Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Physical Rehabilitation interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Physical Rehabilitation Interview
Q 1. Describe your experience with different therapeutic modalities (e.g., ultrasound, electrical stimulation).
Throughout my career, I’ve extensively utilized various therapeutic modalities. Ultrasound, for instance, uses high-frequency sound waves to generate heat deep within tissues, promoting healing and reducing inflammation. I often use it for treating conditions like muscle strains and tendonitis. The parameters, including frequency and intensity, are carefully selected based on the specific tissue and the patient’s response. For example, a lower frequency might be used for deeper penetration, while higher intensity is used for increased heating.
Electrical stimulation, on the other hand, uses electrical currents to stimulate nerves and muscles. This can be used for pain management, muscle strengthening, and reducing muscle spasms. There are various waveforms available, such as TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief, and NMES (Neuromuscular Electrical Stimulation) for muscle strengthening. I carefully select the waveform, intensity, and pulse duration based on the treatment goal. For example, for a patient with foot drop following a stroke, I might use NMES to stimulate the dorsiflexor muscles to improve gait.
My experience also includes using other modalities such as thermotherapy (heat packs), cryotherapy (ice packs), and manual therapy techniques like massage and joint mobilization. The choice of modality always depends on the patient’s specific condition, their response to treatment, and my clinical judgment.
Q 2. Explain the difference between a grade 1, 2, and 3 muscle strain.
Muscle strains are graded based on the severity of the muscle fiber damage. Think of it like tearing a piece of fabric; a grade 1 strain is like a small snag, a grade 2 is a significant tear, and a grade 3 is a complete rupture.
- Grade 1: This involves mild stretching or minor tearing of muscle fibers. Patients experience mild pain and tenderness, minimal swelling, and usually retain near-normal muscle strength. Recovery time is generally short.
- Grade 2: This involves a more significant tear of muscle fibers, with moderate pain and swelling. Muscle strength is noticeably decreased, and there may be palpable bruising. Recovery takes longer than a grade 1 strain.
- Grade 3: This represents a complete rupture of the muscle, often resulting in severe pain and significant swelling. Muscle strength is severely impaired, and there’s often a palpable gap in the muscle. Recovery is lengthy and may require surgical intervention.
For example, a grade 1 hamstring strain might only cause slight discomfort during running, while a grade 3 strain would likely result in immediate, intense pain and inability to walk.
Q 3. How do you assess a patient’s range of motion (ROM)?
Assessing a patient’s range of motion (ROM) is crucial for determining the extent of joint limitation and guiding treatment. I use a combination of methods for a comprehensive assessment.
Firstly, I conduct an active ROM assessment, where the patient moves the joint themselves through the available range. This helps assess their active participation and motor control. Then, I conduct a passive ROM assessment, where I move the joint for the patient, identifying any limitations due to tissue tightness or joint restrictions. Throughout these assessments, I use a goniometer to measure the angles and document the findings accurately. The goniometer is a simple device that measures joint angles, providing objective data.
Furthermore, I observe the quality of movement, noting any pain, muscle guarding, or crepitus (grinding sound). For example, if a patient has limited shoulder abduction (raising the arm to the side) I’d assess the active and passive range and check for pain or muscle spasm during the movement to determine if there are muscular limitations, joint restrictions or pain from inflammation. This helps me formulate a tailored treatment plan to address the underlying cause of restricted ROM.
Q 4. What are the key components of a comprehensive patient assessment in physical rehabilitation?
A comprehensive patient assessment is the cornerstone of effective physical rehabilitation. It involves gathering information from multiple sources to create a holistic picture of the patient’s condition and needs. Key components include:
- Patient History: This includes medical history, current medications, past injuries, and the patient’s description of their symptoms, and how it affects their daily life. Understanding the context of their injury is crucial.
- Systems Review: This involves a brief assessment of various body systems to identify potential contributing factors or co-morbidities. I look for any neurological, cardiovascular, or respiratory issues that could affect the rehabilitation process.
- Musculoskeletal Examination: This is the most detailed part, including posture assessment, palpation for muscle tenderness or abnormalities, ROM assessments (as previously described), strength testing, and functional assessments of daily activities.
- Neurological Examination (if applicable): If indicated by the patient’s history or symptoms, a neurological exam checks reflexes, sensation, and coordination to assess any nerve damage or neurological dysfunction.
- Functional Assessment: This assesses how the patient’s condition impacts their daily life activities such as walking, dressing, or lifting. I’d ask about their goals and what activities they want to be able to return to.
Using this information, I develop a personalized treatment plan that addresses the patient’s unique needs and aims to achieve their goals.
Q 5. Describe your experience with gait analysis and intervention.
Gait analysis involves observing and analyzing a patient’s walking pattern to identify any deviations or impairments. My experience includes using both observational gait analysis and more advanced methods. Observational gait analysis involves carefully watching the patient walk, noting any asymmetries in stride length, cadence, or foot placement. This is often the first step and is a critical component for identifying any potential gait issues.
For more detailed analysis, we may use motion capture systems or other technologies to quantify the gait parameters. These systems record multiple kinematic data points such as joint angles, joint moments, and ground reaction forces that give detailed information on the patient’s gait pattern. We use these data points to identify areas where the patient’s movement is abnormal, which in turn guides the creation of a more precise and effective treatment plan.
Gait intervention may involve strengthening exercises to improve muscle function, balance training to enhance stability, and orthotic devices such as braces or splints to correct biomechanical abnormalities. For example, a patient with a foot drop may require strengthening exercises for their dorsiflexor muscles and a functional electrical stimulation unit to assist in improving their gait pattern. I always tailor interventions to meet the individual patient’s needs and capabilities.
Q 6. How do you adapt treatment plans for patients with co-morbidities?
Patients often present with co-morbidities (additional medical conditions) that can significantly influence their rehabilitation. Adapting treatment plans requires careful consideration of these factors to ensure patient safety and effectiveness. For instance, a patient with diabetes and a knee injury will require adjustments to their exercise plan to avoid excessive stress on their joints and to consider their overall health status. A patient with heart failure requires careful monitoring of their cardiovascular response to exercise.
My approach involves:
- Collaboration with other healthcare professionals: I work closely with physicians, nurses, and other specialists to coordinate care and ensure the treatment plan aligns with the patient’s overall health status.
- Modifying intensity and duration of exercise: I might reduce the intensity or duration of exercises to account for the patient’s limitations imposed by their co-morbidities.
- Selecting appropriate exercises: Certain exercises might need to be avoided or modified to prevent further complications. For example, high-impact exercises could be detrimental for patients with osteoporosis.
- Frequent monitoring of vital signs: This is crucial, particularly for patients with cardiovascular or respiratory conditions, to ensure safety during treatment. I regularly monitor heart rate, blood pressure, and oxygen saturation levels.
The ultimate goal is to create a safe and effective rehabilitation program that addresses the patient’s primary condition while respecting their overall health status and mitigating any potential risks.
Q 7. Explain the principles of neuromuscular re-education.
Neuromuscular re-education focuses on restoring optimal function of the nervous and muscular systems. It aims to improve motor control, coordination, and muscle strength. This is particularly important in patients recovering from neurological injuries or surgeries. The principles underpinning this approach are:
- Motor Learning: This emphasizes the importance of repetition and practice to improve motor skills. It’s like learning a new dance routine – repeated practice is required to improve execution.
- Feedback Mechanisms: Providing patients with feedback about their performance is critical. This may involve visual, auditory, or kinesthetic feedback. For example, a patient learning to walk again might use a mirror to monitor their gait or receive verbal cues from the therapist.
- Proprioception Training: This focuses on improving the body’s awareness of its position in space. Exercises involving balance boards, wobble boards, and other unstable surfaces are commonly used.
- Functional Training: Exercises are focused on functional movements relevant to the patient’s daily life. For example, instead of isolating muscle groups, we focus on training the patient to perform functional activities like walking, reaching, and lifting.
- Task-Specific Training: Training activities directly relate to the tasks that the patient struggles with. This helps to improve their performance in real-world situations.
Successful neuromuscular re-education requires a patient-centered approach, tailoring exercises to individual needs and constantly assessing progress. It requires a combination of skilled interventions and the patients’ active engagement and motivation.
Q 8. Describe your experience with different types of assistive devices.
My experience with assistive devices spans a wide range, encompassing both mobility and daily living aids. I’m proficient in assessing patient needs and recommending appropriate devices, considering factors like the individual’s physical capabilities, home environment, and budget.
- Mobility Aids: I have extensive experience fitting and training patients on the use of wheelchairs (manual and powered), walkers, canes, crutches, and gait trainers. For example, I recently worked with a stroke patient who required a customized wheelchair to accommodate her hemiparesis. We carefully considered seat height, armrest positioning, and the addition of specialized features to optimize her independence.
- Daily Living Aids: I’m familiar with a variety of adaptive equipment designed to assist with activities of daily living (ADLs), including reachers, dressing sticks, adaptive utensils, and bath benches. I often collaborate with occupational therapists to ensure a holistic approach to ADL assistance. For instance, I helped a patient with arthritis select appropriate adaptive kitchen tools that minimized strain on her joints while preparing meals.
- Prosthetics and Orthotics: While not directly involved in fabrication, I collaborate closely with prosthetists and orthotists to ensure appropriate fitting and rehabilitation following limb loss or injury. I focus on the functional aspects, assisting patients in adapting to their new devices and improving their gait and mobility.
My approach emphasizes patient education and empowerment, ensuring they understand how to safely and effectively use their assistive devices to maximize their independence and quality of life.
Q 9. How do you measure and document patient progress?
Measuring and documenting patient progress is crucial for effective rehabilitation. It involves a multifaceted approach that combines objective and subjective data to track improvement over time.
- Objective Measurements: These include quantifiable data such as range of motion (ROM) using a goniometer, strength testing with dynamometry, timed functional tasks (e.g., time to walk 10 meters), and distance walked during gait analysis. I meticulously record these measurements in the patient’s chart, often using standardized assessment tools.
- Subjective Measurements: These capture the patient’s perception of their progress. I regularly ask patients about their pain levels (using a visual analog scale or numeric rating scale), their functional abilities (ability to perform ADLs), and their overall satisfaction with their progress. I encourage open communication to understand any challenges or concerns they may have.
- Functional Assessments: I employ standardized functional assessments such as the Berg Balance Scale, Functional Gait Assessment, and Timed Up and Go test to provide a comprehensive picture of the patient’s functional abilities. These assessments allow me to track improvement over time and adjust treatment as needed.
This combined data allows for a detailed and accurate depiction of the patient’s progress, enabling me to modify interventions and optimize treatment plans for optimal outcomes. For instance, if a patient’s strength is not improving as anticipated, I might adjust the exercise program to focus on different muscle groups or resistance levels.
Q 10. What is your experience with developing and implementing home exercise programs (HEPs)?
Developing and implementing effective home exercise programs (HEPs) is a cornerstone of physical rehabilitation. My approach emphasizes creating programs that are individualized, safe, and achievable for each patient.
- Patient Assessment: The process begins with a thorough assessment of the patient’s physical condition, functional limitations, and goals. I carefully consider their medical history, available resources at home, and their level of understanding and motivation.
- Program Design: I tailor the HEP to address specific impairments and functional limitations. Exercises are carefully chosen based on evidence-based practice and incorporate principles of progressive overload and specificity. I provide clear instructions, demonstrations, and visual aids (videos, pictures) to ensure the patient understands the exercises correctly.
- Safety Considerations: Safety is paramount. I emphasize proper body mechanics, modify exercises as needed, and provide clear guidelines for when to stop and seek medical attention. I often provide patients with contact information to ensure easy communication.
- Follow-up and Modifications: I schedule regular follow-up appointments or phone calls to monitor progress, address any concerns, and make necessary adjustments to the HEP. Patient feedback is crucial for refining the program and ensuring its effectiveness.
For example, for a patient recovering from a knee replacement, I would design a HEP that focuses on range of motion exercises, strengthening of the quadriceps and hamstrings, and balance training. The program would be gradually progressed based on the patient’s response and tolerance. A written and visual HEP would be provided to improve adherence.
Q 11. Explain your understanding of evidence-based practice in physical rehabilitation.
Evidence-based practice (EBP) is fundamental to my approach to physical rehabilitation. EBP involves integrating the best available research evidence with clinical expertise and patient values to make informed decisions about patient care.
- Research Literature: I regularly review peer-reviewed research articles, clinical guidelines, and systematic reviews to stay updated on the latest evidence regarding treatment approaches, assessment tools, and rehabilitation techniques. This ensures that my practice is informed by the most current scientific findings.
- Clinical Expertise: My years of experience provide me with a deep understanding of various conditions, treatment options, and patient responses. I use my clinical judgment to interpret research findings and adapt them to individual patient needs.
- Patient Values and Preferences: I actively involve patients in the decision-making process, respecting their preferences and considering their values and goals. Understanding their concerns and expectations guides the treatment plan and fosters a strong therapeutic alliance.
For instance, when deciding on a specific exercise regimen for a patient with osteoarthritis, I would consult research on the effectiveness of different exercise modalities (e.g., strengthening, aerobic, aquatic therapy) and select the approach most supported by the evidence while considering the patient’s preferences and physical limitations.
Q 12. How do you manage patients with pain?
Pain management is a crucial aspect of physical rehabilitation. My approach is holistic and considers both pharmacological and non-pharmacological interventions.
- Pain Assessment: I meticulously assess the patient’s pain using validated scales (visual analog scale, numeric rating scale), location, character, intensity, duration, and aggravating/relieving factors. This provides a baseline for monitoring progress and evaluating the effectiveness of interventions.
- Non-pharmacological Interventions: These form the cornerstone of my approach and include modalities such as therapeutic exercise, manual therapy (mobilization, massage), electrotherapy (TENS, ultrasound), heat/ice therapy, and patient education on pain management strategies.
- Pharmacological Interventions: While I don’t prescribe medication, I collaborate closely with physicians and other healthcare providers to coordinate pain medication management and ensure it aligns with the rehabilitation plan.
- Psychological Interventions: Addressing the psychological aspects of pain, such as anxiety and depression, is crucial. I may refer patients to psychologists or counselors if necessary or incorporate relaxation techniques into the rehabilitation program.
For example, a patient with chronic low back pain might benefit from a combination of core strengthening exercises, manual therapy to address joint restrictions, and education on proper posture and lifting techniques, along with appropriate medication management as prescribed by their physician.
Q 13. Describe your experience with wound care management.
While not a primary focus of my practice, I have experience with wound care management, particularly in the context of pressure injuries and other wounds that may occur in individuals with limited mobility or compromised circulation.
- Assessment and Documentation: I assess wound characteristics (size, depth, location, exudate, presence of infection) and meticulously document findings. This allows for monitoring of healing progress and identification of any complications.
- Wound Cleansing and Debridement: I perform wound cleansing and debridement under the guidance of a physician or wound care specialist, adhering to strict aseptic techniques.
- Wound Dressing Selection: I choose appropriate wound dressings based on the wound type and characteristics. My knowledge of different dressings (gauze, hydrocolloids, alginates, foams) allows me to optimize the healing environment.
- Collaboration with Wound Care Specialists: For complex wounds or infections, I collaborate with wound care specialists and physicians to ensure optimal management. I often assist in educating patients about wound care at home and emphasize the importance of adherence to prescribed treatment.
For instance, I’ve assisted in the management of pressure injuries in patients with limited mobility by ensuring proper positioning, implementing pressure-relieving measures, and applying appropriate wound dressings under the guidance of a physician.
Q 14. How do you communicate effectively with patients and their families?
Effective communication is crucial for successful patient care. My approach emphasizes active listening, clear explanations, and empathy.
- Active Listening: I actively listen to patients to understand their concerns, goals, and perspectives. I use open-ended questions to encourage them to share their experiences and build rapport.
- Clear Explanations: I explain complex medical information in clear, simple language, avoiding jargon. I utilize visual aids (diagrams, models) when appropriate to enhance understanding.
- Empathy and Compassion: I demonstrate empathy and compassion, acknowledging the patient’s emotional and psychological needs. I create a safe and supportive environment where patients feel comfortable sharing their feelings and concerns.
- Family Involvement: I actively involve family members in the rehabilitation process, providing education, answering questions, and coordinating care. I ensure that all communication is clear, consistent, and respectful.
- Documentation: Clear and concise documentation of all patient interactions and treatment plans is crucial for effective communication among healthcare professionals.
For instance, I always ensure patients understand their diagnosis, treatment plan, and prognosis in terms they can easily grasp, and encourage them to ask questions. Involving family members in the process ensures a cohesive approach to care and supports the patient’s rehabilitation journey.
Q 15. Explain your understanding of the stages of wound healing.
Wound healing is a complex process typically divided into four overlapping stages: hemostasis, inflammation, proliferation, and maturation. Think of it like building a house; each stage is crucial for a strong and stable final structure.
- Hemostasis: This initial phase involves blood clotting to stop bleeding and form a fibrin clot, which acts as a scaffold for new tissue growth. It’s like laying the foundation for our ‘house’.
- Inflammation: This stage, lasting a few days, involves white blood cells clearing debris and fighting infection, causing redness, swelling, and pain. This is akin to clearing the land before construction begins.
- Proliferation: This phase focuses on building new tissue. Fibroblasts produce collagen, creating a granulation tissue that fills the wound bed. This is the construction phase of our ‘house’, where the walls and roof are built.
- Maturation: This final stage involves collagen remodeling, strengthening the scar tissue, and returning the wound to its normal appearance. This is like the landscaping and finishing touches after construction is complete. The scar may remain but becomes less noticeable over time.
Understanding these stages allows us to tailor treatment, such as debridement (removal of dead tissue) in the inflammation phase or promoting collagen synthesis in the proliferation phase. For example, a patient with a pressure ulcer might require frequent wound dressing changes and meticulous infection control during the inflammation phase, followed by the application of growth factors during the proliferation phase to enhance tissue regeneration.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure patient safety during treatment?
Patient safety is paramount in physical rehabilitation. My approach is multifaceted and begins with a thorough assessment of each patient’s medical history, current condition, and any potential risks. This includes reviewing medication lists, identifying allergies, and understanding any cognitive or physical limitations.
- Risk Assessment: I perform a detailed assessment to identify potential risks such as falls, skin breakdown, or adverse reactions to treatment. For instance, patients with balance impairments would require extra support during exercises.
- Safe Environment: I ensure the treatment environment is safe, free from obstacles, and appropriately equipped. This involves checking equipment functionality, using appropriate assistive devices, and maintaining a clean and organized space.
- Communication: Clear and consistent communication with the patient is essential. I explain each procedure, emphasizing patient participation in decision-making and encouraging them to voice any discomfort or concerns. This fosters trust and builds a safer experience.
- Documentation: Meticulous documentation of all treatments, assessments, and any incidents is crucial for tracking progress and identifying potential problems early.
- Emergency Preparedness: I’m familiar with emergency procedures and have access to emergency equipment. Knowledge of CPR and first aid are fundamental.
For example, with a patient exhibiting signs of dizziness, I would modify the exercise intensity and incorporate strategies to improve balance and proprioception (body awareness) before progressing to more challenging activities. Safety protocols are continuously adapted to the patient’s changing condition and response to therapy.
Q 17. Describe your experience with patients with neurological conditions.
I have extensive experience working with patients experiencing various neurological conditions, including stroke, multiple sclerosis (MS), Parkinson’s disease, and traumatic brain injury (TBI). My approach focuses on individualized treatment plans targeting specific functional deficits.
For instance, a stroke patient with hemiparesis (weakness on one side of the body) would benefit from targeted strengthening exercises, functional training activities like dressing and eating, and constraint-induced movement therapy (CIMT) to improve the affected limb’s function. Similarly, a patient with Parkinson’s disease would require exercises that focus on improving balance, gait, and coordination. A crucial part of this involves patient education on managing symptoms, maximizing independence, and improving overall quality of life. I often collaborate with other healthcare professionals, such as neurologists and occupational therapists, to provide holistic care.
Each case presents unique challenges. I remember one patient with MS who experienced significant fatigue. We carefully tailored the treatment schedule to avoid overexertion, incorporating rest periods throughout the sessions, and focusing on energy conservation strategies.
Q 18. How do you adapt your treatment for patients with cognitive impairments?
Treating patients with cognitive impairments requires a modified approach focused on simplicity, repetition, and clear communication. Adapting treatment involves strategies that accommodate their cognitive abilities and memory limitations.
- Simple Instructions: I use concise and straightforward instructions, avoiding complex terminology. Visual aids like pictures or diagrams can significantly improve understanding.
- Repetition and Reinforcement: I incorporate repetition of exercises and tasks, providing consistent feedback to aid learning and retention. Positive reinforcement is key to motivation.
- Breaking Down Tasks: Complex tasks are broken into smaller, manageable steps to reduce cognitive overload. This helps patients achieve success and build confidence.
- Environmental Modifications: The treatment environment is adapted to reduce distractions and promote focus. This might involve minimizing noise or clutter.
- Caregiver Involvement: Collaborating with caregivers is essential for consistency and reinforcement of the treatment plan outside the therapy sessions.
For example, when working with a patient with dementia, I might teach a simple exercise routine using hand gestures and visual cues, repeating each step several times. Success depends on tailoring the intervention to the individual’s specific cognitive deficits and ensuring they feel safe and understood.
Q 19. What is your experience with functional electrical stimulation (FES)?
Functional electrical stimulation (FES) is a valuable tool in my practice, used to activate muscles using electrical impulses. It’s particularly helpful for patients with neurological conditions causing muscle weakness or paralysis.
My experience with FES includes using it to improve muscle strength and function in patients post-stroke or with spinal cord injuries. For example, FES can be applied to the lower extremities to facilitate walking in patients with paraplegia. It also assists in preventing muscle atrophy and improving range of motion. However, it’s important to remember that FES is not a standalone treatment; it’s often used in conjunction with other therapeutic interventions, such as traditional exercises and manual therapy. Appropriate patient selection and careful monitoring are crucial to ensure safety and effectiveness. For example, patients with certain cardiac conditions may be unsuitable for FES.
The application requires careful consideration of electrode placement, pulse parameters, and patient monitoring to prevent skin irritation and discomfort.
Q 20. How do you utilize outcome measures to assess patient progress?
Outcome measures are crucial for objectively assessing patient progress and the effectiveness of interventions. They provide quantifiable data to track changes over time and inform treatment modifications.
I use a variety of outcome measures, including both standardized tests and patient-reported outcome measures (PROMs). Examples of standardized tests include the Berg Balance Scale (BBS) to assess balance, the Functional Independence Measure (FIM) to evaluate functional abilities, and the 6-Minute Walk Test (6MWT) for assessing endurance. PROMs, like the Patient-Specific Functional Scale (PSFS), allow patients to rate their functional limitations based on their personal goals. The choice of outcome measure depends on the patient’s condition and treatment goals.
The data collected allows me to evaluate the effectiveness of the chosen interventions, justify continued treatment, and provide evidence of progress to the referring physician and the patient. For example, tracking a patient’s walking distance using the 6MWT over several weeks provides objective evidence of improved endurance and informs adjustments to the exercise program.
Q 21. Describe your experience with manual therapy techniques.
Manual therapy techniques are an integral part of my practice, encompassing a wide range of hands-on treatments to address musculoskeletal impairments. These techniques aim to improve joint mobility, reduce pain, and enhance muscle function.
My experience includes various manual therapy approaches, such as mobilization/manipulation of joints, soft tissue mobilization (massage), and muscle energy techniques. For example, I use spinal manipulation to address restricted spinal mobility in patients with back pain, carefully assessing for contraindications before performing any adjustments. Soft tissue mobilization helps alleviate muscle tightness and improve flexibility, while muscle energy techniques engage patient participation to improve muscle strength and lengthen shortened muscles. These techniques are often integrated with exercise programs to maximize benefits.
For instance, a patient with neck pain might benefit from a combination of cervical spine mobilization to restore joint movement, soft tissue massage to release muscle tension, and strengthening exercises to stabilize the neck. The selection of techniques is tailored to the patient’s specific needs and always prioritizes safety and patient comfort. A thorough assessment and clear communication with the patient are critical before and during treatment.
Q 22. How do you prioritize patient care when faced with multiple competing demands?
Prioritizing patient care amidst competing demands is a cornerstone of effective physical rehabilitation. I approach this using a structured prioritization system, combining urgency and importance. I utilize a triage system, similar to what’s used in emergency medicine, mentally assessing each patient’s needs. Patients requiring immediate intervention due to acute pain, risk of further injury, or critical functional limitations take precedence. This might involve a patient who has experienced a sudden fall and needs immediate pain management and mobility assessment. Less urgent, but still important, tasks, such as long-term goal planning or administrative duties, are scheduled strategically throughout the day. I also employ time-blocking techniques to allocate specific time slots for various patient needs and administrative tasks, ensuring that I consistently meet the demands of all patients. Open communication with patients and their families helps manage expectations and ensures they understand the prioritization process. Finally, regular review and adjustment of my schedule is key to ensuring its ongoing effectiveness.
Q 23. Explain your understanding of HIPAA regulations and patient confidentiality.
HIPAA (Health Insurance Portability and Accountability Act) regulations are paramount in my practice. They safeguard patient privacy by outlining strict rules on the handling, storage, and disclosure of protected health information (PHI). PHI includes anything that can identify a patient – from their name and medical records to their social security number and even their treatment location. My understanding of HIPAA encompasses several key areas:
- Confidentiality: I never discuss a patient’s information with anyone unless they have explicit permission or it is required by law (e.g., reporting child abuse).
- Access control: I strictly adhere to access restrictions to electronic health records (EHRs), ensuring only authorized personnel can view patient information. This includes using unique login credentials and adhering to password security protocols.
- Disclosure: I only release PHI with the patient’s written consent, except in limited circumstances permitted by law, such as public health emergencies or legal mandates.
- Data security: I understand the importance of securing patient data both electronically and physically. This means using strong passwords, up-to-date anti-virus software, and securely storing physical files.
Q 24. How do you handle challenging patients or difficult situations?
Handling challenging patients or difficult situations requires empathy, patience, and a problem-solving approach. I begin by actively listening to understand their concerns and perspectives. For example, if a patient is frustrated with their progress, I would collaboratively explore their concerns and adjust the treatment plan if needed. Sometimes this may involve involving the family or caretakers to better understand the individual’s needs. I focus on building rapport, using clear and respectful communication. If a situation escalates, I remain calm and professional, de-escalating the situation through active listening and validating their feelings. If I’m unable to manage the situation effectively on my own, I involve my supervisor or other members of the interdisciplinary team for support and guidance. In some cases, referral to a psychologist or other specialist may be appropriate. Maintaining professional boundaries while demonstrating empathy and care is crucial in these scenarios.
Q 25. What is your experience working with interdisciplinary teams?
I have extensive experience collaborating within interdisciplinary teams, comprising physicians, nurses, occupational therapists, speech therapists, and social workers. In my previous role at [Previous Institution Name], we regularly held case conferences to discuss patient progress, treatment plans, and discharge planning. This collaborative approach has led to enhanced patient outcomes. For instance, during the treatment of a stroke patient, collaborating with occupational therapists on upper limb exercises and speech therapists on swallowing therapy resulted in a significantly better functional recovery for the patient. Effectively communicating with team members, actively listening to their perspectives, and respecting their expertise are crucial aspects of my team approach. I also understand the value of respecting differing opinions and seeking consensus when making treatment decisions, always keeping the patient’s best interests as the central focus.
Q 26. Describe your experience with documentation and electronic health records (EHRs).
I am highly proficient in documentation and utilizing electronic health records (EHRs). Throughout my career, I have used various EHR systems, including [List EHR systems, e.g., Epic, Cerner]. My documentation is detailed, accurate, and compliant with all relevant regulations, including HIPAA. I focus on recording objective measurements, subjective patient reports, interventions performed, and patient’s response to treatment. This includes documenting functional assessments, treatment plans, progress notes, and discharge summaries. Accurate documentation is vital for continuity of care, communication with other healthcare providers, and for tracking patient progress and outcomes. I also understand the importance of proper coding and billing procedures within the EHR system, ensuring accurate claims processing. My goal is to maintain clear, concise, and comprehensive documentation that meets all legal and clinical standards. I regularly participate in continuing education sessions on best practices in EHR usage and medical documentation.
Q 27. How do you stay up-to-date with the latest advancements in physical rehabilitation?
Staying current with advancements in physical rehabilitation is a continuous process. I actively participate in professional development activities such as attending conferences ([List Conferences, e.g., APTA CSM]), workshops, and webinars. I regularly review peer-reviewed journals ([List Journals, e.g., Physical Therapy, Journal of Orthopaedic & Sports Physical Therapy]) and subscribe to relevant professional organizations ([List Organizations, e.g., APTA]). I also actively seek out continuing education opportunities, both online and in-person, to learn about new techniques, technologies, and research findings. This continuous learning approach ensures that I am providing my patients with the most effective and evidence-based care available. Staying abreast of new research in areas such as robotic rehabilitation, telehealth, and innovative treatment approaches is vital for providing optimal patient care.
Q 28. What are your salary expectations?
My salary expectations are in line with the current market rate for experienced physical therapists with my qualifications and experience in [Location/Type of Setting]. I am open to discussing a competitive compensation package that reflects my skills and contributions to your organization. I am confident that my expertise and dedication will be a valuable asset to your team, and I am eager to discuss this further.
Key Topics to Learn for Physical Rehabilitation Interview
- Neuromuscular Rehabilitation: Understanding neurological conditions impacting movement, and applying therapeutic interventions like strengthening, range of motion exercises, and functional training. Practical application includes developing individualized treatment plans for stroke patients focusing on regaining lost motor skills.
- Musculoskeletal Rehabilitation: Diagnosing and managing musculoskeletal injuries (sprains, strains, fractures) through therapeutic exercise, manual therapy, and modalities like ultrasound or electrical stimulation. Practical application involves creating a rehabilitation program post-surgery for a patient with a knee replacement, prioritizing pain management and functional restoration.
- Cardiopulmonary Rehabilitation: Managing conditions affecting the cardiovascular and respiratory systems, implementing exercise programs to improve endurance and functional capacity. Practical application includes designing a graded exercise program for a patient recovering from a heart attack, carefully monitoring vital signs and adjusting intensity.
- Biomechanics and Kinesiology: Applying principles of movement and body mechanics to assess and treat movement disorders. Practical application includes analyzing a patient’s gait pattern to identify compensations and develop strategies to improve efficiency and reduce pain.
- Patient Assessment and Treatment Planning: Mastering the process of conducting thorough patient evaluations, establishing goals, and developing effective treatment plans. This includes understanding various assessment tools and adapting plans based on patient progress and response to treatment.
- Ethical and Legal Considerations: Understanding professional ethics, patient rights, and legal aspects relevant to the field of physical rehabilitation. This includes maintaining patient confidentiality and adhering to professional standards of practice.
Next Steps
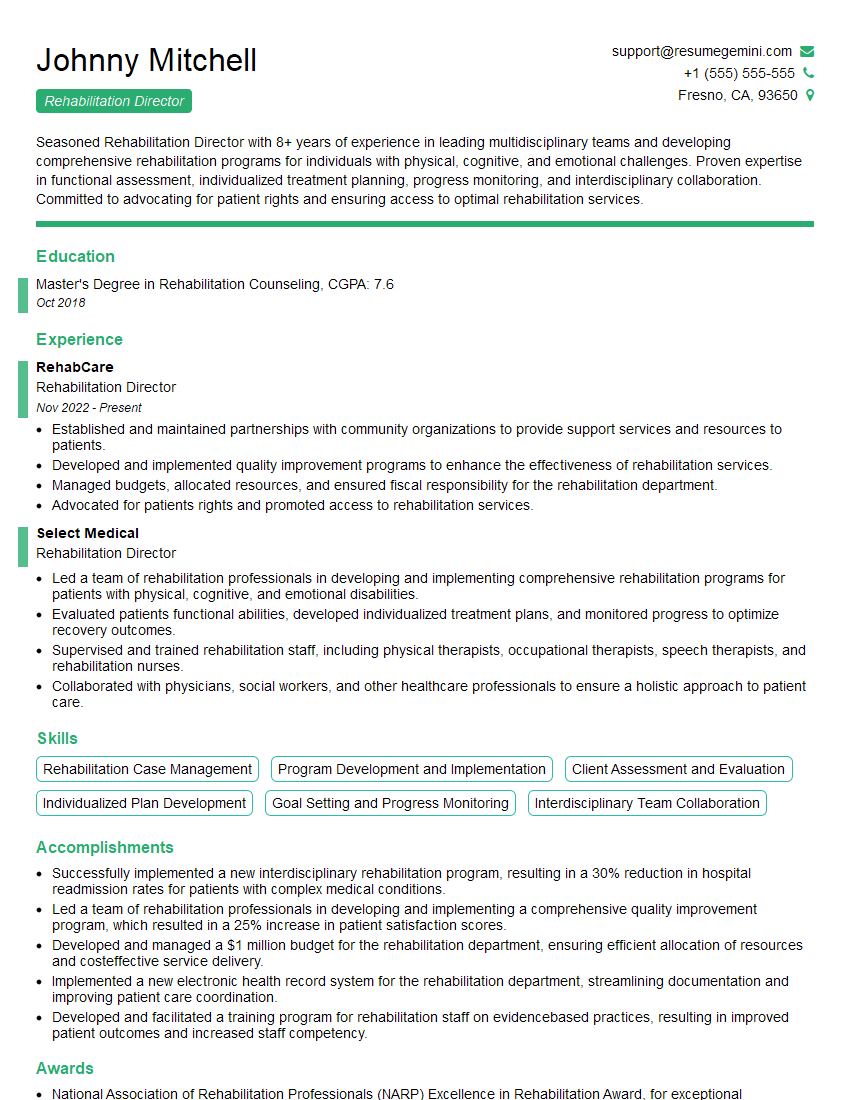
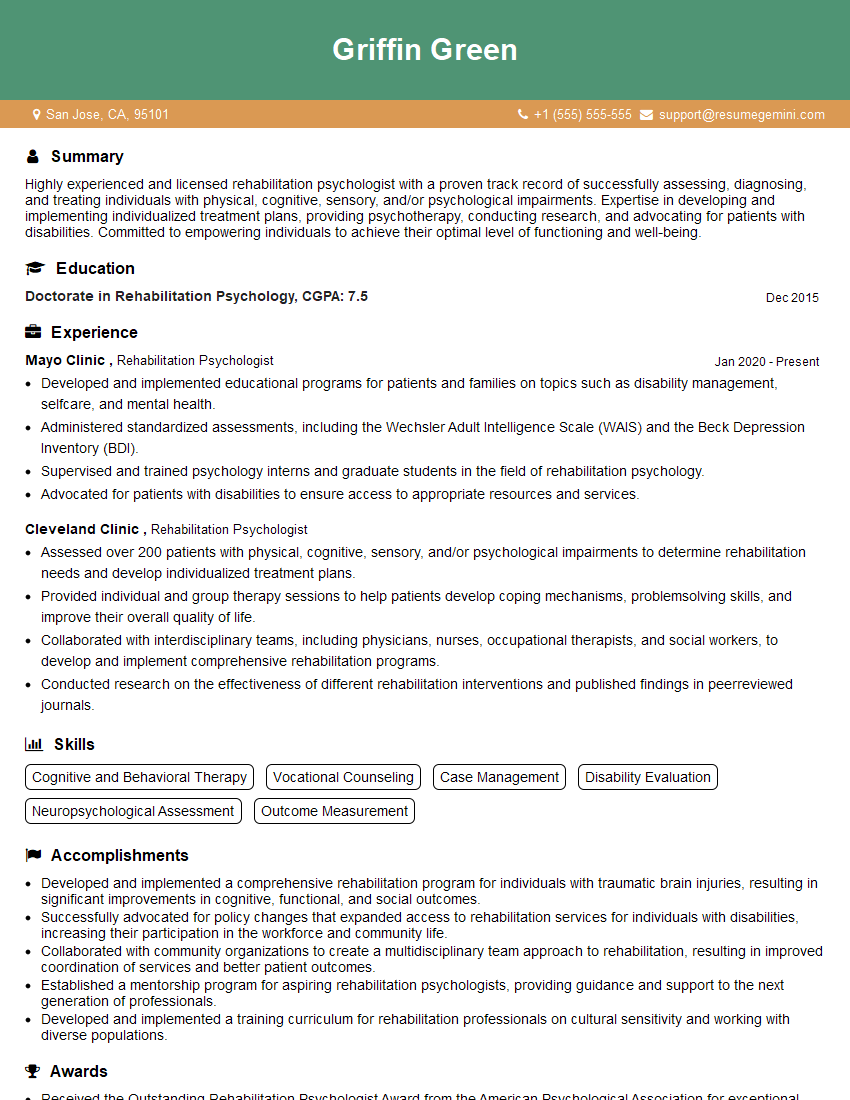
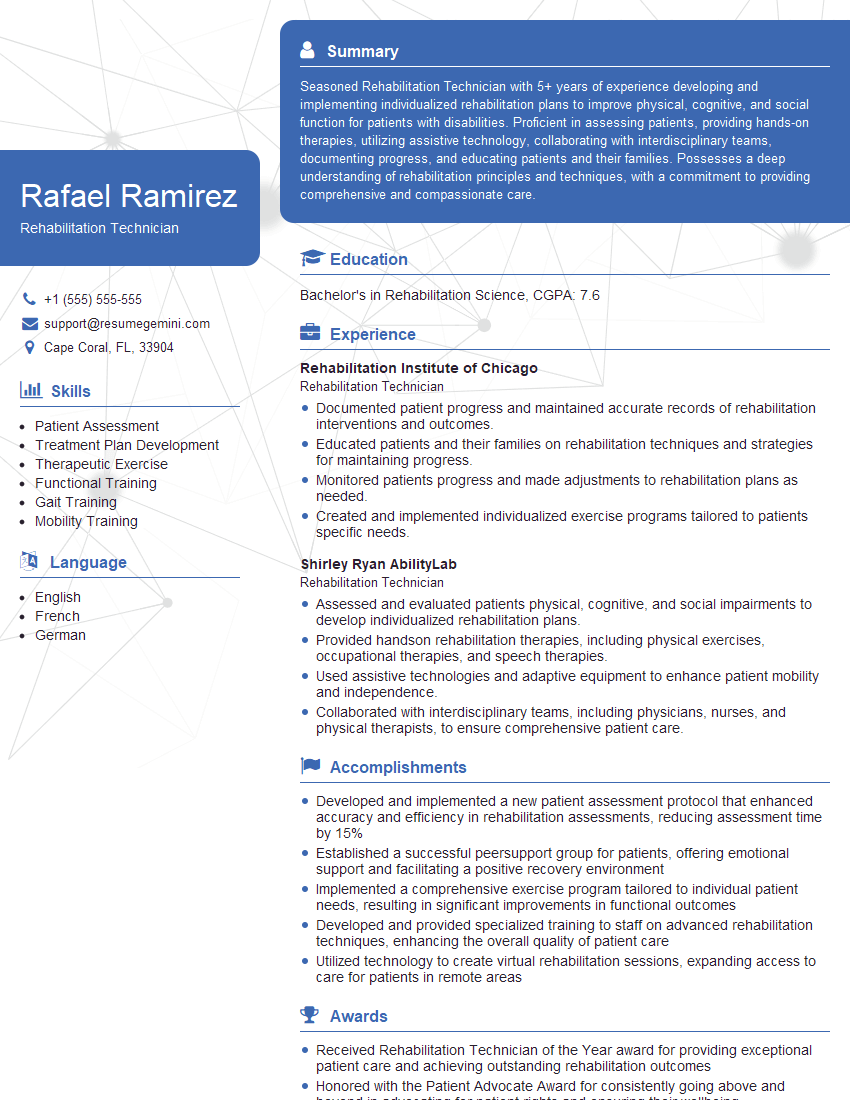
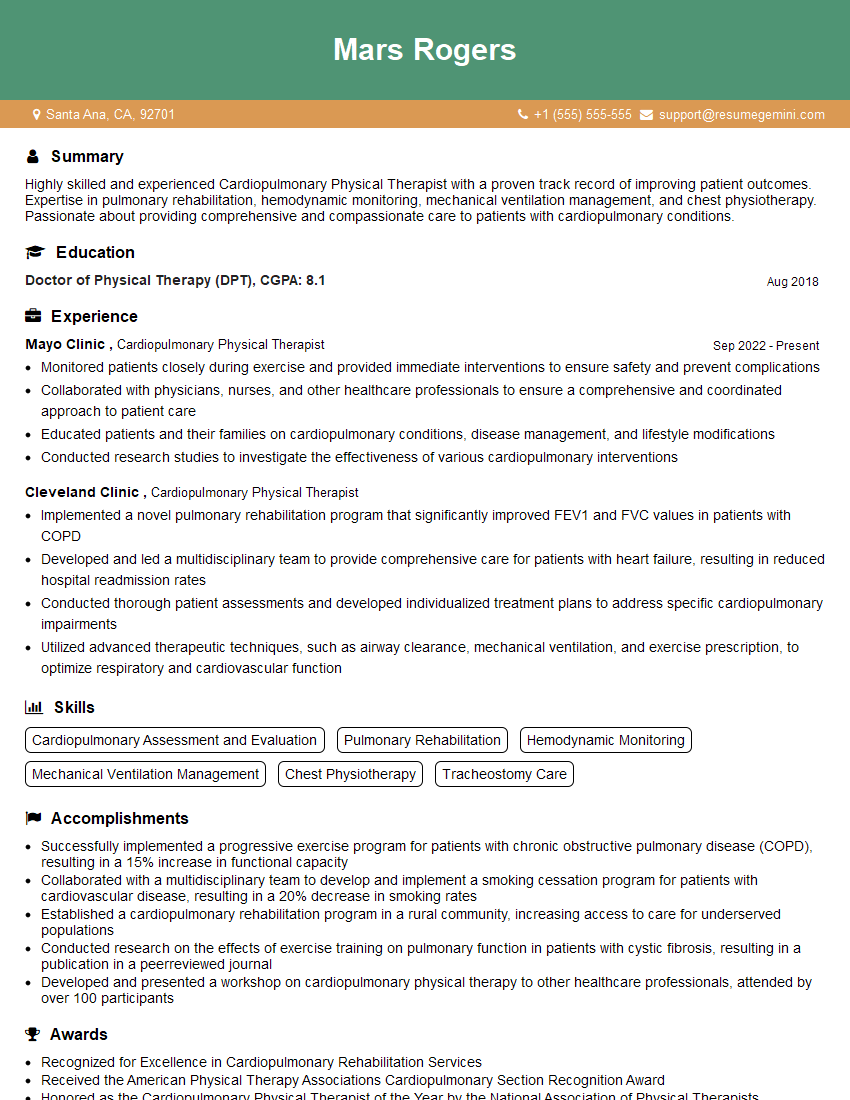
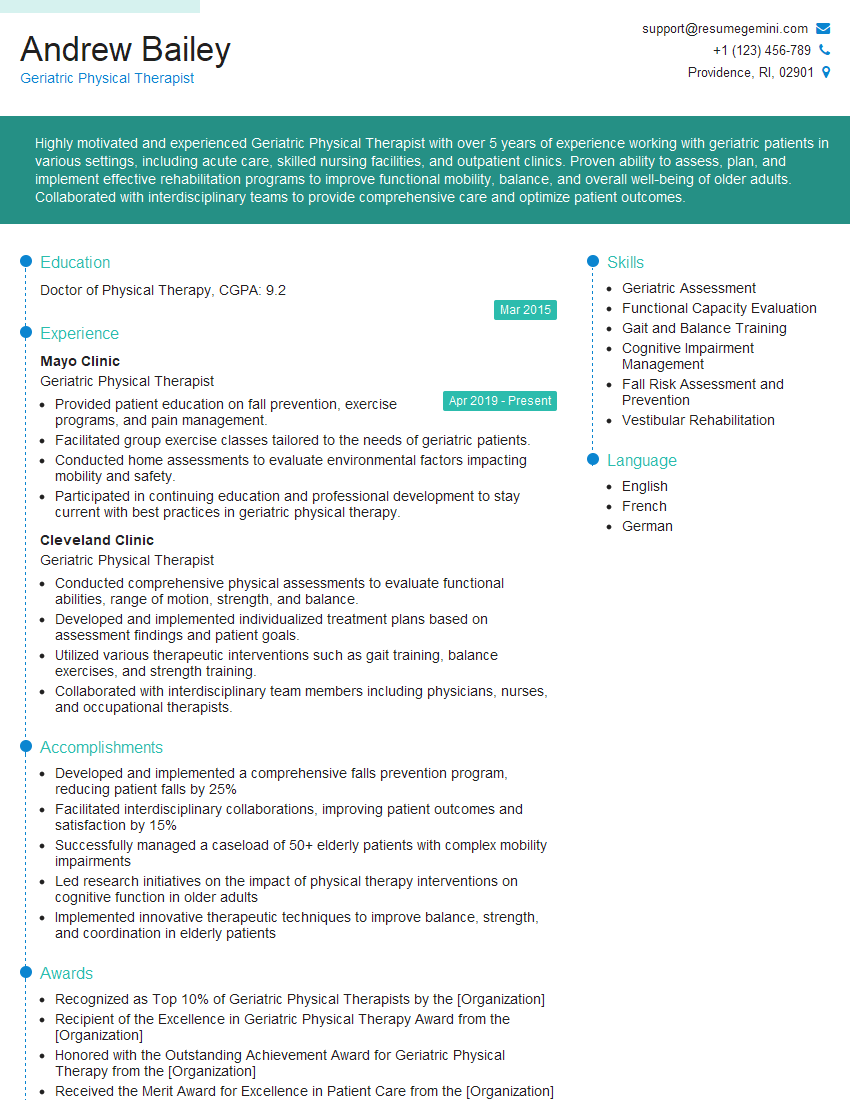
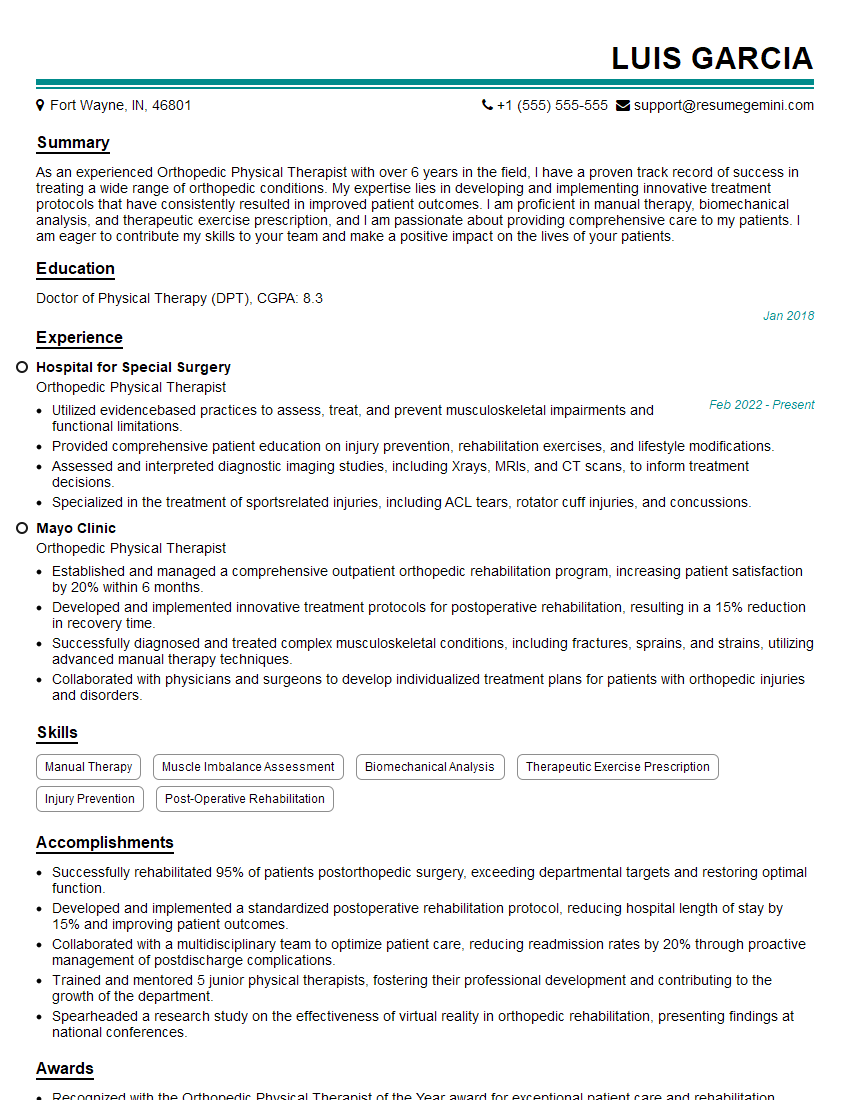
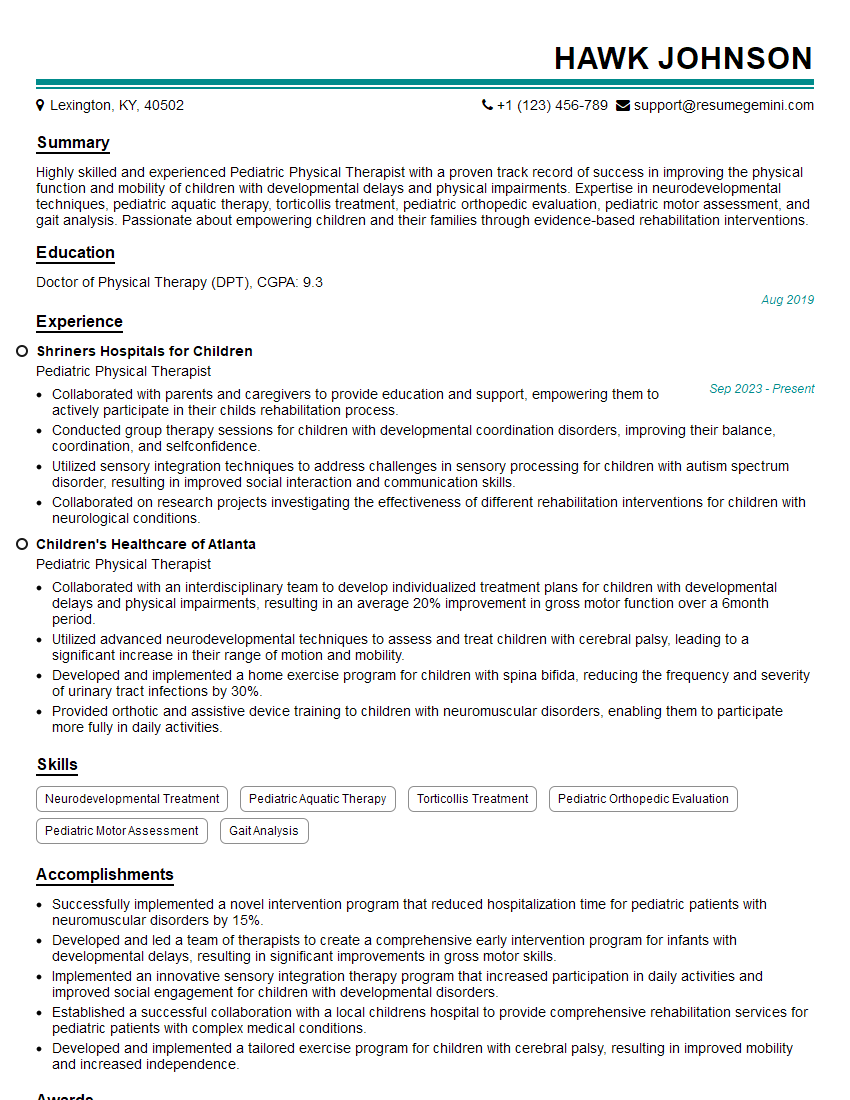
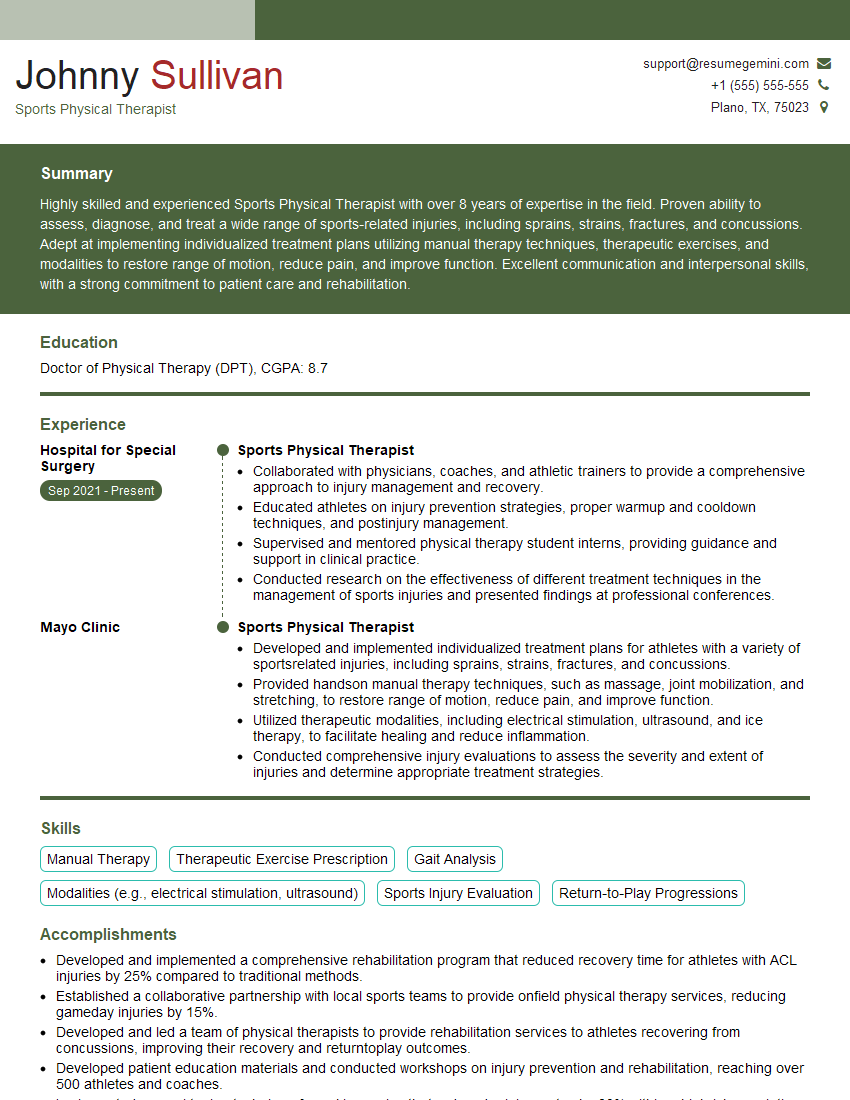
Mastering Physical Rehabilitation opens doors to a rewarding career with significant growth potential, offering opportunities in diverse settings like hospitals, clinics, and private practices. To maximize your job prospects, create a compelling and ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional resume that showcases your qualifications. We provide examples of resumes tailored to Physical Rehabilitation to guide you in crafting a winning application. Invest time in creating a strong resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good