The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Ultrasound-Guided Procedures interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Ultrasound-Guided Procedures Interview
Q 1. Describe the principles of ultrasound image formation.
Ultrasound image formation relies on the principle of piezoelectricity. A transducer, containing piezoelectric crystals, emits high-frequency sound waves into the body. These waves travel through different tissues, reflecting back to the transducer at varying intensities depending on the acoustic impedance of the tissue boundaries. The transducer then converts these reflected waves back into electrical signals. These signals are processed by the ultrasound machine, creating a grayscale image. Denser tissues like bone reflect more sound, appearing bright (hyperechoic), while less dense tissues like fluid reflect less, appearing dark (hypoechoic or anechoic).
Think of it like shining a flashlight in a dark room with objects of different reflectivity. A mirror will reflect a lot of light back, while a dark cloth will absorb more and reflect less. The ultrasound machine “sees” these reflections to build a picture.
The time it takes for the sound waves to return determines the depth of the structure, creating a two-dimensional image in real-time. This allows us to visualize internal organs, blood vessels, and needles during procedures.
Q 2. Explain the different types of ultrasound transducers and their applications.
Ultrasound transducers come in various types, each designed for specific applications. The choice depends on the target tissue and the procedure being performed:
- Linear Transducers: High frequency, excellent resolution for superficial structures like skin, breast, and thyroid. They provide a rectangular image and are ideal for guiding superficial procedures.
- Curvilinear Transducers: Lower frequency, deeper penetration suitable for abdominal, pelvic, and musculoskeletal imaging. They offer a broader field of view and are used in many deeper procedures.
- Phased Array Transducers: Used for cardiac imaging and often intercostal views because of their ability to scan from a variety of angles. Good for visualizing moving structures.
- Endocavitary Transducers: Designed for internal use (e.g., transvaginal, transrectal) and are excellent for detailed visualization of pelvic organs. They are specialized for specific locations.
For example, a linear transducer is best for a superficial biopsy, while a curvilinear transducer would be more appropriate for a guided liver biopsy.
Q 3. How do you ensure patient safety during ultrasound-guided procedures?
Patient safety is paramount in ultrasound-guided procedures. This involves a multi-faceted approach:
- Proper Patient Identification and Consent: Verifying the patient’s identity and obtaining informed consent is crucial to ensure the correct procedure is performed on the intended patient.
- Sterile Technique: Maintaining sterile technique is critical, particularly for invasive procedures, to minimize the risk of infection.
- Image Optimization: Obtaining high-quality images is essential for accurate needle guidance and minimizing the risk of complications. Proper gain, depth, and focus settings are key.
- Continuous Monitoring: Observing the patient’s vital signs throughout the procedure helps to identify any adverse reactions or complications early.
- Needle Visualization: Using ultrasound to precisely guide the needle avoids inadvertent puncture of vital structures like blood vessels or nerves.
- Post-procedural Care: Providing appropriate post-procedural instructions and follow-up care is important for minimizing the risk of complications and ensuring patient recovery.
We always employ ALARA (As Low As Reasonably Achievable) principles for radiation exposure, even though ultrasound itself is non-ionizing radiation.
Q 4. What are the common complications associated with ultrasound-guided procedures and how are they managed?
Complications associated with ultrasound-guided procedures are relatively rare but can include:
- Hematoma: Bleeding at the puncture site. This is managed by applying pressure and monitoring for significant blood loss.
- Infection: Risk is minimized with sterile technique. Treatment involves antibiotics and wound care.
- Pneumothorax: Collapsed lung (most commonly associated with lung biopsies). Managed with chest tube insertion if needed.
- Nerve or Vessel Damage: Injury to nerves or vessels can occur, leading to pain, numbness, or bleeding. Often managed conservatively with observation, but in some cases surgical intervention is necessary.
- Organ Damage: Rare, but possible with incorrect needle placement. The management is situation-specific and can range from observation to surgical repair.
Experienced practitioners minimize complications through careful patient selection, proper image interpretation, and precise needle guidance techniques. A thorough understanding of the patient’s anatomy, including potential variations, is critical.
Q 5. Describe your experience with needle guidance techniques (e.g., in-plane, out-of-plane).
Needle guidance techniques primarily involve in-plane and out-of-plane approaches. In in-plane guidance, the needle is advanced along the ultrasound beam, allowing for direct visualization of the needle tip throughout its trajectory. This is often preferred for its ease of visualization and control. Out-of-plane guidance involves advancing the needle perpendicular to the ultrasound beam. While requiring more experience to master, it allows for accessing targets that are more difficult to reach using the in-plane technique.
I have extensive experience in both. For instance, I routinely use in-plane techniques for thyroid biopsies due to the superficial nature and the need for high precision. However, for some deeper procedures like paracentesis, an out-of-plane approach may be more practical. It’s crucial to choose the optimal technique based on the target anatomy, access route, and patient factors.
Q 6. How do you assess the quality of an ultrasound image?
Assessing ultrasound image quality is crucial for accurate diagnosis and procedure guidance. Key factors include:
- Acoustic Window: A good acoustic window (the area where sound waves can effectively penetrate) is essential. Excess gas or air can obscure the image.
- Depth and Penetration: The image should show adequate penetration depth to visualize the target structure fully.
- Resolution: The image should have good spatial resolution to distinguish between different tissues.
- Artifacts: Recognizing and understanding common artifacts, like shadowing, enhancement, or reverberation, is vital for accurate interpretation. These artifacts can sometimes mask or distort the underlying anatomy.
- Tissue Characterization: Being able to differentiate between different tissue types (e.g., solid, cystic, or fluid-filled) based on their echogenicity is important.
An example of poor image quality might be an ultrasound of the abdomen obscured by bowel gas. In such a case, I would try changing the patient’s position or using different ultrasound settings or even a different type of transducer.
Q 7. Explain the use of Doppler ultrasound in guided procedures.
Doppler ultrasound uses the Doppler effect to measure the velocity and direction of blood flow within vessels. In guided procedures, Doppler provides crucial information:
- Vessel Identification and Localization: Doppler helps visualize and confirm the presence of blood vessels before needle insertion, avoiding accidental puncture.
- Guidance of Vascular Access: In procedures involving vascular access, like central line placement, Doppler ensures accurate needle placement within the target vessel.
- Assessment of Blood Flow: Assessing the flow pattern can help determine the patency of a vessel or detect stenosis (narrowing).
- Monitoring of Needle Position: During procedures, Doppler can help monitor the position of the needle in relation to blood vessels to prevent injury.
For example, during a central line insertion, Doppler helps confirm that the needle tip is correctly positioned within the vessel lumen before injecting the contrast medium.
Q 8. How do you handle unexpected findings during a procedure?
Unexpected findings during an ultrasound-guided procedure are a common occurrence. My approach is systematic and prioritizes patient safety. First, I carefully reassess the ultrasound images, comparing them to previous scans if available, to determine the nature of the unexpected finding. This might involve adjusting the transducer frequency, angle, or depth to obtain a clearer image. I’ll document the finding meticulously, including its location, size, and characteristics.
Then, I carefully consider the implications of the finding for the planned procedure. Does it require a modification to the procedure? Does it necessitate halting the procedure for further evaluation, such as a consultation with a radiologist or another specialist? For instance, if I encounter an unexpected vascular structure during a biopsy, I would immediately adjust the needle trajectory to avoid it.
Communication is key. I always inform the patient and their family about the unexpected finding in clear and understandable terms, explaining the next steps and addressing any concerns they may have. Finally, I incorporate all findings and actions taken into the patient’s medical record. Patient safety and informed consent remain paramount throughout this process.
Q 9. What is your experience with different types of ultrasound contrast agents?
I have experience with various ultrasound contrast agents, both gas-based and microbubble-based. Gas-based agents, like sulfur hexafluoride, are generally used less frequently now due to safety concerns. Microbubble agents are now the standard. They are composed of small gas bubbles encapsulated in a shell that is usually composed of a phospholipid bilayer. These agents enhance the ultrasound signal, increasing the contrast between different tissue types and improving visualization of blood flow.
My experience includes using microbubble contrast agents for various applications including: enhancing the visualization of liver lesions during biopsy, assessing the perfusion of a transplanted kidney and identifying subtle vascular abnormalities in various organs. It’s crucial to understand the different properties of these agents – their persistence in the circulation, potential side effects (though generally rare), and contraindications (such as severe pulmonary hypertension or allergies). Choosing the right agent depends on the specific procedure and the patient’s clinical status.
Q 10. Describe your knowledge of sterile technique and infection control protocols.
Strict adherence to sterile technique and infection control protocols is non-negotiable in ultrasound-guided procedures. This involves a multi-step process. Before any procedure, I ensure a thorough hand hygiene with an alcohol-based hand rub. The ultrasound transducer is meticulously disinfected with a high-level disinfectant according to the manufacturer’s instructions before and after each use.
The procedure site is prepared using a sterile technique, including cleansing with an antiseptic solution. Sterile gloves, drapes, and needles are always utilized. Throughout the procedure, I remain vigilant in maintaining a sterile field, avoiding contamination. Proper disposal of sharps and medical waste is critically important to prevent cross-contamination. I am also familiar with and consistently apply the guidelines provided by the CDC and other relevant organizations to minimize infection risk. The principles of asepsis and barrier techniques are ingrained in my practice. Post-procedural care includes monitoring the patient for signs of infection and providing appropriate wound care instructions.
Q 11. How do you manage patient anxiety during procedures?
Managing patient anxiety is a significant part of my role. I believe in establishing a trusting relationship built on clear communication and empathy. Before starting any procedure, I take the time to explain the process in detail, using simple language and answering all questions patiently. I show the patient the ultrasound images and explain what I am seeing, demystifying the procedure.
I offer reassurance throughout the procedure, explaining each step and providing positive feedback. Many patients find deep breathing techniques or distraction methods helpful. I may suggest these, or simply offer a comforting presence. In cases of significant anxiety, pre-procedural anxiolytic medication could be considered after consultation with the anesthesiologist. The goal is to create a calm and supportive environment to reduce stress and optimize the patient’s experience.
Q 12. Explain your understanding of anatomical landmarks relevant to ultrasound-guided procedures.
Accurate identification of anatomical landmarks is fundamental to safe and effective ultrasound-guided procedures. My knowledge encompasses a wide range of anatomical structures, depending on the target region. For example, in a liver biopsy, key landmarks include the costal margin, diaphragm, and major vascular structures such as the portal vein and hepatic veins. In a musculoskeletal procedure, bony landmarks and muscle planes provide crucial guidance.
I utilize a combination of surface anatomy palpation and ultrasound imaging to precisely identify these landmarks. The understanding of the normal anatomical variation is crucial; recognizing potential pitfalls such as anatomical variations is vital to avoid complications. For instance, in the abdomen, the position of organs can vary significantly depending on body habitus and respiratory phase. I constantly compare the ultrasound image with my knowledge of the underlying anatomy to ensure accurate needle placement.
Q 13. Describe your experience with various types of biopsy procedures.
My experience encompasses a variety of biopsy techniques including fine-needle aspiration (FNA), core needle biopsy, and large-core needle biopsy. FNA is often used for cytological evaluation of lesions, while core needle biopsies provide tissue samples for histopathological examination. The choice of technique depends on the size, location, and nature of the lesion, as well as the clinical question.
I’m proficient in using different needle gauges and biopsy guns. I’ve performed biopsies in various organs and locations including the liver, kidney, thyroid, breast, and muscles. Safety and efficiency are paramount considerations. Post-procedure, I carefully monitor the patient for bleeding or other complications. I thoroughly document the procedure and the results obtained. The patient’s clinical presentation and imaging findings are carefully reviewed in deciding the biopsy technique.
Q 14. How do you interpret ultrasound images to guide needle placement?
Interpreting ultrasound images to guide needle placement is a complex skill requiring a high degree of spatial reasoning and understanding of ultrasound physics. I use a combination of anatomical knowledge and image interpretation techniques. I begin by identifying the target lesion and surrounding anatomical structures. I assess the lesion’s characteristics, such as its size, shape, echogenicity, and vascularity.
Once the target is identified, I plan the optimal needle trajectory, considering factors such as the depth, angle, and path of least resistance to avoid vital structures. I use the ultrasound real-time imaging to constantly monitor the needle’s progress, ensuring it stays on the planned path. The ability to visualize the needle tip in real-time is crucial for accurate needle placement and minimizes the risk of complications. The process requires a combination of technical skill, anatomical knowledge, and clinical judgment.
Q 15. What are your strategies for optimizing image quality during a procedure?
Optimizing ultrasound image quality is crucial for accurate and safe procedures. It’s like having a clear map before embarking on a journey – a blurry image can lead to errors. My strategies involve a multi-faceted approach focusing on patient positioning, transducer selection, and image adjustments.
Patient Positioning: Proper patient positioning is paramount. For example, in a shoulder injection, ensuring the arm is abducted and externally rotated to optimally visualize the target structures is essential. Suboptimal positioning can lead to acoustic shadowing and poor visualization.
Transducer Selection: Choosing the right transducer is like selecting the right tool for a job. Higher frequency transducers offer better resolution for superficial structures (e.g., a 15 MHz linear array for nerve blocks in the hand), while lower frequency transducers penetrate deeper (e.g., a 5 MHz curved array for hip injections). I carefully consider the depth and target anatomy before selecting the transducer.
Image Adjustments: Ultrasound machines offer several tools to enhance image quality. These include adjusting gain (amplifying the signal), TGC (Time Gain Compensation, to correct for signal attenuation with depth), depth, and focus. I systematically adjust these parameters to achieve optimal visualization, minimizing artifacts like shadowing and reverberation. Think of this like adjusting the brightness, contrast, and focus on a camera to get the best possible picture. For instance, adjusting the TGC might reveal a hidden structure obscured by bone shadowing.
Gel Coupling: Ensuring adequate gel coupling between the transducer and the skin eliminates air gaps that can interfere with image quality. A proper amount of gel helps transmit the ultrasound waves efficiently.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with different types of guided injections (e.g., nerve blocks, joint injections).
I have extensive experience performing various ultrasound-guided injections, including nerve blocks and joint injections. Each procedure requires a unique understanding of anatomy and technique.
Nerve Blocks: I routinely perform various nerve blocks, such as interscalene brachial plexus blocks, femoral nerve blocks, and popliteal nerve blocks. These procedures require precise needle placement to ensure effective anesthesia while avoiding potential complications like pneumothorax (collapsed lung) or vascular injury. I meticulously identify the nerve using real-time ultrasound guidance, confirming needle placement before injecting the anesthetic.
Joint Injections: I have considerable experience with joint injections in various joints, including shoulder, knee, hip, and wrist. For example, when performing a shoulder injection, I use ultrasound to visualize the joint capsule, avoiding the rotator cuff tendons and ensuring that the medication is precisely deposited into the joint space.
Other Injections: This also includes experience with other injections like trigger point injections, facet joint injections and tendon sheath injections, all requiring precise ultrasound guidance to target specific anatomical structures.
My approach always prioritizes patient safety and comfort. I constantly adapt my technique based on individual patient anatomy and the specific clinical context.
Q 17. How do you handle equipment malfunctions during a procedure?
Equipment malfunctions during a procedure are rare but can be stressful. My response is structured and prioritizes patient safety above all else.
Immediate Assessment: First, I assess the nature and severity of the malfunction. Is it a minor display issue, a transducer problem, or a complete system failure? The extent of the issue will determine my next steps.
Troubleshooting: I attempt basic troubleshooting steps. This could involve checking power supply, cable connections, or trying a different transducer if available. I am familiar with the common causes of malfunctions for different ultrasound machines. I have also been trained to troubleshoot common problems in different brands of equipment.
Escalation: If the problem can’t be resolved quickly, I immediately escalate the issue to the biomedical engineering department or call for assistance from experienced colleagues. Patient safety is never compromised, and the procedure may need to be paused or postponed depending on the circumstances.
Alternative Strategies: In some situations, a minor malfunction may not necessitate immediate termination. I might consider alternative approaches, if feasible and safe, to continue the procedure with modified techniques, ensuring accurate and safe performance of the task.
Documentation: I meticulously document the malfunction, the steps taken to resolve it, and any impact it had on the procedure in the patient’s chart.
Q 18. Describe your experience with image documentation and reporting.
Image documentation and reporting are critical aspects of ultrasound-guided procedures. It’s like keeping a detailed record of a surgical procedure. Accurate documentation protects both the patient and the practitioner.
Image Acquisition: I acquire high-quality images that clearly demonstrate the needle placement, the target anatomy, and the injection process. I use the ultrasound machine’s built-in annotation features to clearly label the images with relevant information such as patient identification, date, time, and the specific procedure performed.
Reporting: My reports are comprehensive and concise, including details of the procedure, the location of the injection, any observed complications, and the patient’s response. I use standardized terminology to ensure clarity and consistency across my reports. The reports are directly integrated into the patient’s electronic medical record.
Storage and Retrieval: All ultrasound images and reports are securely stored in accordance with institutional guidelines, ensuring easy access for future reference and review, in compliance with HIPAA regulations.
Q 19. What are the legal and ethical considerations of ultrasound-guided procedures?
Ultrasound-guided procedures carry significant legal and ethical considerations. It is crucial to adhere strictly to legal and ethical guidelines to ensure patient safety and avoid malpractice.
Informed Consent: Obtaining fully informed consent is paramount. Patients must understand the procedure’s benefits, risks, and alternatives. I ensure the consent process is thorough and documented. This includes explaining potential complications, like hematoma or infection, in clear and understandable language.
Confidentiality: Maintaining patient confidentiality is strictly adhered to, complying with all relevant privacy regulations such as HIPAA. All patient information is handled with utmost care.
Competence: I must maintain and demonstrate a high level of competence, participating in continuous medical education and keeping abreast of the latest advancements in ultrasound techniques. This ensures I am continually improving my skills and following best practices.
Professional Boundaries: Maintaining professional boundaries and acting ethically at all times is vital to avoid potential conflicts of interest or any appearance of impropriety.
Malpractice: Understanding the implications of medical malpractice related to ultrasound-guided procedures and ensuring meticulous attention to detail in all aspects of patient care is paramount in protecting against potential legal issues.
Q 20. How do you ensure accurate patient identification and consent?
Accurate patient identification and informed consent are cornerstones of safe medical practice. Errors can have devastating consequences. My approach to ensure accuracy involves a multi-step verification process.
Multiple Identifiers: I always verify patient identity using at least two independent identifiers – typically, the patient’s name and date of birth – before initiating any procedure. This cross-checking minimizes the risk of misidentification.
Wristband Check: I check the patient’s wristband against their medical record to confirm that the information matches.
Verbal Confirmation: I always verbally confirm the patient’s identity with the patient themselves before proceeding.
Documented Consent: The informed consent process is meticulously documented, ensuring the patient understands the procedure, its risks and benefits, and has voluntarily agreed to proceed. The consent form is signed and witnessed, and a copy is provided to the patient.
This multi-layered approach provides a robust safeguard against errors and ensures that the correct patient receives the correct procedure.
Q 21. Describe your proficiency in using ultrasound equipment from different manufacturers.
I’m proficient in using ultrasound equipment from various manufacturers, including GE, Siemens, Philips, and Sonosite. While the user interfaces and functionalities might differ slightly between brands, the fundamental principles of ultrasound remain consistent.
Adaptability: My experience allows me to quickly adapt to different machine interfaces and optimize image acquisition parameters regardless of the manufacturer. This adaptability ensures efficient workflow and high-quality image acquisition in various clinical settings.
Troubleshooting: Understanding the unique characteristics and potential issues of different ultrasound machines, including their respective software and hardware components, enables efficient troubleshooting, minimizing downtime and ensuring uninterrupted patient care.
Continuous Learning: I actively seek opportunities to maintain and expand my expertise through hands-on training and workshops with different ultrasound systems, ensuring competency across a variety of models.
This broad experience allows me to provide consistent, high-quality care regardless of the equipment available.
Q 22. How do you maintain your skills and knowledge in ultrasound-guided procedures?
Maintaining proficiency in ultrasound-guided procedures requires a multifaceted approach. It’s not a ‘set it and forget it’ skill; continuous learning is paramount.
- Continuing Medical Education (CME): I actively participate in relevant CME courses, workshops, and conferences focusing on advancements in ultrasound technology, new techniques, and best practices. This ensures I stay updated with the latest research and guidelines.
- Hands-on Practice: Regularly performing procedures is crucial. Even experienced professionals benefit from maintaining a consistent caseload. This allows for refinement of technique and problem-solving skills. I actively seek opportunities to perform a variety of procedures to maintain diverse skill sets.
- Case Review and Peer Discussion: I regularly review challenging cases, both successes and complications, with colleagues. These discussions provide valuable learning opportunities and help identify areas for improvement in my technique and decision-making.
- Self-directed Learning: I stay abreast of the latest literature through journals and online resources. This allows me to explore new research and emerging technologies in the field. For example, I recently completed an online module on the application of AI in ultrasound image analysis.
- Mentorship and Collaboration: I actively seek mentorship from experienced colleagues and participate in collaborative research projects. This provides exposure to different perspectives and allows for continuous learning and improvement.
Q 23. What is your experience with different types of ultrasound imaging modes (e.g., B-mode, M-mode, Doppler)?
I am proficient in various ultrasound imaging modes, each offering unique information during procedures.
- B-mode (Brightness mode): This is the most commonly used mode, providing a grayscale anatomical image. It’s essential for visualizing tissue structures, identifying the target area, and guiding needle placement. For example, I use B-mode extensively during biopsies to identify the lesion and ensure accurate needle placement.
- M-mode (Motion mode): M-mode provides a time-motion display, crucial for assessing cardiac activity and visualizing moving structures. While less frequently used in many interventional procedures, it can be vital in situations like pericardiocentesis to monitor cardiac function during the procedure.
- Doppler (Pulsed-wave and Color Doppler): Doppler modes visualize blood flow. Pulsed-wave Doppler measures the velocity of blood flow at a specific point, while color Doppler provides a visual representation of the direction and velocity of blood flow in a larger area. This is invaluable in procedures such as vascular access and interventional radiology to assess vascular patency and identify potential complications.
Understanding the strengths and limitations of each mode is critical for selecting the most appropriate imaging technique for a specific procedure.
Q 24. Explain your understanding of the acoustic window and its importance in procedure success.
The acoustic window refers to the area of the body where ultrasound waves can effectively penetrate and provide a clear image. It’s essentially the ‘window’ through which we ‘see’ the target anatomy. The choice of acoustic window is crucial for procedural success.
Importance: A poor acoustic window leads to suboptimal image quality, obscuring the target anatomy, making accurate needle placement challenging and potentially increasing the risk of complications. For example, a thick layer of subcutaneous fat can significantly impair the acoustic window, making it harder to visualize deeper structures during a liver biopsy.
Choosing the right window: The selection involves considering factors like patient anatomy, the location of the target, and the presence of interfering structures (e.g., gas, bone). Sometimes, manipulating the patient’s position or using different transducer frequencies can optimize the acoustic window. In some cases, alternate access points might be required.
Q 25. How do you assess the depth and location of target structures using ultrasound?
Assessing depth and location relies on several ultrasound features:
- Depth Calibration: The ultrasound machine has a depth scale, allowing us to measure the distance from the transducer to the target. This is often expressed in centimeters.
- Anatomical Landmarks: We use visible anatomical landmarks (e.g., ribs, vessels, organs) as references to determine the target’s precise location. This often involves a combination of systematic scanning and knowledge of regional anatomy.
- Measurement Tools: The ultrasound machine provides tools to measure distances and angles. This allows for precise measurement of the target’s depth and position relative to surrounding structures.
- Image Orientation: Understanding the orientation of the ultrasound image (e.g., transverse, longitudinal) is crucial for accurate depth and location assessment. This requires careful attention to the transducer’s position and the image display.
For instance, during a nerve block, identifying the nerve’s location relative to surrounding muscles and vessels is crucial for safe and effective injection.
Q 26. Describe your experience with advanced ultrasound techniques (e.g., elastography, fusion imaging).
I have experience with several advanced ultrasound techniques that enhance the accuracy and safety of procedures.
- Elastography: This technique assesses tissue stiffness. It helps differentiate between benign and malignant lesions based on their elastic properties. For example, elastography is frequently used in breast biopsies to help distinguish between benign and malignant nodules.
- Fusion Imaging: This integrates ultrasound images with other imaging modalities like MRI or CT. This improves the accuracy of target localization, particularly when the target is difficult to visualize on ultrasound alone. I’ve used fusion imaging in complex cases involving the localization of small lesions or structures close to critical anatomical areas.
These advanced techniques improve diagnostic accuracy, reduce the risk of complications, and enhance the overall procedural outcome.
Q 27. How would you approach a challenging case where the target is difficult to visualize?
When facing a challenging case with poor visualization, a systematic approach is crucial.
- Optimize the Acoustic Window: I would first attempt to optimize the acoustic window by adjusting the patient’s position, using different transducer frequencies, or selecting an alternative access route. Sometimes, using a gel pad with different acoustic properties can also help.
- Employ Advanced Techniques: If necessary, I would incorporate advanced techniques such as elastography or fusion imaging to improve visualization. Fusion imaging, for example, can help when the target is obscured on ultrasound but is clearly visible on another modality, such as MRI.
- Utilize Contrast-Enhanced Ultrasound (CEUS): In some cases, CEUS can be used to enhance the visibility of specific structures or lesions by using contrast agents that improve the visualization of blood vessels or tissue structures.
- Seek Consultation: If the visualization remains poor, I would consult with a colleague for a second opinion or consider referring the patient to a center with more advanced imaging capabilities.
- Patient Safety First: If visualization remains inadequate and safe needle placement cannot be guaranteed, I would prioritize patient safety by postponing the procedure until better visualization is achieved.
The key is to carefully assess the situation, utilize all available resources, and prioritize patient safety.
Key Topics to Learn for Ultrasound-Guided Procedures Interview
- Image Acquisition and Optimization: Understanding transducer selection, image adjustments (gain, depth, frequency), and artifact recognition for optimal visualization.
- Anatomy and Landmark Identification: Mastering the precise identification of anatomical structures relevant to the procedures you’ll be performing. This includes understanding variations in anatomy and how to adapt your approach.
- Needle Guidance Techniques: Proficiency in various needle insertion techniques (e.g., in-plane, out-of-plane), understanding the advantages and limitations of each approach, and adapting based on patient anatomy and procedure requirements.
- Safety Considerations and Complications: Thorough understanding of potential complications (e.g., hematoma, pneumothorax, nerve injury) and strategies for prevention and management. This includes patient preparation and post-procedure monitoring.
- Procedure-Specific Knowledge: Deep dive into the specific procedures you’ll be questioned on. This involves understanding the indications, contraindications, steps involved, and potential complications for each.
- Bioeffects and Safety Regulations: Knowledge of ALARA principle (As Low As Reasonably Achievable) and understanding the potential bioeffects of ultrasound and how to minimize exposure.
- Troubleshooting and Problem Solving: Be prepared to discuss how you would handle technical difficulties during a procedure, such as poor image quality or unexpected anatomical variations. Showcase your problem-solving skills.
- Infection Control and Sterile Technique: Demonstrate understanding of maintaining sterile conditions throughout the procedure to minimize the risk of infection.
Next Steps
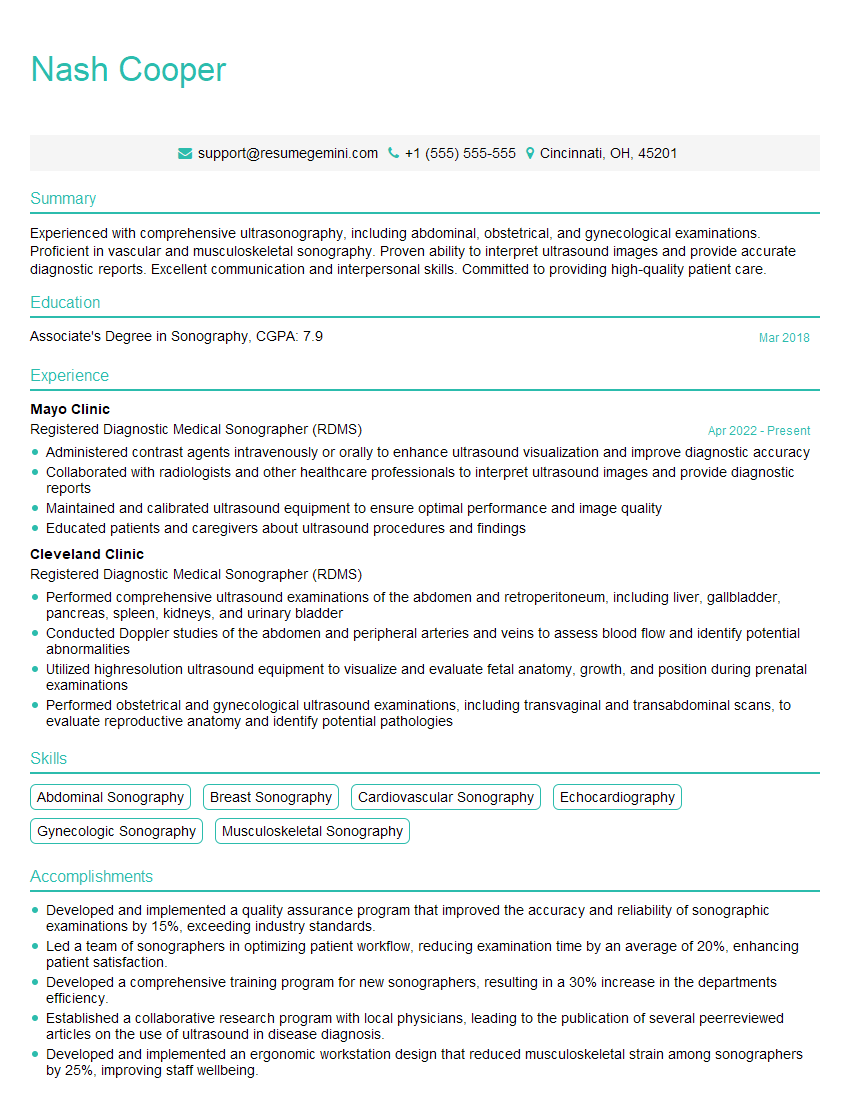
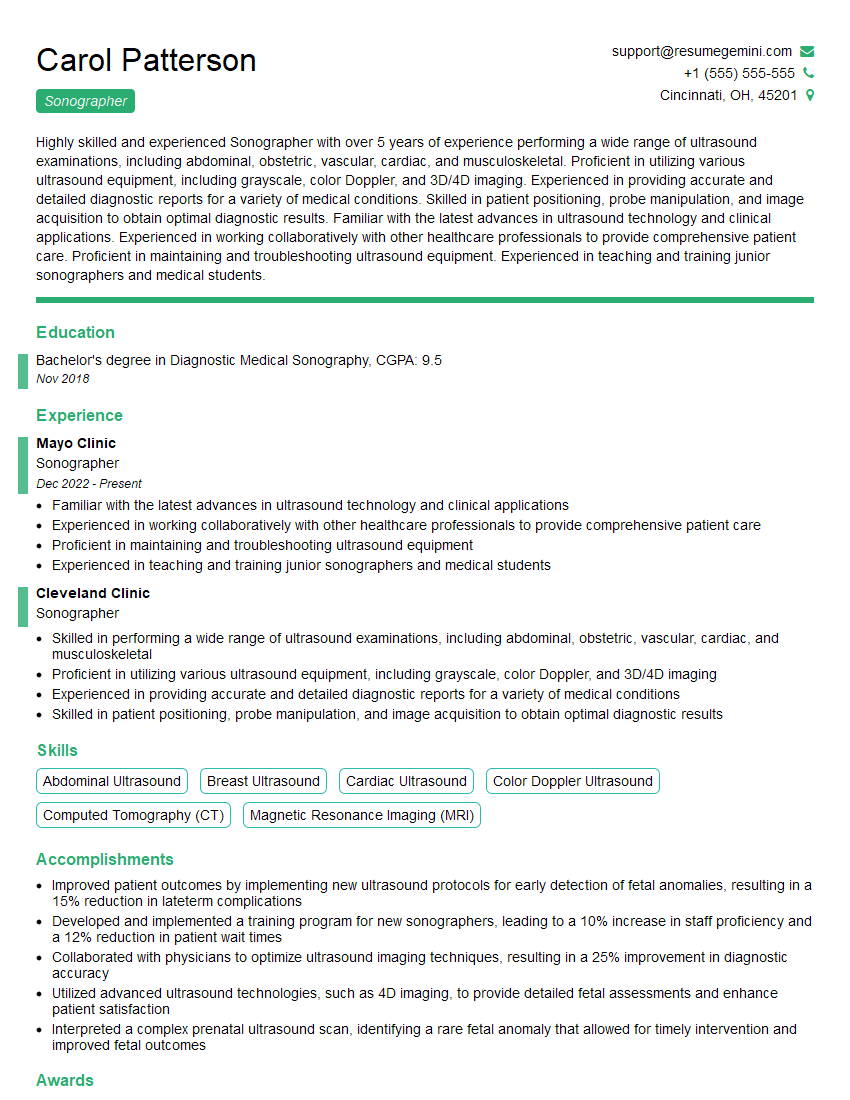
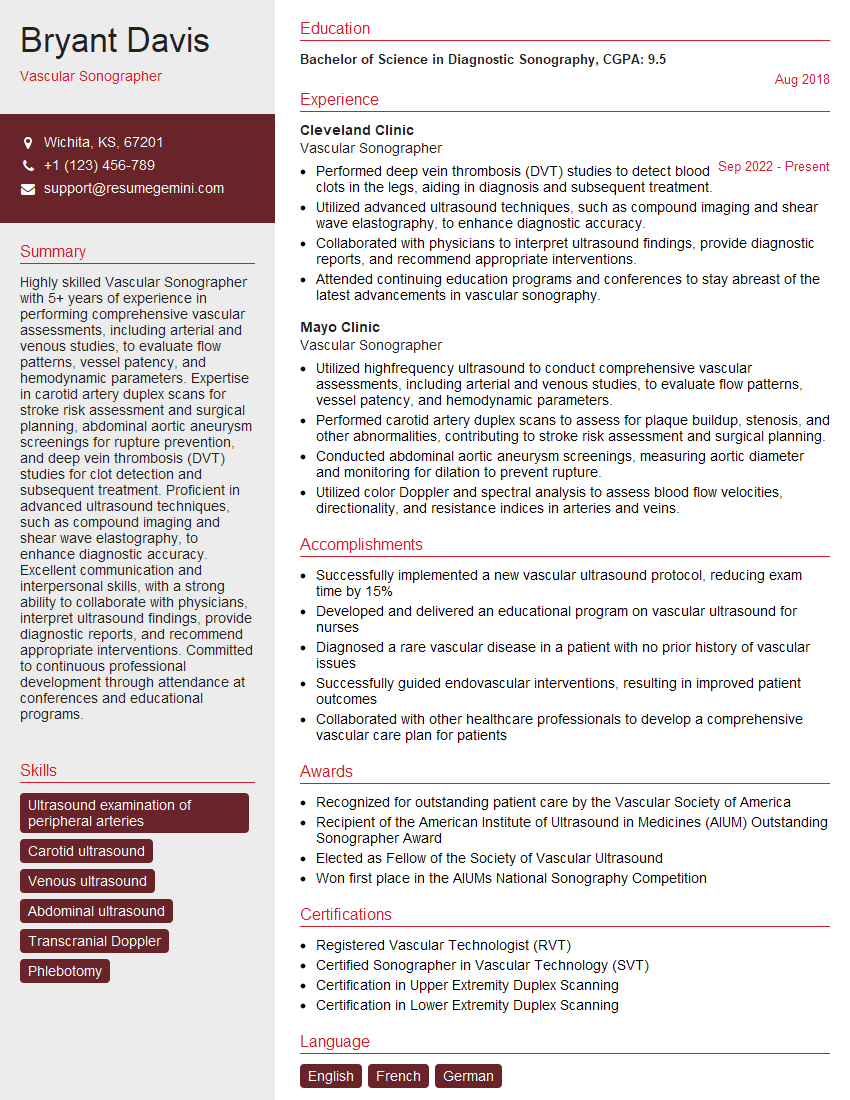
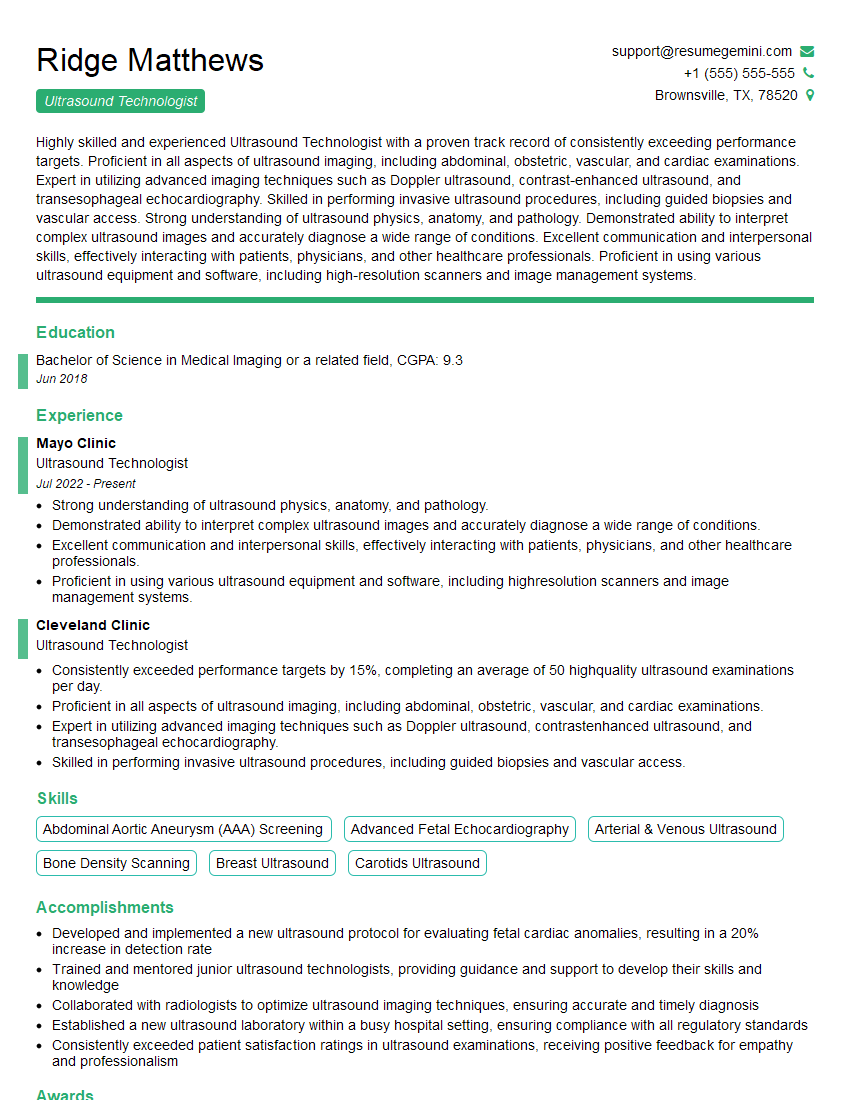
Mastering Ultrasound-Guided Procedures is crucial for career advancement in this dynamic field. It opens doors to specialized roles and significantly enhances your value as a skilled healthcare professional. To maximize your job prospects, creating a strong, ATS-friendly resume is essential. ResumeGemini can help you build a professional and impactful resume that highlights your expertise in Ultrasound-Guided Procedures. Leverage their resources and take advantage of the provided resume examples tailored to this specialized area to significantly improve your chances of landing your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hello,
We found issues with your domain’s email setup that may be sending your messages to spam or blocking them completely. InboxShield Mini shows you how to fix it in minutes — no tech skills required.
Scan your domain now for details: https://inboxshield-mini.com/
— Adam @ InboxShield Mini
Reply STOP to unsubscribe
Hi, are you owner of interviewgemini.com? What if I told you I could help you find extra time in your schedule, reconnect with leads you didn’t even realize you missed, and bring in more “I want to work with you” conversations, without increasing your ad spend or hiring a full-time employee?
All with a flexible, budget-friendly service that could easily pay for itself. Sounds good?
Would it be nice to jump on a quick 10-minute call so I can show you exactly how we make this work?
Best,
Hapei
Marketing Director
Hey, I know you’re the owner of interviewgemini.com. I’ll be quick.
Fundraising for your business is tough and time-consuming. We make it easier by guaranteeing two private investor meetings each month, for six months. No demos, no pitch events – just direct introductions to active investors matched to your startup.
If youR17;re raising, this could help you build real momentum. Want me to send more info?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
Hi, I represent an SEO company that specialises in getting you AI citations and higher rankings on Google. I’d like to offer you a 100% free SEO audit for your website. Would you be interested?
good