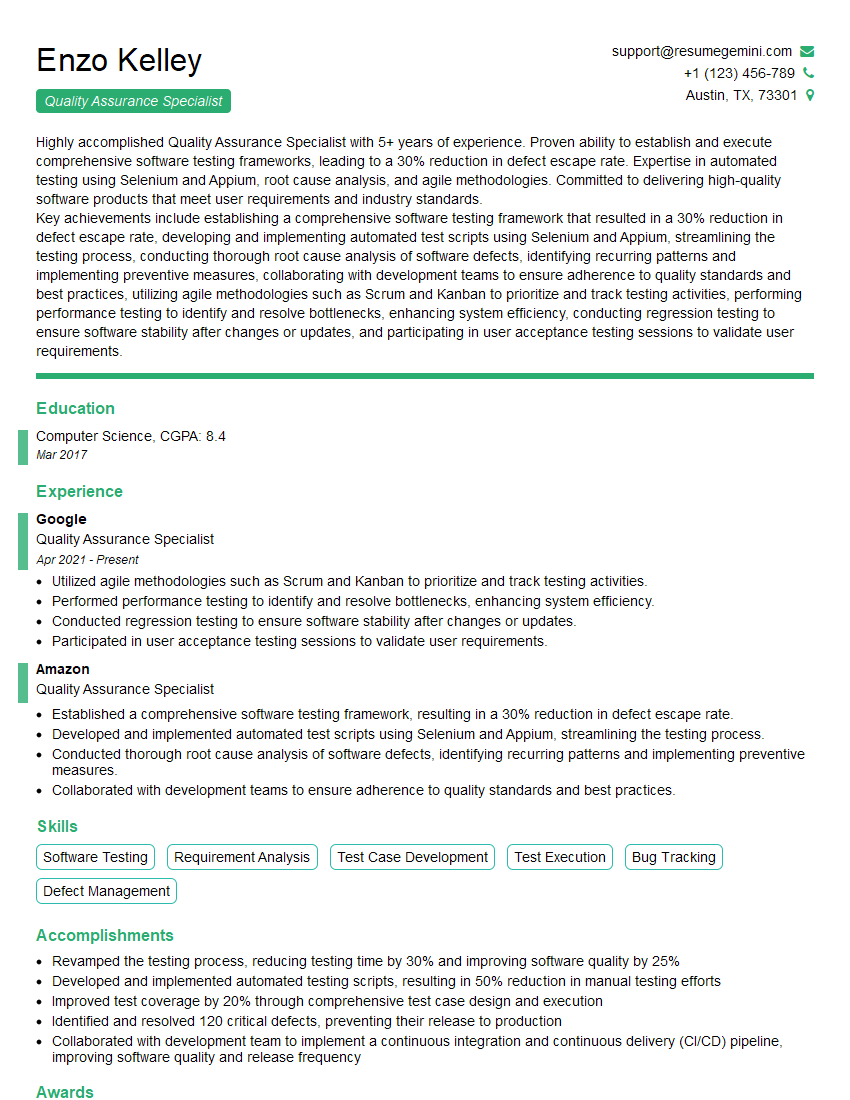
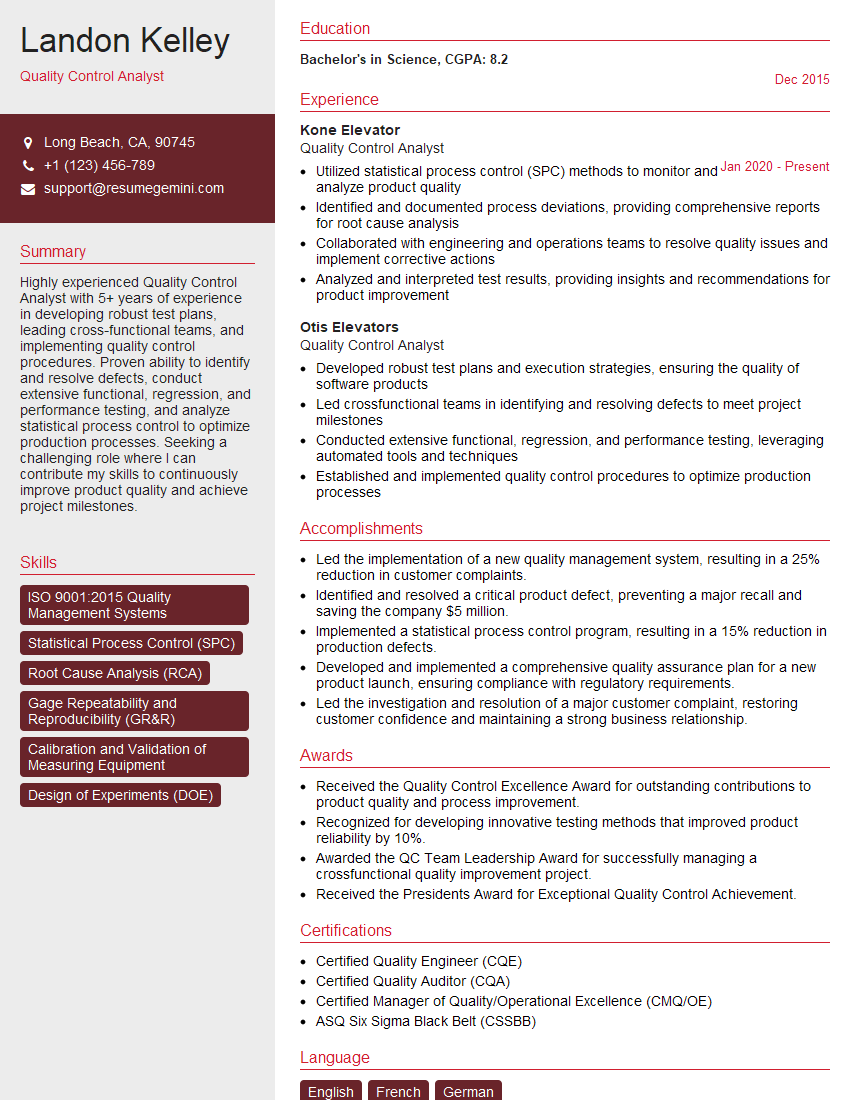
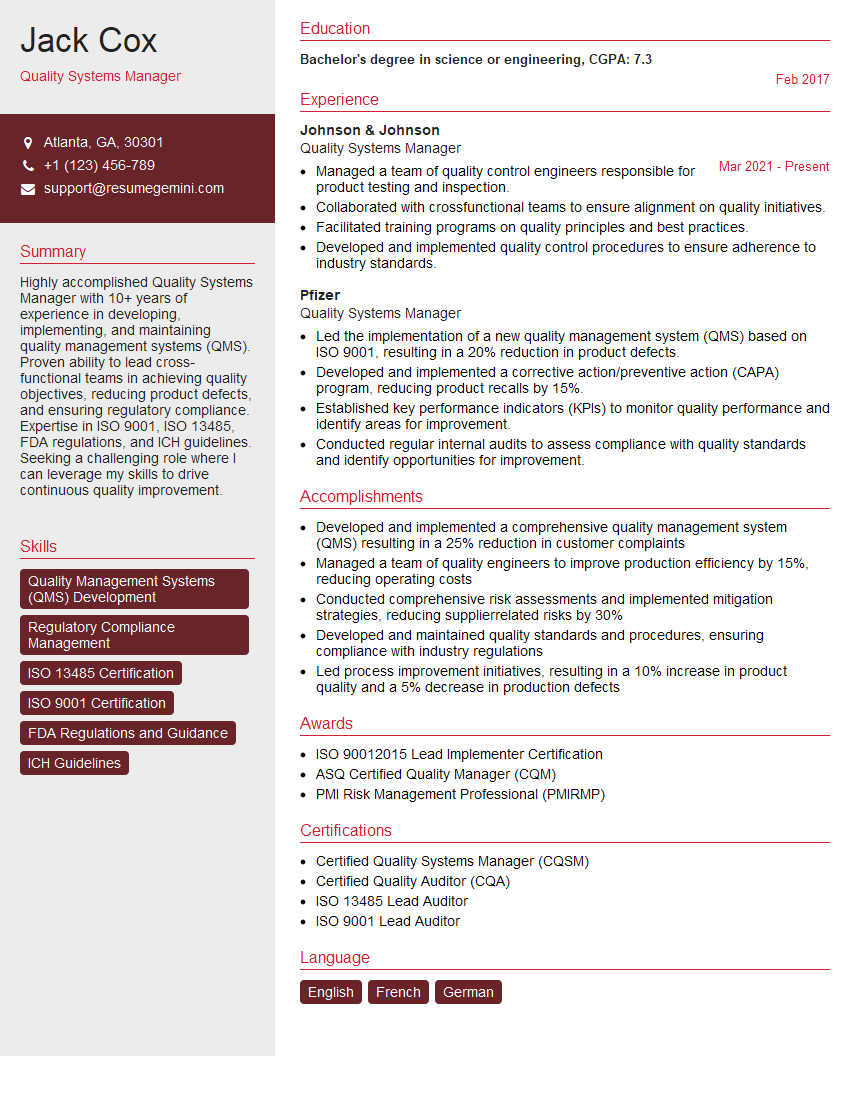
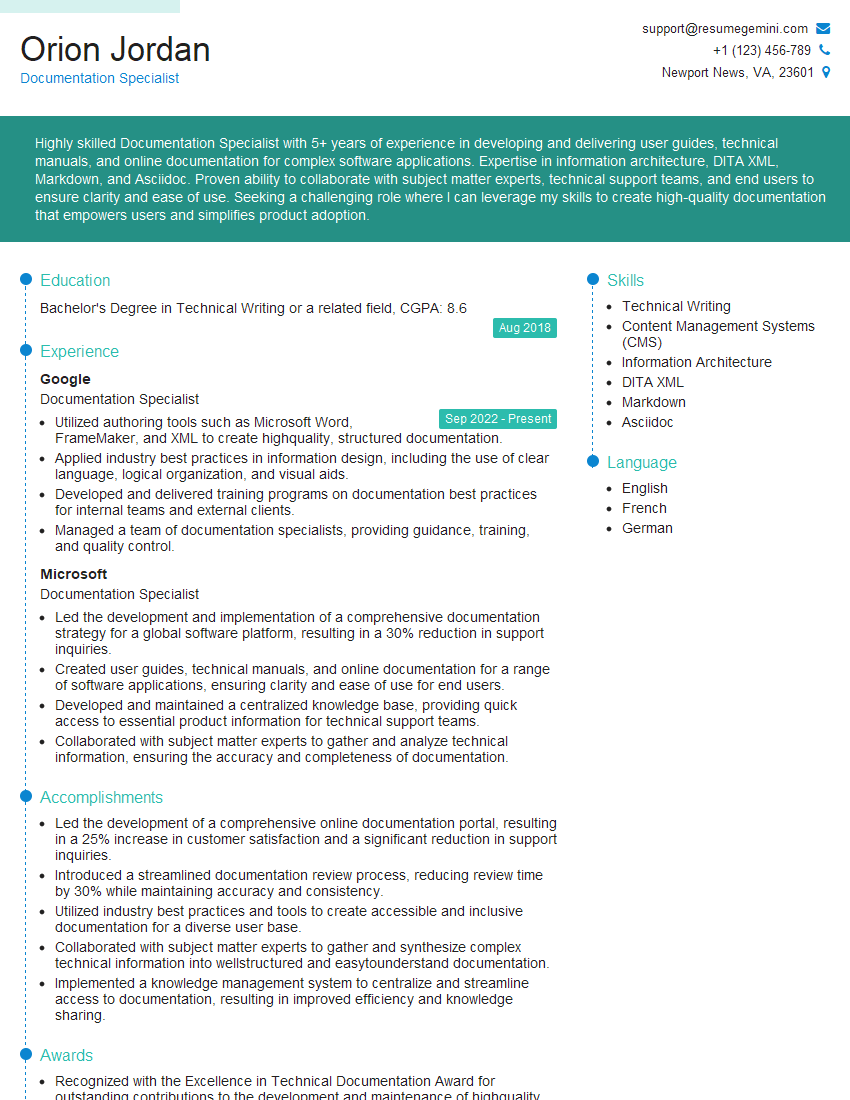
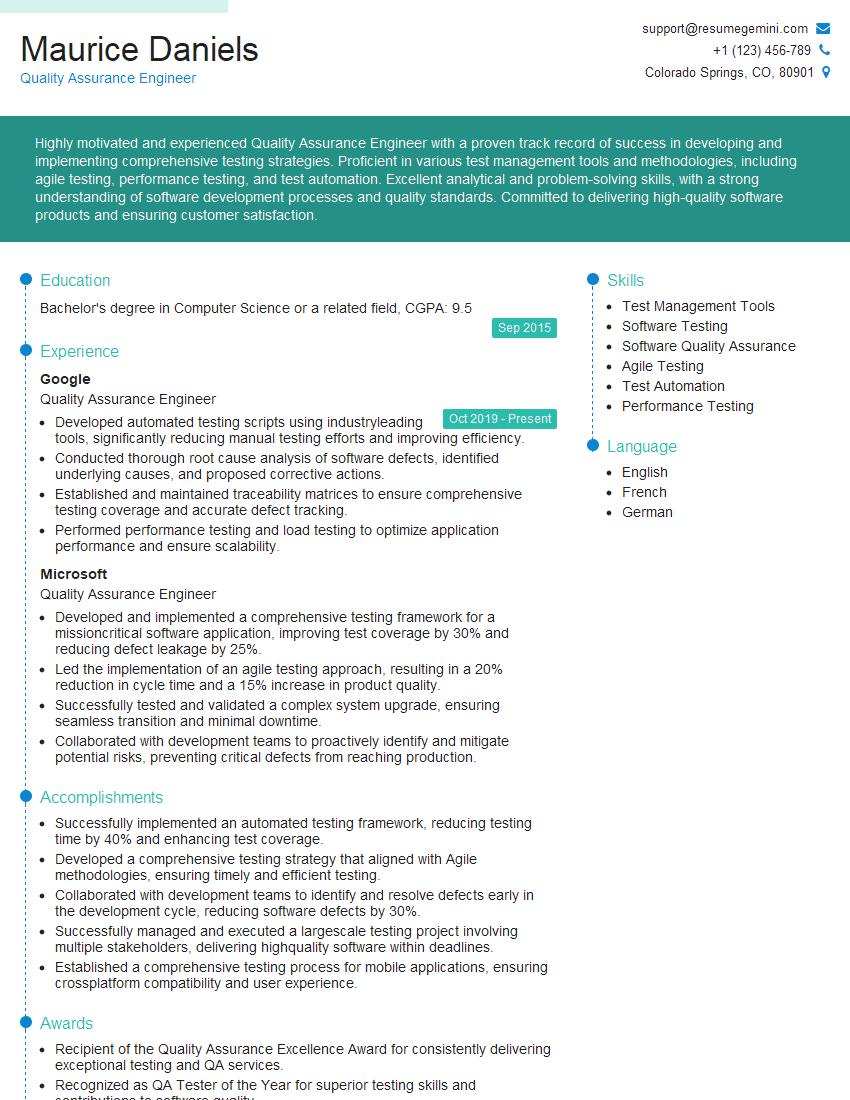
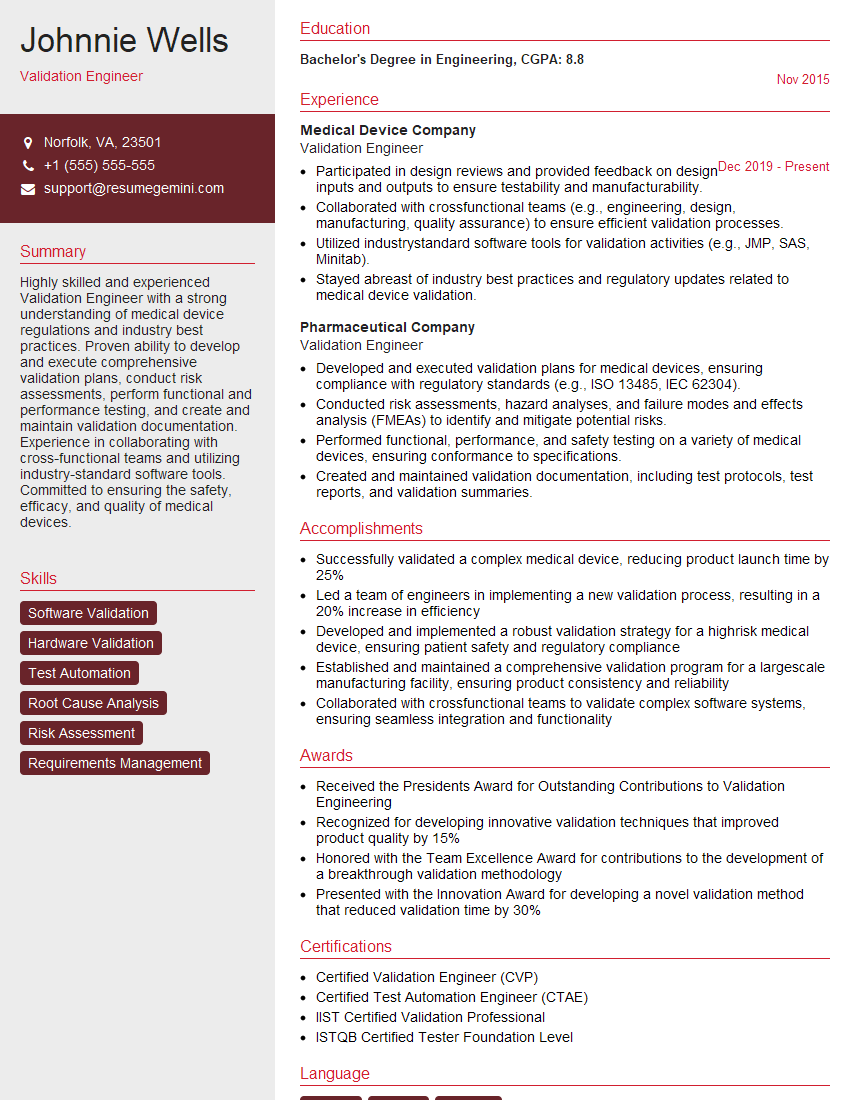
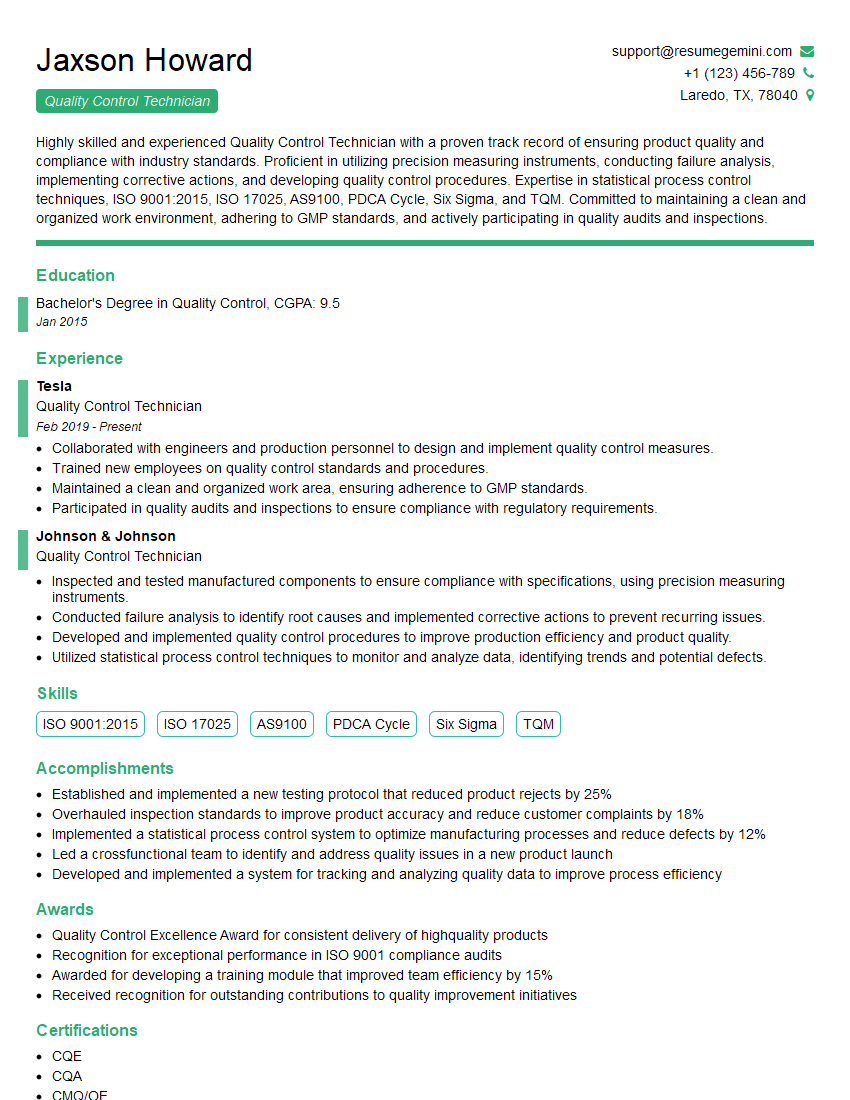
Mastering Pharmaceutical Quality Assurance (PQA) is crucial for a rewarding and impactful career in the pharmaceutical industry. It opens doors to diverse roles with increasing responsibility and higher earning potential. To maximize your job prospects, focus on creating a strong, ATS-friendly resume that effectively showcases your skills and experience. We highly recommend using ResumeGemini, a trusted resource for building professional resumes. ResumeGemini provides examples of resumes tailored to Pharmaceutical Quality Assurance (PQA) roles, helping you craft a compelling document that gets noticed by recruiters.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good