Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Ovulation Timing interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Ovulation Timing Interview
Q 1. Explain the different methods for tracking ovulation.
Tracking ovulation involves several methods, each with its own strengths and weaknesses. The goal is to pinpoint the approximate 12-24 hour period when the ovary releases a mature egg, maximizing the chances of conception.
- Ovulation Predictor Kits (OPKs): These home tests detect the surge in luteinizing hormone (LH) that precedes ovulation. They’re easy to use, providing a relatively quick result.
- Basal Body Temperature (BBT) Charting: This method involves taking your temperature every morning before getting out of bed. A slight increase in temperature typically indicates ovulation has occurred. This is a retrospective method, meaning you know you ovulated *after* it’s happened.
- Cervical Mucus Method (CMM): This involves observing changes in your cervical mucus throughout your cycle. The mucus becomes clearer, more stretchy (like egg white), and more abundant around ovulation.
- Ovulation Calendar/Tracking Apps: Based on the length of your menstrual cycles, these tools can estimate your ovulation days. However, their accuracy depends on the regularity of your cycles.
- Ultrasound: A medical professional uses ultrasound to visualize the ovaries and follicles. This is the most accurate method but requires a visit to a doctor or fertility clinic.
Choosing the best method depends on individual preferences, cycle regularity, and access to resources.
Q 2. Describe the hormonal changes that occur during ovulation.
Ovulation is orchestrated by a complex interplay of hormones. The key players include:
- Follicle-Stimulating Hormone (FSH): Stimulates the growth of follicles in the ovary, each containing an egg.
- Estrogen: Produced by the growing follicles, estrogen levels rise throughout the follicular phase, leading to the LH surge.
- Luteinizing Hormone (LH): A surge in LH triggers ovulation, causing the mature follicle to rupture and release the egg.
- Progesterone: After ovulation, the ruptured follicle transforms into the corpus luteum, which produces progesterone. Progesterone prepares the uterine lining for potential implantation of a fertilized egg.
Think of it like a relay race: FSH starts the process, estrogen prepares the way, LH triggers the final event, and progesterone sets the stage for possible pregnancy.
Q 3. What are the signs and symptoms of ovulation?
Recognizing ovulation can be tricky, as signs and symptoms vary from woman to woman. Some common indicators include:
- Mid-cycle pain (Mittelschmerz): A sharp, one-sided pain in the lower abdomen.
- Changes in cervical mucus: As described above, the mucus becomes clear, stretchy, and abundant.
- Slight increase in basal body temperature (BBT): A noticeable temperature shift after ovulation.
- Increased libido: Some women experience a heightened sex drive around ovulation.
- Breast tenderness: Breast swelling or tenderness can be experienced.
It’s important to note that not all women experience all of these symptoms, and some may not experience any at all.
Q 4. How accurate are ovulation predictor kits (OPKs)?
OPKs are generally accurate in detecting the LH surge, but their accuracy isn’t perfect. Factors like following instructions carefully, timing of testing, and individual hormone levels can affect results. While they can significantly improve the chances of identifying the fertile window, they don’t guarantee pinpointing ovulation to the exact hour.
Studies suggest that OPKs are around 80-90% accurate in detecting the LH surge. However, remember that ovulation occurs 12-36 hours *after* the surge is detected, adding a degree of uncertainty.
Q 5. Explain the concept of the fertile window.
The fertile window refers to the period during a woman’s menstrual cycle when she is most likely to conceive. It’s not just the day of ovulation; sperm can survive in the female reproductive tract for several days, and the egg can remain viable for about 12-24 hours after release. Therefore, the fertile window typically spans several days, usually around five days – from approximately five days before ovulation to the day of ovulation itself.
Understanding the fertile window is crucial for couples trying to conceive or avoid pregnancy. Accurate ovulation prediction methods are essential for maximizing or minimizing chances of conception.
Q 6. What are the limitations of basal body temperature (BBT) charting?
BBT charting, while a valuable tool, has several limitations:
- Retrospective Method: You only know you ovulated *after* it has happened, making it less useful for actively trying to conceive during that specific cycle.
- Requires Consistency: Accurate charting demands taking your temperature at the same time each day, every day, which can be challenging for some individuals.
- Affected by External Factors: Illness, stress, alcohol consumption, and insufficient sleep can skew BBT readings, leading to inaccurate interpretations.
- Not Suitable for Irregular Cycles: BBT charting is less reliable for women with irregular menstrual cycles.
Despite these limitations, BBT charting, when done meticulously, can provide valuable insights into overall cycle patterns and hormonal balance, even if not solely for predicting ovulation in a given cycle.
Q 7. How does cervical mucus change during ovulation?
Cervical mucus changes dramatically throughout the menstrual cycle, reflecting hormonal fluctuations. These changes are a key indicator of ovulation.
- Before Ovulation: Mucus is typically thick, sticky, and scant.
- Around Ovulation: Mucus becomes clear, slippery, stretchy (like egg white), abundant, and more easily visible. This texture is optimal for sperm passage.
- After Ovulation: Mucus becomes thick and sticky again.
Think of it as nature’s way of creating a highway for sperm to reach the egg. The change in mucus consistency is a natural, reliable indicator, offering a simple, non-invasive way to track fertility.
Q 8. Describe the role of LH in ovulation.
LH, or luteinizing hormone, plays a pivotal role in triggering ovulation. Think of it as the final ‘go’ signal for the egg release. Throughout the menstrual cycle, LH levels gradually rise, but a significant surge in LH is what initiates the rupture of the mature follicle in the ovary, releasing the egg into the fallopian tube. This surge typically occurs 24-36 hours before ovulation. Without this LH surge, ovulation wouldn’t happen.
For example, imagine a volcano. The build-up of pressure (rising LH) is the precursor to the eruption (ovulation). The LH surge is the crucial trigger for that eruption, releasing the egg – the ‘magma’ – from the ovary.
Q 9. What is the typical length of the menstrual cycle?
The typical length of a menstrual cycle is around 28 days, but this can vary significantly between individuals. A normal cycle can range from 21 to 35 days. It’s measured from the first day of bleeding (menstruation) to the first day of the next period. It’s important to note that regularity is key; significant variation beyond this range could indicate an underlying issue.
Consider this: Some women might have a very regular 26-day cycle, while others might experience cycles ranging from 28 to 32 days. Both are considered normal, as long as there’s consistent predictability. However, a woman who experiences cycles that are sometimes 21 days and sometimes 40 days needs to consult with a healthcare professional to investigate.
Q 10. How can stress affect ovulation?
Stress can significantly disrupt the intricate hormonal balance needed for regular ovulation. Chronic stress can affect the hypothalamus, a key brain region that regulates the hormonal cascade leading to ovulation. This disruption can lead to irregular cycles, anovulation (absence of ovulation), or even amenorrhea (absence of menstruation). This is because stress triggers the release of cortisol, a hormone that can interfere with the production of other reproductive hormones, such as GnRH (gonadotropin-releasing hormone), FSH (follicle-stimulating hormone), and LH.
For instance, a woman experiencing significant job-related stress might notice her cycles becoming irregular or experiencing missed periods, demonstrating the direct link between stress and reproductive health. Managing stress through techniques such as exercise, yoga, or mindfulness might help restore regular ovulation.
Q 11. Explain the impact of age on ovulation.
Age has a profound effect on ovulation and fertility. As women age, the number of eggs in their ovaries decreases, and the quality of those eggs declines. This leads to a decreased chance of ovulation and conception. The decline in ovarian reserve typically accelerates as a woman approaches her late 30s and 40s, culminating in menopause when ovulation ceases entirely. This natural decline in fertility is a gradual process, but the impact becomes more noticeable in the years leading up to menopause.
Imagine a flower garden. In youth, the garden is full of vibrant, healthy flowers (eggs). As time passes, the flowers become fewer and less vibrant, decreasing the likelihood of a successful bloom (pregnancy).
Q 12. What are some common causes of anovulation?
Anovulation, the absence of ovulation, can stem from various causes. These include hormonal imbalances (like polycystic ovary syndrome or PCOS, hypothyroidism, or hyperprolactinemia), weight issues (both underweight and overweight), stress, certain medical conditions (like pituitary tumors or thyroid disorders), and intense physical activity. Certain medications can also interfere with ovulation.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder characterized by irregular periods, excess androgen production, and ovarian cysts.
- Hypothyroidism: An underactive thyroid gland leading to hormonal imbalances.
- Hyperprolactinemia: Elevated levels of prolactin, a hormone primarily associated with lactation.
Understanding the underlying cause is crucial for effective treatment.
Q 13. How can ovulation disorders be diagnosed?
Diagnosing ovulation disorders involves a combination of methods. A detailed medical history and physical examination form the foundation. This is followed by tracking menstrual cycles and using ovulation prediction kits (OPKs) to detect the LH surge. Ultrasound examinations can visualize the ovaries and follicles to assess follicular development and ovulation. Blood tests measure hormone levels (FSH, LH, estradiol, progesterone) to identify hormonal imbalances. Basal body temperature (BBT) charting, while less precise, can also provide insights into ovulation patterns.
For example, a woman with irregular periods might undergo blood tests to rule out hormonal imbalances like PCOS. Ultrasound scans can confirm the presence or absence of follicular development and ovulation.
Q 14. Describe various treatments for ovulation disorders.
Treatment for ovulation disorders is tailored to the underlying cause. Lifestyle modifications, such as weight management, stress reduction, and regular exercise, can be effective in some cases. Medication plays a vital role in many others. Clomiphene citrate is a common medication that stimulates ovulation by increasing the production of FSH and LH. Other medications, like letrozole or gonadotropins (injectable hormones), may be used for those who don’t respond to clomiphene. In cases of severe anovulation or underlying conditions, assisted reproductive technologies (ART), such as intrauterine insemination (IUI) or in-vitro fertilization (IVF), might be considered.
Each treatment plan is carefully individualized depending on the woman’s specific situation and underlying condition.
Q 15. What are the ethical considerations surrounding ovulation timing technologies?
Ethical considerations surrounding ovulation timing technologies primarily revolve around informed consent, accuracy, and potential misuse. Patients must fully understand the methods used, their limitations, and potential side effects before using any ovulation timing technology. The accuracy of these methods varies, and over-reliance on a single method can lead to inaccurate predictions and frustration. Additionally, there are ethical concerns regarding the use of these technologies for sex selection or other purposes that may be considered discriminatory or socially problematic. For example, using ovulation prediction kits solely to conceive a child of a specific gender raises serious ethical questions. Responsible use requires clear communication between healthcare providers and patients to ensure ethical application.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain how ovulation timing is used in fertility treatments.
Ovulation timing is crucial in fertility treatments. Precise timing of intercourse or intrauterine insemination (IUI) is essential for maximizing the chances of conception. In IUI, for instance, the sperm is introduced into the uterus around the time of ovulation, increasing the likelihood that sperm will encounter the egg. In IVF (in-vitro fertilization), ovulation timing is managed through medications to control the development and release of multiple eggs, increasing the number of eggs available for fertilization in the lab. Accurate ovulation timing allows for optimized timing of procedures, maximizing the efficiency and success of the treatment.
Q 17. How can you counsel a patient about ovulation timing methods?
Counseling a patient about ovulation timing methods requires a thorough understanding of their individual circumstances, medical history, and desired outcome. I begin by explaining the various methods available, such as the calendar method, basal body temperature (BBT) charting, ovulation predictor kits (OPKs), and ultrasound. We discuss the pros and cons of each method, considering factors like cycle regularity, ease of use, and cost. For instance, while the calendar method is simple, it’s less reliable for those with irregular cycles. I also address the patient’s concerns and questions, ensuring they feel comfortable and confident in using their chosen method. Finally, I emphasize that these methods are tools to increase the likelihood of conception, not guarantees, and that persistence and patience are essential. A realistic expectation is crucial to avoid disappointment. For example, I might say, ‘While tracking your ovulation can significantly improve your chances, it doesn’t guarantee pregnancy in every cycle.’
Q 18. Describe the difference between calendar method, BBT, and OPK.
The calendar method estimates ovulation based on the length of past menstrual cycles. It’s simple but unreliable for women with irregular cycles. Basal body temperature (BBT) charting involves taking your temperature daily upon waking. A slight rise in temperature usually indicates ovulation has occurred, but this method identifies ovulation *after* it has happened. Ovulation predictor kits (OPKs) detect the surge in luteinizing hormone (LH) in urine, which usually precedes ovulation by 24-36 hours. OPKs provide a more timely prediction compared to BBT, making them a more popular choice. Think of it like this: the calendar method is like guessing the arrival time of a train with an unreliable schedule, BBT is like seeing the train leave the station, and OPKs give you a heads-up before the train arrives.
Q 19. How do you interpret a patient’s ovulation tracking data?
Interpreting a patient’s ovulation tracking data involves looking for consistent patterns and key indicators. For BBT charting, I look for a sustained increase in temperature post-ovulation. With OPKs, I look for the peak LH surge. Combining data from multiple methods helps confirm ovulation timing. For example, a positive OPK followed by a rise in BBT strongly suggests successful ovulation. Irregular patterns or the absence of expected changes can signal ovulatory dysfunction, requiring further investigation and potentially medical intervention.
Q 20. What are the potential risks associated with ovulation induction?
Ovulation induction, using medications to stimulate ovulation, carries potential risks, including ovarian hyperstimulation syndrome (OHSS), multiple pregnancies, and ectopic pregnancy (pregnancy outside the uterus). OHSS can range from mild discomfort to severe symptoms requiring hospitalization. Multiple pregnancies increase risks for both mother and babies. Ectopic pregnancies can be life-threatening. These risks are discussed extensively with patients before initiating treatment, and careful monitoring is essential throughout the process.
Q 21. How do you address patient concerns about ovulation timing?
Addressing patient concerns about ovulation timing requires empathy, patience, and clear communication. I start by actively listening to their concerns, validating their feelings, and providing reassurance. If they are experiencing anxiety or frustration due to unsuccessful attempts, I explain that conception can take time and that these methods improve but don’t guarantee success. I might share success stories of other patients, emphasizing the importance of persistence. If their concerns stem from a lack of understanding, I provide additional education on the chosen method and its limitations. If there are underlying medical issues that may be contributing to their difficulty conceiving, I will refer them to a specialist for appropriate evaluation and treatment.
Q 22. Explain the role of ultrasound in assessing ovulation.
Ultrasound plays a crucial role in confirming ovulation by visualizing changes in the ovaries. Specifically, transvaginal ultrasound allows for a detailed view of the ovaries, enabling the detection of a dominant follicle (the fluid-filled sac containing the egg) as it matures and then the visualization of the corpus luteum, the structure left behind after ovulation.
How it works: The follicle grows steadily during the menstrual cycle, reaching a size of 18-24mm just before ovulation. The ultrasound can track this growth. After ovulation, the follicle collapses and transforms into the corpus luteum, which can also be seen on ultrasound. The presence of a corpus luteum is a strong indicator that ovulation has occurred.
Example: A patient undergoing fertility treatment might have regular ultrasound scans to monitor follicle growth and predict the precise timing of ovulation for timed intercourse or intrauterine insemination (IUI).
Q 23. How do you calculate the fertile window using different methods?
Calculating the fertile window requires understanding that sperm can survive for up to 5 days in the female reproductive tract and that the egg lives for approximately 12-24 hours after ovulation. Several methods exist:
- Calendar Method (Rhythm Method): This involves tracking menstrual cycle lengths for several months to identify the shortest and longest cycles. The fertile window is estimated by subtracting 18 days from the shortest cycle length and subtracting 11 days from the longest cycle length. This is a less accurate method, particularly for those with irregular cycles.
- Basal Body Temperature (BBT) Charting: This method tracks your body temperature each morning before getting out of bed. A slight increase in temperature after ovulation signals that it has occurred. This method is best used retrospectively, as it only confirms ovulation *after* it’s happened.
- Ovulation Predictor Kits (OPKs): These home tests detect the surge in luteinizing hormone (LH) that typically occurs 24-36 hours before ovulation. A positive test indicates that ovulation is likely to occur soon. This method is more proactive than BBT charting but can yield false positives or negatives.
- Ultrasound Monitoring: As mentioned earlier, ultrasound provides the most accurate assessment of ovulation by directly visualizing follicular growth and the presence of a corpus luteum.
Example: A patient with regular 28-day cycles might estimate their fertile window using the calendar method (28-18 = day 10 and 28-11 = day 17, resulting in a fertile window from day 10 to day 17). However, using OPKs and BBT charting would provide more precise timing.
Q 24. What is the impact of irregular cycles on ovulation timing?
Irregular cycles significantly complicate ovulation prediction. When cycles are irregular, the timing of ovulation is unpredictable, making it challenging to pinpoint the fertile window. The length of the cycle can vary greatly from month to month, rendering methods like the calendar method unreliable.
Impact: Irregular cycles often stem from hormonal imbalances, such as polycystic ovary syndrome (PCOS), or other underlying medical conditions. This unpredictability makes conception more difficult, as the timing of intercourse is less likely to coincide with ovulation. Fertility tracking methods become less effective, requiring more advanced techniques like ultrasound monitoring to accurately determine when ovulation is occurring.
Example: A patient with irregular cycles ranging from 25 to 40 days will find it nearly impossible to reliably predict her fertile window using only the calendar method. She will likely benefit from using OPKs in conjunction with BBT charting, or even ultrasound monitoring to improve chances of conception.
Q 25. How do you differentiate between true ovulation and false positives?
Differentiating between true ovulation and false positives requires a multi-faceted approach. False positives can occur with OPKs due to factors like stress, hormonal fluctuations, or certain medications. False positives with BBT charting can result from inaccurate temperature readings or illness.
True Ovulation Indicators: The most reliable indicators are the visualization of a dominant follicle and then a corpus luteum on ultrasound, a sustained rise in BBT, and a positive OPK followed by a temperature shift. The absence of a corpus luteum on ultrasound, an inconsistent temperature rise, or a positive OPK without subsequent temperature rise suggest a false positive.
Example: A positive OPK followed by a clear rise in BBT *and* confirmation of a corpus luteum on ultrasound strongly supports true ovulation. Conversely, a positive OPK without a temperature rise or evidence of a corpus luteum on ultrasound suggests a false positive.
Q 26. Discuss the role of technology in improving ovulation prediction.
Technology has significantly improved ovulation prediction accuracy and convenience. Several technological advancements have transformed how we approach ovulation timing:
- Ovulation predictor kits (OPKs): These are now more sensitive and easier to use, providing clear results.
- Smartphone apps: These apps integrate various tracking methods (BBT, cycle length, OPKs) to provide personalized predictions and insights.
- Wearable sensors: Some devices track physiological parameters like basal body temperature and subtle hormonal changes to provide more accurate estimations of the fertile window.
- Ultrasound technology: Improvements in imaging techniques allow for clearer and more reliable visualization of follicular development and ovulation.
- Artificial intelligence (AI): AI algorithms can analyze data from various sources (OPKs, BBT, ultrasound) to offer more accurate and personalized ovulation predictions.
Example: Using a fertility tracking app that integrates data from OPKs and BBT charting can provide a more precise prediction than using either method alone. The use of AI algorithms within such apps is continuously refining the accuracy of ovulation prediction.
Q 27. Explain the difference between spontaneous and induced ovulation.
The key difference lies in how ovulation is triggered.
- Spontaneous Ovulation: This is the natural process where the ovaries release an egg under the body’s own hormonal regulation. This is the typical way ovulation occurs in healthy women of reproductive age.
- Induced Ovulation: This involves using medication to stimulate the ovaries to release one or more eggs. This is commonly used in fertility treatment for women who are not ovulating regularly or who require assistance to conceive.
Example: A woman with regular menstrual cycles experiences spontaneous ovulation. In contrast, a woman undergoing in-vitro fertilization (IVF) undergoes induced ovulation with the use of medications like clomiphene citrate or gonadotropins to stimulate multiple follicle growth and egg release.
Q 28. How would you explain the concept of ovulation timing to a patient with limited medical knowledge?
Imagine your ovaries as tiny treasure chests, and each month one of them releases a precious pearl – an egg. Ovulation is the moment when this egg is released. It’s a short window of opportunity for getting pregnant, because the egg only lives for about a day.
To maximize your chances of getting pregnant, we need to figure out when this egg is released. We can do that by looking at your cycle (the time between your periods), tracking your temperature, using special tests to detect hormonal changes, or even using ultrasound. Once we know when you’re ovulating, we can time intercourse to increase your chances of conceiving.
It’s like planning a party—you wouldn’t invite guests if you didn’t know when you’d be home. Similarly, we need to know when the egg is ready to be ‘met’ by sperm. We use different methods to help figure out the best time for trying to get pregnant.
Key Topics to Learn for Ovulation Timing Interview
- Understanding the Ovarian Cycle: Master the physiological processes involved, including follicle development, hormone fluctuations (FSH, LH, estrogen, progesterone), and the role of the hypothalamus and pituitary gland.
- Methods for Ovulation Prediction: Become proficient in various methods such as basal body temperature charting, ovulation predictor kits (OPKs), cervical mucus monitoring, and calendar methods. Understand their limitations and accuracy.
- Clinical Applications: Explore the practical applications of ovulation timing in fertility awareness, family planning, assisted reproductive technologies (ART), and the management of irregular cycles.
- Interpreting Data and Identifying Patterns: Practice analyzing data from different ovulation prediction methods. Develop the ability to identify patterns and predict ovulation accurately.
- Troubleshooting and Problem-Solving: Learn to identify and address potential challenges in accurately predicting ovulation, such as irregular cycles, hormonal imbalances, and the impact of stress or illness.
- Ethical Considerations: Understand the ethical implications of ovulation timing, including informed consent, patient autonomy, and the responsible use of reproductive technologies.
- Technological Advancements: Stay updated on the latest advancements in ovulation prediction technology and their impact on clinical practice.
Next Steps
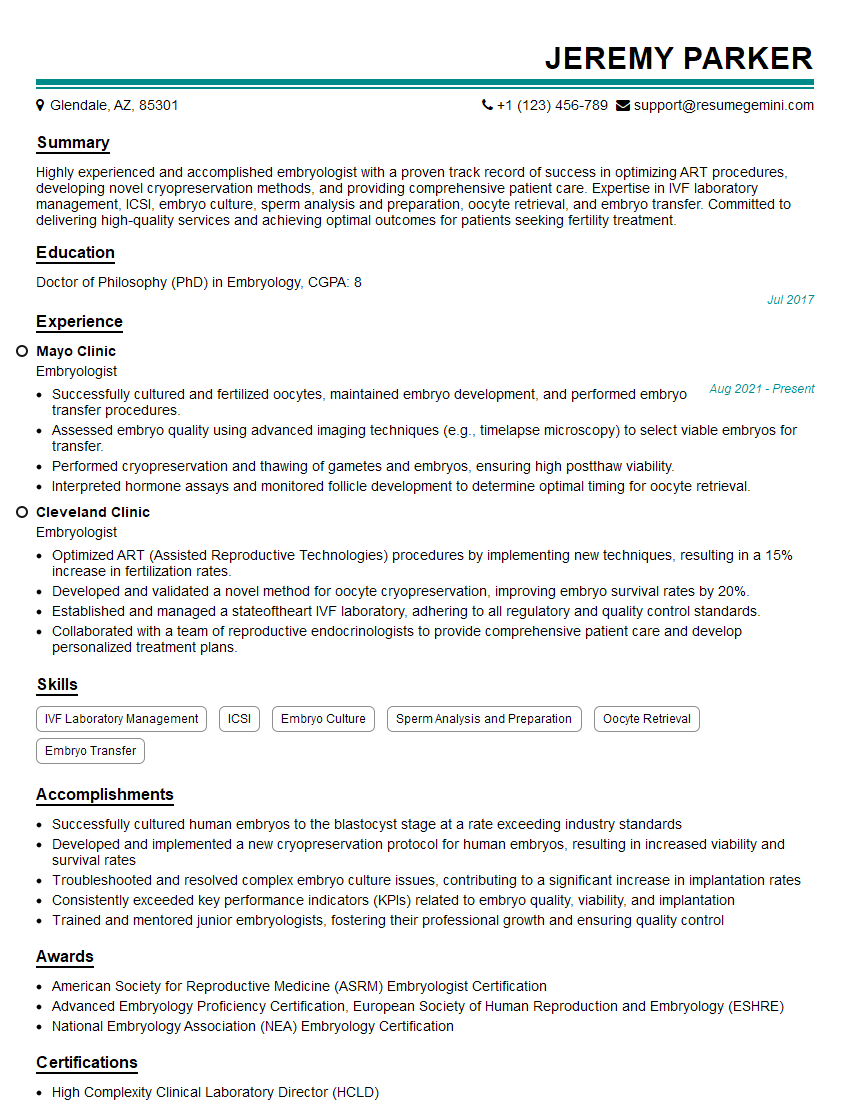
Mastering ovulation timing opens doors to exciting career opportunities in reproductive healthcare, research, and related fields. A strong understanding of these concepts is crucial for career advancement and demonstrating your expertise to potential employers. To maximize your job prospects, invest time in crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored to Ovulation Timing to guide you in showcasing your unique qualifications. Take advantage of these resources to present yourself in the best possible light and secure your dream job!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good