Preparation is the key to success in any interview. In this post, we’ll explore crucial Semen Storage and Handling interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Semen Storage and Handling Interview
Q 1. Describe the optimal temperature and conditions for semen storage.
Optimal semen storage requires maintaining a precise balance of temperature and conditions to ensure the viability and fertilizing capacity of the sperm cells. The ideal temperature is generally considered to be -196°C, achieved through immersion in liquid nitrogen. This ultra-low temperature halts virtually all biological activity, preventing degradation. Beyond temperature, maintaining sterility is paramount. This involves using sterile containers, equipment, and employing strict aseptic techniques throughout the entire process to avoid contamination that could damage or kill the sperm.
Think of it like putting precious seeds in a deep freeze – you need the right temperature to prevent them from sprouting prematurely and you need to protect them from any pests or mold that could destroy them.
Q 2. Explain the process of semen cryopreservation.
Semen cryopreservation, or freezing, is a complex process aimed at preserving sperm for future use. It’s a multi-step procedure starting with sample collection and initial evaluation of sperm concentration, motility, and morphology. Next, a cryoprotective agent (CPA) is added to the semen sample. This CPA acts as an antifreeze, preventing the formation of ice crystals that could damage the sperm cells during the freezing process. The sample is then gradually cooled, often using a controlled-rate freezer, to allow the sperm cells to adapt to the decreasing temperatures. Finally, the straws containing the frozen semen are stored in liquid nitrogen tanks at -196°C for long-term preservation.
Imagine it like carefully packing a delicate cake to withstand a long journey – you need special materials (CPA) and a slow, controlled approach to prevent damage.
Q 3. What are the common cryoprotective agents used in semen freezing?
Cryoprotective agents (CPAs) are essential for protecting sperm cells during freezing. They work by reducing the formation of ice crystals and minimizing cellular damage caused by dehydration. Common CPAs include glycerol, dimethyl sulfoxide (DMSO), and egg yolk. Glycerol is a widely used, relatively inexpensive CPA, but it can have some toxic effects at higher concentrations. DMSO offers better protection but carries a higher risk of toxicity. Egg yolk serves as a protective buffer adding additional benefits to the process. Often, a combination of these CPAs is used to optimize protection and minimize adverse effects. The choice of CPA depends on the species of semen being frozen and the specific protocol being used.
Think of CPAs as a specialized ‘antifreeze’ that keeps your valuable cargo (sperm) safe from damage during the freeze.
Q 4. How do you assess semen quality before and after cryopreservation?
Semen quality assessment is critical before and after cryopreservation. Pre-freeze evaluation involves analyzing several key parameters, including sperm concentration (number of sperm per milliliter), motility (percentage of moving sperm), morphology (shape and structure of sperm), and viability (percentage of live sperm). These parameters are assessed using specialized equipment like a hemocytometer and computer-aided semen analysis (CASA) systems. Post-thaw evaluation follows the same parameters to assess the impact of freezing and thawing on sperm quality. A significant drop in motility and viability after thawing is often observed, indicating potential damage during the process. The degree of damage can impact the success rate of subsequent fertilization attempts.
Imagine it like a pre- and post-flight check on an airplane. We need to make sure everything is in optimal condition before and after the ‘flight’ to ensure the journey was successful.
Q 5. What are the potential risks and challenges associated with semen storage?
Semen storage, while offering invaluable benefits, also presents several risks and challenges. These include the potential for contamination by bacteria or fungi during handling, leading to decreased sperm quality or complete loss. Improper freezing or thawing techniques can also result in significant sperm damage. There’s also the risk of ice crystal formation which is devastating to sperm. Furthermore, long-term storage necessitates robust quality control measures and reliable monitoring of liquid nitrogen levels to prevent sample loss due to temperature fluctuations. Finally, the ethical considerations surrounding the storage, access, and use of frozen semen also represent a significant challenge in clinical settings.
It’s like storing valuable antiques – you need secure storage conditions, insurance, and strict protocols to avoid loss or damage.
Q 6. Describe the different methods for semen thawing.
Semen thawing is a crucial step in semen processing, requiring careful attention to detail. The most common method involves a rapid thaw in a water bath set at 37°C. The straw containing the frozen semen is submerged in the water bath until completely thawed. This rapid warming helps to minimize the formation of large ice crystals which can damage sperm cells. Other techniques, such as using a specialized electric thawing device that rapidly warms the straws are also available but require specialized equipment. The speed of thawing significantly impacts sperm survival. Too slow a thaw increases the risk of ice crystal damage while too rapid a thaw can also cause cellular stress. Finding the ideal balance is critical for maximizing sperm survival and function.
Think of it as carefully defrosting a frozen meal – you need to do it slowly and evenly to prevent it from getting ruined.
Q 7. Explain the importance of maintaining a sterile environment during semen handling.
Maintaining a sterile environment is paramount throughout semen handling to prevent contamination by bacteria, fungi, or viruses. These contaminants can severely compromise sperm quality, reduce fertilization rates, and potentially cause infection. Aseptic techniques are crucial at every step, from sample collection to storage. This involves using sterile equipment such as gloves, syringes, and containers, working in a clean environment (ideally a laminar flow hood), and adhering to strict protocols for disinfection and sterilization. Even a single moment of lapse in sterility can have catastrophic consequences. This stringent approach is designed to safeguard sperm quality and ensure the success of subsequent reproductive procedures.
Maintaining sterility is like operating in a surgical theater – even the smallest contaminant can have significant consequences. It’s about diligence and attention to detail to protect the biological material.
Q 8. How do you prevent contamination during semen processing?
Preventing contamination during semen processing is paramount to ensuring sample viability and preventing transmission of infectious agents. It’s a multi-step process involving strict adherence to aseptic techniques throughout the entire procedure, from collection to cryopreservation.
- Cleanliness: The entire processing area must be meticulously cleaned and disinfected using appropriate agents, such as a 10% bleach solution, before and after each procedure. All equipment and work surfaces should be thoroughly cleaned and disinfected.
- Personal Protective Equipment (PPE): Personnel must wear appropriate PPE, including gloves, lab coats, and masks, at all times during semen handling. Gloves should be changed frequently.
- Aseptic Technique: All procedures must be performed using strict aseptic techniques, minimizing the introduction of microorganisms. This includes working under a laminar flow hood for many procedures.
- Equipment Sterilization: Equipment that comes into contact with the semen sample must be sterilized using appropriate methods (autoclaving, chemical sterilization) before use. Single-use, sterile materials are highly preferable whenever possible.
- Regular Monitoring: Regular monitoring and quality control procedures should be implemented to identify and prevent contamination. Environmental monitoring of the laboratory is crucial.
Imagine a surgeon performing an operation – the level of cleanliness and meticulousness is similar when handling precious semen samples.
Q 9. What are the regulatory guidelines for semen storage and handling?
Regulatory guidelines for semen storage and handling vary depending on the country and specific application (e.g., assisted reproductive technology, animal breeding). However, some common themes include:
- Good Laboratory Practices (GLP): Adherence to GLP is essential, ensuring standardized procedures and record-keeping.
- Quality Control (QC): Strict QC measures are required throughout the entire process, from collection to storage, ensuring semen quality and viability.
- Safety Regulations: Regulations addressing the safe handling of human biomaterials, including appropriate disposal methods, are crucial to prevent exposure to infectious agents.
- Personnel Training: Thorough training of personnel in aseptic techniques, safety protocols, and quality control is mandatory. Regular refresher training should also be implemented.
- Record Keeping: Detailed and accurate record-keeping is vital, documenting each step of the process, including donor information, processing techniques, and storage conditions. This is critical for traceability and legal compliance.
- Licensing and Accreditation: Facilities often require specific licenses and/or accreditation to operate legally and ensure adherence to quality standards.
These regulations are designed to protect both the patient and the integrity of the sample.
Q 10. Describe the different types of semen storage containers and their uses.
Semen storage containers are designed to maintain optimal conditions for sperm survival and are usually cryogenic-compatible for long-term storage. Different containers serve different purposes:
- Straws (0.25-0.5 mL): Small, individual straws are commonly used for cryopreservation, allowing for easy individual handling and thawing. They are often made of plastic and sealed to prevent contamination.
- Cryovials (1-2 mL): Cryovials are small, screw-cap tubes typically made of plastic and used for both short-term and long-term storage in liquid nitrogen or vapor phase freezers. These offer more volume compared to straws.
- Freezing containers: Designed specifically for controlled freezing of semen samples by reducing the rate of temperature decline. These containers are typically made of materials that facilitate slow freezing process.
- Storage tanks/dewars: Large containers used for long-term storage of cryopreserved semen in liquid nitrogen. They come in varying sizes to accommodate different sample volumes.
The choice of container depends on the volume of semen, the storage method, and the desired length of storage.
Q 11. What are the quality control measures implemented to ensure semen viability?
Quality control measures are critical for ensuring semen viability and ensuring that the semen meets the standards set by the governing regulatory bodies. These measures are implemented throughout the entire process:
- Pre-freeze evaluation: This involves assessing sperm concentration, motility, morphology, and viability before freezing. This helps predict post-thaw results and identify potential issues early on. Commonly used methods include computer-assisted semen analysis (CASA).
- Freezing protocols: Using standardized, optimized freezing protocols is essential to minimize damage during the freezing and thawing processes. These protocols dictate the specific cryoprotectants and freezing rates.
- Post-thaw evaluation: After thawing, the sperm sample is reassessed for motility, viability, and morphology to determine the success of the cryopreservation process.
- Regular maintenance of equipment: Regular checks of the liquid nitrogen tanks and freezers are needed to prevent fluctuations in temperature, which could affect the semen quality.
- Staff training and competency assessment: Ongoing training and assessment of the staff involved in semen handling and storage is needed to reduce human errors.
Think of it like baking a cake. Each step of the process needs to be precise, or the final product will be subpar.
Q 12. How do you troubleshoot issues related to low post-thaw motility?
Low post-thaw motility is a common problem in semen cryopreservation. Troubleshooting requires a systematic approach, investigating several potential causes:
- Improper freezing technique: Incorrect freezing rate, use of inappropriate cryoprotectants, or inadequate equilibration time can damage sperm during freezing. Review and optimize the freezing protocol.
- Poor semen quality before freezing: If the semen sample had low motility prior to freezing, post-thaw motility will naturally also be low. Select samples of high initial quality.
- Suboptimal thawing technique: Too rapid or slow thawing can damage sperm. Optimize the thawing procedure.
- Contamination: Bacterial contamination can significantly reduce sperm motility. Ensure strict aseptic techniques throughout the entire process.
- Cryoprotectant toxicity: Excessive exposure to cryoprotectants can be toxic to sperm. Optimize the concentration and exposure time to the cryoprotectant.
- Storage conditions: Improper storage temperature or exposure to fluctuations in temperature can reduce sperm motility. Maintain appropriate storage conditions.
Troubleshooting is like detective work. You need to systematically eliminate each potential cause until you find the culprit.
Q 13. Explain the process of semen labeling and documentation.
Semen labeling and documentation are essential for sample traceability and legal compliance. Every step should be meticulously documented.
- Donor Identification: The label should clearly identify the donor, using a unique identifier (e.g., donor number). Complete anonymity is maintained when appropriate.
- Collection Date and Time: The exact date and time of semen collection should be recorded on the label and in the database.
- Processing Date and Time: The date and time of each processing step (e.g., dilution, freezing) should also be recorded.
- Storage Location: The location where the sample is stored should be clearly identified on both the label and the database, with details of the storage container.
- Quality Control Results: The results of all quality control tests (e.g., pre- and post-thaw analysis) must be meticulously documented and linked to the sample.
- Database Management: A comprehensive database system is needed to manage the large volumes of information generated during the semen storage and handling process, allowing for easy retrieval of information when needed.
Accurate labeling and documentation are like building blocks. Each component must be present for the overall structure to stand strong. Failure to document appropriately can lead to serious implications.
Q 14. What are the safety protocols for handling human semen?
Safety protocols for handling human semen are critical to prevent exposure to infectious agents and to comply with relevant regulations. These protocols include:
- Universal Precautions: Treat all semen samples as potentially infectious. Always use appropriate PPE.
- Aseptic Techniques: Maintain strict aseptic techniques to prevent contamination.
- Sharps Disposal: Needles and other sharps should be disposed of in appropriate containers.
- Waste Disposal: Semen samples and related waste should be disposed of according to the relevant regulations.
- Spill Management: A clear protocol must be in place for dealing with accidental spills of semen. It must be neutralized and cleaned following guidelines.
- Training and Education: Personnel must receive adequate training on safe handling practices and emergency procedures.
- Biohazard Labeling: All containers should be clearly labeled with biohazard symbols to alert others to potential risks.
Think of handling semen similar to handling any biohazardous material. Care and caution are paramount.
Q 15. How do you manage semen samples with low sperm concentration?
Managing semen samples with low sperm concentration requires a multifaceted approach focusing on maximizing the chances of successful fertilization. This often involves techniques to concentrate the sample and optimize the insemination process.
First, we utilize techniques like centrifugation to increase sperm density. This involves spinning the sample at a specific speed to pellet the sperm cells at the bottom of the tube, allowing us to remove the seminal plasma and resuspend the sperm in a smaller volume, effectively increasing the concentration. We carefully monitor the process to avoid damaging the sperm during this procedure.
Second, we might employ techniques like swim-up or density gradient centrifugation which further separate motile (moving) sperm from immotile sperm and seminal fluid debris. This results in a higher concentration of healthy, motile sperm, crucial for successful fertilization. These techniques improve the quality of the sperm rather than simply increasing the raw number.
Finally, intra-cytoplasmic sperm injection (ICSI) might be considered if other methods fail. ICSI is a specialized procedure where a single sperm is injected directly into an egg, bypassing the need for high sperm motility and concentration normally required for natural fertilization.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the procedures for quarantine and disposal of semen samples.
Quarantine and disposal of semen samples are critical aspects of maintaining biosafety and adhering to ethical guidelines. Any sample suspected of contamination, exhibiting unusual characteristics, or from a donor with a newly discovered infectious disease must be immediately quarantined.
Quarantine procedures typically involve isolating the sample in a designated area with clear labeling indicating its quarantine status. Detailed records of the sample, including the reason for quarantine, are meticulously maintained. Strict adherence to infection control protocols is essential throughout the quarantine period.
Disposal of semen samples is conducted according to established safety protocols and regulations. Typically, this involves autoclaving (sterilization using high-pressure steam) followed by disposal as medical waste. The process ensures inactivation of any potentially infectious agents. Detailed records of sample disposal, including the method used and the date of disposal, are meticulously documented to ensure traceability and compliance.
Q 17. What are the ethical considerations related to semen storage?
Ethical considerations surrounding semen storage are multifaceted and complex. Informed consent is paramount. Donors must fully understand the procedures, risks, and implications of semen storage, including potential future uses of their genetic material. Anonymity and confidentiality of donors must be strictly maintained, unless otherwise agreed upon and documented.
Another key consideration is the duration of storage. Clear guidelines are needed to establish reasonable storage periods that balance the needs of individuals seeking fertility treatment with the ethical implications of long-term storage and disposal. Furthermore, ethical guidelines must address issues related to access to stored samples, ensuring appropriate authorization and preventing unauthorized use.
The disposal of unused or unwanted samples presents another set of ethical challenges. Clear guidelines and procedures must be established to ensure respectful and compliant disposal in line with regulatory requirements and the donor’s wishes, wherever possible.
Q 18. How do you maintain accurate records of semen samples?
Maintaining accurate records of semen samples is crucial for traceability, quality control, and legal compliance. A robust database system, either electronic or paper-based (though electronic is strongly preferred), is essential. This system should uniquely identify each sample with a sequential identification number, alongside details of the donor (while maintaining anonymity where needed) and the date and time of collection.
The database should also include information about the sample’s characteristics, including volume, sperm concentration, motility, morphology, and any other relevant analytical data. Records of all handling procedures, including cryopreservation, thawing, and any transfers, must be carefully documented. Furthermore, any events related to sample quarantine or disposal should also be meticulously recorded.
Regular audits and quality control checks are essential to ensure the accuracy and completeness of the records. Strict adherence to data privacy and security regulations is paramount to protect the confidentiality of the donors.
Q 19. Explain the importance of proper training in semen handling techniques.
Proper training in semen handling techniques is paramount to ensure sample integrity, prevent contamination, and maintain the safety of both the personnel handling the samples and the recipients. Training should cover aseptic techniques to minimize the risk of bacterial contamination, which can significantly affect sperm viability and fertility potential.
Detailed instruction on the proper use and maintenance of laboratory equipment, such as centrifuges, cryopreservation systems, and microscopes, is critical. The training should also cover the interpretation of semen analysis results and the identification of abnormalities. This ensures that personnel can accurately assess sample quality and take appropriate actions.
Furthermore, training should include the proper handling of hazardous materials and the application of relevant safety protocols. Regular refresher courses and competency assessments are essential to ensure that personnel remain proficient in all aspects of semen handling and analysis. A well-trained staff is the cornerstone of a successful and ethical semen processing laboratory.
Q 20. Describe the different types of equipment used in a semen analysis laboratory.
A semen analysis laboratory employs a range of sophisticated equipment. This includes microscopes, both light and phase-contrast, for visualizing sperm morphology and motility. Automated semen analyzers provide objective assessments of sperm concentration, motility, and morphology, significantly increasing efficiency and reducing subjectivity.
Centrifuges are used for concentrating sperm samples, while cryopreservation systems, including freezers and liquid nitrogen tanks, are essential for storing samples at ultra-low temperatures. Incubators are used to maintain optimal temperature and humidity for sperm culture. Specialized equipment like micro-manipulators might be present for advanced procedures like ICSI.
Finally, the lab needs equipment for sample preparation and handling, including pipettes, tubes, and other consumables, along with data management and analysis software to maintain detailed records and process the large amounts of data generated. The specific equipment used might vary based on the lab’s size and capabilities.
Q 21. What are the limitations of current semen cryopreservation techniques?
Current semen cryopreservation techniques, while effective, are not without limitations. Cryopreservation, the process of freezing sperm for long-term storage, inevitably leads to some degree of sperm damage. Ice crystal formation during freezing and thawing can disrupt cell membranes, affecting sperm viability, motility, and morphology.
The cryoprotectants used to protect sperm during freezing can also be toxic to the sperm cells at high concentrations. Optimizing the concentration and type of cryoprotectant remains an active area of research. Furthermore, the success rate of cryopreservation varies depending on factors such as the initial sperm quality, the age of the donor, and the specific cryopreservation protocol used.
Research continues to explore improvements in cryopreservation techniques, including the development of novel cryoprotectants, optimized freezing and thawing protocols, and the use of advanced vitrification techniques, which aim to reduce ice crystal formation and improve post-thaw sperm survival and function.
Q 22. How do you calculate sperm concentration and motility?
Calculating sperm concentration and motility involves analyzing a semen sample under a microscope. Sperm concentration, or sperm count, refers to the number of sperm present in a milliliter (mL) of semen. This is typically determined using a hemocytometer, a specialized counting chamber, where a known volume of diluted semen is examined. The number of sperm counted is then extrapolated to determine the concentration per mL. The formula is essentially: (Number of sperm counted) x (Dilution factor) / (Volume of sample examined in mL) = Sperm Concentration (million/mL).
Motility, on the other hand, refers to the percentage of sperm that are actively moving. We assess motility by observing the sample under a microscope and categorizing sperm based on their movement: progressive motility (moving in a straight line), non-progressive motility (moving but not in a straight line), and immotility (not moving at all). A percentage is calculated for each category, providing a comprehensive motility profile. For instance, a report might state: Progressive motility: 40%, Non-progressive motility: 20%, Immotility: 40%.
Both concentration and motility are critical indicators of semen quality and fertility potential. Low values in either can significantly impact a couple’s chances of natural conception.
Q 23. What are the effects of cryopreservation on sperm DNA integrity?
Cryopreservation, or freezing, of sperm can impact DNA integrity. The process involves exposing the sperm to potentially damaging conditions, including ice crystal formation and oxidative stress. Ice crystals can physically damage the sperm DNA, causing strand breaks and fragmentation. Oxidative stress, resulting from the production of reactive oxygen species during freezing and thawing, can also lead to DNA damage. The extent of this damage varies depending on the cryopreservation protocol used – the specific freezing and thawing rates, cryoprotectant agents used (like glycerol or egg yolk), and the quality of the initial sample.
We assess DNA integrity using techniques such as the Sperm Chromatin Structure Assay (SCSA) or the TUNEL assay, which measure DNA fragmentation. While some DNA damage is unavoidable, the goal is to minimize it using optimized cryopreservation techniques. Factors like sample preparation, the concentration of cryoprotective agents, and controlled freezing rates all play crucial roles in mitigating DNA damage.
In a clinical setting, we often counsel patients about the potential risks of cryopreservation to DNA integrity, especially if they are concerned about genetic conditions that could be passed on to offspring. The use of high-quality cryopreservation protocols reduces the risk and improves the chances of successful outcome after thawing.
Q 24. Describe the process of semen sample preparation for IUI.
Semen sample preparation for intrauterine insemination (IUI) is a crucial step to maximize the chances of fertilization. The process begins with a semen analysis to assess the sperm parameters. The aim is to obtain a concentrated, highly motile sperm suspension for insemination. This usually involves several steps:
- Liquefaction: The semen sample is allowed to liquefy at room temperature (typically for 30-60 minutes). This allows the semen to become less viscous, making processing easier.
- Washing and Density Gradient Centrifugation (DGC): This is the most important part for IUI sample preparation. DGC separates sperm based on their motility and morphology from seminal plasma components (which can contain substances that are harmful to sperm or the fertilization process). The sperm is layered onto a density gradient medium in a centrifuge tube and spun. Highly motile sperm pellet at the bottom, while debris and less motile sperm remain on top.
- Swim-up Technique: An alternative to DGC, the swim-up technique involves layering the liquefied semen over a culture medium. Motile sperm swim up into the medium, separating from the less motile sperm and seminal plasma. This is less efficient than DGC, but gentler on sperm.
- Final Preparation: After either DGC or swim-up, the concentrated sperm pellet is resuspended in a suitable medium and counted again. The final sperm concentration and motility are assessed before IUI.
The specific protocol used might vary based on the laboratory’s methods and the quality of the initial sample. The goal is to obtain a pellet of highly motile, morphologically normal sperm ready for immediate insemination.
Q 25. Explain the role of a cryopreservation system in semen storage.
A cryopreservation system is essential for safe and effective long-term storage of semen. It involves a combination of equipment and protocols that control the rate of cooling and freezing to prevent the formation of damaging ice crystals within the sperm cells. This system typically comprises the following components:
- Controlled-rate freezer: This device precisely controls the rate at which the semen sample is cooled, typically at a rate of -1°C to -2°C per minute, ensuring slow, controlled freezing. This prevents the formation of large, damaging ice crystals.
- Cryo-containers (e.g., liquid nitrogen tanks): These containers store the frozen semen at ultra-low temperatures (-196°C) in liquid nitrogen. They maintain a stable temperature, ensuring long-term preservation of the sperm.
- Cryoprotective agents: These substances, such as glycerol, are added to the semen sample before freezing. They help to protect the sperm from damage during the freezing and thawing processes. The selection and concentration are critical for optimal cryoprotection.
- Monitoring systems: These systems continuously monitor the temperature within the cryostorage containers to ensure that the samples are maintained at the optimal temperature for long-term viability.
The cryopreservation system is designed to minimize sperm damage during the freezing and thawing processes, allowing for the long-term preservation of fertility, which is crucial for assisted reproductive technologies and various applications in both human and animal reproduction.
Q 26. How do you manage discrepancies in semen analysis results?
Discrepancies in semen analysis results can arise due to several factors: pre-analytical (sample collection and handling), analytical (laboratory technique), or post-analytical (data entry and interpretation). Managing these requires a systematic approach:
- Repeat analysis: The first step is usually to repeat the semen analysis to verify the initial results. Ideally, a new sample should be collected to eliminate any issues related to sample collection or handling.
- Assess pre-analytical variables: Review the sample collection method, transport conditions, and the time elapsed between collection and analysis. Inaccurate information or inadequate handling can significantly affect the results.
- Review analytical variables: If discrepancies persist after repeating the analysis, the laboratory’s methods and equipment need to be investigated for potential errors. This may involve checking the calibration of equipment, reviewing the technicians’ techniques, and ensuring quality control measures are adhered to.
- Consult with specialists: If the discrepancy is significant or remains unexplained, consulting with a reproductive endocrinologist or andrologist is essential. They can provide expert advice and potentially recommend further investigations, such as hormonal testing or genetic analysis, to identify the underlying cause.
- Documentation: Meticulous documentation of all analysis steps, including any inconsistencies, is crucial for transparency and to facilitate resolution of the discrepancies.
Addressing discrepancies helps ensure accurate diagnostic information is provided, leading to appropriate clinical management and reproductive choices.
Q 27. What are the best practices for maintaining semen sample traceability?
Maintaining semen sample traceability is paramount for ensuring patient safety and the integrity of any procedures using these samples. A robust traceability system utilizes unique identifiers and comprehensive documentation at every step.
- Unique identification numbers: Each sample must be assigned a unique alphanumeric identifier that follows the sample from collection to storage and any eventual use.
- Detailed laboratory information management system (LIMS): A LIMS is essential for managing sample information electronically. This software tracks the sample’s journey, including the date and time of collection, donor identity (protected according to regulations), analysis results, storage location, and any subsequent procedures performed using the sample.
- Chain of custody: A chain of custody document meticulously tracks who handled the sample at every stage and when. This ensures accountability and verifies the sample’s integrity.
- Barcoding and RFID tagging: Barcoding or Radio-Frequency Identification (RFID) tagging allows for efficient tracking and prevents human error. These can be scanned at each stage of handling.
- Secure storage: The storage location must be secure and appropriately monitored to prevent unauthorized access or sample mishandling.
Strict adherence to these best practices ensures accurate record-keeping, prevents sample mix-ups, and allows for easy retrieval of sample history if needed.
Q 28. Describe your experience with different semen cryopreservation protocols.
My experience encompasses various semen cryopreservation protocols, each tailored to specific needs and the type of sample. These include slow-freezing protocols, using controlled-rate freezers as described above, and more recently, vitrification protocols. Slow freezing uses a gradual reduction in temperature, which allows the cells to gradually dehydrate. Vitrification, in contrast, involves extremely rapid cooling, achieving a glassy state that essentially bypasses ice crystal formation. Both have their advantages and disadvantages.
Slow freezing is a well-established technique, generally considered gentler on the sperm, but it is more time-consuming. Vitrification is faster and often requires less cryoprotectant, but it can be more technically challenging and requires specialized equipment. The choice depends on the intended use. For example, slow freezing is often preferred for long-term storage in assisted reproduction, while vitrification might be preferable for short-term storage and applications needing immediate use post-thaw.
In my experience, the use of various cryoprotectants (glycerol, dimethylsulfoxide, egg yolk) along with optimizing the freezing and thawing rates has a significant impact on the post-thaw sperm quality. I’ve worked extensively with various modifications of these methods, constantly seeking to optimize the protocols to achieve higher post-thaw motility, viability, and DNA integrity.
Key Topics to Learn for Semen Storage and Handling Interview
- Semen Collection Techniques: Understanding various collection methods, their advantages and disadvantages, and the impact on semen quality.
- Semen Evaluation: Mastering the assessment of semen parameters (volume, concentration, motility, morphology) and interpreting the results to determine sample quality.
- Cryopreservation Techniques: Learning about the process of freezing and thawing semen, including the use of cryoprotectants and optimal freezing protocols.
- Storage Conditions and Monitoring: Understanding the importance of maintaining optimal temperature, humidity, and other environmental factors during storage, and the methods used for monitoring these parameters.
- Quality Control and Assurance: Implementing procedures to ensure the quality and integrity of stored semen samples, including proper labeling, record-keeping, and inventory management.
- Safety and Hygiene Protocols: Adhering to strict hygiene and safety procedures to prevent contamination and ensure the safety of both personnel and samples.
- Troubleshooting Common Issues: Developing problem-solving skills to address potential issues such as low motility, poor morphology, or contamination during storage and handling.
- Regulatory Compliance: Familiarity with relevant regulations and guidelines pertaining to semen storage and handling in your specific region or industry.
- Advanced Techniques: Exploring advanced technologies and methods in semen preservation, such as vitrification or improved cryoprotectants.
- Ethical Considerations: Understanding the ethical implications of semen storage and handling, including donor anonymity and consent.
Next Steps
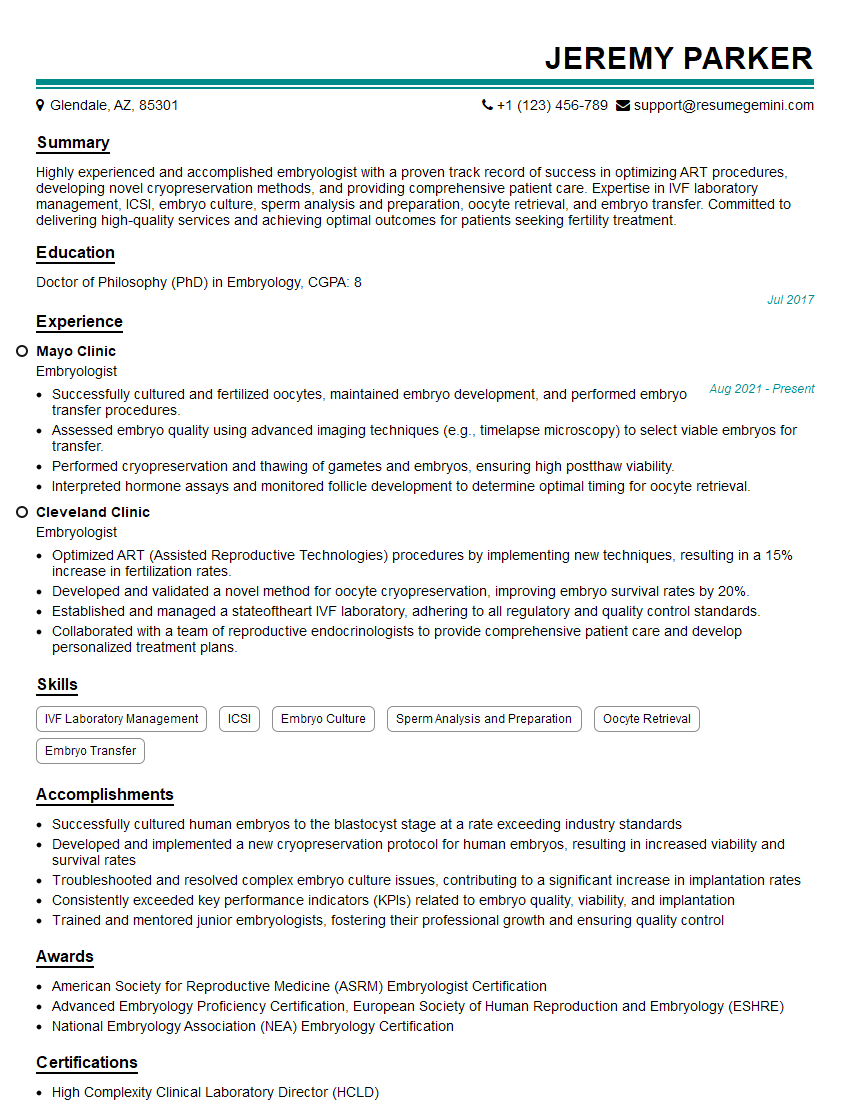
Mastering semen storage and handling is crucial for career advancement in fields such as animal breeding, assisted reproductive technologies, and research. A strong understanding of these principles demonstrates valuable technical expertise and commitment to quality. To significantly boost your job prospects, create a professional, ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a compelling resume that showcases your qualifications. Examples of resumes tailored to Semen Storage and Handling are available to help guide your resume creation process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
good