Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Therapeutic Relationship Building interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Therapeutic Relationship Building Interview
Q 1. Describe your approach to establishing rapport with a client during the initial session.
Establishing rapport in the initial session is crucial for building a trusting therapeutic relationship. My approach involves creating a safe and welcoming environment where the client feels comfortable sharing their experiences. This begins with a warm greeting and a clear explanation of the therapeutic process. I actively listen to the client’s concerns, using open-ended questions to encourage them to elaborate. I pay close attention to their verbal and nonverbal cues, reflecting back what I hear to ensure understanding. I also strive to be genuine and authentic in my interactions, allowing the client to see me as a person, not just a therapist. For example, I might start by saying something like, “Thank you for coming in today. I understand this can be a difficult step, and I appreciate your courage in seeking help.” This sets a tone of respect and collaboration, laying the foundation for a strong working relationship.
Q 2. Explain the importance of empathy in therapeutic relationship building.
Empathy is the cornerstone of a successful therapeutic relationship. It’s the ability to understand and share the feelings of another person, stepping into their shoes and experiencing the world from their perspective. This doesn’t mean agreeing with their actions or beliefs, but rather acknowledging and validating their emotional experience. Empathy fosters trust and allows clients to feel understood and accepted, encouraging them to open up and engage more fully in the therapeutic process. Imagine a client struggling with grief. Simply saying, “That sounds incredibly difficult,” and offering a quiet, attentive presence conveys empathy more effectively than offering unsolicited advice. The feeling of being truly heard and understood helps them process their emotions and move forward.
Q 3. How do you handle transference and countertransference in the therapeutic relationship?
Transference refers to the client unconsciously transferring feelings and patterns of relating from past relationships onto the therapist. Countertransference is the therapist’s emotional reaction to the client, often influenced by their own unresolved issues. Managing these dynamics requires self-awareness and careful attention to the therapeutic process. I utilize regular supervision and self-reflection to identify potential countertransference issues. When transference arises, I address it gently and collaboratively with the client, exploring the origins of these feelings and how they might be impacting their current relationships. For example, if a client displays anger towards me reminiscent of their relationship with a parent, I might say, “I notice you seem frustrated with me right now. I wonder if this reminds you of anyone else in your life.” This approach encourages the client to explore their feelings in a safe and controlled environment.
Q 4. What techniques do you use to manage boundaries with clients?
Setting and maintaining clear boundaries is essential for a healthy therapeutic relationship and for protecting both the client and the therapist. This includes establishing clear guidelines regarding session length, cancellations, confidentiality, and the nature of the therapeutic relationship. I explicitly discuss these boundaries during the initial session and revisit them as needed. For example, I clearly state my policy on missed appointments and explain the limits of confidentiality. I also maintain professional distance, avoiding dual relationships and personal disclosures that might blur the boundaries of the therapeutic relationship. It’s important to communicate these boundaries respectfully but firmly, ensuring clients understand their importance in creating a safe and effective therapeutic space.
Q 5. Describe a situation where you had to repair a damaged therapeutic relationship.
In one instance, a client became increasingly resistant to therapy, missing sessions and expressing dissatisfaction with our work. I realized I had inadvertently misinterpreted some of their nonverbal cues, leading to misunderstandings. To repair the relationship, I initiated a session dedicated to reflecting on our interactions and addressing their concerns. I apologized for any misinterpretations and actively listened to their feedback, acknowledging their feelings of frustration and disappointment. We collaboratively redefined our goals and adjusted our approach, focusing more on their specific needs. This open and honest communication, along with a demonstrable shift in my approach, helped to rebuild trust and strengthen the therapeutic alliance.
Q 6. How do you adapt your communication style to meet the needs of diverse clients?
Adapting my communication style to meet diverse client needs involves being mindful of cultural differences, individual communication preferences, and potential language barriers. I actively listen to understand each client’s unique communication style, adjusting my language, tone, and approach accordingly. I may employ techniques like using simpler language if needed, validating different expressions of emotions across cultures, and seeking clarification to ensure mutual understanding. For example, I might adjust my level of formality based on the client’s preference, and be sensitive to nonverbal communication styles that might differ across cultures. Employing interpreters when necessary is another critical part of ensuring access to effective care.
Q 7. Explain the concept of therapeutic alliance and its significance.
The therapeutic alliance is the collaborative relationship between the therapist and the client, characterized by trust, mutual respect, and a shared understanding of the therapeutic goals. It is widely considered the most important predictor of successful therapy. This strong bond allows clients to feel safe and comfortable exploring their vulnerabilities and engaging in the difficult work of self-discovery. The alliance is built upon empathy, active listening, and consistent effort from both the therapist and client. A strong therapeutic alliance fosters motivation for change, enhances the effectiveness of therapeutic interventions, and contributes to better overall outcomes. It’s like a team working together towards a common goal, where both members contribute to the process and celebrate successes along the way.
Q 8. How do you address cultural differences in the therapeutic relationship?
Addressing cultural differences is paramount in building a therapeutic relationship. It’s not just about acknowledging differences; it’s about understanding how those differences shape a client’s worldview, communication style, and understanding of mental health itself. This requires cultural humility – a lifelong commitment to self-reflection and learning, recognizing that my own cultural background shapes my perceptions.
- Cultural Sensitivity Training: I continually engage in cultural sensitivity training to broaden my understanding of diverse cultural norms and values. This helps me avoid inadvertently causing offense or misinterpreting client behaviors.
- Active Listening and Inquiry: I prioritize active listening, paying close attention to both verbal and nonverbal cues. Asking open-ended questions like, “Tell me more about your experiences,” allows clients to share their perspectives in their own terms. I avoid making assumptions about their background or experiences.
- Adapting My Approach: My therapeutic approach is flexible. For instance, direct eye contact, considered a sign of respect in some cultures, might be perceived as aggressive in others. I adapt my communication style to be respectful and sensitive to cultural norms.
- Seeking Consultation: If I encounter cultural nuances I don’t fully understand, I seek consultation from colleagues with expertise in the relevant culture or from cultural consultants.
For example, working with a client from a collectivist culture, I would adjust my focus from individualistic goals to incorporate family dynamics and community support systems into the therapeutic plan.
Q 9. Describe your approach to managing difficult client behaviors.
Managing difficult client behaviors requires a multifaceted approach rooted in safety, empathy, and clear boundaries. It’s crucial to remember that these behaviors often stem from underlying pain or distress.
- Safety First: If a client’s behavior poses a risk to themselves or others, my priority is ensuring safety. This might involve developing a safety plan, involving other professionals, or hospitalizing the client if necessary.
- Understanding the Behavior: I work to understand the function of the behavior – what needs is the client trying to meet? Is it a way of expressing unmet needs, managing overwhelming emotions, or communicating distress?
- Clear Boundaries: I set clear and consistent boundaries regarding acceptable behavior in sessions. This is communicated calmly and firmly, focusing on the impact of the behavior rather than making personal attacks.
- Collaboration: I work collaboratively with the client to develop strategies for managing the behavior. This might include identifying triggers, developing coping mechanisms, or practicing alternative behaviors.
- Self-Care: Managing difficult client behaviors can be emotionally draining. I prioritize self-care to prevent burnout and maintain my own well-being.
For instance, if a client is consistently interrupting, I might gently say, “I understand you’re eager to share, and I want to hear everything. To make sure we both get the chance to fully discuss this, let’s try taking turns speaking.”
Q 10. How do you maintain ethical and professional standards in your work?
Maintaining ethical and professional standards is the cornerstone of my practice. This involves adhering to a strict code of ethics, continuously updating my knowledge, and prioritizing client well-being above all else.
- Adherence to Ethical Codes: I meticulously follow the ethical guidelines established by my professional organizations, ensuring that my actions align with the highest standards of professional conduct.
- Continuing Education: I actively participate in continuing education to stay abreast of current best practices, research findings, and legal updates relevant to my field.
- Supervision: I regularly engage in supervision with experienced colleagues, utilizing this as a forum for ethical reflection and case consultation.
- Self-Reflection: I prioritize regular self-reflection to identify any potential biases or areas for improvement in my practice. This is essential for maintaining objectivity and providing ethical care.
- Documentation: Meticulous record-keeping ensures transparency and accountability, providing a clear record of sessions and decisions made throughout the therapeutic process.
For example, maintaining client confidentiality is paramount. I only share information with other professionals when legally required or when the client has given explicit consent.
Q 11. How do you navigate ethical dilemmas related to client confidentiality?
Navigating ethical dilemmas regarding confidentiality requires careful consideration of legal and ethical guidelines, prioritizing client well-being and safety.
- Duty to Warn/Protect: In situations where there is a credible threat of harm to the client or others, I have a legal and ethical obligation to break confidentiality and take appropriate protective actions, such as notifying authorities or involving relevant individuals.
- Consultation: When faced with an ethical dilemma, I consult with supervisors, colleagues, or ethics committees to gain clarity and guidance on the best course of action. This collaborative approach helps ensure responsible decision-making.
- Legal Requirements: I am aware of mandatory reporting laws concerning child abuse, elder abuse, and other forms of harm. I adhere strictly to these legal requirements.
- Informed Consent: I ensure clients are fully informed about the limits of confidentiality at the outset of treatment. This open communication reduces misunderstandings and fosters trust.
For example, if a client reveals an intention to harm themselves or another person, I would take steps to ensure their safety, which might involve contacting emergency services or relevant authorities, even if it means compromising confidentiality.
Q 12. What are the signs of a strong therapeutic alliance?
A strong therapeutic alliance is characterized by a collaborative relationship built on trust, respect, and a shared understanding of goals. It’s the foundation for successful therapy.
- Trust and Rapport: Clients feel comfortable sharing their thoughts and feelings openly and honestly. There is a sense of safety and mutual respect between the client and therapist.
- Collaboration and Shared Goals: Therapist and client work together to establish clear, achievable goals and collaboratively develop strategies to reach those goals. The client feels a sense of agency and ownership in the therapeutic process.
- Empathy and Understanding: The therapist demonstrates genuine empathy and understanding of the client’s experiences, fostering a sense of connection and validation.
- Positive Communication: Communication is open, honest, and respectful. Both therapist and client feel heard and understood. There is effective collaboration in problem-solving and decision-making.
- Agreement on Treatment Methods: Both therapist and client are in agreement regarding the types of therapeutic interventions used.
A client exhibiting active participation in sessions, expressing comfort with the therapist, and demonstrating progress toward their goals are all indications of a strong therapeutic alliance.
Q 13. How do you assess the client’s readiness for termination of therapy?
Assessing client readiness for termination involves a collaborative process that considers various factors. Premature termination can be detrimental, while prolonging therapy unnecessarily can also be counterproductive.
- Goal Attainment: Have the client’s primary goals been met? Has the client achieved sufficient progress to manage their challenges independently?
- Symptom Reduction: Have the client’s symptoms significantly reduced? Are they able to cope with challenges without significant distress?
- Improved Functioning: Is the client functioning better in their daily life – in relationships, work, and overall well-being?
- Client Self-Reflection: Does the client feel ready to end therapy? Are they confident in their ability to maintain progress and manage future challenges? This includes a realistic assessment of their support systems.
- Relapse Prevention Plan: A plan for managing potential setbacks or future challenges is in place.
The process typically involves regular discussions about progress and termination planning, gradually decreasing session frequency to facilitate a smooth transition.
Q 14. How do you handle situations where a client is resistant to treatment?
Resistance to treatment is a common occurrence and often reflects underlying anxieties or concerns about the therapeutic process. Understanding and addressing resistance is crucial for positive outcomes.
- Explore the Resistance: I gently inquire about the client’s resistance, attempting to understand the reasons behind it. This involves active listening and creating a safe space for the client to express their concerns.
- Collaborative Problem-Solving: We work together to address the underlying issues causing the resistance. This might involve adjusting the treatment plan, exploring alternative therapeutic approaches, or addressing any power dynamics or mistrust in the therapeutic relationship.
- Empathy and Validation: I validate the client’s feelings and experiences, ensuring they feel heard and understood. This helps foster trust and collaboration.
- Reframing Resistance: Resistance can sometimes be reframed as a positive sign of engagement. It indicates that the client is actively processing difficult emotions and experiences.
- Patience and Perseverance: Addressing resistance requires patience and persistence. It’s crucial to avoid pressuring the client or prematurely abandoning the therapeutic relationship.
For instance, if a client consistently avoids discussing a specific trauma, I might explore their reluctance by asking open-ended questions like, “It seems like it’s difficult to talk about this. Can you tell me more about what’s making it challenging?”
Q 15. Explain the importance of self-awareness in therapeutic relationship building.
Self-awareness is the cornerstone of effective therapeutic relationship building. It’s the ability to understand your own thoughts, feelings, biases, and how they might impact your interactions with clients. Without it, your personal experiences and perspectives could unintentionally influence the therapeutic process, hindering the client’s progress. For example, a therapist struggling with unresolved grief might unconsciously project those feelings onto a grieving client, potentially misinterpreting their behavior or offering unhelpful advice.
Developing self-awareness involves regular self-reflection, possibly through journaling, supervision, or personal therapy. It requires honestly confronting your strengths and weaknesses, recognizing potential blind spots, and understanding how your personal values might intersect with a client’s needs. This awareness allows for mindful engagement, ensuring the therapeutic space remains truly focused on the client’s well-being and not colored by the therapist’s unresolved issues.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage your own emotional responses in challenging therapeutic situations?
Managing emotional responses in challenging situations is crucial for maintaining professional boundaries and providing effective therapy. When faced with a difficult client interaction—for instance, a client expressing intense anger or sharing deeply distressing experiences—my first response is to utilize mindfulness techniques to center myself. This might involve deep breathing exercises or briefly stepping away to regain composure. I rely heavily on my training in countertransference, constantly reflecting on whether my emotional response is stemming from the client’s situation or my own unresolved issues.
Furthermore, maintaining professional boundaries is paramount. While empathy is essential, I ensure I don’t become emotionally entangled with the client. Supervision plays a vital role; discussing challenging cases with a supervisor provides an external perspective and helps ensure my emotional responses are managed appropriately and do not compromise the therapeutic process. Self-care practices, including adequate rest and engaging in activities that promote well-being, are also integral to maintaining resilience.
Q 17. What are your strategies for ensuring client safety and well-being?
Client safety and well-being are my top priorities. My strategies include a thorough assessment of risk factors at the outset of therapy, including suicidality, self-harm, and potential harm to others. This assessment informs the treatment plan and helps identify necessary interventions.
If a client expresses thoughts of self-harm or harming others, I have clear protocols for immediate action. This involves direct questioning to assess the level of risk, creating a safety plan collaboratively with the client, and, when necessary, contacting appropriate authorities such as emergency services or the client’s family, always adhering to mandated reporting laws. Regular monitoring of the client’s emotional state and progress throughout therapy is also critical to detecting and addressing any emerging safety concerns. Maintaining open communication with the client fosters a safe therapeutic space where they feel comfortable sharing their concerns without fear of judgment.
Q 18. Describe your experience with different therapeutic modalities and how you integrate them.
My therapeutic approach is integrative, drawing upon various modalities to tailor treatment to each client’s unique needs. I have experience with Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and psychodynamic approaches. CBT helps clients identify and modify maladaptive thought patterns and behaviors. DBT is particularly effective for individuals struggling with emotion regulation and interpersonal difficulties. Psychodynamic therapy helps explore unconscious patterns and relationships to gain insight into current challenges.
Integration involves thoughtfully selecting techniques from different modalities to create a holistic treatment plan. For instance, I might use CBT strategies for managing anxiety alongside DBT skills for interpersonal effectiveness, while also incorporating psychodynamic insights to understand the root causes of the client’s issues. The key is flexibility and tailoring the therapeutic approach to best suit the individual client, rather than rigidly adhering to a single modality.
Q 19. How do you utilize feedback to improve your therapeutic relationships?
Feedback is vital for continuous improvement in therapeutic relationships. I actively solicit feedback from clients throughout the therapeutic process. This can be done formally through structured questionnaires or informally through open-ended questions during sessions. I also seek feedback from supervisors, peers, and through self-reflection.
Constructive criticism, whether from clients or supervisors, is viewed as an opportunity for growth. For example, if a client comments on feeling unheard, I would reflect on my communication style, perhaps recognizing a need to actively listen more attentively or to adjust the pace of the session. I document feedback and use it to refine my techniques and approach, ensuring I’m providing the most effective and sensitive care possible. Regular supervision discussions allow for systematic analysis of feedback and development of new strategies.
Q 20. How do you document client interactions and progress notes ethically and accurately?
Ethical and accurate documentation is crucial for maintaining client confidentiality, ensuring continuity of care, and meeting legal and professional standards. My documentation includes detailed progress notes that accurately reflect client sessions, focusing on key themes, client’s presenting problems, and progress made toward established goals. I use clear and concise language, avoiding jargon, and ensuring the notes are objective and factual.
Confidentiality is paramount. All records are securely stored and access is restricted to authorized personnel only, strictly adhering to HIPAA guidelines (or relevant local regulations). Client information is never shared without explicit consent, except in mandated reporting situations. I regularly review my documentation practices to ensure compliance with ethical guidelines and legal requirements, including maintaining accurate timestamps and proper record-keeping procedures. Maintaining meticulous records is not only ethically sound but also essential for providing excellent and safe client care.
Q 21. Describe a time you had to make a difficult decision regarding a client’s treatment plan.
One particularly challenging case involved a client struggling with severe depression and suicidal ideation. Initially, the client was ambivalent towards treatment, making it difficult to establish a strong therapeutic alliance. After several sessions of limited engagement, I had to decide whether to continue with the current approach or explore alternative strategies that might better engage the client.
After careful consideration, including consultation with my supervisor and thorough assessment of the client’s risk level, I decided to incorporate motivational interviewing techniques to better understand their ambivalence and collaboratively explore their readiness for change. This involved shifting from a direct, problem-focused approach to a more collaborative and empathetic one. Fortunately, this change led to increased engagement and a more positive therapeutic relationship, which ultimately helped the client navigate their suicidal thoughts and find more hope.
Q 22. How do you maintain professional boundaries while still creating a supportive environment?
Maintaining professional boundaries while fostering a supportive environment is a delicate balancing act. It’s about creating a safe and trusting space for clients to explore their thoughts and feelings without blurring the lines of the professional relationship. Think of it like this: you’re a guide, not a friend. You offer support and empathy, but you remain objective and focused on the client’s therapeutic goals.
Clear Communication: From the outset, I clearly define the boundaries of the therapeutic relationship. This includes discussing session times, cancellation policies, methods of communication, and limits to self-disclosure (on my part).
Maintaining Professional Demeanor: I avoid dual relationships – for example, I wouldn’t socialize with a client outside of therapy. I also maintain appropriate physical distance and avoid overly casual language or behavior.
Self-Awareness: Recognizing my own emotional responses and potential countertransference (my unconscious feelings towards the client) is crucial. Regular supervision helps me monitor this and ensure I am maintaining appropriate professional distance.
Ethical Decision-Making: If a situation arises that blurs the boundaries, I consult with supervisors or colleagues to ensure ethical practice and client well-being.
For example, if a client invites me to their birthday party, I would kindly but firmly decline, explaining that maintaining professional boundaries is essential for their therapy.
Q 23. What is your understanding of informed consent and how do you obtain it from clients?
Informed consent is the cornerstone of ethical practice. It means clients understand the nature of therapy, its potential benefits and risks, their rights, and responsibilities. Obtaining informed consent is an ongoing process, not a one-time event.
Initial Session: I spend considerable time in the first session explaining my approach, the therapeutic process, fees, confidentiality limits (e.g., mandated reporting for child abuse), and the client’s right to withdraw from therapy at any time.
Written Documents: I provide clients with a written informed consent form that outlines all the essential information discussed. They have the opportunity to review it and ask questions before signing.
Ongoing Dialogue: Informed consent isn’t static. Throughout the therapeutic process, I regularly check in with clients to ensure they are still comfortable with the direction of therapy and any changes that may occur.
Capacity Assessment: I ensure the client has the capacity to understand the information and make informed decisions. If there are concerns about capacity, I’ll consult with other professionals or obtain necessary legal authorizations.
For example, if a client expresses discomfort with a specific aspect of our therapeutic approach, I will adjust accordingly and re-establish informed consent. If a client seems overwhelmed by information, I would break down complex concepts into simpler terms.
Q 24. How do you effectively collaborate with other professionals involved in a client’s care?
Effective collaboration with other professionals is crucial for holistic client care. This involves open communication, mutual respect, and shared goals.
Information Sharing: I use HIPAA-compliant methods to share relevant information with other professionals involved in the client’s care, such as doctors, psychiatrists, or social workers. I only share information that is directly relevant to their involvement and with the client’s consent (unless legally mandated).
Regular Communication: I schedule regular meetings or calls with other professionals to discuss the client’s progress, concerns, and treatment plans. This collaborative approach allows us to create a cohesive and effective care plan.
Respectful Communication: I listen attentively to the perspectives of other professionals, valuing their expertise and acknowledging their contributions to the client’s overall well-being.
Case Conferences: Participating in case conferences, when appropriate, allows me to gain broader perspectives on the client’s needs and treatment goals.
For instance, if a client is struggling with substance abuse, I collaborate closely with their psychiatrist to coordinate medication management and therapeutic interventions. Open communication prevents duplicating efforts and maximizes therapeutic effectiveness.
Q 25. Describe your experience with crisis intervention in the therapeutic context.
Crisis intervention is a critical skill in therapeutic practice. It involves providing immediate support to clients experiencing acute emotional distress, preventing harm to themselves or others.
Assessment: In a crisis, my first priority is to assess the client’s immediate safety and the nature of the crisis. This involves asking direct questions about suicidal thoughts, self-harm behaviors, or threats to others.
Emotional Support: I offer empathy, validation, and active listening to help the client feel heard and understood. My goal is to reduce their immediate distress and instill a sense of hope.
Collaboration: If the client is at imminent risk of harm, I may need to collaborate with emergency services (911), hospital staff, or other support systems. This involves ensuring a safe transfer of care and following established protocols.
Safety Planning: Once the immediate crisis has subsided, I work with the client to develop a safety plan for future crises, including identifying warning signs, coping mechanisms, and support resources.
For example, if a client expresses suicidal ideation, I would immediately assess the level of risk, provide emotional support, and involve emergency services if necessary. We would then collaborate on a safety plan to help prevent future crises.
Q 26. How do you ensure client autonomy within the therapeutic process?
Client autonomy is essential, meaning clients have the right to make their own choices about their treatment. This involves empowering them to participate actively in the therapeutic process and respecting their decisions, even if I disagree with them.
Shared Decision-Making: I work collaboratively with clients to set their goals and develop a treatment plan. This is not a directive process; rather, it’s a partnership where I offer my expertise while respecting their choices.
Providing Options: I offer clients a range of options within the therapeutic process, allowing them to choose the approaches that feel most comfortable and effective for them.
Respecting Boundaries: I respect clients’ decisions to change their treatment plan, discontinue therapy, or refuse certain interventions.
Empowerment: I focus on empowering clients to take ownership of their therapeutic journey and develop the skills to make informed decisions about their lives.
For example, if a client wants to focus on a particular issue that differs from my initial assessment, I will adjust the treatment plan accordingly, prioritizing their autonomy. Ultimately, the therapeutic process is guided by their choices and needs.
Q 27. How do you recognize and address potential biases in your therapeutic work?
Recognizing and addressing biases is a crucial part of ethical and effective practice. We all hold unconscious biases that can influence our perceptions and interactions. Addressing this requires ongoing self-reflection and awareness.
Self-Reflection: I regularly engage in self-reflection, examining my own values, beliefs, and experiences to identify potential biases that may impact my work.
Supervision: Regular supervision allows me to discuss my clinical work with a qualified supervisor, who can help me identify and address any potential biases in my interactions with clients.
Cultural Humility: I strive to cultivate cultural humility, acknowledging that I may not fully understand the experiences of individuals from different cultural backgrounds. I actively listen and learn from my clients to gain a deeper understanding of their perspectives.
Continuing Education: I consistently engage in continuing education to stay current on best practices related to diversity, equity, and inclusion. This enhances my ability to work effectively with a diverse range of clients.
For instance, if I notice myself making assumptions about a client based on their race or socioeconomic status, I would pause, reflect on my biases, and strive to approach the situation with greater empathy and understanding. Seeking supervision might help in this process.
Q 28. Explain your approach to utilizing technology in the therapeutic relationship (e.g., telehealth).
Technology can be a valuable tool in enhancing the therapeutic relationship, particularly through telehealth. However, it’s essential to use it ethically and effectively.
Confidentiality: I use HIPAA-compliant platforms that provide secure communication channels to protect client confidentiality. This includes understanding and complying with data privacy regulations.
Informed Consent: Before using technology, I obtain informed consent from clients, ensuring they understand the platform’s limitations, the risks involved (e.g., potential tech issues), and the security measures in place.
Technology Limitations: I am aware of the limitations of telehealth and adapt my approach accordingly. For example, I might need to make adjustments for clients with limited technological access or those who prefer in-person sessions.
Professional Boundaries: Even in a virtual setting, I maintain professional boundaries. This includes avoiding informal communication outside of scheduled sessions and adhering to ethical guidelines.
For example, I would make sure my virtual office is private and free from distractions to create a safe and professional environment for online sessions. If a client has a technology issue, I offer alternative methods of communication or reschedule the session as needed.
Key Topics to Learn for Therapeutic Relationship Building Interview
- Empathy and Active Listening: Understanding and responding to clients’ emotions effectively. Practical application: Describe a situation where you demonstrated deep empathy and how it fostered trust.
- Building Rapport and Trust: Establishing a safe and collaborative therapeutic space. Practical application: Explain strategies you use to build rapport with diverse clients, considering cultural sensitivity.
- Setting Boundaries and Maintaining Professionalism: Defining roles and responsibilities within the therapeutic relationship. Practical application: Describe how you handle challenging client behaviors while maintaining professional boundaries.
- Cultural Competence and Sensitivity: Recognizing and respecting diverse cultural backgrounds and beliefs. Practical application: Provide an example of how you adapted your approach to meet the specific needs of a client from a different cultural background.
- Communication Styles and Techniques: Utilizing effective verbal and nonverbal communication to facilitate the therapeutic process. Practical application: Discuss your preferred communication style and how you adapt it to different client needs.
- Ethical Considerations: Understanding and applying ethical principles in therapeutic practice. Practical application: Describe a situation where you had to address an ethical dilemma and how you resolved it.
- Working Collaboratively with a Team: Effective communication and coordination with colleagues and supervisors. Practical application: Describe your experience working effectively within a multidisciplinary team.
- Self-Awareness and Reflection: Recognizing your own biases and limitations and how they impact the therapeutic relationship. Practical application: Explain how you engage in self-reflection to improve your therapeutic practice.
Next Steps
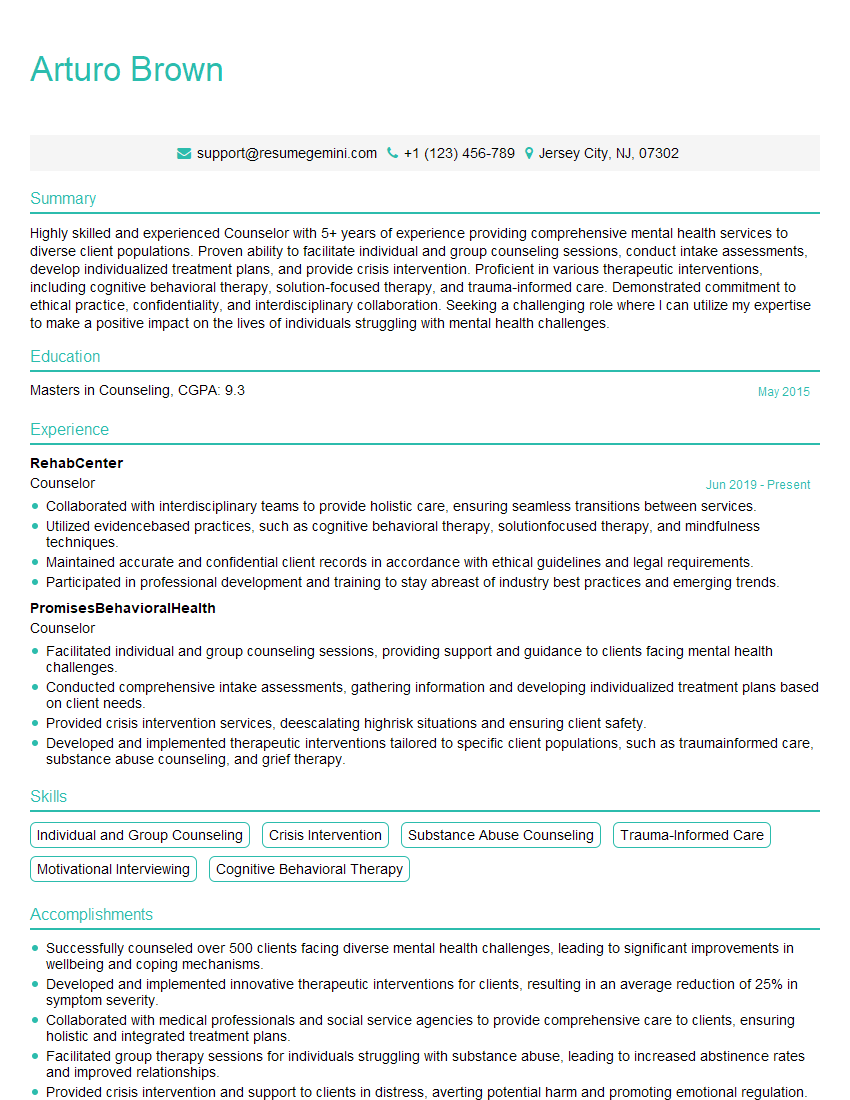
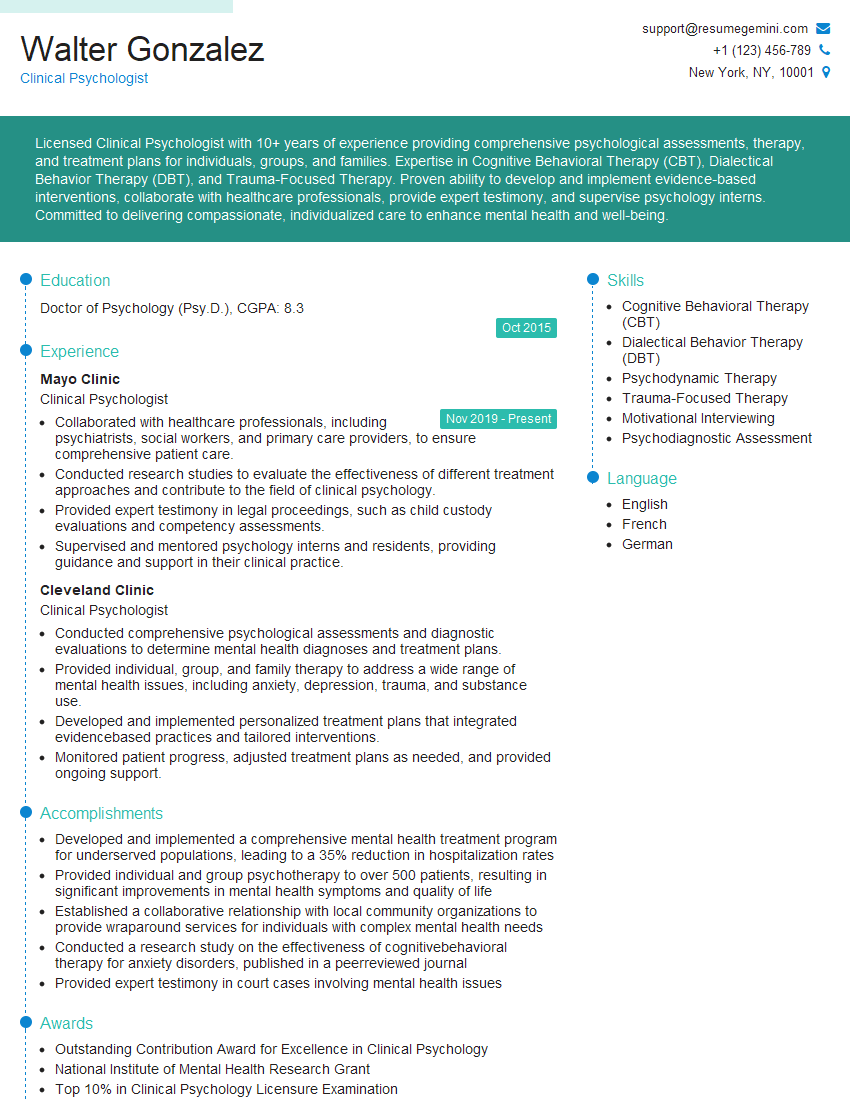
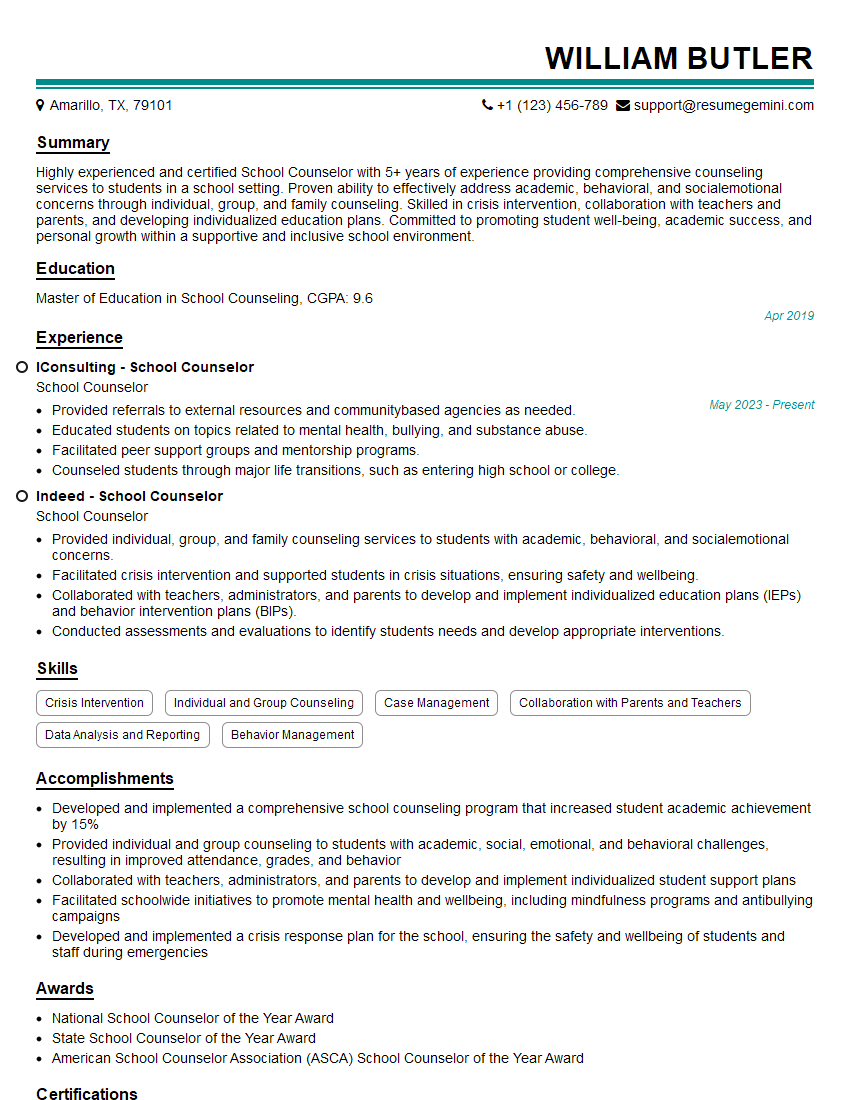
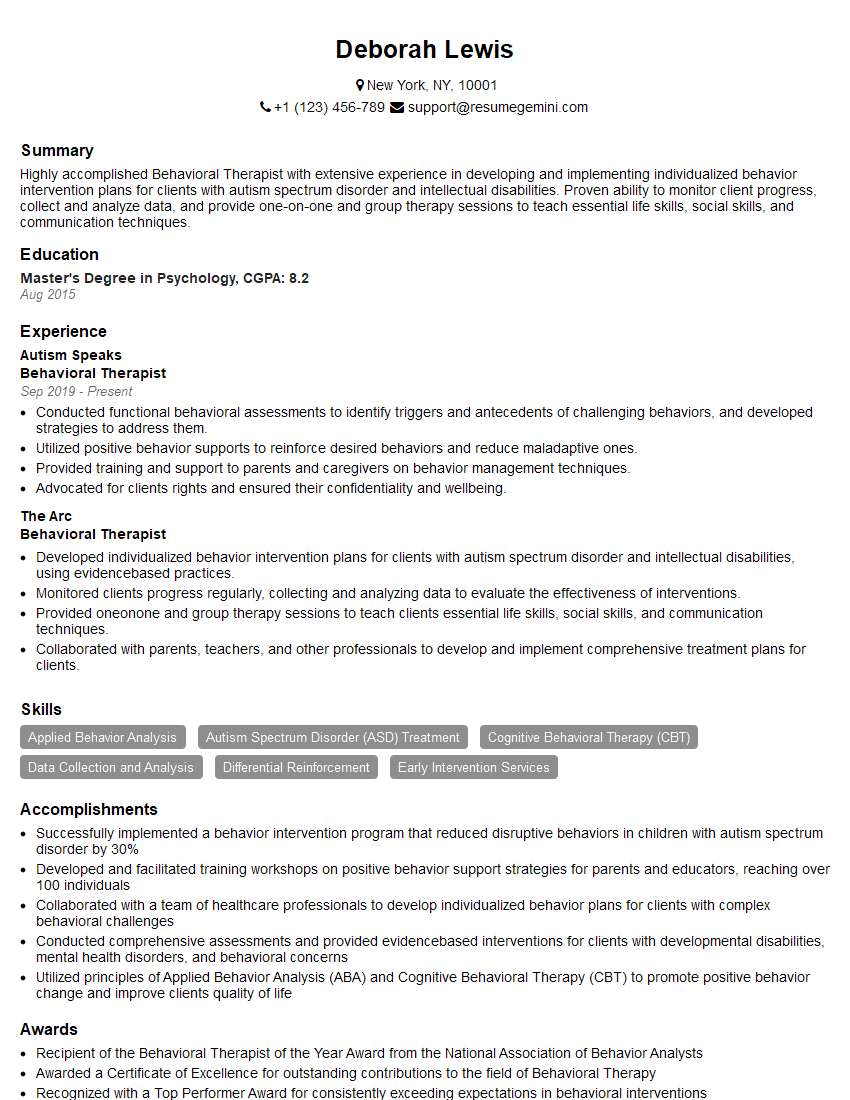
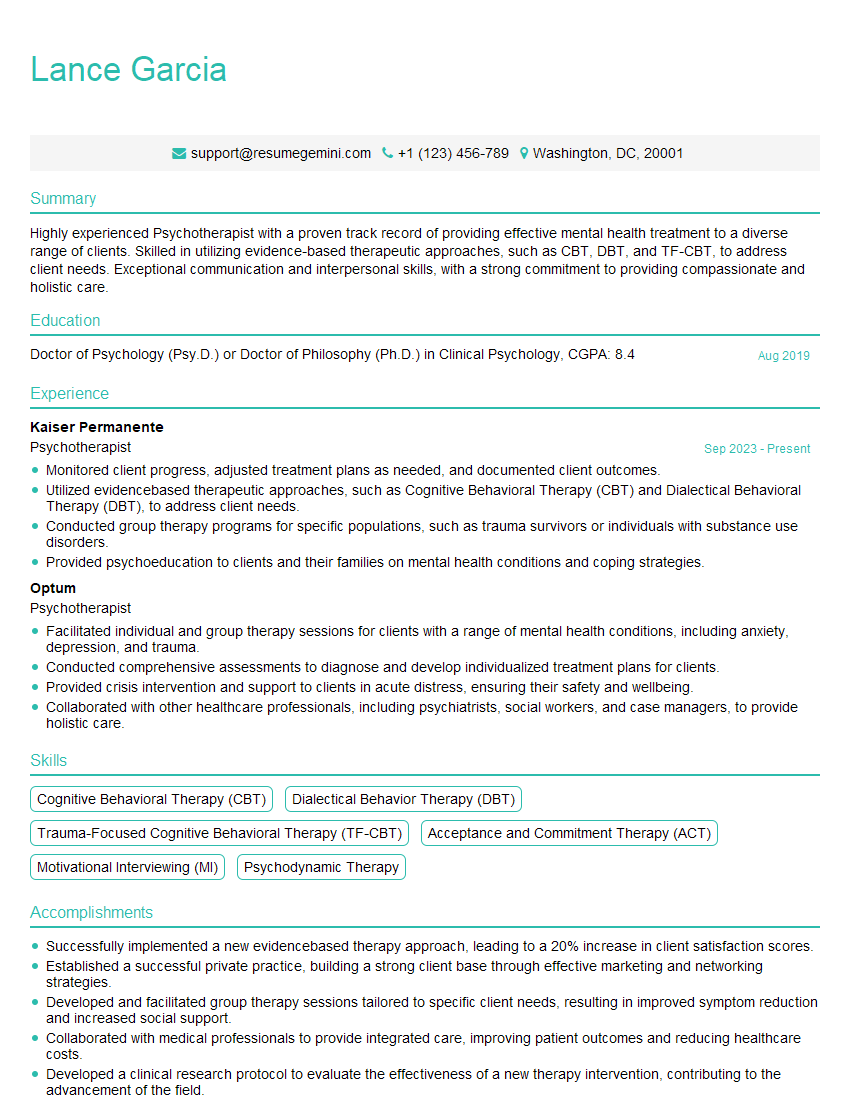
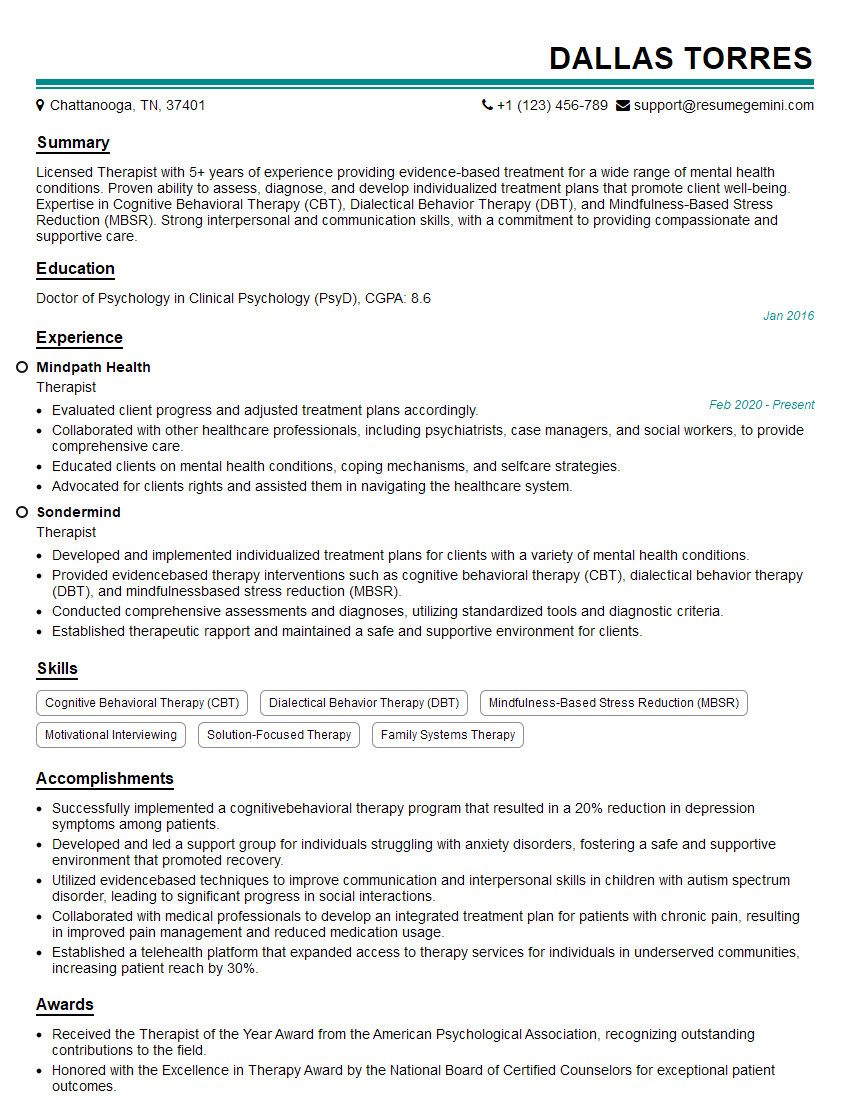
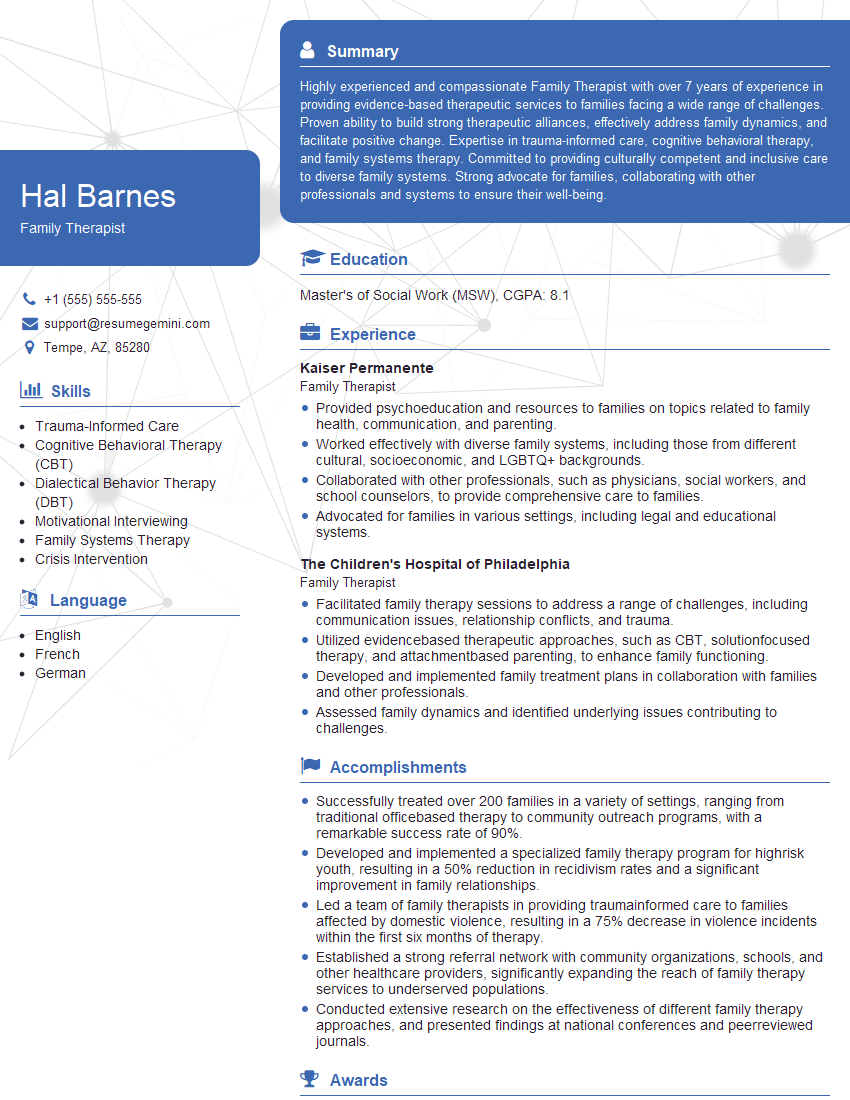
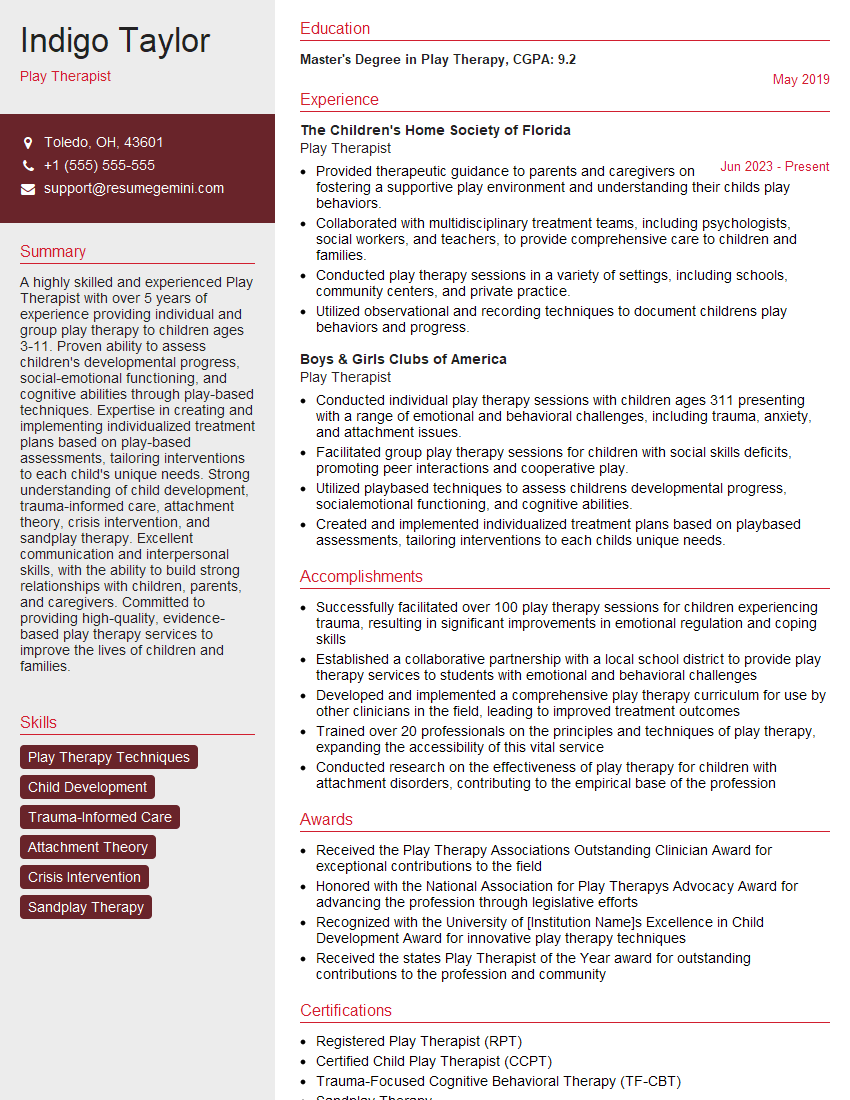
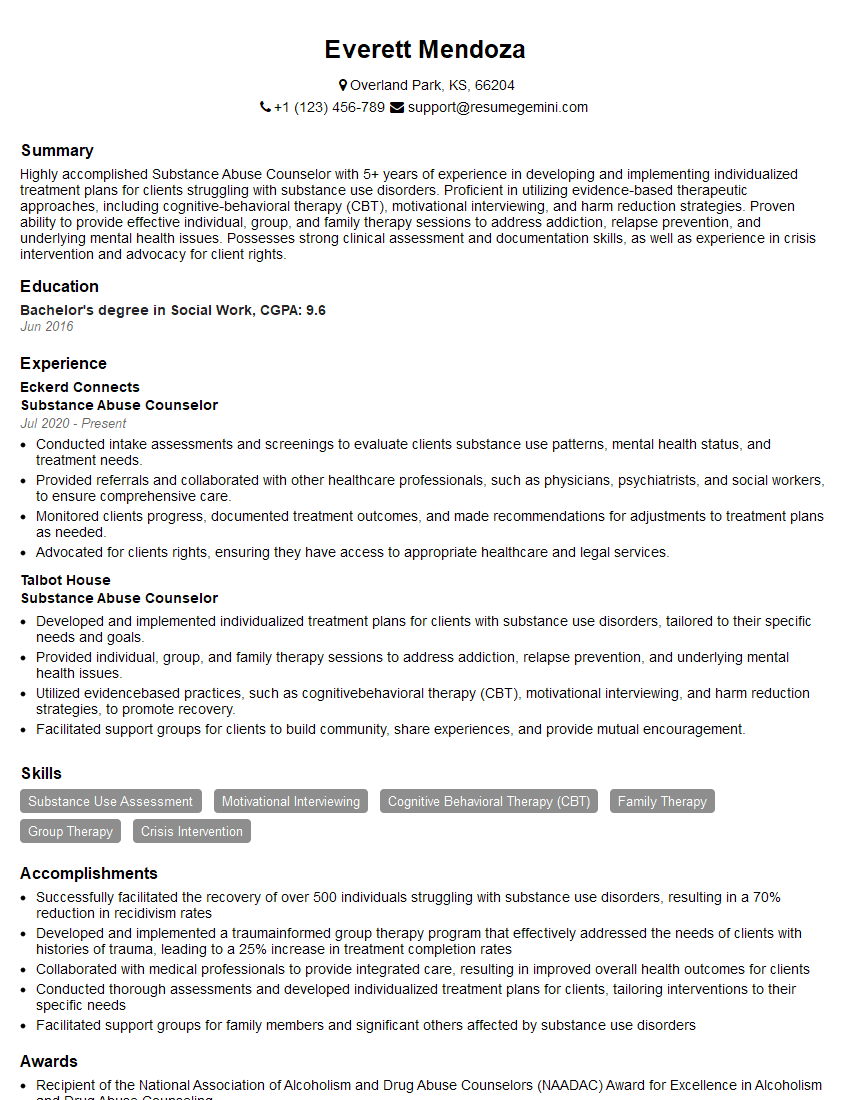
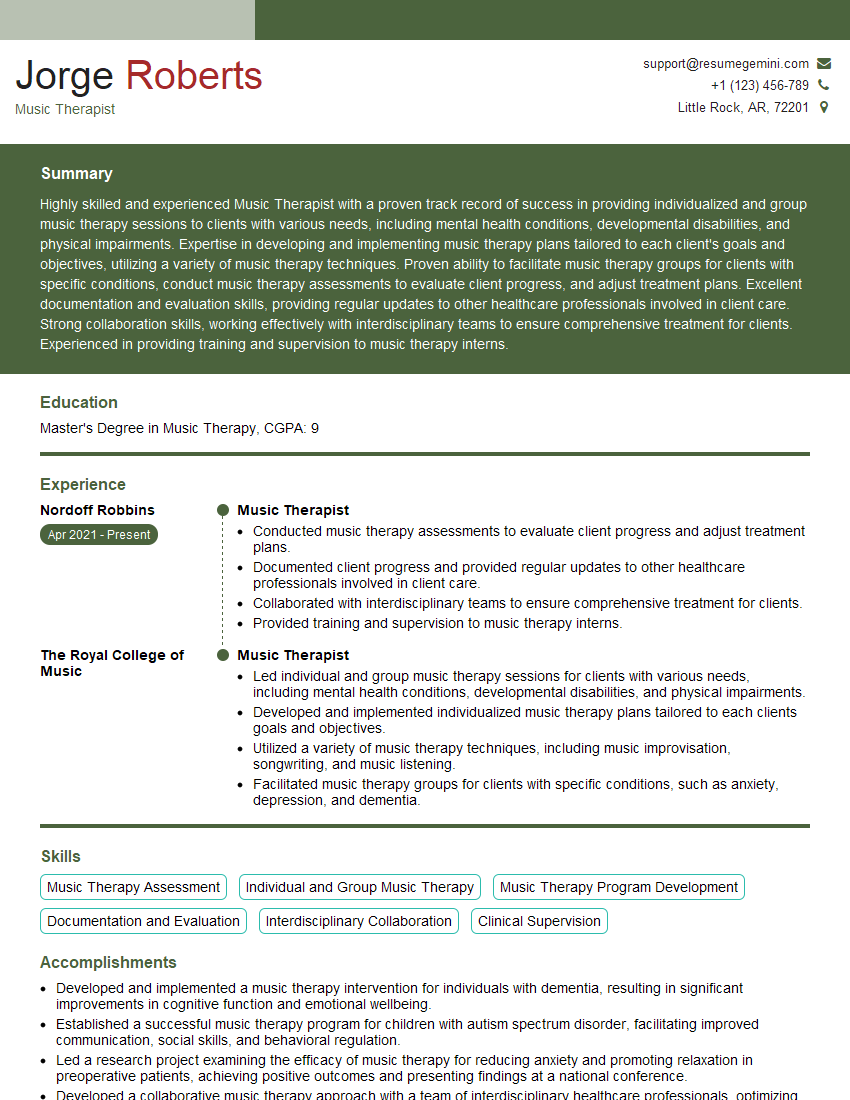
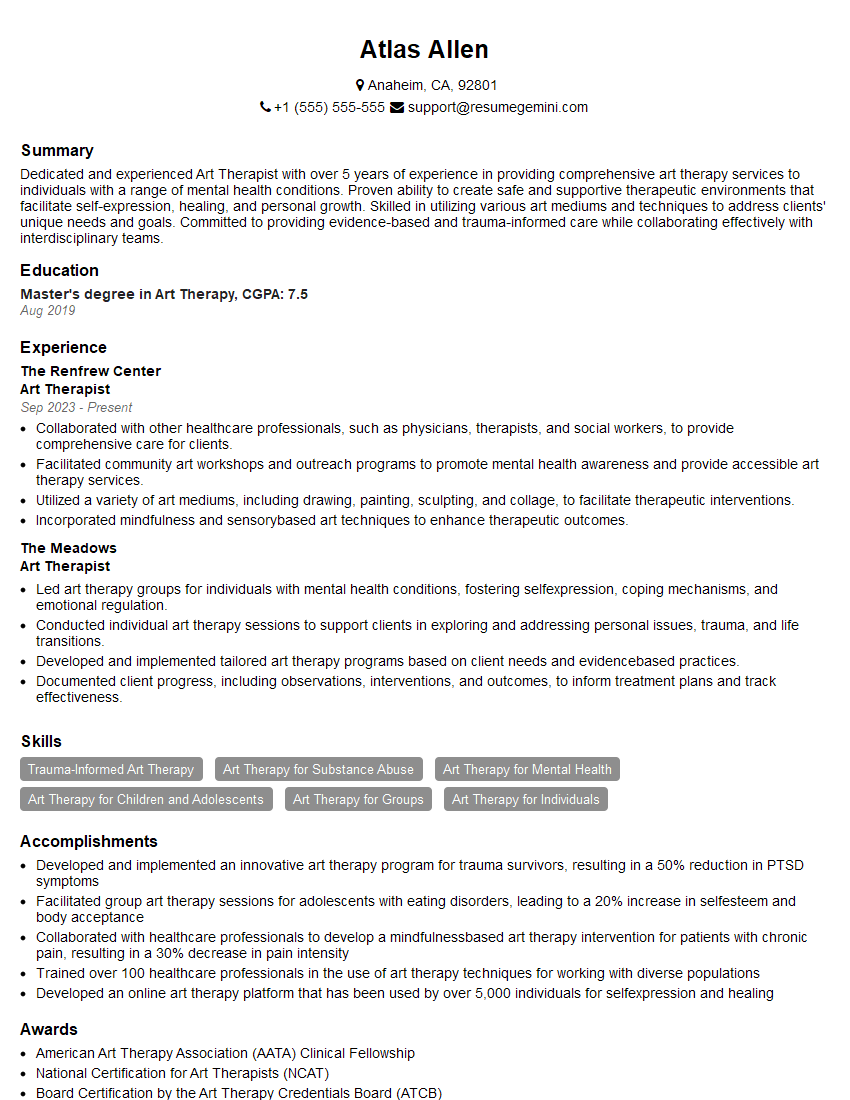
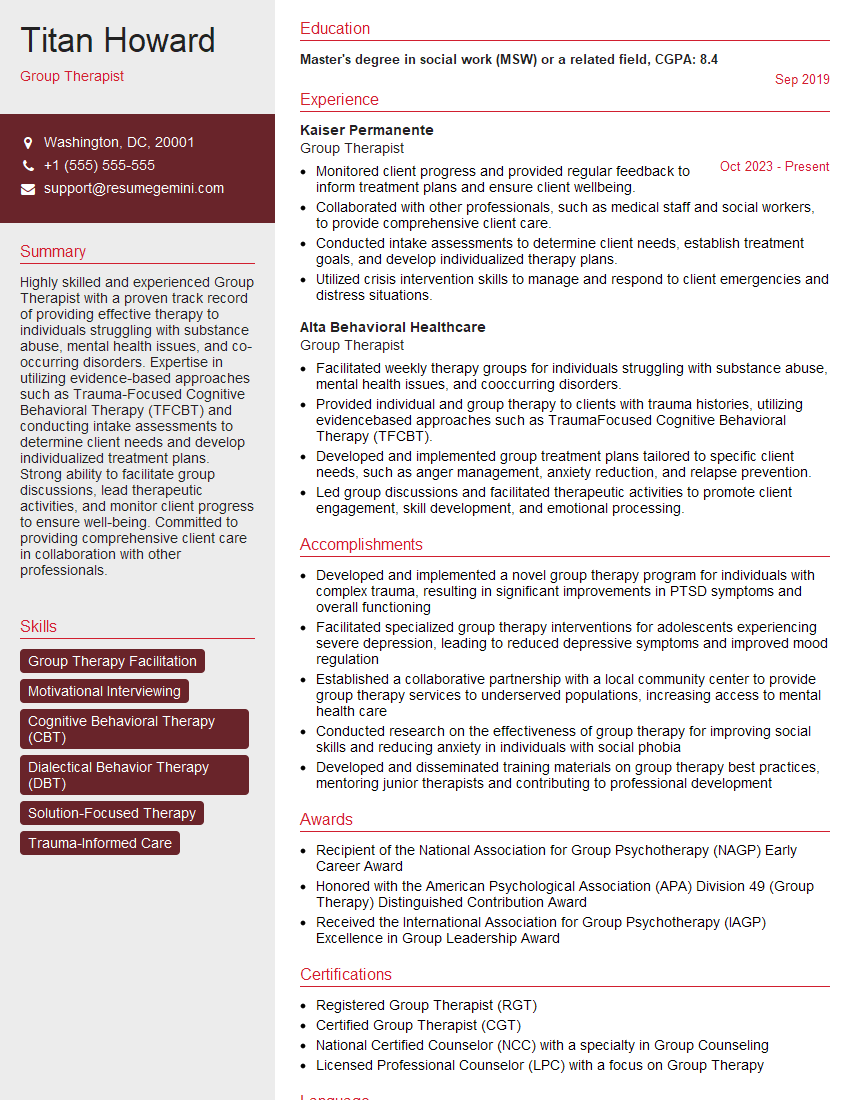
Mastering therapeutic relationship building is crucial for career advancement in this field. It demonstrates your ability to connect with clients, build trust, and achieve positive outcomes. To significantly improve your job prospects, crafting an ATS-friendly resume is paramount. This ensures your qualifications are effectively highlighted to potential employers. We strongly recommend using ResumeGemini to build a professional and impactful resume. ResumeGemini provides valuable tools and resources, including examples of resumes specifically tailored to showcasing expertise in Therapeutic Relationship Building, to help you stand out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good