Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Pharmacological Interventions interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Pharmacological Interventions Interview
Q 1. Explain the difference between pharmacokinetics and pharmacodynamics.
Pharmacokinetics and pharmacodynamics are two crucial branches of pharmacology that describe how drugs behave in the body. Think of it like this: pharmacokinetics describes what the body does to the drug, while pharmacodynamics describes what the drug does to the body.
Pharmacokinetics focuses on the movement of the drug through the body. This involves absorption (how the drug gets into the bloodstream), distribution (how the drug spreads to different tissues and organs), metabolism (how the drug is broken down), and excretion (how the drug leaves the body). It’s all about the drug’s journey.
Pharmacodynamics, on the other hand, deals with the effects of the drug on the body. This includes the drug’s mechanism of action (how it interacts with its target), its efficacy (how well it works), and its potency (how much drug is needed to produce an effect). It’s about the drug’s impact.
For example, a drug might be highly potent (meaning a small dose has a big effect), but its pharmacokinetic profile might limit its usefulness because it’s quickly metabolized and excreted, resulting in a short duration of action.
Q 2. Describe the four main processes of pharmacokinetics (absorption, distribution, metabolism, excretion).
The four main processes of pharmacokinetics are:
- Absorption: This is the process by which a drug enters the bloodstream from its site of administration. Factors influencing absorption include the route of administration (e.g., oral, intravenous), the drug’s formulation (e.g., tablet, capsule), and the patient’s physiological state (e.g., gastric pH, gut motility). For example, a drug taken orally must pass through the stomach and intestines before being absorbed into the bloodstream, while a drug injected intravenously goes directly into the bloodstream.
- Distribution: Once in the bloodstream, the drug is distributed to various tissues and organs throughout the body. The rate of distribution depends on factors such as blood flow, the drug’s ability to cross cell membranes, and its binding to plasma proteins. Some drugs are highly distributed throughout the body, while others remain largely confined to the bloodstream.
- Metabolism: This is the process by which the drug is chemically altered, usually in the liver, to make it more water-soluble and easier to excrete. The liver contains enzymes (like cytochrome P450 enzymes) that catalyze these metabolic reactions. Metabolism can either activate a prodrug (an inactive form that becomes active after metabolism) or inactivate an active drug.
- Excretion: This is the process by which the drug and its metabolites are eliminated from the body, primarily through the kidneys in the urine, but also through the feces, sweat, and breath. The rate of excretion depends on factors such as kidney function and the drug’s properties.
Q 3. What are the different routes of drug administration and their advantages/disadvantages?
Different routes of drug administration each have their own advantages and disadvantages:
- Oral (PO): Convenient, but absorption can be variable and slower than other routes. Food can affect absorption. It’s subject to first-pass metabolism (the drug passes through the liver before reaching systemic circulation).
- Intravenous (IV): Rapid onset of action, predictable bioavailability (100%), but requires skilled administration and carries a risk of infection or embolism.
- Intramuscular (IM): Faster absorption than oral, but can be painful and may cause tissue damage.
- Subcutaneous (SC): Slower absorption than IM, suitable for sustained-release formulations, but limited volume can be injected.
- Transdermal: Provides sustained drug delivery over a period of time, but absorption can be slow and unpredictable.
- Inhalation: Rapid delivery to the lungs for respiratory conditions, but dosage can be difficult to control.
- Rectal: Useful when oral administration is not possible (e.g., vomiting), but can be inconvenient and irregular absorption.
The choice of route depends on the specific drug, its properties, the desired onset and duration of action, and the patient’s condition.
Q 4. Explain the concept of drug bioavailability.
Bioavailability refers to the fraction of an administered dose of a drug that reaches the systemic circulation in an unchanged form. In simpler terms, it tells us what proportion of the drug actually makes it into the bloodstream to have an effect. It’s expressed as a percentage.
For example, if a drug has a bioavailability of 50%, it means that only half of the administered dose reaches the systemic circulation. The rest is either lost during absorption, metabolized before reaching the bloodstream (first-pass effect), or otherwise eliminated from the body.
Several factors affect bioavailability, including the route of administration, the drug’s formulation, and the patient’s individual characteristics such as gut motility.
Q 5. What is the therapeutic index, and why is it important?
The therapeutic index (TI) is a measure of a drug’s safety. It’s the ratio of the toxic dose (TD) to the therapeutic dose (ED), where TD50 is the dose that is lethal to 50% of the population and ED50 is the dose that produces a therapeutic effect in 50% of the population. A higher TI indicates a safer drug.
TI = TD50 / ED50
A large therapeutic index means there’s a wide gap between the dose that produces a therapeutic effect and the dose that causes toxicity. For example, a drug with a TI of 100 is much safer than a drug with a TI of 2, because there’s a much larger margin of error before toxicity is reached.
The therapeutic index is crucial in determining the appropriate dose range and monitoring patients for adverse effects. Drugs with narrow therapeutic indices (like warfarin) require careful monitoring of blood levels to avoid toxicity.
Q 6. Describe the different types of drug interactions.
Drug interactions occur when the effect of one drug is altered by the presence of another drug. There are several types:
- Pharmacokinetic interactions: These interactions affect the absorption, distribution, metabolism, or excretion of a drug. For instance, some drugs induce or inhibit liver enzymes, thereby altering the metabolism of other drugs.
- Pharmacodynamic interactions: These interactions occur when two drugs affect the same physiological system, either synergistically (enhancing each other’s effects) or antagonistically (counteracting each other’s effects). For example, two drugs that both lower blood pressure might produce additive or even supra-additive effects, increasing the risk of hypotension.
- Additive effects: The combined effect of two drugs is equal to the sum of their individual effects.
- Synergistic effects: The combined effect of two drugs is greater than the sum of their individual effects.
- Antagonistic effects: The combined effect of two drugs is less than the sum of their individual effects (one drug blocks the action of the other).
Understanding drug interactions is vital to prevent adverse events and ensure optimal treatment outcomes. Clinicians carefully review patients’ medication histories to identify potential interactions.
Q 7. How do you determine the appropriate dose of a medication for a patient?
Determining the appropriate dose of medication is a complex process involving many factors, including:
- Patient’s age, weight, and renal and hepatic function: Dosage adjustments are often necessary for elderly patients, children, or patients with compromised organ function. Children often require different pediatric formulations due to their lower body weight.
- Patient’s disease state and severity: The dosage might be adjusted based on the severity of the illness being treated.
- Other medications the patient is taking: Potential drug interactions must be considered, possibly necessitating dose adjustments or alternative medications.
- Patient’s genetic makeup: Pharmacogenomics helps tailor dosage based on individual genetic variations affecting drug metabolism and response.
- Drug’s pharmacokinetic and pharmacodynamic properties: A drug’s half-life (time it takes for half the drug to be eliminated) and therapeutic window significantly impact dosing frequency and amount.
Dosage information is typically found in drug prescribing information. Clinicians utilize clinical guidelines, experience, and sometimes therapeutic drug monitoring to fine-tune a patient’s dosage, often beginning with a lower dose and gradually increasing it as needed while closely monitoring for therapeutic effects and adverse reactions.
Q 8. Explain the concept of drug metabolism and the role of cytochrome P450 enzymes.
Drug metabolism is the process by which the body modifies drugs, primarily to facilitate their elimination. Think of it like your body’s recycling plant for medications. The liver is the major site of drug metabolism, and cytochrome P450 (CYP450) enzymes are the key players in this process. These enzymes are a large family of proteins that catalyze the oxidation of many different drugs and other xenobiotics (foreign substances). They act by adding oxygen atoms to the drug molecule, making it more water-soluble and easier to excrete through the kidneys.
For example, many medications are metabolized by CYP3A4, a major CYP450 enzyme. If a patient is taking multiple drugs that are metabolized by the same CYP450 enzyme, there’s a risk of drug interactions. One drug might inhibit or induce the enzyme, altering the metabolism and hence blood levels of the other drug. This could lead to either toxicity (if levels rise too high) or treatment failure (if levels drop too low).
Understanding CYP450 enzymes is crucial in pharmacokinetics (the study of drug movement and metabolism in the body). It allows us to predict drug interactions and tailor dosages to maximize therapeutic efficacy and minimize adverse effects.
Q 9. What are the key factors to consider when designing a clinical trial for a new drug?
Designing a clinical trial involves meticulous planning to ensure the safety and efficacy of a new drug are thoroughly assessed. Key factors include:
- Defining the research question: Clearly stating the objective, like establishing efficacy against a placebo or a standard treatment.
- Selecting the study population: Identifying the target patient group, their inclusion/exclusion criteria, and sample size calculation. This requires considering factors like age, gender, ethnicity, disease severity and comorbid conditions.
- Choosing the study design: Selecting the appropriate design (e.g., randomized controlled trial, open-label study) to address the research question. Randomization is crucial for minimizing bias and ensuring comparable groups.
- Selecting the endpoints: Defining how efficacy and safety will be measured. This might involve clinical outcomes (e.g., reduction in tumor size, improvement in blood pressure), laboratory measurements, or patient-reported outcomes (e.g., quality of life questionnaires).
- Ensuring ethical considerations: Obtaining informed consent, managing data privacy, and having an independent ethics committee review the protocol are essential.
- Statistical planning: Determining the statistical methods for data analysis prior to the start of the trial to avoid bias.
For example, a Phase III trial for a new cancer drug would involve a large number of patients with a specific type of cancer, randomized to receive either the new drug or the standard treatment. The primary endpoint could be overall survival, while secondary endpoints could include tumor response rate and quality of life.
Q 10. Describe the different phases of clinical trials.
Clinical trials are conducted in phases to systematically evaluate a new drug’s safety and efficacy. Each phase has specific objectives and characteristics.
- Phase I: Focuses on safety and tolerability in a small group of healthy volunteers. The main goal is to determine the safe dosage range and identify potential side effects.
- Phase II: Assesses the drug’s effectiveness and further evaluates its safety in a larger group of patients with the target disease. It aims to optimize dosage and identify optimal treatment regimens.
- Phase III: A large-scale trial comparing the new drug to a placebo or standard treatment. This phase confirms the drug’s efficacy, monitors long-term side effects, and gathers data to support regulatory approval.
- Phase IV: Post-market surveillance, where the drug’s effectiveness and safety are monitored after it’s been approved and is being used in the broader population. This phase aims to detect rare adverse events or to identify optimal ways to use the drug in different patient populations.
Q 11. What are some common adverse drug reactions, and how are they managed?
Adverse drug reactions (ADRs) are unintended and undesirable effects caused by a medication. They range in severity from mild discomfort to life-threatening complications.
- Common ADRs: Nausea, vomiting, diarrhea, headache, dizziness, rash, allergic reactions (ranging from mild skin reactions to anaphylaxis).
- Management: Management depends on the severity and type of ADR. Mild ADRs might only require supportive care (e.g., symptomatic treatment for nausea). More serious reactions may require discontinuation of the drug, administration of counteracting medications (e.g., antihistamines for allergic reactions), or hospitalization. Careful monitoring of vital signs and laboratory values is crucial.
For example, a patient experiencing severe nausea and vomiting after starting a new antibiotic might need to switch to a different antibiotic. A patient experiencing an allergic reaction (such as hives or difficulty breathing) would require immediate medical attention, potentially including the administration of epinephrine.
Q 12. Explain the concept of pharmacogenomics and its implications for drug therapy.
Pharmacogenomics studies the influence of an individual’s genetic makeup on their response to drugs. It’s essentially personalized medicine applied to drug therapy. Understanding a person’s genetic profile can help predict how they will metabolize a drug and whether they are likely to experience adverse effects.
For instance, some people have genetic variations in enzymes involved in drug metabolism (like CYP450 enzymes). This can affect how quickly a drug is broken down, leading to either increased risk of toxicity or reduced efficacy. Pharmacogenomics allows us to tailor drug selection and dosage to individual genetic profiles, increasing treatment effectiveness and reducing adverse effects. Some drugs, like warfarin (a blood thinner), already have pharmacogenomic testing guidelines that help guide dosage adjustments.
The implications are significant for improving patient care. It reduces adverse drug reactions, improves efficacy of treatment, reduces healthcare costs by decreasing hospitalizations due to adverse drug events, and offers a more targeted approach to drug development.
Q 13. What are the ethical considerations in pharmacological research?
Ethical considerations are paramount in pharmacological research. These include:
- Informed consent: Participants must be fully informed about the study’s purpose, procedures, potential benefits and risks, and their right to withdraw at any time.
- Beneficence and non-maleficence: The research must maximize benefits and minimize harm to participants. This involves careful risk assessment and mitigation strategies.
- Justice and equity: Research should be conducted fairly and equitably, ensuring that all populations have access to the benefits of new treatments.
- Confidentiality and data privacy: Protecting the identity and sensitive information of participants is essential.
- Animal welfare: If animal models are used, appropriate care and ethical treatment of animals is mandatory.
Ethical review boards (IRBs or ERBs) play a critical role in overseeing research studies to ensure compliance with ethical standards.
Q 14. How do you interpret a pharmacokinetic/pharmacodynamic (PK/PD) profile?
A pharmacokinetic/pharmacodynamic (PK/PD) profile describes the relationship between drug concentration in the body (PK) and its effects (PD). It provides insights into how a drug is absorbed, distributed, metabolized, and eliminated (PK), and how these processes relate to its therapeutic and adverse effects (PD).
Interpreting a PK/PD profile involves analyzing parameters such as:
- PK parameters: AUC (area under the curve – representing overall drug exposure), Cmax (maximum concentration), Tmax (time to reach maximum concentration), clearance, half-life.
- PD parameters: Effect size (e.g., reduction in blood pressure, pain relief), onset and duration of effect, relationship between drug concentration and effect (e.g., Emax – maximum effect achievable).
By analyzing the PK/PD profile, we can determine the optimal dosing regimen to achieve the desired therapeutic effect while minimizing adverse effects. For instance, a drug with a short half-life might require more frequent dosing, whereas a drug with a long half-life might require less frequent dosing. A steep concentration-effect curve might indicate a narrow therapeutic index, requiring careful monitoring of drug levels.
Q 15. Explain the difference between agonist and antagonist drugs.
Agonists and antagonists are two types of drugs that interact with receptors in the body, but they have opposite effects. Think of a receptor as a lock and a drug as a key. An agonist is like a key that fits perfectly and turns the lock, initiating a response. It activates the receptor and produces a biological effect. For example, morphine is an agonist at opioid receptors, causing analgesia (pain relief). An antagonist, on the other hand, is like a key that fits the lock but doesn’t turn it. It blocks the receptor, preventing other molecules (like an agonist or endogenous ligand) from binding and producing an effect. For instance, naloxone is an opioid receptor antagonist; it blocks the effects of opioids like morphine.
The key difference lies in their action: agonists activate receptors, while antagonists block them.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the different types of drug receptors?
Drug receptors are macromolecules, usually proteins, located on or within cells. They can be categorized in several ways. One common classification is based on their location and the signaling pathways they trigger:
- Ligand-gated ion channels: These channels open or close in response to a specific ligand binding, directly affecting ion flow across the membrane. An example is the nicotinic acetylcholine receptor.
- G protein-coupled receptors (GPCRs): These receptors are the largest family, mediating diverse cellular responses through G proteins. Many hormones and neurotransmitters use GPCRs, such as beta-adrenergic receptors for adrenaline.
- Enzyme-linked receptors: These receptors possess intrinsic enzymatic activity or are directly associated with enzymes. A classic example is the insulin receptor, which has tyrosine kinase activity.
- Intracellular receptors: These receptors are located within the cell, typically in the cytoplasm or nucleus. Steroid hormones, like cortisol, bind to these receptors, altering gene expression.
Another classification focuses on the type of ligand they bind: some are specific for certain neurotransmitters, hormones, or drugs, while others have broader specificity.
Q 17. Describe the mechanism of action of a specific drug class (e.g., beta-blockers, ACE inhibitors).
Let’s consider beta-blockers. These drugs are primarily used to treat hypertension (high blood pressure), angina (chest pain), and some cardiac arrhythmias. They achieve their effects by blocking beta-adrenergic receptors, specifically β1 and β2 subtypes. These receptors are found in the heart and other organs, and their activation by adrenaline (epinephrine) or noradrenaline (norepinephrine) causes increased heart rate, contractility, and blood pressure.
By competitively binding to these receptors and blocking the effects of endogenous catecholamines, beta-blockers reduce heart rate and contractility, leading to decreased cardiac output and blood pressure. For example, metoprolol is a selective β1-blocker, meaning it predominantly targets β1 receptors in the heart, minimizing effects on β2 receptors in the lungs (which could cause bronchospasm).
The mechanism involves preventing the binding of catecholamines, thus inhibiting the activation of adenylate cyclase and subsequent downstream signaling pathways that regulate heart function.
Q 18. What is the role of pharmacoepidemiology in drug safety?
Pharmacoepidemiology plays a crucial role in drug safety by studying the effects of drugs on large populations in real-world settings. This allows identification of rare or unexpected adverse effects that might not be apparent during clinical trials, which usually involve smaller, more controlled groups of patients.
Through analyzing data from various sources like electronic health records, insurance claims, and clinical registries, pharmacoepidemiologists can assess post-market drug safety, identify risk factors for adverse events, and evaluate the effectiveness of drugs in diverse populations. This information is critical for updating drug labels, formulating risk management plans, and making informed decisions about drug use and regulation.
For instance, pharmacoepidemiology studies may reveal a previously unrecognized association between a particular drug and a specific adverse event, leading to a warning being added to the drug’s prescribing information or even withdrawal from the market.
Q 19. Explain the concept of drug tolerance and dependence.
Drug tolerance refers to the decreased responsiveness to a drug after repeated administration. The body adapts to the drug’s presence, requiring higher doses to achieve the same effect. This is often due to changes in receptor sensitivity, drug metabolism, or homeostatic adjustments.
Drug dependence, on the other hand, involves a state where the body adapts to the presence of a drug to the extent that discontinuation leads to withdrawal symptoms. This reflects a physical or psychological dependence on the drug. Physical dependence involves physiological changes requiring the drug to maintain homeostasis, while psychological dependence is characterized by craving and compulsive drug-seeking behavior.
Tolerance and dependence are distinct but related concepts, often co-occurring with some drugs, but not always. For example, opioids can cause both tolerance to their analgesic effects and physical dependence, leading to withdrawal symptoms upon cessation.
Q 20. How do you assess the efficacy and safety of a new drug?
Assessing the efficacy and safety of a new drug involves a rigorous process, starting with preclinical studies (in vitro and in vivo) and progressing to clinical trials involving human subjects.
Efficacy is evaluated through clinical trials, measuring the drug’s ability to produce the desired therapeutic effect compared to a placebo or standard treatment. Outcome measures vary depending on the indication, such as reduction in blood pressure for hypertension or improved symptoms in depression.
Safety is assessed throughout the development process, monitoring for adverse events (side effects) of varying severity. The risk-benefit ratio is a critical aspect of drug evaluation, weighing the drug’s potential benefits against its potential harms. Pharmacovigilance (post-market surveillance) continues after the drug is approved to monitor long-term safety and identify rare adverse effects.
Statistical analysis plays a crucial role in interpreting the results of these studies, determining if the observed effects are clinically meaningful and statistically significant, thereby ensuring that the drug is both efficacious and safe.
Q 21. Describe the process of drug regulatory approval.
The drug regulatory approval process is complex and varies somewhat depending on the country but generally involves these steps:
- Preclinical testing: Laboratory and animal studies to evaluate the drug’s safety and efficacy.
- Investigational New Drug (IND) application: Submission of data from preclinical testing to regulatory authorities (e.g., FDA in the US, EMA in Europe) to obtain permission to conduct clinical trials in humans.
- Clinical trials: A series of phases (Phase I, II, III) involving increasing numbers of participants to assess the drug’s safety, efficacy, dosage, and optimal administration. These trials are designed to gather comprehensive data and establish the drug’s effectiveness and safety profile.
- New Drug Application (NDA) or Marketing Authorization Application (MAA): Submission of comprehensive data from preclinical and clinical trials to regulatory authorities for review and approval.
- Regulatory review: A rigorous evaluation of the submitted data by regulatory agencies, potentially involving multiple rounds of review and revisions.
- Post-market surveillance: Ongoing monitoring of the drug’s safety and effectiveness after it is approved for market sale, detecting and addressing any potential issues.
The entire process can take many years and requires significant resources, but it is essential to ensure that new drugs are safe and effective before they are made available to patients.
Q 22. What are some common challenges in drug development?
Drug development is a complex and lengthy process, fraught with challenges. One major hurdle is the high attrition rate. A significant percentage of drug candidates fail during preclinical or clinical trials due to issues like lack of efficacy, toxicity, or poor pharmacokinetic properties. Think of it like a funnel – you start with many potential candidates and only a few make it to the market.
- Target identification and validation: Finding the right biological target for a disease is crucial, but sometimes the target isn’t as effective as initially thought.
- Drug formulation and delivery: Ensuring the drug reaches the intended site of action in the right concentration and form is challenging. For example, oral bioavailability can be low for some drugs.
- Regulatory hurdles: The regulatory pathway is rigorous and time-consuming, requiring extensive data and meeting strict standards. This process can significantly extend the development timeline.
- Cost and time: Drug development is incredibly expensive and can take many years (often 10-15 years or more), creating financial pressures for pharmaceutical companies.
- Clinical trial recruitment and retention: Finding and keeping enough participants for clinical trials is a significant logistical and ethical challenge.
For example, a promising cancer drug might show great efficacy in preclinical models, but fail in human trials due to unforeseen toxicity or poor absorption.
Q 23. How do you handle unexpected adverse events during clinical trials?
Unexpected adverse events (AEs) during clinical trials are handled with utmost seriousness and priority. Our first step is to immediately report the event to the appropriate regulatory authorities (e.g., the FDA) and the independent ethics committee (IRB) overseeing the trial. We then implement a series of steps:
- Assess the severity and causality of the AE: A detailed evaluation is done to determine if the event is related to the drug, and how serious it is. This often involves review by medical experts.
- Implement appropriate medical interventions: This may involve adjusting the drug dosage, administering supportive care, or discontinuing the drug completely, depending on the severity and the individual’s condition.
- Modify the study protocol if necessary: Based on the AE, the protocol might need revision, including inclusion/exclusion criteria or safety monitoring plans. This can sometimes lead to a temporary hold on recruitment.
- Conduct a thorough investigation: To understand the underlying cause, we perform a comprehensive review of the patient’s data, including their medical history and other medications.
- Communicate transparently: All relevant stakeholders, including the participants, investigators, regulatory bodies, and ethical review boards are kept informed throughout the process.
For instance, if a new cardiovascular drug unexpectedly causes increased heart rate in a significant number of participants, the trial would be paused, the data analyzed thoroughly, and potential risk mitigation strategies (like dosage adjustment) would be explored.
Q 24. What are the different types of drug delivery systems?
Drug delivery systems are designed to control how and where a drug is released in the body. The choice of system depends on various factors, including the drug’s properties, the target site, and patient-specific needs. Here are some examples:
- Oral: This is the most common route, involving tablets, capsules, liquids, etc. It’s convenient but has limitations like variable absorption.
- Parenteral: Injections (intravenous, intramuscular, subcutaneous) bypass the digestive system for rapid action but require skilled administration.
- Transdermal: Patches deliver drugs slowly through the skin, offering sustained release and avoiding the first-pass metabolism in the liver.
- Inhalation: Used for respiratory drugs, inhalers deliver medication directly to the lungs.
- Topical: Creams, ointments, and lotions are applied to the skin for local effects.
- Targeted drug delivery: This advanced approach uses nanoparticles or other carriers to direct drugs specifically to diseased cells or tissues, minimizing side effects.
Think about insulin delivery: while initially administered via injections, advancements have led to insulin pumps and even inhaled insulin, each improving patient convenience and medication management.
Q 25. Explain the concept of personalized medicine in pharmacology.
Personalized medicine, also known as precision medicine, tailors medical treatment to individual patients based on their genetic makeup, lifestyle, and environment. In pharmacology, this means developing drugs and treatment strategies that are most effective for specific patient subpopulations. This approach relies heavily on understanding the genetic variations that influence drug response.
For example, some individuals have genetic variations that affect how they metabolize certain drugs. Knowing this allows doctors to prescribe dosages that are both effective and safe. Pharmacogenomics is a crucial element, focusing on how genes influence drug response. This can help avoid adverse reactions and ensure optimal efficacy.
Another facet of personalized medicine is considering a patient’s lifestyle factors, such as diet and exercise, which can significantly impact drug response and overall health outcomes. A holistic approach considering all relevant factors results in better treatment outcomes.
Q 26. What is your understanding of the FDA guidelines for drug development?
The FDA (Food and Drug Administration) guidelines for drug development are extensive and cover all aspects of the process, from preclinical testing to post-market surveillance. These regulations aim to ensure that new drugs are both safe and effective. The process is rigorous and involves several phases:
- Preclinical testing: This involves laboratory and animal studies to assess drug safety, efficacy, and pharmacokinetic properties.
- Clinical trials (Phase 1-3): These involve testing the drug in humans, with escalating doses and increasing numbers of participants to evaluate safety and efficacy.
- New Drug Application (NDA): A comprehensive application submitted to the FDA that contains all the data gathered during preclinical and clinical trials.
- Review and approval: The FDA reviews the NDA, and if approved, grants marketing authorization.
- Post-market surveillance: Continuous monitoring of the drug’s safety and effectiveness after it’s on the market.
Compliance with these guidelines is mandatory, and failure to meet the required standards can result in delays or rejection of the drug. These guidelines are continuously updated to reflect advances in scientific understanding and ensure patient safety.
Q 27. How do you stay updated on the latest advancements in pharmacology?
Staying current in the rapidly evolving field of pharmacology requires a multi-faceted approach:
- Peer-reviewed journals and publications: Reading leading journals like the Journal of Pharmacology and Experimental Therapeutics, Nature Reviews Drug Discovery, and others provides access to the latest research findings.
- Conferences and meetings: Attending scientific conferences and meetings allows for networking with colleagues and learning about groundbreaking discoveries firsthand.
- Professional organizations: Membership in organizations such as the American Society for Pharmacology and Experimental Therapeutics (ASPET) provides access to resources, publications, and networking opportunities.
- Online resources: Utilizing reputable online databases like PubMed and Google Scholar to search for relevant publications and information.
- Continuing medical education (CME): Participating in CME courses and webinars keeps my knowledge and skills updated.
By actively pursuing these methods, I ensure I remain informed about advancements in drug discovery, development, and therapeutic strategies.
Q 28. Describe a situation where you had to troubleshoot a problem in a pharmacological experiment.
During an experiment studying the effects of a novel compound on cellular signaling, we encountered unexpected results. The compound showed significantly lower potency than predicted from preclinical assays. After carefully reviewing the experiment, we identified several possible sources of error:
- Reagent quality: We discovered that a batch of our key reagent had degraded, potentially affecting the results. We repeated the experiment with fresh reagents.
- Assay conditions: We realized that the cell culture conditions (incubation temperature, media composition) were subtly different from the conditions used in the preclinical tests. We optimized these parameters.
- Data analysis: We re-analyzed the data using different statistical methods to ensure the validity of our interpretations.
By systematically investigating each aspect of the experiment, we identified the degraded reagent as the primary cause of the discrepancy. Repeating the experiment with fresh reagents produced results consistent with the preclinical findings, resolving the initial problem. This experience highlighted the importance of meticulous attention to detail and rigorous quality control in pharmacological research.
Key Topics to Learn for Pharmacological Interventions Interview
- Pharmacokinetics & Pharmacodynamics: Understanding drug absorption, distribution, metabolism, excretion (ADME) and their relationship to drug effects. Consider practical applications like calculating drug dosages and predicting potential drug interactions.
- Drug Targets & Mechanisms of Action: Explore the various ways drugs interact with biological targets (receptors, enzymes, ion channels etc.) and the resulting physiological effects. Be prepared to discuss specific examples and their clinical relevance.
- Therapeutic Drug Monitoring (TDM): Learn about the principles and applications of TDM, including the interpretation of drug concentration data and its impact on treatment optimization. Consider case studies to illustrate your understanding.
- Adverse Drug Reactions (ADRs) & Drug Interactions: Develop a strong understanding of common ADRs, their mechanisms, and management strategies. Be able to discuss potential drug interactions and how to mitigate risks.
- Drug Development & Approval Process: Familiarize yourself with the stages of drug development, from preclinical studies to clinical trials and regulatory approval. Understanding the regulatory landscape is crucial.
- Specific Therapeutic Areas: Depending on the specific role, focus on therapeutic areas relevant to the position (e.g., oncology, cardiovascular, infectious disease). Be ready to discuss specific drug classes and their applications within these areas.
- Problem-Solving & Case Studies: Practice analyzing clinical scenarios involving pharmacological interventions. Be prepared to discuss your approach to problem-solving and decision-making in complex situations.
Next Steps
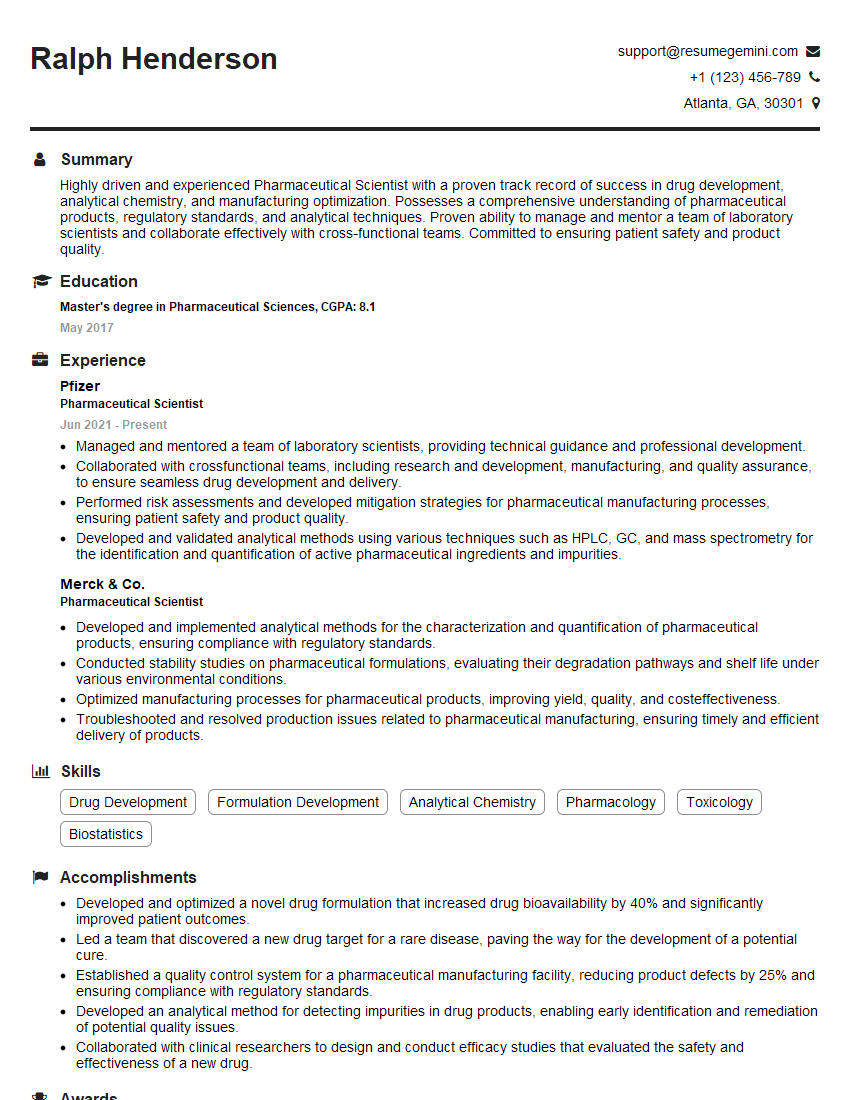
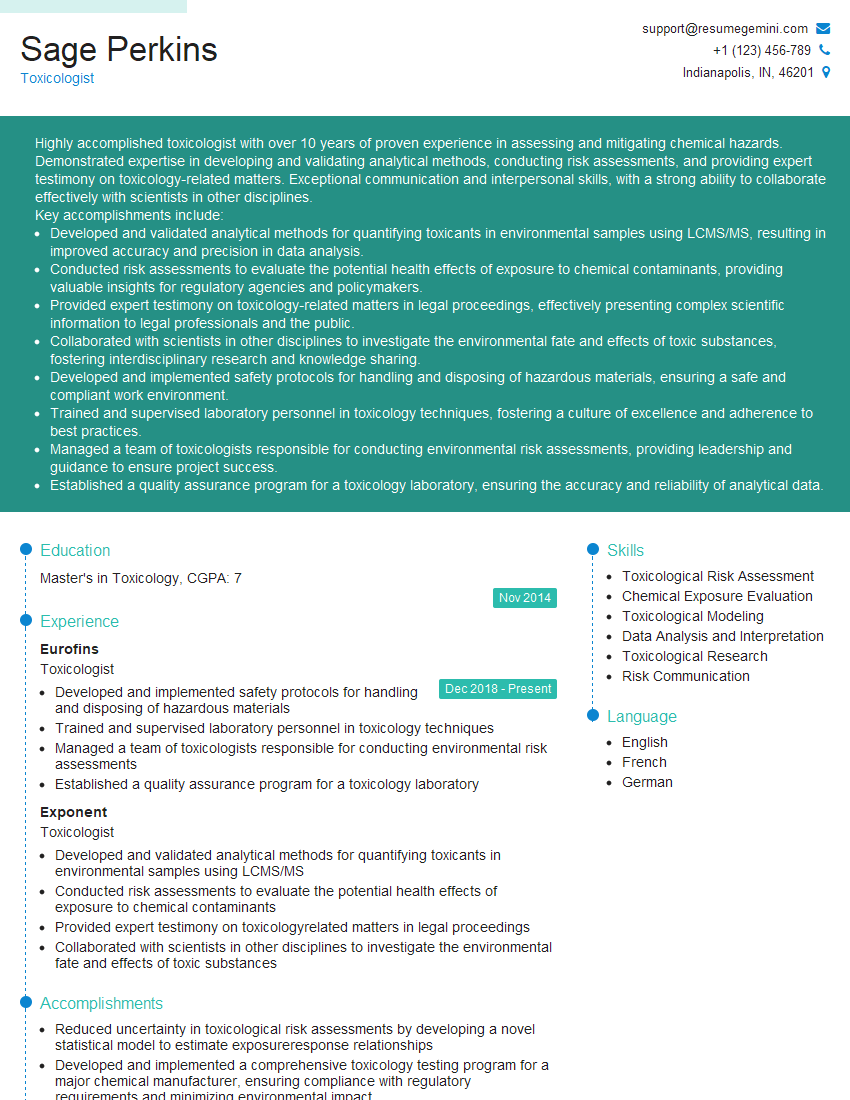
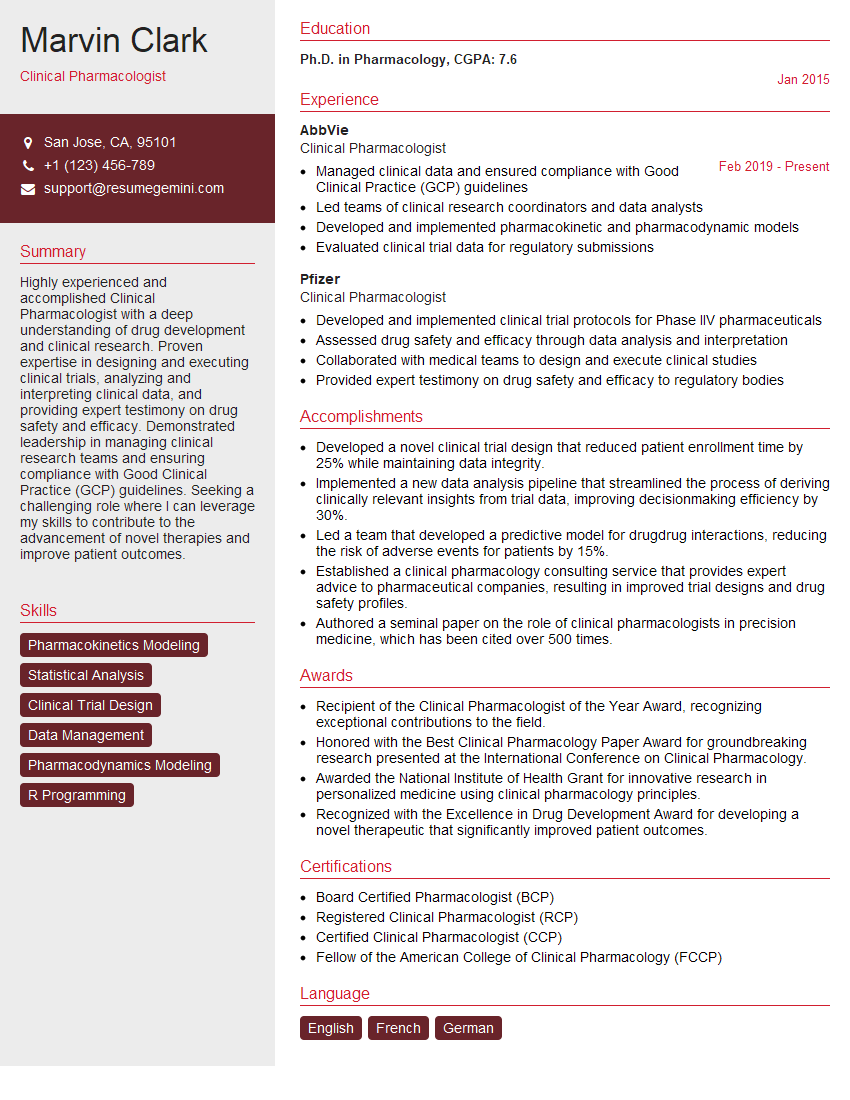
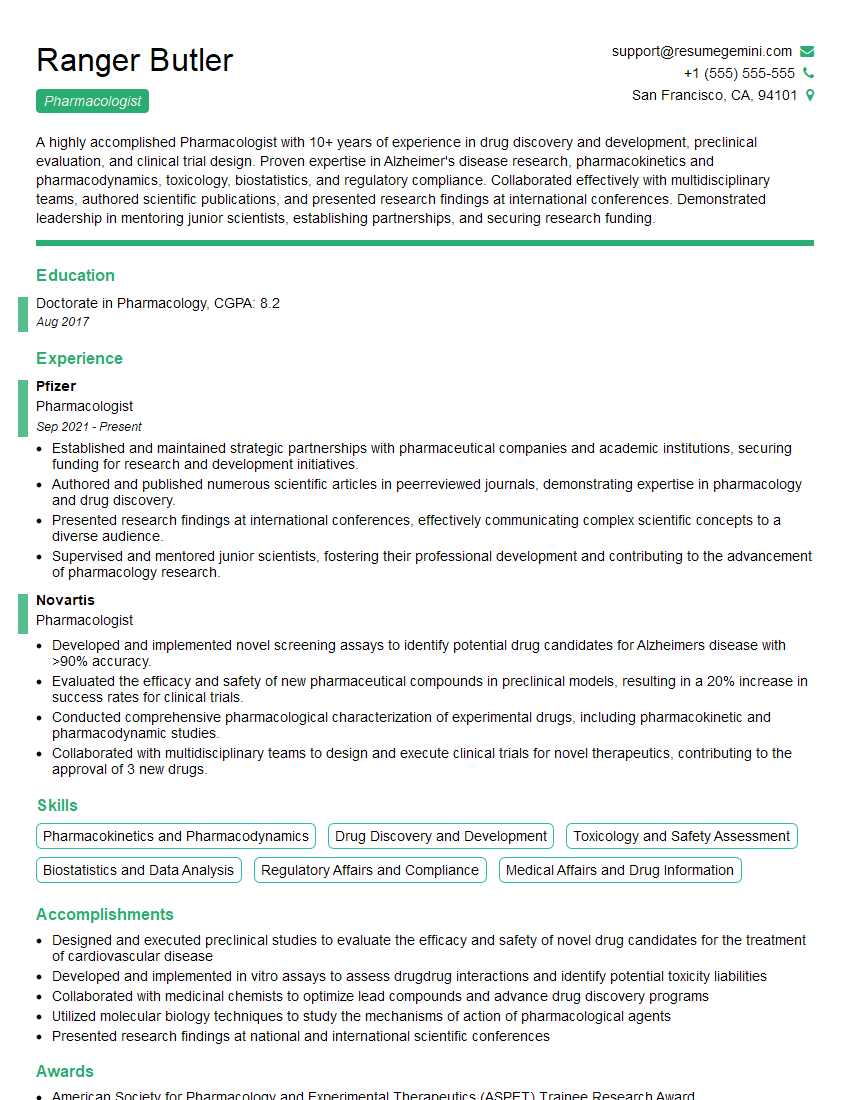
Mastering pharmacological interventions is crucial for career advancement in the pharmaceutical industry. A strong understanding of these concepts demonstrates your expertise and increases your competitiveness in a demanding job market. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini can help you build a professional and impactful resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Pharmacological Interventions to help you craft the perfect application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good