The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Speech and Language Pathology interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Speech and Language Pathology Interview
Q 1. Explain the difference between articulation and phonological disorders.
Both articulation and phonological disorders affect speech sound production, but they differ significantly in their underlying causes. Articulation disorders involve difficulties producing specific speech sounds due to motor challenges—problems with the physical movements of the tongue, lips, and jaw. Think of it like a malfunctioning instrument; the notes (sounds) are known, but the mechanism to play them is impaired. For example, a child might consistently substitute a /w/ for an /r/, producing “wabbit” instead of “rabbit.” This is a motor-based difficulty.
Phonological disorders, on the other hand, are rooted in the child’s understanding of the sound system (phonology) of their language. They might have trouble organizing sounds into patterns, resulting in consistent sound errors across multiple sounds. It’s like having the notes but lacking the musical knowledge to create a coherent melody. A child with a phonological disorder might simplify their speech, leaving out consonant clusters or using a single sound to replace many sounds, such as using /t/ for /k/, /g/, and /tʃ/. The key difference lies in whether the problem is motor execution or linguistic organization.
Q 2. Describe the assessment process for childhood apraxia of speech.
Assessing childhood apraxia of speech (CAS) requires a comprehensive approach involving multiple professionals. It’s crucial to rule out other disorders first. The process typically begins with a detailed case history, including developmental milestones and family history.
Assessment components may include:
- Oral-motor examination: Assessing the structure and function of the oral-motor mechanism to identify any anatomical limitations.
- Speech sound assessment: Evaluating the child’s ability to produce different sounds in various contexts—single words, sentences, spontaneous speech—to pinpoint patterns of errors.
- Language assessment: Determining the child’s receptive and expressive language abilities as CAS can coexist with other language disorders.
- Play-based assessment: Observing the child’s speech production during spontaneous play activities, as this can reveal more natural speech patterns.
- Dynamic assessment: Providing support and observing how the child responds to cues and strategies to gauge their learning potential.
Standardized tests might be used, but careful observation and analysis of speech samples during interaction are paramount. There isn’t one single definitive test for CAS; the diagnosis relies on a clinical judgment based on the constellation of findings.
Q 3. How do you differentiate between fluency disorders like stuttering and cluttering?
Both stuttering and cluttering are fluency disorders, but they present differently. Stuttering is characterized by disruptions in the flow of speech, including repetitions of sounds, syllables, or words; prolongations of sounds; and blocks (interruptions of airflow). It often involves secondary behaviors such as eye blinks or head movements. The speaker is usually aware of their disfluencies and experiences tension and anxiety.
Cluttering is a faster-than-normal rate of speech often combined with other characteristics such as disorganized syntax (sentence structure), imprecise articulation, and frequent interruptions. Unlike stuttering, individuals who clutter might not be fully aware of their disfluency and often have more difficulty with planning and organizing their utterances. Cluttering also tends to be associated with less tension than stuttering.
In short: Stuttering is marked by repetitions and blocks, often with accompanying anxiety, while cluttering involves a rapid, disorganized, and less-precise speech flow with less awareness on the part of the speaker.
Q 4. What are the common causes of dysphagia in adults?
Dysphagia in adults has multiple potential causes, often interconnected:
- Neurological conditions: Stroke, Parkinson’s disease, multiple sclerosis, and traumatic brain injury are frequent culprits, impacting the neural control of swallowing muscles.
- Structural abnormalities: Head and neck cancers, anatomical variations, and prior surgeries (e.g., neck surgery) can physically impede swallowing.
- Degenerative diseases: Conditions like Alzheimer’s disease and dementia can gradually impair swallowing mechanisms due to cognitive decline.
- Medications: Certain drugs can have side effects that lead to dry mouth, muscle weakness, or other swallowing difficulties.
- Other medical conditions: Conditions like gastroesophageal reflux disease (GERD), infections, and neuromuscular disorders can also contribute to dysphagia.
Understanding the underlying medical condition is key to effective treatment planning for dysphagia.
Q 5. Outline the stages of swallowing and how to assess each stage.
Swallowing (deglutition) is a complex process involving four main stages:
- Oral preparatory phase: Food is manipulated in the mouth, chewed, mixed with saliva, and formed into a bolus (a cohesive mass). Assessment involves observing bolus formation, lip closure, tongue movement, and mastication (chewing) efficiency.
- Oral phase: The bolus is propelled posteriorly (back) into the pharynx (throat) by the tongue. Assessment focuses on tongue movement, strength, and timing of the bolus transit.
- Pharyngeal phase: This is a rapid, involuntary sequence of events. The soft palate elevates to prevent nasal regurgitation, the larynx elevates and the epiglottis inverts to protect the airway, and the pharyngeal constrictors propel the bolus down into the esophagus. Assessment relies on observing laryngeal elevation, pharyngeal contraction, and airway protection using videofluoroscopy (modified barium swallow study).
- Esophageal phase: The bolus is transported through the esophagus to the stomach. This phase is usually assessed with endoscopy or esophageal manometry.
Assessment methods include clinical bedside evaluations, videofluoroscopy (VFSS), fiberoptic endoscopic evaluation of swallowing (FEES), and manometry.
Q 6. What are the different types of augmentative and alternative communication (AAC) systems?
Augmentative and alternative communication (AAC) systems encompass a wide range of options to support individuals who cannot rely solely on spoken language. They can be broadly categorized as:
- No-tech AAC: These systems don’t require any electronic devices. Examples include picture cards, communication boards, real objects, and gestures. They are simple, accessible, and cost-effective.
- Low-tech AAC: These use simple technology such as picture exchange systems (PECS), where individuals exchange pictures to communicate. They are generally portable and user-friendly.
- High-tech AAC: These involve sophisticated electronic devices, such as speech-generating devices (SGDs) with synthesized speech or digitized recordings. These can offer a vast vocabulary, flexibility, and customized features.
The choice of AAC system depends on individual needs, cognitive abilities, physical limitations, and available resources.
Q 7. Explain your experience with using various AAC systems.
Throughout my career, I’ve had extensive experience with various AAC systems. I’ve worked with children using PECS to improve their communication skills and have aided adults with complex communication needs by selecting and programming high-tech SGDs. I’ve helped families choose appropriate no-tech options, such as communication boards tailored to the individual’s interests and environment.
For instance, I worked with a young boy with autism who initially struggled with communication. We implemented PECS, gradually increasing the complexity of the exchange system. His progress was remarkable, demonstrating the effectiveness of well-chosen low-tech AAC.
I also assisted an adult with aphasia after a stroke. Working closely with the patient and family, we selected and programmed a sophisticated SGD that provided both synthesized and digitized speech, allowing him to regain a significant level of communication. Proper training and ongoing support were crucial for success in this case. My approach prioritizes client-centered care, ensuring the AAC system chosen meets their unique needs and preferences.
Q 8. Describe your approach to therapy for a child with a language delay.
My approach to therapy for a child with a language delay is highly individualized and data-driven. It begins with a comprehensive assessment to pinpoint the specific areas of weakness. This might include receptive language (understanding what’s said), expressive language (speaking), phonology (sound production), pragmatics (social use of language), and morphology/syntax (grammar). Based on the assessment, I develop a personalized plan focusing on their strengths and targeting their weaknesses. I utilize a play-based approach, understanding that children learn best through engaging activities. For example, if a child struggles with verb tense, we might incorporate it into a storytelling activity where they manipulate toys to illustrate actions in different tenses. I believe in frequent progress monitoring and adjusting the therapy plan as needed. Regular communication with parents and caregivers is crucial to ensure consistency and support across different settings.
For instance, I worked with a child who had difficulty with expressive language. Through play therapy involving puppets, we gradually built his vocabulary and sentence structures. We began with simple sentences and gradually increased complexity, always maintaining a fun and interactive learning environment. We also incorporated activities that required him to follow multi-step instructions, thereby working on his receptive language skills as well.
Q 9. How do you assess receptive and expressive language skills?
Assessing receptive and expressive language skills requires a multifaceted approach. For receptive language, I use standardized tests like the Peabody Picture Vocabulary Test (PPVT) or the Receptive One-Word Picture Vocabulary Test (ROWPVT), which assess a child’s understanding of vocabulary. I also use informal measures, such as following directions, answering questions, and responding to commands. For expressive language, I observe spontaneous speech samples, analyzing vocabulary, grammar, sentence structure, and fluency. Standardized tests like the Clinical Evaluation of Language Fundamentals (CELF) or the Expressive Vocabulary Test (EVT) provide a quantitative measure of expressive abilities. I also consider the child’s narrative skills, which involves assessing their ability to tell stories and describe events.
For example, during an assessment, I might ask a child to point to a picture of a specific object (receptive) or describe their favorite toy (expressive). Observation in natural settings, like during play or a conversation, provides rich qualitative data that complements standardized testing. A combination of both formal and informal measures allows for a more complete and accurate picture of a child’s language abilities.
Q 10. What are the key components of a comprehensive language assessment?
A comprehensive language assessment involves more than just testing receptive and expressive language. It needs to explore various aspects to gain a holistic understanding of the child’s communication skills. Key components include:
- Case History:Gathering information about the child’s developmental history, medical history, family history, and current educational performance. This gives vital context to the assessment.
- Oral-Motor Examination: Assessing the structure and function of the oral-motor mechanism – including tongue, lips, and palate – to rule out any physical limitations affecting speech production.
- Hearing Screening: Identifying any potential hearing loss that could contribute to language difficulties. A referral to an audiologist is necessary if a hearing impairment is suspected.
- Receptive Language Assessment: Evaluating comprehension skills through standardized tests and informal measures, as described earlier.
- Expressive Language Assessment: Evaluating verbal production skills, as described earlier.
- Pragmatic Language Assessment: Observing the child’s social use of language, including turn-taking, topic maintenance, and social appropriateness. This is often observed during play or conversational interactions.
- Cognitive Assessment: In some cases, assessing cognitive abilities to understand the relationship between cognitive skills and language development. This may involve tasks evaluating attention, memory, and problem-solving.
Integrating all this information provides a complete picture enabling effective therapy planning.
Q 11. Discuss your experience with implementing evidence-based practices in speech therapy.
Evidence-based practice is the cornerstone of my speech therapy approach. I regularly consult peer-reviewed journals and research databases to stay abreast of the latest findings and best practices. For example, I’ve implemented focused stimulation, a technique supported by extensive research, to enhance vocabulary acquisition in children with language delays. This method involves repeatedly presenting the target word within a meaningful context. Similarly, I’ve utilized the principles of milieu teaching, which integrates language therapy into the child’s natural environment using play and their interests, effectively maximizing engagement and learning. I meticulously document my client’s progress, employing standardized measures and collecting data to monitor the effectiveness of my interventions. This data informs adjustments to the therapy plan, ensuring I’m using evidence-based methods that are producing the best results for each individual.
I regularly attend professional development workshops and conferences to update my knowledge of new evidence-based interventions and refine my skills.
Q 12. Describe your experience working with individuals with traumatic brain injury.
My experience with individuals with traumatic brain injury (TBI) has involved a variety of challenges and rewarding outcomes. The severity of the injury significantly impacts the nature of the communication deficits encountered. These can range from mild aphasia (difficulty with language processing) to significant impairments in all aspects of communication, including speech, swallowing, and cognitive functions. My approach involves a thorough assessment of the individual’s cognitive abilities, including attention, memory, and executive functions. I collaborate closely with other healthcare professionals, such as neuropsychologists and occupational therapists, to develop a holistic treatment plan. Therapy often focuses on improving functional communication skills, such as initiating conversations, expressing needs, and understanding instructions. I adapt my therapy techniques based on the individual’s cognitive capacity and level of fatigue, ensuring sessions are manageable and productive. In some cases, I also utilize augmentative and alternative communication (AAC) systems to help individuals communicate when verbal speech is severely impaired.
I remember one client who experienced significant aphasia after a TBI. Through intensive therapy focusing on verbal cuing and gradually increasing sentence complexity, he was able to slowly regain his expressive language abilities. The progress was gradual but immensely rewarding for both him and me.
Q 13. How do you adapt your therapy approach to meet the diverse needs of your clients?
Adapting my therapy approach to meet diverse client needs is essential. This involves considering factors such as age, cultural background, learning style, and cognitive abilities. I prioritize building rapport and creating a safe and comfortable therapeutic environment for each client. For children, I use a play-based approach, tailoring activities to their interests and developmental levels. For adults, I may focus on more structured therapy addressing specific communication needs in their workplace or daily life. I’m aware of cultural differences in communication styles and incorporate culturally relevant materials and techniques into my sessions. I collaborate with interpreters when needed and actively seek information about a client’s cultural and linguistic background.
I also utilize different therapeutic approaches depending on the client’s learning style. Some clients respond better to visual aids, while others benefit from hands-on activities. Regularly evaluating therapy efficacy and adapting techniques based on progress and feedback is key to personalized care.
Q 14. Explain your understanding of the principles of motor learning in speech therapy.
Motor learning principles are crucial in speech therapy, particularly for articulation disorders and fluency disorders. Motor learning refers to the process of acquiring and refining motor skills through practice and feedback. Three key principles guide my approach: practice, feedback, and task specificity.
- Practice: Repetitive practice of the target speech sounds or motor patterns is essential for strengthening the neural pathways responsible for producing those movements. I structure practice sessions to optimize learning by using techniques like spaced retrieval and massed practice, varying the context and difficulty level of practice activities.
- Feedback: Providing immediate and informative feedback is crucial. This helps the client understand where they need to improve and refine their motor performance. Feedback can be auditory (listening to their speech), visual (watching themselves in a mirror), or kinesthetic (feeling the movements in their mouth). I adapt the type and frequency of feedback based on the client’s learning style and progress.
- Task Specificity: The practice activities should be relevant and directly related to the client’s communication goals. If a client struggles with /s/ sounds, I wouldn’t focus on unrelated movements; instead, I would select tasks specifically focusing on producing /s/ in different words and contexts.
Applying these principles ensures that therapy is not simply about repetition, but about structured practice leading to improved motor control and efficient speech production.
Q 15. Describe your experience with conducting functional communication assessments.
Functional communication assessments are crucial for understanding how a client uses communication in their daily lives. Instead of just focusing on isolated skills, we assess how communication impacts their ability to participate in activities and achieve their goals. For example, we wouldn’t just test articulation; we’d observe how their speech difficulties affect their interactions during mealtimes or requesting help.
My approach involves a combination of methods. I start with direct observation in natural settings, like the child’s classroom or home, to understand their communication in context. I’ll then use standardized tests to assess specific skills (e.g., receptive and expressive language), supplemented by informal assessments tailored to the individual’s needs. These informal assessments might include play-based activities, structured tasks, or analyzing samples of their communication to understand the ‘function’ of their communication behaviors (e.g., attention-seeking, requesting, protesting). For instance, I might observe a child repeatedly hitting to get a toy, demonstrating the functional communication of obtaining a desired object. Following this, I develop targeted interventions to address the identified needs and improve functional communication.
I always involve caregivers in the process, gaining their perspective on the client’s communication in everyday life. This collaborative approach yields a comprehensive understanding, leading to more effective and personalized intervention plans.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you collaborate with other professionals (e.g., teachers, doctors) in a multidisciplinary team?
Collaboration is essential for optimal client outcomes. I regularly communicate with teachers, doctors, and other therapists, sharing information and coordinating our efforts. For example, with a child struggling with articulation and attention, I’d work closely with their teacher to implement strategies in the classroom that support both goals. We might use consistent terminology and strategies across settings, like using visual supports to aid communication and attention regulation. I’d also communicate with the doctor regarding any medical conditions that may impact speech and language development, ensuring the therapy aligns with the child’s overall health plan. Regular meetings with the multidisciplinary team allow us to efficiently share updates, adjust interventions as needed, and ensure a holistic approach to the client’s care.
I use various communication methods—formal meetings, informal email exchanges, progress reports—to keep everyone informed and engaged. This ensures everyone is on the same page and working towards the same goals for the client.
Q 17. What are your strategies for managing challenging behaviors in therapy sessions?
Managing challenging behaviors requires a thorough functional behavioral assessment (FBA) to understand the underlying cause of the behavior. It’s not about suppressing the behavior, but identifying its purpose and teaching more appropriate communication strategies. For example, if a child is hitting to get attention, we’d work on teaching alternative ways to communicate their needs, like using words or gestures. The FBA process usually involves gathering information through observation, interviews, and reviewing records. It helps determine the antecedents (what triggers the behavior), the behavior itself, and the consequences (what maintains the behavior).
My strategies involve positive behavior support (PBS), focusing on proactive strategies to prevent challenging behaviors. This might involve creating a structured and predictable therapy environment, incorporating preferred activities, and providing clear expectations. If a challenging behavior occurs, I use consistent and predictable consequences, but primarily focus on reinforcing appropriate behaviors using positive reinforcement techniques. I always tailor my approach to the individual client’s needs and involve their caregivers in the process to ensure consistency across settings.
Q 18. How do you document client progress and communicate with families?
Documentation is paramount for tracking progress and communicating effectively. I meticulously document each therapy session, including goals addressed, activities completed, client responses, and overall progress. This information forms the basis for progress reports shared with families. These reports aren’t just summaries; they explain the client’s progress in clear, non-technical language, highlighting achievements and areas needing further attention. I use visuals, graphs and data to illustrate progress and make it more easily understood.
I regularly communicate with families through various means, such as phone calls, email, and face-to-face meetings. These interactions offer opportunities to discuss progress, address concerns, and collaboratively plan for continued support. Open communication builds trust and ensures that everyone is informed and involved in the therapeutic journey.
Q 19. Explain your experience with data collection and analysis in speech therapy.
Data collection and analysis are crucial for ensuring therapy effectiveness. I use a variety of methods to collect data, including direct observation, frequency counts, percentage data, duration recordings, and rating scales depending on the client’s needs and the specific goals we are targeting. For example, I might track the number of times a child uses a target sound correctly during a session or measure the duration of their fluent speech during a conversational activity. This data isn’t just collected; it’s analyzed regularly to evaluate the efficacy of the interventions.
I use graphs and charts to visualize the data, making it easy to see patterns and trends in the client’s progress. This data-driven approach helps me make informed decisions about modifying treatment plans, ensuring that they remain effective and tailored to the client’s ongoing needs. If progress plateaus, I analyze the data to identify potential barriers and adjust my strategies accordingly.
Q 20. Describe your experience with various assessment tools and instruments.
I have extensive experience with various assessment tools. For articulation, I use standardized tests like the Goldman-Fristoe Test of Articulation or the Khan-Lewis Phonological Analysis. For language assessment, I utilize tests like the Clinical Evaluation of Language Fundamentals (CELF) or the Preschool Language Scale (PLS). I also use informal assessments, which are tailored to the individual client’s needs and communication context. These might include analyzing language samples from play, conversation, or narrative tasks. My selection of assessment tools depends on the client’s age, suspected areas of difficulty, and communication needs. I always consider cultural and linguistic backgrounds when selecting and interpreting assessment results.
Beyond standardized tests, I utilize other instruments such as communication checklists and rating scales from caregivers or teachers to gain a holistic view of the client’s abilities.
Q 21. How do you maintain confidentiality and adhere to ethical standards?
Maintaining confidentiality and adhering to ethical standards are non-negotiable aspects of my practice. I strictly follow the American Speech-Language-Hearing Association (ASHA) Code of Ethics, ensuring client information remains protected. This includes securing client records, using passwords to protect electronic data, and only sharing information with authorized individuals (e.g., other members of the multidisciplinary team, caregivers with client consent). I always obtain informed consent from clients or their legal guardians before initiating any assessments or treatments, ensuring they understand the process and their rights.
If there are concerns about client safety or wellbeing, I would follow mandated reporting procedures as required by law and professional guidelines. Maintaining professional boundaries, avoiding conflicts of interest, and continuing my education to stay abreast of ethical guidelines are all parts of my commitment to ethical practice.
Q 22. How do you handle situations where a client is not making progress?
When a client isn’t progressing as expected, my first step is a thorough reassessment. This involves reviewing the initial assessment, current treatment goals, and the client’s overall performance. I analyze the data to pinpoint potential areas of difficulty. Is the therapy approach appropriate for the client’s learning style and cognitive abilities? Are the goals realistic and appropriately challenging? Are there any external factors impacting progress, such as stress, medical conditions, or lack of carryover practice at home?
For instance, if a child with phonological disorders isn’t improving articulation, I might analyze whether the targeted sounds are too complex, if the therapy techniques aren’t engaging enough, or if they are consistently practicing at home. I might adjust the therapy intensity, modify the approach by incorporating play-based activities or technological aids like apps, or consult with the parents or caregivers to ensure consistent home practice. Collaboration is key; I might involve the client’s teacher or other specialists, if appropriate.
If modifications to the treatment plan still don’t show improvement, I’d consider referring the client for a comprehensive medical evaluation to rule out any underlying medical issues affecting their progress. Ultimately, open communication with the client and their family, along with ongoing monitoring and flexible adaptation, are crucial for navigating these challenging situations.
Q 23. What are your professional development goals in speech-language pathology?
My professional development goals center around expanding my expertise in neurogenic communication disorders and incorporating technology effectively into my practice. I’m particularly interested in advanced techniques for treating aphasia and apraxia of speech following stroke or traumatic brain injury. This involves pursuing continuing education courses focusing on evidence-based therapeutic interventions, such as constraint-induced language therapy or melodic intonation therapy.
Furthermore, I aim to become proficient in utilizing telepractice technologies to improve client access to care and to integrate technology-assisted assessment and treatment methods. This includes mastering various teletherapy platforms and learning how to leverage digital tools for data collection, progress monitoring, and remote client engagement. This goal also includes staying current on the latest research and best practices in the field through attending conferences, joining professional organizations (like ASHA), and actively engaging with peer-reviewed literature.
Q 24. Explain your understanding of the impact of cultural and linguistic diversity on communication.
Cultural and linguistic diversity significantly impacts communication. Understanding this impact is crucial for providing culturally competent and effective speech-language therapy. A client’s cultural background influences their communication styles, non-verbal cues, and even their perceptions of health and illness. For example, some cultures may prioritize indirect communication, while others are more direct. Misinterpreting these differences can lead to inaccurate diagnoses and ineffective treatment.
Similarly, linguistic diversity plays a vital role. If a client is bilingual or multilingual, their language skills in each language might vary, influencing their communication abilities. A diagnosis of a communication disorder in one language doesn’t automatically translate to the same disorder in another. We must carefully assess their skills in all relevant languages and consider the potential impact of language interference or dominance. It’s essential to use culturally and linguistically sensitive assessment tools and treatment strategies, and ideally have access to interpreters or bilingual clinicians when necessary.
Ignoring these factors can lead to misdiagnosis, ineffective treatment, and even create barriers to accessing care. To counteract this, I strive to continually enhance my cultural awareness, understand different communication styles, and learn about the linguistic nuances of diverse populations.
Q 25. Describe your experience with different therapeutic approaches for voice disorders.
My experience encompasses various therapeutic approaches for voice disorders, tailored to the specific needs of each client. For example, I use Lee Silverman Voice Treatment (LSVT) LOUD for individuals with Parkinson’s disease, focusing on increasing vocal intensity and improving vocal clarity through intensive, high-intensity exercises. For patients with vocal nodules or polyps, I might employ techniques like vocal rest, hydration strategies, and modification of vocal habits, along with potential referral to an otolaryngologist.
In cases of muscle tension dysphonia (MTD), I utilize a combination of behavioral voice therapy which includes relaxation techniques, breath support exercises, and techniques to reduce vocal fold tension, combined with physiological voice therapy which might include laryngeal massage or manual therapy. Additionally, I’ve worked with clients on resonance therapy to improve the quality of their voice by modifying the way sound resonates in the vocal tract. The choice of approach always depends on the underlying cause and the specific characteristics of the voice disorder. A comprehensive assessment is paramount to guide my therapeutic decisions.
Q 26. How do you assess and manage voice disorders?
Assessing voice disorders involves a multi-faceted approach, combining perceptual judgments with objective measures. I begin with a thorough case history, inquiring about the onset and progression of symptoms, associated medical conditions, and the impact on the client’s quality of life. Next, I conduct a perceptual evaluation, assessing the patient’s voice quality, pitch, loudness, and breath support. This involves listening to their speech samples and observing their vocal behaviors.
Objective measures are also crucial. I utilize acoustic analysis, using software to measure parameters like fundamental frequency, jitter, and shimmer. I might also use videostroboscopy (a procedure using a scope to visualize the vocal folds during phonation) to examine the vocal fold structure and function, though this is usually done by an ENT specialist and results are used to inform treatment decisions. The information gleaned from these methods informs the development of a personalized treatment plan tailored to address the individual’s specific needs. Management might involve voice therapy, medical intervention (if needed), and patient education on vocal hygiene and lifestyle modifications.
Q 27. What is your experience with telepractice and its challenges?
I have significant experience with telepractice, having utilized it extensively throughout the past few years. It’s proven to be a valuable tool in expanding access to care, particularly for clients in remote areas or those with mobility challenges. Using platforms like Zoom or dedicated telehealth platforms, I can conduct assessments, provide therapy sessions, and even monitor progress remotely. I utilize digital tools for data collection and sharing materials, such as recordings of therapy sessions or digital workbooks.
However, telepractice presents unique challenges. Technical difficulties, such as internet connectivity issues or software glitches, can disrupt sessions and impact the quality of service. Maintaining client confidentiality in a remote setting requires additional measures, ensuring secure communication channels and adherence to HIPAA regulations. The lack of in-person interaction can sometimes limit the effectiveness of certain therapeutic techniques, especially those requiring close physical observation or hands-on manipulation. Finally, building rapport with clients remotely can require more effort to overcome the distance barrier.
To mitigate these challenges, I ensure a reliable internet connection, use backup systems, and establish clear communication protocols with clients. I carefully explain the technical aspects of the sessions, proactively address any technological difficulties, and adapt the therapy approach, incorporating visual aids and interactive activities to enhance engagement.
Key Topics to Learn for Speech and Language Pathology Interview
- Articulation Disorders: Understanding different types of articulation disorders (e.g., phonological processes, apraxia of speech), assessment methods (e.g., phonetic inventory, speech sound discrimination), and intervention strategies (e.g., articulation therapy, phonological therapy).
- Fluency Disorders: Knowledge of stuttering, cluttering, and their assessment and treatment. This includes understanding various therapeutic approaches and their practical application in diverse clinical settings.
- Language Disorders: Comprehensive understanding of language development milestones, types of language disorders (e.g., receptive and expressive language disorders, specific language impairment), and assessment and intervention techniques across different age groups.
- Voice Disorders: Familiarity with vocal anatomy and physiology, common voice disorders (e.g., vocal nodules, polyps, spasmodic dysphonia), assessment procedures (e.g., perceptual evaluation, acoustic analysis), and therapeutic interventions.
- Cognitive-Communication Disorders: Understanding the impact of cognitive impairments (e.g., traumatic brain injury, stroke) on communication and swallowing, and the application of assessment and treatment strategies tailored to specific cognitive deficits.
- Swallowing Disorders (Dysphagia): Knowledge of the phases of swallowing, common dysphagia types, assessment techniques (e.g., clinical bedside swallow examination, videofluoroscopic swallow study), and management strategies (e.g., diet modifications, compensatory techniques).
- Assessment and Intervention Approaches: Demonstrate a strong understanding of various assessment tools and intervention strategies used in speech-language pathology. Be prepared to discuss your experience with different assessment and treatment models and your ability to adapt your approach to individual client needs.
- Ethical Considerations and Professional Practice: Showcase your understanding of ethical principles, legal requirements, and professional responsibilities within the field of speech-language pathology. Be ready to discuss case studies and how you’d navigate ethical dilemmas.
Next Steps
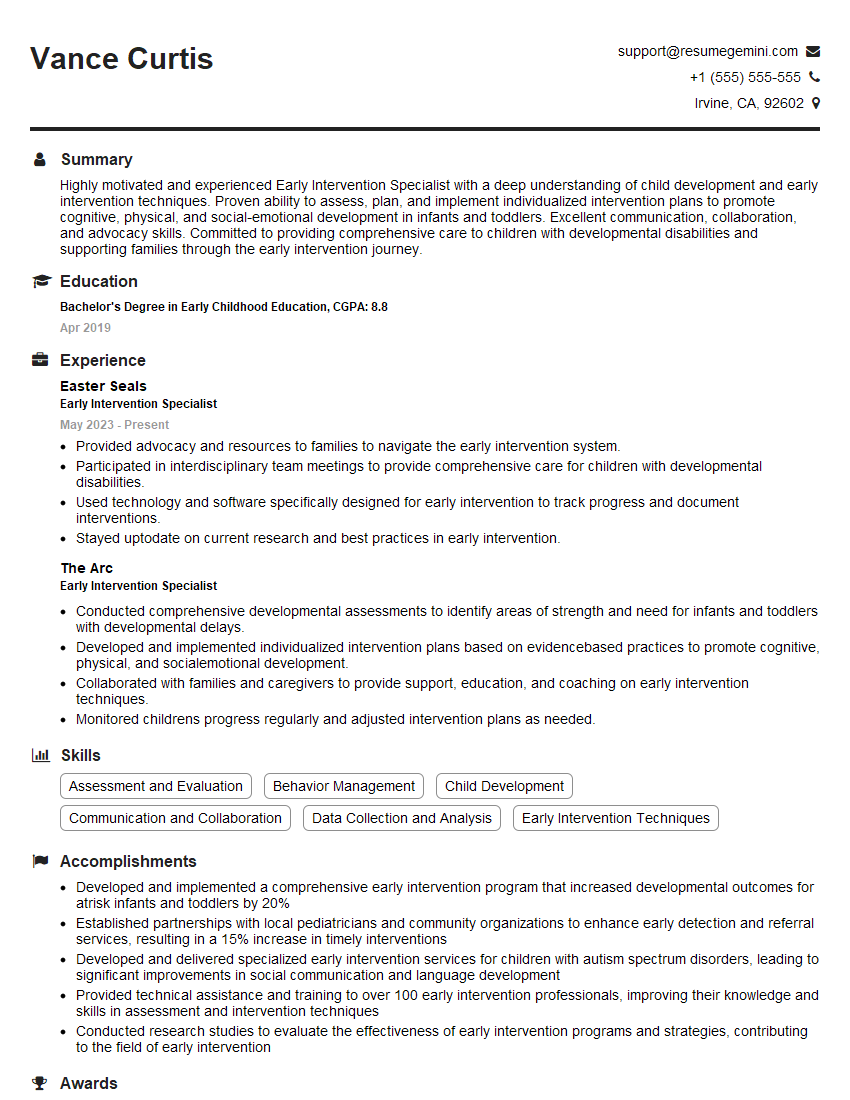
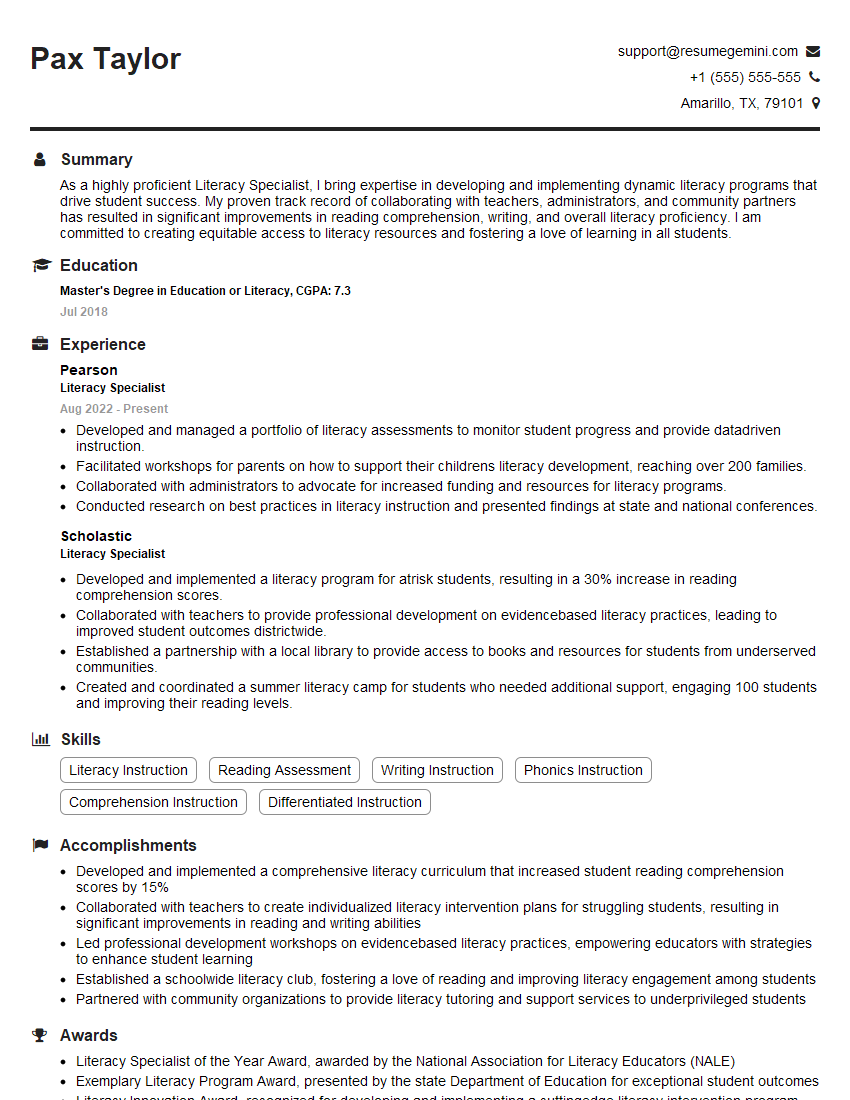
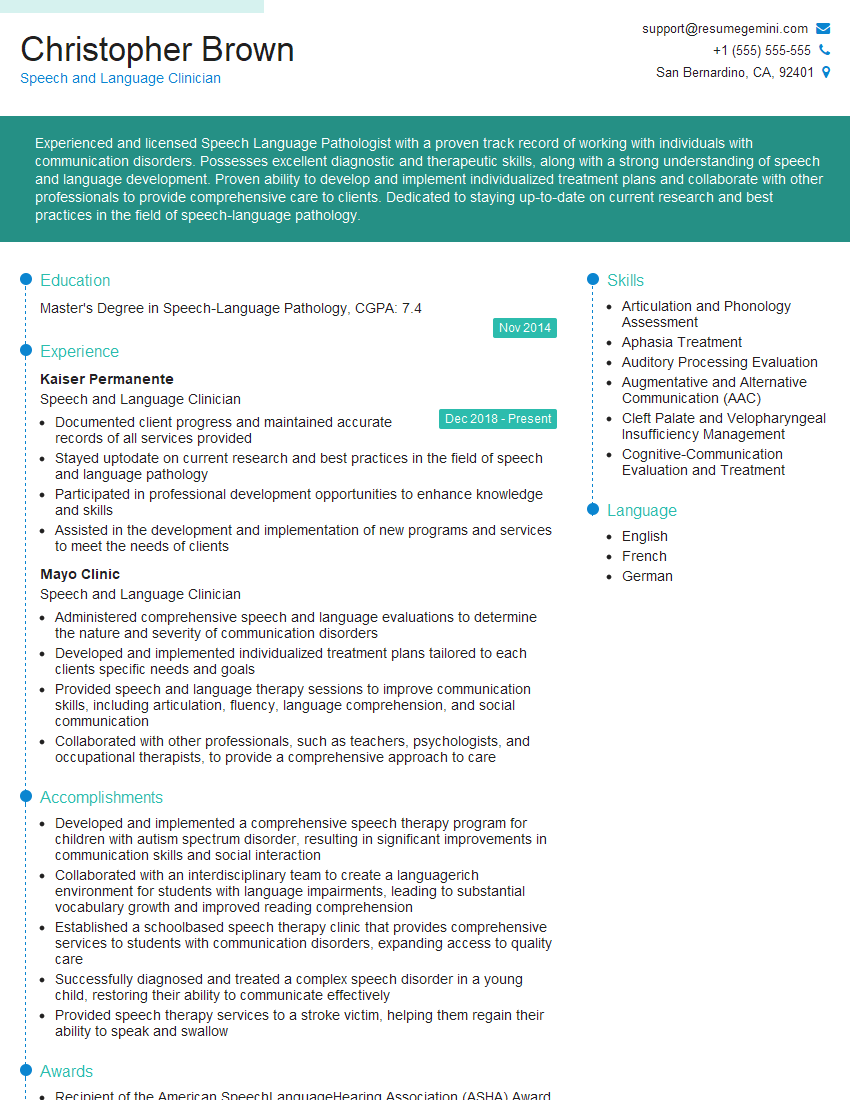
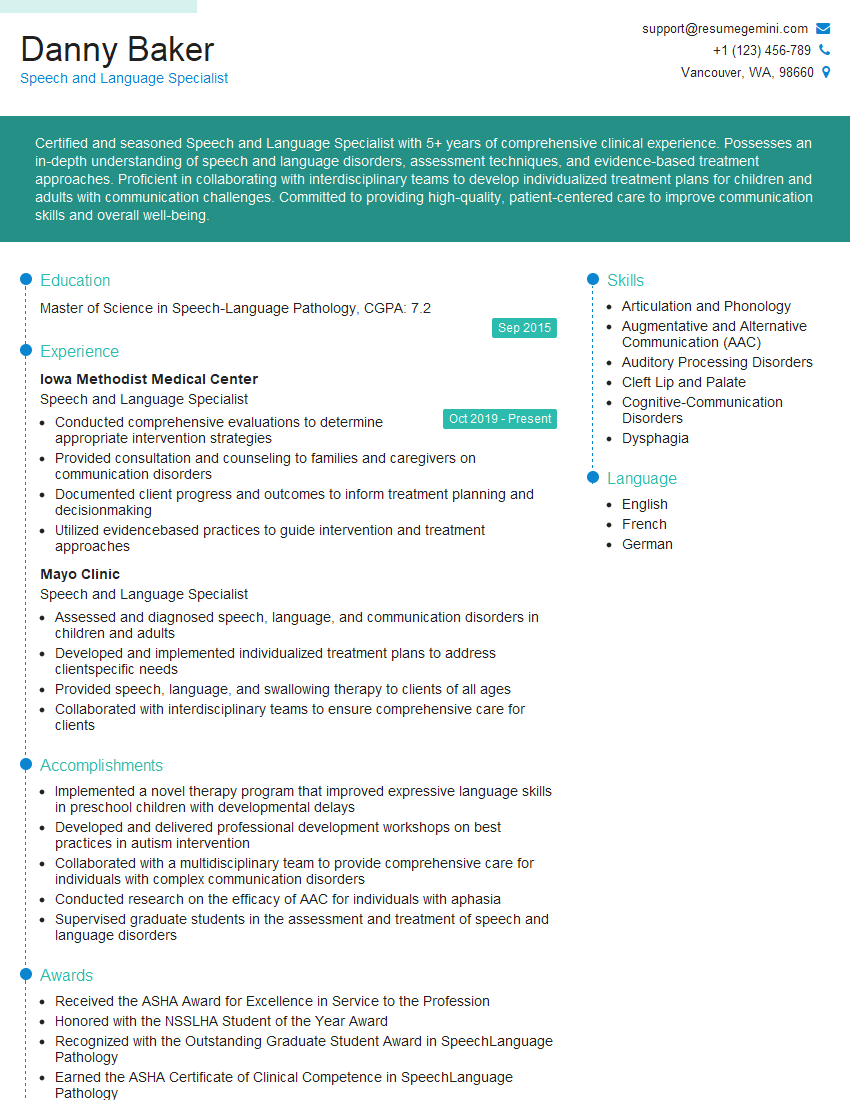
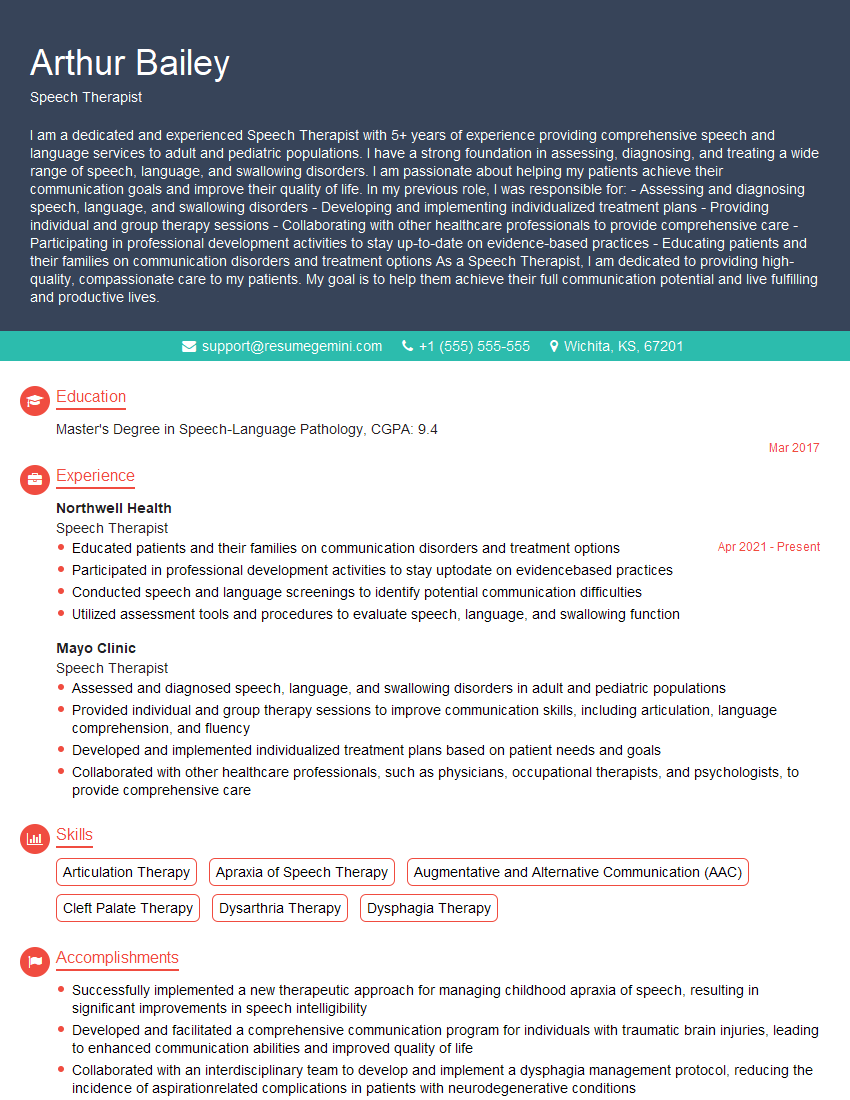
Mastering Speech and Language Pathology opens doors to a rewarding career with diverse opportunities for growth and specialization. To maximize your job prospects, crafting a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. They provide examples of resumes tailored specifically to Speech and Language Pathology to help guide you. Invest the time in creating a compelling resume – it’s your first impression and a key step in securing your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good