The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Therapeutic Management interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Therapeutic Management Interview
Q 1. Describe your experience in developing and implementing therapeutic treatment plans.
Developing and implementing therapeutic treatment plans involves a systematic approach that prioritizes the client’s unique needs and goals. It begins with a thorough assessment, followed by the creation of a personalized plan, its implementation, ongoing monitoring, and necessary adjustments.
For example, I worked with a client struggling with anxiety. After a comprehensive assessment, including interviews, questionnaires, and observations, I discovered that her anxiety stemmed from social situations and a fear of public speaking. We collaboratively developed a treatment plan incorporating Cognitive Behavioral Therapy (CBT) techniques, specifically focusing on exposure therapy and cognitive restructuring. We started with small steps, like practicing public speaking in a safe environment, gradually increasing the challenge level. Regular sessions focused on identifying and challenging negative thought patterns and developing coping mechanisms. The plan was continuously reviewed and modified based on her progress and feedback, ultimately leading to a significant reduction in her anxiety symptoms.
Another example involved a child with ADHD. Their treatment plan focused on behavioral therapy techniques like positive reinforcement and consistent routines combined with medication management in consultation with their physician. The plan’s effectiveness was tracked through regular check-ins with the parents and school to ensure the strategies were effective in both home and school settings.
Q 2. Explain your approach to assessing a client’s needs and developing individualized goals.
Assessing a client’s needs and developing individualized goals is a crucial step in therapeutic management. My approach is multifaceted and holistic, incorporating various assessment methods to gain a comprehensive understanding. This includes:
- Clinical Interviews: Open-ended questions to understand the client’s history, current struggles, and personal goals.
- Psychological Assessments: Standardized tests and questionnaires to measure specific symptoms, personality traits, and cognitive abilities.
- Behavioral Observations: Observing the client’s behavior in different settings to identify patterns and triggers.
- Collateral Information: Gathering information from family members, teachers, or other relevant sources.
Once the assessment is complete, I work collaboratively with the client to set realistic and achievable goals. These goals are measurable, specific, achievable, relevant, and time-bound (SMART goals). For instance, instead of a broad goal like “reduce anxiety,” a SMART goal would be “reduce anxiety scores on the GAD-7 scale by 50% within three months.” This approach ensures that progress is trackable and reinforces motivation.
Q 3. How do you prioritize client needs when faced with limited resources?
Prioritizing client needs with limited resources requires a thoughtful and ethical approach. I use a framework based on urgency, severity, and potential for positive impact.
Urgency: Addressing immediate crises, such as suicidal ideation or imminent harm, takes top priority. Severity: Conditions with the most significant impact on the client’s well-being and functioning are prioritized. Potential for positive impact: Interventions with the highest likelihood of producing meaningful change are preferred, even if they aren’t the most urgent or severe.
I also prioritize collaboration with other professionals and agencies to leverage resources effectively and coordinate care. For example, if a client lacks access to financial resources needed for therapy, I might connect them with local organizations offering reduced-fee services or financial assistance. This collaborative, multi-agency approach allows more clients to receive the support they need.
Q 4. How do you handle difficult or challenging client behaviors?
Handling challenging client behaviors requires patience, understanding, and a strong foundation in therapeutic techniques. My approach focuses on identifying the underlying causes of the behavior, rather than simply reacting to the surface manifestations.
First, I conduct a thorough functional behavior assessment to determine the antecedents (triggers), behavior itself, and consequences that maintain the behavior. This helps in developing a comprehensive behavioral intervention plan.
Secondly, I utilize de-escalation techniques, such as active listening, empathy, and setting clear boundaries. If needed, I implement strategies like time-out or removal from the situation to prevent escalation.
Finally, I work collaboratively with the client to develop coping strategies to manage triggers and modify their behavior. This involves teaching alternative behaviors, positive reinforcement, and consistent follow-up. For example, if a client exhibits verbal aggression during sessions, we would work to identify triggers (such as feeling overwhelmed or misunderstood) and then practice alternative responses such as taking deep breaths or expressing their feelings assertively.
Q 5. Describe your experience working with diverse populations.
My experience working with diverse populations is extensive. I’ve worked with clients from various cultural backgrounds, socioeconomic statuses, and with diverse sexual orientations and gender identities. I believe that cultural competence is essential for effective therapeutic management.
This includes understanding the impact of culture, race, ethnicity, gender, sexual orientation, religion, and socioeconomic status on mental health and well-being. I incorporate a culturally sensitive approach by adapting my techniques to meet the individual needs and preferences of each client. For example, I would use culturally appropriate language, adapt therapeutic interventions to suit cultural values and beliefs, and be mindful of power dynamics that may exist in the therapeutic relationship. Building trust and rapport with clients from diverse backgrounds is crucial and often requires taking extra time to establish a comfortable therapeutic space.
Q 6. What therapeutic modalities are you proficient in?
I’m proficient in several therapeutic modalities, including:
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and behaviors.
- Dialectical Behavior Therapy (DBT): Specifically designed for individuals with borderline personality disorder and other emotional dysregulation disorders.
- Acceptance and Commitment Therapy (ACT): Helps clients accept difficult thoughts and feelings and focus on living a meaningful life.
- Psychodynamic Therapy: Explores unconscious patterns and past experiences to gain insight into current behavior.
- Solution-Focused Brief Therapy: A short-term approach that emphasizes identifying solutions rather than dwelling on problems.
My selection of modality depends heavily on the individual needs and preferences of the client, their presenting issues, and their overall therapeutic goals. I believe in utilizing a flexible and integrative approach, drawing from various techniques as needed to optimize treatment effectiveness.
Q 7. Explain your understanding of evidence-based practices in therapeutic management.
Evidence-based practices (EBPs) are essential in therapeutic management. EBPs integrate the best available research evidence, clinical expertise, and client values and preferences to guide treatment decisions.
I stay abreast of the latest research findings through continuous professional development, attending workshops and conferences, and regularly reviewing peer-reviewed journals. I ensure my interventions are supported by empirical data and I adjust my strategies based on the available scientific evidence. For example, when treating anxiety disorders, I prioritize CBT techniques due to their strong empirical support. Furthermore, I use outcome measures to track progress and evaluate the effectiveness of interventions, allowing me to make data-driven adjustments to the treatment plan as needed. This ensures that my clients receive the most effective and ethically sound care.
Q 8. How do you maintain client confidentiality and ethical standards?
Maintaining client confidentiality and ethical standards is paramount in therapeutic management. It’s the cornerstone of trust and a crucial aspect of providing effective care. This involves adhering to strict guidelines, primarily informed by professional codes of ethics (like those from the American Psychological Association or similar organizations depending on the location and professional license).
- Confidentiality: I always explain the limits of confidentiality at the outset of therapy. This includes situations where I’m legally obligated to report things like child abuse, elder abuse, or imminent harm to self or others. I ensure clients understand this explicitly and any exceptions to confidentiality.
- Data Security: All client information, whether electronic or paper-based, is stored securely and only accessible by authorized personnel. I utilize HIPAA-compliant electronic health record systems to protect sensitive data from unauthorized access.
- Informed Consent: Before initiating any treatment, I obtain informed consent from the client, ensuring they understand the treatment plan, potential risks and benefits, and their rights as patients.
- Professional Boundaries: Maintaining strict professional boundaries is crucial. This includes avoiding dual relationships (e.g., being a therapist and a friend), managing appropriate interactions, and understanding and adhering to the potential impact of social media interactions with clients.
- Supervision and Consultation: I regularly engage in supervision and consultation with experienced colleagues to discuss ethical dilemmas and ensure I’m maintaining the highest standards of practice.
For example, if a client discloses plans to harm someone, I am legally obligated to break confidentiality and report this to the relevant authorities, even if the client explicitly requests me not to. This is a difficult but necessary aspect of ethical practice.
Q 9. Describe a situation where you had to adapt your treatment plan based on a client’s response.
Adapting treatment plans is a common occurrence in therapeutic work. Clients respond differently to interventions, and their needs evolve over time. One instance involved a client struggling with severe anxiety who was initially responding well to cognitive-behavioral therapy (CBT) techniques. However, after several sessions, their anxiety worsened, and the previously effective strategies seemed ineffective.
After careful assessment, I realized the client was experiencing significant sleep disturbances, which were exacerbating their anxiety. The original CBT focus on thought patterns was not addressing the underlying physical factor. Therefore, I adapted the treatment plan to incorporate relaxation techniques specifically aimed at improving sleep hygiene (e.g., sleep restriction therapy, stimulus control therapy, and relaxation exercises before bed). We also introduced mindfulness meditation, which proved beneficial in managing sleep-related anxiety. By integrating these adjustments, the client experienced a significant reduction in anxiety and improved sleep quality. This highlighted the importance of regular monitoring and assessment of client progress and readiness to adapt the course of therapy as needed.
Q 10. How do you collaborate with other professionals in a multidisciplinary team?
Collaboration in multidisciplinary teams is essential for comprehensive client care. It necessitates effective communication, respect for diverse perspectives, and a shared focus on the client’s well-being.
- Regular Meetings: I participate in regular team meetings, sharing information, updates, and insights regarding the client’s progress, challenges, and treatment plan. This might involve case conferences with psychiatrists, social workers, occupational therapists, and other relevant professionals.
- Information Sharing: I actively and appropriately share relevant client information with the team, maintaining appropriate privacy and adhering to all legal and ethical considerations.
- Shared Goals: I work with the team to establish shared goals for the client and develop a coordinated treatment plan that addresses their needs holistically.
- Open Communication: Maintaining open communication is key. This involves regular updates, clear communication of concerns or challenges, and respectful disagreement when needed.
- Case Management: In some cases, I take a lead role in case management, coordinating appointments, resources, and services for the client.
For instance, when working with a client with substance abuse issues, I collaborate closely with a psychiatrist for medication management, a social worker for support services, and a vocational rehabilitation specialist for job training and placement, ensuring a holistic approach to recovery.
Q 11. How do you measure the effectiveness of your therapeutic interventions?
Measuring the effectiveness of therapeutic interventions is crucial for demonstrating accountability and providing the best possible client care. It relies on a combination of methods.
- Client Self-Report Measures: These include questionnaires and scales assessing symptoms, functional abilities, and quality of life (e.g., Beck Depression Inventory, Generalized Anxiety Disorder 7-item scale). These provide a subjective view of progress from the client’s perspective.
- Objective Measures: Objective data may include physiological measures (e.g., heart rate variability for anxiety), behavioral observations (e.g., frequency of self-harm behaviors), and performance on standardized tests (e.g., cognitive function tests).
- Goal Attainment Scaling (GAS): This method involves collaboratively setting specific, measurable, achievable, relevant, and time-bound goals with the client at the start of therapy. Progress toward these goals is then tracked regularly.
- Session-by-Session Monitoring: Regularly assessing the client’s progress and adjusting the treatment plan based on their responses throughout the sessions is also key.
For example, when working with a client struggling with depression, we might use the PHQ-9 (Patient Health Questionnaire-9) to track their symptoms over time. A reduction in their PHQ-9 score, combined with their self-reported improvement in mood and functioning, would indicate the effectiveness of the intervention.
Q 12. What is your experience with crisis intervention?
Crisis intervention is a critical skill for therapists. It involves providing immediate support and resources to clients experiencing acute distress or a psychological crisis. My experience encompasses various scenarios, including suicidal ideation, acute anxiety attacks, and situations involving interpersonal conflict or trauma.
- Risk Assessment: The first step is a thorough risk assessment to determine the severity and nature of the crisis, including assessing the client’s immediate danger to self or others.
- Safety Planning: Collaborating with the client to develop a safety plan, including identifying warning signs, coping mechanisms, and support systems, is essential.
- Stabilization: The focus is on stabilizing the client’s emotional state through techniques like grounding exercises, relaxation techniques, and empathetic listening.
- Resource Mobilization: Connecting the client with appropriate resources, such as emergency services, crisis hotlines, or inpatient treatment facilities, is crucial.
- Follow-up: Following up with the client to ensure their continued safety and access to appropriate support is important.
I’ve had experience assisting clients in suicidal crises. In these situations, after ensuring their immediate safety, I prioritize building rapport, validating their feelings, and collaboratively developing a safety plan. This may involve contacting their family or friends for support, referring them to a crisis hotline, or arranging for inpatient hospitalization if necessary.
Q 13. How do you manage your own stress and maintain your well-being as a therapist?
Self-care is not merely a suggestion; it’s a necessity for therapists. The emotional intensity of therapeutic work can be draining, and neglecting self-care can lead to burnout and compromise professional effectiveness.
- Supervision: Regular supervision provides a space to process challenging cases, explore ethical dilemmas, and receive support from experienced colleagues.
- Personal Therapy: Many therapists engage in personal therapy to maintain their own mental and emotional well-being and understand their own personal biases and countertransference.
- Boundary Setting: Establishing and maintaining clear boundaries between professional and personal life is important to prevent emotional exhaustion.
- Stress Management Techniques: I utilize various stress management techniques, including exercise, mindfulness meditation, spending time in nature, and pursuing hobbies outside of work.
- Professional Organizations and Support Networks: Joining professional organizations and engaging with support networks provides a sense of community and access to resources for self-care.
Setting aside dedicated time for self-care isn’t selfish; it’s crucial for maintaining both personal well-being and professional competence. It’s analogous to an airplane’s oxygen mask: you must take care of yourself first before you can effectively help others.
Q 14. Explain your knowledge of relevant legislation and regulations related to therapeutic management.
Knowledge of relevant legislation and regulations is essential for ethical and legal practice. The specific laws vary depending on location, but some key areas include:
- Confidentiality Laws (e.g., HIPAA in the US): These laws protect client information and outline the conditions under which confidentiality can be breached (e.g., mandated reporting of child abuse).
- Informed Consent Laws: These laws mandate that clients be fully informed about treatment options, potential risks and benefits, and their rights before agreeing to therapy.
- Licensing and Credentialing Laws: These laws regulate the practice of therapy, including the requirements for licensure, continuing education, and professional conduct.
- Mandatory Reporting Laws: These laws dictate the situations in which therapists are legally required to report certain information to authorities (e.g., child abuse, elder abuse, threats of harm to others).
- Record-Keeping Regulations: These regulations specify the types of client records that must be kept, how long they must be retained, and the security measures needed to protect them.
Staying updated on relevant laws and regulations is a continuous process requiring ongoing professional development and consultation with legal counsel when needed. Understanding these legal frameworks is crucial for protecting both clients and therapists from potential legal repercussions.
Q 15. How do you document client progress accurately and thoroughly?
Accurate and thorough documentation of client progress is crucial for effective therapeutic management and continuity of care. It serves as a record of the client’s journey, informing treatment decisions and ensuring accountability. My approach involves a multi-faceted strategy:
- Structured Note-Taking: I utilize a standardized format, often incorporating the SOAP note method (Subjective, Objective, Assessment, Plan). This ensures consistency and covers all relevant aspects of each session.
- Specific and Measurable Goals: Progress notes clearly define measurable goals established collaboratively with the client. For example, instead of noting ‘improved mood,’ I’d document ‘Client reported a decrease in depressive symptoms, scoring 12 on the PHQ-9 (down from 20 at baseline) and reported engaging in two planned social activities this week.’
- Objective Data Collection: I incorporate objective data whenever possible, such as scores on standardized assessments, behavioral observations, and reports from family members (with client consent). This minimizes bias and enhances the validity of the documentation.
- Client Input: I actively involve the client in the documentation process, ensuring they understand and agree with the information recorded. This fosters transparency and collaboration.
- Regular Review and Updates: I regularly review and update the client’s file, ensuring accuracy and reflecting changes in their presentation and treatment plan. This allows for adjustments to the therapeutic approach as needed.
For instance, with a client struggling with anxiety, I wouldn’t simply write ‘anxiety improved,’ but instead, detail the specific techniques used (e.g., relaxation exercises, cognitive restructuring), the client’s response to those techniques (e.g., reported decreased heart rate during relaxation exercises), and any observable changes in their behavior (e.g., increased participation in social situations).
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience in conducting therapeutic assessments.
Therapeutic assessments are the cornerstone of effective treatment planning. My experience encompasses a range of assessment methodologies, tailored to the individual client’s needs and presenting concerns. This includes:
- Clinical Interviews: I conduct thorough clinical interviews to gather comprehensive information about the client’s history, current symptoms, and personal context. This includes exploring their developmental history, family dynamics, social support systems, and cultural background.
- Standardized Psychological Tests: I utilize various standardized tests such as the Minnesota Multiphasic Personality Inventory (MMPI), Beck Depression Inventory (BDI), and Anxiety Sensitivity Index (ASI) to objectively assess the severity and nature of psychological symptoms.
- Behavioral Observations: I pay close attention to the client’s nonverbal cues, demeanor, and interactions throughout the assessment process. This provides valuable supplemental information.
- Collateral Information: When appropriate and with informed consent, I gather information from family members, significant others, or other professionals involved in the client’s care. This offers a broader perspective and enriches the assessment.
For example, when assessing a child experiencing behavioral difficulties, I would conduct a clinical interview with the child and their parents, observe the child’s behavior in different settings, and administer age-appropriate standardized tests to evaluate their cognitive abilities and emotional functioning. The integration of these methods provides a holistic understanding of the child’s challenges, enabling me to develop a targeted intervention plan.
Q 17. Explain your understanding of different theoretical frameworks used in therapeutic practice.
My therapeutic practice integrates various theoretical frameworks, acknowledging that a flexible and eclectic approach often yields the best outcomes. I draw upon:
- Cognitive Behavioral Therapy (CBT): This evidence-based approach focuses on identifying and modifying maladaptive thoughts, beliefs, and behaviors. I frequently employ CBT techniques like cognitive restructuring and behavioral activation to help clients manage anxiety, depression, and other mental health challenges.
- Psychodynamic Therapy: This approach emphasizes exploring unconscious patterns and past experiences to understand current difficulties. I utilize psychodynamic principles to help clients gain insight into their emotional patterns and relational dynamics.
- Person-Centered Therapy: This humanistic approach emphasizes empathy, unconditional positive regard, and the client’s inherent capacity for self-healing. I create a safe and supportive environment where clients feel empowered to explore their inner world and develop their own solutions.
- Solution-Focused Brief Therapy (SFBT): This approach focuses on identifying and building upon clients’ strengths and resources to achieve specific, achievable goals in a short timeframe. This is particularly useful for clients seeking immediate relief from specific problems.
The choice of framework depends on the individual client’s needs, presenting problem, and personal preferences. Often, I integrate elements from multiple theoretical perspectives to create a customized treatment plan.
Q 18. How do you involve family members in the therapeutic process?
Involving family members in the therapeutic process is often crucial, especially when working with children, adolescents, or individuals with complex family dynamics. My approach emphasizes:
- Informed Consent: I always obtain informed consent from the client before involving family members. This ensures respect for the client’s autonomy and privacy.
- Collaborative Approach: I view family members as valuable sources of information and support. I work collaboratively with them to understand the family system and its impact on the client’s well-being.
- Family Meetings: When appropriate, I conduct family meetings to discuss the client’s treatment goals and progress. This promotes open communication and shared responsibility.
- Education and Support: I provide family members with education about the client’s condition, treatment plan, and coping strategies. I also offer support and guidance in managing their own emotional responses.
- Maintaining Boundaries: It’s critical to maintain clear professional boundaries with family members, ensuring that the client remains the focus of the therapeutic work.
For example, in working with a young adult struggling with substance abuse, I would involve the family in sessions to understand their role in the client’s recovery, educate them on the disease of addiction, and help them develop healthy communication patterns to support the client’s journey.
Q 19. How do you handle situations where there is a conflict of interest?
Conflicts of interest can compromise the integrity of the therapeutic relationship and must be addressed proactively. My approach prioritizes transparency and ethical practice:
- Identification and Disclosure: I diligently assess potential conflicts of interest at the outset of the therapeutic relationship. Any potential conflicts, no matter how minor, are openly disclosed to the client.
- Consultation: If a conflict arises, I consult with supervisors, colleagues, or ethical review boards to ensure I am making responsible and ethical decisions.
- Referral: If a conflict of interest cannot be resolved, I will refer the client to another therapist who can provide unbiased and effective care.
- Documentation: All instances of potential or actual conflicts of interest are meticulously documented in the client’s file.
For instance, if a client’s insurance company is also a client of my practice, I would disclose this potential conflict and explore alternative options for treatment, potentially referring them to another therapist if appropriate. Maintaining transparency and the client’s best interest is always paramount.
Q 20. How do you educate clients about their condition and treatment options?
Educating clients about their condition and treatment options is essential for fostering engagement and adherence. My approach focuses on:
- Accessible Language: I explain complex information in a clear, concise, and understandable way, avoiding jargon and tailoring my language to the client’s level of comprehension.
- Collaborative Approach: I view the educational process as a collaborative dialogue, ensuring the client feels heard, understood, and involved in decision-making.
- Visual Aids and Resources: I may utilize visual aids, handouts, or other resources to enhance understanding and retention.
- Ongoing Education: Client education is an ongoing process, not a one-time event. I revisit and reinforce key information as needed throughout treatment.
- Addressing Concerns and Questions: I create a safe space for clients to express their concerns, ask questions, and explore their treatment options openly.
For example, when explaining the complexities of depression, I would use relatable analogies, explain how therapy works step-by-step, discuss different treatment modalities in simple terms, and answer the client’s questions in a clear and honest way. The client would feel empowered to make informed decisions regarding their treatment plan.
Q 21. Describe your experience with discharge planning.
Discharge planning is a crucial component of effective therapeutic management. It ensures a smooth transition for the client as they move from active treatment to ongoing self-management or maintenance. My approach involves:
- Collaborative Goal Setting: I work collaboratively with the client to establish realistic goals for the discharge phase, ensuring they are prepared for life after formal therapy.
- Skill Development: I focus on teaching the client relapse prevention strategies and coping mechanisms to manage their condition independently.
- Resource Identification and Referral: I help clients identify and access appropriate resources in their community, such as support groups, self-help programs, or continued care providers.
- Follow-up Plan: I develop a follow-up plan to monitor the client’s progress and provide ongoing support as needed. This may involve scheduled check-in calls or brief follow-up sessions.
- Documentation: The discharge plan and any follow-up activities are thoroughly documented in the client’s file.
For instance, when a client is ready to complete their treatment for anxiety, we might collaboratively establish a plan that includes weekly meditation practice, enrollment in a mindfulness group, and a scheduled follow-up appointment to address any challenges that may arise. I also help them find and connect with any community resources such as support groups or specialized wellness programs.
Q 22. What is your experience with working with clients with specific diagnoses?
My experience spans a wide range of diagnoses, including but not limited to anxiety disorders (generalized anxiety disorder, panic disorder, social anxiety disorder), depressive disorders (major depressive disorder, persistent depressive disorder), trauma-related disorders (PTSD, complex PTSD), and personality disorders. I’ve worked extensively with clients experiencing substance use disorders, as well as those grappling with relationship difficulties and grief and loss. Each diagnosis requires a tailored therapeutic approach, carefully considering the individual’s unique presentation, history, and goals. For example, with clients experiencing PTSD, I utilize evidence-based techniques like prolonged exposure therapy and trauma-focused cognitive behavioral therapy (TF-CBT). In working with clients with substance use disorders, I often incorporate motivational interviewing and relapse prevention strategies, collaborating closely with their medical and psychiatric care providers.
My approach is always client-centered, focusing on building a strong therapeutic alliance and fostering a safe and supportive environment for exploration and healing. I regularly track progress using standardized measures and adapt my interventions based on the client’s response and ongoing needs.
Q 23. How do you address ethical dilemmas that arise in therapeutic practice?
Ethical dilemmas in therapeutic practice are inevitable. My approach to addressing these situations involves a systematic process. First, I carefully identify the ethical conflict, clarifying the values and principles involved. This often involves consulting relevant ethical codes, such as those published by the American Psychological Association (APA) or other professional organizations. Next, I gather all relevant information, considering the client’s perspective, my own values, and the legal implications. Then, I carefully weigh the potential consequences of different courses of action, utilizing a decision-making framework that prioritizes the client’s well-being and autonomy, while also adhering to professional standards.
For example, if a client discloses intentions of harming themselves or others, I have a mandatory duty to report this information, even if it compromises confidentiality. This is a critical aspect of my ethical obligations, balancing the client’s right to privacy with their safety and the safety of others. In more ambiguous situations, I find it beneficial to consult with experienced colleagues or supervisors for guidance and support. Documentation of ethical dilemmas and the resolution process is essential for maintaining accountability and transparency.
Q 24. How do you maintain professional boundaries with clients?
Maintaining professional boundaries is paramount in therapeutic relationships. I establish clear boundaries from the outset, outlining the parameters of our work together, such as session times, communication methods, and the nature of our interaction. This includes avoiding dual relationships, such as social interactions or business ventures outside of therapy. I actively monitor my own behavior and emotional responses, ensuring that my interactions remain professional and appropriate.
For example, I avoid self-disclosure beyond what is therapeutically necessary and maintain a consistent and respectful demeanor throughout the sessions. I am conscious of power dynamics inherent in the therapeutic relationship, consistently placing the client’s needs and autonomy at the forefront. If any boundary issues arise, I address them promptly and transparently with the client, often seeking consultation with supervisors or colleagues for additional guidance.
Q 25. Describe your experience working with electronic health records (EHR).
I have extensive experience using electronic health records (EHR) systems, including proficiency in data entry, record maintenance, and generating reports. I am familiar with various EHR platforms and am adept at navigating their functionalities, including scheduling, billing, and client communication. I understand the importance of adhering to HIPAA regulations and maintaining the confidentiality and security of client data. This includes utilizing secure messaging systems, password protection, and adhering to all data privacy policies and procedures. I understand how EHRs streamline administrative tasks, leading to increased efficiency and better organization of client information. Furthermore, I can utilize data from EHRs to track client progress and inform treatment planning adjustments.
Q 26. How do you ensure cultural sensitivity and competence in your practice?
Cultural sensitivity and competence are integral to my practice. I strive to create a culturally affirming space for all clients by actively listening, learning about their unique backgrounds and experiences, and adapting my therapeutic approach accordingly. This includes considering the impact of cultural factors on their mental health, beliefs, and coping mechanisms. I avoid making assumptions based on stereotypes and seek to understand the client’s worldview from their perspective.
For example, I might adjust my communication style to match the client’s comfort level, incorporating nonverbal cues into my interactions, as well as considering the importance of family and community within their culture. I am continuously engaging in self-reflection to address any personal biases and seek out further training and education on cultural competence to expand my understanding of various cultural contexts.
Q 27. How do you deal with burnout and compassion fatigue?
Burnout and compassion fatigue are significant challenges in the helping professions. I actively engage in self-care strategies to mitigate these risks. This includes prioritizing my own well-being through regular exercise, sufficient sleep, a healthy diet, and engaging in activities that bring me joy and relaxation. I also utilize mindfulness and meditation techniques to manage stress and promote emotional regulation. Furthermore, I actively utilize supervision and peer support to process challenging cases and maintain emotional balance. I make sure to set healthy boundaries and avoid overextending myself professionally.
Recognizing the signs of burnout and compassion fatigue is crucial. I regularly reflect on my emotional and physical state, paying attention to symptoms such as exhaustion, emotional numbness, cynicism, and a decreased sense of accomplishment. If I experience these symptoms, I prioritize adjusting my workload, seeking support from colleagues, or taking time off to recharge.
Q 28. Explain your knowledge of different therapeutic techniques and when you would utilize them.
My therapeutic approach is integrative, drawing on a range of evidence-based techniques to tailor treatment to each client’s unique needs. I utilize Cognitive Behavioral Therapy (CBT) to help clients identify and modify negative thought patterns and behaviors. Dialectical Behavior Therapy (DBT) is particularly effective for clients experiencing intense emotions and difficulties regulating them, often seen in borderline personality disorder. Acceptance and Commitment Therapy (ACT) helps clients accept difficult thoughts and feelings while focusing on valued actions. I also incorporate mindfulness-based techniques, such as meditation and breathwork, to promote self-awareness and emotional regulation. Trauma-focused therapies, such as prolonged exposure therapy and TF-CBT, are used with clients who have experienced traumatic events.
The choice of technique depends heavily on the client’s diagnosis, presenting problems, and personal preferences. For example, CBT might be highly effective for someone with generalized anxiety disorder, while DBT might be a better fit for someone with borderline personality disorder. An integrative approach often allows for a more flexible and adaptable treatment plan that meets the client’s ever-evolving needs.
Key Topics to Learn for Therapeutic Management Interview
- Therapeutic Relationships: Understanding the dynamics of the therapeutic relationship, including building rapport, setting boundaries, and managing transference and countertransference. Practical application: Describe a scenario where you successfully navigated a challenging therapeutic relationship.
- Treatment Planning & Goal Setting: Developing individualized treatment plans based on client needs and utilizing evidence-based practices. Practical application: Outline the steps involved in creating a comprehensive treatment plan, including measurable goals and intervention strategies.
- Crisis Intervention & Risk Assessment: Identifying and responding effectively to crises, conducting thorough risk assessments, and implementing safety plans. Practical application: Describe your approach to managing a client experiencing a severe emotional crisis.
- Ethical and Legal Considerations: Understanding professional ethics, confidentiality, mandated reporting, and legal implications within therapeutic practice. Practical application: Analyze a hypothetical ethical dilemma faced by a therapist and propose a solution aligning with ethical guidelines.
- Case Management & Collaboration: Coordinating care with other professionals, managing client records, and advocating for clients’ needs within a multidisciplinary team. Practical application: Discuss your experience working collaboratively with other healthcare professionals.
- Evidence-Based Practices: Familiarity with various therapeutic modalities (e.g., CBT, DBT, psychodynamic therapy) and their application in different clinical settings. Practical application: Compare and contrast two different therapeutic approaches and discuss their suitability for specific client populations.
- Cultural Competence & Diversity: Demonstrating awareness of cultural differences and their impact on mental health, providing culturally sensitive care. Practical application: Describe how you would adapt your therapeutic approach to meet the needs of a client from a diverse cultural background.
Next Steps
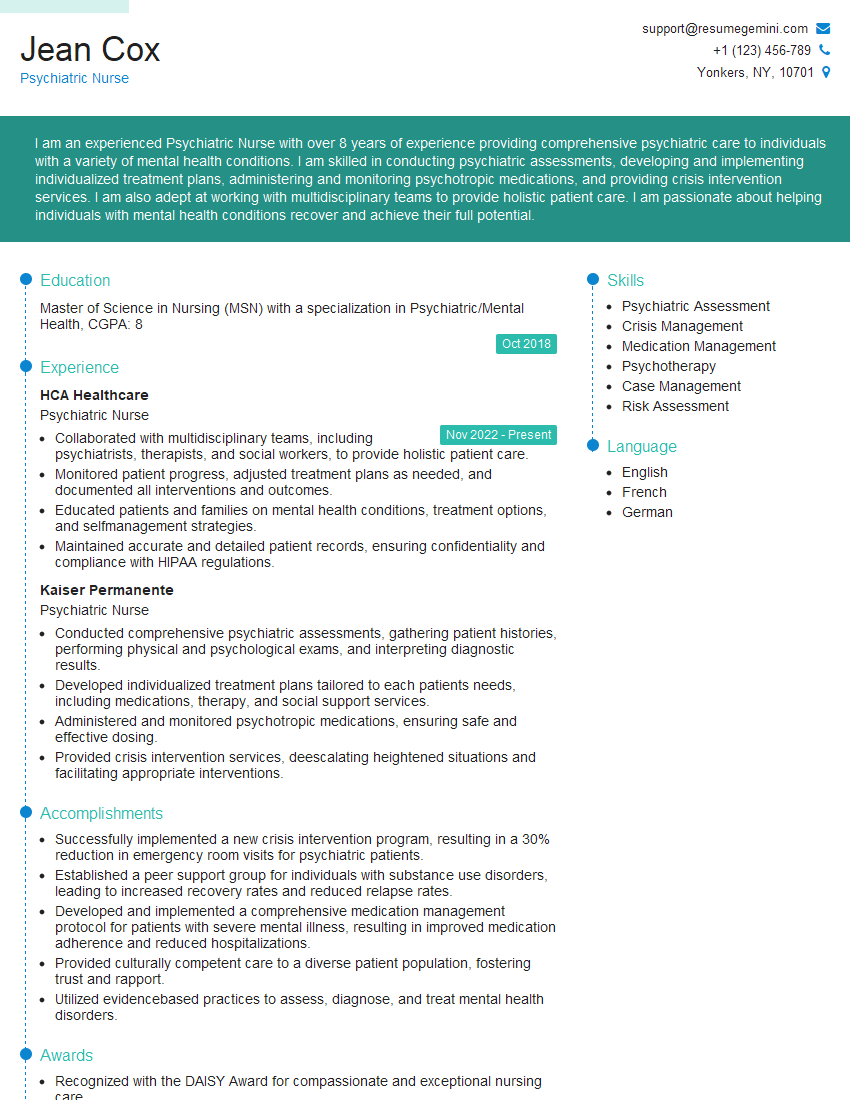
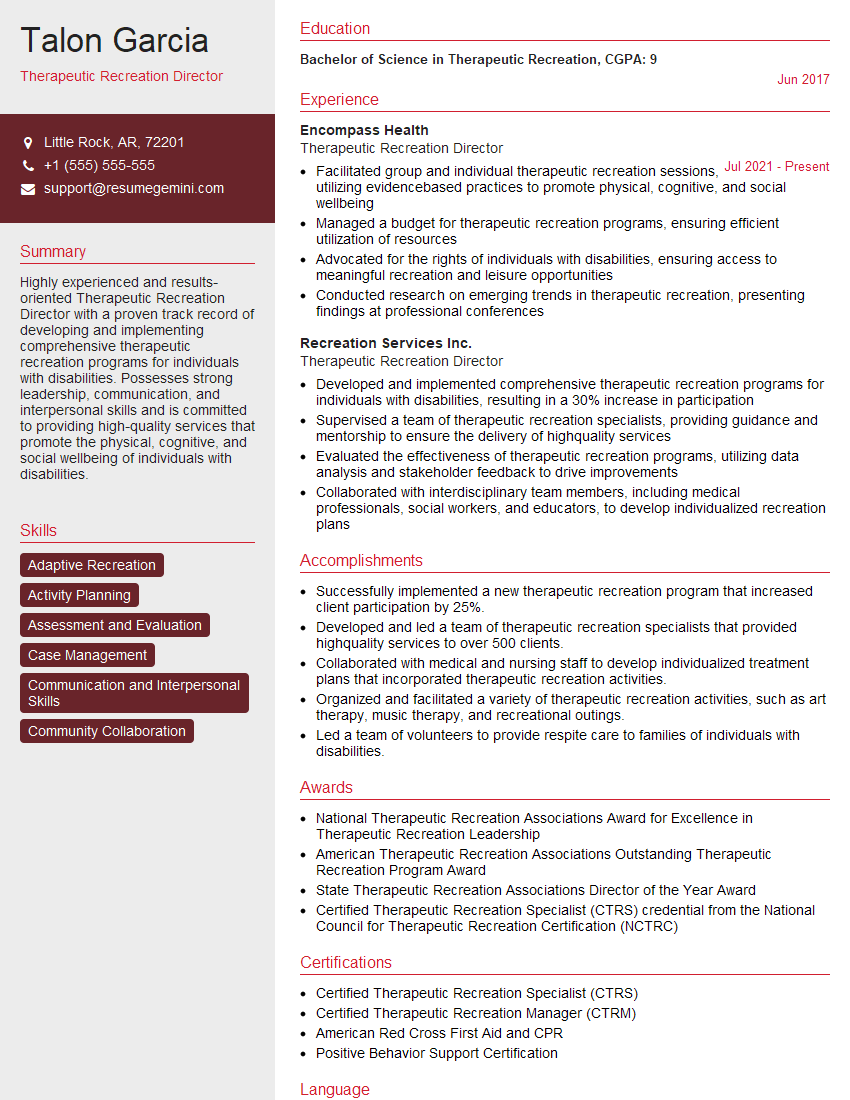
Mastering Therapeutic Management is crucial for career advancement in this dynamic field. A strong understanding of these core concepts will significantly improve your interview performance and open doors to exciting opportunities. To maximize your job prospects, it’s essential to have an ATS-friendly resume that highlights your skills and experience effectively. We highly recommend using ResumeGemini to build a professional and impactful resume. ResumeGemini offers a streamlined process and provides examples of resumes tailored specifically to Therapeutic Management, helping you present your qualifications in the best possible light. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good