The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to PopulationCentric Operations interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in PopulationCentric Operations Interview
Q 1. Define PopulationCentric Operations and its core principles.
PopulationCentric Operations (PCO) is a healthcare management approach that shifts the focus from individual patient encounters to the overall health of a defined population. Instead of treating illnesses reactively, PCO proactively identifies and addresses the needs of an entire population to improve health outcomes and reduce costs. Its core principles revolve around:
- Proactive Care: Preventing disease and managing chronic conditions before they become severe.
- Data-Driven Decisions: Utilizing population health data to identify trends, risks, and opportunities for intervention.
- Holistic Approach: Considering social determinants of health (like housing, income, and access to healthy food) in addition to clinical factors.
- Collaboration: Working across different healthcare sectors and community partners to create a coordinated care system.
- Value-Based Care: Focusing on improving overall population health and reducing costs, rather than solely increasing the volume of services provided.
Think of it like this: instead of fixing individual potholes on a road, PCO is about proactively improving the entire road’s infrastructure to prevent potholes from forming in the first place.
Q 2. Explain the difference between population health management and disease management.
While both population health management (PHM) and disease management (DM) aim to improve patient outcomes, their scope differs significantly. Disease management focuses on individuals with specific chronic conditions (like diabetes or heart failure), providing structured programs to help them manage their disease and prevent complications. It’s a reactive approach, intervening after a condition is diagnosed.
Population health management, on the other hand, takes a broader, proactive approach. It encompasses the entire population within a defined area or group, regardless of their health status. PHM identifies at-risk individuals, targets preventative care, and addresses social determinants of health to improve overall health outcomes and reduce healthcare costs for the entire population. DM is a component of a comprehensive PHM strategy but doesn’t represent the entire scope.
Imagine a city’s healthcare system. DM would be like running a specific program to manage the health of people with heart disease. PHM would be like developing a city-wide plan to improve the overall health of all citizens, including preventing heart disease in the first place through initiatives focused on healthy eating and exercise.
Q 3. Describe your experience with data analysis in a population health context.
In my previous role, I extensively used data analytics to identify high-risk populations and inform care strategies. We utilized several data sources, including electronic health records (EHRs), claims data, and social determinants of health (SDOH) data. My responsibilities included:
- Data Extraction and Cleaning: Pulling data from various sources, standardizing formats, and handling missing data.
- Descriptive Analytics: Calculating rates of disease, identifying trends, and characterizing at-risk subgroups using tools like SQL and R.
- Predictive Modeling: Developing models to identify individuals at high risk of hospitalization, readmission, or developing certain conditions, using techniques like regression analysis and machine learning algorithms.
- Data Visualization: Creating dashboards and reports to communicate findings to stakeholders, using tools like Tableau and Power BI. For example, I created a dashboard visualizing the correlation between SDOH factors like food insecurity and rates of diabetes within specific zip codes.
One project involved using predictive modeling to identify patients at high risk of readmission following a heart attack. By implementing targeted interventions based on the model’s predictions, we successfully reduced readmission rates by 15% within six months.
Q 4. How do you identify at-risk populations within a defined patient cohort?
Identifying at-risk populations requires a multi-faceted approach leveraging data analysis and clinical expertise. We start by defining the patient cohort and then employ several strategies:
- Risk Stratification: Using predictive modeling and clinical guidelines to assign risk scores to individuals based on their likelihood of experiencing adverse health events. This might include factors like age, chronic conditions, medication adherence, and SDOH factors.
- Data Analysis: Identifying patterns and trends in healthcare utilization, diagnoses, and outcomes within the cohort. This could involve analyzing claims data to identify high-cost patients or EHR data to identify those with multiple chronic conditions.
- Clinical Expertise: Incorporating clinical judgment to refine the identification of at-risk individuals. This might involve reviewing patient charts or conducting chart reviews to identify those who might benefit from additional support.
- Social Determinants of Health (SDOH) Assessment: Evaluating the impact of social factors such as housing stability, food security, and transportation access, as these can greatly influence health outcomes.
For instance, a risk stratification model might identify individuals with diabetes who have poor glycemic control, are non-adherent to medication, and live in a food desert as being at high risk of developing complications.
Q 5. What key performance indicators (KPIs) would you track in a PopulationCentric Operations role?
The KPIs tracked in a PCO role depend on the specific goals and objectives. However, some common and crucial KPIs include:
- Cost per Member per Month (CPMM): A measure of the average cost of caring for each member of the population. Lower CPMM indicates better cost-effectiveness.
- Hospitalization Rates: The number of hospitalizations per 1,000 members. Lower rates signal better preventative care and management of chronic conditions.
- Readmission Rates: The percentage of patients readmitted to the hospital within a specified timeframe (e.g., 30 days) after discharge. Lower rates indicate improved care transitions and follow-up.
- Emergency Department (ED) Visit Rates: The number of ED visits per 1,000 members. Lower rates show better management of acute conditions.
- Preventive Care Measures: Rates of screenings (e.g., mammograms, colonoscopies), vaccinations, and adherence to medication regimens. Higher rates demonstrate proactive healthcare engagement.
- Patient Satisfaction Scores: Measure of how satisfied members are with their healthcare experience.
- Improvement in specific health outcomes: For instance, reduction in HbA1c levels for diabetic patients or blood pressure control for hypertensive patients.
These KPIs are tracked over time to monitor progress and identify areas needing improvement.
Q 6. Explain your understanding of risk stratification and its application in population health.
Risk stratification is the process of classifying individuals within a population based on their likelihood of experiencing a specific adverse health event. It’s a crucial component of population health management as it allows for targeted interventions to those most in need. We use various data points, including demographic information, medical history, lifestyle factors, and social determinants of health, to create a risk score for each individual. This score determines their placement within risk strata, ranging from low to high risk. For example, individuals with multiple chronic conditions, poor medication adherence, and limited access to healthy food would receive a higher risk score than those with no chronic conditions and good access to resources.
In practice, risk stratification allows for the efficient allocation of resources. High-risk individuals may receive more intensive interventions, including frequent check-ups, care coordination, and personalized support, while lower-risk individuals may receive more preventive care and educational programs. This targeted approach maximizes the impact of resources and improves overall population health outcomes. This is often used to prioritize outreach, targeted interventions, and potentially allocate greater resources where they can have the greatest impact.
Q 7. How do you utilize predictive modeling in population health management?
Predictive modeling plays a vital role in population health management by enabling proactive identification of at-risk individuals. We leverage historical data (e.g., EHRs, claims data, SDOH data) to build statistical models that predict the probability of future health events. Common techniques include regression analysis, machine learning algorithms (like logistic regression, random forests, or support vector machines), and survival analysis. These models can predict things such as:
- Hospital readmission risk: Identifying patients likely to be readmitted after discharge.
- Disease progression: Predicting the likelihood of developing a specific condition (e.g., diabetes, heart failure).
- Emergency department visits: Identifying patients at high risk of needing emergency care.
The predictions generated by these models inform targeted interventions. For instance, patients with high predicted risk of readmission might receive enhanced discharge planning, home health visits, or close follow-up by a care manager. It is crucial to remember that predictive models are tools to assist clinical judgment, not replace it. The output should always be interpreted in the context of the individual patient’s circumstances and clinical presentation.
For example, a model predicting hospital readmissions might consider factors such as age, number of chronic conditions, medication adherence, and social determinants of health. The model would then assign a probability score indicating the likelihood of readmission, allowing for proactive intervention based on risk level.
Q 8. Describe your experience with different data sources used in population health analytics (e.g., EHR, claims data).
My experience with population health analytics spans a wide range of data sources, each offering unique insights. Electronic Health Records (EHRs) are crucial, providing detailed patient-level information like diagnoses, medications, lab results, and vital signs. Think of EHRs as a comprehensive patient story, detailing their healthcare journey. Claims data, on the other hand, offers a broader perspective, reflecting healthcare utilization patterns – which services were used, how often, and by whom. This allows us to identify trends and patterns across larger populations. For instance, we can track the prevalence of a specific disease or the effectiveness of a treatment plan using claims data across many patients. I’ve also worked extensively with pharmacy data to understand medication adherence and potential drug interactions, and with public health registries to access information on disease outbreaks and vaccination rates. Combining these diverse data sources paints a more holistic picture of population health than any single source could provide alone. For example, integrating EHR data on individual patient outcomes with claims data on treatment costs allows us to assess the value and cost-effectiveness of different interventions.
Q 9. How do you ensure data accuracy and reliability in population health analysis?
Ensuring data accuracy and reliability is paramount in population health analysis. It’s like building a house – a shaky foundation leads to a collapsing structure. My approach is multi-faceted. First, rigorous data validation and cleaning are essential. This involves identifying and correcting errors, inconsistencies, and missing data. Techniques like data profiling and anomaly detection help flag potential issues. Second, data standardization and harmonization are critical. Different data sources use different coding systems and terminologies. Mapping these inconsistencies to a common standard is essential for accurate analysis. Finally, robust quality control measures throughout the analytical process are needed. This includes regular checks on data integrity and consistency, and the use of appropriate statistical methods to account for data limitations. For example, we might use weighted averages to account for potential biases in sampling or employ techniques like multiple imputation to address missing data. Regular audits are also key to verifying the quality of the data and the reliability of the analytical process.
Q 10. What are the ethical considerations when working with patient data in a population health setting?
Ethical considerations are fundamental when working with patient data. Privacy and confidentiality are paramount. We must strictly adhere to regulations like HIPAA in the US, or GDPR in Europe. This includes de-identification of data wherever possible, ensuring no individual can be identified from the aggregated analysis. Data security is also crucial, implementing robust measures to protect data from unauthorized access, use, or disclosure. Transparency is equally important. Stakeholders must understand how the data is being used, ensuring informed consent where applicable. Finally, addressing potential biases in the data is essential to avoid perpetuating health disparities. For instance, we must be aware of and mitigate potential biases related to race, ethnicity, socioeconomic status, or other demographic factors when interpreting results and designing interventions.
Q 11. How do you communicate complex population health data to various stakeholders (e.g., clinicians, administrators)?
Communicating complex population health data effectively requires tailoring the message to the audience. Clinicians need detailed, actionable information about specific patients or patient groups. I typically present this using concise reports focusing on key performance indicators (KPIs) relevant to their practice. Administrators, however, need a broader overview, focusing on cost-effectiveness, resource allocation, and strategic planning. Data visualization is key here. Interactive dashboards, clear charts, and concise summaries are crucial. For example, using heatmaps to visualize geographic variations in disease prevalence, or line graphs to track trends over time. I also use plain language, avoiding technical jargon whenever possible. A good analogy might be explaining the complexity of a machine to a mechanic versus explaining the same machine to a client – different levels of detail and language are needed.
Q 12. Describe your experience with developing and implementing population health interventions.
I have extensive experience in developing and implementing population health interventions. This usually involves a structured process: needs assessment to identify key health problems; identifying appropriate evidence-based interventions; designing feasible interventions for a specific population; implementation and process monitoring to ensure proper implementation; and continuous evaluation and adjustments throughout the process. For example, I worked on a project to reduce hospital readmissions for heart failure patients. We developed a comprehensive intervention incorporating telehealth monitoring, patient education programs, and enhanced care coordination. This involved identifying high-risk patients through data analysis, creating personalized intervention plans, and tracking outcomes to ensure the intervention was effective. The entire process demands strong interdisciplinary collaboration, involving clinicians, nurses, social workers, and administrative staff. Success depends on the engagement of patients and the efficient use of available resources.
Q 13. How do you measure the effectiveness of population health interventions?
Measuring the effectiveness of population health interventions requires carefully defined metrics and a robust evaluation plan. This typically involves comparing outcomes before and after the intervention, using statistical methods to assess the significance of observed changes. Key performance indicators (KPIs) might include changes in disease prevalence, hospitalization rates, mortality rates, or patient satisfaction. For example, to assess the effectiveness of our heart failure readmission reduction program, we compared readmission rates for intervention and control groups. We also used statistical techniques to control for confounding factors, such as patient age and severity of illness. Furthermore, process evaluation is essential to assess the fidelity of implementation. Did the intervention reach its intended target population? Were the intervention components implemented as planned? A combination of quantitative and qualitative data – such as patient feedback – is often used to gain a holistic understanding of the intervention’s effectiveness.
Q 14. What is your experience with value-based care models and their impact on population health?
Value-based care (VBC) models fundamentally shift the focus from volume to value in healthcare. Instead of being reimbursed for the number of services provided, providers are rewarded for achieving improved patient outcomes and reducing costs. This aligns perfectly with population health management. My experience shows that VBC models incentivize investments in proactive, preventative care, leading to better population health outcomes. For example, working in a VBC environment, I helped develop a program to improve diabetes management in a specific population. This involved providing enhanced care coordination, patient education, and remote monitoring. By improving patient outcomes and reducing hospitalizations, we demonstrated the cost-effectiveness of our approach, exceeding the targets set by the VBC contract. This highlights the interconnectedness between population health initiatives and achieving financial success within VBC frameworks. The success relies on effective data-driven strategies, robust data analytics to monitor progress, and a strong commitment to collaborative care.
Q 15. How do you handle challenges related to data integration and interoperability in population health?
Data integration and interoperability are paramount in population health. Imagine trying to build a house with mismatched bricks – it wouldn’t stand! Similarly, fragmented health data across different systems (electronic health records, claims databases, wearable devices) hinders effective population health management. We tackle this challenge through several strategies:
- Standardized Data Formats: Employing standards like HL7 FHIR allows different systems to communicate seamlessly, reducing data transformation efforts. For example, using FHIR allows us to easily share patient allergy information between an EHR and a pharmacy system.
- Data Warehousing and Integration Platforms: Centralizing data into a data warehouse provides a single source of truth. This often requires ETL (Extract, Transform, Load) processes to cleanse, standardize, and integrate data from various sources. We utilize cloud-based solutions for scalability and data security.
- Master Patient Index (MPI): A robust MPI is crucial for accurately identifying and linking patient records across different systems. Without a reliable MPI, we risk duplicate records and inaccurate population analysis. We regularly audit and reconcile our MPI to maintain data integrity.
- Data Governance Framework: This is crucial for ensuring data quality, security, and ethical use. We establish clear data ownership, access controls, and protocols to safeguard patient information while facilitating data sharing for approved purposes. This involves regular data quality checks and audits.
By implementing these strategies, we ensure data consistency, accuracy, and accessibility, leading to more effective population health programs.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of healthcare regulations and their relevance to population health data.
Healthcare regulations, like HIPAA in the US and GDPR in Europe, are fundamental to population health. They establish standards for patient privacy, data security, and the ethical use of health information. These regulations are not just compliance requirements; they are essential for building trust and ensuring responsible data handling.
- HIPAA (Health Insurance Portability and Accountability Act): This governs the privacy and security of Protected Health Information (PHI) in the US. We adhere to HIPAA’s strict rules regarding data access, storage, and transmission. This involves implementing robust security measures, such as encryption and access controls.
- GDPR (General Data Protection Regulation): This applies in Europe and emphasizes individual data rights. It demands transparency, informed consent, and the ability for individuals to access, correct, or delete their data. We apply similar principles globally, prioritizing patient autonomy.
- State and Local Regulations: There are also state and local regulations influencing data handling. For example, specific regulations might dictate how certain types of sensitive data are handled or reported. We must stay abreast of any relevant laws and regulations.
Ignoring these regulations poses significant legal and ethical risks. By incorporating these requirements into our operational procedures and technology infrastructure, we ensure the responsible and ethical use of data for population health initiatives.
Q 17. How do you leverage technology to improve population health outcomes?
Technology is transformative in population health. We leverage various tools to enhance outcomes:
- Predictive Modeling: Using machine learning, we identify individuals at high risk for specific conditions (e.g., diabetes, heart disease). This enables proactive interventions and resource allocation.
- Electronic Health Records (EHR) Integration: Accessing patient data from EHRs through APIs allows for comprehensive population health assessments. This makes it possible to identify trends and gaps in care.
- Population Health Management Platforms: These platforms offer tools for data analysis, care coordination, and reporting. This helps us track key metrics and measure the effectiveness of our programs.
- Wearable Technology and Remote Monitoring: Integrating data from wearable devices provides real-time insights into patient health. This facilitates timely interventions and personalized care.
- Telehealth: Facilitates remote consultations, reducing barriers to care and improving access, particularly for underserved populations.
These technologies enable data-driven decision-making, leading to improved health outcomes, reduced costs, and a more personalized approach to care.
Q 18. Describe your experience with building dashboards and reports for population health monitoring.
I have extensive experience in developing dashboards and reports for population health monitoring. We utilize business intelligence tools (e.g., Tableau, Power BI) to visualize key metrics, such as:
- Prevalence of chronic conditions: Showing the number of patients with diabetes, hypertension, etc., within a defined population.
- Readmission rates: Tracking hospital readmission rates after specific procedures to identify areas for improvement.
- Utilization of healthcare services: Analyzing patterns in doctor visits, emergency room visits, and hospitalizations to understand care patterns.
- Medication adherence: Monitoring medication adherence rates to improve treatment outcomes and reduce adverse events.
- Cost of care: Tracking the cost of care for specific populations to identify areas for cost reduction.
Dashboards are designed to be interactive and user-friendly, allowing stakeholders to easily understand trends and identify areas requiring attention. We use data visualization techniques to effectively communicate complex information, ensuring that insights are readily actionable.
Q 19. How do you prioritize interventions based on cost-effectiveness and impact?
Prioritizing interventions requires a systematic approach. We use a framework that considers both cost-effectiveness and potential impact. We assess interventions based on:
- Population Impact: How many people will benefit from the intervention? We use epidemiological data to estimate the potential reach and effectiveness of each intervention.
- Cost per Outcome: How much will it cost to achieve a specific outcome? This requires careful costing of resources (personnel, technology, materials).
- Feasibility: Is it realistic to implement the intervention given available resources and infrastructure? We consider practical limitations in implementation.
- Equity: Does the intervention address health disparities and promote health equity? We consider the distribution of benefits across the population.
We often use cost-effectiveness analysis to compare different interventions and identify the most efficient use of resources. For example, we might compare the cost-effectiveness of a diabetes prevention program versus a program focusing on managing existing diabetes complications. This allows us to maximize the overall impact of our interventions.
Q 20. What is your experience with different care coordination models?
My experience spans various care coordination models, each with its strengths and limitations:
- Accountable Care Organizations (ACOs): These groups of providers share responsibility for the care of a defined population. I’ve worked with ACOs to improve care coordination, reduce costs, and enhance quality measures.
- Patient-Centered Medical Homes (PCMHs): These provide comprehensive, coordinated care to patients with a focus on prevention and chronic disease management. I’ve supported PCMHs through data analysis and the development of clinical guidelines.
- Value-Based Care (VBC): This payment model rewards providers for delivering high-quality, cost-effective care. I’ve helped design and implement VBC programs by analyzing performance data and providing feedback to providers.
- Disease Management Programs: These focus on managing specific chronic conditions, such as diabetes or heart failure. I’ve developed and implemented disease management programs based on population needs and evidence-based guidelines.
The best model depends on the specific needs of the population and available resources. I assess the strengths and weaknesses of different models and tailor them to the context.
Q 21. Describe a situation where you had to overcome a data quality challenge in population health.
In a previous role, we faced significant challenges with inconsistent data regarding medication adherence. We were using data from multiple sources (pharmacy claims, patient self-reporting, EHRs), and the data often conflicted. This made it difficult to get an accurate picture of medication adherence and hindered our efforts to improve patient outcomes.
To overcome this challenge, we implemented a multi-pronged strategy:
- Data Reconciliation: We systematically compared data from different sources, identifying and resolving discrepancies whenever possible. This was a manual, time-consuming process, but crucial for building confidence in the data.
- Data Cleaning and Standardization: We developed a standardized data format for medication adherence, including clear definitions and coding conventions. This improved data consistency across sources.
- Data Validation: We implemented automated data validation checks to identify and flag inconsistencies in real-time. This reduced the manual effort required for data reconciliation.
- Improved Data Collection: We worked to improve data collection processes, ensuring more accurate and complete information on medication adherence. This included implementing better patient communication and feedback mechanisms.
By addressing data quality issues systematically and implementing improved data management practices, we were able to produce more reliable data, leading to more effective medication adherence interventions. This experience highlighted the importance of proactive data quality management in population health.
Q 22. How do you address biases in data analysis in a population health context?
Addressing biases in population health data analysis is crucial for equitable and effective interventions. Bias can creep in at various stages, from data collection to analysis and interpretation. We must actively mitigate these biases to ensure fairness and accuracy.
Strategies for addressing bias include:
- Careful Data Collection: Employing diverse data collection methods and ensuring representative sampling across all population subgroups. For instance, using multiple languages for surveys or conducting community outreach to engage hard-to-reach populations.
- Data Validation and Cleaning: Rigorously checking for missing data, outliers, and inconsistencies. Applying appropriate statistical techniques to handle missing data and identify potential sources of bias.
- Bias Detection Techniques: Using statistical methods to identify and quantify biases. For example, regression analysis can reveal disparities in outcomes across different demographic groups, and this can highlight potential biases in the data.
- Sensitivity Analysis: Performing multiple analyses using different assumptions and data subsets to assess the robustness of findings and their sensitivity to bias. This helps understand how susceptible results are to potential biases.
- Interdisciplinary Collaboration: Engaging community members, social scientists, and other stakeholders in the design and interpretation of analyses to ensure the perspectives of diverse groups are considered and biases are identified early.
- Transparency and Reporting: Clearly documenting the data collection and analysis methods, limitations, and potential biases in research reports and publications. This increases the transparency and accountability of the analysis.
For example, in a study examining the prevalence of diabetes, we might find that data from certain neighborhoods are missing, potentially due to lower participation rates in healthcare services. Ignoring this would lead to an underestimation of prevalence in those areas. By actively seeking data from these areas and applying suitable statistical techniques, we can produce a more accurate representation.
Q 23. Explain your understanding of the social determinants of health and their impact on population health.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. They encompass a broad spectrum of factors that influence an individual’s health, often beyond their control.
Key SDOH categories include:
- Economic Stability: Poverty, employment, food security, housing stability.
- Education Access and Quality: High school graduation rates, enrollment in higher education.
- Social and Community Context: Social cohesion, civic participation, discrimination, incarceration rates.
- Health Care Access and Quality: Health coverage, access to care, provider quality.
- Neighborhood and Built Environment: Access to healthy food, quality of housing, crime and violence, environmental conditions.
Impact on Population Health: SDOH significantly influence population health outcomes. For instance, individuals living in poverty may experience higher rates of chronic diseases due to limited access to nutritious food, healthcare, and safe housing. Similarly, lack of educational opportunities can lead to lower-paying jobs, increasing stress and impacting mental and physical health. Addressing these upstream determinants is critical to improve overall population health.
Imagine a community with high rates of asthma. While medication can treat the illness, the underlying SDOH, like air quality and access to healthcare, must be tackled to effectively manage this population’s health. A program focusing solely on medication distribution, neglecting factors like pollution control and accessible healthcare, would be incomplete and less effective.
Q 24. How do you collaborate with different departments to achieve population health goals?
Collaboration is paramount in population health management. Effective population health initiatives require integrated efforts across multiple departments. My approach involves building strong working relationships and fostering open communication.
Effective collaboration strategies include:
- Joint Goal Setting: Working with departments (e.g., clinical care, community outreach, social services, public health) to establish shared goals and a unified strategy. This ensures alignment and avoids conflicting priorities. For instance, we would work collaboratively to set goals for diabetes management, with clinical care focusing on treatments, and community outreach aiming at education.
- Data Sharing and Integration: Facilitating the secure sharing of relevant data across departments to provide a holistic view of patient health. This may involve utilizing health information exchange platforms and implementing robust data governance practices to protect privacy while maximizing information flow. For example, sharing patient health records between primary care physicians and specialists.
- Cross-Departmental Teams: Forming multidisciplinary teams consisting of representatives from different departments to tackle specific population health challenges. This provides diverse expertise and perspectives to the problem-solving process.
- Regular Communication and Meetings: Holding regular meetings to discuss progress, challenges, and strategic adjustments. Adopting a clear communication plan ensures everyone is updated and informed about crucial issues.
- Conflict Resolution Mechanisms: Establishing clear processes for resolving disagreements and ensuring a collaborative environment. This might involve mediation or developing protocols for decision-making.
For instance, in addressing childhood obesity, collaboration with schools (nutrition programs), social services (family support), and community organizations (recreational activities) is essential for a comprehensive and sustainable impact.
Q 25. What are some emerging trends in population health management?
The field of population health management is constantly evolving. Several emerging trends are shaping the future.
Key emerging trends include:
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML are being increasingly applied to analyze large datasets, predict health risks, and personalize interventions. This allows for more targeted and effective population health management. For example, predictive modeling for identifying individuals at high risk of developing heart disease.
- Value-Based Care: A shift towards paying healthcare providers based on the quality and outcomes of care rather than the volume of services provided. This encourages a focus on preventative care and population health. This model incentivizes improvements in overall population health.
- Precision Medicine: Tailoring medical treatments to individual characteristics and genetic makeup. This allows for more personalized interventions and improved health outcomes. For example, providing genetic testing to predict the risk of certain diseases.
- Wearable Technology and Remote Monitoring: Utilizing wearable sensors and remote monitoring tools to collect health data and track patient progress, allowing for timely interventions and improved patient engagement. Real-time data can support early interventions.
- Increased Focus on Social Determinants of Health: Growing recognition of the impact of SDOH on population health, leading to integrated programs addressing both medical and social needs. For instance, community-based programs that tackle food insecurity and housing issues.
Q 26. Describe your experience with population health program evaluation.
Evaluating population health programs requires a multifaceted approach to assess their effectiveness and impact. It involves a systematic process to collect, analyze and interpret data to determine the success of a program.
My approach to program evaluation incorporates:
- Clearly Defined Objectives and Metrics: Establish clear objectives and measurable outcomes at the beginning of the program to ensure success can be objectively defined. This ensures that the program’s success can be measured against pre-defined goals.
- Data Collection Methods: Utilizing various data sources, including administrative claims data, surveys, patient feedback, and clinical data, to gather a comprehensive view of the program’s impact. This helps get a complete picture of impact.
- Statistical Analysis: Employing statistical techniques such as regression analysis, time-series analysis, and other appropriate methods to analyze data and determine the program’s effectiveness. These tests provide statistical confidence to the conclusions.
- Qualitative Data Analysis: Incorporating qualitative methods, such as interviews and focus groups, to capture patient experiences and perspectives. This informs deeper understanding beyond numerical data.
- Cost-Effectiveness Analysis: Assessing the cost-effectiveness of the program to determine the return on investment and sustainability. This helps to determine efficiency of resource use.
- Dissemination of Findings: Sharing the evaluation findings with stakeholders to inform program improvements and future initiatives. This enables informed decision-making on program continuation and modifications.
In a recent project evaluating a diabetes prevention program, we used a combination of health records to track improvements in HbA1c levels (a key indicator of diabetes control), and patient surveys to assess satisfaction and adherence to the program’s lifestyle modifications. This provided a rich and comprehensive picture of program effectiveness.
Q 27. How do you stay current with best practices in population health management?
Staying current in population health management is crucial. I employ a multi-pronged approach to maintain my expertise.
My strategies for continuous learning include:
- Professional Organizations: Active membership in professional organizations such as the American Public Health Association (APHA) and the National Association of County and City Health Officials (NACCHO) provides access to research, publications, and networking opportunities. This keeps me updated on policy and best practices.
- Peer-Reviewed Publications: Regularly reviewing peer-reviewed journals and research articles on population health management to stay updated on the latest findings and advancements. This deepens my understanding of current research.
- Conferences and Workshops: Attending conferences and workshops to learn from leading experts and network with peers. This provides exposure to innovative techniques and diverse perspectives.
- Online Courses and Webinars: Engaging in online courses and webinars offered by reputable institutions to enhance my skills and knowledge in specific areas. This offers flexibility and accessibility to ongoing training.
- Mentorship and Collaboration: Seeking mentorship from experienced professionals and engaging in collaborative projects to learn from different perspectives and experiences. This provides opportunities to learn from experts.
- Monitoring Health Policy Changes: Staying abreast of changes in healthcare policy and regulations relevant to population health management. This provides a broader understanding of the context within which the work is being done.
Key Topics to Learn for PopulationCentric Operations Interview
- Population Data Analysis: Understanding and interpreting demographic data, including population size, distribution, density, and growth rates. Practical application: Analyzing census data to inform resource allocation strategies.
- Spatial Analysis Techniques: Utilizing Geographic Information Systems (GIS) and other spatial tools to visualize and analyze population data. Practical application: Mapping population vulnerabilities to natural disasters for effective disaster preparedness.
- Population Modeling and Forecasting: Developing and applying models to predict future population trends and their implications. Practical application: Projecting future healthcare needs based on aging population trends.
- Resource Allocation and Optimization: Strategically allocating resources based on population needs and distribution. Practical application: Optimizing the location of healthcare facilities to improve accessibility.
- Data Visualization and Communication: Effectively presenting population data and analysis findings to diverse audiences. Practical application: Creating compelling infographics to communicate complex population trends to policymakers.
- Ethical Considerations in Population Data: Understanding and addressing privacy concerns and potential biases in population data. Practical application: Ensuring data security and responsible data handling practices.
- Policy and Program Evaluation: Assessing the effectiveness of population-related policies and programs. Practical application: Evaluating the impact of a public health initiative on a specific population group.
Next Steps
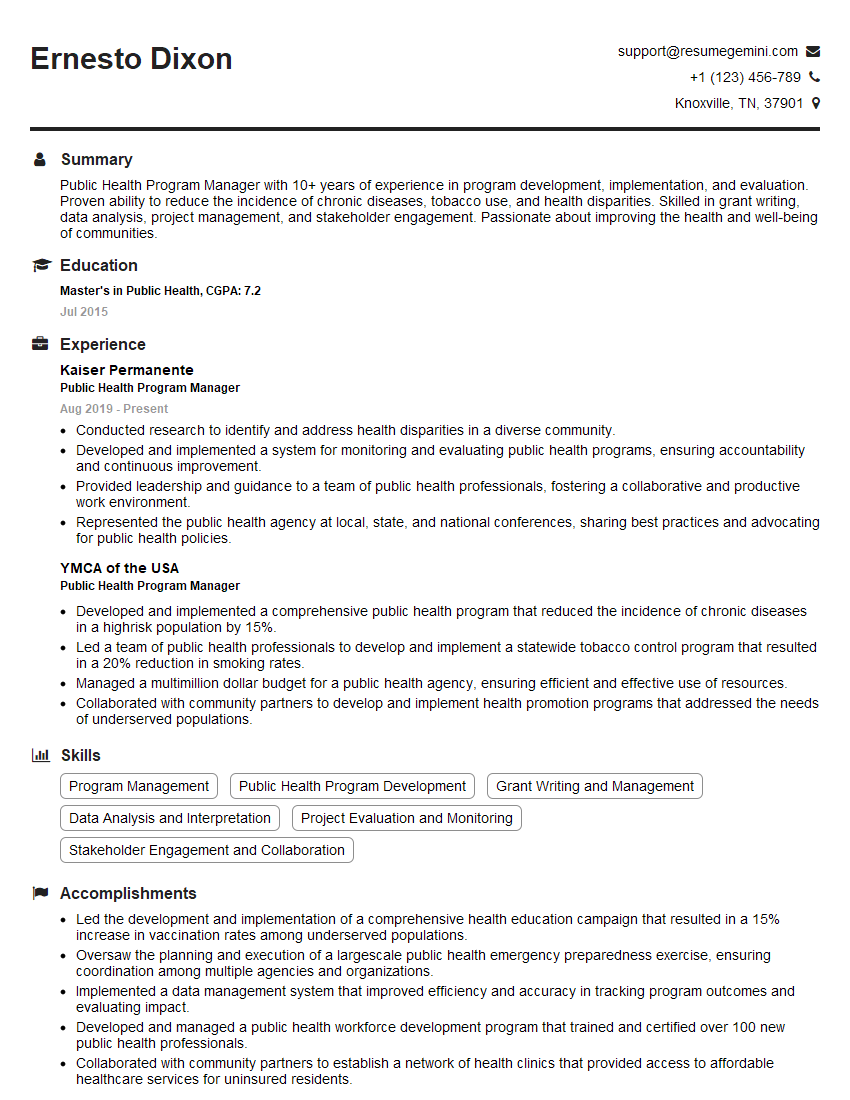
Mastering PopulationCentric Operations is crucial for a successful and impactful career in fields like public health, urban planning, and social services. A strong understanding of these concepts will significantly enhance your problem-solving abilities and strategic thinking, making you a highly valuable asset to any organization. To maximize your job prospects, creating a compelling and ATS-friendly resume is essential. We highly recommend leveraging ResumeGemini, a trusted resource, to build a professional and effective resume that highlights your skills and experience. Examples of resumes tailored to PopulationCentric Operations are available to help guide you in this process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good